Role of Vaccine Hesitancy, eHealth Literacy, and Vaccine Literacy in Young Adults’ COVID-19 Vaccine Uptake Intention in a Lower-Middle-Income Country
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Setting, Design, Participants, and Sampling
2.2. Measures
Outcome Variable
VUI
2.3. Explanatory Variables of Interest
Vaccine Hesitancy
2.4. COVID-19 Vaccine Literacy
2.5. eHealth Literacy
2.6. Control Variables
2.7. Statistical Analyses
2.7.1. Descriptive Analyses
2.7.2. Estimation Technique
3. Results
3.1. Descriptive Statistics
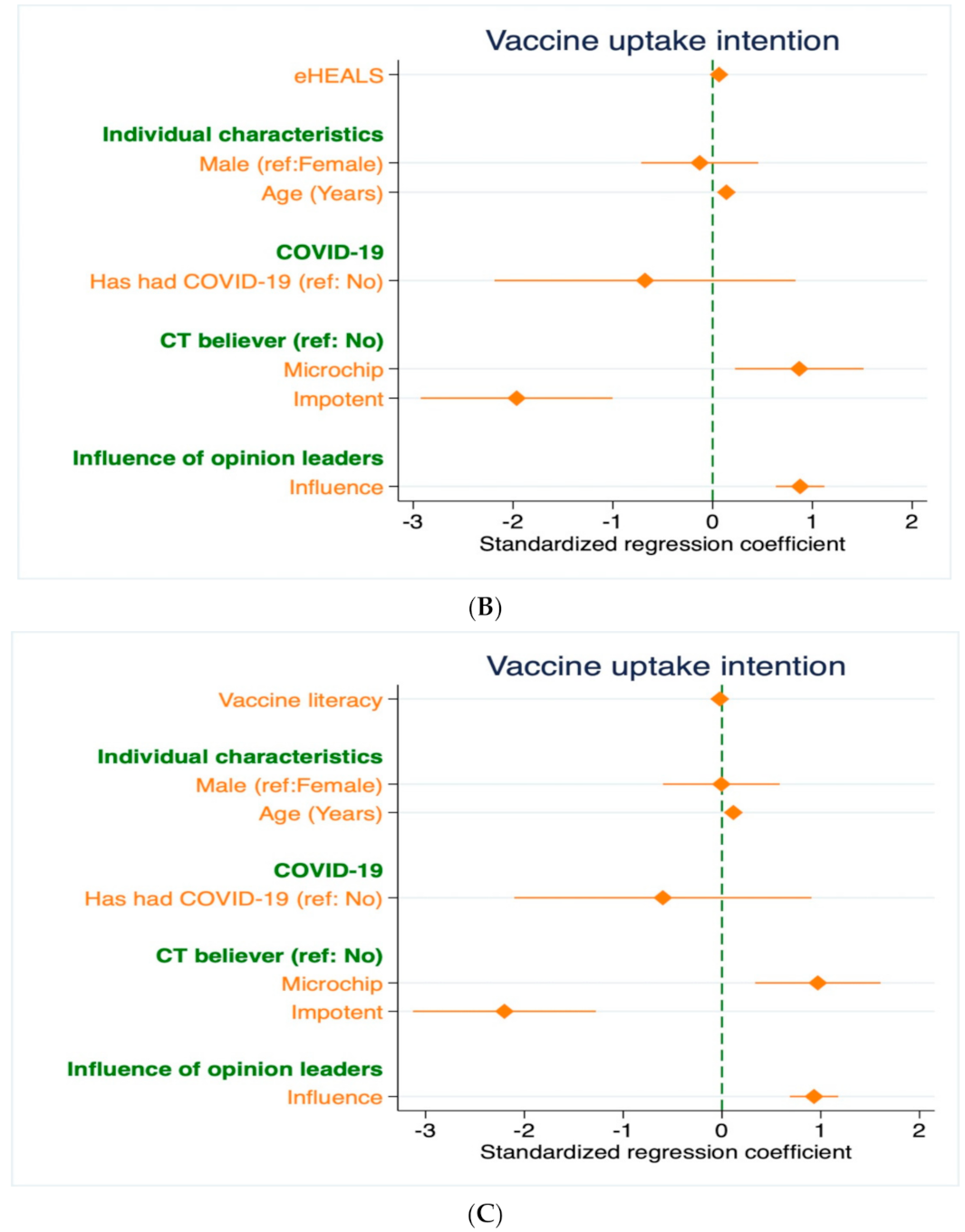
3.2. Main Analysis
3.3. Robustness Checks
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Items |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
- (1)
- Did you find words you didn’t know?
- (2)
- Did you find that the texts were difficult to understand?
- (3)
- Did you need much time to understand them?
- (4)
- Did you or would you need someone to help you understand them?
- (1)
- Have you consulted more than one source of information?
- (2)
- Did you find the information you were looking for?
- (3)
- Have you had the opportunity to use the information?
- (4)
- Did you discuss what you understood about vaccinations with your doctor or other people?
- (5)
- Did you consider whether the information collected was about your condition?
- (6)
- Have you considered the credibility of the sources?
- (7)
- Did you check whether the information was correct?
- (8)
- Did you find any useful information to make a decision on whether or not to get vaccinated?
- How useful do you feel the Internet is in helping you in making decisions about your health? (5 points scale: 1 = Not useful at all; 5 = Very useful)
- How important is it for you to be able to access health resources on the Internet? (5 points scale: 1 = Not important at all; 5 = Very important)
- I know what health resources are available on the Internet (5 points scale: 1 = Strongly disagree; 5 = Strongly agree)
- I know where to find helpful health resources on the Internet (5 points scale: 1 = Strongly disagree; 5 = Strongly agree)
- I know how to find helpful health resources on the Internet (5 points scale: 1 = Strongly disagree; 5 = Strongly agree)
- I know how to use the Internet to answer my questions about health (5 points scale: 1 = Strongly disagree; 5 = Strongly agree)
- I know how to use the health information I find on the Internet to help me (5 points scale: 1 = Strongly disagree; 5 = Strongly agree)
- I have the skills I need to evaluate the health resources I find on the Internet (5 points scale: 1 = Strongly disagree; 5 = Strongly agree)
- I can tell high quality health resources from low quality health resources on the Internet (5 points scale: 1 = Strongly disagree; 5 = Strongly agree)
- I feel confident in using information from the Internet to make health decisions (5 points scale: 1 = Strongly disagree; 5 = Strongly agree)
References
- Adhikari, S.P.; Meng, S.; Wu, Y.; Mao, Y.; Ye, R.; Wang, Q.; Sun, C.; Sylvia, S.; Rozelle, S.; Raat, H.; et al. Epidemiology, Causes, Clinical Manifestation and Diagnosis, Prevention and Control of 2019 Novel Coronavirus during the Early Outbreak Period: A Scoping Review. Infect. Dis. Poverty 2000, 9, 29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Pillai, S.; Siddika, N.; Apu, E.H.; Kabir, R. Situation of European Countries so Far. Arch. Med. Res. 2020, 51, 723–725. [Google Scholar] [CrossRef] [PubMed]
- Alzoubi, H.; Alnawaiseh, N.; Al-Mnayyis, A.; Abu-Lubad, M.; Aqel, A.; Al-Shagahin, H. COVID-19—Knowledge, Attitude and Practice among Medical and Non-Medical University Students in Jordan. J. Pure Appl. Microbiol. 2020, 14, 17–24. [Google Scholar] [CrossRef] [Green Version]
- Bhagavathula, A.S.; Aldhaleei, W.A.; Rahmani, J.; Mahabadi, M.A.; Bandari, D.K. Novel Coronavirus (COVID-19) Knowledge and Perceptions: A Survey of Healthcare Workers. medRxiv 2020. [Google Scholar] [CrossRef]
- Wolf, M.S.; Serper, M.; Opsasnick, L.; O’Conor, R.M.; Curtis, L.M.; Benavente, J.Y.; Wismer, G.; Batio, S.; Eifler, M.; Zheng, P.; et al. Awareness, Attitudes, and Actions Related to COVID-19 Among Adults With Chronic Conditions at the Onset of the U.S. Outbreak: A Cross-Sectional Survey. Ann. Intern. Med. 2020, 173, 100–109. [Google Scholar] [CrossRef] [Green Version]
- Hodgson, S.H.; Mansatta, K.; Mallett, G.; Harris, V.; Emary, K.R.W.; Pollard, A.J. What Defines an Efficacious COVID-19 Vaccine? A Review of the Challenges Assessing the Clinical Efficacy of Vaccines against SARS-CoV-2. Lancet Infect. Dis. 2021, 21, e26–e35. [Google Scholar] [CrossRef]
- Conte, C.; Sogni, F.; Affanni, P.; Veronesi, L.; Argentiero, A.; Esposito, S. Vaccines against Coronaviruses: The State of the Art. Vaccines 2020, 8, 309. [Google Scholar] [CrossRef]
- Kaur, S.P.; Gupta, V. COVID-19 Vaccine: A Comprehensive Status Report. Virus Res. 2020, 288, 198114. [Google Scholar] [CrossRef]
- Hossain, M.B.; Alam, M.Z.; Islam, M.S.; Sultan, S.; Faysal, M.M.; Rima, S.; Hossain, M.A.; Mamun, A.A. Health Belief Model, Theory of Planned Behavior, or Psychological Antecedents: What Predicts COVID-19 Vaccine Hesitancy Better Among the Bangladeshi Adults? Front. Public Health 2021, 9, 1–10. [Google Scholar] [CrossRef]
- Noushad, M.; Nassani, M.Z.; Alsalhani, A.B.; Koppolu, P.; Niazi, F.H.; Samran, A.; Rastam, S.; Alqerban, A.; Barakat, A.; Almoallim, H.S. COVID-19 Vaccine Intention among Healthcare Workers in Saudi Arabia: A Cross-Sectional Survey. Vaccines 2021, 9, 835. [Google Scholar] [CrossRef]
- Dodd, R.H.; Pickles, K.; Nickel, B.; Cvejic, E.; Ayre, J.; Batcup, C.; Bonner, C.; Copp, T.; Cornell, S.; Dakin, T.; et al. Concerns and Motivations about COVID-19 Vaccination. Lancet Infect. Dis. 2021, 21, 161–162. [Google Scholar] [CrossRef]
- MacDonald, N.E.; Eskola, J.; Liang, X.; Chaudhuri, M.; Dube, E.; Gellin, B.; Goldstein, S.; Larson, H.; Manzo, M.L.; Reingold, A.; et al. Vaccine Hesitancy: Definition, Scope and Determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- WHO. Ten threats to global health in 2019. Cukurova Med. J. 2019, 44, 1150–1151. [Google Scholar]
- Larson, H.J.; Jarrett, C.; Eckersberger, E.; Smith, D.M.D.; Paterson, P. Understanding Vaccine Hesitancy around Vaccines and Vaccination from a Global Perspective: A Systematic Review of Published Literature, 2007–2012. Vaccine 2014, 32, 2150–2159. [Google Scholar] [CrossRef]
- Biasio, L.R.; Bonaccorsi, G.; Lorini, C.; Mazzini, D.; Pecorelli, S. Italian Adults’ Likelihood of Getting Covid-19 Vaccine: A Second Online Survey. Vaccines 2021, 9, 268. [Google Scholar] [CrossRef] [PubMed]
- Hong, K.J.; Park, N.L.; Heo, S.Y.; Jung, S.H.; Lee, Y.B.; Hwang, J.H. Effect of EHealth Literacy on COVID-19 Infection-Preventive Behaviors of Undergraduate Students Majoring in Healthcare. Healthcare 2021, 9, 573. [Google Scholar] [CrossRef]
- Korkmaz Aslan, G.; Kartal, A.; Turan, T.; Taşdemir Yiğitoğlu, G.; Kocakabak, C. Association of Electronic Health Literacy with Health-Promoting Behaviours in Adolescents. Int. J. Nurs. Pract. 2021, 27, 1–9. [Google Scholar] [CrossRef]
- Britt, R.K.; Collins, W.B.; Wilson, K.M.; Linnemeier, G.; Englebert, A.M. The Role of EHealth Literacy and HPV Vaccination Among Young Adults: Implications from a Planned Behavior Approach. Commun. Res. Reports 2015, 32, 208–215. [Google Scholar] [CrossRef]
- Arce, J.S.S.; Warren, S.S.; Meriggi, N.F.; Scacco, A.; McMurry, N.; Voors, M.; Syunyaev, G.; Malik, A.A.; Aboutajdine, S.; Armand, A.; et al. COVID-19 vaccine acceptance and hesitancy in low and middle income countries, and implications for messaging. medRxiv 2021. [Google Scholar] [CrossRef]
- Mathieu, E.; Ritchie, H.; Ortiz-Ospina, E.; Roser, M.; Hasell, J.; Appel, C.; Giattino, C.; Rodés-Guirao, L. A global database of COVID-19 vaccinations. Nat. Hum. Behav. 2021, 5, 947–953. [Google Scholar] [CrossRef]
- Wright, L.; Fancourt, D. Do Predictors of Adherence to Pandemic Guidelines Change over Time? A Panel Study of 22,000 UK Adults during the COVID-19 Pandemic. Prev. Med. 2021, 153, 106713. [Google Scholar] [CrossRef]
- Available online: https://osf.io/preprints/socarxiv/8edbj/ (accessed on 12 November 2021).
- TBS. Covid-19: Youth Deaths Are on the Rise in the Second Wave; The Business Standard: Dhaka, Bangladesh, 11 April 2021. [Google Scholar]
- Available online: https://www.worldbank.org/en/country/bangladesh/overview#1 (accessed on 12 November 2021).
- Imtiaz, A.; Khan, N.M.; Hossain, M.A. COVID-19 in Bangladesh: Measuring Differences in Individual Precautionary Behaviors among Young Adults. J. Public Health 2021, 1–12. [Google Scholar] [CrossRef]
- Zhong, B.L.; Luo, W.; Li, H.M.; Zhang, Q.Q.; Liu, X.G.; Li, W.T.; Li, Y. Knowledge, Attitudes, and Practices towards COVID-19 among Chinese Residents during the Rapid Rise Period of the COVID-19 Outbreak: A Quick Online Cross-Sectional Survey. Int. J. Biol. Sci. 2020, 16, 1745–1752. [Google Scholar] [CrossRef]
- Kwok, K.O.; Li, K.; WEI, W.I.; Tang, A.; Wong, S.Y.S.; Lee, S.S. Influenza Vaccine Uptake, COVID-19 Vaccination Intention and Vaccine Hesitancy among Nurses: A Survey. Int. J. Nurs. Stud. 2020, 114, 103854. [Google Scholar] [CrossRef] [PubMed]
- Betsch, C.; Schmid, P.; Heinemeier, D.; Korn, L.; Holtmann, C.; Böhm, R. Beyond Confidence: Development of a Measure Assessing the 5C Psychological Antecedents of Vaccination. PLoS ONE 2018, 13, e0208601. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Biasio, L.R.; Bonaccorsi, G.; Lorini, C.; Pecorelli, S. Assessing COVID-19 Vaccine Literacy: A Preliminary Online Survey. Hum. Vaccines Immunother. 2020, 13, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Hinton, P.; McMurray, I.; Brownlow, C. SPSS Explained; Routledge: London, UK, 2014. [Google Scholar]
- Norman, C.D.; Skinner, H.A. EHEALS: The EHealth Literacy Scale. J. Med. Internet Res. 2006, 8, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jolley, D.; Douglas, K.M. The Effects of Anti-Vaccine Conspiracy Theories on Vaccination Intentions. PLoS ONE 2014, 9, e89177. [Google Scholar] [CrossRef]
- Chen, L.; Zhang, Y.; Young, R.; Wu, X.; Zhu, G. Effects of Vaccine-Related Conspiracy Theories on Chinese Young Adults’ Perceptions of the HPV Vaccine: An Experimental Study. Health Commun. 2021, 36, 1343–1353. [Google Scholar] [CrossRef]
- Anwar, S.; Nasrullah, M.; Hosen, M.J. COVID-19 and Bangladesh: Challenges and How to Address Them. Front. Public Heal. 2020, 8, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Smith, L.E.; Mottershaw, A.L.; Egan, M.; Waller, J.; Marteau, T.M.; Rubin, G.J. The Impact of Believing You Have Had COVID-19 on Self-Reported Behaviour: Cross-Sectional Survey. PLoS ONE 2020, 16, e0248076. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.sciencedirect.com/science/article/pii/S0196655320310026 (accessed on 12 November 2021).
- Painter, E.M.; Ussery, E.N.; Patel, A.; Hughes, M.M.; Zell, E.R.; Moulia, D.L.; Scharf, L.G.; Lynch, M.; Ritchey, M.D.; Toblin, R.L.; et al. Demographic Characteristics of Persons Vaccinated During the First Month of the COVID-19 Vaccination Program—United States, 14 December 2020–14 January 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 174–177. [Google Scholar] [CrossRef] [PubMed]
- Norman, G. Likert scales, levels of measurement and the “laws” of statistics. Adv. Health Sci. Educ. 2010, 15, 625–632. [Google Scholar] [CrossRef]
- Robitzsch, A. Why ordinal variables can (almost) always be treated as continuous variables: Clarifying assumptions of robust continuous and ordinal factor analysis estimation methods. In Frontiers in Education. Frontiers 2020, 5, 177. [Google Scholar] [CrossRef]
- Norris, C.M.; Ghali, W.A.; Saunders, L.D.; Brant, R.; Galbraith, D.; Faris, P.; Knudtson, M.L.; APPROACH Investigators. Ordinal regression model and the linear regression model were superior to the logistic regression models. J. Clin. Epidemiol. 2006, 59, 448–456. [Google Scholar] [CrossRef]
- Zdaniuk, B. Ordinary Least-Squares (OLS) Model. In Encyclopedia of Quality of Life and Well-Being Research; Michalos, A.C., Ed.; Springer: Dordrecht, The Netherlands, 2014. [Google Scholar] [CrossRef]
- Jae Jeong, H. The Level of Collapse We Are Allowed: Comparison of Different Response Scales in Safety Attitudes Questionnaire. Biom. Biostat. Int. J. 2016, 4, 128–134. [Google Scholar] [CrossRef]
- Muturi, N. EHealth Literacy and the Motivators for HPV Prevention among Young Adults in Kenya. Commun. Res. Rep. 2020, 37, 74–86. [Google Scholar] [CrossRef]
- Romer, D.; Jamieson, K.H. Conspiracy Theories as Barriers to Controlling the Spread of COVID-19 in the U.S. Soc. Sci. Med. 2020, 263, 113356. [Google Scholar] [CrossRef]
- Hossain, M.A.; Jahid, M.I.K.; Amran Hossain, K.M.; Walton, L.M.; Uddin, Z.; Haque, M.O.; Kabir, M.F.; Yasir Arafat, S.M.; Sakel, M.; Faruqui, R.; et al. Knowledge Attitudes and Fear of COVID-19 during the Rapid Rise Period in Bangladesh. PLoS ONE 2020, 15, e0239646. [Google Scholar] [CrossRef]
- Ferdous, M.Z.; Islam, M.S.; Sikder, M.T.; Mosaddek, A.S.M.; Zegarra-Valdivia, J.A.; Gozal, D. Knowledge, Attitude, and Practice Regarding COVID-19 Outbreak in Bangladesh: An Onlinebased Cross-Sectional Study. PLoS ONE 2020, 15, e0239254. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. A Global Survey of Potential Acceptance of a COVID-19 Vaccine. Nat. Med. 2021, 27, 225–228. [Google Scholar] [CrossRef] [PubMed]

| Variable | Mean/N (%) | SD | r |
|---|---|---|---|
| Vaccine uptake intention | 7.08 | 3.18 | |
| Vaccine hesitancy | |||
| Confidence | 4.58 | 1.66 | 0.47 *** |
| Complacency | 3.4 | 1.45 | −0.15 *** |
| Constraints | 2.84 | 1.4 | −0.37 *** |
| Calculation | 5.77 | 1.45 | −0.06 |
| Collective responsibility | 4.47 | 1.04 | 0.26 *** |
| Vaccine literacy | 33.86 | 7.21 | −0.05 |
| eHealth literacy | 39.39 | 7.87 | 0.24 *** |
| Age | Median = 21 | Range = 12 | 0.12 ** |
| Influence of opinion leaders | 3.36 | 1.34 | 0.46 *** |
| Sex of the respondents | −0.05 | ||
| Female | 142 (41.40%) | ||
| Male | 201 (58.60%) | ||
| COVID-19 patient | −0.04 | ||
| No | 324 (94.46%) | ||
| Yes | 19 (5.54%) | ||
| Conspiracy theory believer (microchip) | 0.07 | ||
| No | 242 (70.55%) | ||
| Yes | 101 (29.45%) | ||
| Conspiracy theory believer (impotent) | −0.3 *** | ||
| No | 291 (84.84%) | ||
| Yes | 52 (15.16%) | ||
| Variable | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Effect of Vaccine Hesitancy on VUI | |||
| Vaccine hesitancy | |||
| Confidence | 0.94 *** | 0.98 *** | 0.71 *** |
| (0.10) | (0.10) | (0.11) | |
| Complacency | −0.11 | −0.11 | −0.16 |
| (0.11) | (0.11) | (0.11) | |
| Constraints | −0.53 *** | −0.53 *** | −0.52 *** |
| (0.13) | (0.13) | (0.12) | |
| Calculation | −0.62 *** | −0.54 *** | −0.45 *** |
| (0.11) | (0.11) | (0.11) | |
| Collective responsibility | 0.67 *** | 0.58 *** | 0.46 *** |
| (0.14) | (0.14) | (0.13) | |
| Constant | 5.24 *** | 2.31 | 1.17 |
| (1.00) | (1.45) | (1.42) | |
| Controls | Null | Partial | Full |
| Observations | 343 | 343 | 343 |
| VIF | 1.33 | 1.30 | 1.31 |
| R-squared | 0.40 | 0.42 | 0.49 |
| Effect of eHealth literacy on VUI | |||
| eHealth literacy | 0.10 *** | 0.11 *** | 0.07 *** |
| (0.02) | (0.02) | (0.02) | |
| Constant | 3.18 *** | −0.50 | −1.52 |
| (0.85) | (1.46) | (1.32) | |
| Controls | Null | Partial | Full |
| Observations | 343 | 343 | 343 |
| VIF | - | 1.02 | 1.09 |
| R-squared | 0.06 | 0.09 | 0.31 |
| Effect of vaccine literacy on VUI | |||
| Vaccine literacy | −0.02 | −0.02 | −0.02 |
| (0.02) | (0.02) | (0.02) | |
| Constant | 7.79 *** | 5.28 *** | 2.07 |
| (0.78) | (1.48) | (1.38) | |
| Controls | Null | Partial | Full |
| Observations | 343 | 343 | 343 |
| VIF | - | 1.00 | 1.06 |
| R-squared | 0.00 | 0.02 | 0.29 |
| Variable | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Effect of Vaccine Hesitancy on VUI | |||
| Vaccine hesitancy | |||
| Confidence | 0.43 *** | 0.47 *** | 0.38 *** |
| (0.07) | (0.07) | (0.07) | |
| Complacency | −0.10 | −0.12 * | −0.16 ** |
| (0.07) | (0.07) | (0.07) | |
| Constraints | −0.23 *** | −0.23 *** | −0.24 *** |
| (0.07) | (0.07) | (0.07) | |
| Calculation | −0.31 *** | −0.27 *** | −0.25 *** |
| (0.07) | (0.07) | (0.08) | |
| Collective responsibility | 0.31 *** | 0.26 *** | 0.22 ** |
| (0.09) | (0.09) | (0.10) | |
| Constant | 0.02 | −1.86 ** | −3.08 *** |
| (0.60) | (0.93) | (1.00) | |
| Controls | Null | Partial | Full |
| Observations | 343 | 343 | 343 |
| Effect of eHealth literacy on VUI | |||
| eHealth literacy | 0.04 *** | 0.05 *** | 0.04 *** |
| (0.01) | (0.01) | (0.01) | |
| Constant | −1.10 *** | −2.87 *** | −4.05 *** |
| (0.36) | (0.70) | (0.78) | |
| Controls | Null | Partial | Full |
| Observations | 343 | 343 | 343 |
| Effect of vaccine literacy on VUI | |||
| Vaccine literacy | −0.01 | −0.01 | −0.01 |
| (0.01) | (0.01) | (0.01) | |
| Constant | 0.78 ** | −0.31 | −1.96 *** |
| (0.34) | (0.62) | (0.72) | |
| Controls | Null | Partial | Full |
| Observations | 343 | 343 | 343 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nath, R.; Imtiaz, A.; Nath, S.D.; Hasan, E. Role of Vaccine Hesitancy, eHealth Literacy, and Vaccine Literacy in Young Adults’ COVID-19 Vaccine Uptake Intention in a Lower-Middle-Income Country. Vaccines 2021, 9, 1405. https://doi.org/10.3390/vaccines9121405
Nath R, Imtiaz A, Nath SD, Hasan E. Role of Vaccine Hesitancy, eHealth Literacy, and Vaccine Literacy in Young Adults’ COVID-19 Vaccine Uptake Intention in a Lower-Middle-Income Country. Vaccines. 2021; 9(12):1405. https://doi.org/10.3390/vaccines9121405
Chicago/Turabian StyleNath, Rima, Asif Imtiaz, Shobod Deba Nath, and Emran Hasan. 2021. "Role of Vaccine Hesitancy, eHealth Literacy, and Vaccine Literacy in Young Adults’ COVID-19 Vaccine Uptake Intention in a Lower-Middle-Income Country" Vaccines 9, no. 12: 1405. https://doi.org/10.3390/vaccines9121405
APA StyleNath, R., Imtiaz, A., Nath, S. D., & Hasan, E. (2021). Role of Vaccine Hesitancy, eHealth Literacy, and Vaccine Literacy in Young Adults’ COVID-19 Vaccine Uptake Intention in a Lower-Middle-Income Country. Vaccines, 9(12), 1405. https://doi.org/10.3390/vaccines9121405






