Advanced Safety and Genetic Stability in Mice of a Novel DNA-Launched Venezuelan Equine Encephalitis Virus Vaccine with Rearranged Structural Genes
Abstract
1. Introduction
2. Materials and Methods
2.1. Viruses
2.2. Vaccine Replication Kinetics in Brain Tissues
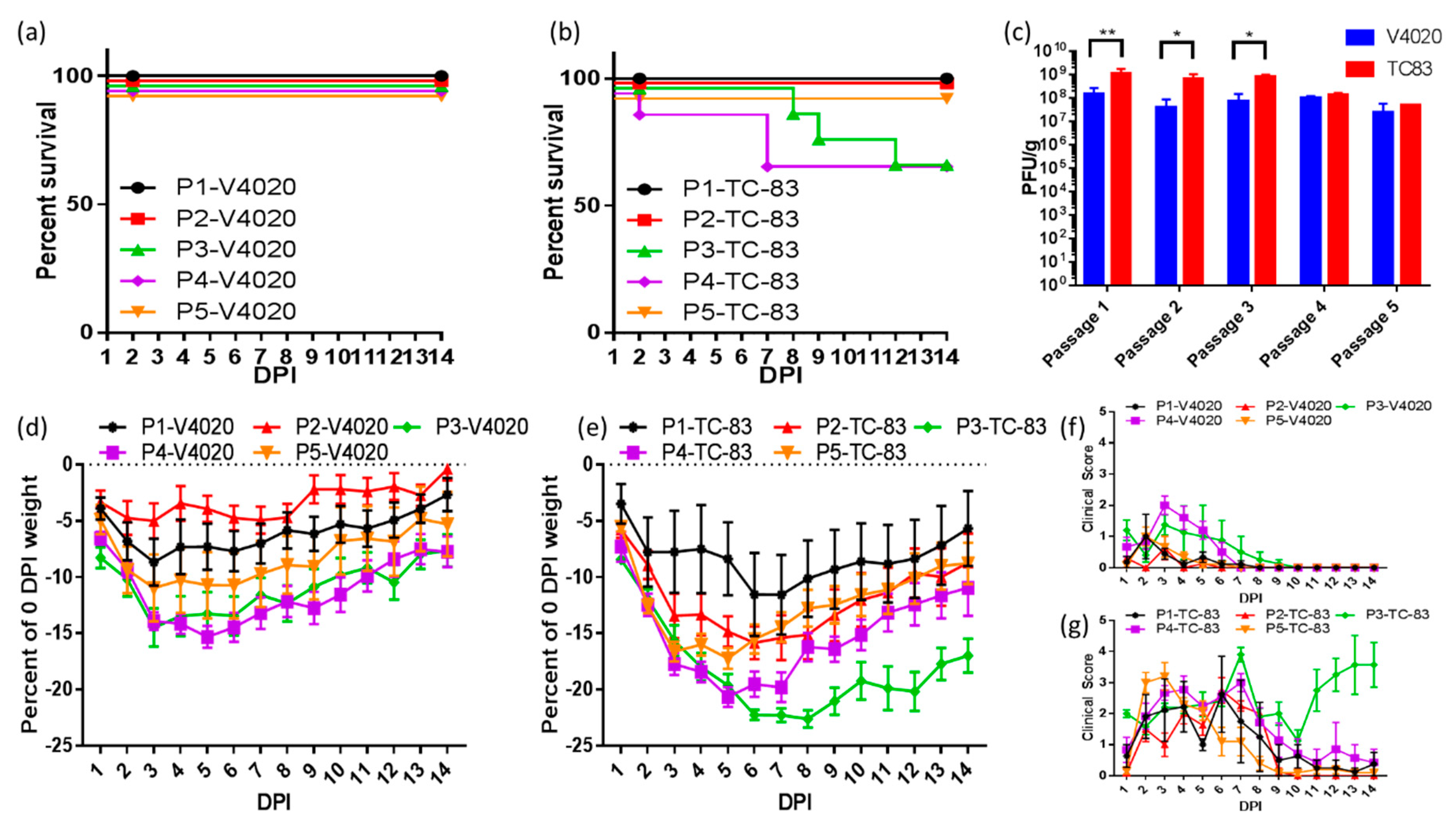
2.3. Sequential IC Passages in Mice
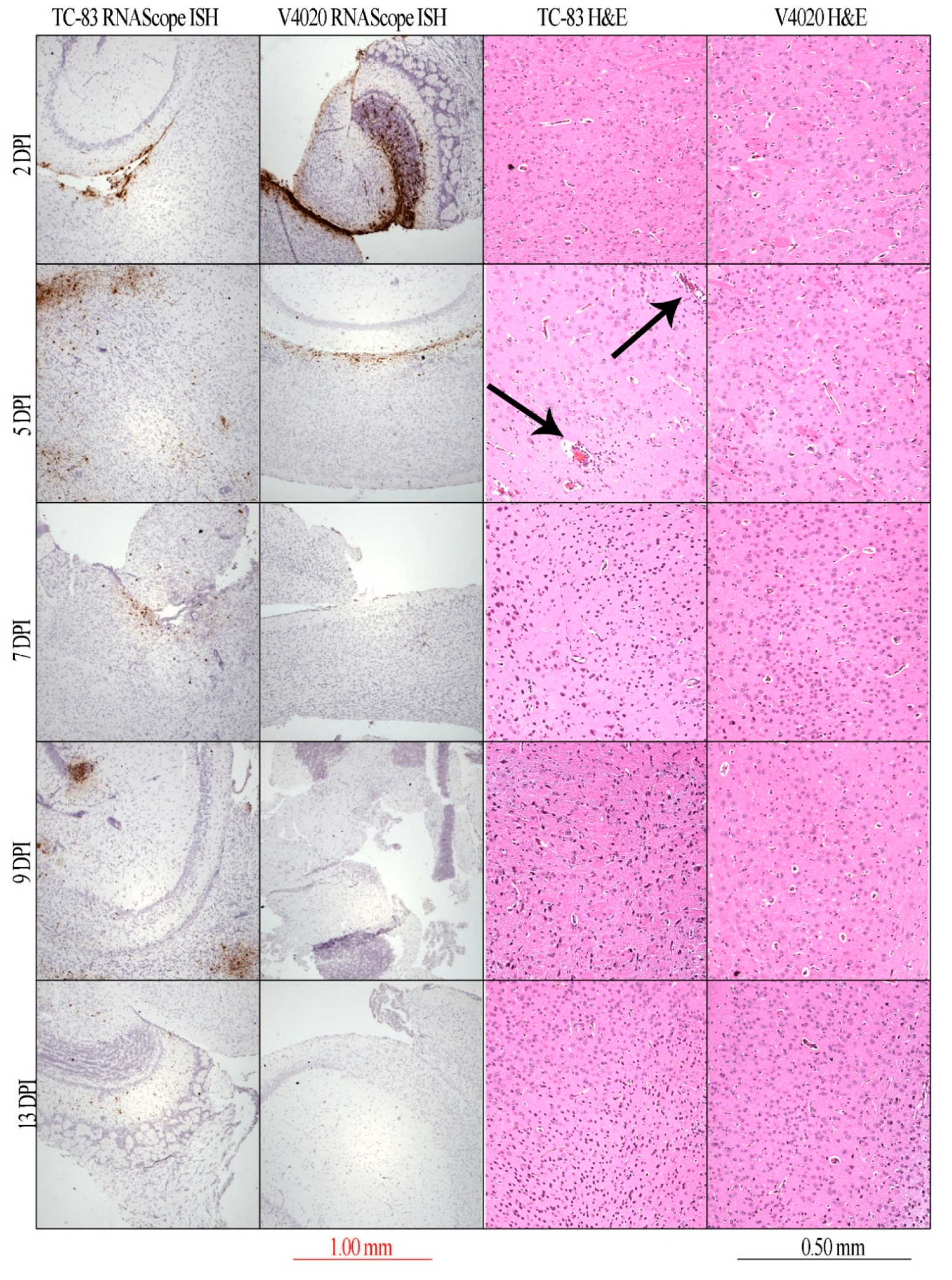
2.4. In Situ Hybridization and Histology
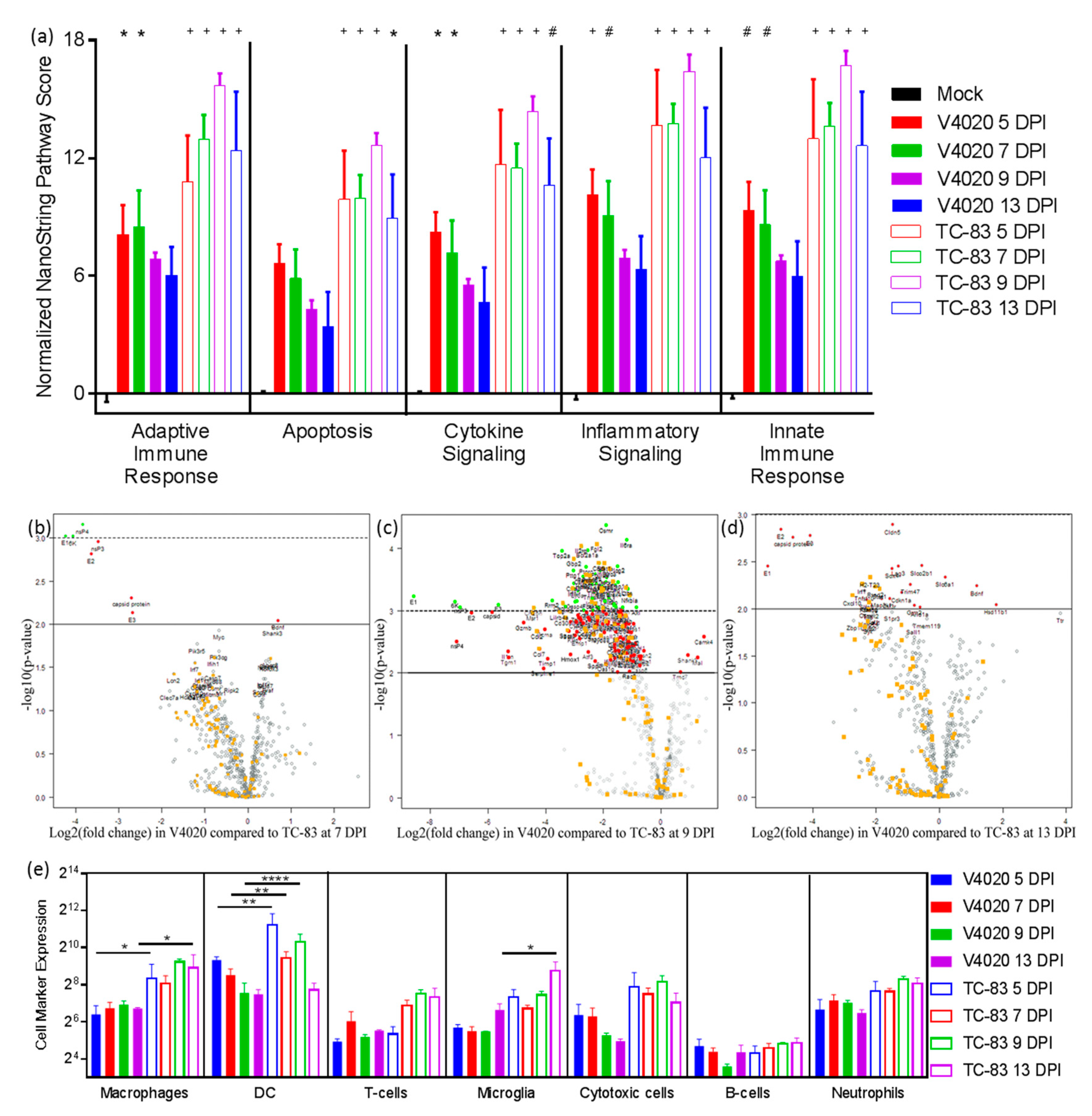
2.5. NanoString Array
2.6. RNA-Seq
2.7. Statistical Analysis
2.8. Ethics Statement
3. Results
3.1. Kinetics Study: Attenuated Replication of V4020 in Brains of Infected Mice
3.2. Neuro-Inflammation in Brain Tissues of Mice Infected with V4020 vs. TC-83 Assessed by Direct Multiplexed Measurement of Gene Expression
3.3. Clinical Profiling of Mice during Serial Intracranial Passages of V4020 and TC-83
3.4. Viral and Host RNA-Seq Profiles of Brain Samples, P1-P5
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Aguilar, P.V.; Estrada-Franco, J.G.; Navarro-Lopez, R.; Ferro, C.; Haddow, A.D.; Weaver, S.C. Endemic Venezuelan equine encephalitis in the Americas: Hidden under the dengue umbrella. Future Virol. 2011, 6, 721–740. [Google Scholar] [CrossRef] [PubMed]
- Beckham, J.D.; Tyler, K.L. 91—Encephalitis. In Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases, 8th ed.; Bennett, J.E., Dolin, R., Blaser, M.J., Eds.; Content Repository Only: Philadelphia, PA, USA, 2015; pp. 1144–1163. [Google Scholar]
- Taylor, K.G.; Paessler, S. Pathogenesis of Venezuelan equine encephalitis. Vet. Microbiol. 2013, 167, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Zacks, M.A.; Paessler, S. Encephalitic alphaviruses. Vet. Microbiol. 2010, 140, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Estrada-Franco, J.G.; Navarro-Lopez, R.; Freier, J.E.; Cordova, D.; Clements, T.; Moncayo, A.; Kang, W.; Gomez-Hernandez, C.; Rodriguez-Dominguez, G.; Ludwig, G.V. Venezuelan equine encephalitis virus, southern Mexico. Emerg. Infect. Dis. 2004, 10, 2113. [Google Scholar] [CrossRef]
- Samy, A.M.; Elaagip, A.H.; Kenawy, M.A.; Ayres, C.F.; Peterson, A.T.; Soliman, D.E. Climate change influences on the global potential distribution of the mosquito Culex quinquefasciatus, vector of West Nile virus and lymphatic filariasis. PLoS ONE 2016, 11, e0163863. [Google Scholar] [CrossRef]
- Hongoh, V.; Berrang-Ford, L.; Scott, M.E.; Lindsay, L.R. Expanding geographical distribution of the mosquito, Culex pipiens, in Canada under climate change. Appl. Geogr. 2012, 33, 53–62. [Google Scholar] [CrossRef]
- Brown, H.E.; Young, A.; Lega, J.; Andreadis, T.G.; Schurich, J.; Comrie, A. Projection of climate change influences on US West Nile virus vectors. Earth Interact. 2015, 19, 1–18. [Google Scholar] [CrossRef]
- Weaver, S.; Paessler, S. Alphaviral encephalitides, in Vaccines for Biodefense and Emerging and Neglected Diseases; Elsevier Inc.: London, UK, 2009; pp. 339–359. [Google Scholar]
- Sharma, A.; Knollmann-Ritschel, B. Current Understanding of the Molecular Basis of Venezuelan Equine Encephalitis Virus Pathogenesis and Vaccine Development. Viruses 2019, 11, 164. [Google Scholar] [CrossRef]
- Bronze, M.S.; Huycke, M.M.; Machado, L.J.; Voskuhl, G.W.; Greenfield, R.A. Viral agents as biological weapons and agents of bioterrorism. Am. J. Med. Sci. 2002, 323, 316–325. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Possession, use, and transfer of select agents and toxins; biennial review. Final rule. Fed. Regist. 2012, 77, 61083. [Google Scholar]
- Lennette, E.H.; Koprowski, H. Human Infection with Venezuelan Equine Encephalomyelitis Virus: A Report on Eight Cases of Infection Acquired in the Laboratory. JAMA 1943, 123, 1088–1095. [Google Scholar] [CrossRef]
- Sulkin, S.E. Laboratory-acquired infections. Bacteriol. Rev. 1961, 25, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Rusnak, J.M.; Dupuy, L.C.; Niemuth, N.A.; Glenn, A.M.; Ward, L.A. Comparison of Aerosol- and Percutaneous-acquired Venezuelan Equine Encephalitis in Humans and Nonhuman Primates for Suitability in Predicting Clinical Efficacy under the Animal Rule. Comp. Med. 2018, 68, 380–395. [Google Scholar] [CrossRef] [PubMed]
- Sutton, L.S.; Brooke, C.C. Venezuelan equine encephalomyelitis due to vaccination in man. J. Am. Med. Assoc. 1954, 155, 1473–1476. [Google Scholar] [CrossRef] [PubMed]
- Berge, T.O.; Banks, I.S.; Tigertt, W.D. Attenuation of Venezuelan Equine Encephalomtelitis Virus by In Vitro Cultivation in Guinea-Pig Heart Cells. Am. J. Epidemiol. 1961, 73, 209–218. [Google Scholar] [CrossRef]
- Kinney, R.M.; Chang, G.J.; Tsuchiya, K.R.; Sneider, J.M.; Roehrig, J.T.; Woodward, T.M.; Trent, D.W. Attenuation of Venezuelan equine encephalitis virus strain TC-83 is encoded by the 5’-noncoding region and the E2 envelope glycoprotein. J. Virol. 1993, 67, 1269–1277. [Google Scholar] [CrossRef]
- Holley, P.; Fine, D.; Terpening, S. Safety of an attenuated Venezuelan equine encephalititis virus (VEEV) vaccine in humans. In Proceedings of the 48th ICAAC/IDSA Meeting, Washington, DC, USA, 25–28 October 2008. [Google Scholar]
- Hyde, J.L.; Gardner, C.L.; Kimura, T.; White, J.P.; Liu, G.; Trobaugh, D.W.; Huang, C.; Tonelli, M.; Paessler, S.; Takeda, K.; et al. A viral RNA structural element alters host recognition of nonself RNA. Science 2014, 343, 783–787. [Google Scholar] [CrossRef]
- Rusnak, J.M.; Glass, P.J.; Weaver, S.C.; Sabourin, C.L.; Glenn, A.M.; Klimstra, W.; Badorrek, C.S.; Nasar, F.; Ward, L.A. Approach to Strain Selection and the Propagation of Viral Stocks for Venezuelan Equine Encephalitis Virus Vaccine Efficacy Testing under the Animal Rule. Viruses 2019, 11, 807. [Google Scholar] [CrossRef]
- Pittman, P.R.; Makuch, R.S.; Mangiafico, J.A.; Cannon, T.L.; Gibbs, P.H.; Peters, C.J. Long-term duration of detectable neutralizing antibodies after administration of live-attenuated VEE vaccine and following booster vaccination with inactivated VEE vaccine. Vaccine 1996, 14, 337–343. [Google Scholar] [CrossRef]
- Alevizatos, A.C.; McKinney, R.W.; Feigin, R.D. Live, attenuated Venezuelan equine encephalomyelitis virus vaccine. I. Clinical effects in man. Am. J. Trop. Med. Hyg. 1967, 16, 762–768. [Google Scholar] [CrossRef]
- Paessler, S.; Ni, H.; Petrakova, O.; Fayzulin, R.Z.; Yun, N.; Anishchenko, M.; Weaver, S.C.; Frolov, I. Replication and clearance of Venezuelan equine encephalitis virus from the brains of animals vaccinated with chimeric SIN/VEE viruses. J. Virol. 2006, 80, 2784–2796. [Google Scholar] [CrossRef] [PubMed]
- Martin, S.S.; Bakken, R.R.; Lind, C.M.; Reed, D.S.; Price, J.L.; Koeller, C.A.; Parker, M.D.; Hart, M.K.; Fine, D.L. Telemetric analysis to detect febrile responses in mice following vaccination with a live-attenuated virus vaccine. Vaccine 2009, 27, 6814–6823. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kenney, J.L.; Volk, S.M.; Pandya, J.; Wang, E.; Liang, X.; Weaver, S.C. Stability of RNA virus attenuation approaches. Vaccine 2011, 29, 2230–2234. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Erasmus, J.H.; Seymour, R.L.; Kaelber, J.T.; Kim, D.Y.; Leal, G.; Sherman, M.B.; Frolov, I.; Chiu, W.; Weaver, S.C.; Nasar, F. Novel Insect-Specific Eilat Virus-Based Chimeric Vaccine Candidates Provide Durable, Mono- and Multivalent, Single-Dose Protection against Lethal Alphavirus Challenge. J. Virol. 2018, 92, e01274-17. [Google Scholar]
- Erasmus, J.H.; Weaver, S.C. Biotechnological Applications of an Insect-Specific Alphavirus. DNA Cell Biol. 2017, 36, 1045–1049. [Google Scholar] [CrossRef]
- Guerbois, M.; Volkova, E.; Forrester, N.L.; Rossi, S.L.; Frolov, I.; Weaver, S.C. IRES-driven expression of the capsid protein of the Venezuelan equine encephalitis virus TC-83 vaccine strain increases its attenuation and safety. PLoS Negl. Trop. Dis. 2013, 7, e2197. [Google Scholar] [CrossRef]
- Rossi, S.L.; Russell-Lodrigue, K.E.; Killeen, S.Z.; Wang, E.; Leal, G.; Bergren, N.A.; Vinet-Oliphant, H.; Weaver, S.C.; Roy, C.J. IRES-Containing VEEV Vaccine Protects Cynomolgus Macaques from IE Venezuelan Equine Encephalitis Virus Aerosol Challenge. PLoS Negl. Trop. Dis. 2015, 9, e0003797. [Google Scholar] [CrossRef]
- Rossi, S.L.; Guerbois, M.; Gorchakov, R.; Plante, K.S.; Forrester, N.L.; Weaver, S.C. IRES-based Venezuelan equine encephalitis vaccine candidate elicits protective immunity in mice. Virology 2013, 437, 81–88. [Google Scholar] [CrossRef]
- Tretyakova, I.; Hearn, J.; Wang, E.; Weaver, S.; Pushko, P. DNA Vaccine Initiates Replication of Live Attenuated Chikungunya Virus In Vitro and Elicits Protective Immune Response in Mice. J. Infect. Dis. 2014, 209, 1882–1890. [Google Scholar] [CrossRef]
- Tretyakova, I.; Tibbens, A.; Jokinen, J.D.; Johnson, D.M.; Lukashevich, I.S.; Pushko, P. Novel DNA-launched Venezuelan equine encephalitis virus vaccine with rearranged genome. Vaccine 2019, 37, 3317–3325. [Google Scholar] [CrossRef]
- Tretyakova, I.; Plante, K.S.; Rossi, S.L.; Lawrence, H.W.S.; Peel, J.E.; Gudjohnsen, S.; Wang, E.; Mirchandani, D.; Tibbens, A.; Lamichhane, T.N.; et al. Venezuelan equine encephalitis vaccine with rearranged genome resists reversion and protects non-human primates from viremia after aerosol challenge. Vaccine 2020. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.M.; Jokinen, J.D.; Lukashevich, I.S. Attenuated Replication of Lassa Virus Vaccine Candidate ML29 in STAT-1(-/-) Mice. Pathogens 2019, 8, 9. [Google Scholar] [CrossRef] [PubMed]
- Cardiff, R.D.; Miller, C.H.; Munn, R.J. Manual hematoxylin and eosin staining of mouse tissue sections. Cold Spring Harb. Protoc. 2014, 2014, 655–658. [Google Scholar] [CrossRef] [PubMed]
- Afgan, E.; Baker, D.; Batut, B.; van den Beek, M.; Bouvier, D.; Čech, M.; Chilton, J.; Clements, D.; Coraor, N.; Grüning, B.A.; et al. The Galaxy platform for accessible, reproducible and collaborative biomedical analyses: 2018 update. Nucleic Acids Res. 2018, 46, W537–W544. [Google Scholar] [CrossRef]
- Bolger, A.M.; Lohse, M.; Usadel, B. Trimmomatic: A flexible trimmer for Illumina sequence data. Bioinformatics 2014, 30, 2114–2120. [Google Scholar] [CrossRef]
- Langmead, B.; Salzberg, S.L. Fast gapped-read alignment with Bowtie 2. Nat. Methods 2012, 9, 357–359. [Google Scholar] [CrossRef]
- Kim, D.; Langmead, B.; Salzberg, S.L. HISAT: A fast spliced aligner with low memory requirements. Nat. Methods 2015, 12, 357–360. [Google Scholar] [CrossRef]
- Anders, S.; Pyl, P.T.; Huber, W. HTSeq--a Python framework to work with high-throughput sequencing data. Bioinformatics 2015, 31, 166–169. [Google Scholar] [CrossRef]
- Love, M.I.; Huber, W.; Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 2014, 15, 550. [Google Scholar] [CrossRef]
- Young, M.D.; Wakefield, M.J.; Smyth, G.K.; Oshlack, A. Gene ontology analysis for RNA-seq: Accounting for selection bias. Genome Biol. 2010, 11, R14. [Google Scholar] [CrossRef]
- Geiss, G.K.; Bumgarner, R.E.; Birditt, B.; Dahl, T.; Dowidar, N.; Dunaway, D.L.; Fell, H.P.; Ferree, S.; George, R.D.; Grogan, T.; et al. Direct multiplexed measurement of gene expression with color-coded probe pairs. Nat. Biotechnol. 2008, 26, 317–325. [Google Scholar] [CrossRef]
- Tsang, H.F.; Xue, V.W.; Koh, S.P.; Chiu, Y.M.; Ng, L.P.; Wong, S.C. NanoString, a novel digital color-coded barcode technology: Current and future applications in molecular diagnostics. Expert Rev. Mol. Diagn. 2017, 17, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Veldman-Jones, M.H.; Brant, R.; Rooney, C.; Geh, C.; Emery, H.; Harbron, C.G.; Wappett, M.; Sharpe, A.; Dymond, M.; Barrett, J.C.; et al. Evaluating Robustness and Sensitivity of the NanoString Technologies nCounter Platform to Enable Multiplexed Gene Expression Analysis of Clinical Samples. Cancer Res. 2015, 75, 2587–2593. [Google Scholar] [CrossRef]
- Makarava, N.; Chang, J.C.-Y.; Molesworth, K.; Baskakov, I.V. Region-specific glial homeostatic signature in prion diseases is replaced by a uniform neuroinflammation signature, common for brain regions and prion strains with different cell tropism. Neurobiol. Dis. 2020, 137, 104783. [Google Scholar] [CrossRef] [PubMed]
- Aaby, P.; Benn, C.S. Developing the concept of beneficial non-specific effect of live vaccines with epidemiological studies. Clin. Microbiol. Infect. 2019, 25, 1459–1467. [Google Scholar] [CrossRef] [PubMed]
- Minor, P.D. Live attenuated vaccines: Historical successes and current challenges. Virology 2015, 479, 379–392. [Google Scholar] [CrossRef] [PubMed]
- Lauring, A.S.; Jones, J.O.; Andino, R. Rationalizing the development of live attenuated virus vaccines. Nat. Biotechnol. 2010, 28, 573–579. [Google Scholar] [CrossRef]
- Ludwig, G.V.; Turell, M.J.; Vogel, P.; Kondig, J.P.; Kell, W.K.; Smith, J.F.; Pratt, W.D. Comparative neurovirulence of attenuated and non-attenuated strains of Venezuelan equine encephalitis virus in mice. Am. J. Trop. Med. Hyg. 2001, 64, 49–55. [Google Scholar] [CrossRef]
- Steele, K.E.; Davis, K.J.; Stephan, K.; Kell, W.; Vogel, P.; Hart, M.K. Comparative neurovirulence and tissue tropism of wild-type and attenuated strains of Venezuelan equine encephalitis virus administered by aerosol in C3H/HeN and BALB/c mice. Vet. Pathol. 1998, 35, 386–397. [Google Scholar] [CrossRef]
- Martin, S.S.; Bakken, R.R.; Lind, C.M.; Garcia, P.; Jenkins, E.; Glass, P.J.; Parker, M.D.; Hart, M.K.; Fine, D.L. Evaluation of formalin inactivated V3526 virus with adjuvant as a next generation vaccine candidate for Venezuelan equine encephalitis virus. Vaccine 2010, 28, 3143–3151. [Google Scholar] [CrossRef][Green Version]
- Bowen, G.S.; Fashinell, T.R.; Dean, P.B.; Gregg, M.B. Clinical aspects of human Venezuelan equine encephalitis in Texas. Bull. Pan. Am. Health Organ. 1976, 10, 46–57. [Google Scholar] [PubMed]
- Fine, D.L.; Roberts, B.A.; Terpening, S.J.; Mott, J.; Vasconcelos, D.; House, R.V. Neurovirulence evaluation of Venezuelan equine encephalitis (VEE) vaccine candidate V3526 in nonhuman primates. Vaccine 2008, 26, 3497–3506. [Google Scholar] [CrossRef] [PubMed]
- McKinney, R.W.; Berge, T.O.; Sawyer, W.D.; Tigertt, W.D.; Crozier, D. Use of an attenuated strain of venezuelan equine encephalomyelitis virus for immunization in man. Am. J. Trop. Med. Hyg. 1963, 12, 597–603. [Google Scholar] [CrossRef] [PubMed]
- Forrester, N.L.; Wertheim, J.O.; Dugan, V.G.; Auguste, A.J.; Lin, D.; Adams, A.P.; Chen, R.; Gorchakov, R.; Leal, G.; Estrada-Franco, J.G.; et al. Evolution and spread of Venezuelan equine encephalitis complex alphavirus in the Americas. PLoS Negl. Trop. Dis. 2017, 11, e0005693. [Google Scholar] [CrossRef]
- Parker, M.D.; Buckley, M.J.; Melanson, V.R.; Glass, P.J.; Norwood, D.; Hart, M.K. Antibody to the E3 glycoprotein protects mice against lethal venezuelan equine encephalitis virus infection. J. Virol. 2010, 84, 12683–12690. [Google Scholar] [CrossRef]
- Kautz, T.F.; Guerbois, M.; Khanipov, K.; Patterson, E.I.; Langsjoen, R.M.; Yun, R.; Warmbrod, K.L.; Fofanov, Y.; Weaver, S.C.; Forrester, N.L. Low-fidelity Venezuelan equine encephalitis virus polymerase mutants to improve live-attenuated vaccine safety and efficacy. Virus Evol. 2018, 4, vey004. [Google Scholar] [CrossRef]


| Target | Probe |
|---|---|
| 6K | ACAAT AACCA ACAGA TGTTC TGGAT TCAAT TGCTG ATCCC TCTGG CCGCC TTGAT CGTAG TGACT CGCCT GCTCA GGTGC GTGTG CTGTG TCGTG CCTTT |
| capsid | ATCGA CAACG ACGTT CTGGC CGCGC TTAAG ACGAA GAAAG CATCC AAATA CGATC TTGAG TATGC AGATG TGCCA CAGAA CATGC GGGCC GATAC ATTCA |
| E1 | CACCA GGGTG TCAGA AACAC CGACA CTTTC AGCGG CCGAA TGCAC TCTTA ACGAG TGCGT GTATT CTTCC GACTT TGGTG GGATC GCCAC GGTCA AGTAC |
| E2 | CTTAA AAGGA AAACT GCATG TCCCA TTCTT GCTGG CAGAC GGCAA ATGCA CCGTG CCTCT AGCAC CAGAA CCTAT GATAA CCTTC GGTTT CAGAT CAGTG |
| E3 | CCACC ATGTG TCTGC TCGCC AATGT GACGT TCCCA TGTGC TCAAC CACCA ATTTG CTACG ACAGA AAACC AGCAG AGACT TTGGC CATGC TCAGC GTTAA |
| nsP3 | GTGTG CTCAT CCTTT CCATT GCCGA AGTAT AGAAT CACTG GTGTG CAGAA GATCC AATGC TCCCA GCCTA TATTG TTCTC ACCGA AAGTG CCTGC GTATA |
| nsP4 | GCTGG TTAGG AGATT AAATG CGGTC CTGCT TCCGA ACATT CATAC ACTGT TTGAT ATGTC GGCTG AAGAC TTTGA CGCTA TTATA GCCGA GCACT TCCAG |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Johnson, D.M.; Sokoloski, K.J.; Jokinen, J.D.; Pfeffer, T.L.; Chu, Y.-K.; Adcock, R.S.; Chung, D.; Tretyakova, I.; Pushko, P.; Lukashevich, I.S. Advanced Safety and Genetic Stability in Mice of a Novel DNA-Launched Venezuelan Equine Encephalitis Virus Vaccine with Rearranged Structural Genes. Vaccines 2020, 8, 114. https://doi.org/10.3390/vaccines8010114
Johnson DM, Sokoloski KJ, Jokinen JD, Pfeffer TL, Chu Y-K, Adcock RS, Chung D, Tretyakova I, Pushko P, Lukashevich IS. Advanced Safety and Genetic Stability in Mice of a Novel DNA-Launched Venezuelan Equine Encephalitis Virus Vaccine with Rearranged Structural Genes. Vaccines. 2020; 8(1):114. https://doi.org/10.3390/vaccines8010114
Chicago/Turabian StyleJohnson, Dylan M., Kevin J. Sokoloski, Jenny D. Jokinen, Tia L. Pfeffer, Yong-Kyu Chu, Robert S. Adcock, Donghoon Chung, Irina Tretyakova, Peter Pushko, and Igor S. Lukashevich. 2020. "Advanced Safety and Genetic Stability in Mice of a Novel DNA-Launched Venezuelan Equine Encephalitis Virus Vaccine with Rearranged Structural Genes" Vaccines 8, no. 1: 114. https://doi.org/10.3390/vaccines8010114
APA StyleJohnson, D. M., Sokoloski, K. J., Jokinen, J. D., Pfeffer, T. L., Chu, Y.-K., Adcock, R. S., Chung, D., Tretyakova, I., Pushko, P., & Lukashevich, I. S. (2020). Advanced Safety and Genetic Stability in Mice of a Novel DNA-Launched Venezuelan Equine Encephalitis Virus Vaccine with Rearranged Structural Genes. Vaccines, 8(1), 114. https://doi.org/10.3390/vaccines8010114







