Targeted Modification of the Foot-And-Mouth Disease Virus Genome for Quick Cell Culture Adaptation
Abstract
1. Introduction
2. Materials and Methods
2.1. Cells and viruses
2.2. Construction of Recombinant FMDV
2.3. Infectivity Assay
2.4. Growth Curves
2.5. Vaccine Formulation
2.6. Guinea Pig Immunization
2.7. Ethics Statement
2.8. Virus Neutralization (VN) Test
2.9. Temperature and pH Sensitivity
2.10. Statistical Analysis
3. Results
3.1. Generation of Recombinant FMD Viruses with Mutations Observed in Passage-Derived Strains
3.2. Characterization of the Recovered FMDV Mutants and Their Parental Strains
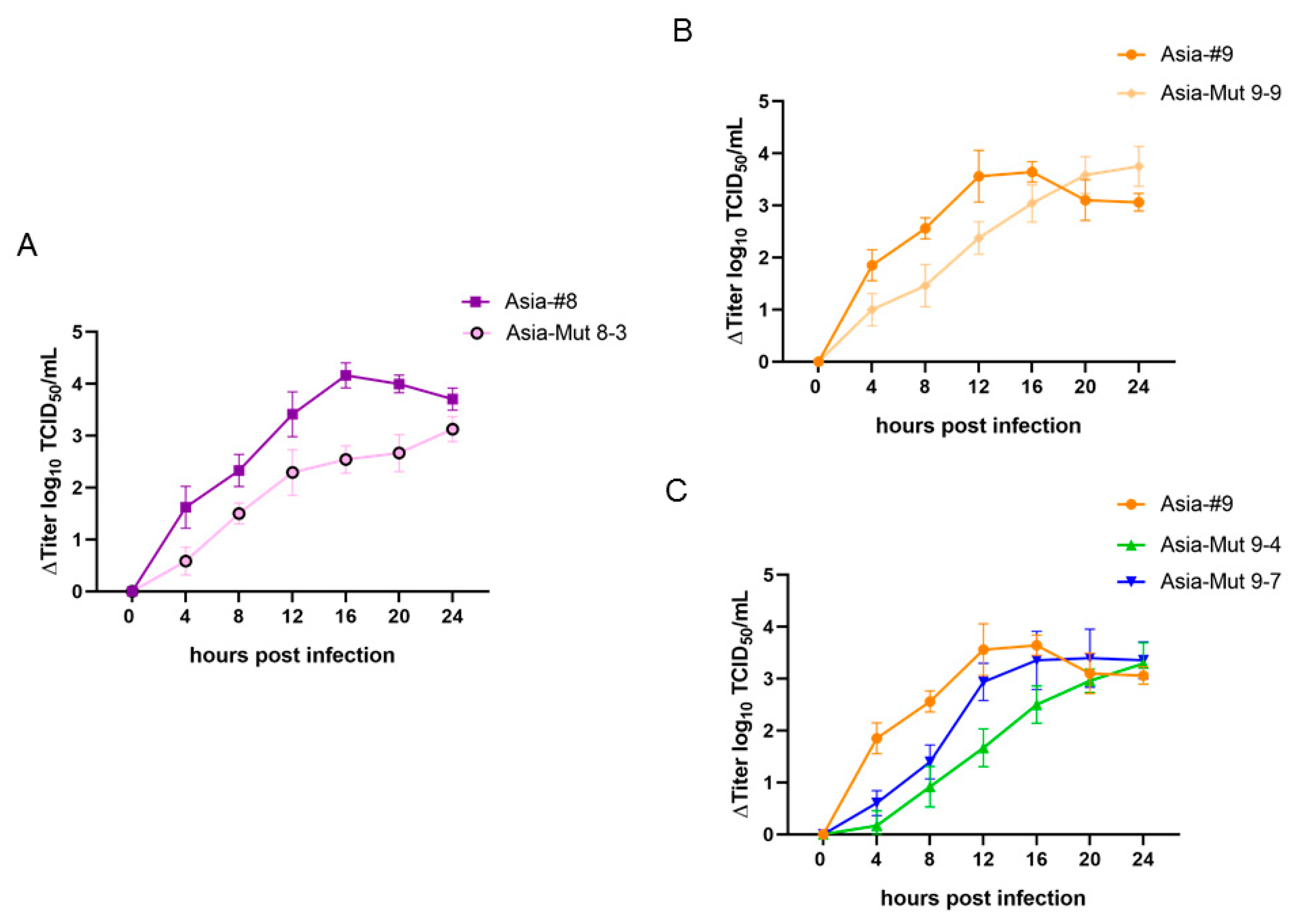
3.3. Recombinant FMDV Variants Have Altered Growth Properties Compared to Passage-Derived Strains
3.4. Immunogenicity of Passage-Derived Strains and Recombinant Viruses
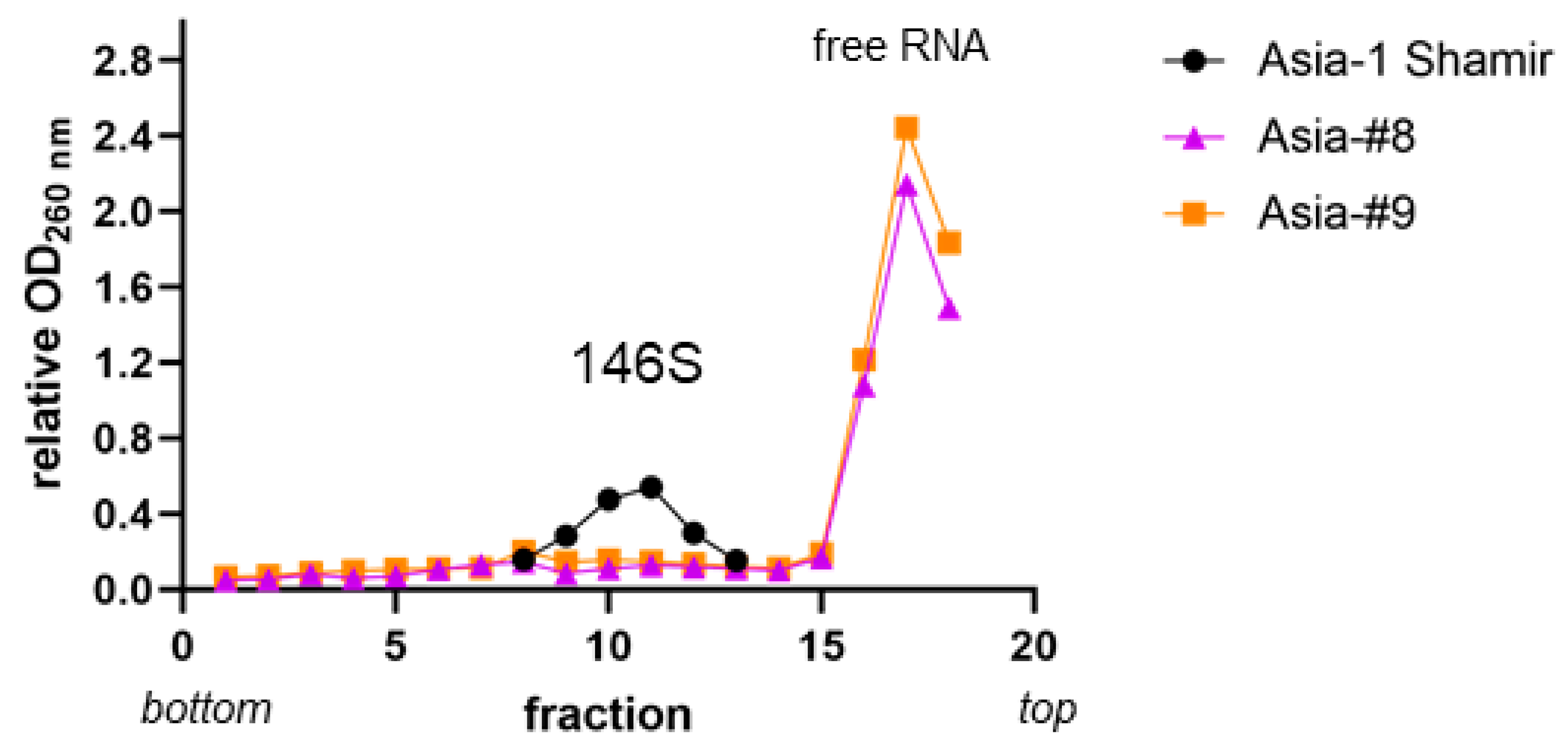
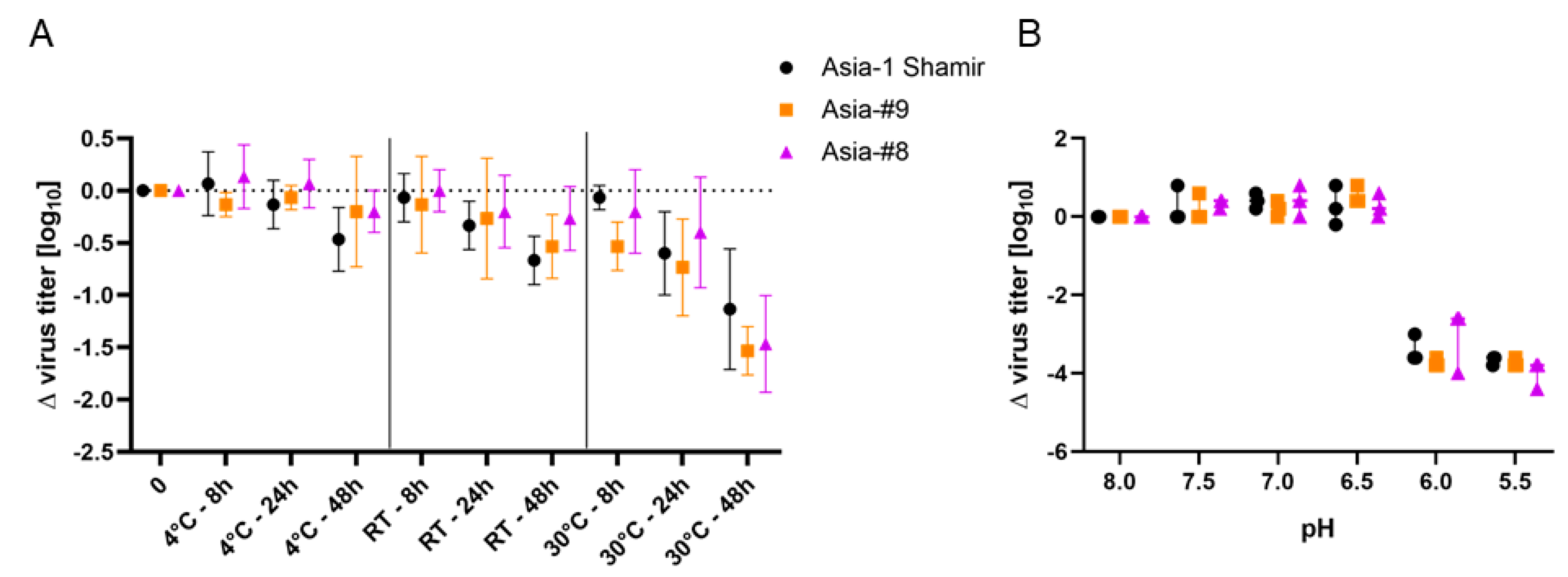
3.5. Virus Strains Asia-#8 and Asia-#9 Do Not Differ in pH and Temperature Sensitivity from the Parental Isolate Asia-1 Shamir but their Virus Particles Are Less Stable
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Brito, B.P.; Rodriguez, L.L.; Hammond, J.M.; Pinto, J.; Perez, A.M. Review of the Global Distribution of Foot-and-Mouth Disease Virus from 2007 to 2014. Transbound. Emerg. Dis. 2017, 64, 316–332. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, K.J.; Cleaveland, S.; Haydon, D.T.; Caron, A.; Kock, R.A.; Lembo, T.; Hopcraft, J.G.; Chardonnet, B.; Nyariki, T.; Keyyu, J.; et al. Evaluating the potential for the environmentally sustainable control of foot and mouth disease in Sub-Saharan Africa. Ecohealth 2013, 10, 314–322. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, L.L.; Gay, C.G. Development of vaccines toward the global control and eradication of foot-and-mouth disease. Expert Rev. Vaccines 2011, 10, 377–387. [Google Scholar] [CrossRef] [PubMed]
- Doel, T.R. FMD vaccines. Virus Res. 2003, 91, 81–99. [Google Scholar] [CrossRef]
- Belsham, G.J. Translation and replication of FMDV RNA. Curr. Top. Microbiol. Immunol. 2005, 288, 43–70. [Google Scholar]
- MacPherson, I.; Stoker, M. Polyoma transformation of hamster cell clones—An investigation of genetic factors affecting cell competence. Virology 1962, 16, 147–151. [Google Scholar] [CrossRef]
- Capstick, P.B.; Telling, R.C.; Chapman, W.G.; Stewart, D.L. Growth of a cloned strain of hamster kidney cells in suspended cultures and their susceptibility to the virus of foot-and-mouth disease. Nature 1962, 195, 1163–1164. [Google Scholar] [CrossRef]
- Telling, R.C.; Elsworth, R. Submerged culture of hamster kidney cells in a stainless steel vessel. Biotechnol. Bioeng. 1965, 7, 417–434. [Google Scholar] [CrossRef]
- Clarke, J.B.; Spier, R.E. Variation in the susceptibility of BHK populations and cloned cell lines to three strains of foot-and-mouth disease virus. Arch. Virol. 1980, 63, 1–9. [Google Scholar] [CrossRef]
- Clarke, J.B.; Spier, R.E. An investigation into causes of resistance of a cloned line of BHK cells to a strain of foot-and-mouth disease virus. Vet. Microbiol. 1983, 8, 259–270. [Google Scholar] [CrossRef]
- Syusyukin, A.A.; Tsvetkova, N.E.; Kudryatseva, G.A.; Syusyukin, M.S.; NI, E. Cultures of foot-and-mouth disease virus in different sublines of BHK 21 cells. Veterinariya 1976, 51, 46–48. [Google Scholar]
- Dill, V.; Hoffmann, B.; Zimmer, A.; Beer, M.; Eschbaumer, M. Adaption of FMDV Asia-1 to Suspension Culture: Cell Resistance Is Overcome by Virus Capsid Alterations. Viruses 2017, 9, 231. [Google Scholar] [CrossRef] [PubMed]
- Ellard, F.M.; Drew, J.; Blakemore, W.E.; Stuart, D.I.; King, A.M.Q. Evidence for the role of His-142 of protein 1C in the acid-induced disassembly of foot-and-mouth disease virus capsids. J. Gen. Virol. 1999, 80 Pt 8, 1911–1918. [Google Scholar] [CrossRef]
- Dill, V.; Beer, M.; Hoffmann, B. Simple, quick and cost-efficient: A universal RT-PCR and sequencing strategy for genomic characterisation of foot-and-mouth disease viruses. J. Virol. Methods 2017, 246, 58–64. [Google Scholar] [CrossRef]
- Bond, S.R.; Naus, C.C. RF-Cloning.org: An online tool for the design of restriction-free cloning projects. Nucleic Acids Res. 2012, 40, W209–W213. [Google Scholar] [CrossRef] [PubMed]
- Jackson, T.; Sheppard, D.; Denyer, M.; Blakemore, W.; King, A.M. The epithelial integrin alphavbeta6 is a receptor for foot-and-mouth disease virus. J. Virol. 2000, 74, 4949–4956. [Google Scholar] [CrossRef]
- Callahan, J.D.; Brown, F.; Osorio, F.A.; Sur, J.H.; Kramer, E.; Long, G.W.; Lubroth, J.; Ellis, S.J.; Shoulars, K.S.; Gaffney, K.L.; et al. Use of a portable real-time reverse transcriptase-polymerase chain reaction assay for rapid detection of foot-and-mouth disease virus. J. Am. Vet. Med. Assoc. 2002, 220, 1636–1642. [Google Scholar] [CrossRef]
- Dill, V.; Hoffmann, B.; Zimmer, A.; Beer, M.; Eschbaumer, M. Influence of cell type and cell culture media on the propagation of foot-and-mouth disease virus with regard to vaccine quality. Virol. J. 2018, 15, 46. [Google Scholar] [CrossRef]
- Bachrach, H.L.; Trautman, R.; Breese, S.S., Jr. Chemical Physical Properties of Virtually Pure Foot-and-Mouth Disease Virus. Am. J. Vet. Res. 1964, 25, 333–342. [Google Scholar]
- OIE. Foot and Mouth Disease. Manual of Diagnostic Tests and Vaccines for Terrestrial Animals. Available online: http://www.oie.int/fileadmin/Home/eng/Health_standards/tahm/2.01.08_FMD.pdf (accessed on 25 September 2017).
- Martin-Acebes, M.A.; Rincon, V.; Armas-Portela, R.; Mateu, M.G.; Sobrino, F. A single amino acid substitution in the capsid of foot-and-mouth disease virus can increase acid lability and confer resistance to acid-dependent uncoating inhibition. J. Virol. 2010, 84, 2902–2912. [Google Scholar] [CrossRef]
- Amadori, M.; Berneri, C. Genotypic and phenotypic changes of BHK-21 cells grown in suspension cultures. Cytotechnology 1993, 11, S106–S108. [Google Scholar] [CrossRef] [PubMed]
- Carrillo-Tripp, M.; Shepherd, C.M.; Borelli, I.A.; Venkataraman, S.; Lander, G.; Natarajan, P.; Johnson, J.E.; Brooks, C.L., 3rd; Reddy, V.S. VIPERdb2: An enhanced and web API enabled relational database for structural virology. Nucleic Acids Res. 2009, 37, D436–D442. [Google Scholar] [CrossRef] [PubMed]
- Berryman, S.; Clark, S.; Kakker, N.K.; Silk, R.; Seago, J.; Wadsworth, J.; Chamberlain, K.; Knowles, N.J.; Jackson, T. Positively charged residues at the five-fold symmetry axis of cell culture-adapted foot-and-mouth disease virus permit novel receptor interactions. J. Virol. 2013, 87, 8735–8744. [Google Scholar] [CrossRef] [PubMed]
- Mohapatra, J.K.; Pandey, L.K.; Rai, D.K.; Das, B.; Rodriguez, L.L.; Rout, M.; Subramaniam, S.; Sanyal, A.; Rieder, E.; Pattnaik, B. Cell culture adaptation mutations in foot-and-mouth disease virus serotype A capsid proteins: Implications for receptor interactions. J. Gen. Virol. 2015, 96, 553–564. [Google Scholar] [CrossRef]
- Lawrence, P.; Rai, D.; Conderino, J.S.; Uddowla, S.; Rieder, E. Role of Jumonji C-domain containing protein 6 (JMJD6) in infectivity of foot-and-mouth disease virus. Virology 2016, 492, 38–52. [Google Scholar] [CrossRef] [PubMed]
- Gladue, D.P.; O’Donnell, V.; Baker-Branstetter, R.; Holinka, L.G.; Pacheco, J.M.; Fernandez-Sainz, I.; Lu, Z.; Brocchi, E.; Baxt, B.; Piccone, M.E.; et al. Foot-and-mouth disease virus nonstructural protein 2C interacts with Beclin1, modulating virus replication. J. Virol. 2012, 86, 12080–12090. [Google Scholar] [CrossRef] [PubMed]
- Sweeney, T.R.; Cisnetto, V.; Bose, D.; Bailey, M.; Wilson, J.R.; Zhang, X.; Belsham, G.J.; Curry, S. Foot-and-mouth disease virus 2C is a hexameric AAA+ protein with a coordinated ATP hydrolysis mechanism. J. Biol. Chem. 2010, 285, 24347–24359. [Google Scholar] [CrossRef]
- Wang, J.; Wang, Y.; Liu, J.; Ding, L.; Zhang, Q.; Li, X.; Cao, H.; Tang, J.; Zheng, S.J. A critical role of N-myc and STAT interactor (Nmi) in foot-and-mouth disease virus (FMDV) 2C-induced apoptosis. Virus Res. 2012, 170, 59–65. [Google Scholar] [CrossRef]
- Gladue, D.P.; O’Donnell, V.; Baker-Branstetter, R.; Holinka, L.G.; Pacheco, J.M.; Fernandez Sainz, I.; Lu, Z.; Ambroggio, X.; Rodriguez, L.; Borca, M.V. Foot-and-mouth disease virus modulates cellular vimentin for virus survival. J. Virol. 2013, 87, 6794–6803. [Google Scholar] [CrossRef]
- Ben-Ze’ev, A. Cell configuration-related control of vimentin biosynthesis and phosphorylation in cultured mammalian cells. J. Cell Biol. 1983, 97, 858–865. [Google Scholar] [CrossRef]
- Grazioli, S.; Fallacara, F.; Brocchi, E. Mapping of antigenic sites of foot-and-mouth disease virus serotype Asia 1 and relationships with sites described in other serotypes. J. Gen. Virol. 2013, 94, 559–569. [Google Scholar] [CrossRef] [PubMed]
- Marquardt, O.; Rahman, M.M.; Freiberg, B. Genetic and antigenic variance of foot-and-mouth disease virus type Asia1. Arch. Virol. 2000, 145, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Sanyal, A.; Venkataramanan, R.; Pattnaik, B. Antigenic features of foot-and-mouth disease virus serotype Asia1 as revealed by monoclonal antibodies and neutralization-escape mutants. Virus Res. 1997, 50, 107–117. [Google Scholar] [CrossRef]
- Reeve, R.; Borley, D.W.; Maree, F.F.; Upadhyaya, S.; Lukhwareni, A.; Esterhuysen, J.J.; Harvey, W.T.; Blignaut, B.; Fry, E.E.; Parida, S.; et al. Tracking the Antigenic Evolution of Foot-and-Mouth Disease Virus. PLoS ONE 2016, 11, e0159360. [Google Scholar] [CrossRef]
- Butchaiah, G.; Morgan, D.O. Neutralization antigenic sites on type Asia-1 foot-and-mouth disease virus defined by monoclonal antibody-resistant variants. Virus Res. 1997, 52, 183–194. [Google Scholar] [CrossRef]
- Dill, V.; Eschbaumer, M. Cell culture propagation of foot-and-mouth disease virus: Adaptive amino acid substitutions in structural proteins and their functional implications. Virus Genes 2020, 56, 1–15. [Google Scholar] [CrossRef]
- Newman, J.F.; Rowlands, D.J.; Brown, F. A physico-chemical sub-grouping of the mammalian picornaviruses. J. Gen. Virol. 1973, 18, 171–180. [Google Scholar] [CrossRef]
- Sieng, S.; Walkden-Brown, S.W.; Kerr, J. Effect of vaccine storage temperatures and dose rate on antibody responses to foot and mouth disease vaccination in Cambodia. Vet. Med. Sci 2018, 4, 35–44. [Google Scholar] [CrossRef]
| Cell Line | Alternative Names | Growth | Collection | Accession Number |
|---|---|---|---|---|
| BHK-21 | BHK-21 clone “Tübingen” | adherent | CCLV 1 | RIE 164 |
| BHK-2P | BHK21CL13-2P | in suspension | ECACC 2 | 84111301 |
| BHK-InVitrus | “cell line #8” | in suspension | ECACC | 05062302 |
| production BHK | “cell line #9” | in suspension | Merck KGaA | n/a |
| CHO-K1 | adherent | ATCC 3 | CCL-61 | |
| CHO677 | PgsD-677 | adherent | ATCC | CRL 2244 |
| Construct | Introduced Mutation/ Amino Acid Exchange | Primers | Backbone |
|---|---|---|---|
| pT7S3_Asia-1 | GTT to GTG in 2C gene | FMD-5143-F a | pT7S3_Asia-1 |
| Asia 2C_GTT-GTG-Rev | |||
| Asia-Mut 8-1 | Q108R | Asia#8_VP1_Q108R-Fw | pT7S3_Asia-1_GTG |
| FMD-4303-R a | |||
| Asia-Mut 8-2 | Q110R | Asia#8_VP1_Q110R-Fw | pT7S3_Asia-1_GTG |
| FMD-4303-R a | |||
| Asia-Mut 8-3 | Q108R + Q110R | Asia#8_Q108R_Q110R-Fw | pT7S3_Asia-1_GTG |
| FMD-4303-R a | |||
| Asia-Mut 9-1 | E59K | Asia#9_VP3_E59K-Fw | pT7S3_Asia-1_GTG |
| FMD-3223-R a | |||
| Asia-Mut 9-2 | E59K + T83A | Asia#9_VP3_E59K-Fw | pT7S3_Asia-1_GTG |
| Asia#9_VP1_T83A-Rev | |||
| Asia-Mut 9-3 | T83A | FMD-3161-F a | pT7S3_Asia-1_GTG |
| Asia#9_VP1_T83A-Rev | |||
| Asia-Mut 9-4 | Q110K + E202K | Asia#9_VP1_Q110K-Fw | pT7S3_Asia-1_GTG |
| Asia#9_VP1_E202K-Rev | |||
| Asia-Mut 9-5 | Q110K | Asia#9_VP1_Q110K-Fw | pT7S3_Asia-1_GTG |
| FMD-4303-R a | |||
| Asia-Mut 9-6 | E202K | FMD-3161-F a | pT7S3_Asia-1_GTG |
| Asia#9_VP1_E202K-Rev | |||
| Asia-Mut 9-7 | T83A + Q110K + E202K | FMD-3161-F a | pT7S3_Asia-1_Mut 4 |
| Asia#9_VP1_T83A-Rev | |||
| Asia-Mut 9-8 | E59K + T83A + Q110K | Asia#9_VP1_Q110K-Fw | pT7S3_Asia-1_Mut 2 |
| FMD-4303-R a | |||
| Asia-Mut 9-9 | E59K + T83A + Q110K + E202K | Asia#9_VP3_E59K-Fw | pT7S3_Asia-1_Mut 4 |
| Asia#9_VP1_T83A-Rev | |||
| Asia-Mut 9-10 | E59K + T83A + E202K | FMD-3161-F a | pT7S3_Asia-1_Mut 2 |
| Asia#9_VP1_E202K-Rev | |||
| Asia-Mut 9-11 | T83A + Q110K | megaprimer of mutant 3 | pT7S3_Asia-1_Mut 5 |
| Asia-Mut 9-12 | E59K + E202K | megaprimer of mutant 1 | pT7S3_Asia-1_Mut 6 |
| Asia-Mut 9-13 | T83A + E202K | megaprimer of mutant 3 | pT7S3_Asia-1_Mut 6 |
| Asia-Mut 9-14 | E59K + Q110K | megaprimer of mutant 1 | pT7S3_Asia-1_Mut 5 |
| Isolate | Amino Acid Exchange | adh. BHK-21 | CHO-K1 | CHO677 | BHK-2P | BHK- InV (#8) | Prod. BHK (#9) |
|---|---|---|---|---|---|---|---|
| Asia-#8 | Q108R+Q110R | 8.3 ± 0.3 | 6.0 ± 0.2 | 4.7 ± 0.4 | 7.8 ± 0.3 | 7.7 ± 0.3 | 8.3 ± 0.4 |
| Asia-Mut 8-1 | Q108R | 7.6 ± 0.1 | n.t. | n.t. | n.t. | 6.6 ± 0.3 | 4.6 ± 0.3 |
| Asia-Mut 8-2 | Q110R | 7.7 ± 0.3 | n.t. | n.t. | n.t. | 6.8 ± 0.5 | 5.8 ± 0.3 |
| Asia-Mut 8-3 | Q108R+Q110R | 7.7 ± 0.2 | 6.0 ± 0.2 | n.t. | 7.2 ± 0.3 | 7.4 ± 0.2 | 7.6 ± 0.1 |
| Isolate | Amino Acid Exchange | adh. BHK-21 | CHO-K1 | CHO677 | BHK-2P | BHK InV (#8) | Prod. BHK (#9) |
|---|---|---|---|---|---|---|---|
| Asia-1 Shamir | none | 7.7 ± 0.3 | n.t. | n.t. | n.t. | 6.3 ± 0.3 | 3.0 ± 0.3 |
| Asia-Mut 9-1 | E59K | 7.8 ± 0.2 | n.t. | n.t. | n.t. | 6.8 ± 0.4 | 4.7 ± 0.3 |
| Asia-Mut 9-2 | E59K+T83A | 7.5 ± 0.2 | n.t. | n.t. | n.t. | 6.9 ± 0.3 | 4.8 ± 0.2 |
| Asia-Mut 9-3 | T83A | 7.7 ± 0.3 | n.t. | n.t. | n.t. | 5.5 ± 0.3 | n.t. |
| Asia-Mut 9-5 | Q110K | 7.8 ± 0.4 | n.t. | n.t. | n.t. | 6.9 ± 0.3 | 4.9 ± 0.3 |
| Asia-Mut 9-6 | E202K | 7.7 ± 0.2 | n.t. | n.t. | n.t. | 6.5 ± 0.1 | 4.1 ± 0.3 |
| Asia-Mut 9-8 | E59K+T83A+ Q110K | 7.9 ± 0.4 | n.t. | n.t. | n.t. | 6.3 ± 0.1 | 5.4 ± 0.3 |
| Asia-Mut 9-11 | T83A+Q110K | 7.6 ± 0.2 | n.t. | n.t. | n.t. | 6.1 ± 0.3 | 5.8 ± 0.2 |
| Asia-Mut 9-13 | T83A+E202K | 7.3 ± 0.3 | n.t. | n.t. | n.t. | 6.6 ± 0.3 | 5.3 ± 0.3 |
| Asia-Mut 9-14 | E59K+Q110K | 7.7 ± 0.4 | n.t. | n.t. | n.t. | 6.8 ± 0.2 | 6.2 ± 0.5 |
| Isolate | Amino Acid Exchange | Adh. BHK-21 | CHO-K1 | CHO677 | BHK-2P | BHK- InV (#8) | Prod. BHK (#9) |
|---|---|---|---|---|---|---|---|
| Asia-#9 | E59K + T83A + Q110K+E202K | 7.5 ± 0.3 | 6.0 ± 0.6 | 5.8 ± 0.2 | 6.8 ± 0.3 | 6.8 ± 0.2 | 7.7 ± 0.3 |
| Asia-Mut 9-4 | Q110K + E202K | 7.6 ± 0.2 | n.t. | n.t. | 7.7 ± 0.4 | 7.5 ± 0.5 | 8.0 ± 0.2 |
| Asia-Mut 9-7 | T83A + Q110K + E202K | 7.4 ± 0.1 | 5.8 ± 0.2 | 6.0 ± 0.3 | 6.8 ± 0.3 | 6.9 ± 0.3 | 7.7 ± 0.3 |
| Asia-Mut 9-9 | E59K + T83A + Q110K + E202K | 8.1 ± 0.3 | 5.3 ± 0.4 | 5.5 ± 0.3 | 7.2 ± 0.4 | 7.4 ± 0.2 | 7.7 ± 0.4 |
| Asia-Mut 9-10 | E59K + T83A+ E202K | 7.6 ± 0.3 | n.t. | n.t. | 4.8 ± 0.2 | 7.3 ± 0.5 | 7.5 ± 0.2 |
| Asia-Mut 9-12 | E59K + E202K | 7.7 ± 0.3 | n.t. | n.t. | 5.8 ± 0.4 | 7.3 ± 0.5 | 7.7 ± 0.3 |
| Isolate | Serum Titer [log10] | r1-Value | |
|---|---|---|---|
| Heterologous | Homologous | ||
| PC | - | 1.8 ± 0.16 | 1 |
| Asia-1 Shamir | - | 1.9 ± 0.27 | 1.1 |
| Asia-#8 | 0 | 0 | 0 |
| Asia-#9 | 0 | 0 | 0 |
| Asia-Mut 9-4 | 0 | 0.94 ± 0.05 | 0 |
| Asia-Mut 9-7 | 0.75 ± 0.00 | 1.28 ± 0.00 | 0.4 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dill, V.; Zimmer, A.; Beer, M.; Eschbaumer, M. Targeted Modification of the Foot-And-Mouth Disease Virus Genome for Quick Cell Culture Adaptation. Vaccines 2020, 8, 583. https://doi.org/10.3390/vaccines8040583
Dill V, Zimmer A, Beer M, Eschbaumer M. Targeted Modification of the Foot-And-Mouth Disease Virus Genome for Quick Cell Culture Adaptation. Vaccines. 2020; 8(4):583. https://doi.org/10.3390/vaccines8040583
Chicago/Turabian StyleDill, Veronika, Aline Zimmer, Martin Beer, and Michael Eschbaumer. 2020. "Targeted Modification of the Foot-And-Mouth Disease Virus Genome for Quick Cell Culture Adaptation" Vaccines 8, no. 4: 583. https://doi.org/10.3390/vaccines8040583
APA StyleDill, V., Zimmer, A., Beer, M., & Eschbaumer, M. (2020). Targeted Modification of the Foot-And-Mouth Disease Virus Genome for Quick Cell Culture Adaptation. Vaccines, 8(4), 583. https://doi.org/10.3390/vaccines8040583






