COVID-19 Vaccine Hesitancy among Italian University Students: A Cross-Sectional Survey during the First Months of the Vaccination Campaign
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting and Participants
2.2. Questionnaire
2.3. Statistical Analysis
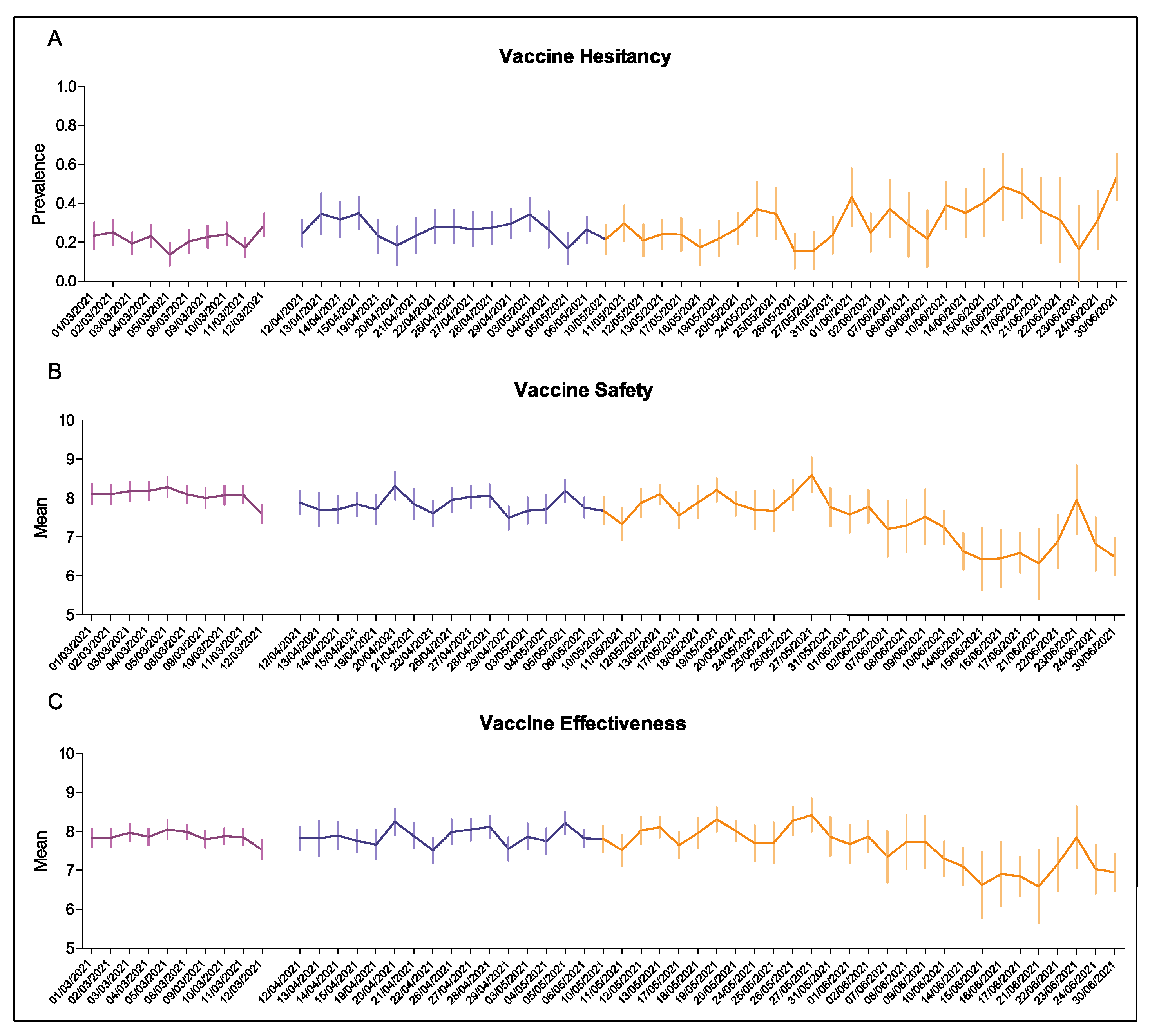
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- European Centre for Disease Prevention and Control (ECDC). Interim Guidance on the Benefits of Full Vaccination against COVID-19 for Transmission and Implications for Non-Pharmaceutical Intervention; ECDC: Stockholm, Sweden, 2021. [Google Scholar]
- Ritchie, H.; Ortiz-Ospina, E.; Beltekian, D.; Edouard, M.; Joe Hasell, B.; Macdonald, C.; Giattino, C.; Appel, L. Coronavirus Pandemic (COVID-19). Our World in Data 2020. Published online at OurWorldInData.org. Available online: https://ourworldindata.org/coronavirus (accessed on 20 September 2021).
- European Centre for Disease Prevention and control (ECDC). Overview of the Implementation of COVID-19 Vaccination Strategies and Vaccine Deployment Plans in the EU/EEA; ECDC: Stockholm, Sweden, 2021. [Google Scholar]
- MacDonald, N.E.; Eskola, J.; Liang, X.; Chaudhuri, M.; Dube, E.; Gellin, B.; Goldstein, S.; Larson, H.; Manzo, M.L.; Reingold, A.; et al. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Ten Threats to Global Health in 2019; World Health Organization: Geneva, Switzerland, 2019; Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 3 September 2021).
- Larson, H.J.; Jarrett, C.; Eckersberger, E.; Smith, D.M.D.; Paterson, P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: A systematic review of published literature, 2007–2012. Vaccine 2014, 32, 2150–2159. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Barriers of Influenza Vaccination Intention and Behavior—A Systematic Review of Influenza Vaccine Hesitancy 2005–2016; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Rosso, A.; Massimi, A.; Pitini, E.; Nardi, A.; Baccolini, V.; Marzuillo, C.; De Vito, C.; Villari, P. Factors affecting the vaccination choices of pregnant women for their children: A systematic review of the literature. Hum. Vaccines Immunother. 2020, 16, 1969–1980. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilder-Smith, A.B.; Qureshi, K. Resurgence of measles in Europe: A systematic review on parental attitudes and beliefs of measles vaccine. J. Epidemiol. Glob. Health 2020, 10, 46–58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baccolini, V.; Sindoni, A.; Adamo, G.; Rosso, A.; Massimi, A.; Bella, A.; Filia, A.; Magurano, F.; Marzuillo, C.; Villari, P.; et al. Measles among healthcare workers in Italy: Is it time to act? Hum. Vaccines Immunother. 2020, 16, 2618–2627. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization (WHO). Behavioural Considerations for Acceptance and Uptake of COVID-19 Vaccines; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Robinson, E.; Jones, A.; Lesser, I.; Daly, M. International estimates of intended uptake and refusal of COVID-19 vaccines: A rapid systematic review and meta-analysis of large nationally representative samples. Vaccine 2021, 39, 2024–2034. [Google Scholar] [CrossRef]
- Sallam, M. COVID-19 vaccine hesitancy worldwide: A concise systematic review of vaccine acceptance rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef]
- Kelekar, A.; Lucia, V.; Afonso, N.; Mascarenhas, A. COVID-19 vaccine acceptance and hesitancy among dental and medical students. J. Am. Dent. Assoc. 2021, 152, 596–603. [Google Scholar] [CrossRef]
- Tavolacci, M.P.; Dechelotte, P.; Ladner, J. COVID-19 vaccine acceptance, hesitancy, and resistancy among university students in france. Vaccines 2021, 9, 654. [Google Scholar] [CrossRef]
- Afifi, T.O.; Salmon, S.; Taillieu, T.; Stewart-Tufescu, A.; Fortier, J.; Driedger, S.M. Older adolescents and young adults willingness to receive the COVID-19 vaccine: Implications for informing public health strategies. Vaccine 2021, 39, 3473–3479. [Google Scholar] [CrossRef] [PubMed]
- Monod, M.; Blenkinsop, A.; Xi, X.; Hebert, D.; Bershan, S.; Tietze, S.; Baguelin, M.; Bradley, V.C.; Chen, Y.; Coupland, H.; et al. Age groups that sustain resurging COVID-19 epidemics in the United States. Science 2021, 371, eabe8372. [Google Scholar] [CrossRef]
- Kim, C.; Kim, W.; Jeon, J.H.; Seok, H.; Kim, S.B.; Choi, H.K.; Yoon, Y.K.; Song, J.Y.; Park, D.W.; Sohn, W.; et al. COVID-19 infection with asymptomatic or mild disease severity in young patients: Clinical course and association between prevalence of pneumonia and viral load. PLoS ONE 2021, 16, e0250358. [Google Scholar]
- Lucia, V.C.; Kelekar, A.; Afonso, N.M. COVID-19 vaccine hesitancy among medical students. Public Health 2020, 43, 445–449. [Google Scholar]
- Barello, S.; Nania, T.; Dellafiore, F.; Graffigna, G.; Caruso, R. ‘Vaccine hesitancy’ among university students in Italy during the COVID-19 pandemic. Eur. J. Epidemiol. 2020, 35, 781–783. [Google Scholar] [CrossRef] [PubMed]
- Gallè, F.; Sabella, E.A.; Roma, P.; De Giglio, O.; Caggiano, G.; Tafuri, S.; Da Molin, G.; Ferracuti, S.; Montagna, M.T.; Liguori, G.; et al. Knowledge and acceptance of COVID-19 vaccination among undergraduate students from central and southern Italy. Vaccines 2021, 9, 638. [Google Scholar] [CrossRef] [PubMed]
- Salerno, L.; Craxì, L.; Amodio, E.; Lo Coco, G. Factors Affecting Hesitancy to mRNA and Viral Vector COVID-19 Vaccines among College Students in Italy. Vaccines 2021, 9, 927. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Survey Tool and Guidance: Behavioural Insights on COVID-19 (2020); World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Talbot, D.; Massamba, V.K.; Talbot, D. A descriptive review of variable selection methods in four epidemiologic journals: There is still room for improvement. Eur. J. Epidemiol. 2019, 34, 725–730. [Google Scholar] [CrossRef] [PubMed]
- Fridman, A.; Gershon, R.; Gneezy, A. COVID-19 and vaccine hesitancy: A longitudinal study. PLoS ONE 2021, 16, e0250123. [Google Scholar] [CrossRef]
- Rosselli, R.; Martini, M.; Bragazzi, N.L. The old and the new: Vaccine hesitancy in the era of the Web 2.0. Challenges and opportunities. J. Prev. Med. Hyg. 2016, 57, E47–E50. [Google Scholar] [PubMed]
- Rosso, A.; Massimi, A.; De Vito, C.; Adamo, G.; Baccolini, V.; Marzuillo, C.; Vacchio, M.R.; Villari, P. Knowledge and attitudes on pediatric vaccinations and intention to vaccinate in a sample of pregnant women from the City of Rome. Vaccine 2019, 37, 1954–1963. [Google Scholar] [CrossRef]
- Lewandowsky, S.; Cook, J.; Schmid, P.; Holford, D.L.; Finn, A.; Leask, J.; Thomson, A.; Lombardi, D.; Al-Rawi, A.K.; Amazeen, M.A.; et al. The COVID-19 Vaccine Communication Handbook. A Practical Guide for Improving Vaccine Communication and Fighting Misinformation. 2021. Available online: https://sks.to/c19vax (accessed on 10 September 2021).
- Loomba, S.; de Figueiredo, A.; Piatek, S.J.; de Graaf, K.; Larson, H.J. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nat. Hum. Behav. 2021, 5, 337–348. [Google Scholar] [CrossRef] [PubMed]
- Italian Medicines Agency (AIFA). COVID-19 Vaccine Surveillance Report #3-Period 27/12/2020–26/03/2021. 2021. Available online: https://www.aifa.gov.it/documents/20142/1315190/Rapporto_sorveglianza_vaccini_COVID-19_3_EN.pdf (accessed on 10 September 2021).
- Wang, C.; Han, B.; Zhao, T.; Liu, H.; Liu, B.; Chen, L.; Xie, M. Vaccination willingness, vaccine hesitancy, and estimated coverage at the first round of COVID-19 vaccination in China: A national cross-sectional study. Vaccine 2020, 39, 2833–2842. [Google Scholar] [CrossRef] [PubMed]
- Kreps, S.E.; Kriner, D.L. Factors influencing Covid-19 vaccine acceptance across subgroups in the United States: Evidence from a conjoint experiment. Vaccine 2021, 39, 3250–3258. [Google Scholar] [CrossRef] [PubMed]
- Mant, M.; Aslemand, A.; Prine, A.; Holland, A.J. University students’ perspectives, planned uptake, and hesitancy regarding the COVID-19 vaccine: A multi-methods study. PLoS ONE 2021, 16, e0255447. [Google Scholar] [CrossRef]
- Walker, A.N.; Zhang, T.; Peng, X.Q.; Ge, J.J.; Gu, H.; You, H. Vaccine acceptance and its influencing factors: An online cross-sectional study among international college students studying in china. Vaccines 2021, 9, 585. [Google Scholar] [CrossRef]
- Mateo-urdiales, A.; Del Manso, M.; Andrianou, X.; Spuri, M.; Ancona, F.D.; Filia, A.; Cristina, M.; Petrone, D.; Fenicia, M.; Riccardo, F.; et al. Initial impact of SARS-Cov-2 vaccination on healthcare workers in Italy–Update on the 28th of March 2021. Vaccine 2021, 39, 4788–4792. [Google Scholar] [CrossRef]
- Pitini, E.; Baccolini, V.; Rosso, A.; Massimi, A.; De Vito, C.; Marzuillo, C.; Villari, P. How public health professionals view mandatory vaccination in italy—A cross-sectional survey. Vaccines 2021, 9, 580. [Google Scholar] [CrossRef] [PubMed]
- Sindoni, A.; Baccolini, V.; Adamo, G.; Massimi, A.; Migliara, G.; De Vito, C.; Marzuillo, C.; Villari, P. Effect of the mandatory vaccination law on measles and rubella incidence and vaccination coverage in Italy (2013–2019). Hum. Vaccines Immunother. 2021. Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Italian Ministry of Health. Decree Law 105/2021. 2021. Available online: https://www.gazzettaufficiale.it/eli/id/2021/07/23/21G00117/sg (accessed on 3 October 2021).
- Baccolini, V.; Rosso, A.; Di Paolo, C.; Isonne, C.; Salerno, C.; Migliara, G.; Prencipe, G.; Massimi, A.; Marzuillo, C.; De Vito, C.; et al. What is the Prevalence of Low Health Literacy in European Union Member States? A Systematic Review and Meta-analysis. J. Gen. Intern. Med. 2021, 36, 753–761. [Google Scholar] [CrossRef] [PubMed]
- Adamo, G.; Baccolini, V.; Marzuillo, C.; Sturabotti, G.; Villari, P. Slow progress in measles and rubella elimination in Italy. Epid. Biost. Pub. Health 2016, 13, e120751–e120752. [Google Scholar]
- Napolitano, F.; Napolitano, P.; Liguori, G.; Angelillo, I.F. Human papillomavirus infection and vaccination: Knowledge and attitudes among young males in Italy. Hum. Vaccines Immunother. 2016, 12, 1504–1510. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adamo, G.; Baccolini, V.; Massimi, A.; Barbato, D.; Cocchiara, R.; Di Paolo, C.; Mele, A.; Cianfanelli, S.; Angelozzi, A.; Castellani, F.; et al. Towards elimination of measles and rubella in Italy: Progress and challenges. PLoS ONE 2019, 14, e0226513. [Google Scholar] [CrossRef] [PubMed]
- Caserotti, M.; Girardi, P.; Rubaltelli, E.; Tasso, A.; Lotto, L.; Gavaruzzi, T. Associations of COVID-19 risk perception with vaccine hesitancy over time for Italian residents. Soc. Sci. Med. 2021, 272, 113688. [Google Scholar] [CrossRef] [PubMed]
- Schneider, C.R.; Dryhurst, S.; Kerr, J.; Freeman, A.L.J.; Recchia, G.; Spiegelhalter, D.; van der Linden, S. COVID-19 risk perception: A longitudinal analysis of its predictors and associations with health protective behaviours in the United Kingdom. J. Risk Res. 2021, 24, 294–313. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control (ECDC). Guidelines for the Implementation of Non-Pharmaceutical Interventions against COVID-19; ECDC: Stockholm, Sweden, 2020. [Google Scholar]
- van Loenhout, J.A.F.; Vanderplanken, K.; Scheen, B.; Van den Broucke, S.; Aujoulat, I. Determinants of adherence to COVID-19 measures among the Belgian population: An application of the protection motivation theory. Arch. Pub. Health 2021, 79, 74. [Google Scholar] [CrossRef] [PubMed]
- Dal-re, R.; Stephens, R.; Sreeharan, N. Let me choose my COVID-19 vaccine. Eur. J. Intern. Med. 2021, 87, 104–105. [Google Scholar] [CrossRef] [PubMed]
- Kawata, K.; Nakabayashi, M. Determinants of COVID-19 vaccine preference: A survey study in Japan. SSM Pop Health 2021, 15, 100902. [Google Scholar] [CrossRef] [PubMed]
- Sprengholz, P.; Eitze, S.; Korn, L.; Siegers, R.; Betsch, C. The power of choice: Experimental evidence that freedom to choose a vaccine against COVID-19 improves willingness to be vaccinated. Eur. J. Intern. Med. 2021, 87, 106–108. [Google Scholar] [CrossRef] [PubMed]
| Survey Period | p-Value * | ||||
|---|---|---|---|---|---|
| #1 1 March– 12 March 2021 N = 1910 | #2 12 April– 9 May 2021 N = 1720 | #3 10 May– 30 June 2021 N = 1739 | |||
| Age (years) | 0.11 | ||||
| Mean (SD) | 23.5 (4.7) | 23.4 (4.5) | 23.5 (4.0) | ||
| Median (IQR) | 22 (21–25) | 22 (21–25) | 23 (21–25) | ||
| Gender | 0.007 | ||||
| Female | 1130 (59.2) | 1054 (61.3) | 1117 (64.2) | ||
| Male | 780 (40.8) | 666 (38.7) | 622 (35.8) | ||
| Nationality | <0.001 | ||||
| Italian | 1744 (91.3) | 1533 (89.1) | 1490 (85.7) | ||
| Non-Italian | 166 (8.7) | 187 (10.9) | 249 (14.3) | ||
| Area of study | |||||
| Healthcare | 574 (30.1) | 613 (35.6) | 356 (20.5) | <0.001 | |
| Science | 544 (28.5) | 421 (24.5) | 582 (33.5) | ||
| Other | 792 (41.5) | 686 (39.9) | 801 (46.1) | ||
| Year of study | <0.001 | ||||
| First or second | 870 (45.6) | 791 (46.0) | 689 (39.6) | ||
| Third or above | 1040 (54.4) | 929 (54.0) | 1050 (60.4) | ||
| Finances | 0.047 | ||||
| I have many difficulties | 101 (5.3) | 91 (5.2) | 107 (6.2) | ||
| I have some difficulties | 453 (27.3) | 473 (27.5) | 434 (25.0) | ||
| Managing well enough | 949 (49.7) | 825 (48.0) | 881 (50.7) | ||
| Managing very well | 407 (21.3) | 331 (19.2) | 317 (18.2) | ||
| Politics | 0.009 | ||||
| Moderate | 1022 (53.5) | 853 (49.6) | 837 (48.1) | ||
| Strongly left-wing | 237 (12.4) | 200 (11.6) | 214 (12.3) | ||
| Strongly right-wing | 13 (0.7) | 22 (1.3) | 21 (1.2) | ||
| I prefer not to answer | 638 (33.4) | 645 (37.5) | 667 (38.4) | ||
| Survey Period | |||||
|---|---|---|---|---|---|
| #1 1 March– 12 March 2021 N = 1910 | #2 12 April– 9 May 2021 N = 1720 | #3 10 May– 30 June 2021 N = 1739 | p-Value * | ||
| Perceived susceptibility to COVID-19 | 4.86 (2.2) | 4.50 (2.3) | 4.00 (2.3) | <0.001 | |
| Perceived COVID-19 severity | 7.76 (1.7) | 7.53 (1.9) | 7.34 (2.1) | <0.001 | |
| Concern about the COVID-19 emergency | 7.95 (1.8) | 7.58 (2.0) | 7.21 (2.2) | <0.001 | |
| COVID-19 infection | <0.001 | ||||
| No infection | 1842 (96.4) | 1614 (93.8) | 1624 (93.4) | ||
| Asymptomatic | 13 (0.7) | 20 (1.2) | 34 (2.0) | ||
| Mild symptoms | 40 (2.1) | 65 (3.8) | 49 (2.8) | ||
| Moderate/severe symptoms | 15 (0.8) | 21 (1.2) | 32 (1.8) | ||
| Vaccine hesitancy | <0.001 | ||||
| No hesitancy | 1489 (78.0) | 1246 (72.4) | 1237 (71.1) | ||
| Some degree of hesitancy | 421 (22.0) | 474 (27.6) | 502 (28.9) | ||
| Reasons for hesitancy (N = 1397) a | 0.382 | ||||
| I don’t believe in the safety of the vaccines available to me to date | 96 (22.8) | 93 (19.6) | 89 (17.7) | ||
| I don’t consider myself at risk | 76 (18.1) | 97 (20.5) | 87 (17.3) | ||
| I am aware of serious reactions that occurred to relatives/acquaintances after receiving the COVID-19 vaccination | 55 (13.1) | 114 (24.1) | 131 (26.1) | ||
| I don’t believe in the effectiveness of the vaccines available to me to date | 67 (15.9) | 31 (6.5) | 34 (6.8) | ||
| I don’t trust the authorities that encourage COVID-19 vaccination | 26 (6.2) | 20 (4.2) | 25 (5.0) | ||
| I prefer getting natural immunity to COVID-19 | 13 (3.1) | 26 (5.5) | 37 (7.4) | ||
| I have already had COVID-19 | 8 (1.8) | 21 (4.4) | 14 (2.8) | ||
| I am suffering from a clinical condition with contraindication to COVID-19 vaccination | 7 (1.7) | 8 (1.7) | 16 (3.1) | ||
| A person and/or an authority I trust encouraged me not to get vaccinated against COVID-19 | 5 (1.2) | 3 (0.6) | 6 (1.2) | ||
| I don’t believe in any vaccine including the COVID-19 vaccine | 3 (0.7) | 0 (0.0) | 2 (0.4) | ||
| Other reasons | 65 (15.4) | 61 (12.9) | 61 (12.2) | ||
| Confidence in vaccine safety | 8.05 (1.7) | 7.82 (1.7) | 7.54 (1.9) | <0.001 | |
| Confidence in vaccine effectiveness | 7.85 (1.6) | 7.9 (1.7) | 7.69 (1.9) | 0.054 | |
| Adherence to mask wearing indoors | 9.19 (1.4) | 9.13 (1.5) | 8.90 (1.8) | <0.001 | |
| Adherence to mask wearing outdoors | 8.67 (2.0) | 8.57 (2.1) | 8.19 (2.3) | <0.001 | |
| Performing hand hygiene | 8.55 (1.7) | 8.72 (1.8) | 8.57 (2.0) | <0.001 | |
| Maintaining physical distancing | 7.87 (1.8) | 7.75 (2.1) | 7.61 (2.1) | 0.025 | |
| Survey Period | ||||
|---|---|---|---|---|
| #2 12 April– 9 May 2021 N = 1720 | #3 10 May– 30 June 2021 N = 1739 | p-Value * | ||
| Prefer to choose which vaccine to take a | 6.76 (3.0) | 6.99 (3.0) | 0.005 | |
| Vaccine feature considered in the choice of vaccine a | 0.613 | |||
| Country of production of the vaccine or of the pharmaceutical company | 60 (3.8) | 77 (4.4) | ||
| Technology used or type of vaccine (mRNA, viral vector, etc.) | 318 (20.4) | 382 (22.0) | ||
| Higher efficacy in trials | 391 (25.0) | 401 (23.2) | ||
| Higher safety in trials | 350 (22.4) | 372 (21.4) | ||
| Fewer side effects reported as personal experiences | 407 (26.0) | 465 (26.8) | ||
| Other features | 38 (2.4) | 41 (2.4) | ||
| COVID-19 Vaccine Hesitancy | |||
|---|---|---|---|
| OR (95% CI) | p-Value | ||
| Survey period | |||
| #1 (1 March–12 March 2021) | Ref. | ||
| #2 (12 April–9 May 2021) | 1.25 (1.04–1.50) | 0.020 | |
| #3 (10 May–30 June 2021) | 0.99 (0.82–1.20) | 0.933 | |
| Age (years) | 1.01 (0.99–1.03) | 0.164 | |
| Gender | |||
| Female | Ref. | ||
| Male | 1.39 (1.18–1.64) | <0.001 | |
| Nationality | |||
| Italian | Ref. | ||
| Non-Italian | 1.23 (0.97–1.57) | 0.083 | |
| Area of study | |||
| Healthcare | Ref. | ||
| Science | 1.33 (1.08–1.64) | 0.007 | |
| Other | 1.40 (1.16–1.70) | <0.001 | |
| Year of study | |||
| Third or above | Ref. | ||
| First or second | 1.18 (1.01–1.38) | 0.049 | |
| Finances | |||
| Having some or many difficulties | Ref. | ||
| Managing well enough or very well | 1.07 (0.91–1.27) | 0.401 | |
| Politics | |||
| Moderate | Ref. | ||
| Strongly left-wing | 1.00 (0.77–1.29) | 0.999 | |
| Strongly right-wing | 1.10 (0.54–2.26) | 0.788 | |
| Prefer not to answer | 1.26 (1.08–1.49) | 0.004 | |
| Perceived susceptibility to COVID-19 | 1.03 (0.99–1.06) | 0.152 | |
| Perceived COVID-19 severity | 0.89 (0.85–0.94) | <0.001 | |
| Concern about the COVID-19 emergency | 0.93 (0.89–0.98) | 0.003 | |
| COVID-19 infection | |||
| No | Ref. | ||
| Yes | 1.08 (0.78–1.49) | 0.639 | |
| Confidence in vaccine safety | 0.56 (0.52–0.61) | <0.001 | |
| Confidence in vaccine effectiveness | 0.79 (0.73–0.86) | <0.001 | |
| Adherence to mask wearing indoors | 0.94 (0.89–0.99) | 0.013 | |
| Adherence to mask wearing outdoors | 0.92 (0.89–0.96) | <0.001 | |
| Performing hand hygiene | 0.98 (0.94–1.03) | 0.425 | |
| Maintaining physical distancing | 1.00 (0.96–1.05) | 0.994 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baccolini, V.; Renzi, E.; Isonne, C.; Migliara, G.; Massimi, A.; De Vito, C.; Marzuillo, C.; Villari, P. COVID-19 Vaccine Hesitancy among Italian University Students: A Cross-Sectional Survey during the First Months of the Vaccination Campaign. Vaccines 2021, 9, 1292. https://doi.org/10.3390/vaccines9111292
Baccolini V, Renzi E, Isonne C, Migliara G, Massimi A, De Vito C, Marzuillo C, Villari P. COVID-19 Vaccine Hesitancy among Italian University Students: A Cross-Sectional Survey during the First Months of the Vaccination Campaign. Vaccines. 2021; 9(11):1292. https://doi.org/10.3390/vaccines9111292
Chicago/Turabian StyleBaccolini, Valentina, Erika Renzi, Claudia Isonne, Giuseppe Migliara, Azzurra Massimi, Corrado De Vito, Carolina Marzuillo, and Paolo Villari. 2021. "COVID-19 Vaccine Hesitancy among Italian University Students: A Cross-Sectional Survey during the First Months of the Vaccination Campaign" Vaccines 9, no. 11: 1292. https://doi.org/10.3390/vaccines9111292
APA StyleBaccolini, V., Renzi, E., Isonne, C., Migliara, G., Massimi, A., De Vito, C., Marzuillo, C., & Villari, P. (2021). COVID-19 Vaccine Hesitancy among Italian University Students: A Cross-Sectional Survey during the First Months of the Vaccination Campaign. Vaccines, 9(11), 1292. https://doi.org/10.3390/vaccines9111292






