Rationally Attenuated Vaccines for Venezuelan Equine Encephalitis Protect Against Epidemic Strains with a Single Dose
Abstract
1. Introduction
2. Materials and Methods
2.1. Cell Lines and Viruses
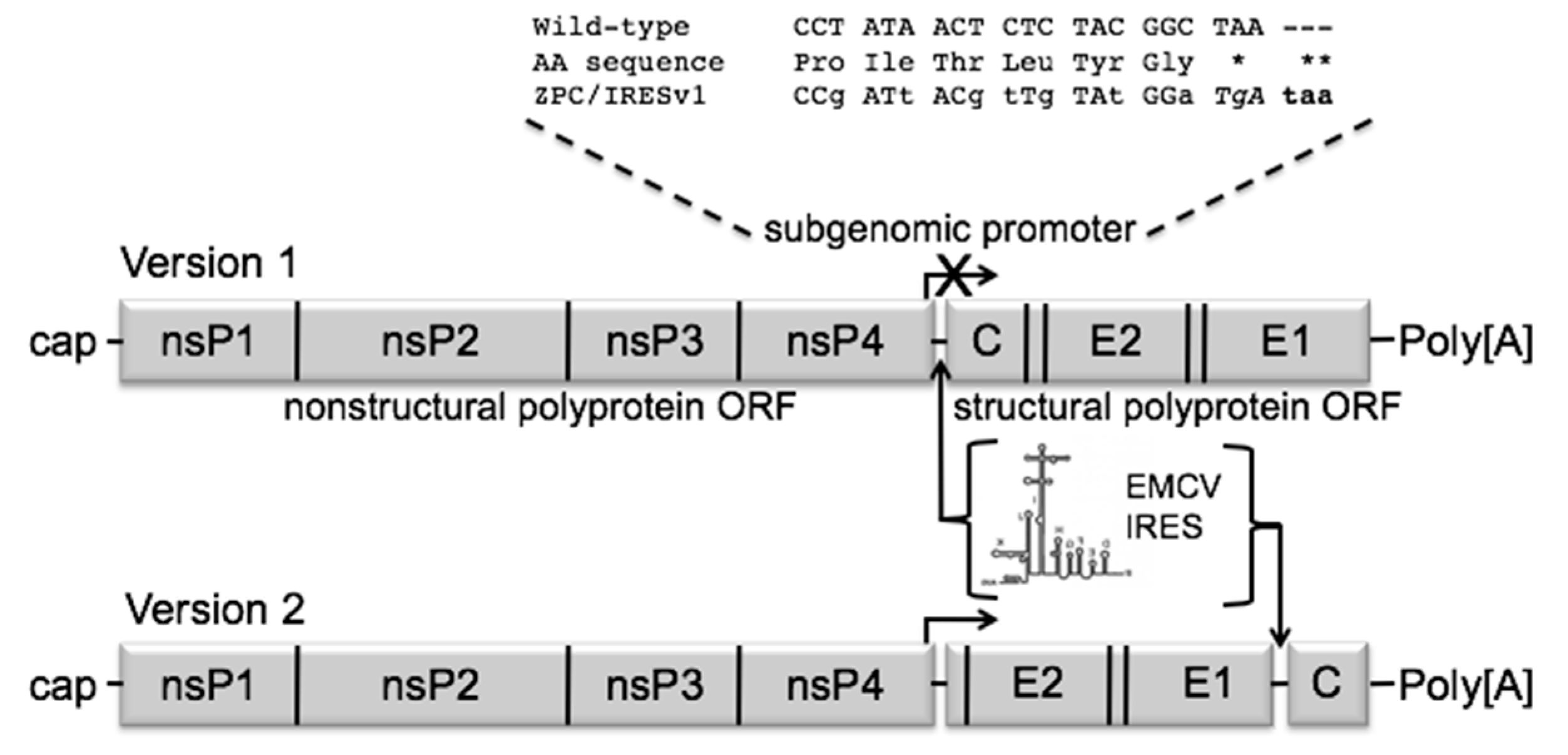
2.2. Creating the IRES Vaccines and Rescue
2.3. Titrations
2.4. Plaque Reduction Neutralization Tests
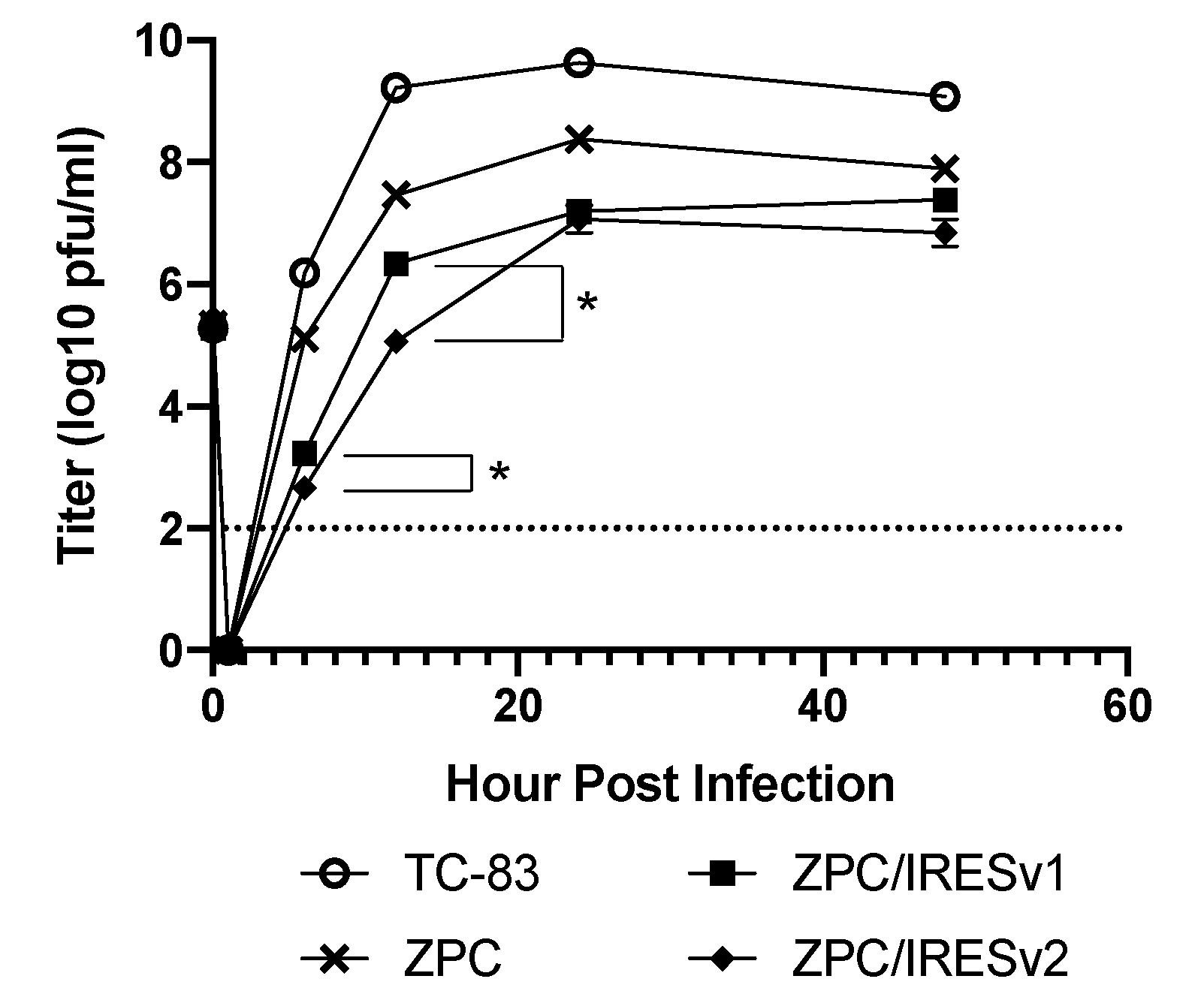
2.5. Replication Curves
2.6. Serial Passage in Vero Cells
2.7. Mouse Studies
2.8. Nonhuman Primate Studies
2.9. Statistical Analyses
3. Results
3.1. Creation and Characterization of VEEV ZPC/IRES Vaccines
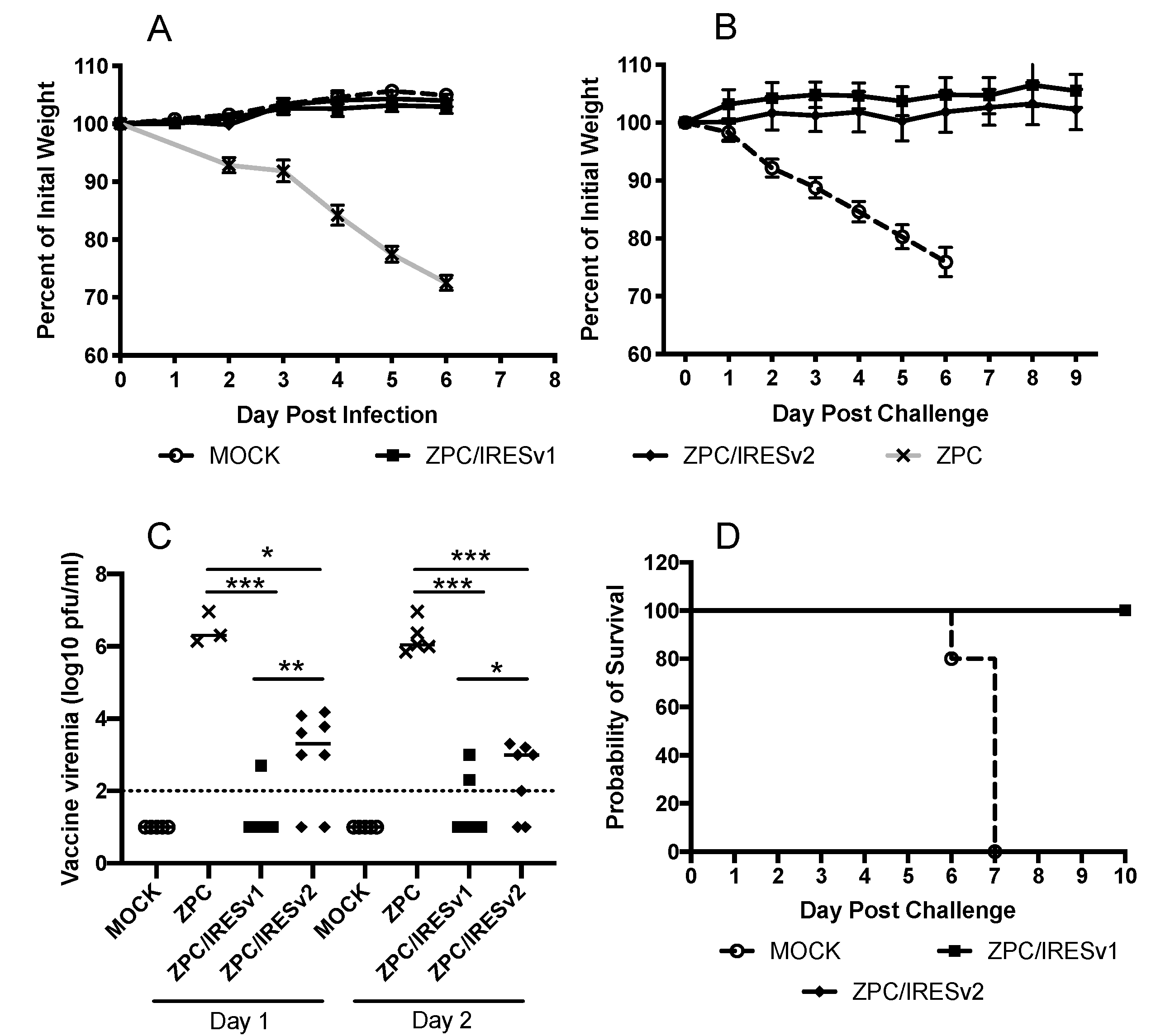
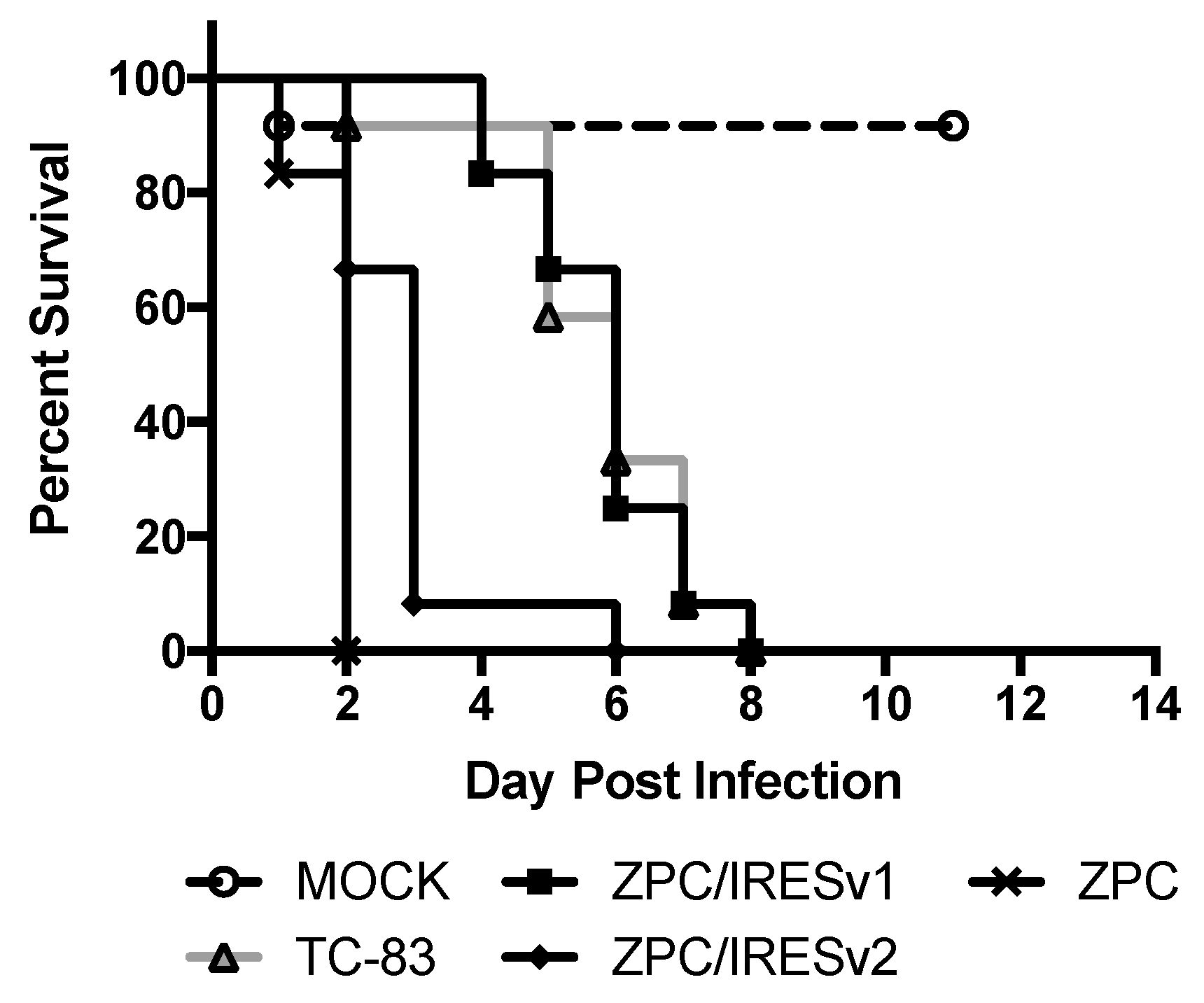
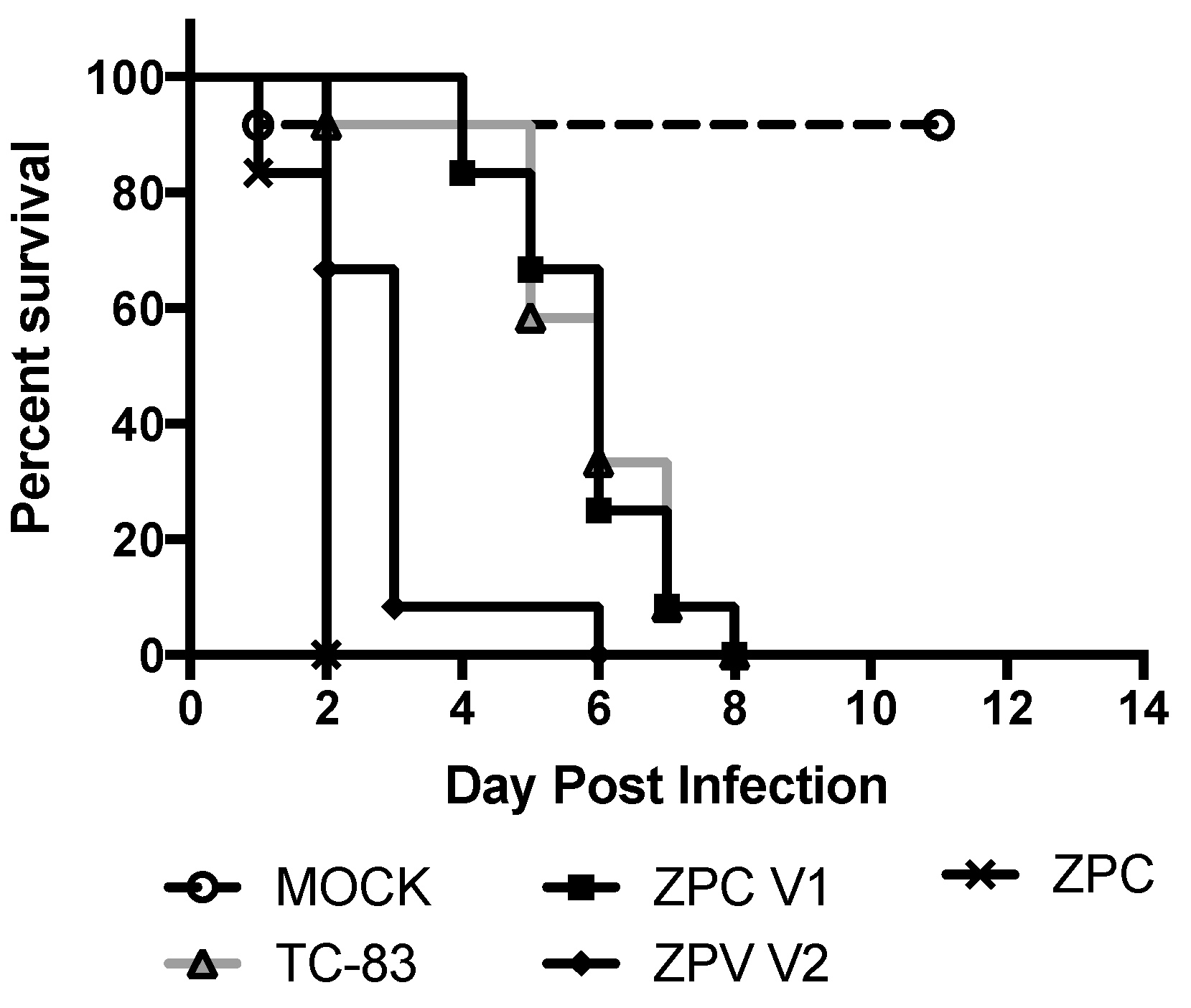
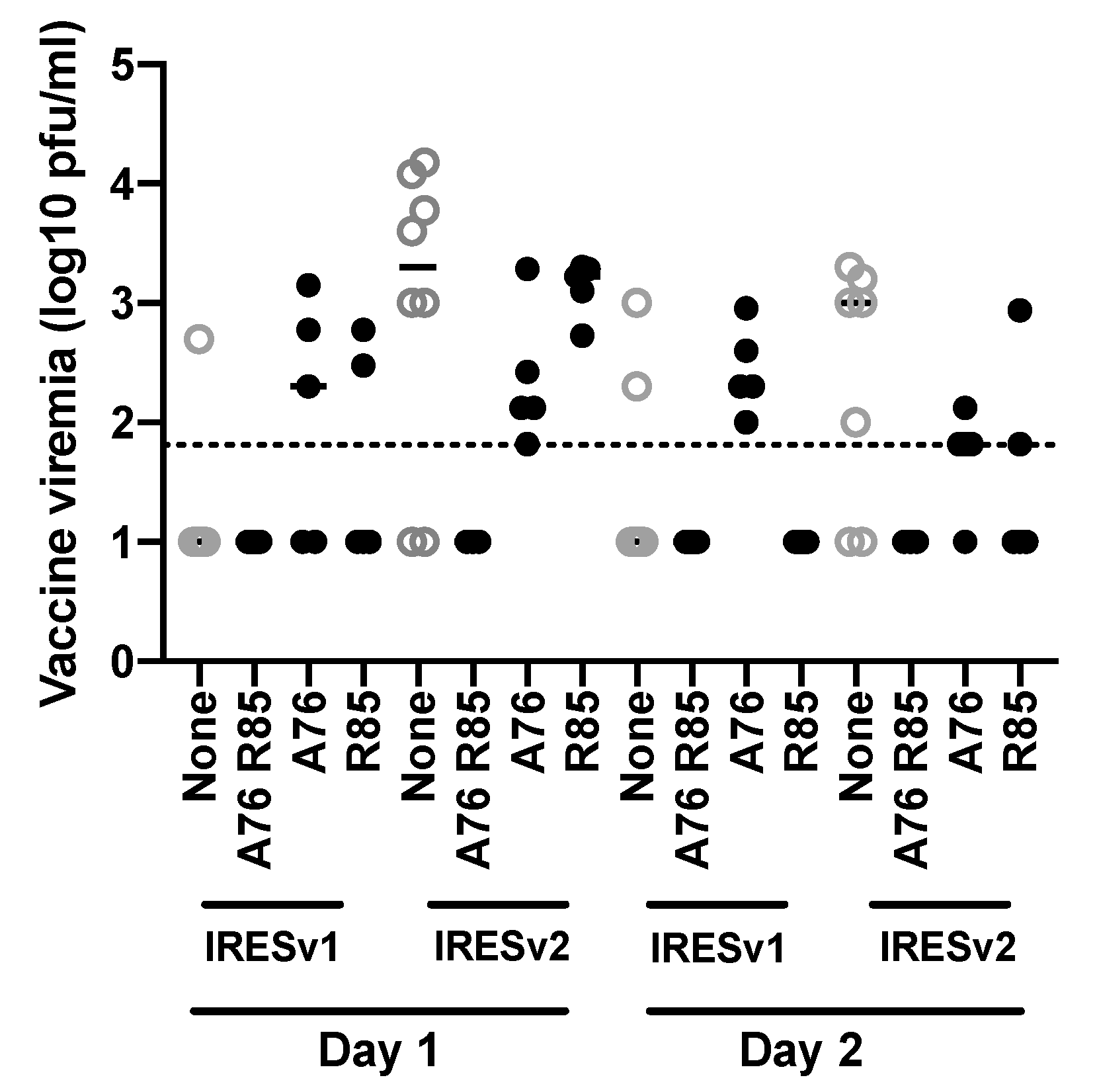
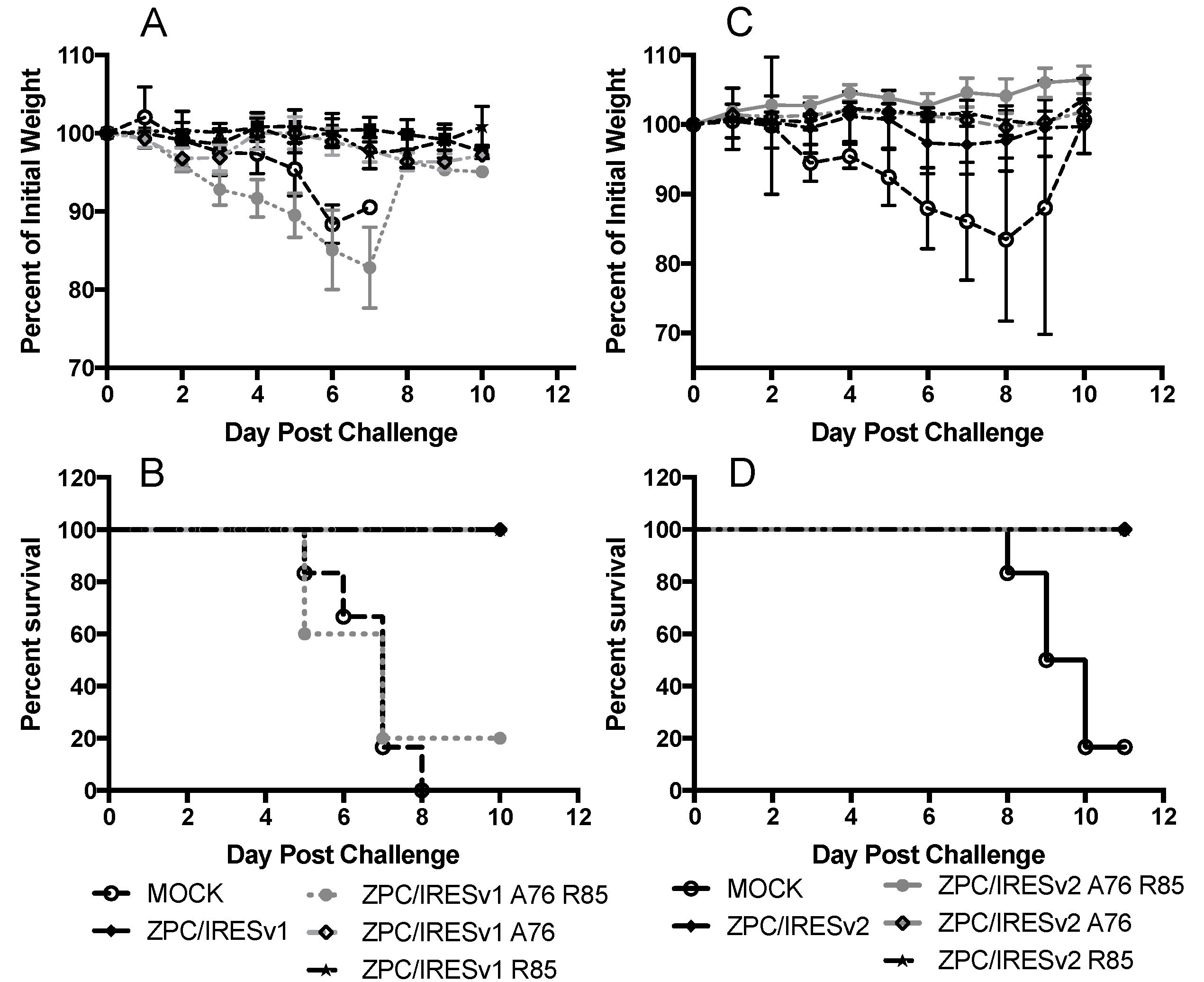
3.2. VEEV ZPC/IRES Are Immunogenic and Protective in Mice
3.3. In Vitro Stability
3.4. VEEV ZPC/IRES Are Immunogenic and Protective in Cynomolgus Macaques
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Weaver, S.; Ferro, C.; Barrera, R.; Boshell, J.; Navarro, J. Venezuelan equine encephalitis. Annu. Rev. Entomol. 2004, 49, 141–174. [Google Scholar] [CrossRef] [PubMed]
- Anishchenko, M.; Bowen, R.A.; Paessler, S.; Austgen, L.; Greene, I.P.; Weaver, S. Venezuelan encephalitis emergence mediated by a phylogenetically predicted viral mutation. Proc. Natl. Acad. Sci. USA 2006, 103, 4994–4999. [Google Scholar] [CrossRef] [PubMed]
- Weaver, S.; Salas, R.; Rico-Hesse, R.; Ludwig, G.V.; Oberste, M.S.; Boshell, J.; Tesh, R.B. Re-emergence of epidemic Venezuelan equine encephalomyelitis in South America. Lancet 1996, 348, 436–440. [Google Scholar] [CrossRef]
- Levine, B.A.; Nurudeen, S.K.; Gosselin, J.T.; Sauer, M.V.; Aguilar, P.V.; Estrada-Franco, J.G.; Navarro-Lopez, R.; Ferro, C.; Haddow, A.D.; Weaver, S. Addressing the fertility needs of HIV-seropositive males. Future Virol. 2011, 6, 299–306. [Google Scholar] [CrossRef] [PubMed]
- Forshey, B.M.; Guevara, C.; Laguna-Torres, V.A.; Céspedes, M.; Vargas, J.; Gianella, A.; Vallejo, E.; Madrid, C.; Aguayo, N.; Gotuzzo, E.; et al. Arboviral Etiologies of Acute Febrile Illnesses in Western South America, 2000–2007. PLoS Negl. Trop. Dis. 2010, 4, e787. [Google Scholar] [CrossRef] [PubMed]
- Rivas, F.; Diaz, L.A.; Cardenas, V.; Daza, E.; Bruzon, L.; Alcala, A.; De La Hoz, O.; Caceres, F.M.; Aristizabal, G.; Martínez, J.W.; et al. Epidemic Venezuelan Equine Encephalitis in La Guajira, Colombia, 1995. J. Infect. Dis. 1997, 175, 828–832. [Google Scholar] [CrossRef]
- Bronze, M.S.; Huycke, M.M.; Machado, L.J.; Voskuhl, G.W.; Greenfield, R.A. Viral Agents as Biological Weapons and Agents of Bioterrorism. Am. J. Med. Sci. 2002, 323, 316–325. [Google Scholar] [CrossRef]
- Berge, T.O.; Banks, I.S.; Tigertt, W.D. Attenuation of Venezuelan equine encephalomyelitis virus by in vitro cultivation in guinea pig heart cells. Am. J. Epidemiol. 1961, 73, 209–218. [Google Scholar] [CrossRef]
- Walton, T.E.; Alvarez, O.; Buckwalter, R.M.; Johnson, K.M. Experimental Infection of Horses with an Attenuated Venezuelan Equine Encephalomyelitis Vaccine (Strain TC-83). Infect. Immun. 1972, 5, 750–756. [Google Scholar] [CrossRef]
- Walton, T.E.; Luedke, A.J.; Jochim, M.M.; Crenshaw, G.L.; A Ferguson, J. Duration of immunity of horses vaccinated with strain TC-83 Venezuelan equine encephalomyelitis virus vaccine. Proc. Annu. Meet. US Anim. Health Assoc. 1973, 77, 196–202. [Google Scholar]
- Pittman, P.; Makuch, R.S.; Mangiafico, J.A.; Cannon, T.L.; Gibbs, P.H.; Peters, C.J. Long-term duration of detectable neutralizing antibodies after administration of live-attenuated VEE vaccine and following booster vaccination with inactivated VEE vaccine. Vaccine 1996, 14, 337–343. [Google Scholar] [CrossRef]
- Rayfield, E.J.; Gorelkin, L.; Curnow, R.T.; Jahrling, P.B. Virus-induced Pancreatic Disease by Venezuelan Encephalitis Virus: Alterations in Glucose Tolerance and Insulin Release. Diabetes 1976, 25, 623–631. [Google Scholar] [CrossRef] [PubMed]
- Bowen, G.S.; Field, E.J.R.; Monath, T.P.; Kemp, G.E. Studies of glucose metabolism in rhesus monkeys after venezuelan equine encephalitis virus infection. J. Med. Virol. 1980, 6, 227–234. [Google Scholar] [CrossRef]
- Kinney, R.M.; Chang, G.J.; Tsuchiya, K.R.; Sneider, J.M.; Roehrig, J.T.; Woodward, T.M.; Trent, D.W. Attenuation of Venezuelan equine encephalitis virus strain TC-83 is encoded by the 5′-noncoding region and the E2 envelope glycoprotein. J. Virol. 1993, 67, 1269–1277. [Google Scholar] [CrossRef] [PubMed]
- Davis, N.L.; Brown, K.W.; Greenwald, G.F.; Zajac, A.J.; Zacny, V.L.; Smith, J.F.; Johnston, R.E. Attenuated Mutants of Venezuelan Equine Encephalitis Virus Containing Lethal Mutations in the PE2 Cleavage Signal Combined with a Second-Site Suppressor Mutation in E1. Virology 1995, 212, 102–110. [Google Scholar] [CrossRef] [PubMed]
- Kenney, J.L.; Volk, S.M.; Pandya, J.; Wang, E.; Liang, X.; Weaver, S. Stability of RNA virus attenuation approaches. Vaccine 2011, 29, 2230–2234. [Google Scholar] [CrossRef][Green Version]
- Martin, S.S.; Bakken, R.R.; Lind, C.M.; García, P.; Jenkins, E.; Glass, P.J.; Parker, M.D.; Hart, M.K.; Fine, D.L. Evaluation of formalin inactivated V3526 virus with adjuvant as a next generation vaccine candidate for Venezuelan equine encephalitis virus. Vaccine 2010, 28, 3143–3151. [Google Scholar] [CrossRef][Green Version]
- Dupuy, L.C.; Richards, M.J.; Ellefsen, B.; Chau, L.; Luxembourg, A.; Hannaman, D.; Livingston, B.D.; Schmaljohn, C.S. A DNA Vaccine for Venezuelan Equine Encephalitis Virus Delivered by Intramuscular Electroporation Elicits High Levels of Neutralizing Antibodies in Multiple Animal Models and Provides Protective Immunity to Mice and Nonhuman Primates. Clin. Vaccine Immunol. 2011, 18, 707–716. [Google Scholar] [CrossRef]
- Hannaman, D.; Dupuy, L.C.; Ellefsen, B.; Schmaljohn, C.S. A Phase 1 clinical trial of a DNA vaccine for Venezuelan equine encephalitis delivered by intramuscular or intradermal electroporation. Vaccine 2016, 34, 3607–3612. [Google Scholar] [CrossRef]
- Paessler, S.; Fayzulin, R.Z.; Anishchenko, M.; Greene, I.P.; Weaver, S.; Frolov, I. Recombinant Sindbis/Venezuelan Equine Encephalitis Virus Is Highly Attenuated and Immunogenic. J. Virol. 2003, 77, 9278–9286. [Google Scholar] [CrossRef]
- Volkova, E.; Frolova, E.; Darwin, J.R.; Forrester, N.L.; Weaver, S.; Frolov, I. IRES-dependent replication of Venezuelan equine encephalitis virus makes it highly attenuated and incapable of replicating in mosquito cells. Virology 2008, 377, 160–169. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Guerbois, M.; Volkova, E.; Forrester, N.L.; Rossi, S.L.; Frolov, I.; Weaver, S. IRES-driven Expression of the Capsid Protein of the Venezuelan Equine Encephalitis Virus TC-83 Vaccine Strain Increases Its Attenuation and Safety. PLoS Negl. Trop. Dis. 2013, 7, e2197. [Google Scholar] [CrossRef] [PubMed]
- Oberste, M.S.; Smith, J.F.; Schmura, S.M.; Weaver, S. Geographic distribution of Venezuelan equine encephalitis virus subtype IE genotypes in Central America and Mexico. Am. J. Trop. Med. Hyg. 1999, 60, 630–634. [Google Scholar] [CrossRef] [PubMed]
- Rossi, S.L.; Guerbois, M.; Gorchakov, R.; Plante, K.S.; Forrester, N.L.; Weaver, S. IRES-based Venezuelan equine encephalitis vaccine candidate elicits protective immunity in mice. Virology 2013, 437, 81–88. [Google Scholar] [CrossRef]
- Rossi, S.L.; Russell-Lodrigue, K.; Killeen, S.Z.; Wang, E.; Leal, G.; Bergren, N.A.; Vinet-Oliphant, H.; Weaver, S.; Roy, C.J. IRES-Containing VEEV Vaccine Protects Cynomolgus Macaques from IE Venezuelan Equine Encephalitis Virus Aerosol Challenge. PLoS Negl. Trop. Dis. 2015, 9, e0003797. [Google Scholar] [CrossRef]
- Oberste, M.S.; Fraire, M.; Kondig, J.F.; Zarate, M.L.; Weaver, S.; Ludwig, G.V.; Navarro, R.; Smith, J.F.; Rico-Hesse, R.; Zepeda, C. Association of Venezuelan equine encephalitis virus subtype IE with two equine epizootics in Mexico. Am. J. Trop. Med. Hyg. 1998, 59, 100–107. [Google Scholar] [CrossRef]
- Powers, A.M.; Oberste, M.S.; Brault, A.C.; Rico-Hesse, R.; Schmura, S.M.; Smith, J.F.; Kang, W.; Sweeney, W.P.; Weaver, S.C. Repeated emergence of epidemic/epizootic Venezuelan equine encephalitis from a single genotype of enzootic subtype ID virus. J. Virol. 1997, 71, 6697–6705. [Google Scholar] [CrossRef]
- Hart, M.K.; Lind, C.; Bakken, R.; Robertson, M.; Tammariello, R.; Ludwig, G.V. Onset and duration of protective immunity to IA/IB and IE strains of Venezuelan equine encephalitis virus in vaccinated mice. Vaccine 2001, 20, 616–622. [Google Scholar] [CrossRef]
- Reed, D.S.; Lind, C.M.; Lackemeyer, M.G.; Sullivan, L.J.; Pratt, W.D.; Parker, M.D. Genetically engineered, live, attenuated vaccines protect nonhuman primates against aerosol challenge with a virulent IE strain of Venezuelan equine encephalitis virus. Vaccine 2005, 23, 3139–3147. [Google Scholar] [CrossRef]
- Barrera, R.; Torres, N.; Freier, J.E.; Navarro, J.; García, C.Z.; Salas, R.; Vasquez, C.; Weaver, S. Characterization of Enzootic Foci of Venezuelan Equine Encephalitis Virus in Western Venezuela. Vector-Borne Zoonotic Dis. 2001, 1, 219–230. [Google Scholar] [CrossRef]
- Forrester, N.L.; Wertheim, J.O.; Dugan, V.G.; Auguste, A.J.; Lin, D.; Adams, A.P.; Chen, R.; Gorchakov, R.; Leal, G.; Estrada-Franco, J.G.; et al. Evolution and spread of Venezuelan equine encephalitis complex alphavirus in the Americas. PLoS Negl. Trop. Dis. 2017, 11, e0005693. [Google Scholar] [CrossRef] [PubMed]
- Anishchenko, M.; Paessler, S.; Greene, I.P.; Aguilar, P.V.; Carrara, A.-S.; Weaver, S. Generation and Characterization of Closely Related Epizootic and Enzootic Infectious cDNA Clones for Studying Interferon Sensitivity and Emergence Mechanisms of Venezuelan Equine Encephalitis Virus. J. Virol. 2004, 78, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Brault, A.C.; Powers, A.M.; Weaver, S. Vector Infection Determinants of Venezuelan Equine Encephalitis Virus Reside within the E2 Envelope Glycoprotein. J. Virol. 2002, 76, 6387–6392. [Google Scholar] [CrossRef] [PubMed]
- Roy, C.J.; Adams, A.P.; Wang, E.; Leal, G.; Seymour, R.L.; Sivasubramani, S.K.; Mega, W.; Frolov, I.; Didier, P.J.; Weaver, S. A chimeric Sindbis-based vaccine protects cynomolgus macaques against a lethal aerosol challenge of eastern equine encephalitis virus. Vaccine 2013, 31, 1464–1470. [Google Scholar] [CrossRef] [PubMed]
- Pandya, J.; Gorchakov, R.; Wang, E.; Leal, G.; Weaver, S. A vaccine candidate for eastern equine encephalitis virus based on IRES-mediated attenuation. Vaccine 2012, 30, 1276–1282. [Google Scholar] [CrossRef] [PubMed]
- Plante, K.; Wang, E.; Partidos, C.D.; Weger-Lucarelli, J.; Gorchakov, R.; Tsetsarkin, K.; Borland, E.M.; Powers, A.M.; Seymour, R.; Stinchcomb, D.T.; et al. Novel Chikungunya Vaccine Candidate with an IRES-Based Attenuation and Host Range Alteration Mechanism. PLoS Pathog. 2011, 7, e1002142. [Google Scholar] [CrossRef]
- Weise, W.J.; Hermance, M.E.; Forrester, N.; Adams, A.P.; Langsjoen, R.; Gorchakov, R.; Wang, E.; Alcorn, M.D.H.; Tsetsarkin, K.; Weaver, S. A Novel Live-Attenuated Vaccine Candidate for Mayaro Fever. PLoS Negl. Trop. Dis. 2014, 8, e2969. [Google Scholar] [CrossRef]
- Plante, K.S.; Rossi, S.L.; Bergren, N.A.; Seymour, R.L.; Weaver, S. Extended Preclinical Safety, Efficacy and Stability Testing of a Live-attenuated Chikungunya Vaccine Candidate. PLoS Negl. Trop. Dis. 2015, 9, e0004007. [Google Scholar] [CrossRef]
- Langsjoen, R.; Haller, S.L.; Roy, C.J.; Vinet-Oliphant, H.; Bergren, N.A.; Erasmus, J.H.; Livengood, J.A.; Powell, T.D.; Weaver, S.; Rossi, S.L. Chikungunya Virus Strains Show Lineage-Specific Variations in Virulence and Cross-Protective Ability in Murine and Nonhuman Primate Models. MBio 2018, 9, e02449-17. [Google Scholar] [CrossRef]
- Roy, C.J.; Adams, A.P.; Wang, E.; Plante, K.; Gorchakov, R.; Seymour, R.L.; Vinet-Oliphant, H.; Weaver, S. Chikungunya Vaccine Candidate Is Highly Attenuated and Protects Nonhuman Primates Against Telemetrically Monitored Disease Following a Single Dose. J. Infect. Dis. 2014, 209, 1891–1899. [Google Scholar] [CrossRef]
- Bear, J.S.; Byrnes, A.; Griffin, D.E. Heparin-binding and patterns of virulence for two recombinant strains of Sindbis virus. Virology 2006, 347, 183–190. [Google Scholar] [CrossRef] [PubMed]
- Klimstra, W.B.; Ryman, K.D.; Johnston, R.E. Adaptation of Sindbis Virus to BHK Cells Selects for Use of Heparan Sulfate as an Attachment Receptor. J. Virol. 1998, 72, 7357–7366. [Google Scholar] [CrossRef] [PubMed]
- Wang, E.; Brault, A.C.; Powers, A.M.; Kang, W.; Weaver, S. Glycosaminoglycan Binding Properties of Natural Venezuelan Equine Encephalitis Virus Isolates. J. Virol. 2003, 77, 1204–1210. [Google Scholar] [CrossRef] [PubMed]
| Position/Gene (Element) | 4449/nsP2 | 7242/nsP4 | 7995/IRES | 9300/E2 | 9327/E2 | 10925/E1 |
|---|---|---|---|---|---|---|
| Wild-type a | GTA | GTG | A | GAG | CAC | GAA |
| Replicate #1 | GTt b | GTa | T/A mix c | GcG | CgC | aAA |
| Replicate #2 | GTt | GTa | T/A mix | GcG | CgC | aAA |
| Replicate #3 | GTt | GTa | T/A mix | GcG | CgC | aAA |
| Mutation | Gly → Gly | Val → Val | n/a | Glu → Ala | His → Arg | Glu → Lys |
| Vaccine | PRNT80: 4-Weeks 1 | % Group Seroconvert | N | PRNT80: 20-Weeks | % Group Seroconvert | N |
|---|---|---|---|---|---|---|
| ZPC/IRESv1 | 40 ± 42.4 | 11/15 (73.3%) | 15 | 142.2 ± 225 | 5/8 (62.5%) | 8 |
| ZPC/IRESv2 | 60.7 ± 55.7 | 12/15 (80%) | 15 | 324 ± 241.8 | 10/10 (100%) | 10 |
| ZPC/IRESv1 A76, R85 | <LOD 2 | 1/10 (10%) | 10 | ND 3 | - | - |
| ZPC/IRESv2 A76, R85 | <LOD | 0/10 (0%) | 10 | ND | - | - |
| ZPC/IRESv1 A76 | 31 ± 27 | 5/10 (50%) | 10 | ND | - | - |
| ZPC/IRESv2 A76 | <LOD | 1/10 (10%) | 10 | ND | - | - |
| ZPC/IRESV1 R85 | 172 ± 372 | 6/10 (60%) | 10 | ND | - | - |
| ZPC/IRESV2 R85 | 36 ± 46.5 | 4/10 (40%) | 10 | ND | - | - |
| NHP # | Vaccination Status | PRNT80 1 35dpv | PRNT50 35dpv | Viremia 1 dpi (log10 PFU/mL)2 | Viremia 2 dpi (log10 PFU/mL) 2 | Viremia 3 dpi (log10 PFU/mL) 2 | Fever Hours |
|---|---|---|---|---|---|---|---|
| 1 | Sham-vaccinated | <20 | <20 | 4.30 | 3.78 | 2 | 150 |
| 2 | Sham-vaccinated | <20 | <20 | 2.69 | 3.70 | 3.70 | 136 |
| 3 | ZPC/IRESv1 | <20 | <20 | <2 | <2 | <2 | 107 |
| 4 | ZPC/IRESv1 | <20 | 40 | <2 | <2 | <2 | 10 |
| 5 | ZPC/IRESv1 | 20 | 20 | <2 | <2 | <2 | 110 |
| 6 | ZPC/IRESv1 | 20 | 160 | <2 | <2 | <2 | 0 |
| 7 | ZPC/IRESv1 | <20 | 20 | <2 | <2 | <2 | 0 |
| NHP # | Vaccination Status | PRNT80 1 28 dpv | PRNT50 28 dpv | Viremia 1 dpi (log10 PFU/mL) 2 | Viremia 2 dpi (log10 PFU/mL) 2 | Viremia 3 dpi (log10 PFU/mL) 2 |
|---|---|---|---|---|---|---|
| 8 | Sham-vaccinated | <20 | <20 | 3.6 | 3.3 | <1.3 |
| 9 | Sham-vaccinated | <20 | <20 | <1.3 | <1.3 | <1.3 |
| 10 | ZPC/IRESv2 | 320 | >640 | <1.3 | <1.3 | <1.3 |
| 11 | ZPC/IRESv2 | 160 | >640 | <1.3 | <1.3 | <1.3 |
| 12 | ZPC/IRESv2 | 320 | >640 | <1.3 | <1.3 | <1.3 |
| 13 | ZPC/IRESv2 | 320 | 320 | <1.3 | <1.3 | <1.3 |
| 14 | ZPC/IRESv2 | 320 | >640 | <1.3 | <1.3 | <1.3 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rossi, S.L.; Russell-Lodrigue, K.E.; Plante, K.S.; Bergren, N.A.; Gorchakov, R.; Roy, C.J.; Weaver, S.C. Rationally Attenuated Vaccines for Venezuelan Equine Encephalitis Protect Against Epidemic Strains with a Single Dose. Vaccines 2020, 8, 497. https://doi.org/10.3390/vaccines8030497
Rossi SL, Russell-Lodrigue KE, Plante KS, Bergren NA, Gorchakov R, Roy CJ, Weaver SC. Rationally Attenuated Vaccines for Venezuelan Equine Encephalitis Protect Against Epidemic Strains with a Single Dose. Vaccines. 2020; 8(3):497. https://doi.org/10.3390/vaccines8030497
Chicago/Turabian StyleRossi, Shannan L., Kasi E. Russell-Lodrigue, Kenneth S. Plante, Nicholas A. Bergren, Rodion Gorchakov, Chad J. Roy, and Scott C. Weaver. 2020. "Rationally Attenuated Vaccines for Venezuelan Equine Encephalitis Protect Against Epidemic Strains with a Single Dose" Vaccines 8, no. 3: 497. https://doi.org/10.3390/vaccines8030497
APA StyleRossi, S. L., Russell-Lodrigue, K. E., Plante, K. S., Bergren, N. A., Gorchakov, R., Roy, C. J., & Weaver, S. C. (2020). Rationally Attenuated Vaccines for Venezuelan Equine Encephalitis Protect Against Epidemic Strains with a Single Dose. Vaccines, 8(3), 497. https://doi.org/10.3390/vaccines8030497







