Predictors of COVID-19 Vaccination among Veterans Experiencing Homelessness
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Data Sources
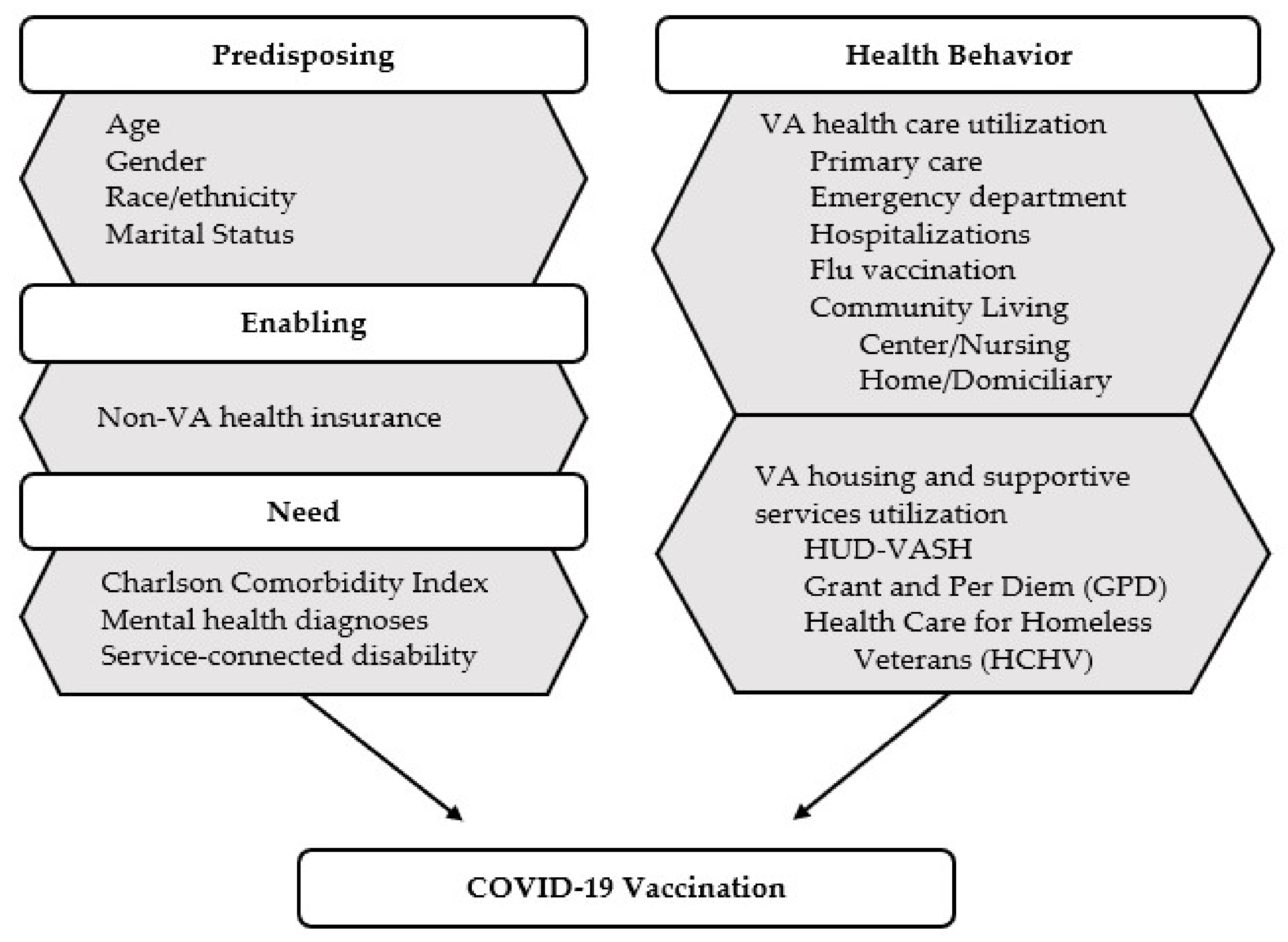
2.2. Conceptual Framework
2.3. Outcome Measure
2.4. Statistical Analyses
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Madhav, N.; Oppenheim, B.; Gallivan, M.; Mulembakani, P.; Rubin, E.; Wolfe, N. Pandemics: Risks, Impacts, and Mitigation. In Disease Control Priorities: Improving Health and Reducing Poverty, 3rd ed.; Jamison, D.T., Ed.; The International Bank for Reconstruction and Development/The World Bank: Washington, DC, USA, 2017; Volume 9, Chapter 17. [Google Scholar] [CrossRef] [Green Version]
- Centers for Disease Control and Prevention. People with Certain Medical Conditions. 12 May 2021. Available online: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html (accessed on 12 July 2021).
- Leung, C.S.; Ho, M.M.; Kiss, A.; Gundlapalli, A.V.; Hwang, S.W. Homelessness and the response to emerging infectious disease outbreaks: Lessons from SARS. J. Urban. Health 2008, 85, 402–410. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsai, J.; Wilson, M. COVID-19: A potential public health problem for homeless populations. Lancet Public Health 2020, 5, e186–e187. [Google Scholar] [CrossRef]
- National Alliance to End Homelessness. Homelessness and Racial Disparities. October 2020. Available online: https://endhomelessness.org/homelessness-in-america/what-causes-homelessness/inequality/ (accessed on 12 July 2021).
- Garg, S.; Kim, L.; Whitaker, M.; O’Halloran, A.; Cummings, C.; Holstein, R.; Prill, M.; Chai, S.J.; Kirley, P.D.; Alden, N.B.; et al. Hospitalization Rates and Characteristics of Patients Hospitalized with Laboratory-Confirmed Coronavirus Disease 2019—COVID-NET, 14 States, March 1–30, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 458–464. [Google Scholar] [CrossRef] [PubMed]
- Moakley, P. Deaths among America’s Homeless Are Soaring in the Pandemic. A Photographer Captures A Community in Crisis. 3 April 2021. Available online: https://time.com/5950759/homeless-deaths-rise-covid-19-west-virginia/ (accessed on 21 October 2021).
- Centers for Disease Control and Prevention. Interim Guidance for Health Departments: COVID-19 Vaccination Implementation for People Experiencing Homelessness. 30 April 2021. Available online: https://www.cdc.gov/coronavirus/2019-ncov/community/homeless-shelters/vaccination-guidance.html (accessed on 12 July 2021).
- U.S. Department of Veterans Affairs. SSVF COVID-19 Vaccine Planning. 29 January 2021. Available online: https://www.va.gov/HOMELESS/ssvf/docs/SSVF_COVID_19_Vaccine_Update.pdf (accessed on 12 July 2021).
- U.S. Department of Veterans Affairs. VA Announces Initial Plans for COVID-19 Vaccine Distribution. 10 December 2020. Available online: https://www.va.gov/opa/pressrel/pressrelease.cfm?id=5580 (accessed on 12 July 2021).
- U.S. Department of Veterans Affairs. VA Receives Janssen COVID-19 Vaccine. 4 March 2021. Available online: https://blogs.va.gov/VAntage/85596/va-receives-janssen-covid-19-vaccine/ (accessed on 12 July 2021).
- Young-Xu, Y.; Korves, C.; Roberts, J.; Powell, E.I.; Zwain, G.M.; Smith, J.; Izurieta, H.S. Coverage and Estimated Effectiveness of mRNA COVID-19 Vaccines among US Veterans. JAMA Netw Open. 2021, 4, e2128391. [Google Scholar] [CrossRef]
- Slack, D. COVID-19 Infections Double at VA Facilities as Agency Mandates Vaccines for Health Care Professionals. USA Today, 26 July 2021. Available online: https://www.usatoday.com/story/news/nation/2021/07/26/va-mandates-employee-vaccines-covid-infections-double/8084671002/ (accessed on 30 July 2021).
- Centers for Disease Control and Prevention. COVID-19 Vaccinations in the United States. 7 September 2021. Available online: https://covid.cdc.gov/covid-data-tracker/#vaccinations_vacc-total-admin-rate-total (accessed on 7 September 2021).
- Kendall, M. COVID Vaccinations Lag, Outbreaks Spread in Bay Area Homeless Shelters. The Mercury News, 13 July 2021. Available online: https://www.mercurynews.com/2021/07/19/covid-vaccination-rates-lag-outbreaks-spread-in-bay-area-homeless-shelters/ (accessed on 20 July 2021).
- O’Donnell, C. For Tampa Bay’s Homeless, Coronavirus Vaccine Can Be a Tough Sell. Tampa Bay Times, 19 July 2021. Available online: https://www.tampabay.com/news/health/2021/06/19/for-tampa-bays-homeless-coronavirus-vaccine-can-be-a-tough-sell/ (accessed on 12 July 2021).
- Pham, O.; Rudowitz, R.; Tolbert, J. Risks and Vaccine Access for Individuals Experiencing Homelessness: Key Issues to Consider 24 March 2021. Available online: https://www.kff.org/medicaid/issue-brief/covid-19-risks-vaccine-access-individuals-experiencing-homelessness-key-issues/ (accessed on 12 July 2021).
- Van Ness, L. States Fail to Prioritize Homeless People for Vaccines Stateline, 1 March 2021. Available online: https://www.pewtrusts.org/en/research-and-analysis/blogs/stateline/2021/03/01/states-fail-to-prioritize-homeless-people-for-vaccines. (accessed on 4 April 2021).
- Beers, L.; Filter, M.; McFarland, M. Increasing influenza vaccination acceptance in the homeless: A quality improvement project. Nurse Pract. 2019, 44, 48–54. [Google Scholar] [CrossRef]
- Kong, K.L.; Chu, S.; Giles, M.L. Factors influencing the uptake of influenza vaccine vary among different groups in the hard-to-reach population. Aust. N. Z. J. Public Health 2020, 44, 163–168. [Google Scholar] [CrossRef]
- Buechler, C.R.; Ukani, A.; Elsharawi, R.; Gable, J.; Petersen, A.; Franklin, M.; Chung, R.; Bell, J.; Manly, A.; Hefzi, N.; et al. Barriers, beliefs, and practices regarding hygiene and vaccination among the homeless during a hepatitis A outbreak in Detroit, MI. Heliyon 2020, 6, e03474. [Google Scholar] [CrossRef]
- Gin, J.L.; Balut, M.D.; Dobalian, A. COVID-19 Vaccine Hesitancy among Homeless Veterans in Transitional Housing. BMC Public Health 2021. under review. [Google Scholar]
- Kuhn, R.; Henwood, B.; Lawton, A.; Kleva, M.; Murali, K.; King, C.; Gelberg, L. COVID-19 vaccine access and attitudes among people experiencing homelessness from pilot mobile phone survey in Los Angeles, CA. PLoS ONE 2021, 16, e0255246. [Google Scholar] [CrossRef]
- Iacoella, C.; Ralli, M.; Maggiolini, A.; Arcangeli, A.; Ercoli, L. Acceptance of COVID-19 vaccine among persons experiencing homelessness in the City of Rome, Italy. Eur Rev. Med. Pharmacol. Sci. 2021, 25, 3132–3135. [Google Scholar] [CrossRef]
- Longchamps, C.; Ducarroz, S.; Crouzet, L.; Vignier, N.; Pourtau, L.; Allaire, C.; Colleville, A.C.; El Aarbaoui, T.; Melchior, M.; ECHO Study Group. COVID-19 vaccine hesitancy among persons living in homeless shelters in France. Vaccine 2021, 39, 3315–3318. [Google Scholar] [CrossRef]
- Gelberg, L.; Andersen, R.M.; Leake, B.D. The Behavioral Model for Vulnerable Populations: Application to medical care use and outcomes for homeless people. Health Serv. Res. 2000, 34, 1273–1302. [Google Scholar]
- Andersen, R.M. A Behavioral Model of Families’ Use of Health Services; Center for Health Administration Studies, University of Chicago: Chicago, IL, USA, 1968; Volume 25, p. xi-111. [Google Scholar]
- Andersen, R.M. Revisiting the behavioral model and access to medical care: Does it matter? J. Health Soc. Behav. 1995, 36, 1–10. [Google Scholar] [CrossRef]
- Gabrielian, S.; Jones, A.L.; Hoge, A.E.; deRussy, A.J.; Kim, Y.I.; Montgomery, A.E.; Blosnich, J.R.; Gordon, A.J.; Gelberg, L.; Austin, E.L.; et al. Primary Care Experiences for Homeless Patients with Serious Mental Illness: Results from a National Survey. J. Prim. Care Community Health 2021, 12, 2150132721993654. [Google Scholar] [CrossRef]
- Gabrielian, S.; Burns, A.V.; Nanda, N.; Hellemann, G.; Kane, V.; Young, A.S. Factors Associated With Premature Exits From Supported Housing. Psychiatr. Serv. 2016, 67, 86–93. [Google Scholar] [CrossRef] [Green Version]
- Jones, A.L.; Hausmann, L.; Haas, G.L.; Mor, M.K.; Cashy, J.P.; Schaefer, J.H.; Gordon, A.J. A national evaluation of homeless and non-homeless veterans’ experiences with primary care. Psychol. Serv. 2017, 14, 174–183. [Google Scholar] [CrossRef]
- Stein, J.A.; Nyamathi, A.M. Completion and subject loss within an intensive hepatitis vaccination intervention among homeless adults: The role of risk factors, demographics, and psychosocial variables. Health Psychol. 2010, 29, 317–323. [Google Scholar] [CrossRef] [Green Version]
- Gallardo, K.R.; Santa Maria, D.; Narendorf, S.; Markham, C.M.; Swartz, M.D.; Hsu, H.T.; Barman-Adhikari, A.; Bender, K.; Shelton, J.; Ferguson, K. Human Papillomavirus Vaccination Initiation and Completion among Youth Experiencing Homelessness in Seven U.S. Cities. Prev. Sci. 2020, 21, 937–948. [Google Scholar] [CrossRef]
- U.S. Centers for Medicare & Medicaid Services. Coding for COVID-19 Vaccine Shots 2021. Available online: https://www.cms.gov/medicare/covid-19/coding-covid-19-vaccine-shots (accessed on 4 August 2021).
- U.S. Department of Veterans Affairs. VA COVID-19 Shared Data Resource 2020. Available online: https://www.hsrd.research.va.gov/for_researchers/cyber_seminars/archives/3810-notes.pdf (accessed on 4 August 2021).
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- U.S. Department of Veterans Affairs. Federal Benefits for Veterans, Dependents and Survivors. 2015. Available online: https://www.va.gov/opa/publications/benefits_book/benefits_chap02.asp (accessed on 8 July 2021).
- U.S. Department of Veterans Affairs. VA Homeless Programs. 19 February 2019. Available online: https://www.va.gov/HOMELESS/housing.asp (accessed on 26 July 2021).
- U.S. Department of Veterans Affairs. VA Homeless Programs: Health Care for Homeless Veterans (HCHV) Program. 21 September 2020. Available online: https://www.va.gov/homeless/hchv.asp (accessed on 26 July 2021).
- U.S. Department of Veterans Affairs. Domiciliary Care for Homeless Veterans Program. 3 August 2021. Available online: https://www.va.gov/homeless/dchv.asp (accessed on 8 August 2021).
- U.S. Department of Veterans Affairs. Community Living Centers (VA Nursing Homes). 24 April 2020. Available online: https://www.va.gov/GERIATRICS/pages/VA_Community_Living_Centers.asp (accessed on 4 August 2021).
- MacDonald, N.E.; SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Quinn, S.; Jamison, A.; Musa, D.; Hilyard, K.; Freimuth, V. Exploring the Continuum of Vaccine Hesitancy between African American and White Adults: Results of a Qualitative Study. PLoS Curr. 2016, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Larson, H.J.; Jarrett, C.; Schulz, W.S.; Chaudhuri, M.; Zhou, Y.; Dube, E.; Schuster, M.; MacDonald, N.E.; Wilson, R.; SAGE Working Group on Vaccine Hesitancy. Measuring vaccine hesitancy: The development of a survey tool. Vaccine 2015, 33, 4165–4175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khubchandani, J.; Sharma, S.; Price, J.H.; Wiblishauser, M.J.; Sharma, M.; Webb, F.J. COVID-19 Vaccination Hesitancy in the United States: A Rapid National Assessment. J. Community Health 2021, 46, 270–277. [Google Scholar] [CrossRef] [PubMed]
- Settembrino, M.R. ‘Sometimes You Can’t Even Sleep at Night:’ Social Vulnerability to Disasters among Men Experiencing Homelessness in Central Florida. Int. J. Mass Emerg. Disasters 2017, 35, 30–48. [Google Scholar]
- Zimmerman, R.K.; Santibanez, T.A.; Janosky, J.E.; Fine, M.J.; Raymund, M.; Wilson, S.A.; Bardella, I.J.; Medsger, A.R.; Nowalk, M.P. What affects influenza vaccination rates among older patients? An analysis from inner-city, suburban, rural, and Veterans Affairs practices. Am. J. Med. 2003, 114, 31–38. [Google Scholar] [CrossRef]
- Bogart, L.M.; Ojikutu, B.O.; Tyagi, K.; Klein, D.J.; Mutchler, M.G.; Dong, L.; Lawrence, S.J.; Thomas, D.R.; Kellman, S. COVID-19 Related Medical Mistrust, Health Impacts, and Potential Vaccine Hesitancy among Black Americans Living with HIV. J. Acquir. Immune Defic. Syndr. 2021, 86, 200–207. [Google Scholar] [CrossRef]
- Chor, J.S.; Pada, S.K.; Stephenson, I.; Goggins, W.B.; Tambyah, P.A.; Clarke, T.W.; Medina, M.; Lee, N.; Leung, T.F.; Ngai, K.L.; et al. Seasonal influenza vaccination predicts pandemic H1N1 vaccination uptake among healthcare workers in three countries. Vaccine 2011, 29, 7364–7369. [Google Scholar] [CrossRef]
- Frew, P.M.; Painter, J.E.; Hixson, B.; Kulb, C.; Moore, K.; del Rio, C.; Esteves-Jaramillo, A.; Omer, S.B. Factors mediating seasonal and influenza A (H1N1) vaccine acceptance among ethnically diverse populations in the urban south. Vaccine 2012, 30, 4200–4208. [Google Scholar] [CrossRef] [Green Version]
- Gin, J.L.; Der-Martirosian, C.; Stanik, C.; Dobalian, A. Roadblocks to Housing after Disaster: Homeless Veterans’ Experiences after Hurricane Sandy. Nat. Hazards Rev. 2019, 20, 04019005. [Google Scholar] [CrossRef] [Green Version]
- Gin, J.L.; Balut, M.D.; Der-Martirosian, C.; Dobalian, A. Managing the unexpected: The role of homeless service providers during the 2017–2018 California wildfires. J. Community Psychol. 2021, 49, 2532–2547. [Google Scholar] [CrossRef]
- Culhane, D.P.; Metraux, S.; Hadley, T. Public service reductions associated with placement of homeless persons with severe mental illness in supportive housing. Hous. Policy Debate 2002, 13, 107–163. [Google Scholar] [CrossRef] [Green Version]
- Tsemberis, S.; Gulcur, L.; Nakae, M. Housing first, consumer choice, and harm reduction for homeless individuals with a dual diagnosis. Am. J. Public Health 2004, 94, 651–656. [Google Scholar] [CrossRef]
- O’Toole, T.P.; Pirraglia, P.A.; Dosa, D.; Bourgault, C.; Redihan, S.; O’Toole, M.B.; Blumen, J.; Primary Care-Special Populations Treatment Team. Building care systems to improve access for high-risk and vulnerable veteran populations. J. Gen. Intern. Med. 2011, 26 (Suppl. 2), 683–688. [Google Scholar] [CrossRef] [Green Version]
- Kirzinger, A.; Sparks, G.; Hamel, L.; Lopes, L.; Kearney, A.; Stokes, M.; Brodie, M. KFF COVID-19 Vaccine Monitor: July 2021. 4 August 2021. Available online: https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-july-2021/ (accessed on 16 August 2021).
- Reback, C.J.; Larkins, S.; Shoptaw, S. Methamphetamine abuse as a barrier to HIV medication adherence among gay and bisexual men. AIDS Care 2003, 15, 775–785. [Google Scholar] [CrossRef]
- Reback, C.J.; Kamien, J.B.; Amass, L. Characteristics and HIV risk behaviors of homeless, substance-using men who have sex with men. Addict. Behav. 2007, 32, 647–654. [Google Scholar] [CrossRef]
- Rodriguez-Barradas, M.C.; Goulet, J.; Brown, S.; Goetz, M.B.; Rimland, D.; Simberkoff, M.S.; Crothers, K.; Justice, A.C. Impact of pneumococcal vaccination on the incidence of pneumonia by HIV infection status among patients enrolled in the Veterans Aging Cohort 5-Site Study. Clin. Infect. Dis. 2008, 46, 1093–1100. [Google Scholar] [CrossRef]
- U.S. Department of Veterans Affairs. COVID-19 National Summary. 19 October 2021. Available online: https://www.accesstocare.va.gov/Healthcare/COVID19NationalSummary (accessed on 21 October 2021).
- Liebermann, O.; Kaufman, E. US military Says a Third of Troops Opt out of Being Vaccinated, but the Numbers Suggest It’s More CNN, 19 March 2021. Available online: https://www.cnn.com/2021/03/19/politics/us-military-vaccinations/index.html (accessed on 13 July 2021).
- Steinhauer, J. Military and V.A Struggle with Vaccination Rates in Their Ranks The New York Times, 2 July 2021. Available online: https://www.nytimes.com/2021/07/01/us/politics/military-va-vaccines.html (accessed on 13 July 2021).
- Der-Martirosian, C.; Strine, T.; Atia, M.; Chu, K.; Mitchell, M.N.; Dobalian, A. General household emergency preparedness: A comparison between veterans and nonveterans. Prehosp. Disaster Med. 2014, 29, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Kranke, D.; Gin, J.; Saia, R.; Heslin, K.; Dobalian, A. A qualitative investigation that applies an ecological strengths-based perspective to veterans’ experience of reintegration into civilian life. Mil. Behav. Health 2016, 4, 75–81. [Google Scholar] [CrossRef]
- Heslin, K.C.; Riopelle, D.; Gin, J.L.; Ordunez, J.; Naranjo, D.E.; Dobalian, A. Confidence in the fairness of local public health systems’ response to disasters: The US Veterans’ perspective. Disaster Med. Public Health Prep. 2013, 7, 75–81. [Google Scholar] [CrossRef]
- Institute of Medicine (US) Committee on Health Care for Homeless People. Health Care Services for Homeless People. In Homelessness, Health, and Human Needs; National Academies Press (US): Washington, DC, USA, 1988; Chapter 5. Available online: https://www.ncbi.nlm.nih.gov/books/NBK218235/ (accessed on 16 August 2021).
- Oreskes, B. Vaccinating the Homeless Population for COVID Adds a Whole New Layer of Difficulty Los Angeles Times. 15 February 2021. Available online: https://www.latimes.com/homeless-housing/story/2021-02-15/la-homeless-covid-vaccine-distribution-extra-difficult (accessed on 16 August 2021).
- U.S. Department of Housing and Urban Development. The 2020 Annual Homeless Assessment Report (AHAR) to Congress. January 2021. Available online: https://www.huduser.gov/portal/sites/default/files/pdf/2020-AHAR-Part-1.pdf (accessed on 13 July 2021).
- National Alliance to End Homelessness. New Report Shows Rise in Homelessness in Advance of COVID-19 Crisis. 19 March 2021. Available online: https://endhomelessness.org/new-report-shows-rise-in-homelessness-in-advance-of-covid-19-crisis/ (accessed on 26 July 2021).
- Oreskes, B. Mass Unemployment over Coronavirus Could Lead to a 45% Jump in Homelessness, Study Finds Los Angeles Times, 14 May 2020. Available online: https://www.latimes.com/homeless-housing/story/2020-05-14/coronavirus-unemployment-homeless-study-increase-45-percent (accessed on 26 July 2021).
- CBS News. Almost all New COVID-19 Cases Are among People Who Have Not Been Vaccinated. 10 July 2021. Available online: https://www.cbsnews.com/news/new-covid-19-cases-united-states-almost-all-among-people-unvaccinated/ (accessed on 23 July 2021).
| Patient Characteristics | % Population | % COVID Vaccinated | |
|---|---|---|---|
| N = 83,528 | 45.8% | ||
| Age Categories: | 18–44 | 24.1% | 28.1% |
| 45–64 | 52.5% | 49.2% | |
| 65–74 | 19.8% | 56.7% | |
| 75+ | 3.6% | 55.7% | |
| Gender | Male | 90.4% | 37.8% |
| Female | 9.6% | 46.6% | |
| Race/Ethnicity | Hispanic or Latino | 6.7% | 48.2% |
| Non-Hispanic Other | 2.8% | 44.0% | |
| Non-Hispanic African American | 37.1% | 47.3% | |
| Non-Hispanic White | 47.6% | 45.5% | |
| Unknown | 5.7% | 38.7% | |
| Marital Status | Married | 13.9% | 42.1% |
| Not Married | 86.1% | 46.6% | |
| Health Insurance (non-VA) | Yes | 36.0% | 54.4% |
| No | 64.0% | 41.0% | |
| Flu Shot 2019–2020 | Yes | 29.3% | 63.6% |
| No | 70.7% | 38.4% | |
| Any Service-Connected Disability | Yes | 49.6% | 45.3% |
| No | 50.4% | 46.4% | |
| Community Living Centers/Nursing Homes/Domiciliary | Yes | 6.0% | 74.7% |
| No | 94.0% | 44.0% | |
| Any Mental Health Diagnoses | Yes | 84.6% | 47.2% |
| No | 15.4% | 38.3% | |
| Charlson Comorbidity Score | 0 | 46.0% | 35.1% |
| 1 | 20.4% | 48.8% | |
| 2+ | 33.6% | 58.7% | |
| Primary Care Visits | 0–2 | 37.1% | 32.6% |
| 3–5 | 25.5% | 47.2% | |
| 6+ | 37.4% | 58.0% | |
| Emergency Department Visits | 0–5 | 89.9% | 44.7% |
| 6+ | 10.1% | 56.1% | |
| Any Hospitalization | Yes | 33.7% | 52.0% |
| No | 66.3% | 42.7% | |
| HUD-VASH | Yes | 48.6% | 51.5% |
| No | 51.4% | 40.5% | |
| Health Care for Homeless Veterans (HCHV) | Yes | 25.2% | 53.2% |
| No | 74.8% | 43.3% | |
| Grant and Per Diem (GPD) | Yes | 9.4% | 60.7% |
| No | 90.6% | 44.3% | |
| Patient Characteristics | Adjusted % COVID Vaccinated | Non-Reference vs. Reference (ref) Difference in % COVID Vaccinated (95% CI) | |
|---|---|---|---|
| Age Categories: | 18–44 (ref) | 34.3% | N/A |
| 45–64 | 48.2% | 13.8% (12.7%, 15.0%) | |
| 65–74 | 52.3% | 17.9% (16.4%, 19.4%) | |
| 75+ | 51.7% | 17.4% (15.0–19.7%) | |
| Gender | Male | 42.8% | −3.4% (−4.5%, −2.4%) |
| Female (ref) | 46.3% | N/A | |
| Race/Ethnicity | Hispanic or Latino | 50.2% | 5.0% (0.3%, 6.8%) |
| Non-Hispanic Other | 47.0% | 1.8% (−1.3%, 4.9%) ns | |
| Non-Hispanic African American | 46.4% | 1.3% (0.2%, 2.3%) | |
| Non-Hispanic White (ref) | 45.2% | N/A | |
| Unknown | 44.0% | −1.1% (−2.9%, 0.5%) ns | |
| Marital Status | Married | 45.1% | −1.0% (−2.0%, 0.0%) ns |
| Not Married (ref) | 46.1% | N/A | |
| Health Insurance (non-VA) | Yes | 48.4% | 3.8% (2.9%, 4.7%) |
| No (ref) | 44.5% | N/A | |
| Flu Shot 2019–2020 | Yes | 58.3% | 17.5% (16.6%, 18.5%) |
| No (ref) | 40.7% | N/A | |
| Any Service-Connected Disability | Yes | 47.1% | 2.3% (1.7%, 2.9%) |
| No (ref) | 44.8% | N/A | |
| Community Living Centers/Nursing Homes/Domiciliary | Yes | 70.9% | 26.6% (24.5%, 28.7%) |
| No (ref) | 44.4% | N/A | |
| Any Mental Health Diagnoses | Yes | 46.2% | 1.6% (0.3%, 2.8%) |
| No (ref) | 44.6% | N/A | |
| Charlson Comorbidity Score | 0 (ref) | 42.9% | N/A |
| 1 | 46.6% | 3.8% (2.7%, 4.7%) | |
| 2+ | 49.4% | 6.5% (5.6%, 7.4%) | |
| Primary Care Visits | 0–2 (ref) | 38.5% | N/A |
| 3–5 | 47.0% | 8.5% (7.7%, 9.4%) | |
| 6+ | 52.3% | 13.9% (12.8%, 15.0%) | |
| Emergency Department Visits | 0–5 (ref) | 45.9% | N/A |
| 6+ | 46.1% | 0.1% (−1.2%, 1.5%) ns | |
| Any Hospitalization | Yes | 46.1% | 0.1% (−0.7%, 1.1%) ns |
| No (ref) | 45.9% | N/A | |
| HUD-VASH | Yes | 50.7% | 9.3% (8.0%, 10.5%) |
| No (ref) | 41.4% | N/A | |
| Health Care for Homeless Veterans (HCHV) | Yes | 49.3% | 4.4% (3.3%, 5.5%) |
| No (ref) | 44.8% | N/A | |
| Grant and Per Diem (GPD) | Yes | 57.1% | 12.3% (10.6%, 14.1%) |
| No (ref) | 44.8% | N/A | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Balut, M.D.; Chu, K.; Gin, J.L.; Dobalian, A.; Der-Martirosian, C. Predictors of COVID-19 Vaccination among Veterans Experiencing Homelessness. Vaccines 2021, 9, 1268. https://doi.org/10.3390/vaccines9111268
Balut MD, Chu K, Gin JL, Dobalian A, Der-Martirosian C. Predictors of COVID-19 Vaccination among Veterans Experiencing Homelessness. Vaccines. 2021; 9(11):1268. https://doi.org/10.3390/vaccines9111268
Chicago/Turabian StyleBalut, Michelle D., Karen Chu, June L. Gin, Aram Dobalian, and Claudia Der-Martirosian. 2021. "Predictors of COVID-19 Vaccination among Veterans Experiencing Homelessness" Vaccines 9, no. 11: 1268. https://doi.org/10.3390/vaccines9111268
APA StyleBalut, M. D., Chu, K., Gin, J. L., Dobalian, A., & Der-Martirosian, C. (2021). Predictors of COVID-19 Vaccination among Veterans Experiencing Homelessness. Vaccines, 9(11), 1268. https://doi.org/10.3390/vaccines9111268






