Development of Therapeutic Vaccines for Ovarian Cancer
Abstract
1. Introduction
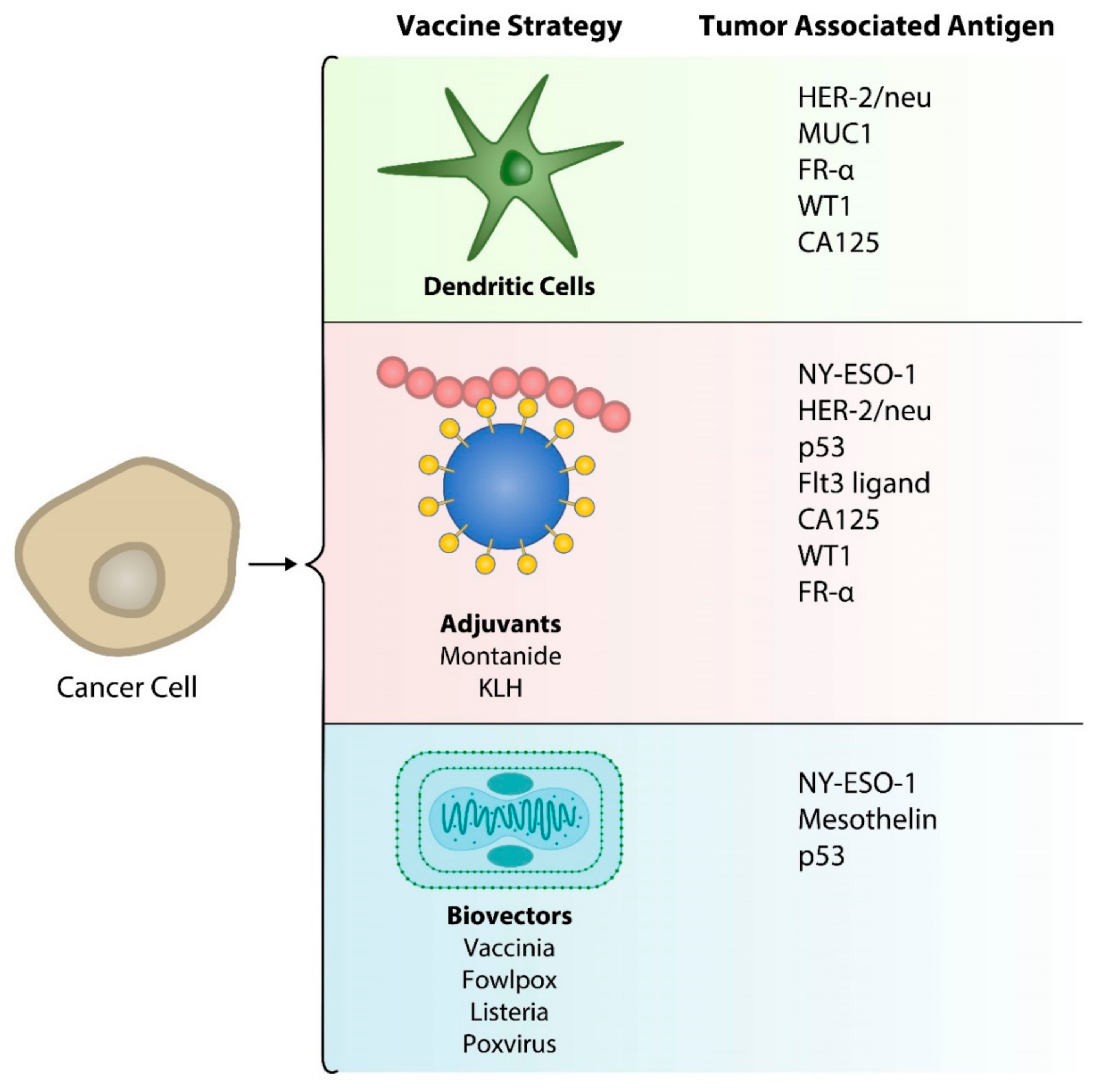
2. Cancer Vaccines
3. Vaccines in Ovarian Cancer
3.1. Dendritic Cell Vaccines
3.2. CTA Vaccines
3.3. Protein/Peptide-Based Vaccines
3.4. Recombinant Viral Vaccines
4. Conclusions and Future Perspectives
Author Contributions
Funding
Conflicts of Interest
References
- Henley, S.J.; Ward, E.M.; Scott, S.; Ma, J.; Anderson, R.N.; Firth, A.U.; Thomas, C.C.; Islami, F.; Weir, H.K.; Lewis, D.R.; et al. Annual report to the nation on the status of cancer, part I: National cancer statistics. Cancer 2020, 126, 2225–2249. [Google Scholar] [CrossRef]
- Ferlay, J.; Colombet, M.; Soerjomataram, I.; Mathers, C.; Parkin, D.M.; Pineros, M.; Znaor, A.; Bray, F. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int. J. Cancer 2019, 144, 1941–1953. [Google Scholar] [CrossRef] [PubMed]
- Lheureux, S.; Gourley, C.; Vergote, I.; Oza, A.M. Epithelial ovarian cancer. Lancet 2019, 393, 1240–1253. [Google Scholar] [CrossRef]
- Schaar, B.; Krishnan, V.; Tallapragada, S.; Chanana, A.; Dorigo, O. Cell-based immunotherapy in gynecologic malignancies. Curr. Opin. Obstet. Gynecol. 2019, 31, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.S.; Mellman, I. Elements of cancer immunity and the cancer-immune set point. Nature 2017, 541, 321–330. [Google Scholar] [CrossRef]
- Hwang, W.T.; Adams, S.F.; Tahirovic, E.; Hagemann, I.S.; Coukos, G. Prognostic significance of tumor-infiltrating T cells in ovarian cancer: A meta-analysis. Gynecol. Oncol. 2012, 124, 192–198. [Google Scholar] [CrossRef]
- Sato, E.; Olson, S.H.; Ahn, J.; Bundy, B.; Nishikawa, H.; Qian, F.; Jungbluth, A.A.; Frosina, D.; Gnjatic, S.; Ambrosone, C.; et al. Intraepithelial CD8+ tumor-infiltrating lymphocytes and a high CD8+/regulatory T cell ratio are associated with favorable prognosis in ovarian cancer. Proc. Natl. Acad. Sci. USA 2005, 102, 18538–18543. [Google Scholar] [CrossRef]
- Zhang, L.; Conejo-Garcia, J.R.; Katsaros, D.; Gimotty, P.A.; Massobrio, M.; Regnani, G.; Makrigiannakis, A.; Gray, H.; Schlienger, K.; Liebman, M.N.; et al. Intratumoral T cells, recurrence, and survival in epithelial ovarian cancer. N. Engl. J. Med. 2003, 348, 203–213. [Google Scholar] [CrossRef]
- Nishikawa, H.; Jager, E.; Ritter, G.; Old, L.J.; Gnjatic, S. CD4+ CD25+ regulatory T cells control the induction of antigen-specific CD4+ helper T cell responses in cancer patients. Blood 2005, 106, 1008–1011. [Google Scholar] [CrossRef]
- Qian, F.; Liao, J.; Villella, J.; Edwards, R.; Kalinski, P.; Lele, S.; Shrikant, P.; Odunsi, K. Effects of 1-methyltryptophan stereoisomers on IDO2 enzyme activity and IDO2-mediated arrest of human T cell proliferation. Cancer Immunol. Immunother. 2012, 61, 2013–2020. [Google Scholar] [CrossRef]
- Qian, F.; Villella, J.; Wallace, P.K.; Mhawech-Fauceglia, P.; Tario, J.D., Jr.; Andrews, C.; Matsuzaki, J.; Valmori, D.; Ayyoub, M.; Frederick, P.J.; et al. Efficacy of levo-1-methyl tryptophan and dextro-1-methyl tryptophan in reversing indoleamine-2,3-dioxygenase-mediated arrest of T-cell proliferation in human epithelial ovarian cancer. Cancer Res. 2009, 69, 5498–5504. [Google Scholar] [CrossRef]
- Huang, R.Y.; Francois, A.; McGray, A.R.; Miliotto, A.; Odunsi, K. Compensatory upregulation of PD-1, LAG-3, and CTLA-4 limits the efficacy of single-agent checkpoint blockade in metastatic ovarian cancer. Oncoimmunology 2017, 6, e1249561. [Google Scholar] [CrossRef]
- Matsuzaki, J.; Gnjatic, S.; Mhawech-Fauceglia, P.; Beck, A.; Miller, A.; Tsuji, T.; Eppolito, C.; Qian, F.; Lele, S.; Shrikant, P.; et al. Tumor-infiltrating NY-ESO-1-specific CD8+ T cells are negatively regulated by LAG-3 and PD-1 in human ovarian cancer. Proc. Natl. Acad. Sci. USA 2010, 107, 7875–7880. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.N.; Kolomeyevskaya, N.; Singel, K.L.; Grimm, M.J.; Moysich, K.B.; Daudi, S.; Grzankowski, K.S.; Lele, S.; Ylagan, L.; Webster, G.A.; et al. Targeting myeloid cells in the tumor microenvironment enhances vaccine efficacy in murine epithelial ovarian cancer. Oncotarget 2015, 6, 11310–11326. [Google Scholar] [CrossRef]
- Sunde, J.S.; Donninger, H.; Wu, K.; Johnson, M.E.; Pestell, R.G.; Rose, G.S.; Mok, S.C.; Brady, J.; Bonome, T.; Birrer, M.J. Expression profiling identifies altered expression of genes that contribute to the inhibition of transforming growth factor-beta signaling in ovarian cancer. Cancer Res. 2006, 66, 8404–8412. [Google Scholar] [CrossRef]
- Zhang, A.W.; McPherson, A.; Milne, K.; Kroeger, D.R.; Hamilton, P.T.; Miranda, A.; Funnell, T.; Little, N.; de Souza, C.P.E.; Laan, S.; et al. Interfaces of Malignant and Immunologic Clonal Dynamics in Ovarian Cancer. Cell 2018, 173, 1755–1769 e1722. [Google Scholar] [CrossRef]
- McCarthy, E.F. The toxins of William, B. Coley and the treatment of bone and soft-tissue sarcomas. Iowa Orthop. J. 2006, 26, 154–158. [Google Scholar]
- Black, M.M.; Opler, S.R.; Speer, F.D. Microscopic structure of gastric carcinomas and their regional lymph nodes in relation to survival. Surg Gynecol. Obstet. 1954, 98, 725–734. [Google Scholar]
- Burnet, M. Cancer: A biological approach. III. Viruses associated with neoplastic conditions. IV. Practical applications. Br. Med. J. 1957, 1, 841–847. [Google Scholar] [CrossRef]
- Odunsi, K. Immunotherapy in ovarian cancer. Ann. Oncol. 2017, 28, viii1–viii7. [Google Scholar] [CrossRef]
- Brossart, P.; Wirths, S.; Stuhler, G.; Reichardt, V.L.; Kanz, L.; Brugger, W. Induction of cytotoxic T-lymphocyte responses in vivo after vaccinations with peptide-pulsed dendritic cells. Blood 2000, 96, 3102–3108. [Google Scholar] [CrossRef] [PubMed]
- Loveland, B.E.; Zhao, A.; White, S.; Gan, H.; Hamilton, K.; Xing, P.X.; Pietersz, G.A.; Apostolopoulos, V.; Vaughan, H.; Karanikas, V.; et al. Mannan-MUC1-pulsed dendritic cell immunotherapy: A phase I trial in patients with adenocarcinoma. Clin. Cancer Res. 2006, 12, 869–877. [Google Scholar] [CrossRef]
- Hernando, J.J.; Park, T.W.; Fischer, H.P.; Zivanovic, O.; Braun, M.; Polcher, M.; Grunn, U.; Leutner, C.; Potzsch, B.; Kuhn, W. Vaccination with dendritic cells transfected with mRNA-encoded folate-receptor-alpha for relapsed metastatic ovarian cancer. Lancet Oncol. 2007, 8, 451–454. [Google Scholar] [CrossRef]
- Peethambaram, P.P.; Melisko, M.E.; Rinn, K.J.; Alberts, S.R.; Provost, N.M.; Jones, L.A.; Sims, R.B.; Lin, L.R.; Frohlich, M.W.; Park, J.W. A phase I trial of immunotherapy with lapuleucel-T (APC8024) in patients with refractory metastatic tumors that express HER-2/neu. Clin. Cancer Res. 2009, 15, 5937–5944. [Google Scholar] [CrossRef]
- Chu, C.S.; Boyer, J.; Schullery, D.S.; Gimotty, P.A.; Gamerman, V.; Bender, J.; Levine, B.L.; Coukos, G.; Rubin, S.C.; Morgan, M.A.; et al. Phase I/II randomized trial of dendritic cell vaccination with or without cyclophosphamide for consolidation therapy of advanced ovarian cancer in first or second remission. Cancer Immunol. Immunother. 2012, 61, 629–641. [Google Scholar] [CrossRef]
- Coosemans, A.; Vanderstraeten, A.; Tuyaerts, S.; Verschuere, T.; Moerman, P.; Berneman, Z.; Vergote, I.; Amant, F.; Van Gool, S.W. Immunological response after WT1 mRNA-loaded dendritic cell immunotherapy in ovarian carcinoma and carcinosarcoma. Anticancer Res. 2013, 33, 3855–3859. [Google Scholar]
- Kobayashi, M.; Chiba, A.; Izawa, H.; Yanagida, E.; Okamoto, M.; Shimodaira, S.; Yonemitsu, Y.; Shibamoto, Y.; Suzuki, N.; Nagaya, M.; et al. The feasibility and clinical effects of dendritic cell-based immunotherapy targeting synthesized peptides for recurrent ovarian cancer. J. Ovarian Res. 2014, 7, 48. [Google Scholar] [CrossRef]
- Gray, H.J.; Benigno, B.; Berek, J.; Chang, J.; Mason, J.; Mileshkin, L.; Mitchell, P.; Moradi, M.; Recio, F.O.; Michener, C.M.; et al. Progression-free and overall survival in ovarian cancer patients treated with CVac, a mucin 1 dendritic cell therapy in a randomized phase 2 trial. J. Immunother. Cancer 2016, 4, 34. [Google Scholar] [CrossRef]
- Morisaki, T.; Hikichi, T.; Onishi, H.; Morisaki, T.; Kubo, M.; Hirano, T.; Yoshimura, S.; Kiyotani, K.; Nakamura, Y. Intranodal Administration of Neoantigen Peptide-loaded Dendritic Cell Vaccine Elicits Epitope-specific T Cell Responses and Clinical Effects in a Patient with Chemorefractory Ovarian Cancer with Malignant Ascites. Immunol. Invest. 2020, 1–18. [Google Scholar] [CrossRef]
- Hernando, J.J.; Park, T.W.; Kubler, K.; Offergeld, R.; Schlebusch, H.; Bauknecht, T. Vaccination with autologous tumour antigen-pulsed dendritic cells in advanced gynaecological malignancies: Clinical and immunological evaluation of a phase I trial. Cancer Immunol. Immunother. 2002, 51, 45–52. [Google Scholar] [CrossRef]
- Kandalaft, L.E.; Powell, D.J., Jr.; Chiang, C.L.; Tanyi, J.; Kim, S.; Bosch, M.; Montone, K.; Mick, R.; Levine, B.L.; Torigian, D.A.; et al. Autologous lysate-pulsed dendritic cell vaccination followed by adoptive transfer of vaccine-primed ex vivo co-stimulated T cells in recurrent ovarian cancer. Oncoimmunology 2013, 2, e22664. [Google Scholar] [CrossRef] [PubMed]
- Chiang, C.L.; Kandalaft, L.E.; Tanyi, J.; Hagemann, A.R.; Motz, G.T.; Svoronos, N.; Montone, K.; Mantia-Smaldone, G.M.; Smith, L.; Nisenbaum, H.L.; et al. A dendritic cell vaccine pulsed with autologous hypochlorous acid-oxidized ovarian cancer lysate primes effective broad antitumor immunity: From bench to bedside. Clin. Cancer Res. 2013, 19, 4801–4815. [Google Scholar] [CrossRef]
- Bapsy, P.P.; Sharan, B.; Kumar, C.; Das, R.P.; Rangarajan, B.; Jain, M.; Suresh Attili, V.S.; Subramanian, S.; Aggarwal, S.; Srivastava, M.; et al. Open-label, multi-center, non-randomized, single-arm study to evaluate the safety and efficacy of dendritic cell immunotherapy in patients with refractory solid malignancies, on supportive care. Cytotherapy 2014, 16, 234–244. [Google Scholar] [CrossRef]
- Tanyi, J.L.; Bobisse, S.; Ophir, E.; Tuyaerts, S.; Roberti, A.; Genolet, R.; Baumgartner, P.; Stevenson, B.J.; Iseli, C.; Dangaj, D.; et al. Personalized cancer vaccine effectively mobilizes antitumor T cell immunity in ovarian cancer. Sci. Transl. Med. 2018, 10, 436. [Google Scholar] [CrossRef]
- Odunsi, K.; Qian, F.; Matsuzaki, J.; Mhawech-Fauceglia, P.; Andrews, C.; Hoffman, E.W.; Pan, L.; Ritter, G.; Villella, J.; Thomas, B.; et al. Vaccination with an NY-ESO-1 peptide of HLA class I/II specificities induces integrated humoral and T cell responses in ovarian cancer. Proc. Natl. Acad. Sci. USA 2007, 104, 12837–12842. [Google Scholar] [CrossRef]
- Diefenbach, C.S.; Gnjatic, S.; Sabbatini, P.; Aghajanian, C.; Hensley, M.L.; Spriggs, D.R.; Iasonos, A.; Lee, H.; Dupont, B.; Pezzulli, S.; et al. Safety and immunogenicity study of NY-ESO-1b peptide and montanide ISA-51 vaccination of patients with epithelial ovarian cancer in high-risk first remission. Clin. Cancer Res. 2008, 14, 2740–2748. [Google Scholar] [CrossRef]
- Sabbatini, P.; Tsuji, T.; Ferran, L.; Ritter, E.; Sedrak, C.; Tuballes, K.; Jungbluth, A.A.; Ritter, G.; Aghajanian, C.; Bell-McGuinn, K.; et al. Phase I trial of overlapping long peptides from a tumor self-antigen and poly-ICLC shows rapid induction of integrated immune response in ovarian cancer patients. Clin. Cancer Res. 2012, 18, 6497–6508. [Google Scholar] [CrossRef]
- Odunsi, K.; Matsuzaki, J.; James, S.R.; Mhawech-Fauceglia, P.; Tsuji, T.; Miller, A.; Zhang, W.; Akers, S.N.; Griffiths, E.A.; Miliotto, A.; et al. Epigenetic potentiation of NY-ESO-1 vaccine therapy in human ovarian cancer. Cancer Immunol. Res. 2014, 2, 37–49. [Google Scholar] [CrossRef]
- Knutson, K.L.; Schiffman, K.; Cheever, M.A.; Disis, M.L. Immunization of cancer patients with a HER-2/neu, HLA-A2 peptide, p369-377, results in short-lived peptide-specific immunity. Clin. Cancer Res. 2002, 8, 1014–1018. [Google Scholar]
- Leffers, N.; Lambeck, A.J.; Gooden, M.J.; Hoogeboom, B.N.; Wolf, R.; Hamming, I.E.; Hepkema, B.G.; Willemse, P.H.; Molmans, B.H.; Hollema, H.; et al. Immunization with a P53 synthetic long peptide vaccine induces P53-specific immune responses in ovarian cancer patients, a phase II trial. Int. J. Cancer 2009, 125, 2104–2113. [Google Scholar] [CrossRef]
- Leffers, N.; Vermeij, R.; Hoogeboom, B.N.; Schulze, U.R.; Wolf, R.; Hamming, I.E.; van der Zee, A.G.; Melief, K.J.; van der Burg, S.H.; Daemen, T.; et al. Long-term clinical and immunological effects of p53-SLP(R) vaccine in patients with ovarian cancer. Int. J. Cancer 2012, 130, 105–112. [Google Scholar] [CrossRef]
- Vermeij, R.; Leffers, N.; Hoogeboom, B.N.; Hamming, I.L.; Wolf, R.; Reyners, A.K.; Molmans, B.H.; Hollema, H.; Bart, J.; Drijfhout, J.W.; et al. Potentiation of a p53-SLP vaccine by cyclophosphamide in ovarian cancer: A single-arm phase II study. Int. J. Cancer 2012, 131, E670–E680. [Google Scholar] [CrossRef]
- Rahma, O.E.; Ashtar, E.; Czystowska, M.; Szajnik, M.E.; Wieckowski, E.; Bernstein, S.; Herrin, V.E.; Shams, M.A.; Steinberg, S.M.; Merino, M.; et al. A gynecologic oncology group phase II trial of two p53 peptide vaccine approaches: Subcutaneous injection and intravenous pulsed dendritic cells in high recurrence risk ovarian cancer patients. Cancer Immunol. Immunother. 2012, 61, 373–384. [Google Scholar] [CrossRef] [PubMed]
- Freedman, R.S.; Vadhan-Raj, S.; Butts, C.; Savary, C.; Melichar, B.; Verschraegen, C.; Kavanagh, J.J.; Hicks, M.E.; Levy, L.B.; Folloder, J.K.; et al. Pilot study of Flt3 ligand comparing intraperitoneal with subcutaneous routes on hematologic and immunologic responses in patients with peritoneal carcinomatosis and mesotheliomas. Clin. Cancer Res. 2003, 9, 5228–5237. [Google Scholar]
- Reinartz, S.; Kohler, S.; Schlebusch, H.; Krista, K.; Giffels, P.; Renke, K.; Huober, J.; Mobus, V.; Kreienberg, R.; DuBois, A.; et al. Vaccination of patients with advanced ovarian carcinoma with the anti-idiotype ACA125: Immunological response and survival (phase Ib/II). Clin. Cancer Res. 2004, 10, 1580–1587. [Google Scholar] [CrossRef]
- Tsuda, N.; Mochizuki, K.; Harada, M.; Sukehiro, A.; Kawano, K.; Yamada, A.; Ushijima, K.; Sugiyama, T.; Nishida, T.; Yamana, H.; et al. Vaccination with predesignated or evidence-based peptides for patients with recurrent gynecologic cancers. J. Immunother. 2004, 27, 60–72. [Google Scholar] [CrossRef]
- Chianese-Bullock, K.A.; Irvin, W.P., Jr.; Petroni, G.R.; Murphy, C.; Smolkin, M.; Olson, W.C.; Coleman, E.; Boerner, S.A.; Nail, C.J.; Neese, P.Y.; et al. A multipeptide vaccine is safe and elicits T-cell responses in participants with advanced stage ovarian cancer. J. Immunother. 2008, 31, 420–430. [Google Scholar] [CrossRef]
- Ohno, S.; Kyo, S.; Myojo, S.; Dohi, S.; Ishizaki, J.; Miyamoto, K.; Morita, S.; Sakamoto, J.; Enomoto, T.; Kimura, T.; et al. Wilms’ tumor 1 (WT1) peptide immunotherapy for gynecological malignancy. Anticancer Res. 2009, 29, 4779–4784. [Google Scholar]
- Miyatake, T.; Ueda, Y.; Morimoto, A.; Enomoto, T.; Nishida, S.; Shirakata, T.; Oka, Y.; Tsuboi, A.; Oji, Y.; Hosen, N.; et al. WT1 peptide immunotherapy for gynecologic malignancies resistant to conventional therapies: A phase II trial. J. Cancer Res. Clin. Oncol. 2013, 139, 457–463. [Google Scholar] [CrossRef]
- Morse, M.A.; Secord, A.A.; Blackwell, K.; Hobeika, A.C.; Sinnathamby, G.; Osada, T.; Hafner, J.; Philip, M.; Clay, T.M.; Lyerly, H.K.; et al. MHC class I-presented tumor antigens identified in ovarian cancer by immunoproteomic analysis are targets for T-cell responses against breast and ovarian cancer. Clin. Cancer Res. 2011, 17, 3408–3419. [Google Scholar] [CrossRef]
- Kawano, K.; Tsuda, N.; Matsueda, S.; Sasada, T.; Watanabe, N.; Ushijima, K.; Yamaguchi, T.; Yokomine, M.; Itoh, K.; Yamada, A.; et al. Feasibility study of personalized peptide vaccination for recurrent ovarian cancer patients. Immunopharmacol. Immunotoxicol. 2014, 36, 224–236. [Google Scholar] [CrossRef]
- Kalli, K.R.; Block, M.S.; Kasi, P.M.; Erskine, C.L.; Hobday, T.J.; Dietz, A.; Padley, D.; Gustafson, M.P.; Shreeder, B.; Puglisi-Knutson, D.; et al. Folate Receptor Alpha Peptide Vaccine Generates Immunity in Breast and Ovarian Cancer Patients. Clin. Cancer Res. 2018, 24, 3014–3025. [Google Scholar] [CrossRef] [PubMed]
- O’Cearbhaill, R.E.; Deng, W.; Chen, L.M.; Lucci, J.A., 3rd; Behbakht, K.; Spirtos, N.M.; Muller, C.Y.; Benigno, B.B.; Powell, M.A.; Berry, E.; et al. A phase II randomized, double-blind trial of a polyvalent Vaccine-KLH conjugate (NSC 748933 IND# 14384) + OPT-821 versus OPT-821 in patients with epithelial ovarian, fallopian tube, or peritoneal cancer who are in second or third complete remission: An NRG Oncology/GOG study. Gynecol. Oncol. 2019, 155, 393–399. [Google Scholar] [CrossRef]
- Jager, E.; Karbach, J.; Gnjatic, S.; Neumann, A.; Bender, A.; Valmori, D.; Ayyoub, M.; Ritter, E.; Ritter, G.; Jager, D.; et al. Recombinant vaccinia/fowlpox NY-ESO-1 vaccines induce both humoral and cellular NY-ESO-1-specific immune responses in cancer patients. Proc. Natl. Acad. Sci. USA 2006, 103, 14453–14458. [Google Scholar] [CrossRef] [PubMed]
- Gulley, J.L.; Arlen, P.M.; Tsang, K.Y.; Yokokawa, J.; Palena, C.; Poole, D.J.; Remondo, C.; Cereda, V.; Jones, J.L.; Pazdur, M.P.; et al. Pilot study of vaccination with recombinant CEA-MUC-1-TRICOM poxviral-based vaccines in patients with metastatic carcinoma. Clin. Cancer Res. 2008, 14, 3060–3069. [Google Scholar] [CrossRef]
- Mohebtash, M.; Tsang, K.Y.; Madan, R.A.; Huen, N.Y.; Poole, D.J.; Jochems, C.; Jones, J.; Ferrara, T.; Heery, C.R.; Arlen, P.M.; et al. A pilot study of MUC-1/CEA/TRICOM poxviral-based vaccine in patients with metastatic breast and ovarian cancer. Clin. Cancer Res. 2011, 17, 7164–7173. [Google Scholar] [CrossRef]
- Odunsi, K.; Matsuzaki, J.; Karbach, J.; Neumann, A.; Mhawech-Fauceglia, P.; Miller, A.; Beck, A.; Morrison, C.D.; Ritter, G.; Godoy, H.; et al. Efficacy of vaccination with recombinant vaccinia and fowlpox vectors expressing NY-ESO-1 antigen in ovarian cancer and melanoma patients. Proc. Natl. Acad. Sci. USA 2012, 109, 5797–5802. [Google Scholar] [CrossRef]
- Hardwick, N.R.; Frankel, P.; Ruel, C.; Kilpatrick, J.; Tsai, W.; Kos, F.; Kaltcheva, T.; Leong, L.; Morgan, R.; Chung, V.; et al. p53-Reactive T Cells Are Associated with Clinical Benefit in Patients with Platinum-Resistant Epithelial Ovarian Cancer After Treatment with a p53 Vaccine and Gemcitabine Chemotherapy. Clin. Cancer Res. 2018, 24, 1315–1325. [Google Scholar] [CrossRef]
- Senzer, N.; Barve, M.; Kuhn, J.; Melnyk, A.; Beitsch, P.; Lazar, M.; Lifshitz, S.; Magee, M.; Oh, J.; Mill, S.W.; et al. Phase I trial of "bi-shRNAi(furin)/GMCSF DNA/autologous tumor cell" vaccine (FANG) in advanced cancer. Mol. Ther. 2012, 20, 679–686. [Google Scholar] [CrossRef]
- Le, D.T.; Brockstedt, D.G.; Nir-Paz, R.; Hampl, J.; Mathur, S.; Nemunaitis, J.; Sterman, D.H.; Hassan, R.; Lutz, E.; Moyer, B.; et al. A live-attenuated Listeria vaccine (ANZ-100) and a live-attenuated Listeria vaccine expressing mesothelin (CRS-207) for advanced cancers: Phase I studies of safety and immune induction. Clin. Cancer Res. 2012, 18, 858–868. [Google Scholar] [CrossRef] [PubMed]
- Holmberg, L.A.; Oparin, D.V.; Gooley, T.; Sandmaier, B.M. The role of cancer vaccines following autologous stem cell rescue in breast and ovarian cancer patients: Experience with the STn-KLH vaccine (Theratope). Clin. Breast Cancer 2003, 3 (Suppl. S4), S144–S151. [Google Scholar] [CrossRef] [PubMed]
- Sabbatini, P.J.; Kudryashov, V.; Ragupathi, G.; Danishefsky, S.J.; Livingston, P.O.; Bornmann, W.; Spassova, M.; Zatorski, A.; Spriggs, D.; Aghajanian, C.; et al. Immunization of ovarian cancer patients with a synthetic Lewis(y)-protein conjugate vaccine: A phase 1 trial. Int. J. Cancer 2000, 87, 79–85. [Google Scholar] [CrossRef]
- Bates, E.E.; Dieu, M.C.; Ravel, O.; Zurawski, S.M.; Patel, S.; Bridon, J.M.; Ait-Yahia, S.; Vega, F., Jr.; Banchereau, J.; Lebecque, S. CD40L activation of dendritic cells down-regulates DORA, a novel member of the immunoglobulin superfamily. Mol. Immunol. 1998, 35, 513–524. [Google Scholar] [CrossRef]
- Sabado, R.L.; Balan, S.; Bhardwaj, N. Dendritic cell-based immunotherapy. Cell Res. 2017, 27, 74–95. [Google Scholar] [CrossRef]
- Sarivalasis, A.; Boudousquie, C.; Balint, K.; Stevenson, B.J.; Gannon, P.O.; Iancu, E.M.; Rossier, L.; Martin Lluesma, S.; Mathevet, P.; Sempoux, C.; et al. A Phase I/II trial comparing autologous dendritic cell vaccine pulsed either with personalized peptides (PEP-DC) or with tumor lysate (OC-DC) in patients with advanced high-grade ovarian serous carcinoma. J. Transl. Med. 2019, 17, 391. [Google Scholar] [CrossRef]
- Rob, L.; Mallmann, P.; Knapp, P.; Melichar, B.; Klat, J.; Minar, L.; Novotny, Z.; Bartunkova, R.; Spisek, J.; Pecen, L.; et al. Dendritic cell vaccine (DCVAC) with chemotherapy (ct) in patients (pts) with epithelial ovarian carcinoma (EOC) after primary debulking surgery (PDS): Interim analysis of a phase 2, open-label, randomized, multicenter trial. J. Clin. Oncol. 2018, 36, 5509. [Google Scholar] [CrossRef]
- Almeida, L.G.; Sakabe, N.J.; de Oliveira, A.R.; Silva, M.C.; Mundstein, A.S.; Cohen, T.; Chen, Y.T.; Chua, R.; Gurung, S.; Gnjatic, S.; et al. CTdatabase: A knowledge-base of high-throughput and curated data on cancer-testis antigens. Nucleic Acids Res. 2009, 37, D816–D819. [Google Scholar] [CrossRef]
- Odunsi, K.; Jungbluth, A.A.; Stockert, E.; Qian, F.; Gnjatic, S.; Tammela, J.; Intengan, M.; Beck, A.; Keitz, B.; Santiago, D.; et al. NY-ESO-1 and LAGE-1 cancer-testis antigens are potential targets for immunotherapy in epithelial ovarian cancer. Cancer Res. 2003, 63, 6076–6083. [Google Scholar]
- Szender, J.B.; Papanicolau-Sengos, A.; Eng, K.H.; Miliotto, A.J.; Lugade, A.A.; Gnjatic, S.; Matsuzaki, J.; Morrison, C.D.; Odunsi, K. NY-ESO-1 expression predicts an aggressive phenotype of ovarian cancer. Gynecol. Oncol. 2017, 145, 420–425. [Google Scholar] [CrossRef] [PubMed]
- Jager, E.; Stockert, E.; Zidianakis, Z.; Chen, Y.T.; Karbach, J.; Jager, D.; Arand, M.; Ritter, G.; Old, L.J.; Knuth, A. Humoral immune responses of cancer patients against "Cancer-Testis" antigen NY-ESO-1: Correlation with clinical events. Int. J. Cancer 1999, 84, 506–510. [Google Scholar] [CrossRef]
- Woloszynska-Read, A.; Mhawech-Fauceglia, P.; Yu, J.; Odunsi, K.; Karpf, A.R. Intertumor and intratumor NY-ESO-1 expression heterogeneity is associated with promoter-specific and global DNA methylation status in ovarian cancer. Clin. Cancer Res. 2008, 14, 3283–3290. [Google Scholar] [CrossRef]
- Disis, M.L.; Grabstein, K.H.; Sleath, P.R.; Cheever, M.A. Generation of immunity to the HER-2/neu oncogenic protein in patients with breast and ovarian cancer using a peptide-based vaccine. Clin. Cancer Res. 1999, 5, 1289–1297. [Google Scholar]
- Disis, M.L.; Goodell, V.; Schiffman, K.; Knutson, K.L. Humoral epitope-spreading following immunization with a HER-2/neu peptide based vaccine in cancer patients. J. Clin. Immunol. 2004, 24, 571–578. [Google Scholar] [CrossRef]
- Disis, M.L.; Rinn, K.; Knutson, K.L.; Davis, D.; Caron, D.; dela Rosa, C.; Schiffman, K. Flt3 ligand as a vaccine adjuvant in association with HER-2/neu peptide-based vaccines in patients with HER-2/neu-overexpressing cancers. Blood 2002, 99, 2845–2850. [Google Scholar] [CrossRef]
- Bartel, F.; Jung, J.; Bohnke, A.; Gradhand, E.; Zeng, K.; Thomssen, C.; Hauptmann, S. Both germ line and somatic genetics of the p53 pathway affect ovarian cancer incidence and survival. Clin. Cancer Res. 2008, 14, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Nijman, H.W.; Lambeck, A.; van der Burg, S.H.; van der Zee, A.G.; Daemen, T. Immunologic aspect of ovarian cancer and p53 as tumor antigen. J. Transl. Med. 2005, 3, 34. [Google Scholar] [CrossRef]
- Soussi, T. p53 Antibodies in the sera of patients with various types of cancer: A review. Cancer Res. 2000, 60, 1777–1788. [Google Scholar]
- Ghiringhelli, F.; Menard, C.; Puig, P.E.; Ladoire, S.; Roux, S.; Martin, F.; Solary, E.; Le Cesne, A.; Zitvogel, L.; Chauffert, B. Metronomic cyclophosphamide regimen selectively depletes CD4+CD25+ regulatory T cells and restores T and NK effector functions in end stage cancer patients. Cancer Immunol. Immunother. 2007, 56, 641–648. [Google Scholar] [CrossRef]
- Lutsiak, M.E.; Semnani, R.T.; De Pascalis, R.; Kashmiri, S.V.; Schlom, J.; Sabzevari, H. Inhibition of CD4(+)25+ T regulatory cell function implicated in enhanced immune response by low-dose cyclophosphamide. Blood 2005, 105, 2862–2868. [Google Scholar] [CrossRef]
- Curiel, T.J.; Coukos, G.; Zou, L.; Alvarez, X.; Cheng, P.; Mottram, P.; Evdemon-Hogan, M.; Conejo-Garcia, J.R.; Zhang, L.; Burow, M.; et al. Specific recruitment of regulatory T cells in ovarian carcinoma fosters immune privilege and predicts reduced survival. Nat. Med. 2004, 10, 942–949. [Google Scholar] [CrossRef]
- Oka, Y.; Tsuboi, A.; Oji, Y.; Kawase, I.; Sugiyama, H. WT1 peptide vaccine for the treatment of cancer. Curr. Opin. Immunol. 2008, 20, 211–220. [Google Scholar] [CrossRef]
- Cheever, M.A.; Allison, J.P.; Ferris, A.S.; Finn, O.J.; Hastings, B.M.; Hecht, T.T.; Mellman, I.; Prindiville, S.A.; Viner, J.L.; Weiner, L.M.; et al. The prioritization of cancer antigens: A national cancer institute pilot project for the acceleration of translational research. Clin. Cancer Res. 2009, 15, 5323–5337. [Google Scholar] [CrossRef]
- Goldsberry, W.N.; Meza-Perez, S.; Londono, A.I.; Katre, A.A.; Mott, B.T.; Roane, B.M.; Goel, N.; Wall, J.A.; Cooper, S.J.; Norian, L.A.; et al. Inhibiting WNT Ligand Production for Improved Immune Recognition in the Ovarian Tumor Microenvironment. Cancers 2020, 12, 766. [Google Scholar] [CrossRef]
- Haseeb, M.; Pirzada, R.H.; Ain, Q.U.; Choi, S. Wnt Signaling in the Regulation of Immune Cell and Cancer Therapeutics. Cells 2019, 8, 1380. [Google Scholar] [CrossRef]
- Carter, J.H.; Deddens, J.A.; Mueller, G.; Lewis, T.G.; Dooley, M.K.; Robillard, M.C.; Frydl, M.; Duvall, L.; Pemberton, J.O.; Douglass, L.E. Transcription factors WT1 and p53 combined: A prognostic biomarker in ovarian cancer. Br. J. Cancer 2018, 119, 462–470. [Google Scholar] [CrossRef]
- Dochez, V.; Caillon, H.; Vaucel, E.; Dimet, J.; Winer, N.; Ducarme, G. Biomarkers and algorithms for diagnosis of ovarian cancer: CA125, HE4, RMI and ROMA, a review. J. Ovarian Res. 2019, 12, 28. [Google Scholar] [CrossRef] [PubMed]
- Felder, M.; Kapur, A.; Gonzalez-Bosquet, J.; Horibata, S.; Heintz, J.; Albrecht, R.; Fass, L.; Kaur, J.; Hu, K.; Shojaei, H.; et al. MUC16 (CA125): Tumor biomarker to cancer therapy, a work in progress. Mol. Cancer 2014, 13, 129. [Google Scholar] [CrossRef] [PubMed]
- Hodge, J.W.; McLaughlin, J.P.; Kantor, J.A.; Schlom, J. Diversified prime and boost protocols using recombinant vaccinia virus and recombinant non-replicating avian pox virus to enhance T-cell immunity and antitumor responses. Vaccine 1997, 15, 759–768. [Google Scholar] [CrossRef]
- Marshall, J.L.; Gulley, J.L.; Arlen, P.M.; Beetham, P.K.; Tsang, K.Y.; Slack, R.; Hodge, J.W.; Doren, S.; Grosenbach, D.W.; Hwang, J.; et al. Phase I study of sequential vaccinations with fowlpox-CEA(6D)-TRICOM alone and sequentially with vaccinia-CEA(6D)-TRICOM, with and without granulocyte-macrophage colony-stimulating factor, in patients with carcinoembryonic antigen-expressing carcinomas. J. Clin. Oncol. 2005, 23, 720–731. [Google Scholar] [CrossRef]
- He, Z.Y.; Zhang, Y.G.; Yang, Y.H.; Ma, C.C.; Wang, P.; Du, W.; Li, L.; Xiang, R.; Song, X.R.; Zhao, X.; et al. In Vivo Ovarian Cancer Gene Therapy Using CRISPR-Cas9. Hum. Gene Ther. 2018, 29, 223–233. [Google Scholar] [CrossRef]
| Vaccine | Description | Total Patients (OC Patients) | Clinical Outcome * | Reference |
|---|---|---|---|---|
| DCs (peptide-pulsed) | ||||
| HER-2/neu or MUC1-derived peptide | Phase 1/2 study in heavily pretreated metastatic breast and ovarian cancer | 10 (3) | 1 SD over 8 months 1 SD over 8 weeks | Brossart et al., 2000 [21] |
| Mannan-MUC1 | Phase 1 study in MUC1+ adenocarcinoma | 11 (1) | 1 SD | Loveland et al., 2006 [22] |
| mRNA-encoded FR-α | Pilot study in a patient with recurrent ovarian cancer | 1 | 1 PR | Hernando et al., 2007 [23] |
| Lapuleucel-T, pulsed with BA7072, a recombinant fusion protein of HER-2/neu sequences linked to GM-CSF | Phase 1 study in HER-2/neu expressing metastatic breast, ovarian, and colorectal cancer | 18 (4) | 2 SD over 15.7–18.3 months | Peethambaram et al., 2009 [24] |
| HER-2/neu, hTERT, and PADRE | Phase 1/2 study in advanced ovarian cancer after first recurrence, randomized to receive low-dose cyclophosphamide prior to vaccination | 11 | 6 NED at 36 months 3-yr PFS 80% 3-yr OS 100% | Chu et al., 2012 [25] |
| WT1 mRNA-loaded DC | Phase 1 study in epithelial ovarian carcinoma (OC) and ovarian carcinosarcoma (OCS) | 2 | OS 19 (OCS) and 12 (OC) months after drug cessation | Coosemans et al., 2013 [26] |
| Combinations of WT1, MUC1, and CA125 | Retrospective study including patients with recurrent ovarian cancer | 56 | 1-yr OS 87% 2-yr OS 65% 2 PR, 14 SD DCR 29% ORR 3.6% | Kobayashi et al., 2014 [27] |
| CVac, MUC-1 targeted DC | Phase 2b study (CAN-003 trial) in epithelial ovarian cancer as maintenance therapy | 56 | PFS 13 months CVac vs. 9 mo standard of care (HR 0.72, p = 0.33) Median OS 25.5 months with standard therapy vs. not yet reached with CVac (HR 0.17; 95% CI 0.02–1.44; p = 0.07) | Gray et al., 2016 [28] |
| Neoantigen peptides | Pilot study in a patient with advance ovarian cancer | 1 | CA-125 decreased from 4470 to 1303 U/mL. Patient expired approx. 1 year from treatment start | Morisaki et al., 2020 [29] |
| DCs (whole tumor lysate-pulsed) | ||||
| Pulsed with KLH and autologous tumor cell lysate | Phase 1 study in advanced gynecologic malignancies | 8 (6) | PFI 25.5 months | Hernando et al., 2002 [30] |
| Pulsed with autologous tumor cell lysate supernatant | Pilot study in advanced ovarian cancer where patients were treated with metronomic cyclophosphamide and bevacizumab followed by vaccination | 6 | 2 PR 2 SD | Kandalaft et al., 2013 [31] |
| DC pulsed with autologous hypochlorous acid-oxidized ov ca lysate | Pilot study in advanced ovarian cancer | 5 | 2 SD 2 PD 1 mixed response | Chiang et al., 2013 [32] |
| APCEDEN, whole-tumor lysate pulsed DCs | Phase 2 study in refractory solid malignancies | 51 (7) | 1 PR 2 SD | Bapsy et al., 2014 [33] |
| Pulsed with oxidized autologous whole-tumor cell lysate | Pilot study in recurrent ovarian cancer using autologous vaccine with bevacizumab and cyclophosphamide | 25 | 2 PR 14 SD | Tanyi et al., 2018 [34] |
| CTA | ||||
| ESO157–170 | Phase 1 study in NY-ESO-1-expressing ovarian cancers | 18 | PFS 19.0 months | Odunsi et al., 2007 [35] |
| NY-ESO-1b peptide and Montanide ISA-51 | Phase 1 study in “high-risk” ovarian cancer | 9 | PFS 13.0 months | Diefenbach et al., 2008 [36] |
| Synthetic overlapping long peptide from NY-ESO-1, Montanide ISA-51, and Poly-ICLC | Phase 1 study in advanced ovarian cancer in 2nd or 3rd remission | 28 | 6 NED PFS range of 17–46 months | Sabbatini et al., 2012 [37] |
| NY-ESO-1, decitabine, and GM-CSF | Phase 1 study in relapsed ovarian cancer receiving doxorubicin as salvage therapy | 12 | 1 PR 5 SD | Odunsi et al., 2014 [38] |
| Protein/Peptide | ||||
| HER-2/neu and GM-CSF | Phase 1 study in stage III or IV breast or ovarian cancer | 6 (2) | Responses short-lived | Knutson et al., 2002 [39] |
| p53-SLP | Phase 2 study in recurrent epithelial ovarian cancer | 20 | 2 SD | Leffers et al., 2009 [40] |
| p53-SLP | Long term outcomes of 2009 phase 2 study | 20 | RR 60.0% Median DSS 44.0 months | Leffers et al., 2012 [41] |
| p53-SLP with cyclophosphamide | Phase 2 study in recurrent ovarian cancer | 10 | 2 SD | Vermeij et al., 2011 [42] |
| Wildtype p53 vaccine with Montanide and GM-CSF; p53-pulsed DC | Phase 2 study in high recurrence risk ovarian cancer. Two p53 vaccine approaches tested | 13 | Median OS 40.8 and 29.6 months arm A and B, respectively Median PFS 4.2 and 8.7 months, respectively | Rahma et al., 2012 [43] |
| Flt3 ligand | Pilot study in peritoneal carcinomatosis or mesothelioma patients | 15 (9) | No objective responses | Freedman et al., 2003 [44] |
| Anti-idiotypic antibody vaccine (ACA125) | Phase 1/2b study in advanced ovarian cancer | 119 | Median OS 19.4 months (range 0.5–56.1 months) Ab3-positive patients had significantly longer survival time (median 23.4 mo, p < 0.0001) compared with Ab3-negative (median 4.9 mo) | Reinartz et al., 2004 [45] |
| Regimen 1: predesignated SART2 or ART4-derived peptide Regimen 2: peptides to which preexisting CTL precursor | Two regimens with different peptide vaccine regimens in recurrent gynecologic cancers | Regimen 1: 4 (2) Regimen 2: 10 (3) | Regimen 1: 0 response Regimen 2: 1 SD | Tsuda et al., 2004 [46] |
| Multipeptide vaccine with Montanide ISA-51 and GM-CSF | Phase 1 study in HLA-A1+, HLA-A2+, or HLA-A3+ epithelial ovarian, fallopian tube, or primary peritoneal carcinoma | 9 | DFS 19 months in 1 patient | Chianese-Bullock et al., 2008 [47] |
| WT1 peptide + Montanide ISA51 | Phase 1 study in gynecological cancer patients with WT1/HLA-A *2402 positive tumors | 12 (6) | 1 SD | Ohno et al., 2009 [48] |
| WT1 peptide vaccine | Phase 2 study in progressive gynecologic cancers | 40 (24) | 10 SD OS HR 1.17 (95% CI 0.44–3.14; p = 0.75) | Miyatake et al., 2013 [49] |
| Multipeptide vaccine with Montanide ISA-51 and CM-CSF | Phase 1 study in HLA-A2+, stage II to IV epithelial ovaria, tubal, or primary peritoneal carcinoma after 1st or 2nd cytoreductive surgery with a complete clinical response | 15 (8) | Median survival not reached | Morse et al., 2011 [50] |
| Personalized peptide vaccine (based on HLA-A types and IgG responses to peptides in pre-vaccinated plasma) with Montanide ISA-51 | Phase 2 study in recurrent or persistent ovarian, fallopian tube, or primary peritoneal carcinoma | 42 | MST in platinum-sensitive vs. platinum-resistant 39.3 vs. 16.2 months, respectively. MST with monotherapy vs. in combination with chemotherapy in platinum-sensitive (39.3 vs. 32.2 months, respectively) and platinum-resistant (16.8 vs. 16.1 months, respectively) | Kawano et al., 2014 [51] |
| Folate receptor alpha with cyclophosphamide priming | Phase 1 study in stage II-IV ovarian cancer and stage II-III breast cancer without evidence of disease | 22 (14) | All patients alive at last follow-up of at least 2 years Median RFS 528 days in patients in first remission Median OS not reached for those in second remission | Kalli et al., 2018 [52] |
| Polyvalent vaccine-KLH conjugate (including Globo-H-KLH, GM2-KLH, Tn-MUC1-32mer-KLH, TF-KLH) with adjuvant OPT-821 | GOG 255 – Randomized, double-blinded, phase 2 study in any stage ovarian, fallopian tube, or primary peritoneal carcinoma in 2nd or 3rd complete remission. Patients were randomized to polyvalent vaccine-KLH conjugate + OPT-821 or OPT-821 alone (reference arm) | 171 | KLH + OPT-821 was not superior to OPT-821 alone (HR 0.98; 2-sided 95% CI, 0.71–1.36) Median OS for KLH + OPT-821 and OPT-821 were 47 and 46 months, respectively. | O’Cearbhaill et al., 2019 [53] |
| Recombinant Viral | ||||
| Recombinant vaccinia- and fowlpox-NY-ESO-1 | Pilot study in advanced NY-ESO-1-expressing cancers | 35 (1) | DFI 8 months | Jager et al., 2006 [54] |
| PANVAC | Pilot study in CEA- or MUC-1-expressing metastatic cancers | 25 (3) | PFS range 2–19 months OS range 6–21 months | Gulley et al., 2008 [55] |
| PANVAC | Pilot study in metastatic ovarian and breast cancer with progressive disease | 26 (14) | Median PFS 2 months (range 1–6 months) Median OS 15.0 months (range 1.5–57+ months) | Mohebtash, et al., 2011 [56] |
| Recombinant vaccinia- and fowlpox-NY-ESO-1 | Two parallel phase 2 studies in NY-ESO-1-expressing epithelial ovarian cancer and melanoma | 47 (22) | Median PFS 21 months (95% CI, 16–29 months) Median OS 48 months (95% CI, not estimable). | Odunsi et al., 2012 [57] |
| Modified Vaccinian Ankara vaccine delivering wildtype human p53 in combination with gemcitabine | Phase 1 study in platinum-resistant recurrent ovarian, fallopian tube, and primary peritoneal carcinoma | 11 | 1 PR 3 SD Median PFS 3 months (range 0.95–9.2 months) | Hardwick et al., 2018 [58] |
| Whole tumor cell | ||||
| FANG, an autologous tumor-based vaccine containing a plasmid encoding GM-CSF and a novel bifunctional short hairpin RNA targeting furin convertase | Phase 1 study in advanced cancers | 27 (5) | 3 SD | Senzer et al., 2012 [59] |
| Live-attenuated | ||||
| ANZ-100, a live-attenuated Listeria vaccine and CRS-207, the live-attenuated Listeria strain expressing human mesothelin | Dual phase 1 study in treatment-refractory mesothelin-expressing cancers (mesothelioma, lung, pancreatic, ovarian) with hepatic metastases | 9 (2) | No clinical responses | Le et al., 2012 [60] |
| Carbohydrate-based | ||||
| Theratope ® | Phase II/III study in advanced breast and ovarian cancer | 70 (17) | Phase II (40 patients total): 27 patients relapsed (5 ovarian, 22 breast); 23 patients died (5 ovarian, 18 breast) Phase III (30 patients total): 18 patients relapsed (9 ovarian, 9 breast); 10 patients died (5 ovarian, 5 breast) | Holmberg et al., 2003 [61] |
| Lewisy-KLH conjugate with QS-21 adjuvant | Phase I study in recurrent or persistent ovarian, fallopian tube, or primary peritoneal carcinoma following primary therapy and were in complete clinical remission following additional chemotherapy | 25 | Median PFS 6 months 5 patients remained in complete clinical remission at 18 months follow up | Sabbatini et al., 2000 [62] |
| Trial | Vaccine | Clinical Trial Phase | Reference (ClinicalTrials.gov Identifier) |
|---|---|---|---|
| Ovarian Cancer Treatment With a Liposome Formulated mRNA Vaccine in Combination With (Neo-)Adjuvant Chemotherapy (OLIVIA) | W_ova1 vaccine, which includes 3 OC TAA RNAs | Phase 1 | NCT04163094 |
| Ovarian Dendritic Cell Vaccine Trial | DC vaccine made with autologous tumor lysate or for patients who are HLA-A2 with peptides of MUC1 and WT1 therapy | Phase 2 | NCT00703105 |
| Intensive Locoregional Chemoimmunotherapy for Recurrent Ovarian Cancer Plus Intranodal DC Vaccines | DC vaccine | Phase 1/2 | NCT02432378 |
| Study of Oncoimmunome for the Treatment of Stage III/IV Ovarian Carcinoma | OncoImmunome includes a mixture of 7–10 peptides identified based upon tumor-specific mutant peptide sequences from each tumor transcriptome | Phase 1 | NCT02933073 |
| Open Label Immunotherapy Trial for Ovarian Cancer (V3-OVA) | Tableted vaccine (V3-OVA) containing ovarian cancer antigens | Phase 2 | NCT03556566 |
| Phase 2 Study of Pembrolizumab, DPX-Survivac Vaccine and Cyclophosphamide in Advanced Ovarian, Primary Peritoneal or Fallopian Tube Cancer | DPX-Survivac | Phase 2 | NCT03029403 |
| Vaccine Therapy in Treating Patients With Metastatic Solid Tumors | Combination of 2 chimeric (Trastuzumab-like and Pertuzumab-like) HER-2 vaccine | Phase 1 | NCT01376505 |
| T-Cell Infusion, Aldesleukin, and Utomilumab in Treating Patients With Recurrent Ovarian Cancer | Aldesleukin, a recombinant human IL-2 | Phase 1 | NCT03318900 |
| Arginase-1 Peptide Vaccine in Patients With Metastatic Solid Tumors | ARG1–18,19,20, an ARG1 peptide vaccine | Phase 1 | NCT03689192 |
| Phase Ib/IIa Trial to Evaluate Oregovomab and Nivolumab in Epithelial Cancer of Ovarian, Tubal or Peritoneal Origin (ORION-01) | Oregovomab, a murine monoclonal antibody against CA125 | Phase 1/2 | NCT03100006 |
| P53MVA and Pembrolizumab in Treating Patients With Recurrent Ovarian, Primary Peritoneal, or Fallopian Tube Cancer | Modified vaccinia virus ankara vaccine expressing p53 | Phase 2 | NCT03113487 |
| Autologous and Allogeneic Whole Cell Cancer Vaccine for Metastatic Tumors | Autologous or allogeneic tumor cells | Phase 1/2 | NCT00722228 |
| Galinpepimut-S in Combination With Pembrolizumab in Patients With Selected Advanced Cancers | galinpepimut-S, a WT1-targeting multivalent heteroclitic peptide vaccine | Phase 1/2 | NCT03761914 |
| DEC-205/NY-ESO-1 Fusion Protein CDX-1401, Poly ICLC, and IDO1 Inhibitor INCB024360 in Treating Patients With Ovarian, Fallopian Tube, or Primary Peritoneal Cancer in Remission | DEC-205/NY-ESO-1 Fusion Protein CDX-1401 | Phase 1/2 | NCT02166905 |
| A Study of DSP-7888 Dosing Emulsion in Combination With Immune Checkpoint Inhibitors in Adult Patients With Advanced Solid Tumors | DSP-7888, a WT1 protein-derived peptide vaccine | Phase 1/2 | NCT03311334 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chow, S.; Berek, J.S.; Dorigo, O. Development of Therapeutic Vaccines for Ovarian Cancer. Vaccines 2020, 8, 657. https://doi.org/10.3390/vaccines8040657
Chow S, Berek JS, Dorigo O. Development of Therapeutic Vaccines for Ovarian Cancer. Vaccines. 2020; 8(4):657. https://doi.org/10.3390/vaccines8040657
Chicago/Turabian StyleChow, Stephanie, Jonathan S. Berek, and Oliver Dorigo. 2020. "Development of Therapeutic Vaccines for Ovarian Cancer" Vaccines 8, no. 4: 657. https://doi.org/10.3390/vaccines8040657
APA StyleChow, S., Berek, J. S., & Dorigo, O. (2020). Development of Therapeutic Vaccines for Ovarian Cancer. Vaccines, 8(4), 657. https://doi.org/10.3390/vaccines8040657





