Health Literacy, Vaccine Confidence and Influenza Vaccination Uptake among Nursing Home Staff: A Cross-Sectional Study Conducted in Tuscany
Abstract
1. Introduction
- Does HL influence vaccination uptake among staff of NHs?
- Does vaccine confidence influence vaccination uptake among staff of NHs?
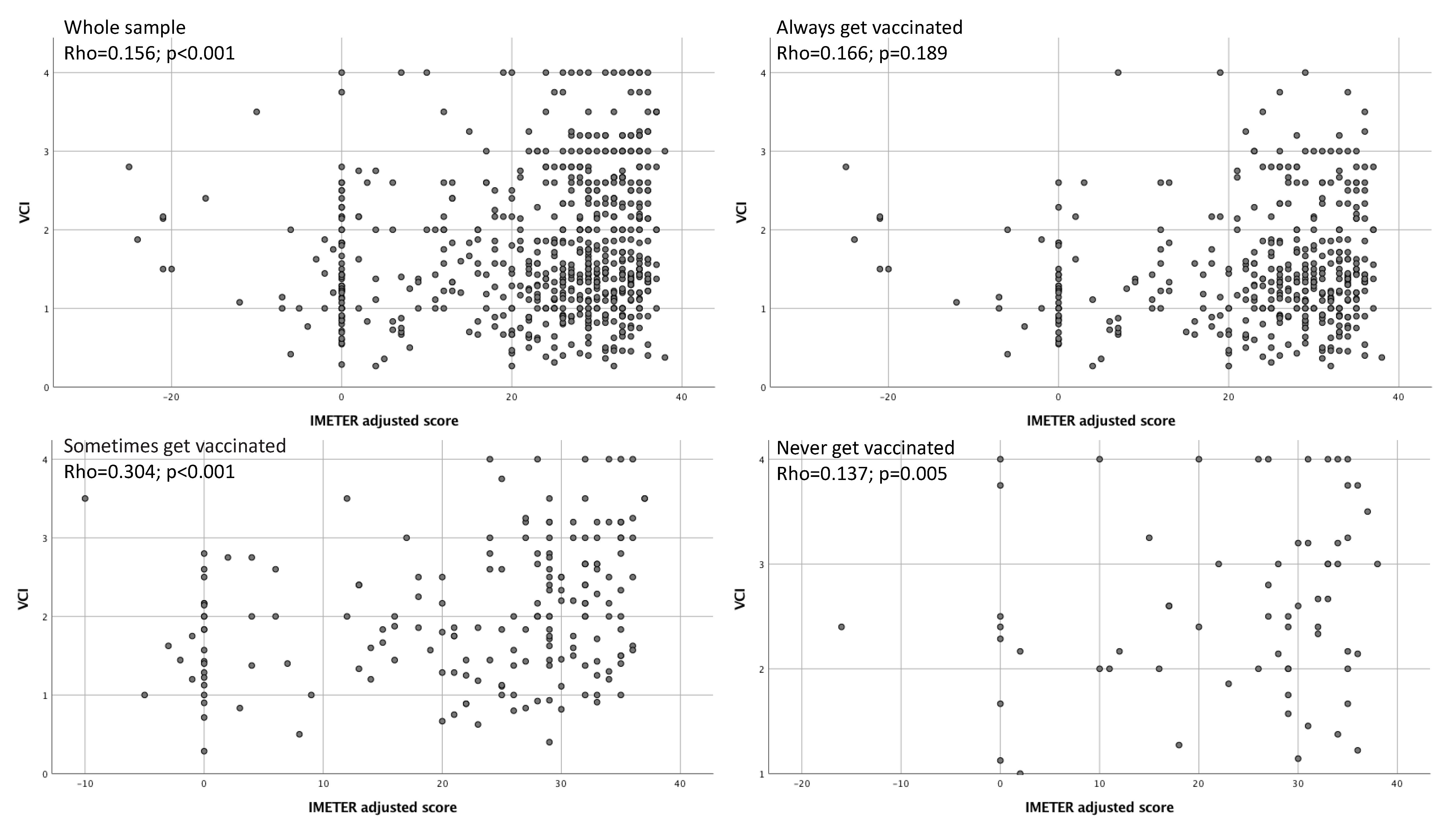
- Are HL and vaccine confidence related?
2. Materials and Methods
2.1. Questionnaires
2.2. Health Literacy Measure: The IMETER Test
2.3. Calculation of the Vaccine Confidence Index
- Influenza is a serious illness (A1)
- Influenza vaccine is effective (A2)
- Healthcare workers must get vaccinated (A3)
- By getting vaccinated I protect people close to me from influenza (A4)
- it is better to contract influenza than to get the vaccination (B1)
- Influenza vaccines have serious side effects (B2)
- Vaccine can cause influenza (B3)
- Opposed to vaccination (B4)
2.4. Statistical Analyses
3. Results
3.1. Characteristics of the Nursing Homes
3.2. Characteristics of the Staff
3.3. IMETER, VCI and Influenza Vaccination
4. Discussion
4.1. Influenza Vaccination
4.2. Health Literacy, Vaccine Confidence and Influenza Vaccination
4.3. Limitations of the Study
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Influenza Fact-Sheets. Available online: https://www.who.int/en/news-room/fact-sheets/detail/influenza-(seasonal) (accessed on 28 February 2020).
- Paget, J.; Spreeuwenberg, P.; Charu, V.; Taylor, R.J.; Iuliano, A.D.; Bresee, J.; Simonsen, L.; Viboud, C.; Global Seasonal Influenza-associated Mortality Collaborator Network and GLaMOR Collaborating Teams. Global mortality associated with seasonal influenza epidemics: New burden estimates and predictors from the GLaMOR Project. J. Global Health 2019, 9, 020421. [Google Scholar] [CrossRef] [PubMed]
- Gaspard, P.; Mosnier, A.; Simon, L.; Ali-Brandmeyer, O.; Rabaud, C.; Larocca, S.; Heck, B.; Aho-Glélé, S.; Pothier, P.; Ambert-Balay, K. Gastroenteritis and respiratory infection outbreaks in French nursing homes from 2007 to 2018: Morbidity and all-cause lethality according to the individual characteristics of residents. PLoS ONE 2019, 14, e0222321. [Google Scholar] [CrossRef] [PubMed]
- Diaz-Decaro, J.D.; Launer, B.; Mckinnell, J.A.; Singh, R.; Dutciuc, T.D.; Green, N.M.; Bolaris, M.; Huang, S.S.; Miller, L.G. Bayesian evidence and epidemiological implications of environmental contamination from acute respiratory infection in long-term care facilities. Epidemiol. Infect. 2018, 146, 832–838. [Google Scholar] [CrossRef] [PubMed]
- McConeghy, K.W.; Lee, Y.; Zullo, A.R.; Banerjee, G.; Daiello, L.; Dosa, D.; Kiel, D.P.; Mor, V.M.; Berry, S.D. Influenza Illness and Hip Fracture Hospitalizations in Nursing Home Residents: Are They Related? J. Gerontol. A Biol. Sci. Med. Sci. 2018, 73, 1638–1642. [Google Scholar] [CrossRef] [PubMed]
- Pop-Vicas, A.; Gravenstein, S. Influenza in the elderly: A mini-review. Gerontology 2011, 57, 397–404. [Google Scholar] [CrossRef] [PubMed]
- Vetrano, D.L.; Collamati, A.; Magnavita, N.; Sowa, A.; Topinkova, E.; Finne-Soveri, H.; van der Roest, H.G.; Tobiasz-Adamczyk, B.; Giovannini, S.; Ricciardi, W.; et al. Health determinants and survival in nursing home residents in Europe: Results from the SHELTER study. Maturitas 2018, 107, 19–25. [Google Scholar] [CrossRef]
- Poscia, A.; Collamati, A.; Carfì, A.; Topinkova, E.; Richter, T.; Denkinger, M.; Pastorino, R.; Landi, F.; Ricciardi, W.; Bernabei, R.; et al. Influenza and pneumococcal vaccination in older adults living in nursing home: A survival analysis on the shelter study. Eur. J. Public Health 2017, 27, 1016–1020. [Google Scholar] [CrossRef]
- Pop-Vicas, A.; Rahman, M.; Gozalo, P.L.; Gravenstein, S.; Mor, V. Estimating the Effect of Influenza Vaccination on Nursing Home Residents’ Morbidity and Mortality. J. Am. Geriatr. Soc. 2015, 63, 1798–1804. [Google Scholar] [CrossRef]
- Smetana, J.; Chlibek, R.; Shaw, J.; Splino, M.; Prymula, R. Influenza vaccination in the elderly. Hum. Vaccines Immunother. 2018, 14, 540–549. [Google Scholar] [CrossRef]
- Frentzel, E.; Jump, R.L.P.; Archbald-Pannone, L.; Nace, D.A.; Schweon, S.J.; Gaur, S.; Naqvi, F.; Pandya, N.; Mercer, W. Infection Advisory Subcommittee of AMDA, The Society for Post-Acute and Long-Term Care Medicine. Recommendations for Mandatory Influenza Vaccinations for Health Care Personnel from AMDA’s Infection Advisory Subcommittee. J. Am. Med. Dir. Assoc. 2020, 21, 25–28.e2. [Google Scholar] [CrossRef]
- Daugherty, J.D.; Blake, S.C.; Grosholz, J.M.; Omer, S.B.; Polivka-West, L.; Howard, D.H. Influenza vaccination rates and beliefs about vaccination among nursing home employees. Am. J. Infect. Control 2015, 43, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Borgey, F.; Henry, L.; Lebeltel, J.; Lescure, P.; Le Coutour, X.; Vabret, A.; Verdon, R.; Thibon, P. Effectiveness of an intervention campaign on influenza vaccination of professionals in nursing homes: A cluster-randomized controlled trial. Vaccine 2019, 37, 1260–1265. [Google Scholar] [CrossRef] [PubMed]
- Looijmans-van den Akker, I.; van Delden, J.J.; Verheij, T.J.; van der Sande, M.A.; van Essen, G.A.; Riphagen-Dalhuisen, J.; Hulscher, M.E.; Hak, E. Effects of a multi-faceted program to increase influenza vaccine uptake among health care workers in nursing homes: A cluster randomised controlled trial. Vaccine 2010, 28, 5086–5092. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Report of the SAGE Working Group on Vaccine Hesitancy. Available online: https://www.who.int/immunization/sage/meetings/2014/october/1_Report_WORKING_GROUP_vaccine_hesitancy_final.pdf (accessed on 28 February 2020).
- Paoli, S.; Lorini, C.; Puggelli, F.; Sala, A.; Grazzini, M.; Paolini, D.; Bonanni, P.; Bonaccorsi, G. Assessing Vaccine Hesitancy among Healthcare Workers: A Cross-Sectional Study at an Italian Paediatric Hospital and the Development of a Healthcare Worker’s Vaccination Compliance Index. Vaccines 2019, 7, 201. [Google Scholar] [CrossRef] [PubMed]
- Wilson, R.J.; Paterson, P.; Jarrett, C.; Larson, H.J. Understanding factors influencing vaccination acceptance during pregnancy globally: A literature review. Vaccine 2015, 33, 6420–6429. [Google Scholar] [CrossRef]
- Karafillakis, E.; Simas, C.; Jarrett, C.; Verger, P.; Peretti-Watel, P.; Dib, F.; De Angelis, S.; Takacs, J.; Ali, K.A.; Pastore Celentano, L.; et al. HPV vaccination in a context of public mistrust and uncertainty: A systematic literature review of determinants of HPV vaccine hesitancy in Europe. Hum. Vaccines Immunother. 2019, 15, 1615–1627. [Google Scholar] [CrossRef]
- Larson, H.; de Figueiredo, A.; Karafillakis, E.; Rawal, M. State of Vaccine Confidence in the EU 2018; European Commission: Luxembourg, 2018. [Google Scholar]
- Larson, H.J.; Schulz, W.S.; Tucker, J.D.; Smith, D.M. Measuring vaccine confidence: Introducing a global vaccine confidence index. PLoS Curr. 2015, 7. [Google Scholar] [CrossRef]
- Kickbusch, I.S. Health literacy: Addressing the health and education divide. Health Promot. Int. 2001, 16, 289–297. [Google Scholar] [CrossRef]
- Sørensen, K.; Van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H.; Consortium Health Literacy Project European. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef]
- Levin-Zamir, D.; Leung, A.Y.M.; Dodson, S.; Rowlands, G. Health literacy in Selected Populations: Individuals, Families and Communities from the International and Cultural Perspective. Stud. Health Technol. Inform. 2017, 240, 392–414. [Google Scholar] [CrossRef]
- Nutbeam, D.; Levin-Zamir, D.; Rowlands, G. Health Literacy in Context. Int. J. Environ. Res. Public Health 2018, 15, 2657. [Google Scholar] [CrossRef] [PubMed]
- Ratzan, S.C. Vaccine literacy: A new shot for advancing health. J. Health Commun. 2011, 16, 227–229. [Google Scholar] [CrossRef] [PubMed]
- Lorini, C.; Santomauro, F.; Donzellini, M.; Capecchi, L.; Bechini, A.; Boccalini, S.; Bonanni, P.; Bonaccorsi, G. Health literacy and vaccination: A systematic review. Hum. Vaccines Immunother. 2018, 14, 478–488. [Google Scholar] [CrossRef] [PubMed]
- Biasio, L.R. Vaccine literacy is undervalued. Hum. Vaccines Immunother. 2019, 15, 2552–2553. [Google Scholar] [CrossRef] [PubMed]
- Bonaccorsi, G.; Lorini, C.; Santomauro, F.; Guarducci, S.; Pellegrino, E.; Puggelli, F.; Balli, M.; Bonanni, P. Predictive factors associated with the acceptance of pandemic and seasonal influenza vaccination in health care workers and students in Tuscany, Central Italy. Hum. Vaccines Immunother. 2013, 9, 2603–2612. [Google Scholar] [CrossRef]
- Bonaccorsi, G.; Lorini, C.; Porchia, B.R.; Niccolai, G.; Martino, G.; Giannarelli, L.; Santomauro, F. Influenza vaccination: Coverage and risk perception among students of the health professions at Florence University, Italy. Ann. Ig. 2013, 25, 181–189. [Google Scholar] [CrossRef]
- Bonaccorsi, G.; Santomauro, F.; Porchia, B.R.; Niccolai, G.; Pellegrino, E.; Bonanni, P.; Lorini, C. Beliefs and Opinions of Health Care Workers and Students Regarding Influenza and Influenza Vaccination in Tuscany, Central Italy. Vaccines 2015, 3, 137–147. [Google Scholar] [CrossRef]
- Biasio, L.R.; Corbellini, G.; D’Alessandro, D. An Italian validation of “meter”, an easy-to-use Health Literacy (hl) screener. Ann. Ig. 2017, 29, 171–178. [Google Scholar] [CrossRef]
- Biasio, L.R.; Lorini, C.; Abbattista, G.; Bozzola, E.; De Castro, P.; Della Seta, M.; Villani, A.; Bonaccorsi, G. Assessment of health literacy skills in family doctors’ patients by two brief, self-administered Italian measures. Annali dell’Istituto Superiore di Sanità 2018, 54, 214–222. [Google Scholar] [CrossRef]
- Rawson, K.A.; Gunstad, J.; Hughes, J.; Spitznagel, M.B.; Potter, V.; Waechter, D.; Rosneck, J. The METER: A brief, self-administered measure of health literacy. J. Gen. Intern. Med. 2009, 25, 67–71. [Google Scholar] [CrossRef]
- Nutbeam, D. Health literacy as a public goal: A challenge for contemporary health education and communication strategies into the 21st century. Health Promot. Int. 2000, 15, 259–267. [Google Scholar] [CrossRef]
- Black, C.L.; Yue, X.; Ball, S.W.; Fink, R.; de Perio, M.A.; Laney, A.S.; Williams, W.W.; Lindley, M.C.; Graitcer, S.B.; Lu, P.J.; et al. Influenza Vaccination Coverage Among Health Care Personnel - United States, 2016-17 Influenza Season. MMWR Morb. Mortal. Wkly. Rep. 2017, 66, 1009–1015. [Google Scholar] [CrossRef] [PubMed]
- Bonaccorsi, G.; Pieralli, F.; Innocenti, M.; Milani, C.; Del Riccio, M.; Bechini, A.; Boccalini, S.; Bonanni, P.; Lorini, C. Non-familial paid caregivers as potential flu carriers and cause of spread: The primary prevention of flu measured through their adhesion to flu vaccination campaigns-A Florentine experience. Hum. Vaccines Immunother. 2019, 15, 2416–2422. [Google Scholar] [CrossRef] [PubMed]
- Bonaccorsi, G.; Lastrucci, V.; Vettori, V.; Lorini, C.; Florence Health Literacy Research Group. Functional health literacy in a population-based sample in Florence: A cross-sectional study using the Newest Vital Sign. BMJ Open 2019, 9, e026356. [Google Scholar] [CrossRef]
- Bonaccorsi, G.; Pieralli, F.; Innocenti, M.; Milani, C.; Del Riccio, M.; Donzellini, M.; Baggiani, L.; Lorini, C. Health Literacy among Non-Familial Caregivers of Older Adults: A Study Conducted in Tuscany (Italy). Int. J. Environ. Res. Public Health 2019, 16, 3771. [Google Scholar] [CrossRef]
- Lindquist, L.A.; Jain, N.; Tam, K.; Martin, G.J.; Baker, D.W. Inadequate health literacy among paid caregivers of seniors. J. Gen. Intern. Med. 2011, 26, 474–479. [Google Scholar] [CrossRef]
- Castro-Sánchez, E.; Vila-Candel, R.; Soriano-Vidal, F.J.; Navarro-Illana, E.; Díez-Domingo, J. Influence of health literacy on acceptance of influenza and pertussis vaccinations: A cross-sectional study among Spanish pregnant women. BMJ Open 2018, 8, e022132. [Google Scholar] [CrossRef]
- Kim, K.; Han, H.R. Potential links between health literacy and cervical cancer screening behaviors: A systematic review. Psychooncology 2016, 25, 122–130. [Google Scholar] [CrossRef]
- Lim, S.; Beauchamp, A.; Dodson, S.; O’Hara, J.; McPhee, C.; Fulton, A.; Wildey, C.; Osborne, R.H. Health literacy and fruit and vegetable intake in rural Australia. Public Health Nutr. 2017, 20, 2680–2684. [Google Scholar] [CrossRef]
- Guntzviller, L.M.; King, A.J.; Jensen, J.D.; Davis, L.A. Self-Efficacy, Health Literacy, and Nutrition and Exercise Behaviors in a Low-Income, Hispanic Population. J. Immigr. Minor. Health 2017, 19, 489–493. [Google Scholar] [CrossRef]
- Altin, S.V.; Finke, I.; Kautz-Freimuth, S.; Stock, S. The evolution of health literacy assessment tools: A systematic review. BMC Public Health 2014, 14, 1207. [Google Scholar] [CrossRef] [PubMed]
| Variables | Range | Centiles | ||
|---|---|---|---|---|
| 25° | 50° | 75° | ||
| Number of residents | 17–118 | 32 | 43 | 59 |
| Staff (total) | 22–146 | 32.7 | 50 | 62.7 |
| Staff: number of | ||||
| Medical doctors * | 0–1 | 0 | 0 | 0 |
| Nurses | 3–14 | 4 | 5.5 | 7.5 |
| Physiotherapists | 1–4 | 1 | 2 | 2.7 |
| Assistants/aides | 11–91 | 19.2 | 22.5 | 29.7 |
| Health educators | 1–5 | 1 | 2 | 2 |
| Cleaning staff | 1–14 | 2.2 | 3.5 | 6.7 |
| Other nonclinical staff | 0–19 | 1.2 | 6 | 7 |
| Percentage of vaccinated residents against influenza | 22.5–100 | 79 | 89 | 97 |
| Percentage of respondents among staff members | 15.2–92.1 | 30.1 | 51.5 | 67.4 |
| N | % | |||
| Mean time of stay of the residents | ||||
| 12 months or less | 2 | 7.1 | ||
| More than 12 months | 26 | 92.9 | ||
| Ownership type | ||||
| Public | 14 | 50 | ||
| Private for-profit | 5 | 17.9 | ||
| Private not-for-profit | 9 | 32.1 | ||
| Variables | Total Sample | Reported Influenza Vaccination Uptake (Row Percentage) * | ||||
|---|---|---|---|---|---|---|
| N | %# | Always Gets Vaccinated N = 68; 9.6%) | Sometimes Gets Vaccinated (N = 199; 28%) | Never Gets Vaccinated (N = 441; 62.1%) | P-Value (Chi2 Test) | |
| Sex | ||||||
| Males | 106 | 14.9 | 11.3 | 32.1 | 56.6 | 0.406 |
| Females | 569 | 80.1 | 9 | 27.6 | 63.4 | |
| Mother Language | ||||||
| Italian | 585 | 82.4 | 9.6 | 27.1 | 63.4 | 0.329 |
| Others | 64 | 9.0 | 4.7 | 32.8 | 62.5 | |
| Educational level | ||||||
| Less than high school diploma | 180 | 25.4 | 11.1 | 26.1 | 62.8 | 0.884 |
| High school degree | 308 | 43.3 | 8.4 | 28.6 | 63 | |
| Bachelor’s degree and higher | 183 | 25.8 | 9.8 | 26.8 | 63.4 | |
| Qualification | ||||||
| Nurses | 93 | 13.1 | 12.9 | 32.3 | 54.8 | 0.407 |
| Physiotherapists | 37 | 5.2 | 8.1 | 18.9 | 73 | |
| Assistants/aides | 364 | 51.3 | 7.7 | 29.5 | 62.8 | |
| Health educators | 25 | 3.5 | 20 | 16 | 64 | |
| Other clinical staff | 40 | 5.6 | 7.5 | 27.5 | 65 | |
| Cleaning staff | 45 | 6.3 | 8.9 | 31.1 | 60 | |
| Other nonclinical staff | 60 | 8.5 | 15 | 25 | 60 | |
| Living with ° | ||||||
| Children of less than 9 years | 142 | 20 | 8.5 | 28.9 | 62.7 | 0.742 |
| Elderly people | 137 | 19.3 | 14.7 | 31.6 | 53.7 | 0.014 |
| People with chronic diseases | 74 | 10.4 | 12.2 | 35.1 | 52.7 | 0.109 |
| At least one of the previously listed condition | 288 | 40.6 | 11.8 | 32.2 | 56.1 | 0.017 |
| Suffering from ° | ||||||
| Cardiovascular chronic diseases | 9 | 1.3 | 0 | 33.3 | 66.7 | 0.581 |
| Respiratory chronic diseases | 53 | 7.5 | 15.1 | 30.2 | 54.7 | 0.294 |
| Renal chronic diseases | 5 | 0.7 | 60 | 0 | 40 | 0.001 |
| Diabetes | 13 | 1.8 | 7.7 | 15.4 | 76.9 | 0.599 |
| Autoimmune diseases | 43 | 6 | 9.3 | 44.2 | 46.5 | 0.028 |
| At least one of the previously listed disease | 106 | 14.9 | 11.3 | 34 | 54.7 | 0.142 |
| Health literacy level (IMETER adjusted-score) | ||||||
| Low HL | 194 | 27.3 | 11.9 | 31.6 | 56.5 | 0.176 |
| Marginal HL | 430 | 60.6 | 34 | 26.6 | 65.5 | |
| Functional HL | 86 | 12.1 | 11 | 27.9 | 59.3 | |
| Reported influenza vaccine uptake | ||||||
| 2016–2017 | 114 | 16 | - | - | - | - |
| 2017–2018 | 118 | 16.6 | - | - | - | |
| Intention to vaccine uptake in 2018–2019 | 202 | 28.4 | - | - | - | |
| Vaccine uptake in 2016–2017, 2017–2018 and intention to vaccinate in 2018–2019 | 68 | 9.6 | - | - | - | |
| Variables | Total Sample | Influenza Vaccination | |||||
|---|---|---|---|---|---|---|---|
| Mean ± SD | Median | Range | Always Get Vaccinated (N = 68; 9.6%) Mean ± SD; Median | Sometimes Get Vaccinated (N = 199; 28%) Mean ± SD; Median | Never Get Vaccinated (N = 441; 62.1%) Mean ± SD; Median | P Value (Kruskal Wallis Test) | |
| Age (years) | 43.3 ± 11 | 44 | [20; 70] | 44.6 ± 12.6; 47 | 43.4 ± 11.4; 45.5 | 43 ± 10.6; 43 | 0.473 |
| Self-perceived health status (score) | 8.1 ± 1.6 | 8 | [1; 10] | 8 ± 1.6; 8 | 8.2 ± 1.5; 8 | 8.14 ± 1.6; 8 | 0.825 |
| IMETER adjusted-score | 23.4 ± 12.3 | 28 | [−25; 38] | 23.2 ± 12.9; 29 | 22.8 ± 12.1; 28 | 23.7 ± 12.4; 28 | 0.649 |
| VCI score | 1.7 ± 0.9 | 1.5 | [0.3; 4] | 2.6 ± 0.9; 2.5 | 2 ± 0.8; 2 | 1.5 ± 0.7; 1.3 | <0.001 |
| Reported Influenza Vaccination Uptake * | Variables | RRR | P > z | [95% Confidence Interval] |
|---|---|---|---|---|
| Never (reference) | - | 1 | - | - |
| Sometimes | Suffering from renal chronic diseases | 4.40 × 10−7 | 0.996 | 0 |
| Suffering from autoimmune diseases | 2.56 | 0.043 | [1.03; 6.36] | |
| Living with elderly people | 1.37 | 0.304 | [0.75; 2.48] | |
| IMETER adjusted-score | 0.99 | 0.195 | [0.97; 1.01] | |
| VCI | 2.84 | 0.000 | [2.10; 3.84] | |
| Cons | 0.10 | <0.001 | [0.03; 0.36] | |
| Always | Suffering from renal chronic diseases | 56.6 | 0.003 | [4.13; 774.53] |
| Suffering from autoimmune diseases | 0.95 | 0.952 | [0.18; 5.02] | |
| Living with elderly people | 3.46 | 0.003 | [1.53; 7.83] | |
| IMETER adjusted-score | 0.98 | 0.315 | [0.95; 1.01] | |
| VCI | 5.69 | 0.000 | [3.58; 9.05] | |
| Cons | 0.003 | <0.001 | [0.001; 0.026] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lorini, C.; Collini, F.; Gasparini, F.; Paolini, D.; Grazzini, M.; Ierardi, F.; Galletti, G.; Zanobini, P.; Gemmi, F.; Bonaccorsi, G. Health Literacy, Vaccine Confidence and Influenza Vaccination Uptake among Nursing Home Staff: A Cross-Sectional Study Conducted in Tuscany. Vaccines 2020, 8, 154. https://doi.org/10.3390/vaccines8020154
Lorini C, Collini F, Gasparini F, Paolini D, Grazzini M, Ierardi F, Galletti G, Zanobini P, Gemmi F, Bonaccorsi G. Health Literacy, Vaccine Confidence and Influenza Vaccination Uptake among Nursing Home Staff: A Cross-Sectional Study Conducted in Tuscany. Vaccines. 2020; 8(2):154. https://doi.org/10.3390/vaccines8020154
Chicago/Turabian StyleLorini, Chiara, Francesca Collini, Francesca Gasparini, Diana Paolini, Maddalena Grazzini, Francesca Ierardi, Giacomo Galletti, Patrizio Zanobini, Fabrizio Gemmi, and Guglielmo Bonaccorsi. 2020. "Health Literacy, Vaccine Confidence and Influenza Vaccination Uptake among Nursing Home Staff: A Cross-Sectional Study Conducted in Tuscany" Vaccines 8, no. 2: 154. https://doi.org/10.3390/vaccines8020154
APA StyleLorini, C., Collini, F., Gasparini, F., Paolini, D., Grazzini, M., Ierardi, F., Galletti, G., Zanobini, P., Gemmi, F., & Bonaccorsi, G. (2020). Health Literacy, Vaccine Confidence and Influenza Vaccination Uptake among Nursing Home Staff: A Cross-Sectional Study Conducted in Tuscany. Vaccines, 8(2), 154. https://doi.org/10.3390/vaccines8020154







