Relationship between Influenza Vaccination Coverage Rate and COVID-19 Outbreak: An Italian Ecological Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Definition of Outcomes and Predictors
2.3. Influenza Vaccination Coverage
2.4. Confounders
2.5. Ethics Committee Approval
2.6. Statistical Analysis
3. Results
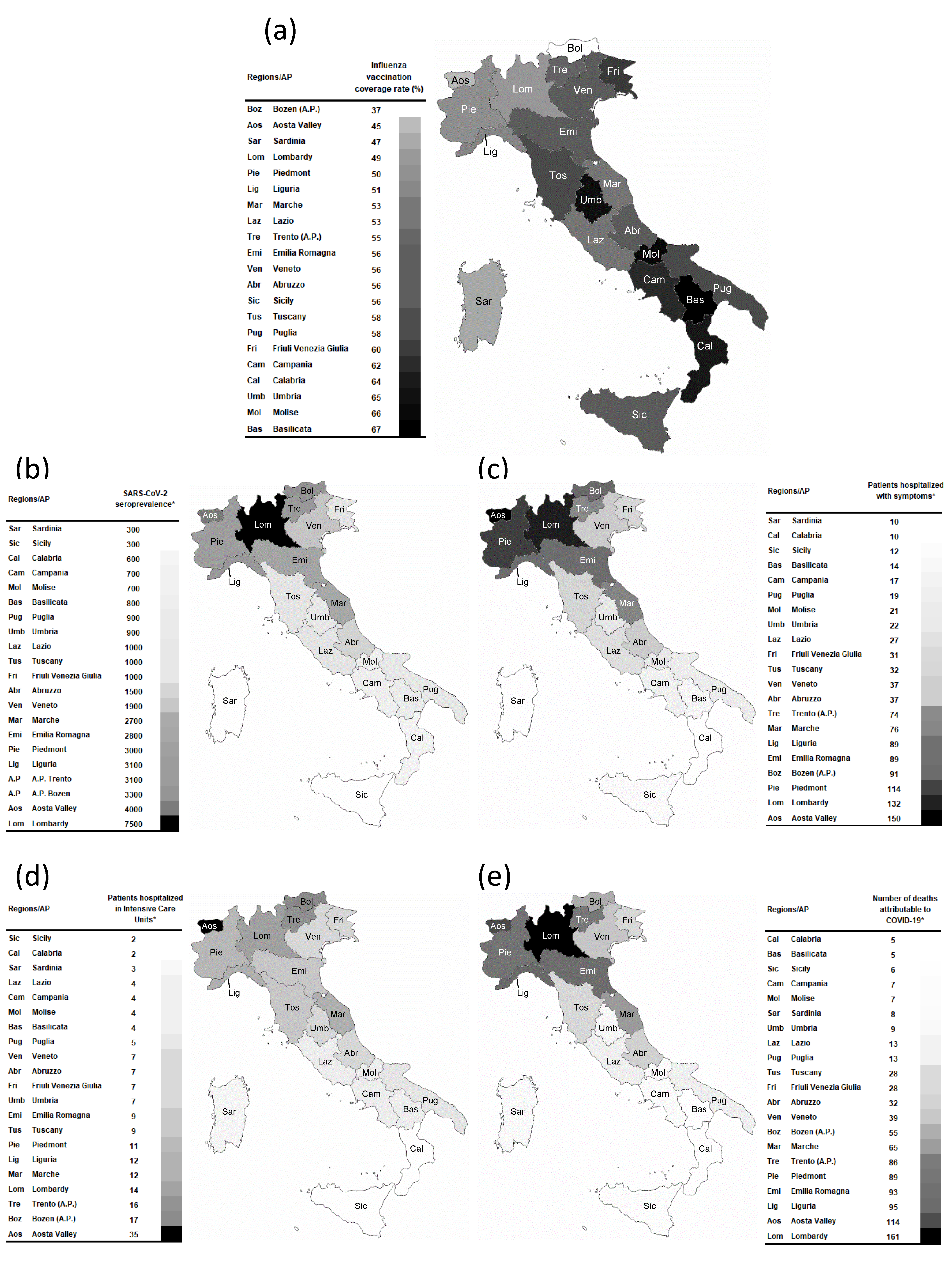
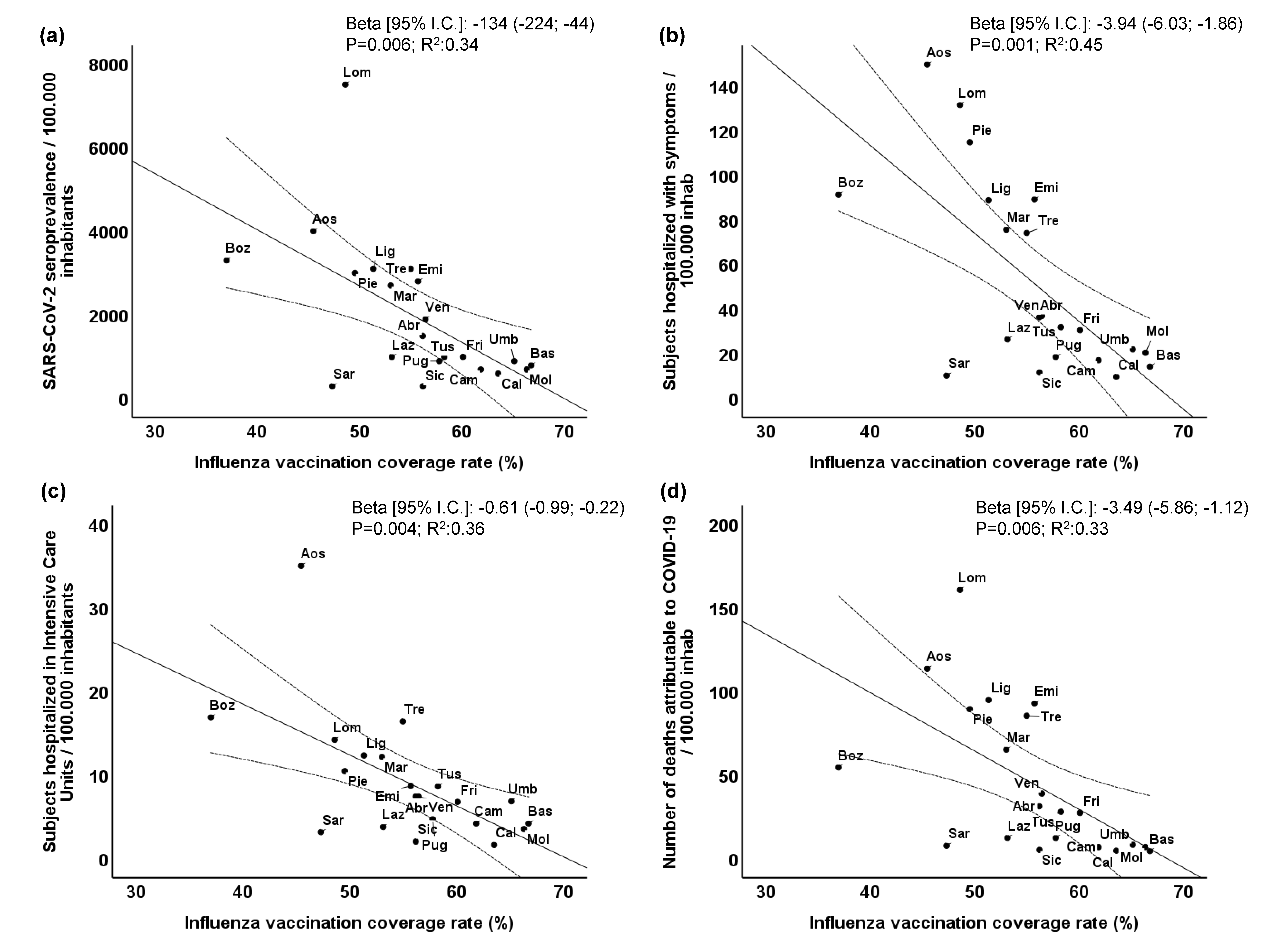
3.1. Influenza Vaccination Coverage Rate and COVID-19 Outcomes
3.2. Role of Potential Confounders
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Espinosa, O.A.; Zanetti, A.D.S.; Antunes, E.F.; Longhi, F.G.; Matos, T.A.; Battaglini, P.F. Prevalence of comorbidities in patients and mortality cases affected by SARS-CoV2: A systematic review and meta-analysis. Rev. Inst. Med. Trop. Sao Paulo 2020, 62, e43. [Google Scholar] [CrossRef] [PubMed]
- WHO. Coronavirus Disease 2019 (COVID-19), Situation Report—51. 2020. Available online: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19pdf?sfvrsn=1ba62e57_10 (accessed on 11 March 2020).
- Remuzzi, A.; Remuzzi, G. COVID-19 and Italy: What next? Lancet 2020, 395, 1225–1228. [Google Scholar] [CrossRef]
- Italian Ministry of Health. Rapporto Epidemiologico InfluNet. 2020. Available online: http://www.salute.gov.it/portale/temi/documenti/epidemiologica/Influnet_2020_17.pdf (accessed on 8 May 2020).
- Petersen, E.; Koopmans, M.; Go, U.; Hamer, D.H.; Petrosillo, N.; Castelli, F.; Storgaard, M.; Al Khalili, S.; Simonsen, L. Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics. Lancet Infect. Dis. 2020, 20, e238–e244. [Google Scholar] [CrossRef]
- Worby, C.J.; Chaves, S.S.; Wallinga, J.; Lipsitch, M.; Finelli, L.; Goldstein, E. On the relative role of different age groups in influenza epidemics. Epidemics 2015, 13, 10–16. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://emedicine.medscape.com/article/2500114-overview#a5 (accessed on 3 August 2020).
- Stokes, E.K.; Zambrano, L.D.; Anderson, K.N.; Marder, E.P.; Raz, K.M.; El Burai Felix, S.; Tie, Y.; Fullerton, K.E. Coronavirus Disease 2019 Case Surveillance—United States, January 22–May 30, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 759–765. [Google Scholar] [CrossRef]
- Netea, M.G.; Dominguez-Andres, J.; Barreiro, L.B.; Chavakis, T.; Divangahi, M.; Fuchs, E.; Joosten, L.A.B.; van der Meer, J.W.M.; Mhlanga, M.M.; Mulder, W.J.M.; et al. Defining trained immunity and its role in health and disease. Nat. Rev. Immunol. 2020, 20, 375–388. [Google Scholar] [CrossRef]
- Italian Ministry of Health. 2020. Available online: http://www.salute.gov.it/portale/influenza/dettaglioContenutiInfluenza.jsp?lingua=italiano&id=686&area=influenza&menu=vuoto&tab=2 (accessed on 6 June 2020).
- World Health Organization. Prevention and Control of Influenza Pandemics and Annual Epidemics. Geneva. 2003. Available online: http://www.who.int/immunization/sage/1_WHA56_19_Prevention_and_control_of_influenza_pandemic.pdf (accessed on 28 May 2003).
- Wise, J. Covid-19: Risk of second wave is very real, say researchers. BMJ 2020, 369, m2294. [Google Scholar] [CrossRef]
- Adebowale, V.; Alderson, D.; Burn, W.; Dixon, J.; Godlee, F.; Goddard, A.; Griffin, M.; Henderson, K.; Horton, R.; Marshall, M.; et al. Covid-19: Call for a rapid forward looking review of the UK’s preparedness for a second wave-an open letter to the leaders of all UK political parties. BMJ 2020, 369, m2514. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.istat.it/it/files//2020/08/ReportPrimiRisultatiIndagineSiero.pdf (accessed on 3 August 2020).
- Available online: https://github.com/pcm-dpc/COVID-19/blob/master/dati-regioni/dpc-covid19-ita-regioni-20200602.csv (accessed on 3 June 2020).
- Available online: http://dati.istat.it/Index.aspx?DataSetCode=DCIS_POPRES1 (accessed on 8 June 2020).
- Italian Ministry of Health. 2019. Available online: http://www.salute.gov.it/imgs/C_17_tavole_19_allegati_iitemAllegati_0_fileAllegati_itemFile_5_file.pdf (accessed on 5 June 2020).
- Asfahan, S.; Shahul, A.; Chawla, G.; Dutt, N.; Niwas, R.; Gupta, N. Early trends of socio-economic and health indicators influencing case fatality rate of COVID-19 pandemic. Monaldi Arch. Chest Dis. 2020, 90. [Google Scholar] [CrossRef]
- Pani, S.K.; Lin, N.H.; RavindraBabu, S. Association of COVID-19 pandemic with meteorological parameters over Singapore. Sci. Total Environ. 2020, 740, 140112. [Google Scholar] [CrossRef]
- Mandal, C.C.; Panwar, M.S. Can the summer temperature drop COVID-19 cases? Public Health 2020, 185, 72–79. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, M.M.; Abid, I.; Hussain, S.; Shahzad, N.; Waqas, M.S.; Iqbal, M.J. The effects of regional climatic condition on the spread of COVID-19 at global scale. Sci. Total Environ. 2020, 739, 140101. [Google Scholar] [CrossRef] [PubMed]
- The Relationship between Human Mobility and Viral Transmissibility during the COVID-19 Epidemics in Italy. Available online: http://sobigdata.eu/covid_report/#/report2 (accessed on 4 June 2020).
- Bontempi, E. Commercial exchanges instead of air pollution as possible origin of COVID-19 initial diffusion phase in Italy: More efforts are necessary to address interdisciplinary research. Environ. Res. 2020, 188, 109775. [Google Scholar] [CrossRef] [PubMed]
- Lau, H.; Khosrawipour, V.; Kocbach, P.; Mikolajczyk, A.; Ichii, H.; Zacharski, M.; Bania, J.; Khosrawipour, T. The association between international and domestic air traffic and the coronavirus (COVID-19) outbreak. J. Microbiol. Immunol. Infect. 2020, 53, 467–472. [Google Scholar] [CrossRef]
- Du, R.H.; Liang, L.R.; Yang, C.Q.; Wang, W.; Cao, T.Z.; Li, M.; Guo, G.Y.; Du, J.; Zheng, C.L.; Zhu, Q.; et al. Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: A prospective cohort study. Eur. Respir. J. 2020, 55, 2000524. [Google Scholar] [CrossRef] [PubMed]
- Clerkin, K.J.; Fried, J.A.; Raikhelkar, J.; Sayer, G.; Griffin, J.M.; Masoumi, A.; Jain, S.S.; Burkhoff, D.; Kumaraiah, D.; Rabbani, L.; et al. COVID-19 and Cardiovascular Disease. Circulation 2020, 141, 1648–1655. [Google Scholar] [CrossRef]
- Zheng, Z.; Peng, F.; Xu, B.; Zhao, J.; Liu, H.; Peng, J.; Li, Q.; Jiang, C.; Zhou, Y.; Liu, S.; et al. Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis. J. Infect. 2020, 81, e16–e25. [Google Scholar]
- Available online: https://www.cergas.unibocconi.eu/wps/wcm/connect/4c40095a-2ca4-4c9f-828c-385db9e4d9db/Cap3OASI_2019.pdf?MOD=AJPERES&CVID=mWPG7t3 (accessed on 29 November 2019).
- Available online: https://www.3bmeteo.com (accessed on 8 June 2020).
- Available online: http://dati.istat.it/viewhtml.aspx?il=blank&vh=0000&vf=0&vcq=1100&graph=0&view-metadata=1&lang=it&QueryId=26435&metadata=DCIS_CMORTE1_RES# (accessed on 27 July 2020).
- Available online: https://assaeroporti.com/statistiche/ (accessed on 18 May 2020).
- Fink, G.; Orlova-Fink, N.; Schindler, T.; Grisi, S.; Ferrer, A.P.; Daubenberger, C.; Brentani, A. Inactivated trivalent influenza vaccine is associated with lower mortality among Covid-19 patients in Brazil. medRxiv 2020. [Google Scholar] [CrossRef]
- Zanettini, C.; Omar, M.; Dinalankara, W.; Imada, E.L.; Colantuoni, E.; Parmigiani, G.; Marchionni, L. Influenza Vaccination and COVID19 Mortality in the USA. medRxiv 2020. [Google Scholar] [CrossRef]
- Marin-Hernandez, D.; Schwartz, R.E.; Nixon, D.F. Epidemiological evidence for association between higher influenza vaccine uptake in the elderly and lower COVID-19 deaths in Italy. J. Med. Virol. 2020. [Google Scholar] [CrossRef]
- O’Neill, L.A.J.; Netea, M.G. BCG-induced trained immunity: Can it offer protection against COVID-19? Nat. Rev. Immunol. 2020, 20, 335–337. [Google Scholar] [CrossRef] [PubMed]
- Miller, A.; Reandelar, M.J.; Fasciglione, K.; Roumenova, V.; Li, Y.; Otazu, G. Correlation between universal BCG vaccination policy and reduced morbidity and mortality for COVID-19: An epidemiological study. medRxiv 2020. [Google Scholar] [CrossRef]
- Horns, F.; Dekker, C.L.; Quake, S.R. Memory B Cell Activation, Broad Anti-influenza Antibodies, and Bystander Activation Revealed by Single-Cell Transcriptomics. Cell Rep. 2020, 30, 905–913.e6. [Google Scholar] [CrossRef]
- Rieckmann, A.; Villumsen, M.; Honge, B.L.; Sorup, S.; Rodrigues, A.; da Silva, Z.J.; Whittle, H.; Benn, C.; Aaby, P. Phase-out of smallpox vaccination and the female/male HIV-1 prevalence ratio: An ecological study from Guinea-Bissau. BMJ Open 2019, 9, e031415. [Google Scholar] [CrossRef] [PubMed]
- Wolff, G.G. Influenza vaccination and respiratory virus interference among Department of Defense personnel during the 2017-2018 influenza season. Vaccine 2020, 38, 350–354. [Google Scholar] [CrossRef]
- Zeng, Q.; Khan, K.; Wu, J.; Zhu, H. The utility of preemptive mass influenza vaccination in controlling a sars outbreak during flu season. Math. Biosci. Eng. 2007, 4, 739–754. [Google Scholar]
- Khan, K.; Muennig, P.; Gardam, M.; Zivin, J.G. Managing febrile respiratory illnesses during a hypothetical SARS outbreak. Emerg. Infect. Dis. 2005, 11, 191–200. [Google Scholar] [CrossRef]
- Li, Q.; Tang, B.; Bragazzi, N.L.; Xiao, Y.; Wu, J. Modeling the impact of mass influenza vaccination and public health interventions on COVID-19 epidemics with limited detection capability. Math. Biosci. 2020, 325, 108378. [Google Scholar] [CrossRef]
- Kleinnijenhuis, J.; Quintin, J.; Preijers, F.; Benn, C.S.; Joosten, L.A.; Jacobs, C.; van Loenhout, J.; Xavier, R.J.; Aaby, P.; van der Meer, J.W.; et al. Long-lasting effects of BCG vaccination on both heterologous Th1/Th17 responses and innate trained immunity. J. Innate Immun. 2014, 6, 152–158. [Google Scholar] [CrossRef]
- Kim, D.; Quinn, J.; Pinsky, B.; Shah, N.H.; Brown, I. Rates of Co-infection between SARS-CoV-2 and Other Respiratory Pathogens. JAMA 2020, 323, 2085–2086. [Google Scholar] [CrossRef]
- Hashemi, S.A.; Safamanesh, S.; Ghasemzadeh-Moghaddam, H.; Ghafouri, M.; Amir, A. High prevalence of SARS-CoV-2 and influenza A virus (H1N1) co-infection in dead patients in Northeastern Iran. J. Med. Virol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.H.; Chang, Y.Y.; Kuo, S.C.; Chen, Y.T. Influenza vaccination and secondary prevention of cardiovascular disease among Taiwanese elders-A propensity score-matched follow-up study. PLoS ONE 2019, 14, e0219172. [Google Scholar] [CrossRef] [PubMed]
- Aidoud, A.; Marlet, J.; Angoulvant, D.; Debacq, C.; Gavazzi, G.; Fougere, B. Influenza vaccination as a novel means of preventing coronary heart disease: Effectiveness in older adults. Vaccine 2020, 38, 4944–4955. [Google Scholar] [CrossRef] [PubMed]
- MacIntyre, C.R.; Mahimbo, A.; Moa, A.M.; Barnes, M. Influenza vaccine as a coronary intervention for prevention of myocardial infarction. Heart 2016, 102, 1953–1956. [Google Scholar] [CrossRef] [PubMed]
- Costantino, C.; Vitale, F. Influenza vaccination in high-risk groups: A revision of existing guidelines and rationale for an evidence-based preventive strategy. J. Prev. Med. Hyg. 2016, 57, E13–E18. [Google Scholar] [PubMed]
- Consortium, E. COVID-19 Severity in Europe and the USA: Could the Seasonal Influenza Vaccination Play a Role? SSRN 2020, 3621446. [Google Scholar] [CrossRef]
- Washio, M.; Oura, A.; Mori, M. Ecological studies on influenza infection and the effect of vaccination: Their advantages and limitations. Vaccine 2008, 26, 6470–6472. [Google Scholar] [CrossRef]
| Regional Features/Variables | Influenza Vaccination Coverage Rate | SARS-CoV-2 Seroprevalence | Patients Hospitalized with Symptoms | Patients Hospitalized in Intensive Care Units | Number of Deaths Attributable to COVID-19 |
|---|---|---|---|---|---|
| Public health expenditures § | 0.54 * | −0.72 # | −0.71 # | −0.60 ** | −0.72 # |
| Mean seasonal temperature | 0.28 | −0.64 ** | −0.64 ** | −0.64 ** | −0.55 ** |
| Delay in applying the lockdown | −0.51 * | 0.45 * | 0.46 * | 0.16 | 0.50 * |
| Import–export with China | −0.21 | 0.46 * | 0.46 * | 0.11 | 0.63 ** |
| International air traffic | −0.18 | 0.17 | 0.17 | −0.07 | 0.29 |
| Mortality from CVD | 0.61 ** | −0.53 * | −0.26 | −0.32 | −0.28 |
| Mortality from respiratory diseases | 0.16 | 0.26 | 0.26 | 0.21 | 0.22 |
| Regional Features/Variables | SARS-CoV-2 Seroprevalence | Patients Hospitalized with Symptoms | Patients Hospitalized in Intensive Care Units | Number of Deaths Attributable to COVID-19 | ||||
|---|---|---|---|---|---|---|---|---|
| Beta [95% C. I.] | p | Beta [95% C. I.] | p | Beta [95% C. I.] | p | Beta [95% C. I.] | p | |
| Influenza vaccination coverage rate | −130 (−198; −62) | 0.001 | −4.16 (−6.27; −2.05) | 0.001 | −0.58 (−1.05; −0.12) | 0.017 | −3.29 (−5.66; −0.93) | 0.01 |
| Public health expenditures * | −224 (−616; 168) | 0.24 | −3.56 (−15.73; 8.6) | 0.54 | −1.94 (−4.59; 0.71) | 0.14 | −7.90 (−21.53; 5.72) | 0.23 |
| Mean seasonal temperature | −123 (−359; 113) | 0.28 | −6.32 (−13.64; 1.01) | 0.09 | −0.73 (−2.33; 0.87) | 0.34 | −2.40 (−10.60; 5.80) | 0.54 |
| Delay in applying the lockdown | −70.8 (−145.1; 3.6) | 0.06 | −0.77 (−3.08; 1.54) | 0.49 | −0.45 (−0.96; 0.05) | 0.07 | −1.28 (−3.86; 1.30) | 0.31 |
| Import–export with China | 0.66 (0.42; 0.90) | <0.0001 | 0.010 (0.001; 0.016) | 0.032 | 0.000 (−0.002; 0.001) | 0.87 | 0.01 (0.01; 0.02) | 0.004 |
| Mortality from CVD | 652 (−88; 1392) | 0.08 | 26.1 (3.1; 49.1) | 0.029 | 1.35 (−3.66; 6.36) | 0.57 | 22.7 (−3.0; 48.5) | 0.08 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amato, M.; Werba, J.P.; Frigerio, B.; Coggi, D.; Sansaro, D.; Ravani, A.; Ferrante, P.; Veglia, F.; Tremoli, E.; Baldassarre, D. Relationship between Influenza Vaccination Coverage Rate and COVID-19 Outbreak: An Italian Ecological Study. Vaccines 2020, 8, 535. https://doi.org/10.3390/vaccines8030535
Amato M, Werba JP, Frigerio B, Coggi D, Sansaro D, Ravani A, Ferrante P, Veglia F, Tremoli E, Baldassarre D. Relationship between Influenza Vaccination Coverage Rate and COVID-19 Outbreak: An Italian Ecological Study. Vaccines. 2020; 8(3):535. https://doi.org/10.3390/vaccines8030535
Chicago/Turabian StyleAmato, Mauro, José Pablo Werba, Beatrice Frigerio, Daniela Coggi, Daniela Sansaro, Alessio Ravani, Palma Ferrante, Fabrizio Veglia, Elena Tremoli, and Damiano Baldassarre. 2020. "Relationship between Influenza Vaccination Coverage Rate and COVID-19 Outbreak: An Italian Ecological Study" Vaccines 8, no. 3: 535. https://doi.org/10.3390/vaccines8030535
APA StyleAmato, M., Werba, J. P., Frigerio, B., Coggi, D., Sansaro, D., Ravani, A., Ferrante, P., Veglia, F., Tremoli, E., & Baldassarre, D. (2020). Relationship between Influenza Vaccination Coverage Rate and COVID-19 Outbreak: An Italian Ecological Study. Vaccines, 8(3), 535. https://doi.org/10.3390/vaccines8030535












