Utility of Healthcare System-Based Interventions in Improving the Uptake of Influenza Vaccination in Healthcare Workers at Long-Term Care Facilities: A Systematic Review
Abstract
1. Introduction
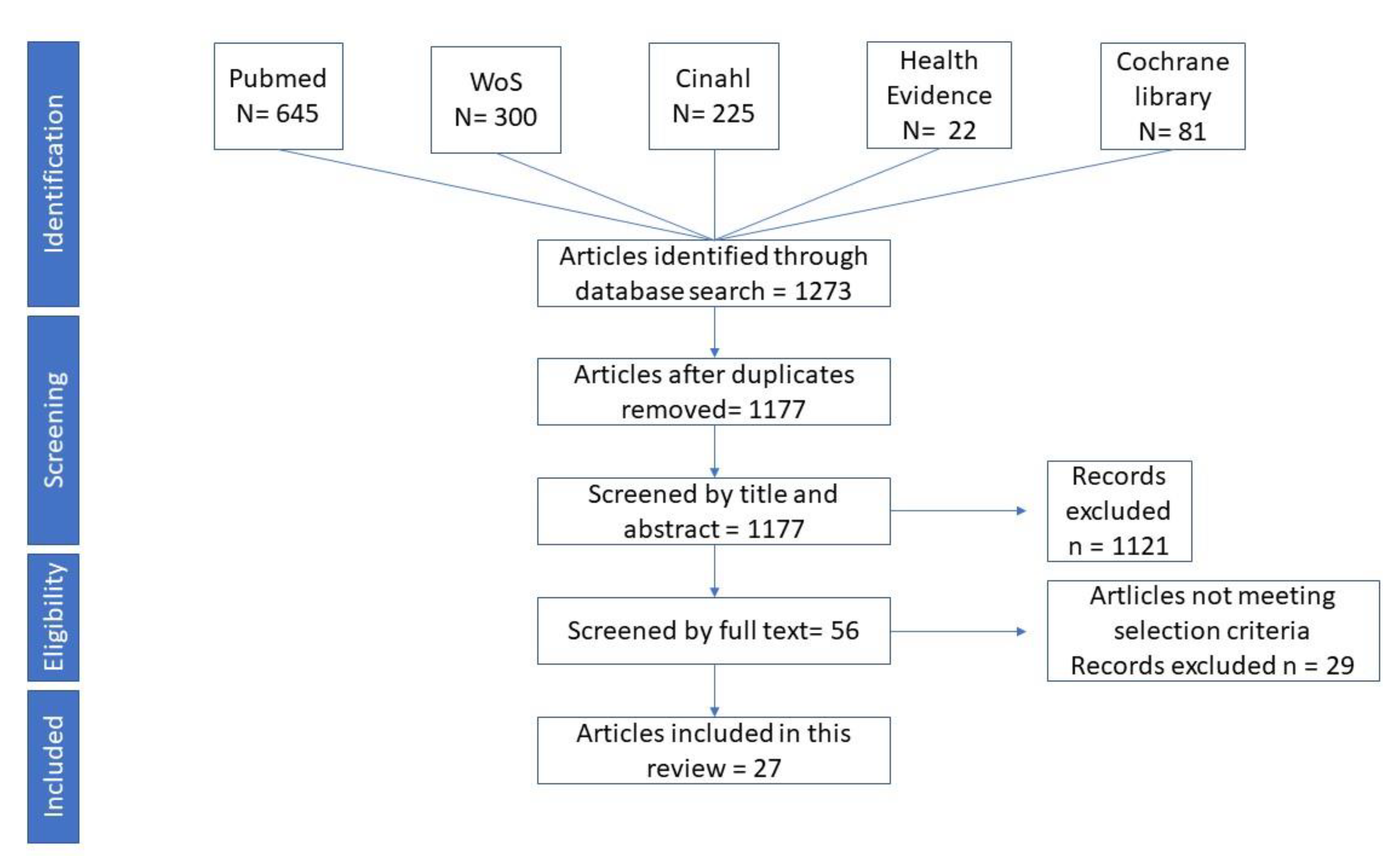
2. Materials and Methods
2.1. Search Strategy
2.2. Definition of HCWs, LTCFs, Type of Intervention
- (a)
- Interventions aimed at enhancing access to vaccination services (expanded access in healthcare settings, reduced or free vaccination costs, on-site vaccination, etc.),
- (b)
- Interventions to eliminate individual barriers (reminder and recall systems, education, incentives, etc.),
- (c)
- Policy/leadership interventions directed to mandate vaccination coverage in HCWs (mandatory vaccination as a condition for employment, severe restrictions for unvaccinated HCWs, declination forms, etc.).
2.3. Quality Assessment
3. Results
3.1. General Description of the Collected Studies
3.2. Type of Interventions
3.3. Studies with Interventions Related to One Area
3.4. Studies with Interventions Related to Two Areas
3.5. Studies with Interventions Related to Three Areas
4. Discussion
4.1. General Issue
4.2. Main Considerations about the Results
4.3. Strengths and Weaknesses
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Iuliano, A.D.; Roguski, K.M.; Chang, H.H.; Muscatello, D.J.; Palekar, R.; Tempia, S.; Cohen, C.; Gran, J.M.; Schanzer, D.; Cowling, B.J.; et al. Global Seasonal Influenza-associated Mortality Collaborator Network. Estimates of global seasonal influenza-associated respiratory mortality: A modelling study. Lancet 2018, 391, 1285–1300. [Google Scholar] [CrossRef]
- WHO. Influenza (Seasonal) Fact Sheet. Available online: http://www.who.int/mediacentre/factsheets/fs211/en/ (accessed on 4 February 2019).
- Redlberger-Fritz, M.; Aberle, J.H.; Popow-Kraupp, T.; Kundi, M. Attributable deaths due to influenza: A comparative study of seasonal and pandemic influenza. Eur. J. Epidemiol. 2012, 27, 567–575. [Google Scholar] [CrossRef] [PubMed]
- Vaccines against influenza WHO position paper—November 2012. Wkly. Epidemiol. Rec. 2012, 87, 461–476.
- Michiels, B.; Govaerts, F.; Remmen, R.; Vermeire, E.; Coenen, S. A systematic review of the evidence on the effectiveness and risks of inactivated influenza vaccines in different target groups. Vaccine 2011, 29, 9159–9170. [Google Scholar] [CrossRef] [PubMed]
- Vellozzi, C.; Burwen, D.R.; Dobardzic, A.; Ball, R.; Walton, K.; Haber, P. Safety of trivalent inactivated influenza vaccines in adults: Background for pandemic influenza vaccine safety monitoring. Vaccine 2009, 27, 2114–2120. [Google Scholar] [CrossRef] [PubMed]
- Kuster, S.P.; Shah, P.S.; Coleman, B.L.; Lam, P.P.; Tong, A.; Wormsbecker, A.; McGeer, A. Incidence of influenza in healthy adults and healthcare workers: A systematic review and meta-analysis. PLoS ONE 2011, 6, e26239. [Google Scholar] [CrossRef]
- Salgado, C.D.; Farr, B.M.; Hall, K.K.; Hayden, F.G. Influenza in the acute hospital setting. Lancet Infect. Dis. 2002, 2, 145–155. [Google Scholar] [CrossRef]
- Bridges, C.B.; Kuehnert, M.J.; Hall, C.B. Transmission of influenza: Implications for control in health care settings. Clin. Infect. Dis. 2003, 37, 1094–1101. [Google Scholar]
- Bonanni, P.; Boccalini, S.; Zanobini, P.; Dakka, N.; Lorini, C.; Santomauro, F.; Bechini, A. The appropriateness of the use of influenza vaccines: Recommendations from the latest seasons in Italy. Hum. Vaccines Immunother. 2018, 14, 699–705. [Google Scholar] [CrossRef]
- Public Health England Sets Country Rules for Effective Flu Prevention: An Example to Follow for Italian Regions. Available online: https://www.bmj.com/content/360/bmj.k602/rr (accessed on 4 April 2020).
- Boccalini, S.; Tacconi, F.M.; Lai, P.L.; Bechini, A.; Bonanni, P.; Panatto, D. Appropriateness and preferential use of different seasonal influenza vaccines: A pilot study on the opinion of vaccinating physicians in Italy. Vaccine 2019, 37, 915–918. [Google Scholar] [CrossRef]
- Bonanni, P.; Bonaccorsi, G.; Lorini, C.; Santomauro, F.; Tiscione, E.; Boccalini, S.; Bechini, A. Focusing on the implementation of 21st century vaccines for adults. Vaccine 2018, 36, 5358–5365. [Google Scholar] [CrossRef]
- Bridges, C.B.; Thompson, W.W.; Meltzer, M.I.; Reeve, G.R.; Talamonti, W.J.; Cox, N.J.; Lilac, H.A.; Hall, H.; Klimov, A.; Fukuda, K. Effectiveness and cost-benefit of influenza vaccination of healthy working adults: A randomized controlled trial. JAMA 2000, 284, 1655–1663. [Google Scholar] [CrossRef]
- UN Population Division. World Population Prospects 2019. Available online: https://population.un.org/wpp/ (accessed on 4 February 2019).
- Rivetti, D.; Jefferson, T.; Thomas, R.; Rudin, M.; Rivetti, A.; Di Pietrantonj, C.; Demicheli, V. Vaccines for preventing influenza in the elderly. Cochrane Database Syst. Rev. 2006, 3, CD004876. [Google Scholar]
- Demicheli, V.; Jefferson, T.; Di Pietrantonj, C.; Ferroni, E.; Thorning, S.; Thomas, R.E.; Rivetti, A. Vaccines for preventing influenza in the elderly. Cochrane Database Syst. Rev. 2018, 2, CD004876. [Google Scholar] [CrossRef]
- Bonanni, P.; Boccalini, S.; Bechini, A. The expected impact of new vaccines and vaccination policies. J. Public Health 2008, 16, 253–259. [Google Scholar] [CrossRef]
- Thomas, R.E.; Jefferson, T.; Lasserson, T.J. Influenza vaccination for healthcare workers who care for people aged 60 or older living in long-term care institutions. Cochrane Database Syst. Rev. 2016, 6, CD005187. [Google Scholar] [CrossRef]
- Ridgway, J.P.; Bartlett, A.H.; Garcia-Houchins, S.; Cariño, S.; Enriquez, A.; Marrs, R.; Perez, C.; Shah, M.; Guenette, C.; Mosakowski, S.; et al. Influenza among afebrile and vaccinated healthcare workers. Clin. Infect. Dis. 2015, 60, 1591–1595. [Google Scholar] [CrossRef] [PubMed]
- Taylor, G.; Mitchell, R.; McGeer, A.; Frenette, C.; Suh, K.N.; Wong, A.; Katz, K.; Wilkinson, K.; Amihod, B.; Gravel, D.; et al. Healthcare-associated influenza in Canadian hospitals from 2006 to 2012. Infect. Control Hosp. Epidemiol. 2014, 35, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Prevention strategies for seasonal influenza in healthcare settings. Available online: https://www.cdc.gov/flu/professionals/infectioncontrol/healthcaresettings.htm (accessed on 4 February 2019).
- Nguyen-Van-Tam, J.; Granfield, R.; Pearson, J.; Fleming, D.; Keating, N. Do influenza epidemics affect patterns of sickness absence among British hospital staff? Infect. Control Hosp. Epidemiol. 1999, 20, 691–694. [Google Scholar] [CrossRef] [PubMed]
- Yassi, A.; McGill, M.; Holton, D.; Nicolle, L. Morbidity, cost and role of health care worker transmission in an influenza outbreak in a tertiary care hospital. Can. J. Infect. Dis. 1993, 4, 52–56. [Google Scholar] [CrossRef]
- Hammond, G.W.; Cheang, M. Absenteeism among hospital staff during an influenza epidemic: Implications for immunoprophylaxis. Can. Med. Assoc. J. 1984, 131, 449–452. [Google Scholar] [PubMed]
- Yassi, A.; Kettner, J.; Hammond, G.; Cheang, M.; McGill, M. Effectiveness and cost-benefit of an influenza vaccination program for health care workers. Can. J. Infect. Dis. 1991, 2, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Stevenson, C.G.; McArthur, M.A.; Naus, M.; Abraham, E.; McGeer, A.J. Prevention of influenza and pneumococcal pneumonia in Canadian long-term care facilities: How are we doing? CMAJ 2001, 164, 1413–1419. [Google Scholar]
- Potter, J.; Stott, D.J.; Roberts, M.A.; Elder, A.G.; O’Donnell, B.; Knight, P.V.; Carman, W.F. Influenza vaccination of health care workers in long-term-care hospitals reduces the mortality of elderly patients. J. Infect. Dis. 1997, 175, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, K.G. Should staff in long-stay hospitals for elderly patients be vaccinated against influenza? Lancet 2000, 355, 83–84. [Google Scholar] [CrossRef]
- Nichol, K.L.; Grimm, M.B.; Peterson, D.C. Immunizations in long-term care facilities: Policies and practice. J. Am. Geriatr. Soc. 1996, 44, 349–355. [Google Scholar] [CrossRef]
- Dille, J.H. A worksite influenza immunization program: Impact on lost work days, health care utilization, and health care spending. AAOHN J. 1999, 47, 301–309. [Google Scholar] [CrossRef]
- Carman, W.F.; Elder, A.G.; Wallace, L.A.; McAulay, K.; Walker, A.; Murray, G.D.; Stott, D.J. Effects of influenza vaccination of health-care workers on mortality of elderly people in long-term care: A randomised controlled trial. Lancet 2000, 355, 93–97. [Google Scholar] [CrossRef]
- Everts, R.J.; Hanger, H.C.; Jennings, L.C.; Hawkins, A.; Sainsbury, R. Outbreaks of influenza A among elderly hospital inpatients. N. Z. Med. J. 1996, 109, 272–274. [Google Scholar]
- Adal, K.A.; Flowers, R.H.; Anglim, A.M.; Hayden, F.G.; Titus, M.G.; Coyner, B.J.; Farr, B.M. Prevention of nosocomial influenza. Infect. Control Hosp. Epidemiol. 1996, 17, 641–648. [Google Scholar] [CrossRef]
- Pachucki, C.T.; Pappas, S.A.; Fuller, G.F.; Krause, S.L.; Lentino, J.R.; Schaaff, D.M. Influenza A among hospital personnel and patients. Implications for recognition, prevention, and control. Arch. Intern. Med. 1989, 149, 77–80. [Google Scholar] [CrossRef] [PubMed]
- Salgado, C.D.; Giannetta, E.T.; Hayden, F.G.; Farr, B.M. Preventing nosocomial influenza by improving the vaccine acceptance rate of clinicians. Infect. Control Hosp. Epidemiol. 2004, 25, 923–928. [Google Scholar] [CrossRef] [PubMed]
- Nichol, K. Cost-benefit analysis of a strategy to vaccinate healthy working adults against influenza. Arch. Intern. Med. 2001, 161, 749–759. [Google Scholar] [CrossRef] [PubMed]
- Kumpulainen, V.; Makela, M. Influenza vaccination among healthy employees: A cost benefit analysis. Scand. J. Infect. Dis. 1997, 29, 181–185. [Google Scholar] [CrossRef]
- Advisory Committee on Immunization Practices; Centers for Disease Control and Prevention (CDC). Immunization of health-care personnel: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm. Rep. 2011, 60, 1–45. [Google Scholar]
- Goldstein, A.O.; Kincade, J.E.; Gamble, G.; Bearman, R.S. Policies and practices for improving influenza immunization rates among healthcare workers. Infect. Control Hosp. Epidemiol. 2004, 25, 908–911. [Google Scholar] [CrossRef]
- Seasonal Influenza Vaccination in Europe. Vaccination Recommendations and Coverage Rates in the EU Member States for Eight Influenza Seasons: 2007–2008 to 2014–2015. Stockholm: ECDC. 2017. Available online: https://ecdc.europa.eu/sites/portal/files/documents/influenza-vaccination-2007%E2%80%932008-to-2014%E2%80%932015.pdf (accessed on 7 December 2010).
- Black, C.L.; Yue, X.; Ball, S.W.; Fink, R.V.; de Perio, M.A.; Laney, A.S.; Williams, W.W.; Graitcer, S.B.; Fiebelkorn, A.P.; Lu, P.J.; et al. Influenza Vaccination Coverage Among Health Care Personnel—United States, 2017–2018 Influenza Season. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 1050–1054. [Google Scholar] [CrossRef]
- WHO. Everybody’s Business. Strengthening Health Systems to Improve Health Outcomes: WHO’s Framework for Action; WHO: Geneva, Switzerland, 2007. [Google Scholar]
- Community Preventive Services Task Force. Increasing Appropriate Vaccination: Health Care System-Based Interventions Implemented in Combination; US Department of Health and Human Services, the Community Preventive Services Task Force: Washington, DC, USA, 2015. [Google Scholar]
- Wensing, M.; Wollersheim, H.; Grol, R. Organizational interventions to implement improvements in patient care: A structured review of reviews. Implement. Sci. 2016, 1, 2. [Google Scholar] [CrossRef]
- Higgins, J.P.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration. Version 5.1.0. March 2011. Available online: http://handbook-5-1.cochrane.org/ (accessed on 1 February 2019).
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Protocol for Point Prevalence Surveys of Healthcare-Associated Infections and Antimicrobial Use in European Long-Term Care Facilities—Version 2.1. Available online: https://www.ecdc.europa.eu/sites/portal/files/media/en/publications/Publications/HALT-3-LTCF-PPS-Protocol-v2.1.pdf (accessed on 4 April 2020).
- Effective Public Health Practice Project. Quality Assessment Tool for Quantitative Studies; 2009. Available online: https://www.ephpp.ca/PDF/Quality%20Assessment%20Tool_2010_2.pdf (accessed on 4 April 2020).
- Chambers, L.W.; Crowe, L.; Lam, P.P.; MacDougall, D.; McNeil, S.; Roth, V.; Suh, K.; Dalzell, C.; Baker, D.; Ramsay, H.; et al. A new approach to improving healthcare personnel influenza immunization programs: A randomized controlled trial. PLoS ONE 2015, 10, e0118368. [Google Scholar] [CrossRef]
- Borgey, F.; Henry, L.; Lebeltel, J.; Lescure, P.; Coutour, X.L.; Vabret, A.; Verdon, R.; Thibon, P. Effectiveness of an Intervention Campaign on Influenza Vaccination of Professionals in Nursing Homes: A Cluster-Randomized Controlled Trial. Vaccine 2019, 37, 1260–1265. [Google Scholar] [CrossRef]
- Dey, P.; Halder, S.; Collins, S.; Benons, L.; Woodman, C. Promoting uptake of influenza vaccination among health care workers: A randomized controlled trial. J. Public Health Med. 2001, 23, 346–348. [Google Scholar] [CrossRef]
- Hayward, A.C.; Harling, R.; Wetten, S.; Johnson, A.M.; Munro, S.; Smedley, J.; Murad, S.; Watson, J.M. Effectiveness of an influenza vaccine programme for care home staff to prevent death, morbidity, and health service use among residents: Cluster randomised controlled trial. BMJ 2006, 333, 1241. [Google Scholar] [CrossRef] [PubMed]
- Kimura, A.C.; Nguyen, C.N.; Higa, J.I.; Hurwitz, E.L.; Vugia, D.J. The effectiveness of vaccine day and educational interventions on influenza vaccine coverage among health care workers at long-term care facilities. Am. J. Public Health 2007, 97, 684–690. [Google Scholar] [CrossRef] [PubMed]
- Lemaitre, M.; Meret, T.; Rothan-Tondeur, M.; Belmin, J.; Lejonc, J.L.; Luquel, L.; Piette, F.; Salom, M.; Verny, M.; Vetel, J.M.; et al. Effect of influenza vaccination of nursing home staff on mortality of residents: A cluster-randomized trial. J. Am. Geriatr. Soc. 2009, 57, 1580–1586. [Google Scholar] [CrossRef] [PubMed]
- Looijmans-van den Akker, I.; van Delden, J.J.; Verheij, T.J.; van der Sande, M.A.; van Essen, G.A.; Riphagen-Dalhuisen, J.; Hulscher, M.E.; Hak, E. Effects of a multi-faceted program to increase influenza vaccine uptake among health care workers in nursing homes: A cluster randomised controlled trial. Vaccine 2010, 28, 5086–5092. [Google Scholar] [CrossRef] [PubMed]
- Ksienski, D.S. Mandatory seasonal influenza vaccination or masking of British Columbia health care workers: Year 1. Can. J. Public Health 2014, 105, e312–e316. [Google Scholar] [CrossRef]
- Nace, D.A.; Perera, S.; Handler, S.M.; Muder, R.; Hoffman, E.L. Increasing influenza and pneumococcal immunization rates in a nursing home network. J. Am. Med. Dir. Assoc. 2011, 12, 678–684. [Google Scholar] [CrossRef]
- Nace, D.A.; Handler, S.M.; Hoffman, E.L.; Perera, S. Impact of the raising immunizations safely and effectively (RISE) program on healthcare worker influenza immunization rates in long term care settings. J. Am. Med. Dir. Assoc. 2012, 13, 806–810. [Google Scholar] [CrossRef]
- Ofstead, C.L.; Amelang, M.R.; Wetzler, H.P.; Tan, L. Moving the needle on nursing staff influenza vaccination in long-term care: Results of an evidence-based intervention. Vaccine 2017, 35, 2390–2395. [Google Scholar] [CrossRef]
- Sand, K.L.; Lynn, J.; Bardenheier, B.; Seow, H.; Nace, D.A. Increasing influenza immunization for long-term care facility staff using quality improvement. J. Am. Geriatr. Soc. 2007, 55, 1741–1747. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.R.; Winsted, B.; Koontz, C. Improving neglected influenza vaccination among healthcare workers in long-term care. J. Am. Geriatr. Soc. 1993, 41, 928–930. [Google Scholar] [CrossRef] [PubMed]
- Black, C.L.; Yue, X.; Ball, S.W.; Fink, R.; de Perio, M.A.; Laney, A.S.; Williams, W.W.; Lindley, M.C.; Graitcer, S.B.; Lu, P.J.; et al. Influenza Vaccination Coverage Among Health Care Personnel—United States, 2016–2017 Influenza Season. MMWR Morb. Mortal. Wkly. Rep. 2017, 66, 1009–1015. [Google Scholar] [CrossRef] [PubMed]
- Apenteng, B.A.; Opoku, S.T. Employee influenza vaccination in residential care facilities. Am. J. Infect. Control 2014, 42, 294–299. [Google Scholar] [CrossRef]
- Bentele, H.; Bergsaker, M.R.; Hauge, S.H.; Bjørnholt, J.V. Vaccination coverage for seasonal influenza among residents and health care workers in Norwegian nursing homes during the 2012/13 season, a cross-sectional study. BMC Public Health 2014, 14, 434. [Google Scholar] [CrossRef]
- Borlaug, G.; Newman, A.; Pfister, J.; Davis, J.P. Factors that influenced rates of influenza vaccination among employees of Wisconsin acute care hospitals and nursing homes during the 2005–2006 influenza season. Infect. Control Hosp. Epidemiol. 2007, 28, 1398–1400. [Google Scholar] [CrossRef]
- Halliday, L.; Thomson, J.A.; Roberts, L.; Bowen, S.; Mead, C. Influenza vaccination of staff in aged care facilities in the ACT: How can we improve the uptake of influenza vaccine? Aust. N. Z. J. Public Health 2003, 27, 70–75. [Google Scholar] [CrossRef]
- Hauri, A.M.; Uphoff, H.; Gussmann, V.; Gawrich, S. Factors that affect influenza vaccine uptake among staff of long-term care facilities. Infect. Control Hosp. Epidemiol. 2006, 27, 638–641. [Google Scholar] [CrossRef]
- Henry, B.; Naus, M.; Stirling, R. Impact of Influenza Vaccination Policies on Staff Coverage in Long-Term care Facilities; ScienceDirect: Amsterdam, The Netherlands, 2001; Volume 1219, pp. 671–675. [Google Scholar]
- McArthur, M.A.; Simor, A.E.; Campbell, B.; McGeer, A. Influenza vaccination in long-term-care facilities: Structuring programs for success. Infect. Control Hosp. Epidemiol. 1999, 20, 499–503. [Google Scholar] [CrossRef]
- Russell, M.L. Influenza vaccination in Alberta long-term care facilities. CMAJ 2001, 164, 1423–1427. [Google Scholar]
- Shroufi, A.; Copping, J.; Musonda, P.; Vivancos, R.; Langden, V.; Armstrong, S.; Slack, R. Influenza vaccine uptake among staff in care homes in Nottinghamshire: A random cluster sample survey. Public Health 2009, 123, 645–649. [Google Scholar] [CrossRef] [PubMed]
- Vaux, S.; Noël, D.; Fonteneau, L. Influenza vaccination coverage of healthcare workers and residents and their determinants in nursing homes for elderly people in France: A cross-sectional survey. BMC Public Health 2010, 10, 159. [Google Scholar] [CrossRef] [PubMed]
- Yue, X.; Black, C.; Ball, S.; Donahue, S.; Perio, M.A.D.; Laney, A.S.; Greby, S. Workplace Interventions and Vaccination-Related Attitudes Associated With Influenza Vaccination Coverage Among Healthcare Personnel Working in Long-Term Care Facilities, 2015‒2016 Influenza Season. J. Am. Med. Dir. Assoc. 2019, 20, 718–724. [Google Scholar] [CrossRef] [PubMed]
- Campbell, L.J.; Li, Q.; Li, Y. Health care worker influenza vaccination in Oregon nursing homes: Correlates of facility characteristics. J. Am. Med. Dir. Assoc. 2014, 15, 847–848. [Google Scholar] [CrossRef][Green Version]
- Nace, D.A.; Hoffman, E.L.; Resnick, N.M.; Handler, S.M. Achieving and sustaining high rates of influenza immunization among long-term care staff. J. Am. Med. Dir. Assoc. 2007, 8, 128–133. [Google Scholar] [CrossRef]
- Lansbury, L.E.; Brown Nguyen-Van-Tam, J.S. Influenza in long-term care facilities. Influenza Respir. Viruses 2017, 11, 356–366. [Google Scholar] [CrossRef]
- Maltezou, H.C.; Poland, G.A. Immunization of Health-Care Providers: Necessity and Public Health Policies. Healthcare 2016, 4, 47. [Google Scholar] [CrossRef]
- World Health Organization—Office for Europe. Prevention and Control of Outbreaks of Seasonal Influenza in Long-Term Care Facilities: A Review of the Evidence and Best-Practice Guidance; WHO: Geneva, Switzerland, 2017. [Google Scholar]
- Elias, C.; Fournier, A.; Vasiliu, A.; Beix, N.; Demillac, R.; Tillaut, H.; Guillois, Y.; Eyebe, S.; Mollo, B.; Crépey, P. Seasonal influenza vaccination coverage and its determinants among nursing homes personnel in western France. BMC Public Health 2017, 17, 634. [Google Scholar] [CrossRef]
- Guthmann, J.P.; Fonteneau, L.; Ciotti, C.; Bouvet, E.; Pellissier, G.; Lévy-Bruhl, D.; Abiteboul, D. Vaccination coverage of health care personnel working in health care facilities in France: Results of a national survey, 2009. Vaccine 2012, 30, 4648–4654. [Google Scholar] [CrossRef]
- The Organisation of Formal Long-Term Care for the Elderly: Results from the 21 European Country Studies in the ANCIEN Project. Available online: http://aei.pitt.edu/32969/1/RR_No_95__ANCIEN__Organisation_of_Formal_LTC.pdf (accessed on 4 April 2020).
- Leichsenring, K.; Billings, J.; Nies, H. Long-Term Care in Europe: Improving Policy and Practice; Springer: Berlin, Germany, 2013. [Google Scholar]
- McGrail, K.M.; McGregor, M.J.; Cohen, M.; Tate, R.B.; Ronald, L.A. For-profit versus not-for-profit delivery of long-term care. CMAJ 2007, 176, 57–58. [Google Scholar] [CrossRef]
- Eligibility and Inclusiveness of Long-Term Care Institutional Frameworks in Europe: A Cross-Country Comparison. Available online: http://dx.doi.org/10.2139/ssrn.2541246 (accessed on 4 April 2020).
- The Development of Long-Term Care in Post-Socialist Member States of the EU. Available online: http://dx.doi.org/10.2139/ssrn.2207861 (accessed on 4 April 2020).
- Zimmerman, D.R. Improving nursing home quality of care through outcomes data: The MDS quality indicators. Int. J. Geriatr. Psychiatry 2003, 18, 250–257. [Google Scholar] [CrossRef] [PubMed]
- Leichsenring, K. Achieving Quality Long-Term Care in Residential Facilities. Synthesis Report of the German Peer Review in Social Protection and Social Inclusion. Available online: https://ec.europa.eu/social/main.jsp?catId=1024&langId=en&newsId=1414&moreDocuments=yes&tableName=news (accessed on 4 April 2020).
- Giorgio, L.D.; Filippini, M.; Masiero, G. Is higher nursing home quality more costly? Eur. J. Health Econ. 2016, 17, 1011–1026. [Google Scholar] [CrossRef] [PubMed]
- OECD/European Commission. A Good Life in Old Age? Monitoring and Improving Quality in Long-Term Care: OECD Health Policy Studies; OECD Publishing: Paris, France, 2013. [Google Scholar]
- Van Buynder, P.G.; Konrad, S.; Kersteins, F.; Preston, E.; Brown, P.D.; Keen, D.; Murray, N.J. Healthcare worker influenza immunization vaccinate or mask policy: Strategies for cost effective implementation and subsequent reductions in staff absenteeism due to illness. Vaccine 2015, 33, 1625–1628. [Google Scholar] [CrossRef] [PubMed]
- Katz, P.R.; Karuza, J.; Lima, J.; Intrator, O. Nursing home medical staff organization: Correlates with quality indicators. J. Am. Med. Dir. Assoc. 2011, 12, 655–659. [Google Scholar] [CrossRef]
- Bardenheier, B.H.; Wortley, P.; Ahmed, F.; Hales, C.; Shefer, A. Influenza immunization coverage among residents of long-term care facilities certified by CMS, 2005–2006: The newest MDs quality indicator. J. Am. Med. Dir. Assoc. 2010, 11, 59–69. [Google Scholar] [CrossRef]
- Bonaccorsi, G.; Lorini, C.; Santomauro, F.; Guarducci, S.; Pellegrino, E.; Puggelli, F.; Balli, M.; Bonanni, P. Predictive factors associated with the acceptance of pandemic and seasonal influenza vaccination in health care workers and students in Tuscany, Central Italy. Hum. Vaccin. Immunother. 2013, 9, 2603–2612. [Google Scholar] [CrossRef]
- Bonaccorsi, G.; Santomauro, F.; Porchia, B.R.; Niccolai, G.; Pellegrino, E.; Bonanni, P.; Lorini, C. Beliefs and Opinions of Health Care Workers and Students Regarding Influenza and Influenza Vaccination in Tuscany, Central Italy. Vaccines 2015, 3, 137–147. [Google Scholar] [CrossRef]
- Rothman, K.J. Six persistent research misconceptions. J. Gen. Intern. Med. 2014, 29, 1060–1064. [Google Scholar] [CrossRef]
- Grimes, D.A.; Schulz, K.F. Descriptive studies: What they can and cannot do. Lancet 2002, 359, 145–149. [Google Scholar] [CrossRef]
- Dwan, K.; Gamble, C.; Williamson, P.R.; Kirkham, J.J.; for the Reporting Bias Group. Systematic Review of the Empirical Evidence of Study Publication Bias and Outcome Reporting Bias—An Updated Review. PLoS ONE 2013, 8, e66844. [Google Scholar] [CrossRef]
| Area | Interventions | Code |
|---|---|---|
| Interventions to improve the access to vaccination | Vaccination available at work, in any locations | 1a |
| Offering vaccine during new hire orientation | 1b | |
| Temporal access (vaccination offered during day and night shifts) | 1c | |
| Continuing to provide vaccines throughout the season | 1d | |
| Holding vaccination kick-off events | 1e | |
| Free vaccination offered | 1f | |
| Provide vaccination at reduced cost | 1g | |
| Interventions to eliminate individual barriers (attitudes/opinions) | Identification of the individual and context barriers to vaccination | 2a |
| Improve vaccination confidence for directors | 2b | |
| Providing in-service educational seminars or educational sessions for staff | 2c | |
| Displaying educational written materials (posters, leaflets,…) | 2d | |
| Offering incentives (treats, raffle tickets) to vaccinated health care workers | 2e | |
| Providing additional education to staff who declined the vaccine | 2f | |
| Individual counselling sessions | 2g | |
| Facilities provide reminders to staff to be immunized | 2h | |
| Policy/leadership interventions directed to lead to vaccination | Introduce a policy on immunization | 3a |
| Mandatory vaccination policy | 3b | |
| Facility recommends influenza immunization for staff | 3c | |
| Requiring completion of declining forms | 3d | |
| Consider vaccination rate as a target for quality improvement | 3e | |
| Identified lead persons to arrange for vaccination sessions and vaccination promotion | 3f | |
| Facilitation support by experts | 3g | |
| Discussing proposed policies and goals with researchers | 3h | |
| Continual performance feedback and shared learning | 3j | |
| Communicating with staff about vaccination goal | 3k | |
| Sharing vaccination rates with staff | 3l | |
| Communicating with staff about new policies on immunization | 3m | |
| Requiring vaccine receipt or masking throughout the season | 3n | |
| Discussing vaccination policy during new hire orientation | 3o |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bechini, A.; Lorini, C.; Zanobini, P.; Mandò Tacconi, F.; Boccalini, S.; Grazzini, M.; Bonanni, P.; Bonaccorsi, G. Utility of Healthcare System-Based Interventions in Improving the Uptake of Influenza Vaccination in Healthcare Workers at Long-Term Care Facilities: A Systematic Review. Vaccines 2020, 8, 165. https://doi.org/10.3390/vaccines8020165
Bechini A, Lorini C, Zanobini P, Mandò Tacconi F, Boccalini S, Grazzini M, Bonanni P, Bonaccorsi G. Utility of Healthcare System-Based Interventions in Improving the Uptake of Influenza Vaccination in Healthcare Workers at Long-Term Care Facilities: A Systematic Review. Vaccines. 2020; 8(2):165. https://doi.org/10.3390/vaccines8020165
Chicago/Turabian StyleBechini, Angela, Chiara Lorini, Patrizio Zanobini, Francesco Mandò Tacconi, Sara Boccalini, Maddalena Grazzini, Paolo Bonanni, and Guglielmo Bonaccorsi. 2020. "Utility of Healthcare System-Based Interventions in Improving the Uptake of Influenza Vaccination in Healthcare Workers at Long-Term Care Facilities: A Systematic Review" Vaccines 8, no. 2: 165. https://doi.org/10.3390/vaccines8020165
APA StyleBechini, A., Lorini, C., Zanobini, P., Mandò Tacconi, F., Boccalini, S., Grazzini, M., Bonanni, P., & Bonaccorsi, G. (2020). Utility of Healthcare System-Based Interventions in Improving the Uptake of Influenza Vaccination in Healthcare Workers at Long-Term Care Facilities: A Systematic Review. Vaccines, 8(2), 165. https://doi.org/10.3390/vaccines8020165








