Low Seroprevalence of Measles-Specific IgG in Children of Three Ethnic Groups from Mexico: Influence of Age, Sex, Malnutrition and Family Size
Abstract
1. Introduction
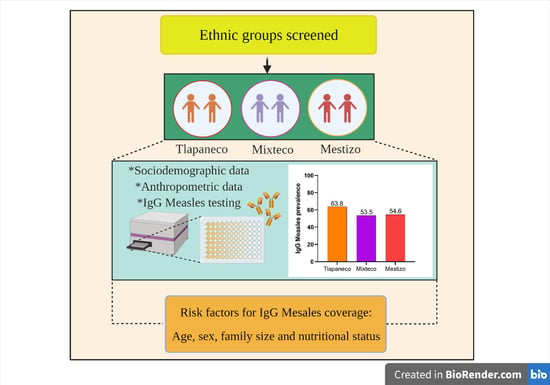
2. Materials and Methods
2.1. Study Population
2.2. Data Collection
2.3. Laboratory Measurements
2.4. Statistical Analysis
3. Results
3.1. Anthropometrical Characteristics According Ethnic Group
3.2. Demographic Characteristics According to Ethnic Group
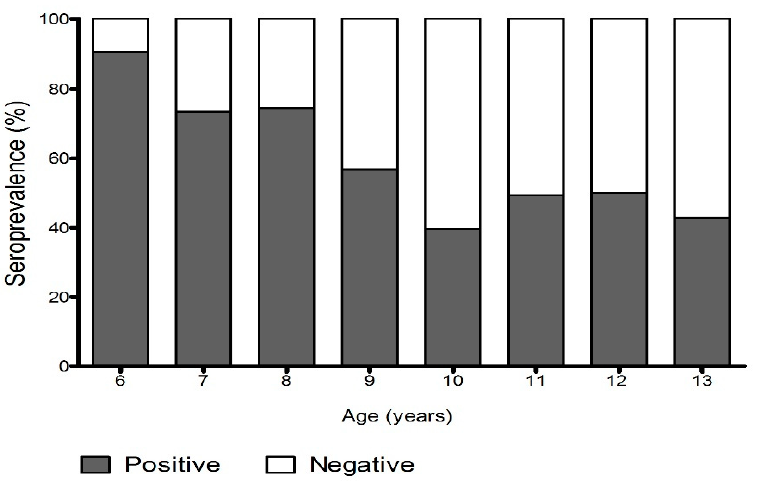
3.3. Seroprevalence Assessment to Measles Antibodies
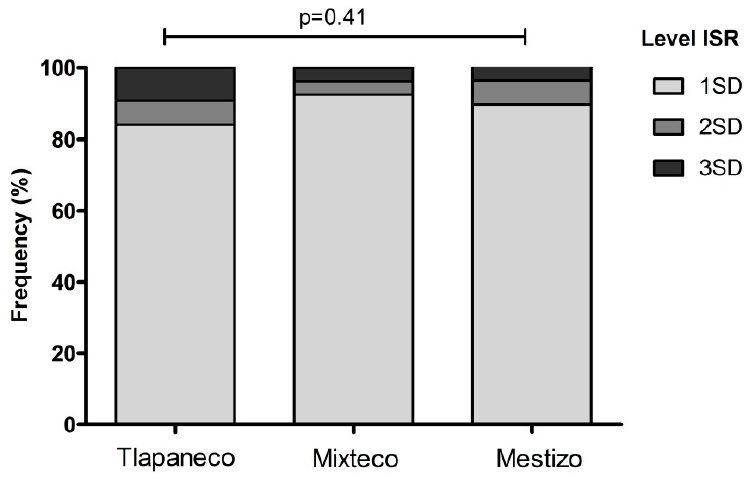
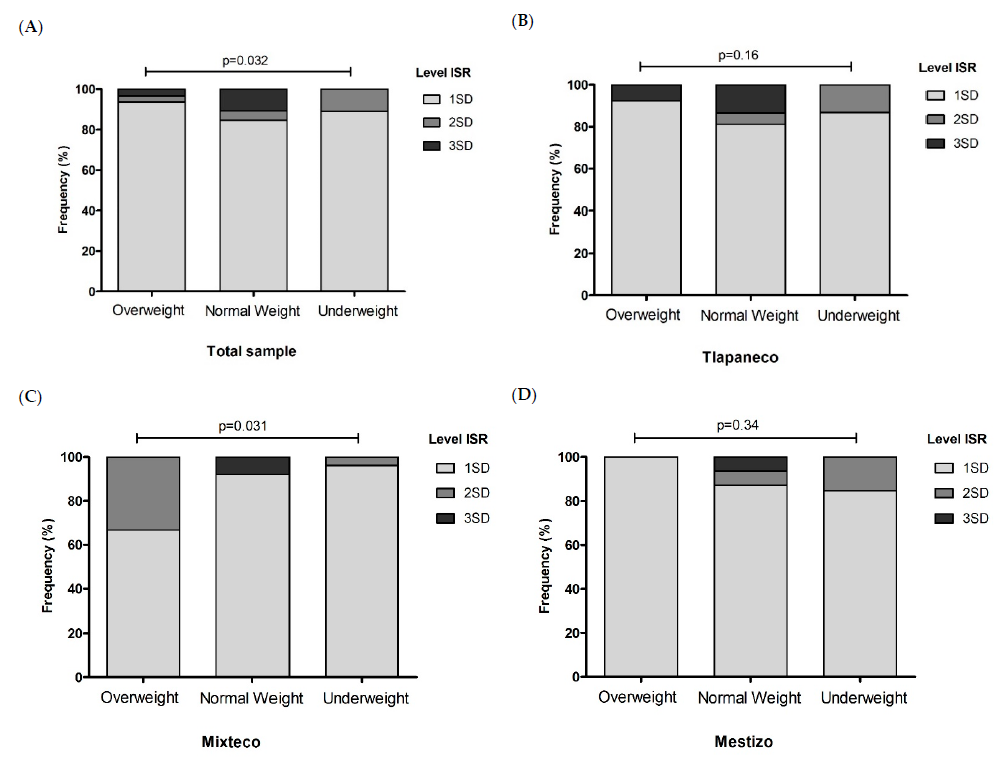
3.4. Levels of Measles Antibodies and the Relationship with Age and Weigh Status in the Ethnic Groups
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Griffin, D. Measles Virus. In Fields Virology, 6th ed.; Wolters Kluwer Health Adis (ESP), 2013; Volume 1. [Google Scholar]
- Uzicanin, A.; Zimmerman, L. Field effectiveness of live attenuated measles-containing vaccines: A review of published literature. J. Infect. Dis. 2011, 204, S133–S148. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Measles-Global Situation. 2019. Available online: https://www.who.int/csr/don/26-november-2019-measles-global_situation/en/ (accessed on 18 January 2020).
- Pan American Health Organization. 55th Directing Council. 68th Session of the Regional Committee of WHO for the Americas. Plan of Action for Maintaining Measles, Rubella, and Congenital Rubella Syndrome Elimination in the Region of the Americas: Final Report. 2016. Available online: https://www.paho.org/hq/dmdocuments/2016/CD55-INF-10-e.pdf (accessed on 18 January 2020).
- Pan American Health Organization. Measles: Epidemiological Alerts and Updates. 2019. Available online: https://www.paho.org/hq/index.php?option=com_topics&view=rdmore&cid=2183&Itemid=40899&lang=es (accessed on 6 June 2020).
- European Centre for Disease Prevention and Control. Monthly Measles and Rubella Monitoring Report. April 2020. Period covered: 1 March 2019–29 February 2020. Available online: https://www.ecdc.europa.eu/sites/default/files/documents/measles-rubella-monthly-report-april-2020.pdf (accessed on 6 June 2020).
- Situación Epidemiológica de Sarampión. Aviso Epidemiológico CONAVE/01/2019/SARAMPION 15 de febrero del 2019. Available online: https://www.gob.mx›cms›attachment›file›AE-Sarampion-15022019 (accessed on 30 August 2019).
- Santos, J.I.; Nakamura, M.A.; Godoy, M.V.; Kuri, P.; Alvarez, C.L.; Coyer, R.T. Measles in Mexico, 1941–2001: Interruption of Endemic Transmission and Lessons Learned. J. Infect. Dis. 2004, 189, S243–S250. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Gómez, J.; Valdespino, J.J.; Olaiz-Fernández, G.; Arias-Toledo, E.; Sepúlveda, J. Measles serologic survey in Mexican children: Evidence for its elimination in Mexico. Salud Publica. Mex. 2007, 49, S370–S376. [Google Scholar] [CrossRef]
- Díaz-Ortega, J.L.; Cruz-Hervert, L.P.; Ferreira-Guerrero, E.; Ferreyra-Reyes, L.D.; Delgado-Sánchez, G.; García-García, M.L. Vaccination Coverage and Proportion of Incomplete Vaccination Schedule in Children Under Seven Years of Age in Mexico. Salud Publica. Mex. 2018, 60, 338–346. [Google Scholar] [CrossRef] [PubMed]
- Campos-Navarro, R.; Peña-Sánchez, E.Y.; Maya, A.P. A Critical Examination of Public Policies Related to Indigenous Health, Traditional Medicine, and Interculturality in Mexico (1990–2016). Salud Colect. 2017, 13, 443–455. [Google Scholar] [CrossRef][Green Version]
- Sánchez-Pérez, H.J.; Hernán, M.A.; Ríos-González, A.; Arana-Cedeño, M.; Navarro, A.; Ford, D.; Micek, M.A.; Brentlinger, P. Malnutrition Among Children Younger Than 5 Years-Old in Conflict Zones of Chiapas, Mexico. Am. J. Public. Health 2007, 97, 229–232. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control. Measles Outbreaks Still Ongoing in 2018 and Fatalities Reported from Four Countries. 2018. Available online: http://ecdc.europa.eu/en/news-events/measles-outbreaks-still-ongoing-2018-and-fatalities-reported-four-countries (accessed on 18 June 2020).
- Siani, A. Measles Outbreaks in Italy: A Paradigm of the Re-Emergence of Vaccine-Preventable Diseases in Developed Countries. Prev. Med. 2019, 121, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez, J.P.; Rivera-Dommarco, J.; Shamah-Levy, T.; Villalpando-Hernández, S.; Franco, A.; Cuevas-Nasu, L.; Romero-Martínez, M.; Hernández-Ávila, M. Encuesta Nacional de Salud y Nutrición 2012; Resultados Nacionales; Instituto Nacional de Salud Pública: Cuernavaca, México, 2012. [Google Scholar]
- Díaz-Ortega, J.L.; Ferreira-Guerrero, E.; Trejo-Valdivia, B.; Téllez-Rojo, M.M.; Ferreyra-Reyes, L.; Hernández-Serrato, M.; Montoya-Rodríguez, A.A.; García-García, L. Vaccination Coverage in Children and Adolescents in Mexico: Vaccinated, Under Vaccinated and Non Vaccinated. Salud Publica. Mex. 2013, 55, S289–S299. [Google Scholar]
- Secretaria de Salud y Asistencia. Cobertura de Vacunación con Esquema Completo por Institución 2014. Available online: https://www.gob.mx/cms/uploads/attachment/file/265939/Coberturas_2014 (accessed on 12 March 2020).
- Colson, K.E.; Zúñiga-Brenes, P.; Ríos-Zertuche, D.; Conde-Glez, C.J.; Gagnier, M.C.; Palmisano, E.; Ranganathan, D.; Usmanova, G.; Salvatierra, B.; Nazar, A.; et al. Comparative Estimates of Crude and Effective Coverage of Measles Immunization in Low-Resource Settings: Findings from Salud Mesoamérica 2015. PLoS ONE 2015, 10, e0130697. [Google Scholar] [CrossRef]
- Cruz-Romero, E.V.; Pacheco-Ríos, A. Causes of Failure and Delay of Primary Immunization Schedule in Children Treated at the Federico Gomez Children’s Hospital of Mexico. Aten. Fam. 2013, 20, 6–11. [Google Scholar] [CrossRef]
- Bárcenas-López, R.M.; Curiel-Reyes, R.; Caballero-Hoyos, R.; Villaseñor-Sierra, A. Low Vaccine Coverage in Indigenous Migrant Boys and Girls. Salud Publica. Mex. 2012, 54, 361–362. [Google Scholar] [CrossRef]
- Bester, J.C. Measles and Measles Vaccination: A Review. JAMA Pediatr. 2016, 170, 1209–1215. [Google Scholar] [CrossRef]
- Moss, W.J. Measles. Lancet 2017, 390, 2490–2502. [Google Scholar] [CrossRef]
- Lewnard, J.A.; Grad, Y.H. Vaccine Waning and Mumps Re-emergence in the United States. Sci. Trans. Med. 2018, 10, eaao5945. [Google Scholar] [CrossRef]
- Seagle, E.E.; Bednarczyk, R.A.; Hill, T.; Fiebelkorn, A.P.; Hickman, C.J.; Icenogle, J.P.; Belongia, E.A.; McLean, H.Q. Measles, Mumps and Rubella Antibody Patterns of Persistence and Rate of Decline Following the Second Dose of the MMR Vaccine. Vaccine 2018, 36, 818–826. [Google Scholar] [CrossRef]
- Cardemil, C.V.; Dahl, R.M.; James, L.; Wannemuehler, K.; Gary, H.E.; Shah, M.; Marin, M.; Riley, J.; Feikin, D.R.; Patel, M.; et al. Effectiveness of a Third Dose of MMR Vaccine for Mumps Outbreak Control. N. Engl. J. Med. 2017, 377, 947–956. [Google Scholar] [CrossRef]
- Haralambieva, I.H.; Ovsyannikova, I.G.; Kennedy, R.B.; Larrabee, B.R.; Zimmermann, M.T.; Grill, D.E.; Schaid, D.J.; Poland, G.A. Genome-wide associations of CD46 and IFI44L genetic variants with neutralizing antibody response to measles vaccine. Hum. Genet. 2017, 136, 421–435. [Google Scholar] [CrossRef]
- Kremer, J.R.; Scheneider, F.; Muller, C.P. Waning Antibodies in Measles and Rubella Vaccines—A Longitudinal Study. Vaccine 2006, 24, 2594–2601. [Google Scholar] [CrossRef]
- Anichini, G.; Gandolfo, C.; Fabrizi, S.; Miceli, G.B.; Terrosi, C.; Savellini, G.G.; Prathyumnan, S.; Orsi, D.; Battista, G.; Cusi, M.G. Seroprevalence to Measles Virus after Vaccination or Natural Infection in an Adult Population, in Italy. Vaccines 2020, 8, 66. [Google Scholar] [CrossRef]
- Kizito, D.; Tweyongyere, R.; Namatovu, A.; Webb, E.L.; Muhangi, L.; Lule, S.A.; Bukenya, H.; Cose, S.; Elliott, A.M. Factors affecting the infant antibody response to measles immunisation in Entebbe-Uganda. BMC Public. Health 2013, 13, 619. [Google Scholar] [CrossRef]
- Burgos-Peláez, R. Desnutrición y enfermedad. Nutr. Hosp. Supl. 2013, 6, 10–23. [Google Scholar]
- Cediel, G.; Olivares, M.; Brito, A.; de Romaña, D.L.; Cori, H.; La Frano, M.R. Interpretation of Serum Retinol Data From Latin America and the Caribbean. Food Nutr. Bull. 2015, 36, S98–S108. [Google Scholar] [CrossRef]
- Shamah-Levy, T.; Castellanos-Amaya, M.A.; Cuevas-Nasu, L. Desnutrición y obesidad: Doble carga en México. Rev. Dig. Univ. UNAM 2015, 6, 1–17. [Google Scholar]
- Mundo-Rosas, V.; Rodríguez-Ramírez, S.; Shamah-Levy, T. Energy and Nutrient Intake in Mexican Children 1 to 4 years old. Results from the Mexican National Health and Nutrition Survey 2006. Salud Publica Mex. 2009, 51, S530–S539. [Google Scholar] [CrossRef]
- Jiménez-Aguilar, A.; Gaona-Pineda, E.B.; Mejía-Rodríguez, F.; Gómez-Acosta, L.M.; Mendez-Gómez Humarán, I.; Flores-Aldama, M. Consumption of fruits and vegetables and health status of Mexican children from the National Health and Nutrition Survey 2012. Salud Publica Mex. 2014, 56, S103–S112. [Google Scholar] [CrossRef]
- Rodríguez-Martín, A.; Novalbos-Ruiz, J.P.; Jiménez-Rodríguez, A.; Baglietto-Ramos, M.; Romero-Sánchez, J.M. Implications of malnutrition in primary care. Nutr. Hosp. 2010, 25, S67–S79. [Google Scholar]
- Greenwood, B.M.; Bradley-Moore, A.M.; Bradley, A.K.; Kirkwood, B.R.; Gilles, H.M. The immune response to vaccination in undernourished and well-nourished Nigerian children. Ann. Trop. Med. Parasitol. 1986, 80, 537–544. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, F.; Khan, A.I.; Hossain, M.I.; Malek, M.A.; Faruque, A.S.; Ahmed, T.; Salam, M.A. Young children non-immunized against measles: Characteristics and programmatic implications. Acta Paediatr. 2006, 95, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Bloss, E.; Wainaina, F.; Bailey, R.C. Prevalence and predictors of underweight, stunting, and wasting among children aged 5 and under in western Kenya. J. Trop. Pediatr. 2004, 50, 260–270. [Google Scholar] [CrossRef] [PubMed]
- Rytther, M.J.; Kolte, L.; Briend, A.; Friss, H.; Christensen, V.B. The immune system in children with malnutrition: A systematic review. PLoS ONE 2014, 9, e105017. [Google Scholar] [CrossRef] [PubMed]
- Díaz-Quíñónez, J.A. The risk of reintroduction of measles in Mexico. Gac. Med. Mex. 2019, 155, 421–422. [Google Scholar] [CrossRef]
- Organización Panamericana de Salud. Actualización Epidemiológica Sarampión. 2019. Available online: https://www.paho.org/hq/index.php?option=com_docman&view=download&category_slug=sarampion-2183&alias=50913-1-de-noviembre-de-2019-sarampion-actualizacion-epidemiologica-2&Itemid=270&lang=es (accessed on 1 November 2020).
- Dirección General de Epidemiología. Secretaria de Salud. Sarampión, México: Casos confirmados. 2019. Available online: https://www.gob.mx/cms/uploads/attachment/file/510285/Sarampion_Mexico_CasosConfirmados_20191113_12hrs.pdf (accessed on 21 March 2020).
- Secretaria de Gobernación. Tabla de Resumen de Casos Confirmados por Sarampión 2020. Available online: https://www.gob.mx/cms/uploads/attachment/file/558769/Tabla_resumen_casos_confirmados_sarampion_2020.06.19.pdf (accessed on 19 June 2020).
| Variable | Tlapaneco (n = 207) | Mixteco (n = 101) | Mestizo (n = 108) | p Value |
|---|---|---|---|---|
| Age, (years) a | 10 (6–12) | 9 (6–12) | 9 (6–12) | 0.50 |
| Height, (m) a | 1.28 (1.09–1.46) | 1.25 (1.08–1.45) | 1.31 (1.1–1.52) | 0.003 * |
| Weight, (kg) a | 26.7 (17.9–44) | 25.2 (17.9–39.2) | 28.2 (18.2–53.7) | 0.007 * |
| BMI, (kg/m2) | 16.5 (14.1–21.2) | 15.8 (13.8–20.9) | 16.4 (13.9–24.5) | 0.015 * |
| WC, (cm) a | 59 (51–73.5) | 58 (51–70.5) | 59 (51.5–83) | 0.144 |
| Arm, (cm) a | 18 (14.5–24) | 18 (15–21.6) | 18.5 (15.3–25.5) | 0.021 * |
| Weight Category b | <0.001 * | |||
| Underweight, % | 73 (35.3) | 46 (45.6) | 24 (22.2) | |
| Normal Weight, % | 116 (56.0) | 49 (48.5) | 56 (51.9) | |
| Overweight, % | 18 (8.7) | 6 (5.9) | 28 (25.9) |
| Variable | Tlapaneco (n = 207) | Mixteco (n = 101) | Mestizo (n = 108) | p Value |
|---|---|---|---|---|
| Gender, n (%) a | 0.97 | |||
| Male | 101 (48.8) | 48 (47.5) | 53 (49.1) | |
| Female | 106 (51.2) | 53 (52.5) | 55 (50.9) | |
| Age category, n (%) a | 0.35 | |||
| 6 | 21 (10.1) | 7 (6.9) | 14 (13) | |
| 7 to 9 | 80 (38.7) | 49 (48.5) | 43 (39.8) | |
| 10 to 13 | 106 (51.2) | 45 (44.6) | 51 (74.2) | |
| Parent’s occupation, n (%) a | <0.001 * | |||
| Farmers | 139 (67.2) | 70 (69.3) | 31 (28.7) | |
| Traders | 14 (6.8) | 3 (3) | 21 (19.4) | |
| Others | 54 (26.1) | 28 (27.7) | 56 (51.9) | |
| House building material, n (%) a | <0.001 * | |||
| Adobe | 76 (36.7) | 59 (58.4) | 39 (36.1) | |
| Wood | 73 (35.2) | 27 (26.7) | 20 (18.5) | |
| Bricks | 58 (28.1) | 15 (14.9) | 49 (45.4) | |
| Members per household, n (%) a | 0.04 * | |||
| 2–4 | 54 (26.1) | 20 (19.8) | 27 (25) | |
| 5–7 | 96 (46.4) | 63 (62.4) | 63 (58.3) | |
| ≥8 | 57 (27.5) | 18 (17.8) | 18 (16.7) |
| Variable | n | Seropositive IgG Anti-Measles% (CI95%) | p Value |
|---|---|---|---|
| Gender, n (%) a | |||
| Male | 202 | 53.5 (46.5–60.4) | 0.029 * |
| Female | 214 | 64.0 (57.5–70.5) | |
| Age category, n (%) a | <0.001 * | ||
| 6 | 42 | 90.5 (81.2–99.7) | |
| 7 to 9 | 172 | 66.9 (59.7–73.9) | |
| 10 to 13 | 202 | 45.5 (38.6–52.5) | |
| Ethnic group, n (%) a | 0.13 | ||
| Tlapaneco | 207 | 63.8 (57.1–70.3) | |
| Mixteco | 101 | 53.5 (43.5–63.3) | |
| Mestizo | 108 | 54.6 (45.1–64.2) | |
| Weight category, n (%) a | 0.99 | ||
| Underweight | 143 | 58.7 (50.5–69.9) | |
| Normal weight | 221 | 58.8 (52.2–65.3) | |
| Overweigh | 52 | 59.6 (45.8–73.4) | |
| Parent’s occupation, n (%) a | 0.82 | ||
| Farmers | 240 | 57.9 (51.6–64.2) | |
| Traders | 38 | 63.2 (47.1–79.2) | |
| Others | 138 | 59.4 (51.1–67.7) | |
| House building material, n (%) a | 0.95 | ||
| Adobe | 174 | 59.8 (52.4–67.1) | |
| Wood | 120 | 58.3 (49.3–67.3) | |
| Bricks | 122 | 58.2 (49.3–67.1) | |
| Members per household, n (%) a | 0.36 | ||
| 2–4 | 101 | 59.4 (49.7–69.1) | |
| 5–7 | 222 | 61.3 (54.8–67.7) | |
| ≥8 | 93 | 52.7 (42.3–63.0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sánchez-Alemán, M.A.; Gutiérrez-Pérez, I.A.; Díaz-Salgado, N.; Zaragoza-García, O.; Olamendi-Portugal, M.; Castro-Alarcón, N.; Parra-Rojas, I.; Guzmán-Guzmán, I.P. Low Seroprevalence of Measles-Specific IgG in Children of Three Ethnic Groups from Mexico: Influence of Age, Sex, Malnutrition and Family Size. Vaccines 2021, 9, 295. https://doi.org/10.3390/vaccines9030295
Sánchez-Alemán MA, Gutiérrez-Pérez IA, Díaz-Salgado N, Zaragoza-García O, Olamendi-Portugal M, Castro-Alarcón N, Parra-Rojas I, Guzmán-Guzmán IP. Low Seroprevalence of Measles-Specific IgG in Children of Three Ethnic Groups from Mexico: Influence of Age, Sex, Malnutrition and Family Size. Vaccines. 2021; 9(3):295. https://doi.org/10.3390/vaccines9030295
Chicago/Turabian StyleSánchez-Alemán, Miguel A., Ilse A. Gutiérrez-Pérez, Nayeli Díaz-Salgado, Oscar Zaragoza-García, María Olamendi-Portugal, Natividad Castro-Alarcón, Isela Parra-Rojas, and Iris P. Guzmán-Guzmán. 2021. "Low Seroprevalence of Measles-Specific IgG in Children of Three Ethnic Groups from Mexico: Influence of Age, Sex, Malnutrition and Family Size" Vaccines 9, no. 3: 295. https://doi.org/10.3390/vaccines9030295
APA StyleSánchez-Alemán, M. A., Gutiérrez-Pérez, I. A., Díaz-Salgado, N., Zaragoza-García, O., Olamendi-Portugal, M., Castro-Alarcón, N., Parra-Rojas, I., & Guzmán-Guzmán, I. P. (2021). Low Seroprevalence of Measles-Specific IgG in Children of Three Ethnic Groups from Mexico: Influence of Age, Sex, Malnutrition and Family Size. Vaccines, 9(3), 295. https://doi.org/10.3390/vaccines9030295