A Rapid Systematic Review of Factors Influencing COVID-19 Vaccination Uptake in Minority Ethnic Groups in the UK
Abstract
:1. Introduction
1.1. Review Aims
1.2. Review Questions
- 1.
- What are the differences between minority ethnic groups’ intentions and uptake of COVID-19 vaccination in the UK?
- 2.
- What are the barriers to COVID-19 vaccination acceptance in minority ethnic groups in the UK?
- 3.
- What are the facilitators to COVID-19 vaccination acceptance in minority ethnic groups in the UK?
- 4.
- Are there any differences in barriers and facilitators to COVID-19 vaccination acceptance between minority ethnic groups in the UK?
2. Method
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction
2.4. Risk of Bias
2.5. Procedure
3. Results
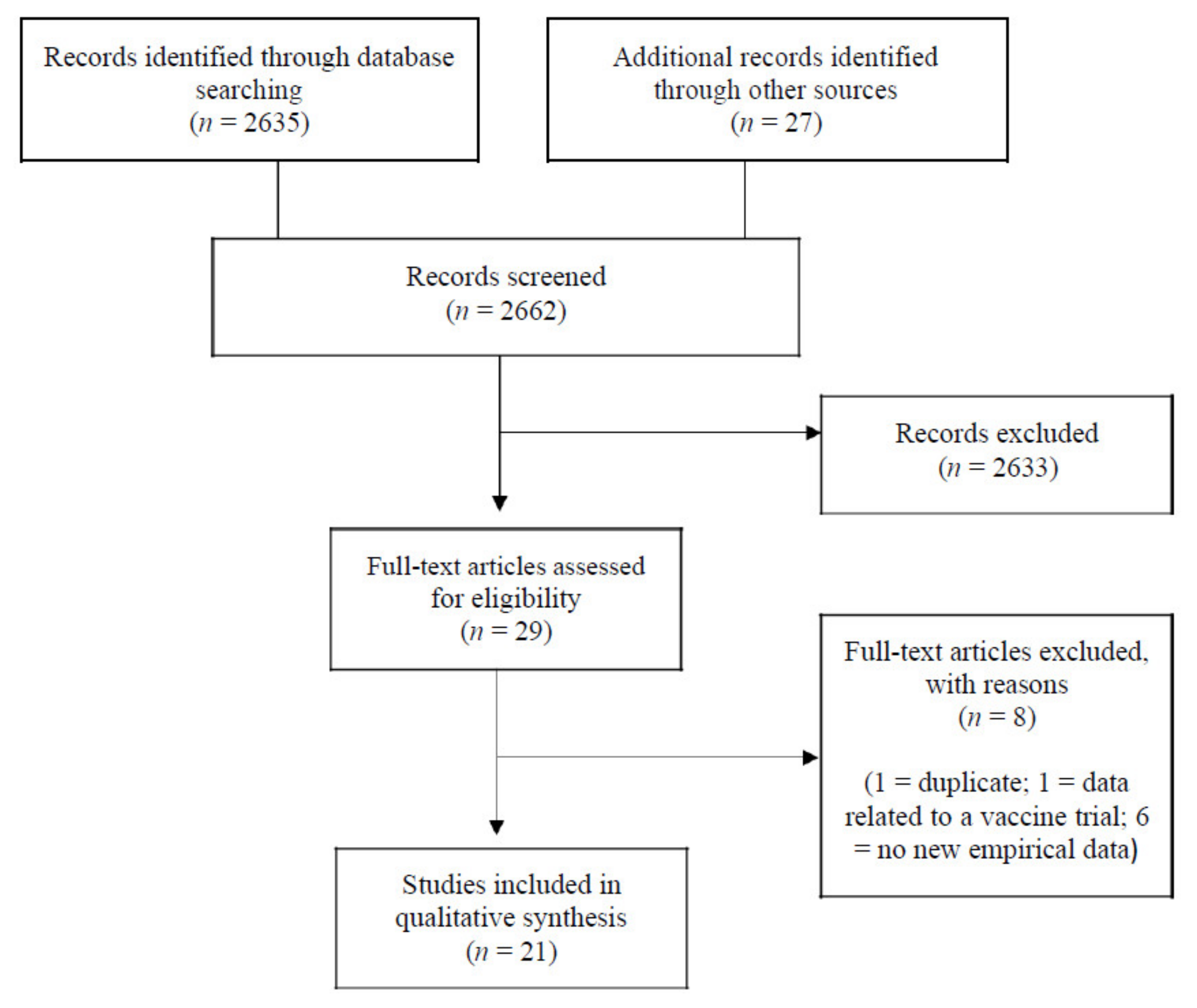
3.1. Search Results
3.2. Risk of Bias Analysis
3.3. Narrative Synthesis
3.3.1. Differences in Minority Ethnic Groups’ Intention and Uptake
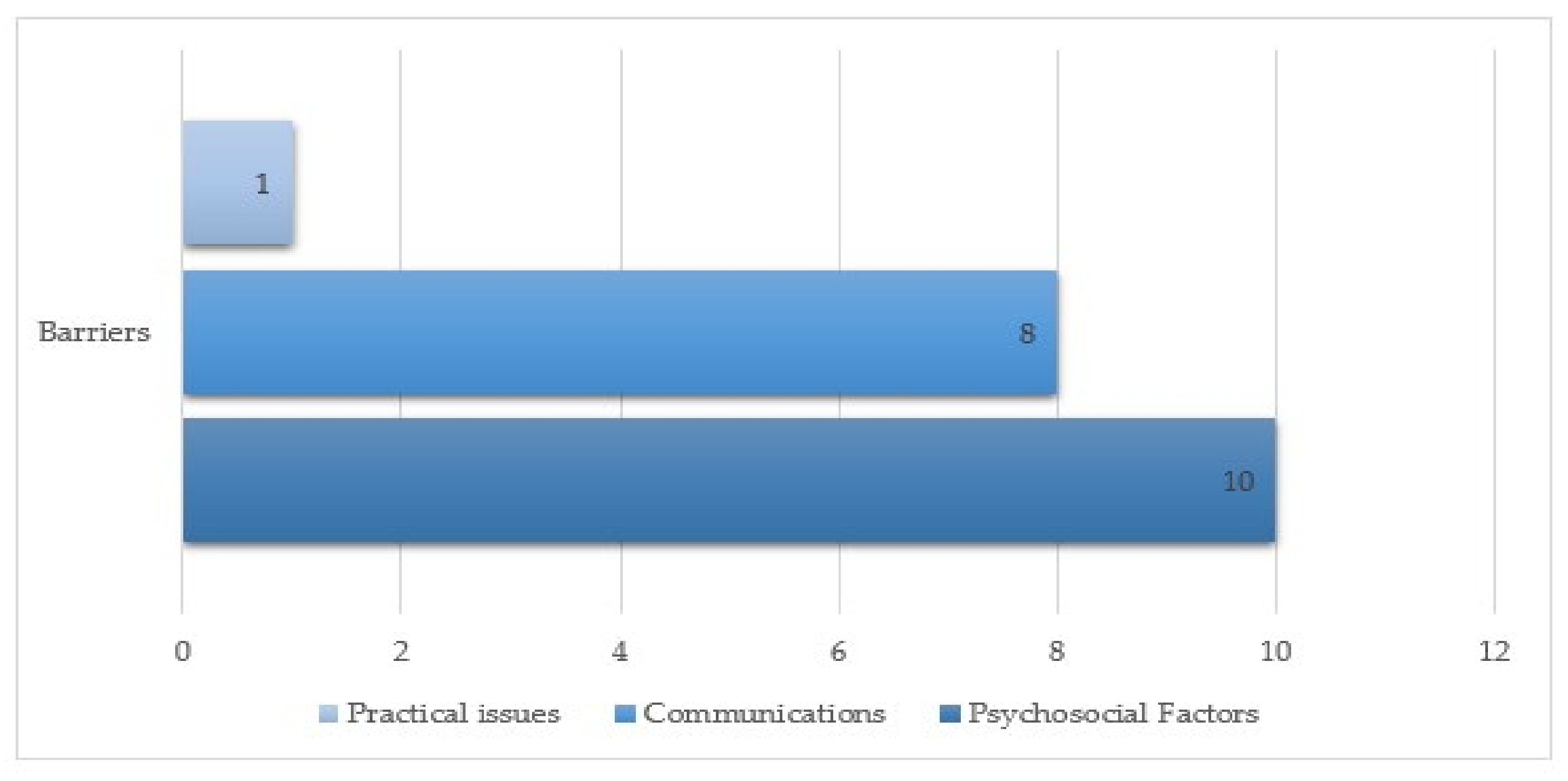
3.3.2. Barriers to COVID-19 Vaccination Acceptance in Minority Ethnic Groups
Communications: Source, Content and Access
Practical Issues: Logistics
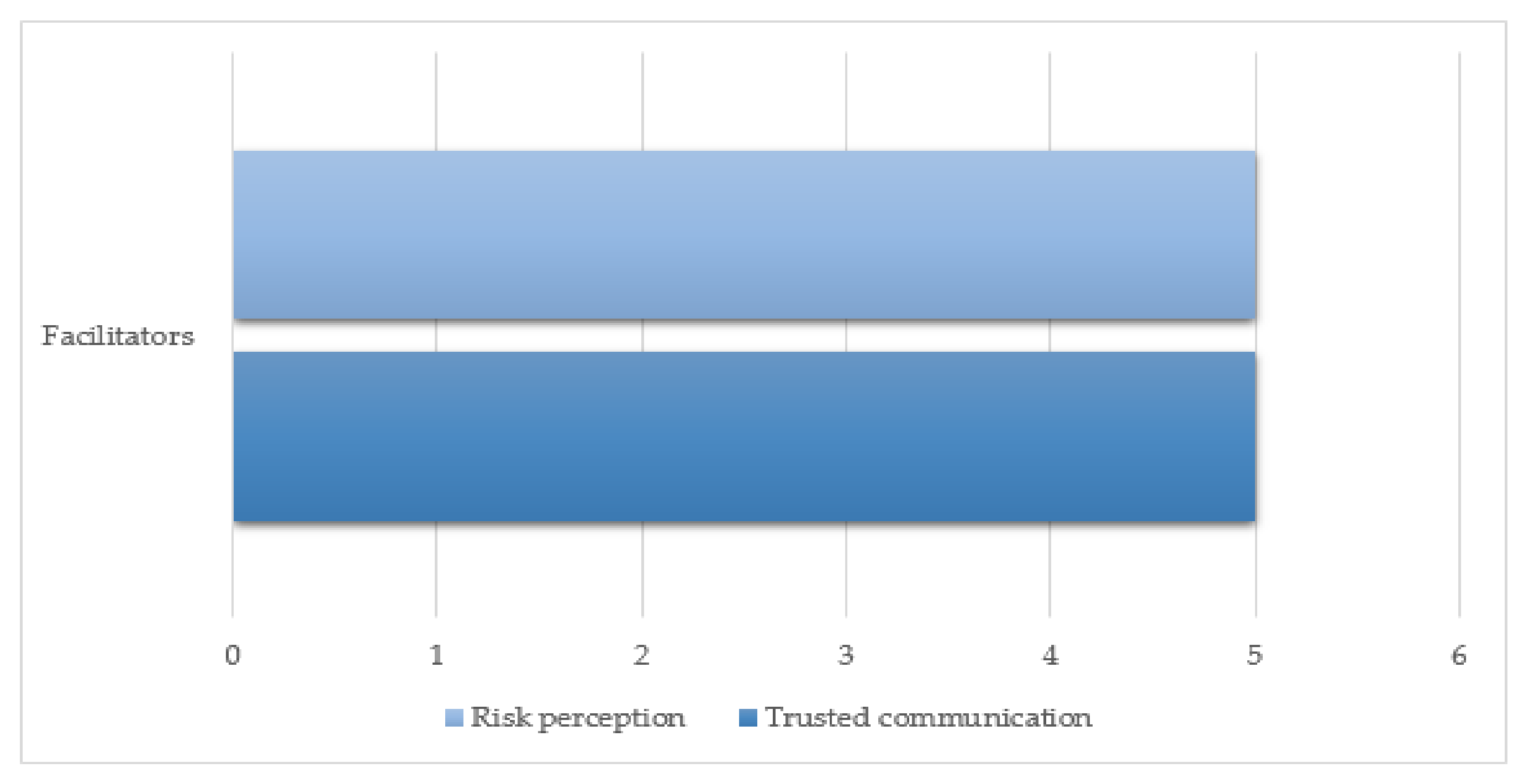
3.3.3. Facilitators to COVID-19 Vaccination Acceptance in Minority Ethnic Groups
Trusted Communication: Family, Social and Professional Influences
Risk Perception: Confidence in Risk Reduction Outcome of Vaccine
3.3.4. Differences in Barriers and Facilitators between Minority Ethnic Groups
4. Discussion
4.1. Recommendations
4.1.1. Community Engagement
4.1.2. Inclusive Communications
4.1.3. Practical Application and Service Delivery
4.1.4. Resources
4.1.5. Further Research
4.2. Strengths and Limitations of the Review
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Hanif, W.; Ali, S.N.; Patel, K.; Khunti, K. Cultural competence in covid-19 vaccine rollout. BMJ 2020, 371, m4845. [Google Scholar] [CrossRef]
- Sze, S.; Pan, D.; Nevill, C.R.; Gray, L.J.; Martin, C.A.; Nazareth, J.; Minhas, J.S.; Divall, P.; Khunti, K.; Abrams, K.R.; et al. Ethnicity and clinical outcomes in COVID-19: A systematic review and meta-analysis. EClinicalMedicine 2020, 12, 100630. [Google Scholar] [CrossRef] [PubMed]
- Office for National Statistics. Coronavirus and Vaccine Hesitancy, Great Britain: 31 March to 25 April 2021; Office for National Statistics: London, UK, May 2021. [Google Scholar]
- MacDonald, N.E. SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- SAGE Ethnicity Group. Factors Influencing COVID-19 Vaccine Uptake among Minority Ethnic Groups; 2020. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/952716/s0979-factors-influencing-vaccine-uptake-minority-ethnic-groups.pdf (accessed on 4 January 2021).
- Gov.UK. UK Population by Ethnicity; 2018. Available online: https://www.ethnicity-facts-figures.service.gov.uk/uk-population-by-ethnicity/national-and-regional-populations/population-of-england-and-wales/latest (accessed on 1 September 2021).
- Osama, T.; Razai, M.S.; Majeed, A. COVID-19 vaccine allocation: Addressing the United Kingdom’s colour-blind strategy. J. R. Soc. Med. 2021, 114, 240–243. [Google Scholar] [CrossRef] [PubMed]
- Kamal, A.; Rubin, J.; Rogers, B. Using behavioural science to develop public health messages for racial and ethnic minority communities during COVID-19. PsyArXiv 2021. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kamal, A.; Pearce, J.; Hodson, A.; A Rapid Systematic Review of Factors Influencing COVID-19 Vaccination Uptake in Minority Ethnic Groups in the UK. PROSPERO 2021 CRD42021253728. Available online: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021253728 (accessed on 20 July 2021).
- Hong, Q.N.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.P.; Griffiths, F.; Nicolau, B.; O’Cathain, A.; et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ. Inf. 2018, 34, 285–291. [Google Scholar] [CrossRef] [Green Version]
- Smith, L.E.; Hodson, A.; Rubin, G.J. Parental attitudes towards mandatory vaccination: A systematic review. Vaccine 2021, 39, 4046–4053. [Google Scholar] [CrossRef] [PubMed]
- Allington, D.; McAndrew, S.; Moxham-Hall, V.; Duffy, B. Coronavirus conspiracy suspicions, general vaccine attitudes, trust and coronavirus information source as predictors of vaccine hesitancy among UK residents during the COVID-19 pandemic. Psychol. Med. 2021, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Allington, D.; McAndrew, S.; Moxham-Hall, V.L.; Duffy, B. Media usage predicts intention to be vaccinated against SARS-CoV-2 in the US and the UK. Vaccine 2021, 39, 2595–2603. [Google Scholar] [CrossRef] [PubMed]
- Bell, S.; Clarke, R.; Mounier-Jack, S.; Walker, J.L.; Paterson, P. Parents’ and guardians’ views on the acceptability of a future COVID-19 vaccine: A multi-methods study in England. Vaccine 2020, 38, 7789–7798. [Google Scholar] [CrossRef] [PubMed]
- British Red Cross. New Research into COVID-19 Vaccine Hesitancy: Family Conversations Could Be Key to Increasing Take Up in B.A.M.E Communities, Suggests Poll; British Red Cross: London, UK, February 2021. [Google Scholar]
- Freeman, D.; Loe, B.S.; Chadwick, A.; Vaccari, C.; Waite, F.; Rosebrock, L.; Jenner, L.; Petit, A.; Lewandowsky, S.; Vanderslott, S.; et al. COVID-19 vaccine hesitancy in the UK: The Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol. Med. 2020, 1–15. [Google Scholar]
- Healthwatch. Getting to Vaccine Centres More of a Barrier for Black Communities. Healthwatch: London, UK, 2021. Available online: https://www.healthwatch.co.uk/news/2021-02-22/getting-vaccine-centres-more-barrier-black-communities (accessed on 1 September 2021).
- Healthwatch Camden. Black, Asian and Minority Ethnic Views on the COVID-19 Vaccine. 2021. Available online: https://healthwatchcamden.co.uk/resources/black-asian-and-minority-ethnic-views-covid-19-vaccine (accessed on 1 September 2021).
- Woolf, K.; McManus, I.C.; Martin, C.A.; Nellums, L.B.; Guyatt, A.L.; Melbourne, C.; Bryant, L.; Gogoi, M.; Wobi, F.; Al-Oraibi, A.; et al. Ethnic differences in SARS-CoV-2 vaccine hesitancy in United Kingdom healthcare workers: Results from the UK-REACH prospective nationwide cohort study. Lancet Reg. Health Eur. 2021, 100180, In press. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, L.H.; Joshi, A.D.; Drew, D.A.; Merino, J.; Ma, W.; Lo, C.H.; Kwon, S.; Wang, K.; Graham, M.S.; Polidori, L.; et al. Racial and ethnic differences in COVID-19 vaccine hesitancy and uptake. medRxiv 2021. [Google Scholar] [CrossRef]
- Robertson, E.; Reeve, K.S.; Niedzwiedz, C.L.; Moore, J.; Blake, M.; Green, M.; Katikireddi, S.V.; Benzeval, M.J. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain Behav. Immun. 2021, 94, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Royal Society for Public Health. New Poll Finds Ethnic Minority Groups Less likely to Want COVID Vaccine; Royal Society for Public Health: London, UK, December 2020. [Google Scholar]
- Williams, L.; Flowers, P.; McLeod, J.; Young, D.; Rollins, L. The Catalyst Project Team. Social Patterning and Stability of Intention to Accept a COVID-19 Vaccine in Scotland: Will Those Most at Risk Accept a Vaccine? Vaccines 2021, 9, 17. [Google Scholar] [CrossRef] [PubMed]
- You Gov. Who Do BAME Britons Trust When It Comes to COVID-19? 2021. Available online: https://yougov.co.uk/topics/politics/articles-reports/2021/03/17/who-do-bame-britons-trust-when-it-comes-covid-19 (accessed on 1 September 2021).
- Office for National Statistics. Coronavirus and Vaccination Rates in People Aged 70 Years and over by Socio-Demographic Characteristic, England: 8 December 2020 to 11 March 2021; Office for National Statistics: London, UK, 29 March 2021. [Google Scholar]
- Office for National Statistics. Coronavirus and Vaccination Rates in People Aged 50 Years and over by Socio-Demographic Characteristic, England: 8 December 2020 to 12 April 2021; Office for National Statistics: London, UK, May 2021. [Google Scholar]
- MacKenna, B.; Curtis, H.J.; Morton, C.E.; Inglesby, P.; Walker, A.J.; Morley, J.; Mehrkar, A.; Bacon, S.; Hickman, G.; Bates, C.; et al. Trends, regional variation, and clinical characteristics of COVID-19 vaccine recipients: A retrospective cohort study in 23.4 million patients using OpenSAFELY. MedRxiv 2021. [Google Scholar] [CrossRef]
- Curtis, H.J.; Inglesby, P.; Morton, C.E.; MacKenna, B.; Walker, A.J.; Morley, J.; Mehrkar, A.; Bacon, S.; Hickman, G.; Bates, C.; et al. Trends and clinical characteristics of COVID-19 vaccine recipients: A federated analysis of 57.9 million patients’ primary care records in situ using OpenSAFELY. medRxiv 2021. [Google Scholar] [CrossRef]
- Knights, F.; Carter, J.; Deal, A.; Crawshaw, A.F.; Hayward, S.; Jones, L.; Hargreaves, S. Impact of COVID-19 on Migrants’ Access to Primary Care and Implications for Vaccine Roll Out: A National Qualitative Study. Br. J. Gen. Pract. 2021, 71, e583–e595. [Google Scholar] [CrossRef] [PubMed]
- Caribbean and African Health Network. COVID-19 Vaccines and the Caribbean and African Community; Covid-19 Vaccines Event Report; Caribbean and African Health Network: Manchester, UK, February 2021. [Google Scholar]
- Lockyer, B.; Islam, S.; Rahman, A.; Dickerson, J.; Pickett, K.; Sheldon, T.; Wright, J.; McEachan, R.; Sheard, L.; Bradford Institute for Health Research COVID-19 Scientific Advisory Group. Understanding COVID-19 misinformation and vaccine hesitancy in context: Findings from a qualitative study involving citizens in Bradford, UK. Health Expect. 2021, 24, 1158–1167. [Google Scholar] [CrossRef] [PubMed]
- Barts Health NHS Trust. Staff Share COVID-19 Vaccine Messages in 19 Languages; Barts Health NHS Trust: London, UK, April 2021. [Google Scholar]
- Department of Health and Social Care. Community Champions to Give COVID-19 Vaccine Advice and Boost Take up; Department of Health and Social Care: London, UK, January 2021. [Google Scholar]
- Scientific Advisory Group for Emergencies. Role of Community Champions Networks to Increase Engagement in Context of COVID-19: Evidence and Best Practice. 2020. Available online: https://www.gov.uk/government/publications/role-of-community-champions-networks-to-increase-engagement-in-context-of-covid-19-evidence-and-best-practice-22-october-2020 (accessed on 1 September 2021).
- Bulmer, S.; Mordaunt, E.; Penniston, R.; Biddle, M.; Shand, J. Delivering the COVID-19 vaccine across London: Evaluation Report. 20 July 2021. [Google Scholar]
- National Health Service. COVID-19 Vaccinations. August 2021. Available online: https://www.england.nhs.uk/statistics/statistical-work-areas/covid-19-vaccinations/ (accessed on 16 September 2021).
- CDC Centers for Disease Control and Prevention. COVID Data Tracker. In September 2021. Available online: https://covid.cdc.gov/covid-data-tracker/#vaccination-demographics-trends (accessed on 16 September 2021).
- Scientific Advisory Group for Emergencies. Evidence Summary of Impacts to Date of Public Health Communications to Minority Ethnic Groups and Related Challenges. Available online: https://www.gov.uk/government/publications/evidence-summary-of-impacts-to-date-of-public-health-communications-to-minority-ethnic-groups-and-related-challenges-23-september-2020 (accessed on 1 September 2021).
- The Finance Info. Vaccine Uptake Rises among England’s Ethnic Minorities. 2021. Available online: https://thefinanceinfo.com/2021/04/23/vaccine-uptake-rises-among-englands-ethnic-minorities/ (accessed on 26 July 2021).
- Gov.UK. JCVI Issues Updated Advice on COVID-19 Booster Vaccination. Available online: https://www.gov.uk/government/news/jcvi-issues-updated-advice-on-covid-19-booster-vaccination (accessed on 16 September 2021).
| First Author, Date | Country, Region | Study Design | Data Collection Period | Population Characteristics | Topics Investigated | Top-Line Findings | Risk of Bias Score |
|---|---|---|---|---|---|---|---|
| Allington, 2021a | UK | Quantitative | November— December 2020 | n = 4343 Gender (F) = 51% Age (mean) = 46.23 Ethnic group (White = 91%, Other = 7%) * weighted averages reported | Vaccine hesitancy | Ethnic minority status is associated with vaccine hesitancy, conspiracy suspicions, use of social media for information about coronavirus, negative vaccine attitudes and age. Very weak correlation between membership of an other-than-white ethnic group and trust in scientists, and slightly stronger negative correlation with trust in medical professionals. | 9 (Good) |
| Allington, 2021b | UK | Quantitative | Study 3 and Study 4: June 2020 | Study 3: n = 1663 Age (mean) = 50.0 Gender (F) = 55.1% Ethnicity (White = 94.3%, Other = 5.7%) Study 4: n = 2237 Age (mean) 44.5 Gender (F) 49.7% Ethnicity (White = 89.7%, Other = 10.3%) | Vaccine intention | Study 3: voting history and frequency of legacy media consumption associated with SARS-CoV-2 vaccine intentions. Vaccine intentions negatively associated with other than white ethnicity. Study 4: voting history and informational reliance on legacy and social media associated with SARS-CoV-2 vaccine intentions. Vaccine intentions negatively associated with other than white ethnicity. | 9 (Good) |
| Bell, 2020 | England | Mixed-methods | Survey: April–May 2020 Interviews: April–May 2020 | Survey: n = 1252 Gender: Female (95.0%; n = 1190) White British 1082 (86.4) White Irish 20 (1.6) White Other White background 76 (6.1) Black or Black British—African 3 (0.2) Black or Black British—Caribbean 1 (0.1) Mixed: White and Black Caribbean 7 (0.6) Mixed: White and Black African 1 (0.1) Mixed: White and Asian 9 (0.7) Mixed: Other mixed background 7 (0.6) Asian or Asian British—Indian 15 (1.2) Asian or Asian British—Pakistani 10 (0.8) Asian or Asian British—Bangladeshi 3 (0.2) Asian or Asian British—Other Asian background 3 (0.2) Chinese 2 (0.2) Other ethnic group 7 (0.6) Do not wish to say 6 (0.5) Interview: n = 19 Age (mean) = 33.4 White British (11) Other White background (3) Mixed White and Black Caribbean (2) Mixed White and Asian (1) Asian or Asian British: Pakistani (1) Chinese (1) | Vaccine intention | Black, Asian, Chinese, Mixed or Other ethnicity participants were 2.7 times more likely to reject a COVID-19 vaccine for themselves and for their child than White British, White Irish and White Other participants. | 9 (Good) |
| British Red Cross, 2021 | UK | Quantitative | February 2021 | UK nationally representative sample (n = 2005) Boost of ethnic minorities (excluding White ethnic minorities) sample (n = 1000) Boost of people from Black ethnic groups (n = 503) Boost of people from South Asian ethnic groups (n = 508) | Vaccine hesitancy | Minority ethnic respondents are more likely to get vaccine information from friends and family, trust family more than other sources of vaccine information other than health professionals, discuss their decision about having the vaccine with extended family, and are more likely to have received information encouraging them not to have the vaccine. | 9 (Good) |
| Caribbean and African Health Network, 2021 | UK | Quantitative (survey with open-ended question responses) | January 2021 | n = 220 | Vaccine attitudes, vaccine intention | Vaccine knowledge and intention improved after an educational session. | 7 (Moderate) |
| Freeman, 2020 | UK, North East 192 (3.8%) North West 567 (11.1%) Yorkshire and the Humber 414 (8.1%) East Midlands 357 (7.0%) West Midlands 470 (9.2%) East 405 (7.9%) London 723 (14.1%) South East 731 (14.3%) South West 427 (8.3%) Wales 257 (5.0%) Scotland 465 (9.1%) Northern Ireland 106 (2.1%) | Quantitative | September–October 2020 | n = 5114 Age: 18−24 571 (11.2%); 25−34 898 (17.6%); 35−44 883 (17.3%); 45−54 929 (18.2%); 55−64 761 (14.9%); 65−99 1072 (21.0%). Gender: male 2574; female 2515; nonbinary 20; prefer not say 5. White: English/Welsh/Scottish/Northern Irish/British 4056 (79.3%); Irish 57 (1.1%); Gypsy or Irish Traveller 8 (0.2%); any other White background 204 (4.0%). Mixed: White and Black Caribbean 43 (0.8%); White and Black African 17 (0.3%); White and Asian 34 (0.7%); any other Mixed/Multiple ethnic background 27 (0.5%). Asian/Asian British: Indian 146 (2.9%); Pakistani 105 (2.1%); Bangladeshi 50 (1.0%); Chinese 49 (1.0%); any other Asian background 51 (1.0%). Black/African/Caribbean/Black British: African 128 (2.5%); Caribbean 71 (1.4%); any other Black/African/Caribbean background 16 (0.3%). Other ethnic group: Arab 13 (0.3%); Any other ethnic group 13 (0.3%). | Vaccine hesitancy | Vaccine hesitancy is associated with Black or mixed ethnicity | 9 (Good) |
| Healthwatch, 2021 | Not available | Quantitative | January 2021 | n = 2431 | Vaccine hesitancy | Vaccine hesitancy exists among Black, Asian, and minority ethnic groups | 7 (Moderate) |
| Healthwatch Camden, 2021 | Camden, London | Quantitative | February 2021 | n = 223 (97% BAME) Arab (~1%) Black African & Asian (~1%) Black African & White (~1%) Asian/Asian British: Indian (~2%) Black/Black British: Caribbean (~2%) Asian & White (~2%) Other ethnic background (~2%) Any other White background (~3%) White: British/N. Irish/Scottish/Welsh (~4%) Any other Black/Black British background (~5%) I’d prefer not to say (~8%) Asian/Asian British: Chinese (~9%) Black/Black British: African (~12%) Black/Black British: Somali (~20%) Asian/Asian British: Bangladeshi (~27%) | Vaccine attitudes, vaccine hesitancy | Vaccine hesitancy higher among Black, Asian, and minority ethnic groups compared to national data. | 6 (Moderate) |
| Knights, 2021 | England | Qualitative | June–November 2020 | n = 81 Phase 1: n = 64 clinicians and administrative staff Age (mean) = 45 Gender (F) = 54 (84.4%) White British 32 (50.0%) White Irish 3 (4.7%) African 4 (6.2%) Caribbean 1 (1.6%) Indian 11 (17.2%) Pakistani 3 (4.7%) Other Asian background 2 (3.1%) Other Mixed background 3 (4.7%) Other White background 5 (7.8%) Phase 2: n = 17 migrants Age (mean) ** = 37.9 Gender (F) = 11 (64.7%) WHO Region of Origin (%) = African (Mauritius, Nigeria, Zimbabwe, other) 4 (23.5%), The Americas (Venezuela) 1 (5.9%) Eastern Mediterranean (Afghanistan, Egypt, Iraq, Pakistan, Palestine) 3 (17.6%) South East Asian (Sri Lanka) 4 (23.5%) | Vaccine roll-out | Pre-existing distrust of vaccinations and the NHS alongside low health literacy and widespread misinformation are likely to negatively affect uptake of a potential COVID-19 vaccine in some migrants. Migrants reported views ranging from acceptance to misinformation, often originating from social media or word of mouth. | 10 (Good) |
| Lockyer, 2021 | Bradford, UK | Qualitative | September–October 2020 | n = 20 Age (range 20–85) most aged 25–54 Asian or Asian British (Pakistani, Indian and Bangladeshi) (10) White British (6) White Other (Eastern European, Gypsy or Irish Traveller) (4) | Vaccine hesitancy | Mixed findings: nine would accept a COVID-19 vaccine (with caveats around safety), five felt mixed, and six were not willing to have it. Results were not reported by ethnicity. | 10 (Good) |
| Nguyen, 2021 | UK | Quantitative | March 2020–February 2021 | n = 4,427,024 White (n = 1,204,721) Black (n = 9615) South Asian (n = 17,628) Middle East/East Asian (n = 7689) More than one/other (n = 14,641) Sex (F) and ethnicity: White n = 71,1693 (59.1) Black n = 5642 (58.7) South Asian n = 9883 (56.1) Middle East/East Asian n = 4438 (57.7) More than one/other n = 9016 (61.6) | Vaccine hesitancy, vaccine uptake | 95% of all participants willing to accept vaccine. Racial/ethnic minorities were more likely to report being unsure or unwilling to undergo vaccination. Black frontline healthcare workers had lower vaccine uptake than their White counterparts. | 8 (Good) |
| Office for National Statistics, 2021a | England | Quantitative | December 2020–March 2021 | Age group (vaccination rate %): 70–74 (88.6%), 75–79 (91.5%), 80–84 (92.6%), 85–89 (91.0%), 90–94 (88.0%), 95–99 (83.0%), 100+ (71.1%) Sex (vaccination rate %): Female (90.4%), Male (90.0%) Ethnic group (vaccination rate %): White British (91.3%) Indian (86.2%) White other (81.6%) Mixed (80.4%) Other (77.6%) Chinese (76.7%) Pakistani (74.0%) Bangladeshi (72.7%) Black Caribbean (68.7%) Black African (58.8%) | Vaccine uptake | The percentage vaccinated was lower among all ethnic minority groups compared with the White British population. | 7 (Moderate) |
| Office for National Statistics, 2021b | England | Quantitative | December 2020– April 2021 | Age group (vaccination rate %): 50–59 (89.0%), 60–69 (92.9%), 70–79 (93.2%), 80–89 (96.3%), 90+ (94.9%) Sex (vaccination rate %): Female (92.4%), Male (91.6%) Ethnic group (vaccination rate %): White British (93.7%) Indian (90.9%) Bangladesh (86.9%) Chinese (83.7%) Mixed (81.2%) Other (80.8%) White other (80.8%) Pakistani (78.4%) Black African (71.2%) Black Caribbean (66.8%) | Vaccine uptake | Among people aged 50 years and over, vaccination rates for the first dose of a COVID-19 vaccine were lower for all ethnic minority groups when compared with White British group. | 7 (Moderate) |
| Office for National Statistics, 2021c | UK | Quantitative | March–April 2021 | All adults (16,360) White (15,240) Asian or Asian British (550) Black or Black British (220) Mixed (210) Other ethnic group (120) | Vaccine uptake, vaccine hesitancy | The percentage vaccinated was lower among all ethnic minority groups compared with the White population. | 7 (Moderate) |
| Robertson, 2021 | UK | Quantitative | November–December 2020 | n = 12,035 (12,035 participants completed the Covid-19 wave 6 survey online and the weighted sample is 9981) Gender: Male 4666 (46.8%) Female 5290 (53.0%) Prefer not to say 25 (0.3%) Age: 16–24 920 (9.2%), 25–34 1382(13.8%), 35–44 1543 (15.5%), 45–54 1784 (17.9%), 55–64 1938 (19.4%), 65–74 1532 (15.3%), 75+ 882 (8.8%) White British or Irish 8713 (87.3%) Other White background 269 (2.7%) Mixed 168 (1.7%) Asian or Asian British—Indian 176 (1.8%) Asian or Asian British—Pakistani/Bangladeshi 198 (2.0%) Asian or Asian British—any other group 106 (1.1%) Black or Black British 190 (1.9%) Other Ethnic Group 59 (0.6%) Missing 102 (1.0%); Born in UK: Born in UK 8991 (90.1%) Not Born in UK 824 (8.3%) Missing 166 (1.7%) UK Country: England 8424 (84.4%) Wales 507 (5.1%) Scotland 775 (7.8%) Northern Ireland 275 (2.8%) | Vaccine hesitancy | Higher vaccine hesitancy was seen in most minority ethnic groups compared to the White British or Irish group. | 10 (Good) |
| Royal Society for Public Health, 2020 | UK | Quantitative | December 2020 | n = 2076 | Vaccine attitudes, vaccine intention | Willingness to be vaccinated was lower among people from Black, Asian or Minority Ethnic backgrounds. Respondents from minority backgrounds were more receptive to changing their minds about getting the vaccine if given more information compared with White respondents. | 8 (Good) |
| The OpenSAFELY Collaborative, 2021a | UK | Quantitative | December 2020–January 2021 | n = 1,160,062 (F = 669,278) White = 788,806 Unknown = 325,637 South Asian = 26,936 Black = 10,329 Other = 5539 Mixed = 2805 Age 80+ 476,375; 70–79 years 74,108; health or social care workers under 70 years 378,921; care home residents aged 65 + 32, 174. | Vaccine uptake | The proportion vaccinated was highest in White groups and lower in all ethnic minority groups. | 8 (Good) |
| The OpenSAFELY Collaborative, 2021b | UK | Quantitative | December 2020–March 2021 | n = 2,558,906 F = 1,400,532; M = 1,021,944 White 1,515,535 Unknown 923,363. South Asian 65,975 Black 34,517 Other 10,934 Mixed 8554 | Vaccine uptake | The proportion vaccinated was highest in White groups and lower in all ethnic minority groups. | 8 (Good) |
| Williams, 2021 | Scotland | Quantitative | Time 1: May–June 2020 Time 2: August 2020 | Time 1: Age 18–49 (1847, 53.8%); 50+ (1578, 45.9%) Female (2219, 79.1%) Male (666, 19.4%) White (3308, 96.3%) Black, Asian and Minority Ethnic group (101, 2.9%) Time 2: n = 2016 (59% follow-up rate) Age 18–49 (947, 48.3%); 50+ (1034, 51.5%) Female (1632, 82.1%) Male (355, 17.9%) White (1949, 96.7%) Black, Asian and Minority Ethnic group (52, 2.6%) | Vaccine intention | Participants of White ethnicity had higher levels of intention than those from Black, Asian and Minority Ethnic groups. | 10 (Good) |
| Woolf, 2021 | UK | Mixed-methods | December 2020–March 2021 | Healthcare workers. Cohort Study: n = 11,584 Age, median (IQR): 45 (34–54) Sex (%): Female 2797 (24.2%) White: 6907 (60.8%); Irish 209 (1.8%); Other/Gypsy Irish Traveller 878 (7.7%). Asian: Indian 1187 (10.4%); Pakistani 315 (2.8%); Bangladeshi 69 (0.6%); Chinese 253 (2.2%); Other 365 (3.2%). Black: African 349 (3.1%); Caribbean 102 (0.9%); Other 20 (0.2%). Mixed: White & Black African 66 (0.6%); White & Black Caribbean 84 (0.7%); White & Asian 179 (1.6%); Other 142 (1.3%). Other: Arab 122 (1.1%); Other 123 (1.1%). Qualitative Study: n= 99; 41 interviews (n = 24) and focus groups (n = 17), and 58 from the longitudinal cohort study (free text comments provided about vaccinations). 27 (66%) were women Ethnicity of qualitative participants— Asian 13 (32%) Black 12 (29%) White 10 (24%) 24 were born in the UK (59%) Ethnicity of the 58 cohort participants: White 42 (72%) Asian 8 (14%) Black 4 (7%) 48 participants (83%) were women | Vaccine hesitancy | Healthcare workers from Black Caribbean, Black African and White Other ethnic groups were significantly more likely to be vaccine hesitant compared to White British healthcare workers. | 10 (Good) |
| YouGov, 2021a | UK Region: London = 400 Rest of South = 200 Midlands/Wales = 210 North = 160 Scotland = 30 | Quantitative | February 2021 | Male 482; Female 518 Age: 18–24 = 155; 25–49 = 579; 50–64 = 184; 65+ = 82. Black = 241 Indian = 201 Pakistani = 149 Other ethnicity = 118 Other Asian = 110 Mixed = 84 Bangladeshi = 56 Chinese = 40 Country of birth—UK = 370; Outside of the UK = 630. | Vaccine attitudes, Vaccine intention | The majority of respondents had positive intentions of getting a vaccine and a more favourable attitude towards the Pfizer-BioNtech coronavirus vaccine compared with the AstraZeneca and Moderna vaccine. | 6 (Moderate) |
| First Author, Date | Facilitators | Barriers | Differences between MEGs | Recommendations |
|---|---|---|---|---|
| Allington, 2021a | - | Conspiracy suspicions Vaccine attitudes Lower scientific and medical trust | - | Further data required to understand reasons for different vaccine attitudes and conspiracy suspicions. |
| Allington, 2021b | - | Reduced use of legacy media Social media inadequate replacement to legacy media | - | - |
| Bell, 2020 | - | - | - | - |
| British Red Cross, 2021 | Key communications with trusted sources such as healthcare professional and scientists Family conversations | Concerns about side effects Misinformation | Black Caribbean, Black African or Pakistani groups are most likely to reject the vaccine. Indian and Chinese communities are just as likely to have already had/planning to have the vaccine as the UK average. | Individuals from minority ethnic backgrounds should not be approached as one homogenous group. Adopt a person-centred approach to communications. |
| Caribbean and African Health Network, 2021 | Key communications with individuals they identify with and influential others such as Black medical professionals and religious leaders | Perceived health inequalities Misinformation Lower scientific and medical trust | - | Community-led online events with medical professionals. Health messaging and education should target the Black community, with integration of faith and community leaders. Build trust in medical professionals (for example after historic medical mistreatment of Black individuals) and provide education on the UK’s health and social care system (e.g., clinical trials). |
| Freeman, 2020 | Beliefs about collective importance of a COVID-19 vaccine | Mistrust | - | Enhancing and improving health messaging to emphasise prosocial benefits of the vaccine; attuned to different kinds of collective identities; transparent about safety and efficacy. |
| Healthwatch, 2021 | Wait until others have the vaccine before getting it themselves | Logistical issues such as location of vaccination sites and using public transport Mistrust of vaccine programme/rollout | - | Find out what differences exist in attitudes and barriers for different parts of the Black and Asian communities. |
| Healthwatch Camden, 2021 | More information | - | People from Black or Black British (mainly Somali, African, Caribbean, or other Black/Black British) background were more hesitant to get the vaccine. People who identified as Asian or Asian British (mainly Bangladeshi, Chinese, and Indian) had less vaccine hesitancy than the ethnic minority group average. | Integrate views of Black, Asian and Minority Ethnic groups into NHS practice and care. Conduct further research into the informational needs of minority ethnic communities including what information is needed, when, where and in what format. Coproduce communication campaigns. |
| Knights, 2021 | - | Pre-existing distrust of vaccinations and the NHS Concerns about vaccine safety Migrant communities have not been included in trials Low health literacy Misinformation and contradiction of information between different information sources Seeking information from country of origin Digitalisation resulted in lack of access to knowledge and communication barriers Beliefs COVID-19 is a Western disease Fear of discrimination or being used as ‘guinea pigs’ Reliance on home remedies | - | Innovations in service delivery such as translated health advice using text templates and YouTube. Practices should seek to ensure they can identify migrants, that they understand their needs through proactive engagement, and that they are providing language-specific advice about COVID-19 and changes in service provision in the pandemic through multiple modalities (e.g., text, email, letter and posters in local community hubs). Use of patient participation groups and other local community groups to codesign delivery approaches. Ensure availability of interpreters and translated culturally-appropriate vaccine advice, alongside integration of migrant ambassadors into vaccine centres, and information-sharing campaigns. |
| Lockyer, 2021 | Will wait 3–6 months to see what the effects of the vaccine are on others. | Concerns about speed of vaccine development and unknown side effects Social media stories about misinformation and severe side effects which results in confusion and not refusal Rumours that ethnic groups are being targeted to test the vaccine or used to harm them | - | Hesitancy is rooted in anxiety fuelled by misinformation which needs to be mediated by clear, honest and responsive information that is sensitively framed and nonjudgemental. Provide health, social and community workers with an up-to-date summary of locally circulating misinformation with resources to help them counter concerns and provide informed reassurance. |
| Nguyen, 2021 | - | Mistrust of the medical system Lack of diverse representation in clinical trials The speed with which vaccines were approved has raised suspicions over whether regulatory standards meant to protect vulnerable populations were relaxed for expediency | Black groups more hesitant or unsure followed by Middle East/East Asian, South Asian, and Other groups. Vaccine uptake highest in South Asian group and lower in Black healthcare workers. | Need to address long-standing systemic disparities to achieve the health equity required for population-scale immunity. |
| Office for National Statistics, 2021a | - | - | The lowest vaccination rates were among Black African, Black Caribbean, Bangladeshi and Pakistani groups. The vaccination rate among people from an Indian background was lower than that of the White British group but was high overall. | - |
| Office for National Statistics, 2021b | - | - | Vaccination rates were lowest for Black Caribbean, Black African and Pakistani groups. Although lower than the White British group, vaccination rates among Indian and Bangladeshi groups remained high. | - |
| Office for National Statistics, 2021c | - | - | Around 1 in 3 Black or Black British adults reported vaccine hesitancy, the highest compared with all ethnic groups. | - |
| Robertson, 2021 | If the vaccine was demonstrated to be safe and reduced their risk | Lack of trust in vaccines Concerns about side effects | Black or Black British were the ethnic group with the highest rate of vaccine hesitancy followed by Pakistani/Bangladeshi groups and those of Mixed ethnicity. Black participants were more likely to state they do not trust vaccines and Pakistani/Bangladeshi groups cited worries about side effects. | Include subgroups that are hesitant in the planning and development of engagement programmes. Initiatives to improve uptake in Black ethnic groups within the UK should be an urgent priority; for example, by working in close partnership with communities and making use of community champions. |
| Royal Society for Public Health, 2020 | Information about the vaccine from GP or another health professional Information about the effectiveness, side effects and ingredients of the vaccine Social media influences Family and friends influence | Concerns about side effects Vaccine not tested in diverse ethnic groups Mistrust | Lowest willingness to be vaccinated in Asian respondents. The sample sizes were too small to draw any substantive conclusions, but the levels of confidence in the vaccine appear to be broadly similar across minority groups. | Support people to have productive conversations with their peers and relatives about common concerns surrounding the vaccine. Healthcare professionals need to be equipped with both the resources and the time to address the concerns of individual patients about the Covid-19 vaccine. Further research to understand why vaccine confidence is lower in minority ethnic groups. |
| The OpenSAFELY Collaborative, 2021a | - | - | The proportion vaccinated was lowest in Black people followed by mixed, other and South Asian ethnicities. People from Black African groups had the lowest vaccination rates followed by Other Black and Mixed Black, Caribbean, Pakistani and Bangladeshi groups. | The reasons underpinning variation in vaccination coverage are not yet understood. Further research is needed to understand and address the disparity between ethnic groups. |
| The OpenSAFELY Collaborative, 2021b | - | - | Vaccination coverage was lowest in all Black groups with the lowest uptake in Black African followed by Mixed White and Black African, any other Black background, Black Caribbean, and Mixed White and Caribbean groups. The lowest uptake in Asian groups was Pakistani followed by Chinese, Any other ethnic group, and Bangladeshi groups. | - |
| Williams, 2021 | - | - | - | A better understanding of the barriers to vaccination in subpopulations and diverse communities is required to collectively be better prepared to deliver appropriate evidence-based culturally and community-appropriate messaging aimed at maximising COVID-19 vaccine uptake. |
| Woolf, 2021 | Vaccine confidence among family, friends and community members Increased risk perception based on previous infection, knowing people who had been unwell or passed away from COVID-19, and concerns about infection of their families and loved ones Increased visibility of less well represented groups in the media More proactive involvement and engagement of healthcare workers from diverse ethnic backgrounds | Complex information, conflicting and changing guidance, overwhelming amounts of material, and poor provision of information in other languages Mistrust of mainstream media Conspiracy beliefs Underrepresentation of individuals from ethnic minority backgrounds in vaccine trials Lack of inclusion of marginalised communities throughout the pandemic | Black Caribbean healthcare workers were most hesitant followed by Mixed White and Black Caribbean, Black African, Chinese, Pakistani, and White Other groups compared with Indian and Bangladeshi healthcare workers who had lower levels of hesitancy. | Develop inclusive communication through a range of media and languages, and engage directly with people to respond to questions or concerns, and tackle misinformation. Use language which avoids assumptions or stereotyping associated with ethnicity. Equity in accessibility and opportunity to have the vaccine is paramount for improving delivery. |
| YouGov, 2021a | Hearing positive things about the vaccine | Don’t know enough about the vaccine Concerns about safety Lack of trust in science underpinning vaccine Hearing negative stories | Chinese groups had the strongest intention to get vaccinated followed by Indian and Mixed groups, and people in the Black group had the lowest intention to get vaccinated. | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kamal, A.; Hodson, A.; Pearce, J.M. A Rapid Systematic Review of Factors Influencing COVID-19 Vaccination Uptake in Minority Ethnic Groups in the UK. Vaccines 2021, 9, 1121. https://doi.org/10.3390/vaccines9101121
Kamal A, Hodson A, Pearce JM. A Rapid Systematic Review of Factors Influencing COVID-19 Vaccination Uptake in Minority Ethnic Groups in the UK. Vaccines. 2021; 9(10):1121. https://doi.org/10.3390/vaccines9101121
Chicago/Turabian StyleKamal, Atiya, Ava Hodson, and Julia M. Pearce. 2021. "A Rapid Systematic Review of Factors Influencing COVID-19 Vaccination Uptake in Minority Ethnic Groups in the UK" Vaccines 9, no. 10: 1121. https://doi.org/10.3390/vaccines9101121
APA StyleKamal, A., Hodson, A., & Pearce, J. M. (2021). A Rapid Systematic Review of Factors Influencing COVID-19 Vaccination Uptake in Minority Ethnic Groups in the UK. Vaccines, 9(10), 1121. https://doi.org/10.3390/vaccines9101121






