Nocebo-Prone Behavior Associated with SARS-CoV-2 Vaccine Hesitancy in Healthcare Workers
Abstract
:1. Introduction
- Evidence before this study
- The nocebo effect refers to unfavorable health changes after medical treatment that are attributable to patients’ negative expectations and not the treatment itself, and it has been associated with increased reporting of vaccine-related adverse effects. Despite the crucial significance of SARS-Cov2 vaccination in the global battle against the COVID-19 pandemic, there is a non-negligible proportion of healthcare workers (HCWs) that experience exaggerated fears of SARS-CoV-2 vaccine-related AEs and hesitancy, which could be linked to nocebo-related mechanisms.
- Added value of this study
- This study evaluated the rates of predisposition to nocebo effects among HCWs, along with attitudes toward vaccination and reported AEs. The main findings are that nocebo-prone behavior is associated with reluctance towards SARS-CoV-2 vaccination but not with post-vaccination AE reporting.
- Implications of all available evidence
- SARS-Cov-2 vaccine hesitancy and nocebo-prone behavior may share common underlying mechanisms, therefore, communication strategies targeting the nocebo are worthy of investigation as a potential mitigation.
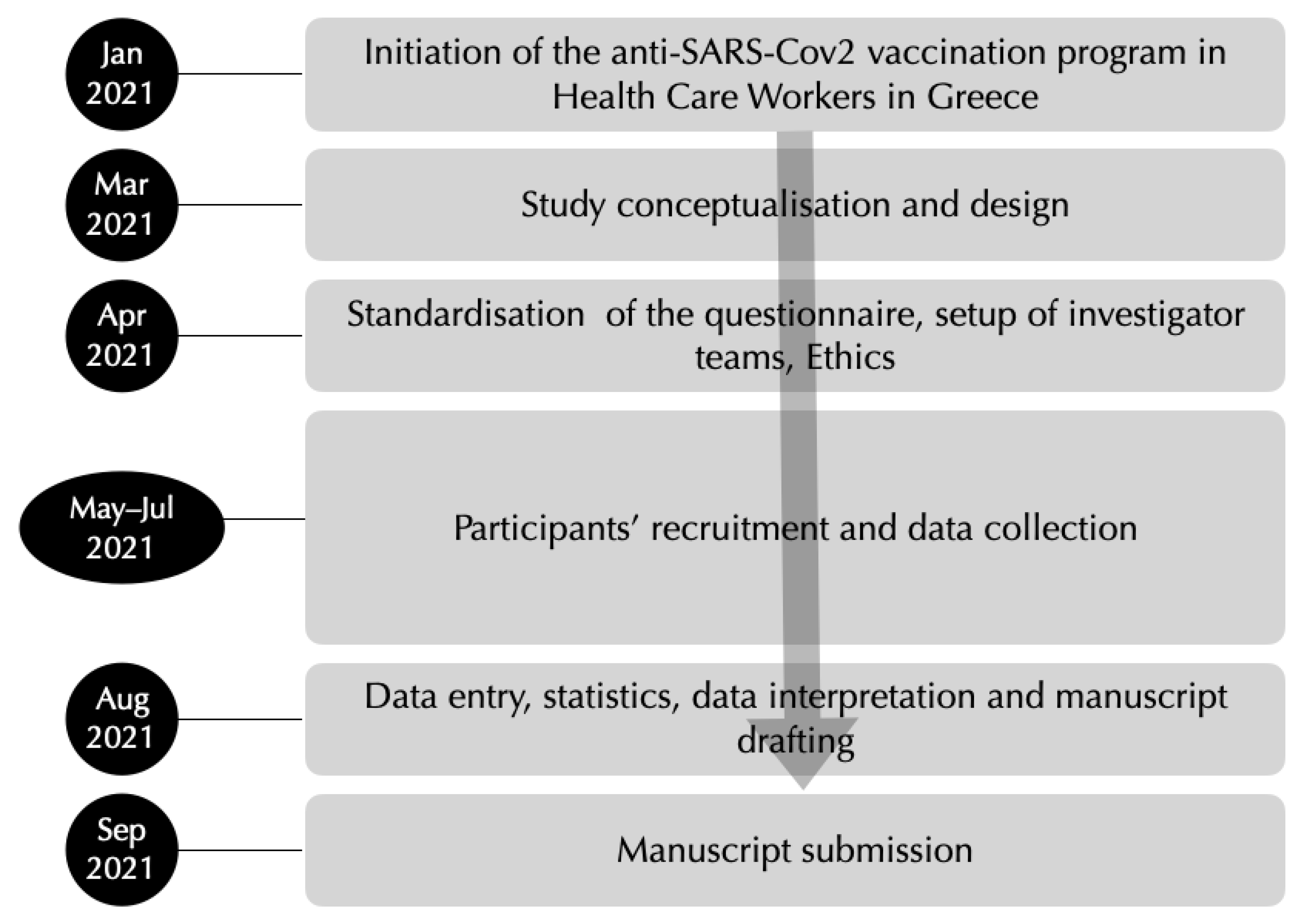
2. Methods
2.1. Study Design, Participants, and Instruments Used
2.2. Statistics
3. Findings
3.1. Vaccination Status and Hesitancy
3.2. Nocebo-Prone Behavior and Vaccine Hesitancy
3.3. Adverse Events Reported after Vaccination
4. Discussion
4.1. Hesitancy to Anti-SAR-CoV-2 Vaccines and Nocebo-Prone Behavior among HCWs
4.2. Adverse Events in Anti-SAR-CoV-2 Vaccines and Nocebo Effect among HCWs
4.3. Study Strengths and Limitations
4.4. Conclusions
4.5. Interpretation
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Solís Arce, J.S.; Warren, S.S.; Meriggi, N.F.; Scacco, A.; McMurry, N.; Voors, M.; Syunyaev, G.; Malik, A.A.; Aboutajdine, S.; Adeojo, O.; et al. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat. Med. 2021. Epub ahead of print. [Google Scholar] [CrossRef]
- Holzmann-Littig, C.; Braunisch, M.C.; Kranke, P.; Popp, M.; Seeber, C.; Fichtner, F.; Littig, B.; Carbajo-Lozoya, J.; Allwang, C.; Frank, T.; et al. COVID-19 Vaccination Acceptance and Hesitancy among Healthcare Workers in Germany. Vaccines 2021, 9, 777. [Google Scholar] [CrossRef]
- Woolf, K.; McManus, I.C.; Martin, C.A.; Nellums, L.B.; Guyatt, A.L.; Melbourne, C.; Bryant, L.; Gogoi, M.; Wobi, F.; Al-Oraibi, A.; et al. Ethnic differences in SARS-CoV-2 vaccine hesitancy in United Kingdom healthcare workers: Results from the UK-REACH prospective nationwide cohort study. Lancet Reg. Health Eur. 2021, 100180, Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Paris, C.; Bénézit, F.; Geslin, M.; Polard, E.; Baldeyrou, M.; Turmel, V.; Tadié, É.; Garlantezec, R.; Tattevin, P. COVID-19 vaccine hesitancy among healthcare workers. Infect. Dis Now. 2021, 51, 484–487. [Google Scholar] [CrossRef] [PubMed]
- Scales, D.; Gorman, J.; Jamieson, K.H. The Covid-19 Infodemic—Applying the Epidemiologic Model to Counter Misinformation. N. Engl. J. Med. 2021, 385, 678–681. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, N.E.; SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- Larson, H.J.; Jarrett, C.; Schulz, W.S.; Chaudhuri, M.; Zhou, Y.; Dube, E.; Schuster, M.; MacDonald, N.E.; Wilson, R.; SAGE Working Group on Vaccine Hesitancy. Measuring vaccine hesitancy: The development of a survey tool. Vaccine 2015, 33, 4165–4175. [Google Scholar] [CrossRef] [Green Version]
- Jarrett, C.; Wilson, R.; O’Leary, M.; Eckersberger, E.; Larson, H.J.; SAGE Working Group on Vaccine Hesitancy. Strategies for addressing vaccine hesitancy—A systematic review. Vaccine 2015, 33, 4180–4190. [Google Scholar] [CrossRef] [Green Version]
- Paterson, P.; Meurice, F.; Stanberry, L.R.; Glismann, S.; Rosenthal, S.L.; Larson, H.J. Vaccine hesitancy and healthcare providers. Vaccine 2016, 34, 6700–6706. [Google Scholar] [CrossRef] [Green Version]
- Karafillakis, E.; Dinca, I.; Apfel, F.; Cecconi, S.; Wűrz, A.; Takacs, J.; Suk, J.; Celentano, L.P.; Kramarz, P.; Larson, H.J. Vaccine hesitancy among healthcare workers in Europe: A qualitative study. Vaccine 2016, 34, 5013–5020. [Google Scholar] [CrossRef]
- Mitsikostas, D.D.; Blease, C.; Carlino, E.; Colloca, L.; Geers, A.L.; Howick, J.; Evers, A.W.M.; Flaten, M.A.; Kelley, J.M.; Kirsch, I.; et al. European Headache Federation recommendations for placebo and nocebo terminology. J. Headache Pain 2020, 21, 117. [Google Scholar] [CrossRef]
- Colloca, L.; Barsky, A.J. Placebo and Nocebo Effects. N. Engl. J. Med. 2020, 382, 554–561. [Google Scholar] [CrossRef]
- Amanzio, M.; Vase, L.; Mitsikostas, D.D. Editorial: Nocebo Effects and Their Influence on Clinical Trials and Practice: Modulating Factors in Healthy and Pathological Conditions. Front. Pharmacol. 2020, 11, 100. [Google Scholar] [CrossRef] [Green Version]
- Zis, P.; Mitsikostas, D.D. Nocebo Responses in Brain Diseases: A Systematic Review of the Current Literature. Int. Rev. Neurobiol. 2018, 139, 443–462. [Google Scholar] [CrossRef]
- Kravvariti, E.; Kitas, G.D.; Mitsikostas, D.D.; Sfikakis, P.P. Nocebos in rheumatology: Emerging concepts and their implications for clinical practice. Nat. Rev. Rheumatol. 2018, 14, 727–740. [Google Scholar] [CrossRef]
- Kravvariti, E.; Kitas, G.D.; Sfikakis, P.P. The role of the Nocebo effect in the use of biosimilars in routine rheumatology clinical practice. Mediterr. J. Rheumatol. 2019, 30 (Suppl. 1), 63–68. [Google Scholar] [CrossRef] [PubMed]
- Okaïs, C.; Gay, C.; Seon, F.; Buchaille, L.; Chary, E.; Soubeyrand, B. Disease-specific adverse events following nonlive vaccines: A paradoxical placebo effect or a nocebo phenomenon? Vaccine 2011, 29, 6321–6326. [Google Scholar] [CrossRef] [PubMed]
- Amanzio, M.; Cipriani, G.E.; Bartoli, M. How do nocebo effects in placebo groups of randomized controlled trials provide a possible explicative framework for the COVID-19 pandemic? Expert Rev. Clin. Pharmacol. 2021, 14, 439–444. [Google Scholar] [CrossRef]
- Mitsikostas, D.D.; Deligianni, C.I. Q-No: A questionnaire to predict nocebo in outpatients seeking neurological consultation. Neurol. Sci. 2015, 36, 379–381. [Google Scholar] [CrossRef] [PubMed]
- Mitsikostas, D.D.; Belesioti, I.; Arvaniti, C.; Mitropoulou, E.; Deligianni, C.; Kasioti, E.; Constantinidis, T.; Dermitzakis, M.; Vikelis, M.; Hellenic Headache Society. Patients’ preferences for headache acute and preventive treatment. J. Headache Pain. 2017, 18, 102. [Google Scholar] [CrossRef] [Green Version]
- Fragoulis, G.E.; Evangelatos, G.; Arida, A.; Bournia, V.K.; Fragiadaki, K.; Karamanakos, A.; Kravvariti, E.; Laskari, K.; Panopoulos, S.; Pappa, M.; et al. Nocebo-Prone Behaviour in Patients with Autoimmune Rheumatic Diseases during the COVID-19 Pandemic. Mediterr. J. Rheumatol. 2020, 31 (Suppl. 2), 288–294. [Google Scholar] [CrossRef] [PubMed]
- Yiangou, A.; Mitchell, J.L.; Fisher, C.; Edwards, J.; Vijay, V.; Alimajstorovic, Z.; Grech, O.; Lavery, G.G.; Mollan, S.P.; Sinclair, A.J. Erenumab for headaches in idiopathic intracranial hypertension: A prospective open-label evaluation. Headache 2021, 61, 157–169. [Google Scholar] [CrossRef] [PubMed]
- Papagiannis, D.; Rachiotis, G.; Malli, F.; Papathanasiou, I.V.; Kotsiou, O.; Fradelos, E.C.; Giannakopoulos, K.; Gourgoulianis, K.I. Acceptability of COVID-19 Vaccination among Greek Health Professionals. Vaccines 2021, 9, 200. [Google Scholar] [CrossRef]
- Gagneux-Brunon, A.; Detoc, M.; Bruel, S.; Tardy, B.; Rozaire, O.; Frappe, P.; Botelho-Nevers, E. Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: A cross-sectional survey. J. Hosp. Infect. 2021, 108, 168–173. [Google Scholar] [CrossRef]
- Riad, A.; Pokorná, A.; Attia, S.; Klugarová, J.; Koščík, M.; Klugar, M. Prevalence of COVID-19 Vaccine Side Effects among Healthcare Workers in the Czech Republic. J. Clin. Med. 2021, 10, 1428. [Google Scholar] [CrossRef]
- Klosterhalfen, S.; Kellermann, S.; Braun, S.; Kowalski, A.; Schrauth, M.; Zipfel, S.; Enck, P. Gender and the nocebo response following conditioning and expectancy. J. Psychosom. Res. 2009, 66, 323–328. [Google Scholar] [CrossRef] [PubMed]
- Vambheim, S.M.; Flaten, M.A. A systematic review of sex differences in the placebo and the nocebo effect. J. Pain Res. 2017, 10, 1831–1839. [Google Scholar] [CrossRef] [Green Version]
- Swider, K.; Bąbel, P. The effect of the sex of a model on nocebo hyperalgesia induced by social observational learning. Pain 2013, 154, 1312–1317. [Google Scholar] [CrossRef] [PubMed]
- Balant, L.P.; Balant-Gorgia, E.A. Cultural differences: Implications on drug therapy and global drug development. Int. J. Clin. Pharmacol. Ther. 2000, 38, 47–52. [Google Scholar] [CrossRef]
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Pérez Marc, G.; Moreira, E.D.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef]
- Roberto, G.; Zanoni, G. Disease-related adverse events following non-live vaccines: Investigation of a newly described reporting bias through the analysis of the WHO Global ICSR Database, VigiBase. Vaccine 2014, 32, 3328–3335. [Google Scholar] [CrossRef]
- Faasse, K.; Porsius, J.T.; Faasse, J.; Martin, L.R. Bad news: The influence of news coverage and Google searches on Gardasil adverse event reporting. Vaccine 2017, 35 Pt B, 6872–6878. [Google Scholar] [CrossRef]
- Gao, J.; Zheng, P.; Jia, Y.; Chen, H.; Mao, Y.; Chen, S.; Wang, Y.; Fu, H.; Dai, J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE 2020, 15, e0231924. [Google Scholar]
- Daniali, H.; Flaten, M.A. Experiencing COVID-19 symptoms without the disease: The role of nocebo in reporting of symptoms. Scand. J. Public Health 2021, 14034948211018385. [Google Scholar] [CrossRef]
- Benedetti, F.; Piedimonte, A. The neurobiological underpinnings of placebo and nocebo effects. Semin. Arthritis Rheum. 2019, 49, S18–S21. [Google Scholar] [CrossRef] [PubMed]
- Kong, J.; Gollub, R.L.; Polich, G.; Kirsch, I.; Laviolette, P.; Vangel, M.; Rosen, B.; Kaptchuk, T.J. A functional magnetic resonance imaging study on the neural mechanisms of hyperalgesic nocebo effect. J. Neurosci. 2008, 28, 13354–13362. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Question | Rating (1 = Never, 5 = Always) |
|---|---|
| I read the summary of product characteristics (SPC) before taking a medication | |
| I have discontinued a medication because of adverse effects in the past | |
| I ask my physician for potential adverse effects of the medication he/she gives me | |
| I take into account the adverse effects reported in the summary of product characteristics (SPC) seriously | |
| total | (4–20) |
| All | Female | Male | Phys. | Nurses | Admin. | Other | Q-No ≥ 15 | Q-No < 15 | |
|---|---|---|---|---|---|---|---|---|---|
| N | 1309 | 866 | 421 | 557 | 364 | 148 | 213 | 325 | 984 |
| % | 100 | 67.2 | 32.6 | 43.4 | 28.4 | 11.5 | 16.6 | 24.8 | 75.2 |
| Mean age | 41.6 | 41.3 | 41.6 | 37.9 | 42.3 | 47.1 | 56.5 | 43.6 | 40.9 |
| SD | 10.9 | 10.9 | 11.0 | 10.4 | 10.5 | 9.3 | 10.7 | 11.4 | 10.7 |
| Vaccinees * | 1072 | 670 | 382 | 524 | 270 | 114 | 138 | 220 | 852 |
| % | 81.9 | 77.4 | 90.7 | 94.1 | 74.2 | 77.0 | 64.8 | 67.7 | 86.6 |
| 95% CI | 79.7–83.9 | 74.5–80.0 | 87.6–93.2 | 91.8–95.8 | 69.4–78.4 | 69.5–83.1 | 58.1–70.9 | 62.4–72.6 | 84.3–88.6 |
| Hesitant | 237 | 196 | 39 | 33 | 94 | 34 | 75 | 105 | 132 |
| % | 18.1 | 22.6 | 9.3 | 5.9 | 25.8 | 23.0 | 25.2 | 32.3 | 13.4 |
| 95% CI | 16.1–20.3 | 20.0–25.5 | 6.83–12.4 | 4.2–8.2 | 21.6–30.6 | 16.9–30.4 | 29.0–41.9 | 27.4–37.6 | 11.4–15.7 |
| Vaccinees * with any AE | 709 | 477 | 223 | 364 | 177 | 74 | 82 | 143 | 566 |
| % | 67.5 | 72.8 | 59.3 | 70.1 | 67.6 | 66.7 | 61.2 | 66.8 | 67.6 |
| 95% CI | 64.6–70.2 | 69.3–76.1 | 54.3–64.2 | 66.0–73.9 | 61.6–73.0 | 57.4–74.9 | 52.7–69.1 | 60.2–72.8 | 64.4–70.7 |
| Q-No ≥ 15 | 325 | 237 | 83 | 87 | 122 | 40 | 72 | - | - |
| % | 24.8 | 27.4 | 19.7 | 15.6 | 33.5 | 27.0 | 33.8 | - | - |
| 95% CI | 22.6–27.2 | 24.5–30.4 | 16.8–23.8 | 12.8–18.9 | 28.9–38.5 | 20.5–34.8 | 27.7–40.4 | - | - |
| Q-No < 15 | 984 | 629 | 338 | 470 | 242 | 108 | 141 | - | - |
| % | 75.2 | 72.6 | 80.3 | 84.4 | 66.5 | 72.9 | 66.2 | - | - |
| 95% CI | 72.8–77.4 | 69.6–75.5 | 76.2–83.8 | 81.1–87.2 | 61.5–71.2 | 65.2–79.5 | 59.6–72.3 | - | - |
| Vaccination | OR. | St.Err. | p-Value | [95% Conf | Interval] |
|---|---|---|---|---|---|
| Q-No score ≥ 15 | 0.425 | 0.073 | <0.001 | 0.303 | 0.596 |
| Age | 1.013 | 0.008 | 0.091 | 0.998 | 1.029 |
| Physicians | 4.727 | 1.046 | <0.001 | 3.064 | 7.293 |
| Females | 0.580 | 0.127 | 0.013 | 0.378 | 0.890 |
| Constant | 5.799 | 1.277 | <0.001 | 3.766 | 8.929 |
| N | % | 95% CI | |
|---|---|---|---|
| Vaccinees with any AE after 1st dose | |||
| Severe AEs | 4 | 0.4 | 0.1–1.0 |
| Moderate AEs | 56 | 5.3 | 4.1–6.8 |
| Mild AEs | 470 | 44.5 | 41.5–47.5 |
| No AEs | 527 | 49.9 | 46.8–52.9 |
| Total | 1057 | 100.00 | |
| Missing data | 15 | ||
| Vaccinees with any AE after 2nd dose | |||
| Severe AEs | 6 | 0.6 | 0.27–1.31 |
| Moderate AEs | 127 | 12.5 | 10.6–14.7 |
| Mild AEs | 437 | 43.1 | 40.1–46.2 |
| No AEs | 444 | 43.8 | 40.8–46.9 |
| Total | 1014 | 100.0 | |
| Missing data | 21 | ||
| Grand Total | 1035 * | ||
| Adverse Events (AE) after 1st Dose | Overall N = 1057 | Q-No Score ≥ 15 N = 217 | Q-No Score < 15 N = 840 | p-Value | |||
|---|---|---|---|---|---|---|---|
| n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | ||
| At least on AE | 530 | 50.1 47.1–53.2 | 106 | 48.8 42.2–55.5 | 424 | 50.5 47.1–53.8 | 0.669 |
| Hypertension | 11 | 1.04 0.6–1.9 | 1 | 0.4 0.7–3.2 | 10 | 1.2 0.6–2.2 | 0.569 |
| Hypotension | 5 | 0.5 0.2–1.1 | 1 | 0.4 0.01–3.2 | 4 | 0.5 0.2–1.3 | >0.999 |
| Tachycardia | 25 | 2.4 1.6–3.5 | 4 | 1.8 0.7–4.8 | 21 | 2.5 1.6–3.8 | 0.751 |
| Rash | 13 | 1.2 0.7–2.1 | 4 | 1.84 0.7–4.8 | 9 | 1.1 0.6–2.0 | 0.566 |
| Dyspnea | 10 | 0.9 0.5–1.7 | 2 | 0.9 0.2–3.6 | 8 | 0.9 0.5–1.9 | >0.999 |
| Dizziness | 53 | 5.0 3.8–6.5 | 9 | 4.1 2.1–7.8 | 44 | 5.2 3.9–7.0 | 0.630 |
| Local pain | 293 | 27.7 25.1–30.5 | 58 | 26.7 21.2–33.0 | 235 | 28.0 25.0–31.1 | 0.779 |
| Headache | 106 | 10.0 8.3–12.0 | 24 | 11.1 7.5–16.0 | 82 | 9.7 7.9–12.0 | 0.659 |
| Fever | 45 | 4.3 3.2–5.7 | 6 | 2.8 1.2–6.1 | 39 | 4.64 3.40–6.3 | 0.302 |
| Fatigue | 71 | 6.7 5.35–8.40 | 12 | 5.5 3.2–9.5 | 59 | 7.02 5.5–9.0 | 0.528 |
| Myalgia | 113 | 10.7 9.0–12.7 | 23 | 10.6 7.1–15.5 | 90 | 10.7 8.8–13.0 | 0.981 |
| Adverse Events (AE) after 2nd Dose | Overall N = 1014 | Q-No Score ≥ 15 N = 204 | Q-No Score < 15 N = 810 | p-Value | |||
|---|---|---|---|---|---|---|---|
| n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | ||
| At least on AE | 570 | 56.2 53.1–59.2 | 112 | 54.9 48.0–6.6 | 458 | 56.5 53.1–59.9 | 0.673 |
| Hypertension | 6 | 0.6 0.3–1.3 | 3 | 1.5 0.5–4.5 | 3 | 0.4 0.1–1.1 | 0.187 |
| Hypotension | 7 | 0.69 0.3–1.4 | 1 | 0.5 0.1–3.4 | 6 | 0.7 0.3–1.6 | >0.999 |
| Tachycardia | 21 | 2.1 1.3–3.1 | 5 | 2.4 1.0–5.8 | 16 | 2.0 1.2–3.2 | 0.880 |
| Rash | 11 | 1.1 0.6–1.9 | 3 | 1.47 0.5–4.5 | 8 | 0.99 0.5–1.9 | 0.552 |
| Dyspnea | 10 | 1.0 0.5–1.8 | 2 | 1.0 0.2–3.8 | 8 | 1.0 0.5–1.9 | >0.999 |
| Dizziness | 58 | 5.7 4.4–7.3 | 15 | 7.3 4.5–11.8 | 43 | 5.3 3.9–7.1 | 0.340 |
| Local pain | 234 | 23.1 20.6–25.8 | 47 | 23.0 17.5–29.3 | 187 | 23.1 20.3–26.1 | >0.999 |
| Headache | 164 | 16.2 14.0–18.6 | 40 | 19.6 14.7–25.6 | 124 | 15.3 13.0–18.7 | 0.166 |
| Fever | 135 | 13.3 11.3–15.5 | 31 | 15.2 10.9–20.8 | 104 | 12.8 10.7–15.3 | 0.441 |
| Fatigue | 106 | 10.4 8.7–12.5 | 16 | 7.8 4.8–12.4 | 90 | 11.1 9.1–13.5 | 0.217 |
| Myalgia | 138 | 13.6 11.6–15.8 | 27 | 13.2 9.2–18.6 | 111 | 13.7 11.5–16.2 | 0.952 |
| Adverse Event | OR | St.Err. | p-Value | [95% Conf. | Interval] |
|---|---|---|---|---|---|
| Q-No score ≥ 15 | 0.901 | 0.159 | 0.555 | 0.638 | 1.273 |
| Age | 0.990 | 0.007 | 0.181 | 0.977 | 1.004 |
| Physician | 1.474 | 0.239 | 0.017 | 1.073 | 2.025 |
| Female | 2.001 | 0.312 | <0.001 | 1.482 | 2.725 |
| Constant | 1.160 | 0.193 | 0.369 | 0.838 | 1.607 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mitsikostas, D.D.; Aravantinou-Fatorou, K.; Deligianni, C.; Kravvariti, E.; Korompoki, E.; Mylona, M.; Vryttia, P.; Papagiannopoulou, G.; Delicha, E.-M.; Dellis, A.; et al. Nocebo-Prone Behavior Associated with SARS-CoV-2 Vaccine Hesitancy in Healthcare Workers. Vaccines 2021, 9, 1179. https://doi.org/10.3390/vaccines9101179
Mitsikostas DD, Aravantinou-Fatorou K, Deligianni C, Kravvariti E, Korompoki E, Mylona M, Vryttia P, Papagiannopoulou G, Delicha E-M, Dellis A, et al. Nocebo-Prone Behavior Associated with SARS-CoV-2 Vaccine Hesitancy in Healthcare Workers. Vaccines. 2021; 9(10):1179. https://doi.org/10.3390/vaccines9101179
Chicago/Turabian StyleMitsikostas, Dimos D., Konstantina Aravantinou-Fatorou, Christina Deligianni, Evrydiki Kravvariti, Eleni Korompoki, Maria Mylona, Pinelopi Vryttia, Georgia Papagiannopoulou, Eumorphia-Maria Delicha, Athanasios Dellis, and et al. 2021. "Nocebo-Prone Behavior Associated with SARS-CoV-2 Vaccine Hesitancy in Healthcare Workers" Vaccines 9, no. 10: 1179. https://doi.org/10.3390/vaccines9101179
APA StyleMitsikostas, D. D., Aravantinou-Fatorou, K., Deligianni, C., Kravvariti, E., Korompoki, E., Mylona, M., Vryttia, P., Papagiannopoulou, G., Delicha, E.-M., Dellis, A., Tsivgoulis, G., Dimopoulos, M. A., Amanzio, M., & Sfikakis, P. P. (2021). Nocebo-Prone Behavior Associated with SARS-CoV-2 Vaccine Hesitancy in Healthcare Workers. Vaccines, 9(10), 1179. https://doi.org/10.3390/vaccines9101179








