Macrophage Activation Assays to Evaluate the Immunostimulatory Capacity of Avibacterium paragallinarum in A Multivalent Poultry Vaccine
Abstract
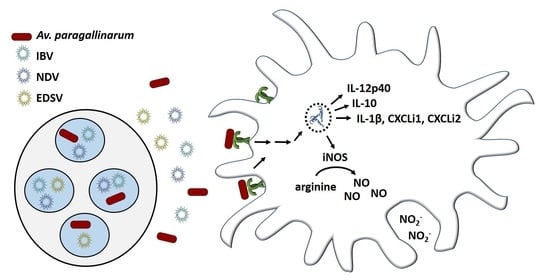
:1. Introduction
2. Materials and Methods
2.1. HD11 Cell Culture and Stimulation
2.2. Griess Test to Evaluate Nitric Oxide Production by Stimulated HD11 Cells
2.3. Relative Expression of iNOS and Cytokines Using Real-Time Quantitative PCR
2.4. Flow Cytometric Assessment of HD11 Cell Viability after Stimulation
2.5. Statistical Analysis
3. Results
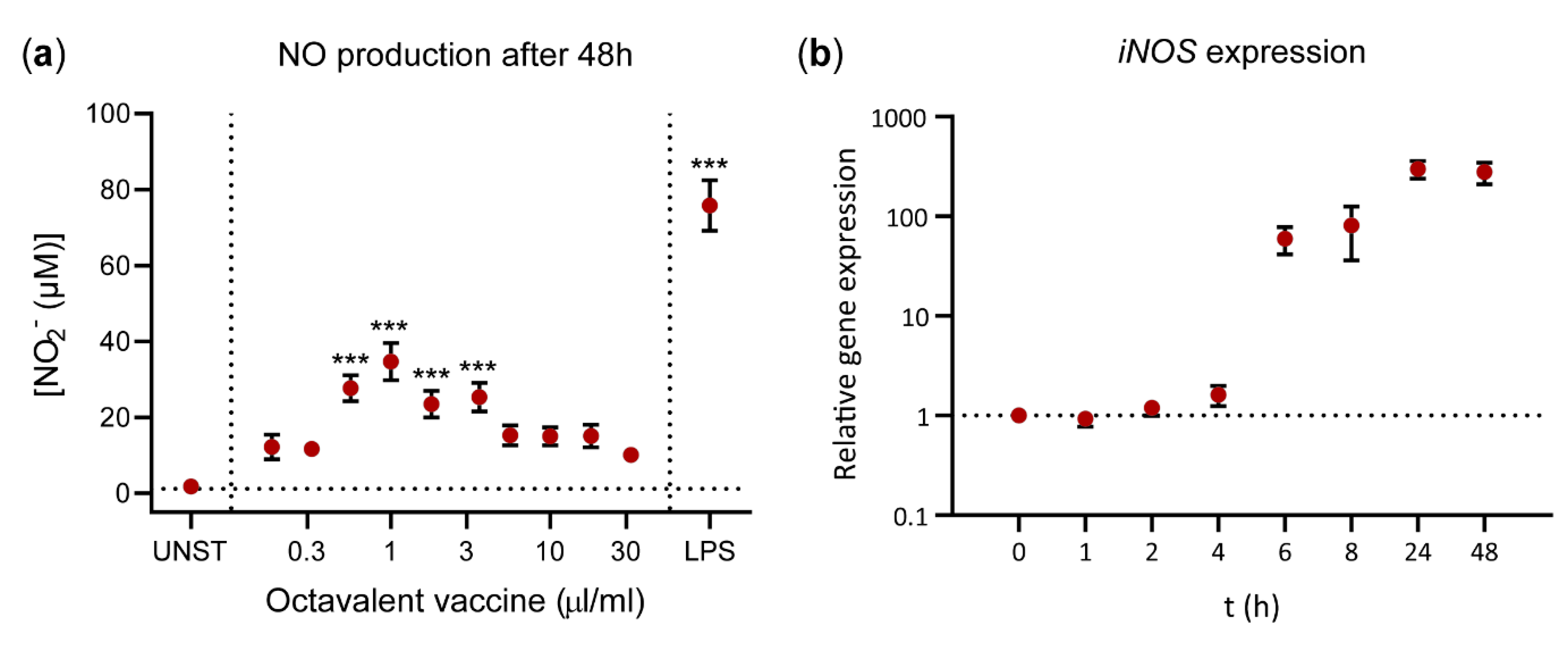
3.1. The Inactivated Octavalent Poultry Vaccine Induces HD11 Cells to Produce Nitric Oxide
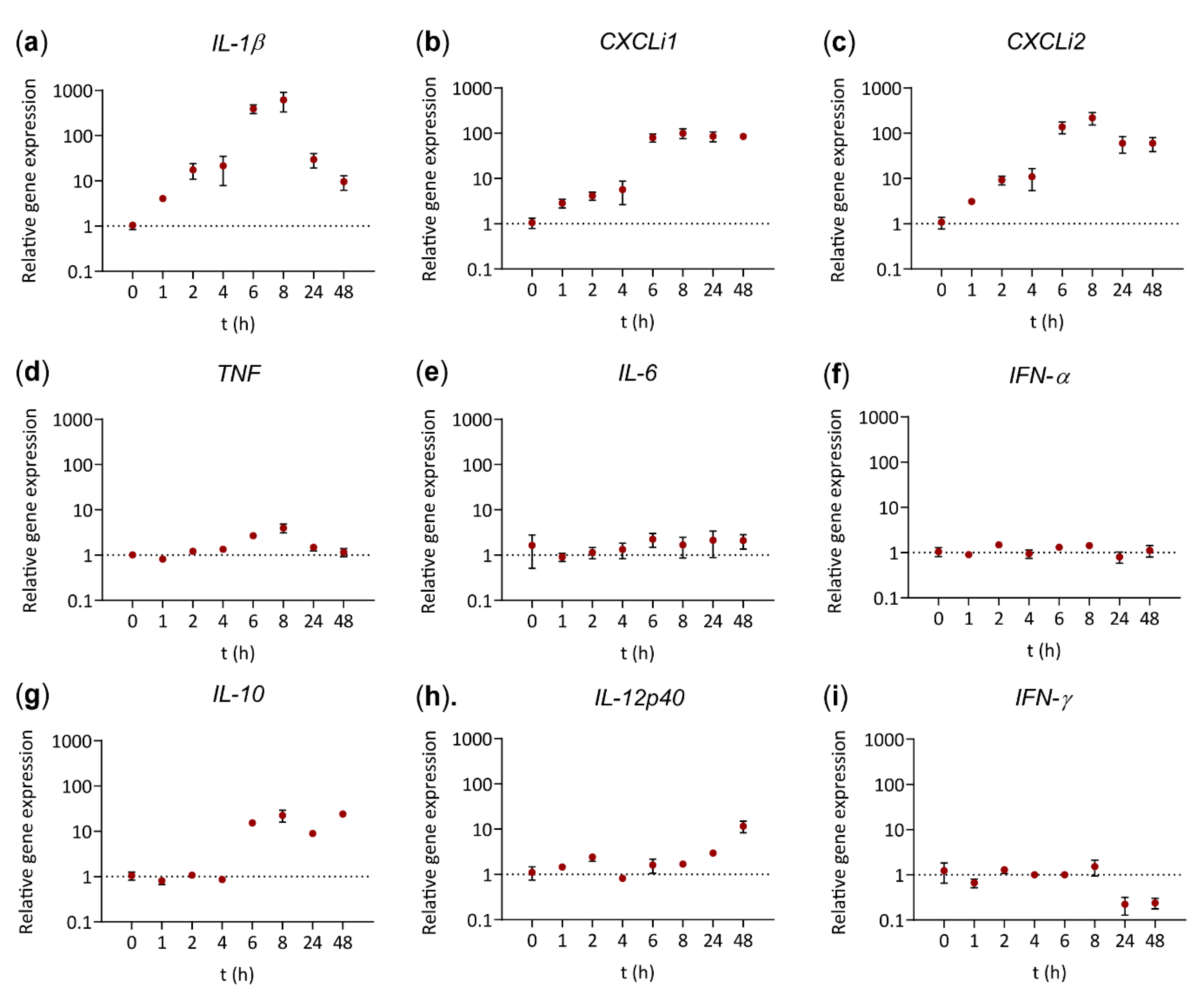
3.2. Stimulation with the Octavalent Vaccine Results in Enhanced Gene Expression of Cytokines and Chemokines
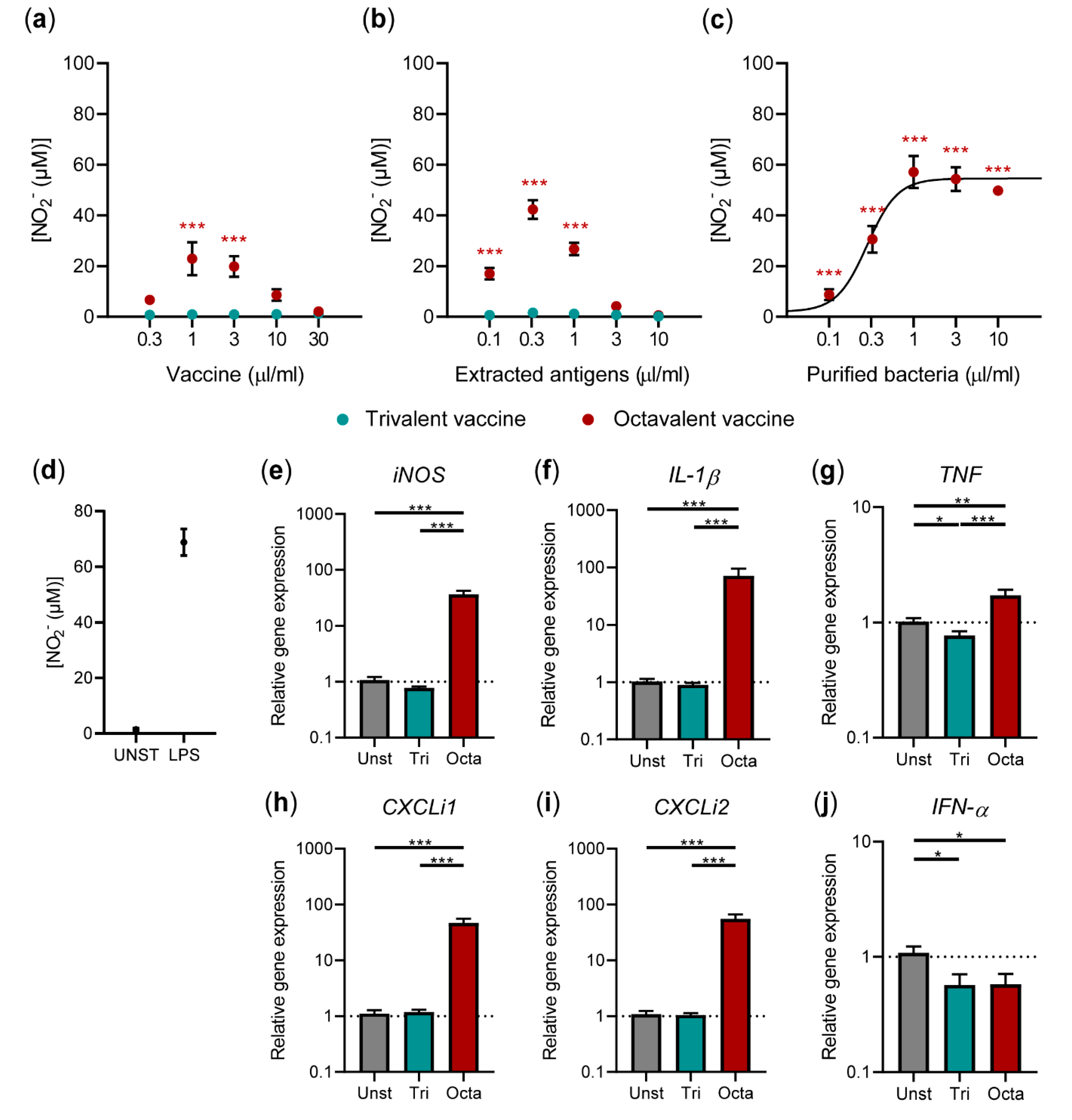
3.3. Av. Paragallinarum Antigens Contribute to the Stimulatory Capacity of the Octavalent Vaccine
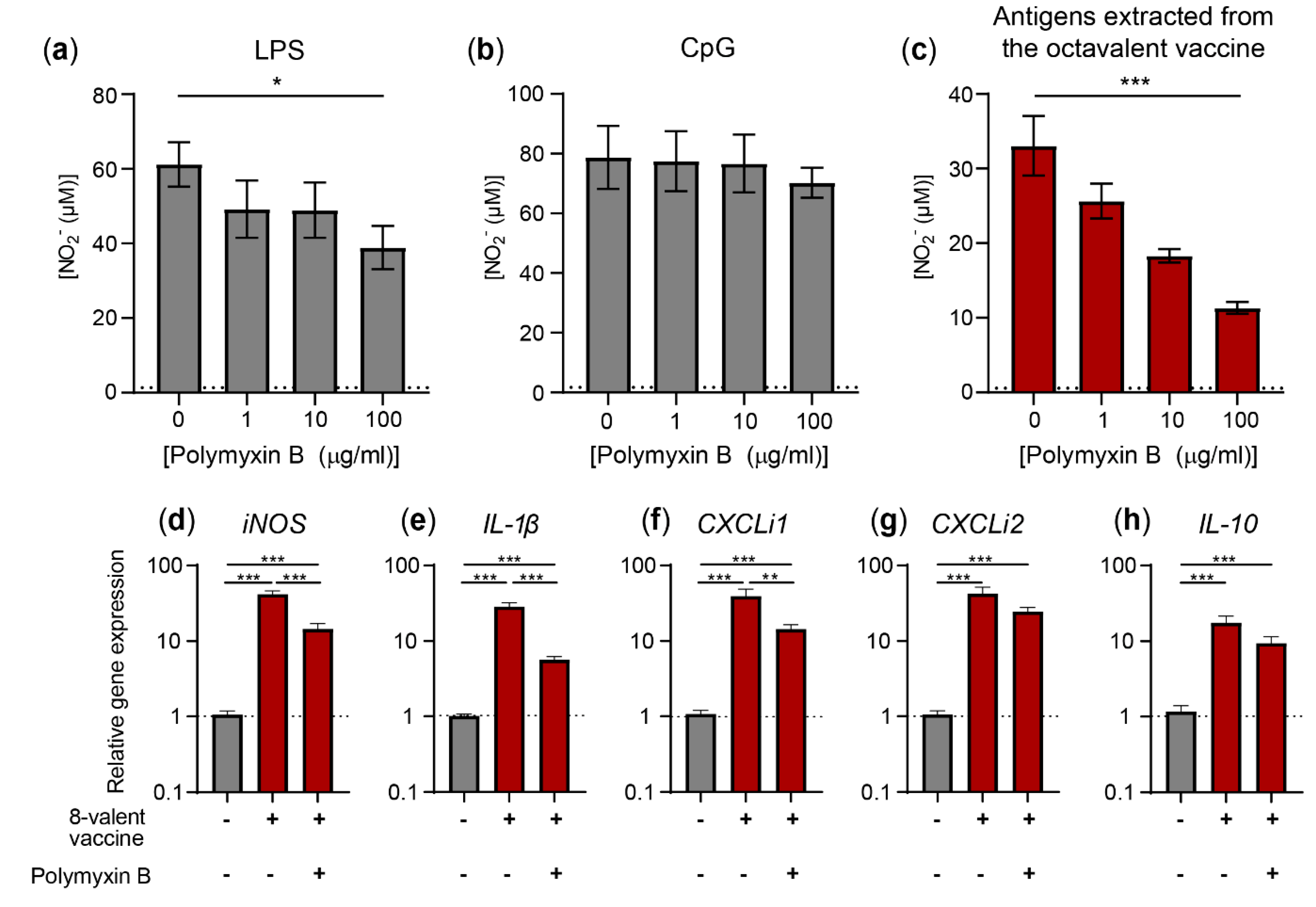
3.4. Activation of HD11 Cells by the Octavalent Vaccine Largely Depends on Av. Paragallinarum Antigen-Associated LPS
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hendriksen, C.; Arciniega, J.L.; Bruckner, L.; Chevalier, M.; Coppens, E.; Descamps, J.; Duchêne, M.; Dusek, D.M.; Halder, M.; Kreeftenberg, H.; et al. The consistency approach for the quality control of vaccines. Biologicals 2008, 36, 73–77. [Google Scholar] [CrossRef]
- Hendriksen, C.F.M. Replacement, reduction and refinement alternatives to animal use in vaccine potency measurement. Expert Rev. Vaccines 2009, 8, 313–322. [Google Scholar] [CrossRef] [PubMed]
- Bruysters, M.W.; Schiffelers, M.-J.; Hoonakker, M.; Jungbaeck, C.; Ragan, I.; Rommel, E.; Van Der Stappen, T.; Viviani, L.; Hessel, E.V.; Akkermans, A.M.; et al. Drivers and barriers in the consistency approach for vaccine batch release testing: Report of an international workshop. Biologicals 2017, 48, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Blackall, P.J.; Soriano, E.V. Infectious Coryza and Related Bacterial Infections. In Diseases of Poultry, 12th ed.; Saif, Y.M., Fadly, A.M., Glisson, J.R., McDougald, L.R., Nolan, L.K., Swayne, D.E., Eds.; Blackwell Publishing: Hoboken, NJ, USA, 2008; pp. 789–803. [Google Scholar]
- Page, L.A. Haemophilus infections in chickens. I. Characteristics of 12 Haemophilus isolates recovered from diseased chickens. Am. J. Vet. Res. 1962, 23, 85–95. [Google Scholar]
- Otsuki, K.; Iritani, Y. Preparation and Immunological Response to a New Mixed Vaccine Composed of Inactivated Newcastle Disease Virus, Inactivated Infectious Bronchitis Virus, and Inactivated Hemophilus gallinarum. Avian Dis. 1974, 18, 297. [Google Scholar] [CrossRef] [PubMed]
- Maas, P.; De Winter, M.; Venema, S.; Oei, H.; Claassen, I.M. Antigen quantification asin vitroalternative for potency testing of inactivated viral poultry vaccines. Vet. Q. 2000, 22, 223–227. [Google Scholar] [CrossRef] [Green Version]
- Claassen, I.; Maas, R.; Oei, H.; Daas, A.; Milne, C. Validation study to evaluate the reproducibility of a candidate in vitro potency assay of newcastle disease vaccines and to establish the suitability of a candidate biological reference preparation. Pharmeur. Bio 2004, 2004, 1–15. [Google Scholar]
- EDQM. Newcastle Disease Vaccine (Inactivated). In European Pharmacopoeia, 10th ed.; Monograph 870; EDQM: Strasbourgh, France, 2019; pp. 1134–1136. [Google Scholar]
- EDQM. Avian Infectious Bronchitis Vaccine (Inactivated). In European Pharmacopoeia, 10th ed.; Monograph 0959; EDQM: Strasbourgh, France, 2019; pp. 1059–1060. [Google Scholar]
- EDQM. Egg Drop Syndrome ’76 Vaccine (Inactivated). In European Pharmacopoeia, 10th ed.; Monograph 1202; EDQM: Strasbourgh, France, 2019; pp. 1100–1101. [Google Scholar]
- EDQM. Vaccines for veterinary use. In European Pharmacopoeia, 10th ed.; EDQM: Strasbourgh, France, 2019; pp. 896–900. [Google Scholar]
- García, A.; Romo, F.; Ortiz, A.M.; Blackall, P.J. The vaccination-challenge trial: The gold standard test to evaluate the protective efficacy of infectious coryza vaccines. Avian Pathol. 2008, 37, 183–186. [Google Scholar] [CrossRef]
- Kleinnijenhuis, J.; Quintin, J.; Preijers, F.; Joosten, L.A.B.; Ifrim, D.C.; Saeed, S.; Jacobs, C.; Van Loenhout, J.; De Jong, D.; Stunnenberg, H.G.; et al. Bacille Calmette-Guerin induces NOD2-dependent nonspecific protection from reinfection via epigenetic reprogramming of monocytes. Proc. Natl. Acad. Sci. USA 2012, 109, 17537–17542. [Google Scholar] [CrossRef] [Green Version]
- David, S.C.; Norton, T.; Tyllis, T.; Wilson, J.J.; Singleton, E.V.; Laan, Z.; Davies, J.; Hirst, T.R.; Comerford, I.; McColl, S.R.; et al. Direct interaction of whole-inactivated influenza A and pneumococcal vaccines enhances influenza-specific immunity. Nat. Microbiol. 2019, 4, 1316–1327. [Google Scholar] [CrossRef]
- Sander, L.E.; Davis, M.J.; Boekschoten, M.V.; Amsen, D.; Dascher, C.C.; Ryffel, B.; Swanson, J.A.; Müller, M.; Blander, J.M. Detection of prokaryotic mRNA signifies microbial viability and promotes immunity. Nat. Cell Biol. 2011, 474, 385–389. [Google Scholar] [CrossRef]
- Ross, P.J.; Sutton, C.E.; Higgins, S.; Allen, A.C.; Walsh, K.; Misiak, A.; Lavelle, E.C.; McLoughlin, R.M.; Mills, K.H. Relative Contribution of Th1 and Th17 Cells in Adaptive Immunity to Bordetella pertussis: Towards the Rational Design of an Improved Acellular Pertussis Vaccine. PLoS Pathog. 2013, 9, e1003264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Higgs, R.; Higgins, S.C.; Ross, P.J.; Mills, K.H.G. Immunity to the respiratory pathogen Bordetella pertussis. Mucosal Immunol. 2012, 5, 485–500. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsuji, S.; Matsumoto, M.; Takeuchi, O.; Akira, S.; Azuma, I.; Hayashi, A.; Toyoshima, K.; Seya, T. Maturation of Human Dendritic Cells by Cell Wall Skeleton of Mycobacterium bovis Bacillus Calmette-Guérin: Involvement of Toll-Like Receptors. Infect. Immun. 2000, 68, 6883–6890. [Google Scholar] [CrossRef] [Green Version]
- Desbien, A.L.; Cauwelaert, N.D.; Reed, S.J.; Bailor, H.R.; Liang, H.; Carter, D.; Duthie, M.S.; Fox, C.B.; Orr, M.T.; Reed, S.G. IL-18 and Subcapsular Lymph Node Macrophages are Essential for Enhanced B Cell Responses with TLR4 Agonist Adjuvants. J. Immunol. 2016, 197, 4351–4359. [Google Scholar] [CrossRef] [Green Version]
- Beug, H.; Von Kirchbach, A.; Döderlein, G.; Conscience, J.-F.; Graf, T. Chicken hematopoietic cells transformed by seven strains of defective avian leukemia viruses display three distinct phenotypes of differentiation. Cell 1979, 18, 375–390. [Google Scholar] [CrossRef]
- Leutz, A.; Beug, H.; Graf, T. Purification and characterization of cMGF, a novel chicken myelomonocytic growth factor. EMBO J. 1984, 3, 3191–3197. [Google Scholar] [CrossRef]
- Iqbal, M.; Philbin, V.J.; Smith, A.L. Expression patterns of chicken Toll-like receptor mRNA in tissues, immune cell subsets and cell lines. Vet. Immunol. Immunopathol. 2005, 104, 117–127. [Google Scholar] [CrossRef]
- Peng, L.; Matthijs, M.G.; Haagsman, H.P.; Veldhuizen, E.J. Avian pathogenic Escherichia coli-induced activation of chicken macrophage HD11 cells. Dev. Comp. Immunol. 2018, 87, 75–83. [Google Scholar] [CrossRef]
- Wisner, A.L.S.; Potter, A.A.; Köster, W. Effect of the Salmonella Pathogenicity Island 2 Type III Secretion System on Salmonella Survival in Activated Chicken Macrophage-Like HD11 Cells. PLoS ONE 2011, 6, e29787. [Google Scholar] [CrossRef]
- Biggelaar, R.H.G.A.V.D.; Van Eden, W.; Rutten, V.P.M.G.; Jansen, C.A. Nitric Oxide Production and Fc Receptor-Mediated Phagocytosis as Functional Readouts of Macrophage Activity upon Stimulation with Inactivated Poultry Vaccines In Vitro. Vaccines 2020, 8, 332. [Google Scholar] [CrossRef] [PubMed]
- Van Dijk, A.; Van Eldik, M.; Veldhuizen, E.J.A.; Bokhoven, H.L.M.T.-V.; De Zoete, M.R.; Bikker, F.J.; Haagsman, H.P. Immunomodulatory and Anti-Inflammatory Activities of Chicken Cathelicidin-2 Derived Peptides. PLoS ONE 2016, 11, e0147919. [Google Scholar] [CrossRef]
- Setta, A.; Barrow, P.A.; Kaiser, P.; Jones, M.A. Immune dynamics following infection of avian macrophages and epithelial cells with typhoidal and non-typhoidal Salmonella enterica serovars; bacterial invasion and persistence, nitric oxide and oxygen production, differential host gene expression, NF-κB signalling and cell cytotoxicity. Vet. Immunol. Immunopathol. 2012, 146, 212–224. [Google Scholar] [CrossRef] [PubMed]
- Crippen, T.L. The selective inhibition of nitric oxide production in the avian macrophage cell line HD11. Vet. Immunol. Immunopathol. 2006, 109, 127–137. [Google Scholar] [CrossRef] [PubMed]
- He, H.; Genovese, K.J.; Swaggerty, C.L.; Nisbet, D.J.; Kogut, M.H. A Comparative Study on Invasion, Survival, Modulation of Oxidative Burst, and Nitric Oxide Responses of Macrophages (HD11), and Systemic Infection in Chickens by Prevalent Poultry Salmonella Serovars. Foodborne Pathog. Dis. 2012, 9, 1104–1110. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- He, H.; Genovese, K.J.; Kogut, M.H. Modulation of chicken macrophage effector function by TH1/TH2 cytokines. Cytokine 2011, 53, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Duff, G.W.; Atkins, E. The inhibitory effect of polymyxin B on endotoxin-induced endogenous pyrogen production. J. Immunol. Methods 1982, 52, 333–340. [Google Scholar] [CrossRef]
- Ariaans, M.P.; Matthijs, M.G.; Van Haarlem, D.; Van De Haar, P.; Van Eck, J.H.H.; Hensen, E.J.; Vervelde, L. The role of phagocytic cells in enhanced susceptibility of broilers to colibacillosis after Infectious Bronchitis Virus infection. Vet. Immunol. Immunopathol. 2008, 123, 240–250. [Google Scholar] [CrossRef] [Green Version]
- Livak, K.J.; Schmittgen, T.D. Analysis of relative gene expression data using real-time quantitative PCR and the 2−ΔΔCT Method. Methods 2001, 25, 402–408. [Google Scholar] [CrossRef]
- Eldaghayes, I.; Rothwell, L.; Williams, A.; Withers, D.; Balu, S.; Davison, F.; Kaiser, P. Infectious Bursal Disease Virus: Strains That Differ in Virulence Differentially Modulate the Innate Immune Response to Infection in the Chicken Bursa. Viral Immunol. 2006, 19, 83–91. [Google Scholar] [CrossRef] [Green Version]
- Degen, W.G.J.; Van Daal, N.; Van Zuilekom, H.I.; Burnside, J.; Schijns, V.E.J.C. Identification and Molecular Cloning of Functional Chicken IL-12. J. Immunol. 2004, 172, 4371–4380. [Google Scholar] [CrossRef] [PubMed]
- Truong, A.D.; Hoang, C.T.; Hong, Y.; Lee, J.; Lee, K.; Lillehoj, H.S.; Hong, Y.H. Functional analyses of the interaction of chicken interleukin 23 subunit p19 with IL-12 subunit p40 to form the IL-23 complex. Mol. Immunol. 2017, 92, 54–67. [Google Scholar] [CrossRef] [PubMed]
- Mittal, S.K.; Roche, P.A. Suppression of antigen presentation by IL-10. Curr. Opin. Immunol. 2015, 34, 22–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keestra, A.M.; Van Putten, J.P.M. Unique Properties of the Chicken TLR4/MD-2 Complex: Selective Lipopolysaccharide Activation of the MyD88-Dependent Pathway. J. Immunol. 2008, 181, 4354–4362. [Google Scholar] [CrossRef] [Green Version]
- Boucher, C.E.; Theron, C.W.; Jansen, A.C.; Bragg, R.R. Transcriptional profiling of chicken immunity-related genes during infection with Avibacterium paragallinarum. Vet. Immunol. Immunopathol. 2014, 158, 135–142. [Google Scholar] [CrossRef]
- Droual, R.; Bickford, A.A.; Charlton, B.R.; Kuney, D.R. Investigation of Problems Associated with Intramuscular Breast Injection of Oil-Adjuvanted Killed Vaccines in Chickens. Avian Dis. 1990, 34, 473. [Google Scholar] [CrossRef]
- Yamanaka, M.; Okabe, T.; Nakai, M.; Goto, N. Local Pathological Reactions and Immune Response of Chickens to ISA-70 and Other Adjuvants Containing Newcastle Disease Virus Antigen. Avian Dis. 1993, 37, 459. [Google Scholar] [CrossRef]
- Reid, G.G.; Blackall, P.J. Comparison of adjuvants for an inactivated infectious coryza vaccine. Avian Dis. 1987, 31, 59–63. [Google Scholar] [CrossRef]
- Zhang, L.; Li, P.; Liu, R.; Zheng, M.; Sun, Y.; Wu, D.; Hu, Y.; Wen, J.; Zhao, G. The Identification of Loci for Immune Traits in Chickens Using a Genome-Wide Association Study. PLoS ONE 2015, 10, e0117269. [Google Scholar] [CrossRef]
- Canthaboo, C.; Xing, D.; Wei, X.Q.; Corbel, M.J. Investigation of Role of Nitric Oxide in Protection from Bordetella pertussis Respiratory Challenge. Infect. Immun. 2002, 70, 679–684. [Google Scholar] [CrossRef] [Green Version]
- Pinge-Filho, P.; Peron, J.; De Moura, T.; Menolli, R.A.; Graça, V.; Estévâo, D.; Tadokoro, C.E.; Jankevicius, J.; Rizzo, L. Protective immunity against Trypanosoma cruzi provided by oral immunization with Phytomonas serpens: Role of nitric oxide. Immunol. Lett. 2005, 96, 283–290. [Google Scholar] [CrossRef] [PubMed]
- Petruzzi, B.; Dalloul, R.A.; Leroith, T.; Evans, N.P.; Pierson, F.W.; Inzana, T.J. Biofilm formation and avian immune response following experimental acute and chronic avian cholera due to Pasteurella multocida. Vet. Microbiol. 2018, 222, 114–123. [Google Scholar] [CrossRef] [PubMed]
- Doan, T.-D.; Wang, H.-Y.; Ke, G.-M.; Cheng, L.-T. N-terminus of Flagellin Fused to an Antigen Improves Vaccine Efficacy against Pasteurella multocida Infection in Chickens. Vaccines 2020, 8, 283. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Ivanov, I.I.; Spolski, R.; Min, R.; Shenderov, K.; Egawa, T.; Levy, D.E.; Leonard, W.J.; Littman, D.R. IL-6 programs TH-17 cell differentiation by promoting sequential engagement of the IL-21 and IL-23 pathways. Nat. Immunol. 2007, 8, 967–974. [Google Scholar] [CrossRef]
- Boucher, C.E.; Theron, C.W.; Hitzeroth, A.C.; Bragg, R.R. Regulation of chicken immunity-related genes and host response profiles against Avibacterium paragallinarum pathogen challenge. Vet. Immunol. Immunopathol. 2015, 167, 70–74. [Google Scholar] [CrossRef]
- Medzhitov, R.; Janeway, C.A. Innate immunity: Impact on the adaptive immune response. Curr. Opin. Immunol. 1997, 9, 4–9. [Google Scholar] [CrossRef]
- Iwasaki, A.; Medzhitov, R. Toll-like receptor control of the adaptive immune responses. Nat. Immunol. 2004, 5, 987–995. [Google Scholar] [CrossRef]
- Manicassamy, S.; Pulendran, B. Modulation of adaptive immunity with Toll-like receptors. Semin. Immunol. 2009, 21, 185–193. [Google Scholar] [CrossRef] [Green Version]
- Dalod, M.; Chelbi, R.; Malissen, B.; Lawrence, T. Dendritic cell maturation: Functional specialization through signaling specificity and transcriptional programming. EMBO J. 2014, 33, 1104–1116. [Google Scholar] [CrossRef]

| Gene | NCBI Reference | Type | Sequences (5′-3′) |
|---|---|---|---|
| iNOS | NM_204961.1 | Forward | TGGGTGGAAGCCGAAATA |
| Reverse | GTACCAGCCGTTGAAAGGAC | ||
| TNF | MF000729.1 | Forward | CGCTCAGAACGACGTCAA |
| Reverse | GTCGTCCACACCAACGAG | ||
| CXCLi1 | NM_205018.1 | Forward | CCAGTGCATAGAGACTCATTCCAAA |
| Reverse | TGCCATCTTTCAGAGTAGCTATGACT | ||
| GAPDH | NM_204305.1 | Forward | GTGGTGCTAAGCGTGTTATC |
| Reverse | GCATGGACAGTGGTCATAAG | ||
| IL-1β | NM_204524.1 | Forward | GCTCTACATGTCGTGTGTGATGAG |
| Reverse | TGTCGATGTCCCGCATGA | ||
| Probe | CCACACTGCAGCTGGAGGAAGCC | ||
| IL-4 | NM_001007079.1 | Forward | AACATGCGTCAGCTCCTGAAT |
| Reverse | TCTGCTAGGAACTTCTCCATTGAA | ||
| Probe | AGCAGCACCTCCCTCAAGGCACC | ||
| IL-6 | NM_204628.1 | Forward | GCTCGCCGGCTTCGA |
| Reverse | GGTAGGTCTGAAAGGCGAACAG | ||
| Probe | AGGAGAAATGCCTGACGAAGCTCTCCA | ||
| CXCLi2 | NM_205498.1 | Forward | GCCCTCCTCCTGGTTTCA |
| Reverse | TGGCACCGCAGCTCATT | ||
| Probe | TCTTTACCAGCGTCCTACCTTGCGACA | ||
| IL-10 | NM_001004414.2 | Forward | CATGCTGCTGGGCCTGAA |
| Reverse | CGTCTCCTTGATCTGCTTGATG | ||
| Probe | CGACGATGCGGCGCTGTCA | ||
| IL-12p35 | NM_213588.1 | Forward | TGGCCGCTGCAAACG |
| Reverse | ACCTCTTCAAGGGTGCACTCA | ||
| Probe | CCAGCGTCCTCTGCTTCTGCACCTT | ||
| IL-12p40 | NM_213571.1 | Forward | TGGGCAAATGATACGGTCAA |
| Reverse | CTGAAAAGCTATAAAGAGCCAAGCAAGACGTTCT | ||
| Probe | CAGAGTAGTTCTTTGCCTCACATTTT | ||
| IFN-α | XM_015277440.2 | Forward | GACAGCCAACGCCAAAGC |
| Reverse | GTCGCTGCTGTCCAAGCATT | ||
| Probe | CTCAACCGGATCCACCGCTACACC | ||
| IFN-γ | NM_205149.1 | Forward | GTGAAGAAGGTGAAAGATATCATGGA |
| Reverse | GCTTTGCGCTGGATTCTCA | ||
| Probe | TGGCCAAGCTCCCGATGAACGA | ||
| 28S | XR_003078040.1 | Forward | GGCGAAGCCAGAGGAAACT |
| Reverse | GACGACCGATTTGCACGTC | ||
| Probe | AGGACCGCTACGGACCTCCACCA |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
van den Biggelaar, R.H.G.A.; van Eden, W.; Rutten, V.P.M.G.; Jansen, C.A. Macrophage Activation Assays to Evaluate the Immunostimulatory Capacity of Avibacterium paragallinarum in A Multivalent Poultry Vaccine. Vaccines 2020, 8, 671. https://doi.org/10.3390/vaccines8040671
van den Biggelaar RHGA, van Eden W, Rutten VPMG, Jansen CA. Macrophage Activation Assays to Evaluate the Immunostimulatory Capacity of Avibacterium paragallinarum in A Multivalent Poultry Vaccine. Vaccines. 2020; 8(4):671. https://doi.org/10.3390/vaccines8040671
Chicago/Turabian Stylevan den Biggelaar, Robin H. G. A., Willem van Eden, Victor P. M. G. Rutten, and Christine A. Jansen. 2020. "Macrophage Activation Assays to Evaluate the Immunostimulatory Capacity of Avibacterium paragallinarum in A Multivalent Poultry Vaccine" Vaccines 8, no. 4: 671. https://doi.org/10.3390/vaccines8040671
APA Stylevan den Biggelaar, R. H. G. A., van Eden, W., Rutten, V. P. M. G., & Jansen, C. A. (2020). Macrophage Activation Assays to Evaluate the Immunostimulatory Capacity of Avibacterium paragallinarum in A Multivalent Poultry Vaccine. Vaccines, 8(4), 671. https://doi.org/10.3390/vaccines8040671