The Use of Analgesics during Vaccination with a Live Attenuated Yersinia pestis Vaccine Alters the Resulting Immune Response in Mice
Abstract
1. Introduction
2. Materials and Methods
2.1. Bacteria
2.2. Animals
2.3. Analgesia
2.4. Vaccination
2.5. Acetaminophen (ACE) Concentrations in Sera
2.6. Animal Challenges
2.7. Enzyme-Linked Immunosorbent Assay (ELISA)
2.8. Spleen Cell Preparations
2.9. Luminex Cytokine Assay
2.10. ELISpot
2.11. Pathology
2.12. Statistical Analyses
3. Results
3.1. Impact of Analgesic Administration on the Clinical Course of the Live Attenuated Y. pestis Vaccine
3.1.1. Clinical Observations
3.1.2. Draining Lymph Nodes
3.1.3. Lethality Associated with Vaccination and Analgesic Treatment
3.1.4. Mouse Weights Post Vaccination
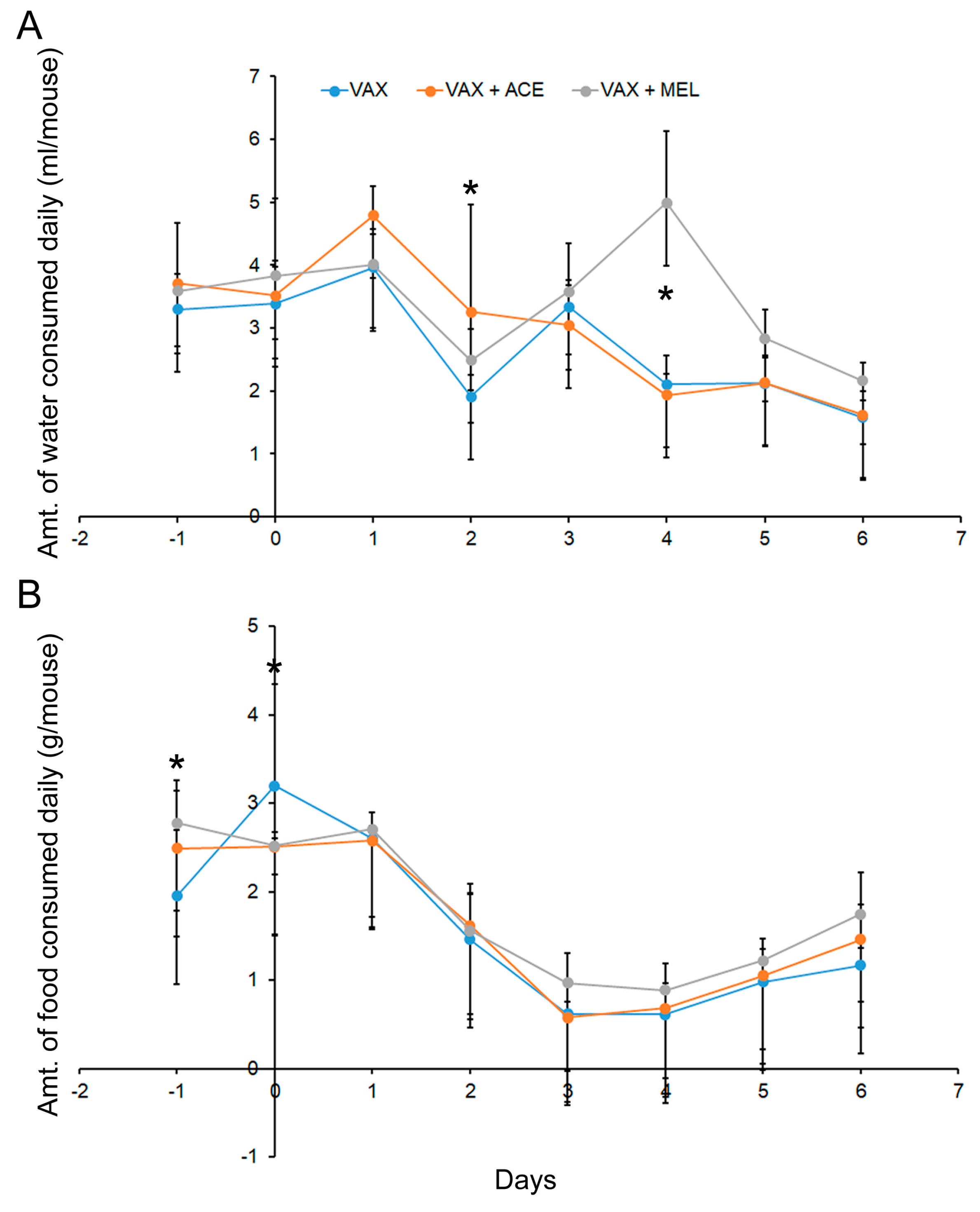
3.1.5. Food and Water Consumption
3.2. Impact of Analgesic Administration on the Resulting Immune Response after Vaccination with Live Y. pestis Vaccine: Cellular Immune Response
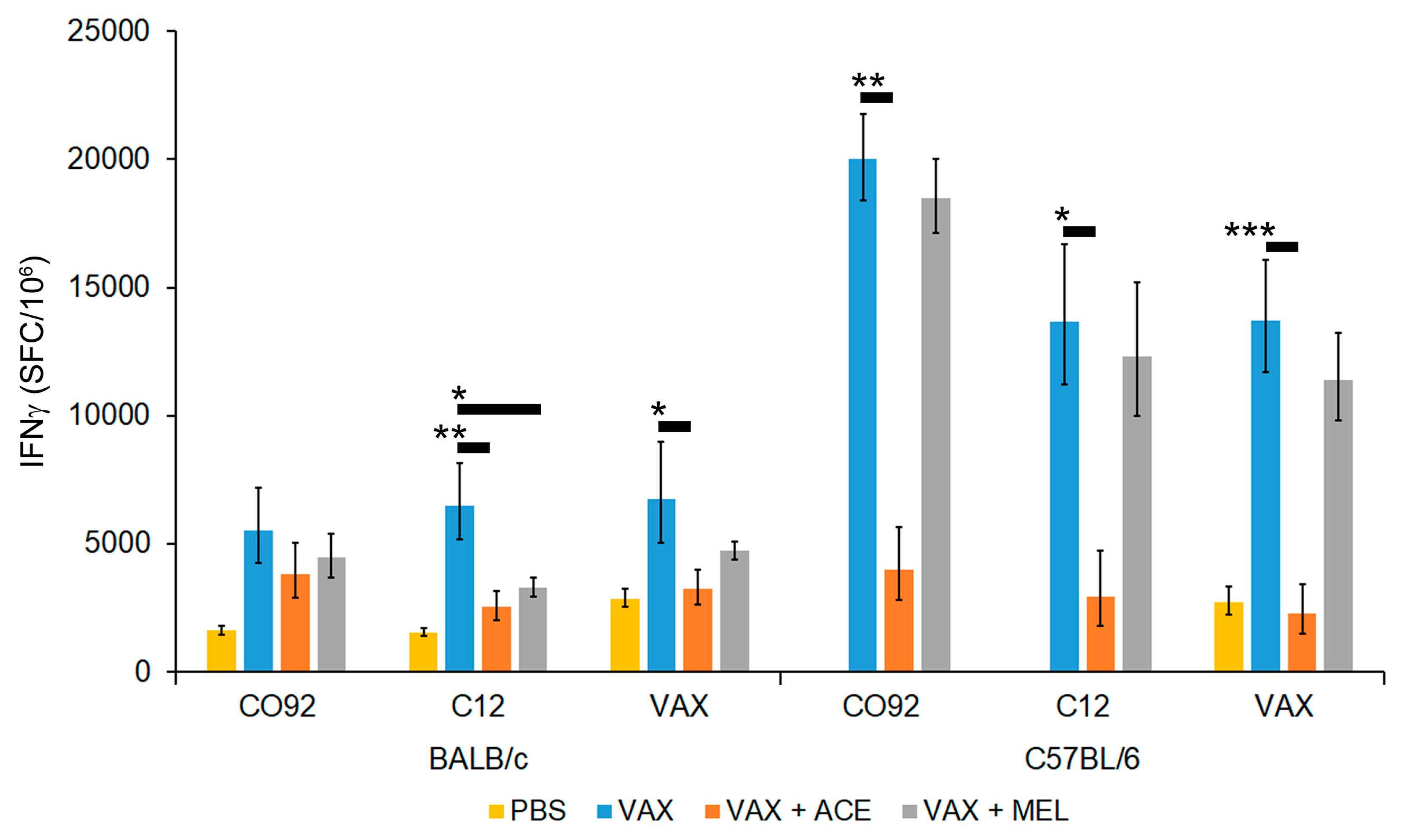
3.2.1. Analgesic Treatment of Mice during Vaccination with VAX Reduced Splenocyte IFN-γ Recall Response
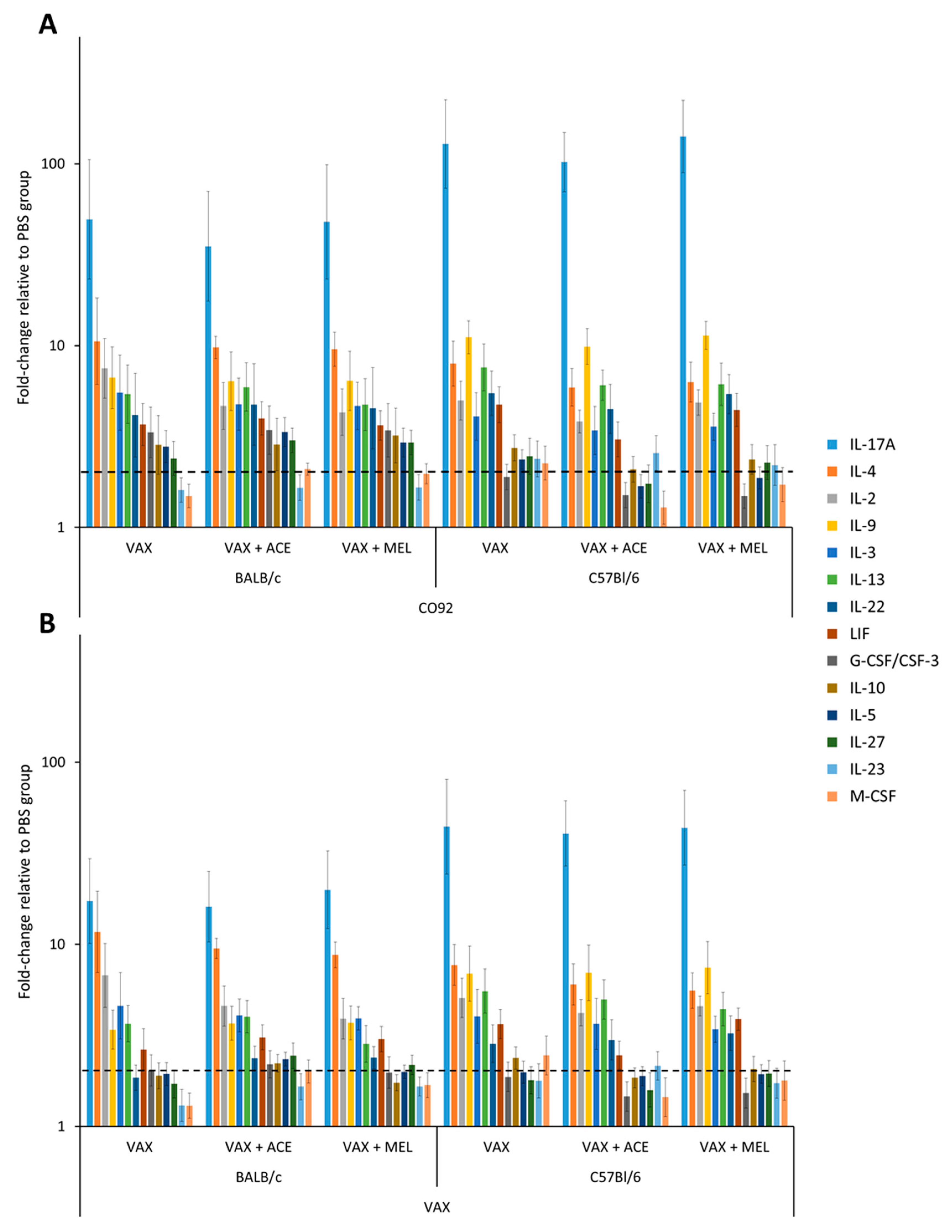
3.2.2. Cytokine Profiles from Vaccinated Mice Differ from Those Obtained from Controls and Show Trends of Cytokine Perturbation Associated with Analgesic Treatment
3.3. Impact of Analgesic Administration on the Resulting Immune Response after Vaccination with Live Y. pestis Vaccine: Humoral Immune Response
3.3.1. Total IgG Titers Were Not Significantly Impacted by Analgesia at Time of Vaccination
3.3.2. The IgG2a-to-IgG1 Titer Ratios Were Significantly Altered in BALB/C by the Use of Acetaminophen or Meloxicam at the Time of Vaccination
3.3.3. The IgG2c-to-IgG1 Titer Ratios Were Significantly Altered in C57BL/6 Mice by the Use of Acetaminophen at the Time of Vaccination
3.4. While Analgesia Did Alter Several Parameters of the Immune Response to the Vaccination, the Mice Were Protected from Infection with Virulent Y. pestis
3.4.1. Total IgG Titers of Mice Surviving Bubonic Plague Challenge Were Not Significantly Impacted by Analgesia Administered at Time of Vaccination
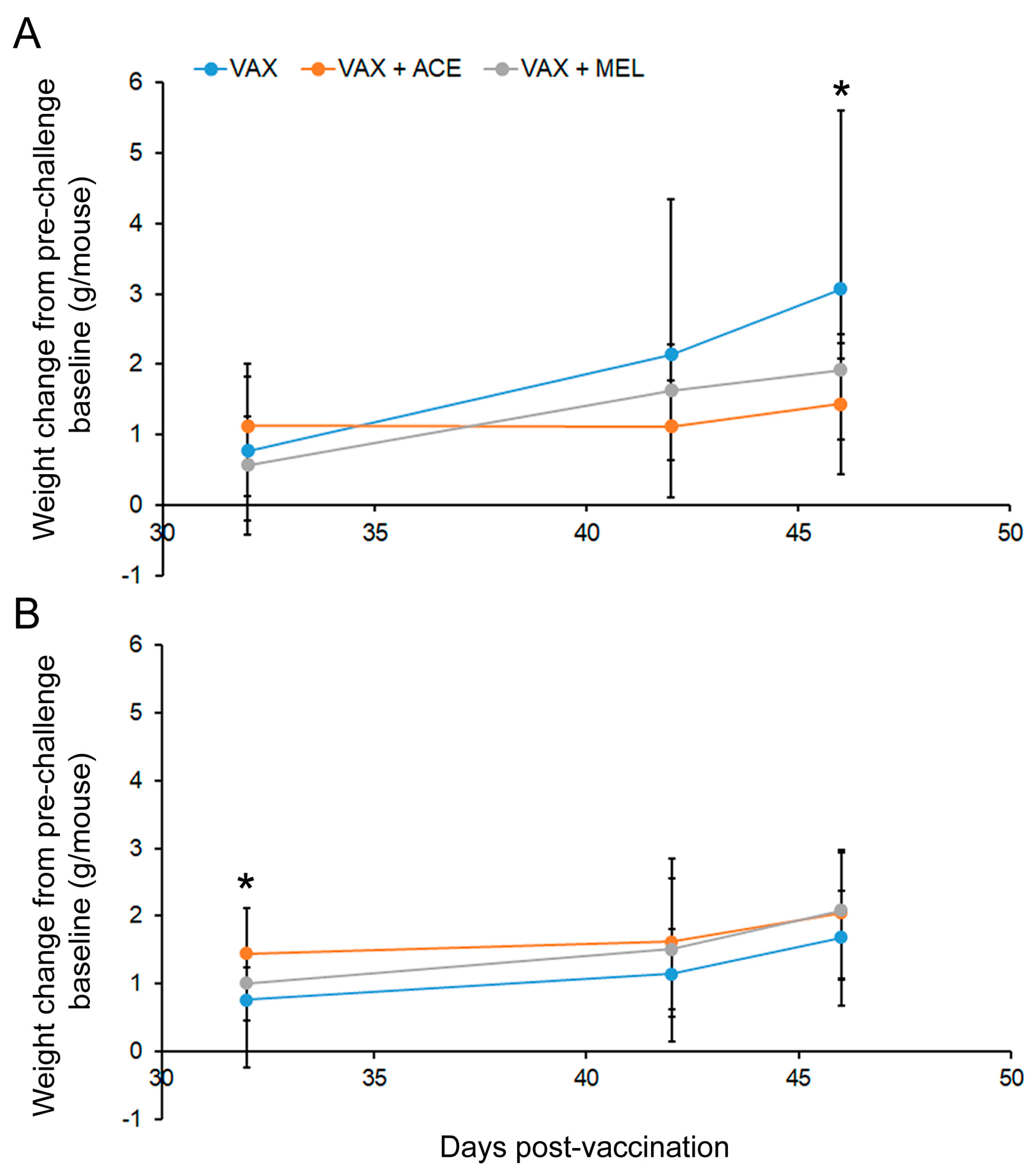
3.4.2. Mouse Weights Post Challenge
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Saleh, E.; Swamy, G.K.; Moody, M.A.; Walter, E.B. Parental approach to the prevention and management of fever and pain following childhood immunizations: A survey study. Clin. Pediatr. 2017, 56, 435–442. [Google Scholar] [CrossRef] [PubMed]
- Saleh, E.; Moody, M.A.; Walter, E.B. Effect of antipyretic analgesics on immune responses to vaccination. Hum. Vaccin. Immunother. 2016, 12, 2391–2402. [Google Scholar] [CrossRef] [PubMed]
- Prymula, R.; Siegrist, C.A.; Chlibek, R.; Zemlickova, H.; Vackova, M.; Smetana, J.; Lommel, P.; Kaliskova, E.; Borys, D.; Schuerman, L. Effect of prophylactic paracetamol administration at time of vaccination on febrile reactions and antibody responses in children: Two open-label, randomised controlled trials. Lancet 2009, 374, 1339–1350. [Google Scholar] [CrossRef]
- Homme, J.H.; Fischer, P.R. Randomised controlled trial: Prophylactic paracetamol at the time of infant vaccination reduces the risk of fever but also reduces antibody response. Evid. Based Med. 2010, 15, 50–51. [Google Scholar] [CrossRef]
- Prymula, R.; Habib, A.; Francois, N.; Borys, D.; Schuerman, L. Immunological memory and nasopharyngeal carriage in 4-year-old children previously primed and boosted with 10-valent pneumococcal non-typeable Haemophilus influenzae protein D conjugate vaccine (PHiD-CV) with or without concomitant prophylactic paracetamol. Vaccine 2013, 31, 2080–2088. [Google Scholar] [CrossRef]
- Whaley, K.; Sloane, D.J. Studies of the action of some anti-inflammatory drugs on complement mediated immune haemolysis. Br. J. Clin. Pharmacol. 1975, 2, 123–129. [Google Scholar] [CrossRef]
- Kolstad, A.M.; Rodriguez, R.M.; Kim, C.J.; Hale, L.P. Effect of pain management on immunization efficacy in mice. J. Am. Assoc. Lab. Anim. Sci. 2012, 51, 448–457. [Google Scholar]
- Minor, P.D. Live attenuated vaccines: Historical successes and current challenges. Virology 2015, 479, 379–392. [Google Scholar] [CrossRef]
- Detmer, A.; Glenting, J. Live bacterial vaccines—A review and identification of potential hazards. Microb. Cell Fact. 2006, 5, 23. [Google Scholar] [CrossRef]
- Chiu, I.M. Infection, Pain, and Itch. Neurosci. Bull. 2018, 34, 109–119. [Google Scholar] [CrossRef]
- Blake, K.J.; Baral, P.; Voisin, T.; Lubkin, A.; Pinho-Ribeiro, F.A.; Adams, K.L.; Roberson, D.P.; Ma, Y.C.; Otto, M.; Woolf, C.J. Staphylococcus aureus produces pain through pore-forming toxins and neuronal TRPV1 that is silenced by QX-314. Nat. Commun. 2018, 9, 37. [Google Scholar] [CrossRef] [PubMed]
- Das, R.R.; Panigrahi, I.; Naik, S.S. The effect of prophylactic antipyretic administration on post-vaccination adverse reactions and antibody response in children: A systematic review. PLoS ONE 2014, 9, e106629. [Google Scholar] [CrossRef] [PubMed]
- Manley, J.; Taddio, A. Acetaminophen and ibuprofen for prevention of adverse reactions associated with childhood immunization. Ann. Pharmacother. 2007, 41, 1227–1232. [Google Scholar] [CrossRef] [PubMed]
- Fleischmann, T.; Arras, M.; Sauer, M.; Saleh, L.; Rulicke, T.; Jirkof, P. Voluntary intake of paracetamol-enriched drinking water and its influence on the success of embryo transfer in mice. Res. Vet. Sci. 2017, 111, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Theisen, E.; McDougal, C.E.; Nakanishi, M.; Stevenson, D.M.; Amador-Noguez, D.; Rosenberg, D.W.; Knoll, L.J.; Sauer, J.D. Cyclooxygenase-1 and -2 play contrasting roles in Listeria-stimulated immunity. J. Immunol. 2018, 200, 3729–3738. [Google Scholar] [CrossRef] [PubMed]
- Vinegar, R.; Truax, J.F.; Selph, J.L. Quantitative comparison of the analgesic and anti-inflammatory activities of aspirin, phenacetin and acetaminophen in rodents. Eur. J. Pharmacol. 1976, 37, 23–30. [Google Scholar] [CrossRef]
- Gladtke, E. Use of antipyretic analgesics in the pediatric patient. Am. J. Med. 1983, 75, 121–126. [Google Scholar] [CrossRef]
- Botting, R.M. Mechanism of action of acetaminophen: Is there a cyclooxygenase 3? Clin. Infect. Dis. 2000, 31, S202–S210. [Google Scholar] [CrossRef]
- Yaffe, S.J. Comparative efficacy of aspirin and acetaminophen in the reduction of fever in children. Arch. Intern. Med. 1981, 141, 286–292. [Google Scholar] [CrossRef]
- Temple, A.R. Review of comparative antipyretic activity in children. Am. J. Med. 1983, 75, 38–46. [Google Scholar] [CrossRef]
- Cuestas, E. Acetaminophen may decrease antibody response in infants being immunized. J. Pediatr. 2010, 156, 857–858. [Google Scholar] [CrossRef] [PubMed]
- Bancos, S.; Bernard, M.P.; Topham, D.J.; Phipps, R.P. Ibuprofen and other widely used non-steroidal anti-inflammatory drugs inhibit antibody production in human cells. Cell. Immunol. 2009, 258, 18–28. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekharan, N.V.; Dai, H.; Roos, K.L.T.; Evanson, N.K.; Tomsik, J.; Elton, T.S.; Simmons, D.L. COX-3, a cyclooxygenase-1 variant inhibited by acetaminophen and other analgesic/antipyretic drugs: Cloning, structure, and expression. Proc. Natl. Acad. Sci. USA 2002, 99, 13926–13931. [Google Scholar] [CrossRef]
- Simmons, D.L.; Wagner, D.; Westover, K. Nonsteroidal anti-inflammatory drugs, acetaminophen, cyclooxygenase 2, and fever. Clin. Infect. Dis. 2000, 31, S211–S218. [Google Scholar] [CrossRef]
- Cooper, D.M.; DeLong, D.; Gillett, C.S. Analgesic efficacy of acetaminophen and buprenorphine administered in the drinking water of rats. Contemp. Top. Lab. Anim. Sci. 1997, 36, 58–62. [Google Scholar]
- Dickinson, A.L.; Leach, M.C.; Flecknell, P.A. The analgesic effects of oral paracetamol in two strains of mice undergoing vasectomy. Lab. Anim. 2009, 43, 357–361. [Google Scholar] [CrossRef]
- Flecknell, P. Rodent analgesia: Assessment and therapeutics. Vet. J. 2018, 232, 70–77. [Google Scholar] [CrossRef]
- Flecknell, P.A. The relief of pain in laboratory animals. Lab. Anim. 1984, 18, 147–160. [Google Scholar] [CrossRef]
- Furedi, R.; Bolcskei, K.; Szolcsanyi, J.; Petho, G. Effects of analgesics on the plantar incision-induced drop of the noxious heat threshold measured with an increasing-temperature water bath in the rat. Eur. J. Pharmacol. 2009, 605, 63–67. [Google Scholar] [CrossRef]
- Lahoti, A.; Kalra, B.S.; Tekur, U. Evaluation of the analgesic and anti-inflammatory activity of fixed dose combination: Non-steroidal anti-inflammatory drugs in experimental animals. Indian J. Dent. Res. 2014, 25, 551–554. [Google Scholar]
- Matsumiya, L.C.; Sorge, R.E.; Sotocinal, S.G.; Tabaka, J.M.; Wieskopf, J.S.; Zaloum, A.; King, O.D.; Mogil, J.S. Using the Mouse Grimace Scale to reevaluate the efficacy of postoperative analgesics in laboratory mice. J. Am. Assoc. Lab. Anim. Sci. 2012, 51, 42–49. [Google Scholar] [PubMed]
- Mickley, G.A.; Hoxha, Z.; Biada, J.M.; Kenmuir, C.L.; Bacik, S.E. Acetaminophen self-administered in the drinking water increases the pain threshold of rats (Rattus norvegicus). J. Am. Assoc. Lab. Anim. Sci. 2006, 45, 48–54. [Google Scholar] [PubMed]
- Richardson, C.A.; Flecknell, P.A. Anaesthesia and post-operative analgesia following experimental surgery in laboratory rodents: Are we making progress? Altern. Lab. Anim. 2005, 33, 119–127. [Google Scholar] [CrossRef] [PubMed]
- Srikiatkhachorn, A.; Tarasub, N.; Govitrapong, P. Acetaminophen-induced antinociception via central 5-HT(2A) receptors. Neurochem. Int. 1999, 34, 491–498. [Google Scholar] [CrossRef]
- St, A.S.L.; Martin, W.J. Evaluation of postoperative analgesia in a rat model of incisional pain. Contemp. Top. Lab. Anim. Sci. 2003, 42, 28–34. [Google Scholar]
- Liu, B.; Qu, L.; Yan, S. Cyclooxygenase-2 promotes tumor growth and suppresses tumor immunity. Cancer Cell Int. 2015, 15, 106. [Google Scholar] [CrossRef]
- Friton, G.M.; Schmidt H Fau-Schrodl, W.; Schrodl, W. Clinical and anti-inflammatory effects of treating endotoxin-challenged pigs with meloxicam. Vet. Rec. 2006, 159, 552–557. [Google Scholar] [CrossRef]
- Chang, C.-L.; Ma, B.; Pang, X.; Wu, T.C.; Hung, C.-F. Treatment with cyclooxygenase-2 inhibitors enables repeated administration of vaccinia virus for control of ovarian cancer. Mol. Ther. 2009, 17, 1365–1372. [Google Scholar] [CrossRef]
- Andrianaivoarimanana, V.; Kreppel, K.; Duplantier, J.M.; Carniel, E.; Rajerison, M.; Jambou, R. Understanding the persistence of plague foci in Madagascar. PLoS Negl. Trop. Dis. 2013, 7, e2382. [Google Scholar] [CrossRef]
- Stenseth, N.C.; Atshabar, B.B.; Begon, M.; Belmain, S.R.; Bertherat, E.; Carniel, E.; Gage, K.L.; Leirs, H.; Rahalison, L. Plague: Past, present, and future. PLoS Med. 2008, 5, e3. [Google Scholar] [CrossRef]
- Andrianaivoarimanana, V.; Piola, P.; Wagner, D.M.; Rakotomanana, F.; Maheriniaina, V.; Andrianalimanana, S.; Chanteau, S.; Rahalison, L.; Ratsitorahina, M.; Rajerison, M. Trends of human plague, madagascar, 1998–2016. Emerg. Infect. Dis. 2019, 25, 220–228. [Google Scholar] [CrossRef] [PubMed]
- Randremanana, R.; Andrianaivoarimanana, V.; Nikolay, B.; Ramasindrazana, B.; Paireau, J.; Ten Bosch, Q.A.; Rakotondramanga, J.M.; Rahajandraibe, S.; Rahelinirina, S.; Rakotomanana, F. Epidemiological characteristics of an urban plague epidemic in Madagascar, August-November, 2017: An outbreak report. Lancet Infect. Dis. 2019, 19, 537–545. [Google Scholar] [CrossRef]
- Connor, M.G.; Pulsifer, A.R.; Chung, D.; Rouchka, E.C.; Ceresa, B.K.; Lawrenz, M.B. Yersinia pestis targets the host endosome recycling pathway during the biogenesis of the Yersinia-containing vacuole to avoid killing by macrophages. MBio 2018, 9, e01800–e01817. [Google Scholar] [CrossRef] [PubMed]
- Perry, R.D.; Fetherston, J.D. Yersinia pestis—Etiologic agent of plague. Clin. Microbiol. Rev. 1997, 10, 35–66. [Google Scholar] [CrossRef]
- Inglesby, T.V.; Dennis, D.T.; Henderson, D.A.; Batlett, J.G.; Ascher, M.S.; Eitzen, E.; Fine, A.D.; Friedlander, A.M.; Hauer, J.; Koerner, J.F. Plague as a biological weapon: Medical and public health management. Work. Group Civ. Biodefense JAMA 2000, 283, 2281–2290. [Google Scholar] [CrossRef]
- Feodorova, V.A.; Motin, V.L. Humoral and cellular immune responses to Yersinia pestis Pla antigen in humans immunized with live plague vaccine. PLoS Negl. Trop. Dis. 2018, 12, e0006511. [Google Scholar] [CrossRef]
- Feodorova, V.A.; Motin, V.L. Plague vaccines: Current developments and future perspectives. Emerg. Microbes Infect. 2012, 1, e36. [Google Scholar] [CrossRef]
- Feodorova, V.A.; Sayapina, L.V.; Motin, V.L. Assessment of live plague vaccine candidates. Methods Mol. Biol. 2016, 1403, 487–498. [Google Scholar]
- Andersson, J.A.; Sha, J.; Erova, T.E.; Fitts, E.C.; Ponnusamy, D.; Kozlova, E.V.; Kirtley, M.L.; Chopra, A.K. Identification of New Virulence Factors and Vaccine Candidates for Yersinia pestis. Front. Cell. Infect. Microbiol. 2017, 7, 448. [Google Scholar] [CrossRef]
- Doll, J.M.; Zeitz, P.S.; Ettestad, P.; Bucholtz, A.L.; Davis, T.; Gage, K. Cat-transmitted fatal pneumonic plague in a person who traveled from Colorado to Arizona. Am. J. Trop. Med. Hyg. 1994, 51, 109–114. [Google Scholar] [CrossRef]
- Worsham, P.L.; Stein, M.P.; Welkos, S.L. Construction of defined F1 negative mutants of virulent Yersinia pestis. Contrib. Microbiol. Immunol. 1995, 13, 325–328. [Google Scholar]
- Welkos, S.; Pitt, M.L.; Martinez, M.; Friedlander, A.; Vogel, P.; Tammariello, R. Determination of the virulence of the pigmentation-deficient and pigmentation-/plasminogen activator-deficient strains of Yersinia pestis in non-human primate and mouse models of pneumonic plague. Vaccine 2002, 20, 2206–2214. [Google Scholar] [CrossRef]
- Welkos, S.L.; Friedlander, A.M.; Davis, K.J. Studies on the role of plasminogen activator in systemic infection by virulent Yersinia pestis strain C092. Microb. Pathog. 1997, 23, 211–223. [Google Scholar] [CrossRef]
- Jenkins, A.L.; Worsham, P.L.; Welkos, S.L. A strategy to verify the absence of the pgm locus in Yersinia pestis strain candidates for select agent exemption. J. Microbiol. Methods 2009, 77, 316–319. [Google Scholar] [CrossRef]
- National Research Council. Guide for the Care and Use of Laboratory Animals, 8th ed.; The National Academies Press: Washington, DC, USA, 2011; p. 246. [Google Scholar]
- Bachmanov, A.A.; Reed, D.R.; Beauchamp, G.K.; Tordoff, M.G. Food intake, water intake, and drinking spout side preference of 28 mouse strains. Behav. Genet. 2002, 32, 435–443. [Google Scholar] [CrossRef]
- Brunell, M.; Olsen, C.; Christy, A.; Maxwell, B.; Bentzel, D. Evaluation of consumption of self-administered acetaminophen in drinking water and two gel delivery system in C57BL/6 mice. Internet J. Vet. Med. 2017, 14, 1–11. [Google Scholar]
- Kohn, D.F.; Wixson, S.K.; White, W.J.; Benson, G.J. (Eds.) Anesthesia and Analgesia in Laboratory Animals, 2nd ed.; Elsevier: New York, NY, USA, 2008; p. 672. [Google Scholar]
- Mayer, J.; Mans, C. Chapter 9-Rodents, in Exotic Animal Formulary, 5th ed.; Carpenter, J.W., Marion, C.J., Eds.; W.B. Saunders: Philadelphia, PA, USA, 2018; pp. 459–493. [Google Scholar]
- Amemiya, K.; Meyers, J.L.; Trevino, S.R.; Chanh, T.C.; Norris, S.L.; Waag, D.M. Interleukin-12 induces a Th1-like response to Burkholderia mallei and limited protection in BALB/c mice. Vaccine 2006, 24, 1413–1420. [Google Scholar] [CrossRef]
- Bearss, J.J.; Hunter, M.; Dankmeyer, J.L.; Fritts, K.A.; Klimko, C.P.; Weaver, C.H.; Shoe, J.L.; Quirk, A.V.; Toothman, R.G.; Webster, W.M. Characterization of pathogenesis of and immune response to Burkholderia pseudomallei K96243 using both inhalational and intraperitoneal infection models in BALB/c and C57BL/6 mice. PLoS ONE 2017, 12, e0172627. [Google Scholar] [CrossRef]
- Fetherston, J.D.; Perry, R.D. The pigmentation locus of Yersinia pestis KIM6+ is flanked by an insertion sequence and includes the structural genes for pesticin sensitivity and HMWP2. Mol. Microbiol. 1994, 13, 697–708. [Google Scholar] [CrossRef]
- Fetherston, J.D.; Schuetze, P.; Perry, R.D. Loss of the pigmentation phenotype in Yersinia pestis is due to the spontaneous deletion of 102 kb of chromosomal DNA which is flanked by a repetitive element. Mol. Microbiol. 1992, 6, 2693–2704. [Google Scholar] [CrossRef]
- Lucier, T.S.; Fetherston, J.D.; Brubaker, R.R.; Perry, R.D. Iron uptake and iron-repressible polypeptides in Yersinia pestis. Infect. Immun. 1996, 64, 3023–3031. [Google Scholar] [PubMed]
- Ferber, D.M.; Brubaker, R.R. Plasmids in Yersinia pestis. Infect. Immun. 1981, 31, 839–841. [Google Scholar] [PubMed]
- Sodeinde, O.A.; Subrahmanyam, Y.V.; Stark, K.; Quan, T.; Bao, Y.; Goguen, J.D. A surface protease and the invasive character of plague. Science 1992, 258, 1004–1007. [Google Scholar] [CrossRef] [PubMed]
- Wilson, S.G.; Smith, S.B.; Chesler, E.J.; Melton, K.A.; Haas, J.J.; Mitton, B.; Strasburg, K.; Hubert, L.; Rodriguez-Zas, S.L.; Mogil, J.S. The heritability of antinociception: common pharmacogenetic mediation of five neurochemically distinct analgesics. J. Pharmacol. Exp. Ther. 2003, 304, 547. [Google Scholar] [CrossRef]
- Saharinen, P.; Tammela, T.; Karkkainen, M.J.; Alitalo, K. Lymphatic vasculature: Development, molecular regulation and role in tumor metastasis and inflammation. Trends Immunol. 2004, 25, 387–395. [Google Scholar] [CrossRef]
- Harrell, M.I.; Iritani, B.M.; Ruddell, A. Lymph node mapping in the mouse. J. Immunol. Methods 2008, 332, 170–174. [Google Scholar] [CrossRef]
- Jiskoot, W.; Kijanka, G.; Randolph, T.W.; Carpenter, J.F.; Koulov, A.V.; Mahler, H.-C.; Joubert, M.K.; Jawa, V.; Narhi, L.O. Mouse models for assessing protein immunogenicity: Lessons and challenges. J. Pharm. Sci. 2016, 105, 1567–1575. [Google Scholar] [CrossRef]
- Morokata, T.; Ishikawa, J.; Yamada, T. Antigen dose defines T helper 1 and T helper 2 responses in the lungs of C57BL/6 and BALB/c mice independently of splenic responses. Immunol. Lett. 2000, 72, 119–126. [Google Scholar] [CrossRef]
- Dash, B.; Shapiro, M.J.; Chung, J.Y.; Romero-Arocha, S.; Shapiro, V.S. Treg-specific deletion of NKAP results in severe, systemic autoimmunity due to peripheral loss of Tregs. J. Autoimmun. 2018, 89, 139–148. [Google Scholar] [CrossRef]
- Hadaschik, E.N.; Wei, X.; Leiss, H.; Heckmann, B.; Niederreiter, B.; Steiner, G.; Ulrich, W.; Enk, A.H.; Smolen, J.S.; Stummvoll, G.H. Regulatory T cell-deficient scurfy mice develop systemic autoimmune features resembling lupus-like disease. Arthritis Res. Ther. 2015, 17, 35. [Google Scholar] [CrossRef]
- Lyon, M.F.; Peters, J.; Glenister, P.H.; Ball, S.; Wright, E. The scurfy mouse mutant has previously unrecognized hematological abnormalities and resembles Wiskott-Aldrich syndrome. Proc. Natl. Acad. Sci. USA 1990, 87, 2433–2437. [Google Scholar] [CrossRef]
- Barthold, S.W.; Griffey, S.M.; Percy, D.H. Pathology of Laboratory Rodents and Rabbits, 4th ed; John Wiley & Sons: Hoboken, NJ, USA, 2016. [Google Scholar]
- Jirkof, P. Side effects of pain and analgesia in animal experimentation. Lab. Anim. 2017, 46, 123–128. [Google Scholar] [CrossRef]
- Sabhnani, L.; Rao, D.N. Identification of immunodominant epitope of F1 antigen of Yersinia pestis. FEMS Immunol. Med. Microbiol. 2000, 27, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Williams, R.C., Jr.; Gewurz, H.; Quie, P.G. Effects of fraction I from Yersinia pestis on phagocytosis in vitro. J. Infect. Dis. 1972, 126, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Friedlander, A.M.; Welkos, S.L.; Worsham, P.L.; Andrews, G.P.; Heath, D.G.; Anderson, G.W.; Pitt, M.L.; Estep, J.; Davis, K. Relationship between virulence and immunity as revealed in recent studies of the F1 capsule of Yersinia pestis. Clin. Infect. Dis. 1995, 21, S178–S181. [Google Scholar] [CrossRef]
- Welkos, S.L.; Davis, K.M.; Pitt, L.M.; Worsham, P.L.; Friedlander, A.M. Studies on the contribution of the F1 capsule-associated plasmid pFra to the virulence of Yersinia pestis. Contrib. Microbiol. Immunol. 1995, 13, 299–305. [Google Scholar]
- Martin, R.M.; Brady, J.L.; Lew, A.M. The need for IgG2c specific antiserum when isotyping antibodies from C57BL/6 and NOD mice. J. Immunol. Methods 1998, 212, 187–192. [Google Scholar] [CrossRef]
- Morgado, M.G.; Cam, P.; Gris-Liebe, C.; Cazenave, P.A.; Jouvin-Marche, E. Further evidence that BALB/c and C57BL/6 gamma 2a genes originate from two distinct isotypes. EMBO J. 1989, 8, 3245–3251. [Google Scholar] [CrossRef]
- Engelhardt, G. Pharmacology of meloxicam, a new non-steroidal anti-inflammatory drug with an improved safety profile through preferential inhibition of COX-2. Br. J. Rheumatol. 1996, 35, 4–12. [Google Scholar] [CrossRef]
- Engelhardt, G.; Homma, D.; Schlegel, K.; Schnitzler, C.; Utzmann, R. General pharmacology of meloxicam—Part II: Effects on blood pressure, blood flow, heart rate, ECG, respiratory minute volume and interactions with paracetamol, pirenzepine, chlorthalidone, phenprocoumon and tolbutamide. Gen. Pharmacol. 1996, 27, 679–688. [Google Scholar] [CrossRef]
- Engelhardt, G.; Homma, D.; Schlegel, K.; Schnitzler, C.; Utzmann, R. General pharmacology of meloxicam—Part I: Effects on CNS, gastric emptying, intestinal transport, water, electrolyte and creatinine excretion. Gen. Pharmacol. 1996, 27, 673–677. [Google Scholar] [CrossRef]
- Bauer, D.J.; Christenson, T.J.; Clark, K.R.; Powell, S.K.; Swain, R.A. Acetaminophen as a postsurgical analgesic in rats: A practical solution to neophobia. Contemp. Top. Lab. Anim. Sci. 2003, 42, 20–25. [Google Scholar] [PubMed]
- Guler, M.L.; Gorham, J.D.; Hsieh, C.S.; Mackey, A.J.; Steen, R.G.; Dietrich, W.F.; Murphy, K.M. Genetic susceptibility to Leishmania: IL-12 responsiveness in TH1 cell development. Science 1996, 271, 984–987. [Google Scholar] [CrossRef] [PubMed]
- Reiner, S.L.; Locksley, R.M. The regulation of immunity to Leishmania major. Annu. Rev. Immunol. 1995, 13, 151–177. [Google Scholar] [CrossRef]
- Xu, D.; Trajkovic, V.; Hunter, D.; Leung, B.P.; Schulz, K.; Gracie, J.A.; McInnes, I.B.; Liew, F.Y. IL-18 induces the differentiation of Th1 or Th2 cells depending upon cytokine milieu and genetic background. Eur. J. Immunol. 2000, 30, 3147–3156. [Google Scholar] [CrossRef]
- Bohn, E.; Heesemann, J.; Ehlers, S.; Autenrieth, I.B. Early gamma interferon mRNA expression is associated with resistance of mice against Yersinia enterocolitica. Infect. Immun. 1994, 62, 3027–3032. [Google Scholar]
- Ulett, G.C.; Ketheesan, N.; Hirst, R.G. Cytokine gene expression in innately susceptible BALB/c mice and relatively resistant C57BL/6 mice during infection with virulent Burkholderia pseudomallei. Infect. Immun. 2000, 68, 2034–2042. [Google Scholar] [CrossRef]
- Autenrieth, I.B.; Beer, M.; Bohn, E.; Kaufmann, S.H.; Heesemann, J. Immune responses to Yersinia enterocolitica in susceptible BALB/c and resistant C57BL/6 mice: An essential role for gamma interferon. Infect. Immun. 1994, 62, 2590–2599. [Google Scholar]
- Kopf, M.; Le Gros, G.; Bachmann, M.; Lamers, M.C.; Bluethmann, H.; Kohler, G. Disruption of the murine IL-4 gene blocks Th2 cytokine responses. Nature 1993, 362, 245–248. [Google Scholar] [CrossRef]
- Ishigame, H.; Nakajima, A.; Saijo, S.; Komiyama, Y.; Nambu, A.; Matsuki, T.; Nakae, S.; Horai, R.; Kakuta, S.; Iwakura, Y. The role of TNFalpha and IL-17 in the development of excess IL-1 signaling-induced inflammatory diseases in IL-1 receptor antagonist-deficient mice. In Ernst Schering Research Foundation Workshop; Springer: Berlin, Germany, 2006; pp. 129–153. [Google Scholar]
- Iwakura, Y.; Ishigame, H. The IL-23/IL-17 axis in inflammation. J. Clin. Investig. 2006, 116, 1218–1222. [Google Scholar] [CrossRef]
- Chinen, T.; Kannan, A.K.; Levine, A.G.; Fan, X.; Klein, U.; Zheng, Y.; Gasteiger, G.; Feng, Y.; Fontenot, J.D.; Rudensky, A.Y. An essential role for the IL-2 receptor in Treg cell function. Nat. Immunol. 2016, 17, 1322–1333. [Google Scholar] [CrossRef] [PubMed]
- Malek, T.R. The main function of IL-2 is to promote the development of T regulatory cells. J. Leukoc. Biol. 2003, 74, 961–965. [Google Scholar] [CrossRef] [PubMed]
- El-Gowelli, H.M.; Helmy, H.M.; Ali, R.W.; El-Mas, M.M. Celecoxib offsets the negative renal influences of cyclosporine via modulation of the TGF-beta1/IL-2/COX-2/endothelin ET(B) receptor cascade. Toxicol. Appl. Pharmacol. 2014, 275, 88–95. [Google Scholar] [CrossRef] [PubMed]
- Hamada, T.; Tsuchihashi, S.; Avanesyan, A.; Duarte, S.; Moore, C.; Busuttil, R.W.; Coito, A.J. Cyclooxygenase-2 deficiency enhances Th2 immune responses and impairs neutrophil recruitment in hepatic ischemia/reperfusion injury. J. Immunol. 2008, 180, 1843–1853. [Google Scholar] [CrossRef] [PubMed]
- Laouini, D.; Elkhal, A.; Yalcindag, A.; Kawamoto, S.; Oettgen, H.; Geha, R.S. COX-2 inhibition enhances the TH2 immune response to epicutaneous sensitization. J. Allergy Clin. Immunol. 2005, 116, 390–396. [Google Scholar] [CrossRef]
- Nakajima, S.; Honda, T.; Sakata, D.; Egawa, G.; Tanizaki, H.; Otsuka, A.; Moniaga, C.S.; Watanabe, T.; Miyachi, Y.; Narumiya, S.; et al. Prostaglandin I2-IP signaling promotes Th1 differentiation in a mouse model of contact hypersensitivity. J. Immunol. 2010, 184, 5595–5603. [Google Scholar] [CrossRef]
- Lin, J.S.; Kummer, L.W.; Szaba, F.M.; Smiley, S.T. IL-17 contributes to cell-mediated defense against pulmonary Yersinia pestis infection. J. Immunol. 2011, 186, 1675–1684. [Google Scholar] [CrossRef]
- Basu, S.; Hodgson, G.; Katz, M.; Dunn, A.R. Evaluation of role of G-CSF in the production, survival, and release of neutrophils from bone marrow into circulation. Blood 2002, 100, 854–861. [Google Scholar] [CrossRef]
- Bohle, B.; Kinaciyan, T.; Gerstmayr, M.; Radakovics, A.; Jahn-Schmid, B.; Ebner, C. Sublingual immunotherapy induces IL-10-producing T regulatory cells, allergen-specific T-cell tolerance, and immune deviation. J. Allergy Clin. Immunol. 2007, 120, 707–713. [Google Scholar] [CrossRef]
- Harizi, H.; Juzan, M.; Pitard, V.; Moreau, J.F.; Gualde, N. Cyclooxygenase-2-issued prostaglandin e(2) enhances the production of endogenous IL-10, which down-regulates dendritic cell functions. J. Immunol. 2002, 168, 2255–2263. [Google Scholar] [CrossRef]
- Hsu, P.; Santner-Nanan, B.; Hu, M.; Skarratt, K.; Lee, C.H.; Stormon, M.; Wong, M.; Fuller, S.J.; Nanan, R. IL-10 Potentiates differentiation of human induced regulatory T Cells via STAT3 and Foxo1. J. Immunol. 2015, 195, 3665–3674. [Google Scholar] [CrossRef] [PubMed]
- Quinton, L.J.; Mizgerd, J.P.; Hilliard, K.L.; Jones, M.R.; Kwon, C.Y.; Allen, E. Leukemia inhibitory factor signaling is required for lung protection during pneumonia. J. Immunol. 2012, 188, 6300–6308. [Google Scholar] [CrossRef] [PubMed]
- Nasef, A.; Mazurier, C.; Bouchet, S.; Ffrancois, S.; Chapel, A.; Thierry, D.; Gorin, N.C.; Fouillard, L. Leukemia inhibitory factor: Role in human mesenchymal stem cells mediated immunosuppression. Cell. Immunol. 2008, 253, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.K.; Ren, L.; Wei, Y.; Zhu, D.X.; Miao, C.H.; Xu, J.M. General anesthesia combined with epidural anesthesia ameliorates the effect of fast-track surgery by mitigating immunosuppression and facilitating intestinal functional recovery in colon cancer patients. Int. J. Colorectal. Dis. 2015, 30, 475–481. [Google Scholar] [CrossRef] [PubMed]
- Sofra, M.; Fei, P.C.; Fabrizi, L.; Marcelli, M.E.; Claroni, C.; Gallucci, M.; Ensoli, F.; Forastiere, E. Immunomodulatory effects of total intravenous and balanced inhalation anesthesia in patients with bladder cancer undergoing elective radical cystectomy: Preliminary results. J. Exp. Clin. Cancer Res. 2013, 32, 6. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Pan, S.B.; Lyu, Q.H.; Wu, P.; Qin, G.M.; Wang, Q.; He, Z.L.; He, X.M.; Wu, M.; Chen, G. Postoperative regulatory T-Cells and natural killer cells in stage i nonsmall cell lung cancer underwent video-assisted thoracoscopic lobectomy or thoracotomy. Chin. Med. J. 2015, 128, 1502–1509. [Google Scholar] [CrossRef] [PubMed]
- Ndure, J.; Noho-Konteh, F.; Adetifa, J.U.; Cox, M.; Barker, F.; Le, M.T.; Sanyang, L.C.; Drammeh, A.; Whittle, H.C.; Clarke, E. Negative correlation between circulating CD+FOXP3+CD127- regulatory T cells and subsequent antibody responses to infant measles vaccine but not diphtheria-tetanus-pertussis vaccine implies regulatory role. Front. Immunol. 2017, 8, 921. [Google Scholar] [CrossRef]
- Liu, B.; Zhao, H.; Poon, M.C.; Han, Z.; Gu, D.; Xu, M.; Jia, H.; Yang, R.; Han, Z.C. Abnormality of CD4+CD25+ regulatory T cells in idiopathic thrombocytopenic purpura. Eur. J. Haematol. 2007, 78, 139–143. [Google Scholar] [CrossRef]
- Miller, E.; Waight, P.; Farrington, P.; Andrews, N.; Stowe, J.; Taylor, B. Idiopathic thrombocytopenic purpura and MMR vaccine. Arch. Dis. Child. 2001, 84, 227–229. [Google Scholar] [CrossRef]
- Sakakura, M.; Wada, H.; Tawara, I.; Nobori, T.; Sugiyama, T.; Sagawa, N.; Shiku, H. Reduced CD4+ CD25+ T cells in patients with idiopathic thrombocytopenic purpura. Thromb. Res. 2007, 120, 187–193. [Google Scholar] [CrossRef]
- Attia, P.; Phan, G.Q.; Maker, A.V.; Robinson, M.R.; Quezado, M.M.; Yang, J.C.; Sherry, R.M.; Topalian, S.L.; Kammula, U.S.; Royal, R.E. Autoimmunity correlates with tumor regression in patients with metastatic melanoma treated with anti-cytotoxic T-lymphocyte antigen-4. J. Clin. Oncol. 2005, 23, 6043–6053. [Google Scholar] [CrossRef] [PubMed]
- Maker, A.V.; Attia, P.; Rosenberg, S.A. Analysis of the cellular mechanism of antitumor responses and autoimmunity in patients treated with CTLA-4 blockade. J. Immunol. 2005, 175, 7746–7754. [Google Scholar] [CrossRef] [PubMed]
- Maker, A.V.; Phan, G.Q.; Attia, P.; Yang, J.C.; Sherry, R.M.; Topalian, S.L.; Kammula, U.S.; Royal, R.E.; Haworth, L.R.; Levy, C. Tumor regression and autoimmunity in patients treated with cytotoxic T lymphocyte-associated antigen 4 blockade and interleukin 2: A phase I/II study. Ann. Surg. Oncol. 2005, 12, 1005–1016. [Google Scholar] [CrossRef] [PubMed]
- Daifalla, N.S.; Bayih, A.G.; Gedamu, L. Differential Immune Response against Recombinant Leishmania donovani Peroxidoxin 1 and Peroxidoxin 2 Proteins in BALB/c Mice. J. Immunol. Res. 2015, 2015, 348401. [Google Scholar] [CrossRef] [PubMed]
- Rostamian, M.; Sohrabi, S.; Kavosifard, H.; Niknam, H.M. Lower levels of IgG1 in comparison with IgG2a are associated with protective immunity against Leishmania tropica infection in BALB/c mice. J. Microbiol. Immunol. Infect. 2017, 50, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Martin, R.M.; Silva, A.; Lew, A.M. The Igh-1 sequence of the non-obese diabetic (NOD) mouse assigns it to the IgG2c isotype. Immunogenetics 1997, 46, 167–168. [Google Scholar] [CrossRef]
- Singh, V.K.; Mehrotra, S.; Agarwal, S.S. The paradigm of Th1 and Th2 cytokines: Its relevance to autoimmunity and allergy. Immunol. Res. 1999, 20, 147–161. [Google Scholar] [CrossRef]
- Snapper, C.M.; Peschel, C.; Paul, W.E. IFN-gamma stimulates IgG2a secretion by murine B cells stimulated with bacterial lipopolysaccharide. J. Immunol. 1988, 140, 2121–2127. [Google Scholar]
- Heffernan, J.M.; Keeling, M.J. Implications of vaccination and waning immunity. Proc. Biol. Sci. 2009, 276, 2071–2080. [Google Scholar] [CrossRef]
- Ivins, B.E.; Fellows, P.F.; Pitt, M.L.M.; Estep, J.E.; Welkos, S.L.; Worsham, P.L.; Friedlander, A.M. Efficacy of standard human anthrax vaccine against Bacillus anthracis aerosol spore challenge in rhesus monkeys. Salisb. Med Bull. 1996, 87, 125–126. [Google Scholar]
- Sarda, V.; Kaslow, D.C.; Williamson, K.C. Approaches to malaria vaccine development using the retrospectroscope. Infect. Immun. 2009, 77, 3130–3140. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Whittle, H.C.; Aaby, P.; Samb, B.; Jensen, H.; Bennett, J.; Simondon, F. Effect of subclinical infection on maintaining immunity against measles in vaccinated children in West Africa. Lancet 1999, 353, 98–102. [Google Scholar] [CrossRef]
- Bowen, W.; Batra, L.; Pulsifer, A.R.; Yolcu, E.S.; Lawrenz, M.B.; Shirwan, H. Robust Th1 cellular and humoral responses generated by the Yersinia pestis rF1-V subunit vaccine formulated to contain an agonist of the CD137 pathway do not translate into increased protection against pneumonic plague. Vaccine 2019, 37, 5708–5716. [Google Scholar] [CrossRef] [PubMed]
- Fink, A.L.; Engle, K.; Ursin, R.L.; Tang, W.Y.; Klein, S. Biological sex affects vaccine efficacy and protection against influenza in mice. Proc. Natl. Acad. Sci. USA 2018, 115, 12477–12482. [Google Scholar] [CrossRef] [PubMed]
- Van Loo, P.L.; van Zutphen, L.F.; Baumans, V. Male management: Coping with aggression problems in male laboratory mice. Lab. Anim. 2003, 37, 300–313. [Google Scholar] [CrossRef] [PubMed]
- Kappel, S.; Hawkins, P.; Mendl, M.T. To group or not to group? Good practice for housing male laboratory mice. Animals 2017, 7, 88. [Google Scholar] [CrossRef]
- Webster Marketon, J.I.; Glaser, R. Stress hormones and immune function. Cell. Immunol. 2008, 252, 16–26. [Google Scholar] [CrossRef]
- Averbuch, M.; Katzper, M. A search for sex differences in response to analgesia. Arch. Intern. Med. 2000, 160, 3424–3428. [Google Scholar] [CrossRef]
- Bartley, E.J.; Fillingim, R.B. Sex differences in pain: A brief review of clinical and experimental findings. Br. J. Anaesth. 2013, 111, 52–58. [Google Scholar] [CrossRef]
- Cho, C.; Michailidis, V.; Lecker, I.; Collymore, C.; Hanwell, D.; Loka, M.; Danesh, M.; Pham, C.; Urban, P.; Bonin, L.J. Evaluating analgesic efficacy and administration route following craniotomy in mice using the grimace scale. Sci. Rep. 2019, 9, 359. [Google Scholar] [CrossRef]
- Gioiosa, L.; Chen, X.; Watkins, R.; Umeda, E.A.; Arnold, A.P. Sex chromosome complement affects nociception and analgesia in newborn mice. J. Pain 2008, 9, 962–969. [Google Scholar] [CrossRef] [PubMed]
- Greenspan, J.D.; Craft, R.M.; LeResche, L.; Arendt-Nielsen, L.; Berkley, K.J.; Fillingim, R.B.; Gold, M.S.; Holdcroft, A.; Lautenbacher, S.; Mayer, E.A. Studying sex and gender differences in pain and analgesia: A consensus report. Pain 2007, 132, S26–S45. [Google Scholar] [CrossRef] [PubMed]
- Rosen, S.F.; Ham, B.; Haichin, M.; Walters, I.C.; Tohyama, S.; Sotocinal, S.G.; Mogil, J.S. Increased pain sensitivity and decreased opioid analgesia in T-cell-deficient mice and implications for sex differences. Pain 2019, 160, 358–366. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Agriculture. Animal Care Policy Manual: October 16, 2015 in Policy no. 11 (ACRG 11), Animal and Plant Health Inspection Service (APHIS); United States Department of Agriculture (USDA): Wasington, DC, USA, 2015.
- Denayer, T.; Stohr, T.; van Roy, M. Animal models in translational medicine: Validation and prediction. New Horiz. Transl. Med. 2014, 2, 5–11. [Google Scholar] [CrossRef]
- Gerdts, V.; Littel-van den Hurk, S.V.; Griebel, P.J.; Babiuk, L.A. Use of animal models in the development of human vaccines. Future Microbiol. 2007, 2, 667–675. [Google Scholar] [CrossRef] [PubMed]
- Sacerdote, P. Opioids and the immune system. Palliat. Med. 2006, 20, 9–15. [Google Scholar] [CrossRef]
- Cho, J.Y. Immunomodulatory effect of nonsteroidal anti-inflammatory drugs (NSAIDs) at the clinically avalable doses. Arch. Pharm. Res. 2007, 30, 64–74. [Google Scholar] [CrossRef]
- Kim, H.J.; Lee, Y.H.; Im, S.A.; Kim, K.; Lee, C.K. Cyclooxygenase inhibitors, aspirin and ibuprofen, inhibit MHC-restricted antigen presentation in dendritic cells. Immune Netw. 2010, 10, 92–98. [Google Scholar] [CrossRef]



| Clinical Score a (SD) b | |||
|---|---|---|---|
| Treatment | Day 0 | Day 1 | Day 2 |
| VAX | 2.0 (1.4) | 3.0 (1.8) | 3.5 (1.7) |
| VAX + ACE | 2.0 (2.4) | 3.0 (1.8) | 2.8 (2.6) |
| VAX + MEL | 0.5 (1.0) | 3.5 (1.7) | 2.0 (1.2) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Culbreth, M.J.; Biryukov, S.S.; Shoe, J.L.; Dankmeyer, J.L.; Hunter, M.; Klimko, C.P.; Rosario-Acevedo, R.; Fetterer, D.P.; Moreau, A.M.; Welkos, S.L.; et al. The Use of Analgesics during Vaccination with a Live Attenuated Yersinia pestis Vaccine Alters the Resulting Immune Response in Mice. Vaccines 2019, 7, 205. https://doi.org/10.3390/vaccines7040205
Culbreth MJ, Biryukov SS, Shoe JL, Dankmeyer JL, Hunter M, Klimko CP, Rosario-Acevedo R, Fetterer DP, Moreau AM, Welkos SL, et al. The Use of Analgesics during Vaccination with a Live Attenuated Yersinia pestis Vaccine Alters the Resulting Immune Response in Mice. Vaccines. 2019; 7(4):205. https://doi.org/10.3390/vaccines7040205
Chicago/Turabian StyleCulbreth, Marilynn J., Sergei S. Biryukov, Jennifer L. Shoe, Jennifer L. Dankmeyer, Melissa Hunter, Christopher P. Klimko, Raysa Rosario-Acevedo, David P. Fetterer, Alicia M. Moreau, Susan L. Welkos, and et al. 2019. "The Use of Analgesics during Vaccination with a Live Attenuated Yersinia pestis Vaccine Alters the Resulting Immune Response in Mice" Vaccines 7, no. 4: 205. https://doi.org/10.3390/vaccines7040205
APA StyleCulbreth, M. J., Biryukov, S. S., Shoe, J. L., Dankmeyer, J. L., Hunter, M., Klimko, C. P., Rosario-Acevedo, R., Fetterer, D. P., Moreau, A. M., Welkos, S. L., & Cote, C. K. (2019). The Use of Analgesics during Vaccination with a Live Attenuated Yersinia pestis Vaccine Alters the Resulting Immune Response in Mice. Vaccines, 7(4), 205. https://doi.org/10.3390/vaccines7040205





