1. Introduction
SARS-CoV-2 has rapidly become a pandemic, with sustained human-to-human transmission [
1,
2] and an exponential rise in the number of COVID-19 cases [
3,
4]. The reasons for the rapid virus spread include its high transmissibility also from asymptomatic or minimally symptomatic carriers, the apparent absence of cross-protective immunity from related coronavirus infections, as well as the tardy public health response measures [
5,
6].
Italy was affected early and badly by the pandemic, with the first outbreaks occurring on the 21st of February in Lombardy and Veneto. On the 31st of January, when COVID-19 was still a Public Health Emergency of International Concern, Veneto region had already organized an emergency coronavirus plan. This included, among other measures, an extended diagnostic approach, specially dedicated first aid and hospital wards, along with a biological and clinical register of COVID-19 cases. The plan became active on the 21st of February when two patients from Vo’ village, admitted at the Schiavonia hospital under suspicion of influenza virus infection, were found positive to SARS-CoV-2. On the 23rd of February, following a regional decree, the hospital was rapidly evacuated, and a complete lockdown was imposed on Vo’ village, whose entire population had to undergo swab testing. Meanwhile, other outbreaks were occurring in the Veneto provinces of Padua, Venice, and Treviso and thousands of diagnostic swabs were executed to suspected and at-risk or exposed individuals. A careful monitoring of the contagion wave was conducted, and all data (clinical, epidemiological, and virus-related) were transmitted daily to the information technology service of Veneto region.
The present study deals with data in Veneto, in the period from 28 February to 15 May, a time lapse during which SARS-CoV-2-positive cases were rapidly growing to reach a peak towards 26 March, and then decreasing with lower speed. We stress that 15 May corresponds approximately to the end of the Italian lockdown. The tested population was homogeneously studied for a number of features and events that include gender, age, positivity to test, comorbidities, care location, and death.
The relation among these parameters is of particular biological relevance, since, ideally, it is unbiased from containment and therapeutic measures that were successively adopted to curb the contagion spread. Moreover, the investigation stems from a geographically uniform population in the early stage of the pandemic.
It is clear that the final control of the pandemic requires the development of a harmless and effective vaccine and subsequent massive vaccination campaign. Waiting for this to happen, useful measures to limit the spread of infection and minimizing mortality have been introduced [
7]. However, a vaccination campaign over a large population needs months (or even a year) to be implemented. During this period, suitable priority criteria should be designed for the administration of the vaccine, aiming at containing both virus diffusion and mortality. The results of our work on the influence on the infection and mortality of some variables like age and comorbidities can be used to formulate such criteria.
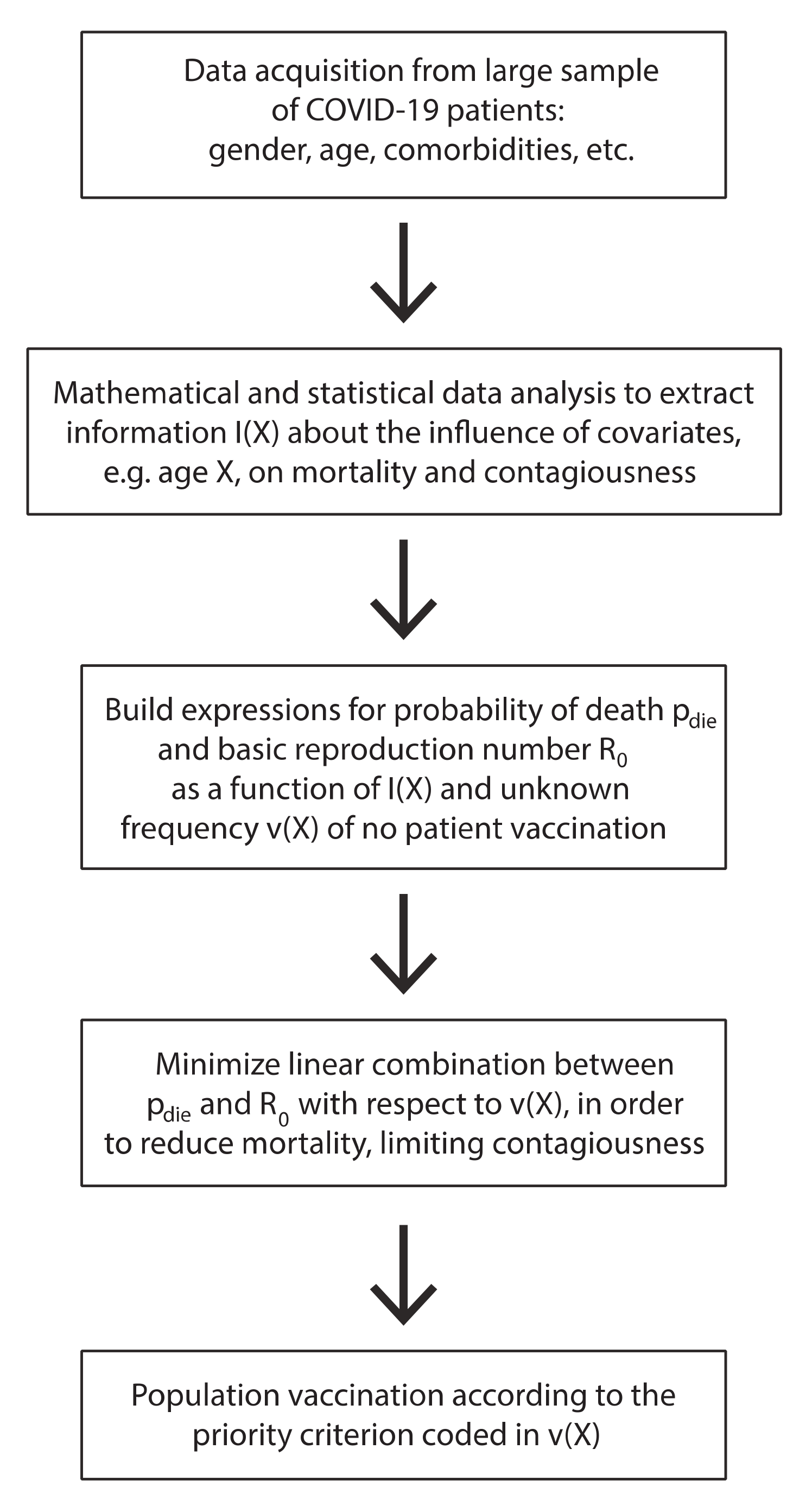
The nature of the work described in this paper is explained in the schematic representation given in
Figure 1.
2. Materials and Methods
The different analyses we conducted are based on robust mathematical and statistical methods and involved two main types of problems: data fitting and hypothesis testing. In both the cases, depending on the specific problem, we adopted either the parametric or the non-parametric approach.
As regards the data fitting, we used the Gaussian kernel density estimation (G-KDE) method for the non-parametric approach [
8,
9,
10], which consists in the linear combination of Gaussian densities centered at observations and with variance depending on a positive parameter, called the bandwidth. The latter’s value was found by an optimal method for the Gaussian kernel. For the parametric approach, we instead used an extended logistic model [
11] with an additional parameter, i.e., the exponent of the denominator. In this case, the parameters were optimized following the least squares criterion. Whenever needed, in order to reduce the periodic effect of the weekly varying number of swabs, we considered an additive pure-sine periodic component.
Concerning the hypothesis testing, within the non-parametric statistics, we performed the Kolmogorov–Smirnov (KS) test [
10,
12] for the null hypothesis of two empirical distributions to be statistically different from each other (e.g., distribution of first symptoms time for males vs. females). The Chi-squared test [
10] was instead adopted when dealing with contingency tables as a parametric method to assess the dependence of the probability of a certain event (e.g., death) on a given factor (e.g., comorbidities).
All the methods were implemented by us in MATLAB language. In particular, we developed the code of the KS test and the contingency table Chi-squared test. The MATLAB (MathWorks, Natick, MA, USA) functions ksdensity and nlinfit were used for Gaussian Kernel density estimation and non-linear fitting of the parametric models to the data, respectively.
4. Impact of the Results on Public Health
The present paper is a really comprehensive description of the epidemiological and clinical impact of the COVID-19 pandemic on Veneto region, an area of 18,399 km2 with nearly 5 million inhabitants.
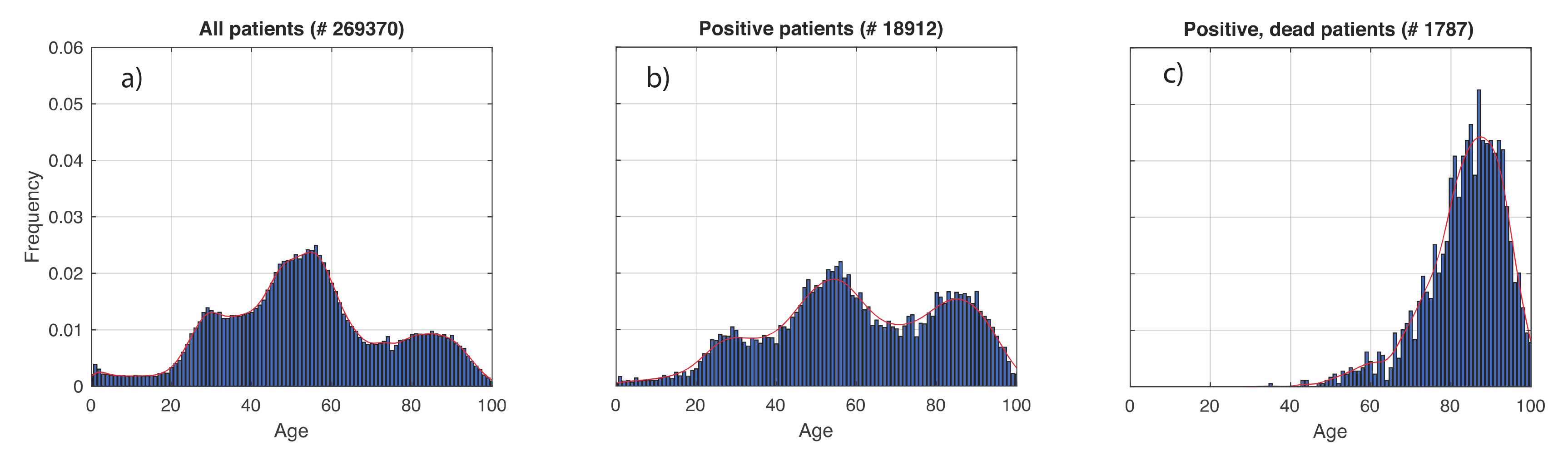
The results show that age is playing a critical and statistically significant role in determining the groups of individuals most prone to being infected by SARS-CoV-2 (group over 70 years) and to die from COVID-19 (group over 80 years). While the age peak for death is similar to that reported in the literature [
14], the prevalent age of COVID-19 incidence is different from the one that occurred in other European nations like Germany, where young individuals were the most affected in the population [
15,
16].
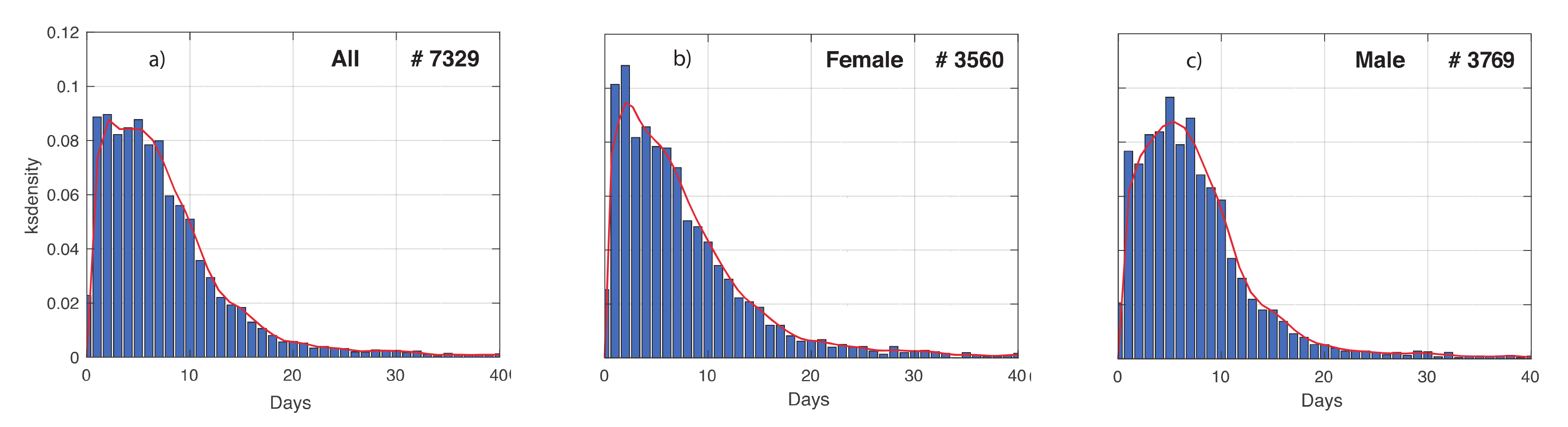
The Veneto cohort also shows that the probability of getting infected or dying from SARS-CoV-2 is greater for males than females, a result similar to what is described by others [
17]. An X chromosome polymorphism of the Angiotensin Converting Enzyme 2 receptor as well as an androgenic hormone-driven expression of the furin-like transmembrane serine protease 2 have been implied [
18,
19]. In addition, a male-specific development of anti-interferon antibodies was recently suggested [
20]. Moreover, females exhibit a significantly shorter time interval between symptoms and first positive test and no statistically significant difference with males between first positive test, cure, or death, features that are more akin to behavioral than to biological differences.
As expected, COVID-19 patients over 60 have a higher death probability when admitted to ICU with respect to patients under 60. A surprising result is the observation that admission to ICU with respect to no ICU admission carries a higher relative death risk increase (60 fold) for younger patients than for older patients (2–3 fold). This paradoxical phenomenon could rest on the fact that patients over 60 may have been suffering for a longer period from a number of multiorgan pathological conditions that intensive care treatment can alleviate but not stop. Instead, patients under 60 could be in a more acute phase of organ damage due to an abrupt virus systemic infection that dramatically increases fatality.
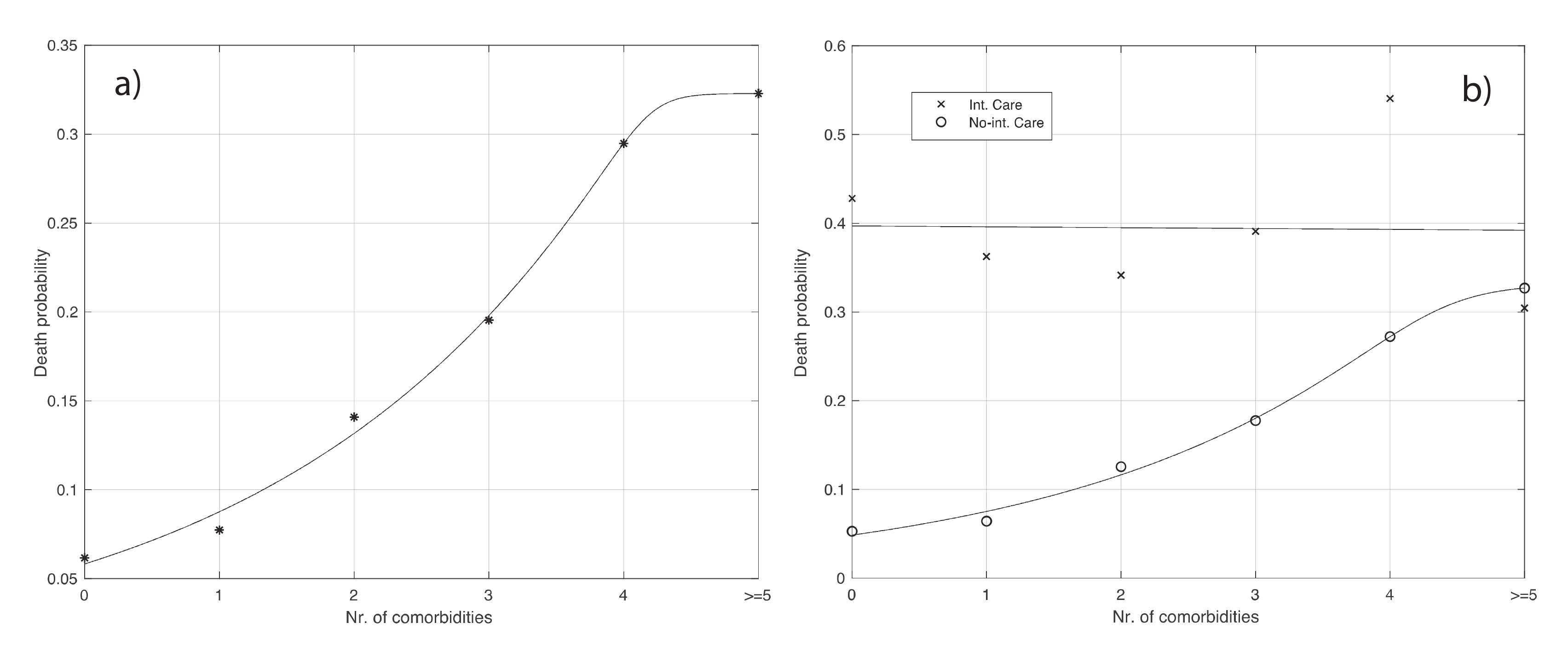
In agreement with several observations [
21], our data also show that the number of comorbidities is directly linked to more severe cases and death. However, this phenomenon does not hold true for patients in ICU, whose clinical status is most likely so serious that comorbidities can have only a minor effect on the chance to live.
We have shown how different clinical and epidemiological variables impacted on COVID-19 evolution at an early stage of the pandemic, under conditions at which medical treatment was not yet optimized due to a lack of properly controlled clinical studies. A number of lessons and insightful thoughts can be drawn from this analysis. First, attention should be payed to prevent contagion spreading to elderly people and subjects suffering from comorbidities, who represent the most exposed and SARS-CoV-2-susceptible populations. They should be carefully protected and isolated. Second, ICUs represent the last resource from which to seek help from, since we have recently shown in different national and regional realities that a direct relation exists between an excess of ICU bed availability and COVID-19 mortality [
22]. Third, when dealing with hospitalized patients, antiviral treatment with Remdesivir, the only effective drug against SARS-CoV-2 lower respiratory tract infection [
23], should be started early in the symptomatic phase, a common practice for many viral infections. Critical manifestations, such as cytokine storms [
24], that necessarily lead to ICU transfer should also be prevented by carefully monitoring markers of inflammation, coagulopathy, alveolar, and endothelial damage [
25]; an appropriate use of inhibitors of these processes could be a life-saving procedure pre-ICU.
5. Mathematical Implementation of Vaccination
In this section, we describe how to use the results previously obtained to implement a SARS-CoV-2 vaccination campaign. The final goal is to eliminate, or significantly reduce, virus circulation. Since it may take several months or even a year to provide the vaccine to some tens of millions of people in a country, selective criteria should be used to limit mortality in the meanwhile. The results presented above on the influence of the contagiousness and mortality of some covariates like age and number of comorbidities, could be used to formulate such criteria quantitatively within a mathematical framework.
Let us now focus on the age covariate. As we have seen in
Figure 2b,c, the probability of being infected and the one of dying significantly depends on age, especially for mortality. Therefore, if we want to limit mortality during the vaccination campaign, priority should be given to older people because of their very high risk of dying. As said before, we also need to limit the spread of the virus to which older people seem to contribute less as being less infected (see
Figure 2b) and they have a lower average number of contacts. Hence, this population layer should not be prioritized for vaccination. The two qualitative criteria conflict with each other and a trade-off between them is needed. A mathematical approach could solve this problem by quantitatively accounting for contagiousness and mortality at the same time. Hereafter, we will first focus on preserving lives of the population. Then, we will move to the case of reducing virus circulation. Finally, we will consider both objectives at the same time.
Let us consider the overall probability of death during vaccination, which is given by:
where
is the probability density function (PDF) of dying from COVID-19 conditioned to the age
of a positive subject,
is the probability of being positive to SARS-CoV-2 of an individual given his age
,
is the PDF of the age
of a subject in the population considered, while
is the probability of non being vaccinated for an individual of age x. For the sake of simplicity, we assume here that vaccinated individuals cannot die from COVID-19. The function
integrate to 1. For practical purposes, we discretize the above equation with the step of one year, obtaining:
with:
where
is the fraction of population not being vaccinated and
, with
being the number of
in the COVID-19 death age support [
of the analyzed set of patients. We then have to solve the constrained optimization problem:
This kind of problem is known as the
linear programming problem [
26], which can be solved by the simplex method [
27]. When applying the proposed methodology to our dataset, the product
corresponds to the empirical histogram in
Figure 2c. Intuitively, to minimize
, small values of
should be associated to large values of
. Here, this product has a peak around 85 years (see
Figure 2c), and therefore, around that peak, we should choose small values of the weights
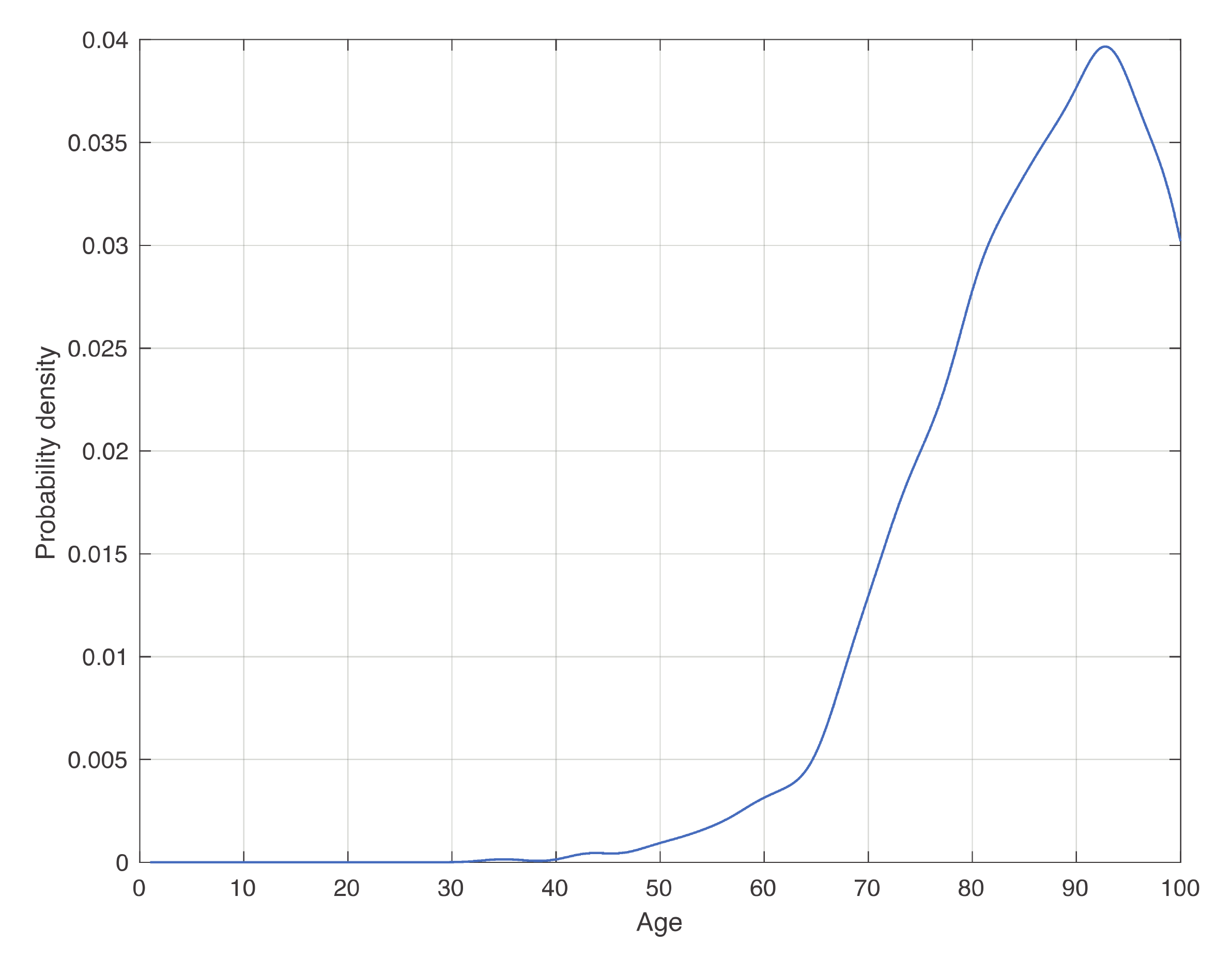
, which corresponds to a high frequency of vaccination. Instead, in a general condition, one can use the estimate of
shown in
Figure 3, while the other two factors should be estimated from data in the specific context considered. Sharp upper and lower bounds for
can also be introduced.
We turn now to the case where we focus on the virus circulation. To do this, let us consider the basic reproduction number
, which represents the mean value of number of infections generated by a single positive individual. It is natural to assume that
depends on age, as it is influenced by both transmissibility and the mean number of contacts of an individual, which, in turn, intuitively depend on age. Then, we can write the mean value of
during vaccination as:
where the meaning of the last three factors is the same as before, and we directly deal with the discretized version. Following the same calculations, after replacing
by
, we end up with a similar linear programming problem.
The final step consists of taking into account mortality and contagiousness at the same time. To deal with this issue, one can consider the linear combination , where . The two extreme choices above correspond respectively to and . The tuning of the value of from 0 to 1 will allow variation of the relative weight of contagiousness and mortality on the final vaccination criterion. One way to proceed consists of first assigning priority to either contagiousness or mortality, that is a political issue. For example, let us give priority to mortality. Then, we consider different values of , and for each of them, we find the weights which minimize the linear combination above. An optimal can therefore be chosen as the smallest value, such that the computed in will not exceed a given threshold value, fixed on the basis of epidemiological knowledge. We could act similarly for the opposite choice.
The procedure above can also be applied for the number of the comorbidities covariate. More specifically, focusing for example on the probability of death, the expression of
becomes:
where
is the death probability for a patient with a number
i of comorbidities,
is the frequency for a patient of the population under study having
i comorbidities,
is the frequency by which an individual with
i comorbidities is not vaccinated, and
is the maximum number of comorbidities in the set of patients considered. Following the same calculations as before, we end up with the following linear programming problem: