Estimation of Reduction in Influenza Vaccine Effectiveness Due to Egg-Adaptation Changes—Systematic Literature Review and Expert Consensus
Abstract
:1. Introduction
2. Methods
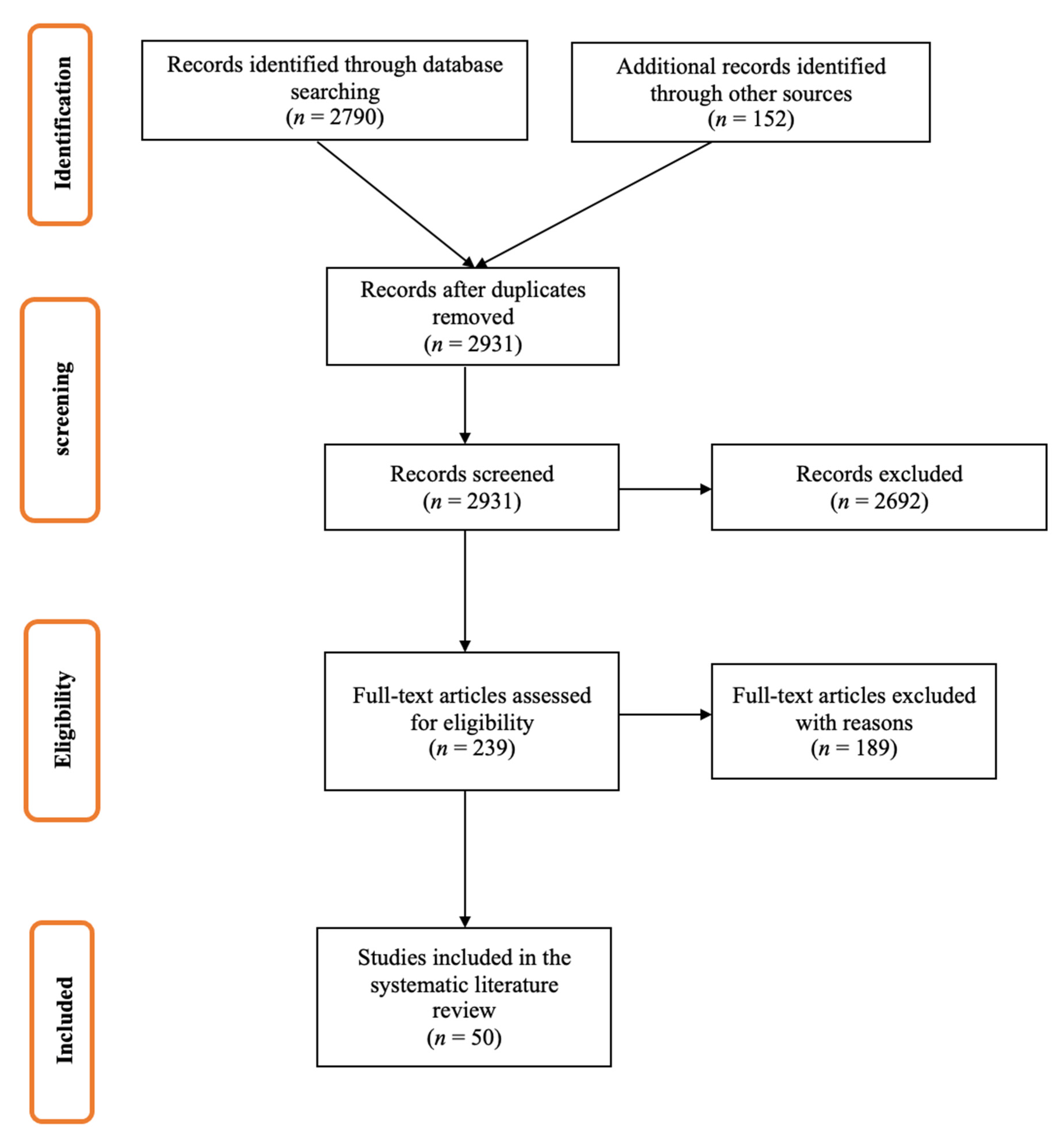
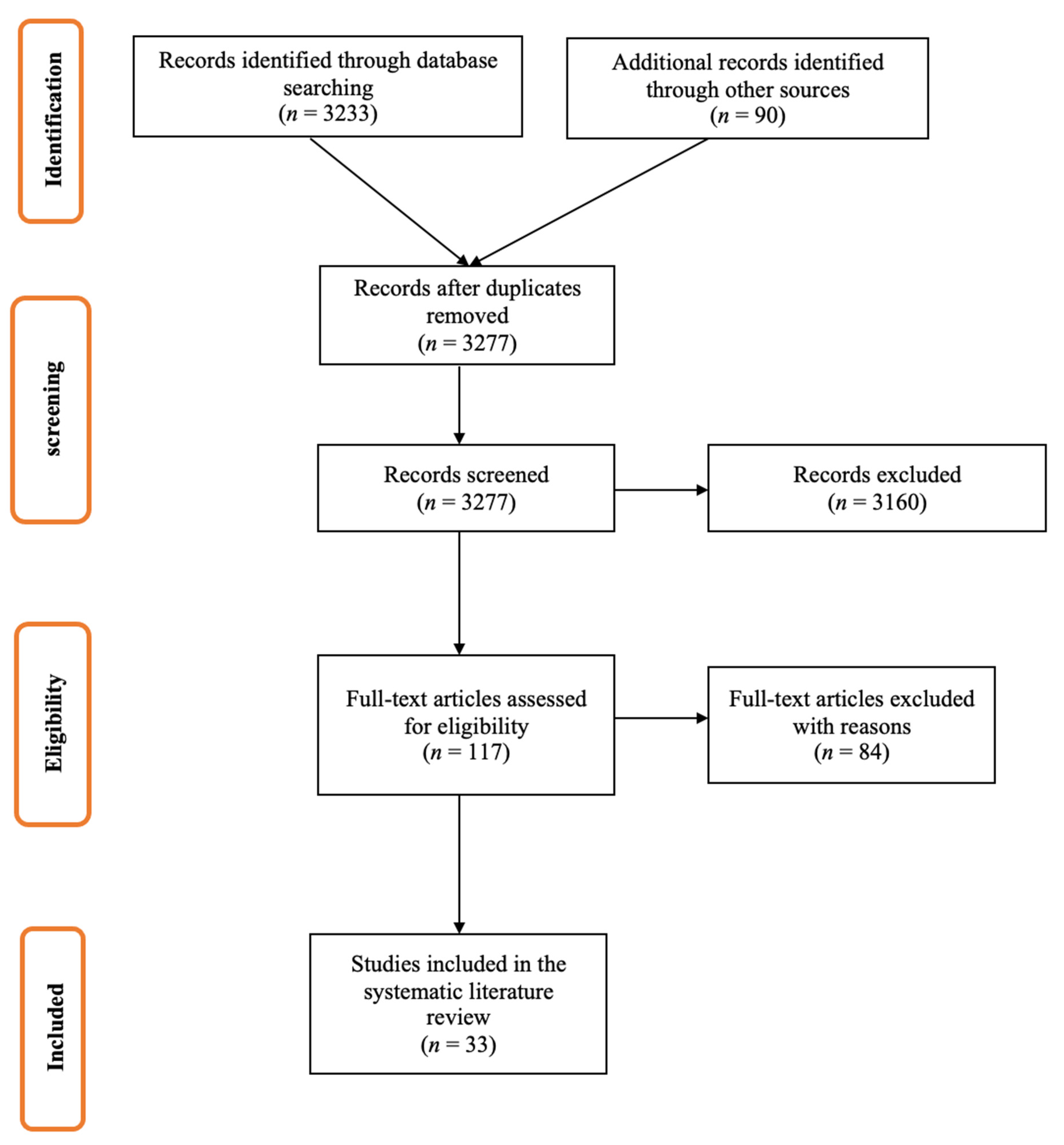
2.1. Systematic Literature Reviews
2.2. Assessment of Expert Opinion
3. Results
3.1. Participants
3.2. Systematic Literature Review
3.3. Survey of Expert Opinion
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Influenza (Sub)Type | Age Group | The Average Increase in Influenza Vaccine Effectiveness without Egg Adaptations (%) | |||||
|---|---|---|---|---|---|---|---|
| ES | IT | DE | UK | FR | EU5 CAT | ||
| A(H3N2) | <18 year | 14 | 26 | 13 | 30 | 8 | 15 |
| 18–64 year | 17 | 23 | 13 | 30 | 8 | 16 | |
| ≥65 year | 14 | 21 | 13 | 10 | 8 | 12 | |
| A(H1N1pdm) | <18 year | 7 | 5 | 5 | 15 | 5 | 7 |
| 18–64 year | 7 | 4 | 5 | 13 | 5 | 7 | |
| ≥65 year | 6 | 4 | 5 | 3 | 5 | 5 | |
| B/Yamagata | <18 year | 4 | 5 | 5 | 15 | 5 | 6 |
| 18–64 year | 4 | 4 | 5 | 8 | 5 | 5 | |
| ≥65 year | 3 | 3 | 5 | 3 | 5 | 4 | |
| B/Victoria | <18 year | 4 | 5 | 5 | 15 | 5 | 6 |
| 18–64 year | 4 | 4 | 5 | 8 | 5 | 5 | |
| ≥65 year | 3 | 3 | 5 | 3 | 5 | 4 | |
| All strains | <18 year | 8 | 11 | 8 | 15 | 7 | 8 |
| 18–64 year | 12 | 9 | 8 | 23 | 7 | 10 | |
| ≥65 year | 8 | 9 | 8 | 3 | 7 | 6 | |
| Influenza (sub)Type | Age Group | The Average Increase in Influenza Vaccine Effectiveness without Antigenic Drift (%) | |||||
|---|---|---|---|---|---|---|---|
| ES | IT | DE | UK | FR | EU5 CAT | ||
| A(H3N2) | <18 year | 15 | 23 | 15 | 30 | 20 | 20 |
| 18–64 year | 13 | 18 | 15 | 10 | 20 | 15 | |
| ≥65 year | 10 | 18 | 15 | 10 | 15 | 17 | |
| A(H1N1pdm) | >18 year | 8 | 10 | 7 | 10 | 10 | 9 |
| 18–64 year | 4 | 9 | 7 | 5 | 10 | 8 | |
| ≥65 year | 2 | 9 | 7 | 5 | 7 | 5 | |
| B/Yamagata | >18 year | 7 | 13 | 7 | 10 | 10 | 8 |
| 18–64 year | 3 | 9 | 7 | 5 | 10 | 6 | |
| ≥65 year | 2 | 8 | 7 | 5 | 10 | 6 | |
| B/Victoria | <18 year | 7 | 13 | 7 | 10 | 10 | 8 |
| 18–64 year | 3 | 9 | 7 | 5 | 10 | 6 | |
| ≥65 year | 2 | 8 | 7 | 5 | 10 | 6 | |
| All strains | <18 year | 7 | 15 | 10 | 10 | 10 | 10 |
| 18–64 year | 10 | 13 | 10 | 5 | 10 | 10 | |
| ≥65 year | 9 | 13 | 10 | 5 | 10 | 9 | |
| Influenza (Sub)Type | The Average Increase in Vaccine Match without Antigenic Drift (%) | |||||
|---|---|---|---|---|---|---|
| ES | IT | DE | UK | FR | EU5 CAT | |
| A(H3N2) | 20 | 30 | 24 | 19 | 15 | 24 |
| A(H1N1pdm) | 10 | 5 | 17 | 0 | 5 | 8 |
| B/Yamagata | 12 | 10 | 17 | 0 | 5 | 10 |
| B/Victoria | 12 | 10 | 17 | 5 | 5 | 10 |
| All strains | 20 | 19 | 17 | 19 | 15 | 19 |
| Influenza (Sub)Type | The Average Increase in Vaccine Match without Egg Adaptations (%) | |||||
|---|---|---|---|---|---|---|
| ES | IT | DE | UK | FR | EU5 CAT | |
| A(H3N2) | 29 | 34 | 9 | 25 | 12 | 21 |
| A(H1N1pdm) | 12 | 7 | 6 | 10 | 5 | 8 |
| B/Yamagata | 12 | 7 | 6 | 5 | 5 | 7 |
| B/Victoria | 12 | 8 | 6 | 5 | 5 | 7 |
| All strains | 23 | 23 | 6 | 25 | 13 | 18 |
References
- Clayville, L.R. Influenza update: A review of currently available vaccines. Pharm. Ther. 2011, 36, 659–684. [Google Scholar]
- Boslaugh, S. Encyclopedia of Epidemiology; Sage Publications: Los Angeles, CA, USA, 2008. [Google Scholar]
- Pérez Rubio, A.; Eiros, J.M. Cell culture-derived flu vaccine: Present and future. Hum. Vaccines Immunother. 2018, 14, 1874–1882. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Uhart, M.; Bricout, H.; Clay, E.; Largeron, N. Public health and economic impact of seasonal influenza vaccination with quadrivalent influenza vaccines compared to trivalent influenza vaccines in Europe. Hum. Vaccines Immunother. 2016, 12, 2259–2268. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- European Centre for Disease Prevention and Control. Factsheet about Seasonal Influenza. Available online: https://www.cdc.gov/flu/about/keyfacts.htm (accessed on 15 November 2020).
- Preaud, E.; Durand, L.; Macabeo, B.; Farkas, N.; Sloesen, B.; Palache, A.; Shupo, F.; Samson, S.I. Annual public health and economic benefits of seasonal influenza vaccination: A European estimate. BMC Public Health 2014, 14, 813. [Google Scholar] [CrossRef] [Green Version]
- Rajaram, S.; Wojcik, R.; Moore, C.; Ortiz de Lejarazu, R.; de Lusignan, S.; Montomoli, E.; Rossi, A.; Pérez-Rubio, A.; Trilla, A.; Baldo, V.; et al. The impact of candidate influenza virus and egg-based manufacture on vaccine effectiveness: Literature review and expert consensus. Vaccine 2020, 38, 6047–6056. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Vaccine Effectiveness: How Well Do the Flu Vaccines Work? Available online: https://www.cdc.gov/flu/vaccines-work/vaccineeffect.htm (accessed on 20 December 2020).
- Belongia, E.A.; McLean, H.Q. Influenza Vaccine Effectiveness: Defining the H3N2 Problem. Clin. Infect. Dis. 2019, 69, 1817–1823. [Google Scholar] [CrossRef]
- Belongia, E.A.; Simpson, M.D.; King, J.P.; Sundaram, M.E.; Kelley, N.S.; Osterholm, M.T.; McLean, H.Q. Variable influenza vaccine effectiveness by subtype: A systematic review and meta-analysis of test-negative design studies. Lancet Infect. Dis. 2016, 16, 942–951. [Google Scholar] [CrossRef]
- Jester, B.J.; Uyeki, T.M.; Jernigan, D.B. Fifty Years of Influenza A(H3N2) Following the Pandemic of 1968. Am. J. Public Health 2020, 110, 669–676. [Google Scholar] [CrossRef]
- Thompson, M.; Shay, D.; Zhou, H.; Bridges, C.; Cheng, P.; Burns, E.; Bresee, J.; Cox, N. Estimates of deaths associated with seasonal influenza-United States, 1976-2007. Morb. Mortal. Wkly. Rep. 2010, 59, 1057–1062. [Google Scholar]
- Jang, H.; Ross, T.M. Preexisting influenza specific immunity and vaccine effectiveness. Expert Rev. Vaccines 2019, 18, 1043–1051. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. How Flu Vaccine Effectiveness and Efficacy are Measured. Available online: https://www.cdc.gov/flu/vaccines-work/effectivenessqa.htm (accessed on 20 December 2020).
- Barr, I.G.; Donis, R.O.; Katz, J.M.; McCauley, J.W.; Odagiri, T.; Trusheim, H.; Tsai, T.F.; Wentworth, D.E. Cell culture-derived influenza vaccines in the severe 2017–2018 epidemic season: A step towards improved influenza vaccine effectiveness. NPJ Vaccines 2018, 3, 44. [Google Scholar] [CrossRef]
- Skowronski, D.M.; Janjua, N.Z.; De Serres, G.; Sabaiduc, S.; Eshaghi, A.; Dickinson, J.A.; Fonseca, K.; Winter, A.-L.; Gubbay, J.B.; Krajden, M.; et al. Low 2012–13 Influenza Vaccine Effectiveness Associated with Mutation in the Egg-Adapted H3N2 Vaccine Strain Not Antigenic Drift in Circulating Viruses. PLoS ONE 2014, 9, e92153. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harding, A.T.; Heaton, N.S. Efforts to Improve the Seasonal Influenza Vaccine. Vaccines 2018, 6, 19. [Google Scholar] [CrossRef] [Green Version]
- Burnet, F.; Bull, D.H. Changes in influenza virus associated with adaptation to passage in chick embryos. Aust. J. Exp. Biol. Med Sci. 1943, 21, 55–69. [Google Scholar] [CrossRef]
- Cianci, R.; Newton, E.E.; Pagliari, D. Efforts to Improve the Seasonal Influenza Vaccine. Vaccines 2020, 8, 645. [Google Scholar] [CrossRef] [PubMed]
- Wu, N.C.; Lv, H.; Thompson, A.J.; Wu, D.C.; Ng, W.W.S.; Kadam, R.U.; Lin, C.W.; Nycholat, C.M.; McBride, R.; Liang, W.; et al. Preventing an Antigenically Disruptive Mutation in Egg-Based H3N2 Seasonal Influenza Vaccines by Mutational Incompatibility. Cell Host Microbe 2019, 25, 836–844.e835. [Google Scholar] [CrossRef] [Green Version]
- Liu, F.; Tzeng, W.P.; Horner, L.; Kamal, R.P.; Tatum, H.R.; Blanchard, E.G.; Xu, X.; York, I.; Tumpey, T.M.; Katz, J.M.; et al. Influence of Immune Priming and Egg Adaptation in the Vaccine on Antibody Responses to Circulating A(H1N1)pdm09 Viruses After Influenza Vaccination in Adults. J. Infect. Dis. 2018, 218, 1571–1581. [Google Scholar] [CrossRef]
- Raymond, D.D.; Stewart, S.M.; Lee, J.; Ferdman, J.; Bajic, G.; Do, K.T.; Ernandes, M.J.; Suphaphiphat, P.; Settembre, E.C.; Dormitzer, P.R.; et al. Influenza immunization elicits antibodies specific for an egg-adapted vaccine strain. Nat. Med. 2016, 22, 1465–1469. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Cell-Based Flu Vaccines | CDC. Available online: https://www.cdc.gov/flu/prevent/how-fluvaccine-made.htm (accessed on 20 December 2020).
- Kissling, E.; Pozo, F.; Buda, S.; Vilcu, A.-M.; Rizzo, C.; Gherasim, A.; Horváth, J.K.; Brytting, M.; Domegan, L.; Meijer, A.; et al. Effectiveness of influenza vaccine against influenza A in Europe in seasons of different A(H1N1)pdm09 and the same A(H3N2) vaccine components (2016–2017 and 2017–2018). Vaccine X 2019, 3, 100042. [Google Scholar] [CrossRef] [PubMed]
- Skowronski, D.M.; Leir, S.; Sabaiduc, S.; Chambers, C.; Zou, M.; Rose, C.; Olsha, R.; Dickinson, J.A.; Winter, A.-L.; Jassem, A.; et al. Influenza Vaccine Effectiveness by A(H3N2) Phylogenetic Subcluster and Prior Vaccination History: 2016–2017 and 2017–2018 Epidemics in Canada. J. Infect. Dis. 2020. [Google Scholar] [CrossRef] [Green Version]
- Skowronski, D.M.; Chambers, C.; Sabaiduc, S.; De Serres, G.; Dickinson, J.A.; Winter, A.L.; Drews, S.J.; Fonseca, K.; Charest, H.; Gubbay, J.B.; et al. Interim estimates of 2014/15 vaccine effectiveness against influenza A(H3N2) from Canada’s Sentinel Physician Surveillance Network, January 2015. Eurosurveillance 2015, 20, 21022. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klein, N.P.; Fireman, B.; Goddard, K.; Zerbo, O.; Asher, J.; Zhou, J.; King, J.; Lewis, N. Vaccine effectiveness of cell-culture relative to egg-based inactivated influenza vaccine during the 2017–2018 influenza season. PLoS ONE 2020, 15, e0229279. [Google Scholar] [CrossRef] [Green Version]
- Boikos, C.; Sylvester, G.C.; Sampalis, J.S.; Mansi, J.A. Relative Effectiveness of the Cell-Cultured Quadrivalent Influenza Vaccine Compared to Standard, Egg-derived Quadrivalent Influenza Vaccines in Preventing Influenza-like Illness in 2017–2018. Clin. Infect. Dis. 2020, 71, e665–e671. [Google Scholar] [CrossRef] [PubMed]
- Izurieta, H.S.; Chillarige, Y.; Kelman, J.; Wei, Y.; Lu, Y.; Xu, W.; Lu, M.; Pratt, D.; Chu, S.; Wernecke, M.; et al. Relative Effectiveness of Cell-Cultured and Egg-Based Influenza Vaccines among Elderly Persons in the United States, 2017–2018. J. Infect. Dis. 2019, 220, 1255–1264. [Google Scholar] [CrossRef]
- Divino, V.; Krishnarajah, G.; Pelton, S.I.; Mould-Quevedo, J.; Anupindi, V.R.; DeKoven, M.; Postma, M.J. A real-world study evaluating the relative vaccine effectiveness of a cell-based quadrivalent influenza vaccine compared to egg-based quadrivalent influenza vaccine in the US during the 2017–2018 influenza season. Vaccine 2020, 38, 6334–6343. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [Green Version]
- Centers for Disease Control and Prevention. How Influenza (Flu) Vaccines Are Made. Available online: https://www.cdc.gov/flu/prevent/how-fluvaccine-made.htm (accessed on 20 May 2021).
- Krietsch Boerner, L. The Flu Shot and the Egg. ACS Cent. Sci. 2020, 6, 89–92. [Google Scholar] [CrossRef] [Green Version]
- Hohmann, E.; Brand, J.C.; Rossi, M.J.; Lubowitz, J.H. Expert Opinion Is Necessary: Delphi Panel Methodology Facilitates a Scientific Approach to Consensus. Arthroscopy 2018, 34, 349–351. [Google Scholar] [CrossRef] [Green Version]
- Jandhyala, R. A novel method for observing proportional group awareness and consensus of items arising from list-generating questioning. Curr. Med. Res. Opin. 2020, 36, 883. [Google Scholar] [CrossRef] [Green Version]
- Rajaram, S.; Boikos, C.; Gelone, D.K.; Gandhi, A. Influenza vaccines: The potential benefits of cell-culture isolation and manufacturing. Ther. Adv. Vaccines Immunother. 2020, 8, 1–10. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. People at Higher Risk of Flu Complications. Available online: https://www.cdc.gov/flu/highrisk/index.htm (accessed on 20 May 2021).
- Putri, W.; Muscatello, D.J.; Stockwell, M.S.; Newall, A.T. Economic burden of seasonal influenza in the United States. Vaccine 2018, 36, 3960–3966. [Google Scholar] [CrossRef] [PubMed]
- Rajaram, S.; Van Boxmeer, J.; Leav, B.; Suphaphiphat, P.; Iheanacho, I.; Kistler, K. 2556. Retrospective Evaluation of Mismatch From Egg-Based Isolation of Influenza Strains Compared With Cell-Based Isolation and the Possible Implications for Vaccine Effectiveness. Open Forum Infect. Dis. 2018, 5, S69. [Google Scholar] [CrossRef] [Green Version]
- Vogel, A.B.; Lambert, L.; Kinnear, E.; Busse, D.; Erbar, S.; Reuter, K.C.; Wicke, L.; Perkovic, M.; Beissert, T.; Haas, H.; et al. Self-Amplifying RNA Vaccines Give Equivalent Protection against Influenza to mRNA Vaccines but at Much Lower Doses. Mol. Ther. 2018, 26, 446–455. [Google Scholar] [CrossRef] [Green Version]

| Influenza (Sub)Type | Mean Increase in VM in the Absence of AD | Mean Increase in VM in the Absence of EA | ||
|---|---|---|---|---|
| Mean Est. (%) | Min–Max (%) | Mean Est. (%) | Min–Max (%) | |
| A(H3N2) | 24 | 20–31 | 21 | 10–30 |
| A(H1N1pdm) | 8 | 8–11 | 8 | 0–8 |
| B/Yamagata | 10 | 5–18 | 7 | 0–7 |
| B/Victoria | 10 | 5–19 | 7 | 0–7 |
| All strains | 19 | 12–26 | 18 | 10–21 |
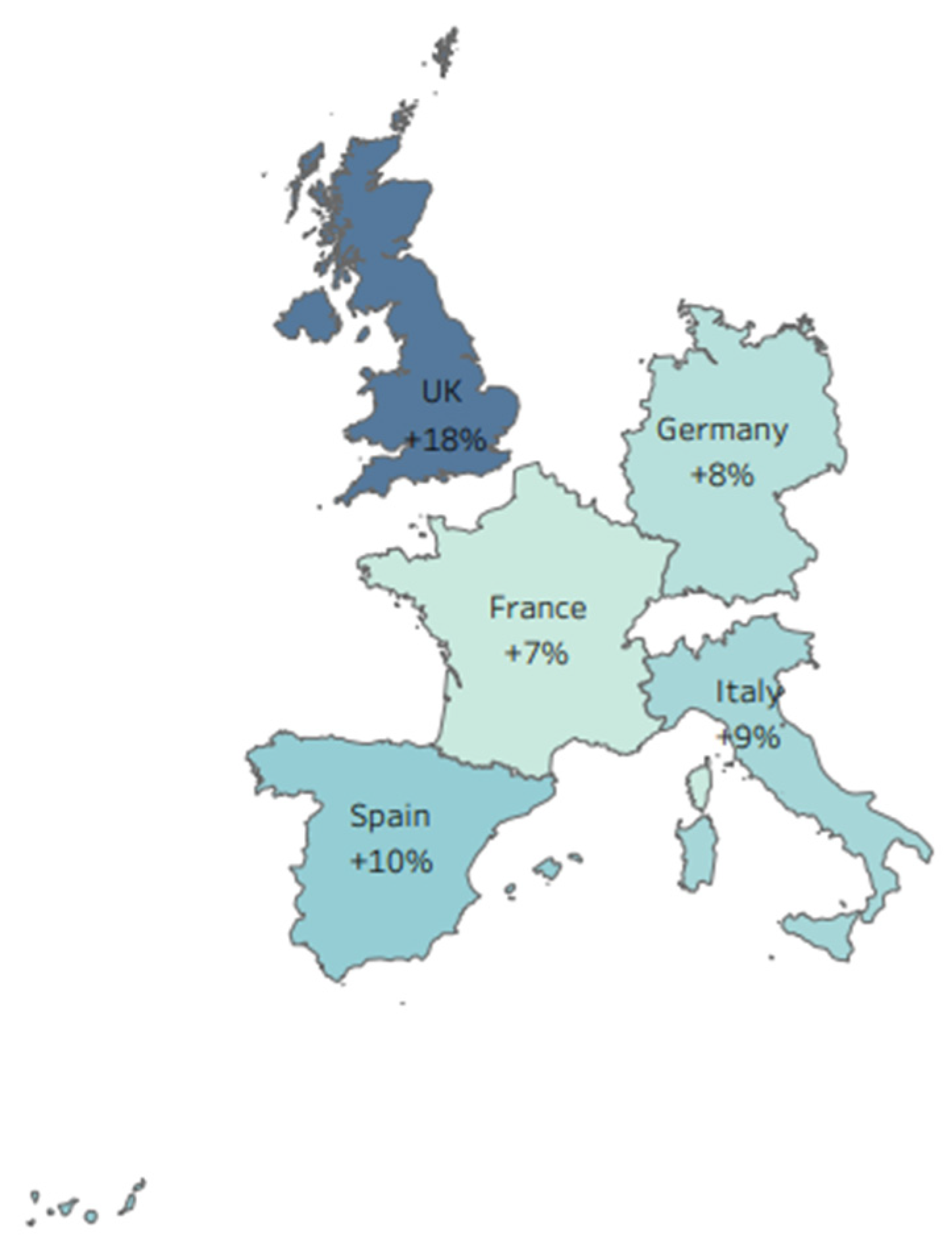
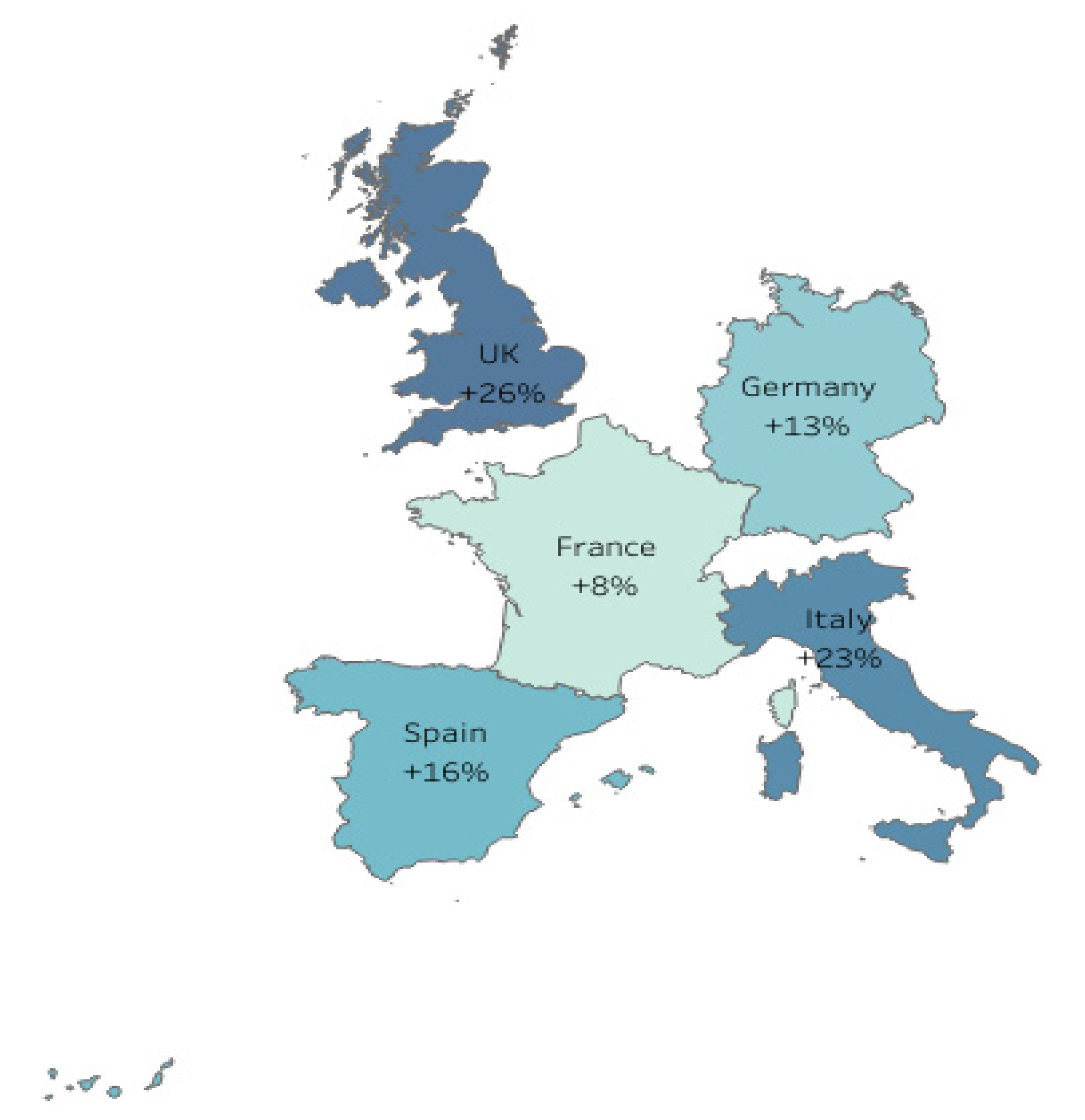
| Country | Mean Increase in VM in the Absence of AD (%) | Mean Increase in VM in the Absence of EA (%) |
|---|---|---|
| UK | 19 | 25 |
| ITA | 30 | 34 |
| FR | 15 | 12 |
| ESP | 20 | 29 |
| DE | 24 | 9 |
| Influenza (Sub)Type | Age Group | EU5 Level Mean Increase w/o AD | EU5 Country Avg. Mean Increase w/o AD | EU5 Level Mean Increase in w/o EA | EU5 Country Avg. Mean Increase w/o EA | ||||
|---|---|---|---|---|---|---|---|---|---|
| Mean Est. (%) | Min–Max (%) | Mean Est. (%) | Min–Max (%) | Mean Est. (%) | Min–Max (%) | Mean Est. (%) | Min–Max (%) | ||
| a | b | c | d | e | f | g | h | ||
| A(H3N2) | <18 year | 20 | 6–22 | 21 | 6–30 | 15 | 5–25 | 18 | 5–30 |
| 18–64 year | 15 | 5–20 | 15 | 5–20 | 16 | 5–22 | 18 | 5–30 | |
| ≥65 year | 17 | 2–40 | 14 | 2–20 | 12 | 5–20 | 13 | 5–23 | |
| A(H1N1pdm) | <18 year | 9 | 7–9 | 9 | 5–12 | 7 | 4–8 | 7 | 3–15 |
| 18–64 year | 8 | 4–9 | 7 | 3–10 | 7 | 4–8 | 7 | 3–13 | |
| ≥65 year | 5 | 1–7 | 6 | 1–9 | 5 | 2–5 | 5 | 2–10 | |
| B/Yamagata | <18 year | 8 | 6–8 | 9 | 5–19 | 6 | 2–6 | 7 | 2–15 |
| 18–64 year | 6 | 1–6 | 7 | 1–10 | 5 | 2–5 | 5 | 2–8 | |
| ≥65 year | 6 | 1–7 | 6 | 1–10 | 4 | 1–5 | 4 | 1–5 | |
| B/Victoria | <18 year | 8 | 6–8 | 9 | 5–19 | 6 | 2–6 | 7 | 2–15 |
| 18–64 year | 6 | 1–6 | 7 | 1–10 | 5 | 2–5 | 5 | 2–8 | |
| ≥65 year | 6 | 1–7 | 6 | 1–10 | 4 | 1–5 | 4 | 1–5 | |
| All strains | <18 year | 10 | 5–13 | 10 | 5–17 | 8 | 5–12 | 10 | 5–15 |
| 18–64 year | 10 | 5–10 | 10 | 5–15 | 10 | 5–14 | 12 | 5–23 | |
| ≥65 year | 9 | 5–10 | 9 | 5–13 | 6 | 2–7 | 7 | 2–13 | |
| Country | Age Group | Mean Increase in VE in the Absence of AD (%) | Mean Increase in VE in the Absence of EA (%) |
|---|---|---|---|
| UK | <18 year | +30 | +30 |
| 18–64 year | +10 | +30 | |
| ≥65 year | +10 | +10 | |
| ITA | <18 year | +23 | +26 |
| 18–64 year | +18 | +23 | |
| ≥65 year | +18 | +21 | |
| FR | <18 year | +20 | +8 |
| 18–64 year | +20 | +8 | |
| ≥65 year | +15 | +8 | |
| ESP | <18 year | +15 | +14 |
| 18–64 year | +13 | +17 | |
| ≥65 year | +10 | +14 | |
| DE | <18 year | +15 | +13 |
| 18–64 year | +15 | +13 | |
| ≥65 year | +15 | +13 | |
| EU5 | <18 year | +20 | +15 |
| 18–64 year | +15 | +16 | |
| ≥65 year | +17 | +12 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ortiz de Lejarazu-Leonardo, R.; Montomoli, E.; Wojcik, R.; Christopher, S.; Mosnier, A.; Pariani, E.; Trilla Garcia, A.; Fickenscher, H.; Gärtner, B.C.; Jandhyala, R.; et al. Estimation of Reduction in Influenza Vaccine Effectiveness Due to Egg-Adaptation Changes—Systematic Literature Review and Expert Consensus. Vaccines 2021, 9, 1255. https://doi.org/10.3390/vaccines9111255
Ortiz de Lejarazu-Leonardo R, Montomoli E, Wojcik R, Christopher S, Mosnier A, Pariani E, Trilla Garcia A, Fickenscher H, Gärtner BC, Jandhyala R, et al. Estimation of Reduction in Influenza Vaccine Effectiveness Due to Egg-Adaptation Changes—Systematic Literature Review and Expert Consensus. Vaccines. 2021; 9(11):1255. https://doi.org/10.3390/vaccines9111255
Chicago/Turabian StyleOrtiz de Lejarazu-Leonardo, Raul, Emanuele Montomoli, Radek Wojcik, Solomon Christopher, Anne Mosnier, Elena Pariani, Antoni Trilla Garcia, Helmut Fickenscher, Barbara C. Gärtner, Ravi Jandhyala, and et al. 2021. "Estimation of Reduction in Influenza Vaccine Effectiveness Due to Egg-Adaptation Changes—Systematic Literature Review and Expert Consensus" Vaccines 9, no. 11: 1255. https://doi.org/10.3390/vaccines9111255
APA StyleOrtiz de Lejarazu-Leonardo, R., Montomoli, E., Wojcik, R., Christopher, S., Mosnier, A., Pariani, E., Trilla Garcia, A., Fickenscher, H., Gärtner, B. C., Jandhyala, R., Zambon, M., & Moore, C. (2021). Estimation of Reduction in Influenza Vaccine Effectiveness Due to Egg-Adaptation Changes—Systematic Literature Review and Expert Consensus. Vaccines, 9(11), 1255. https://doi.org/10.3390/vaccines9111255







