Comparison of Safety and Vector-Specific Immune Responses in Healthy and HIV-Infected Populations Vaccinated with MVA-B
Abstract
1. Introduction
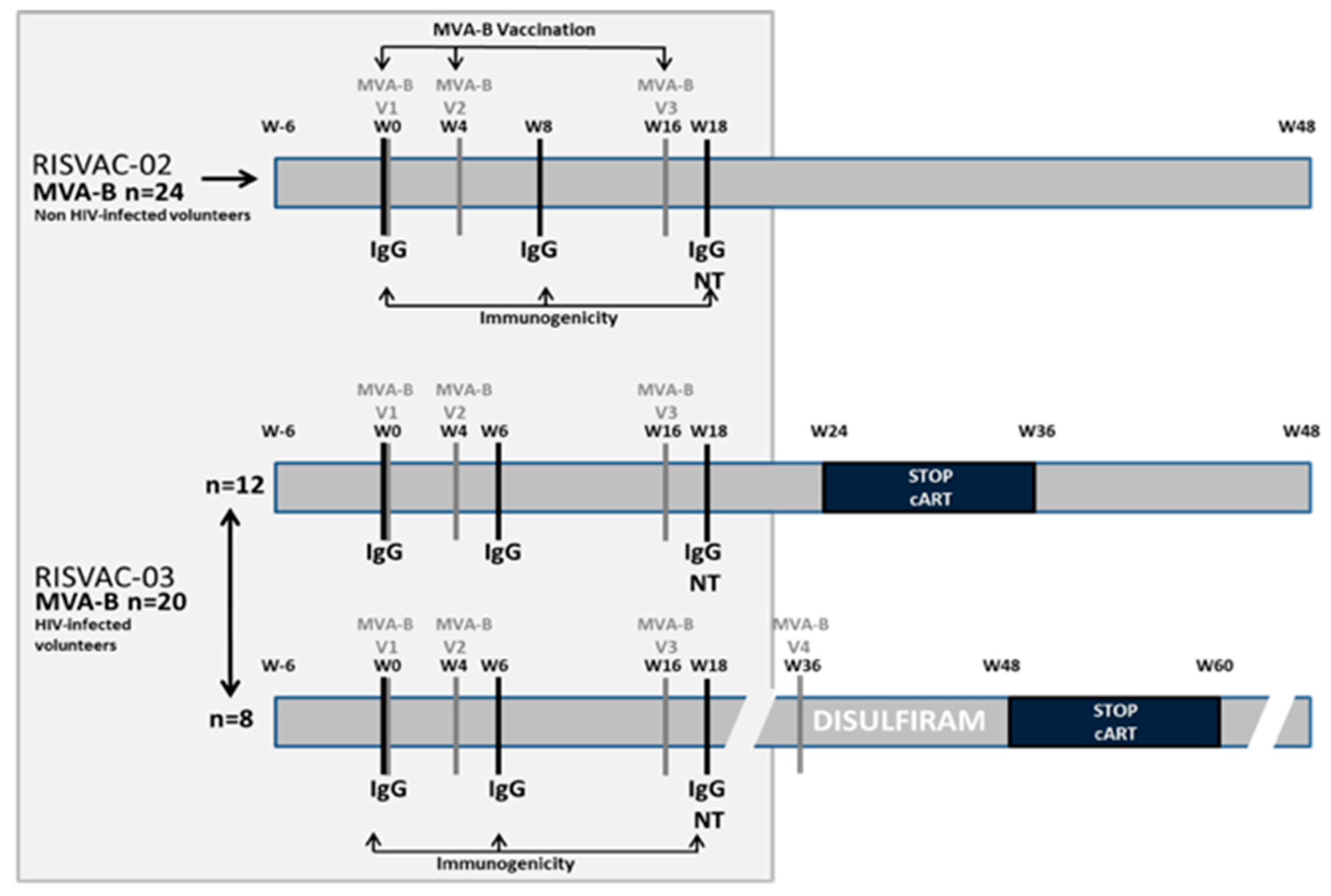
2. Methods
2.1. Safety
2.2. Immunogenicity
2.3. Statistical Analysis
2.4. Ethic Issue
3. Results
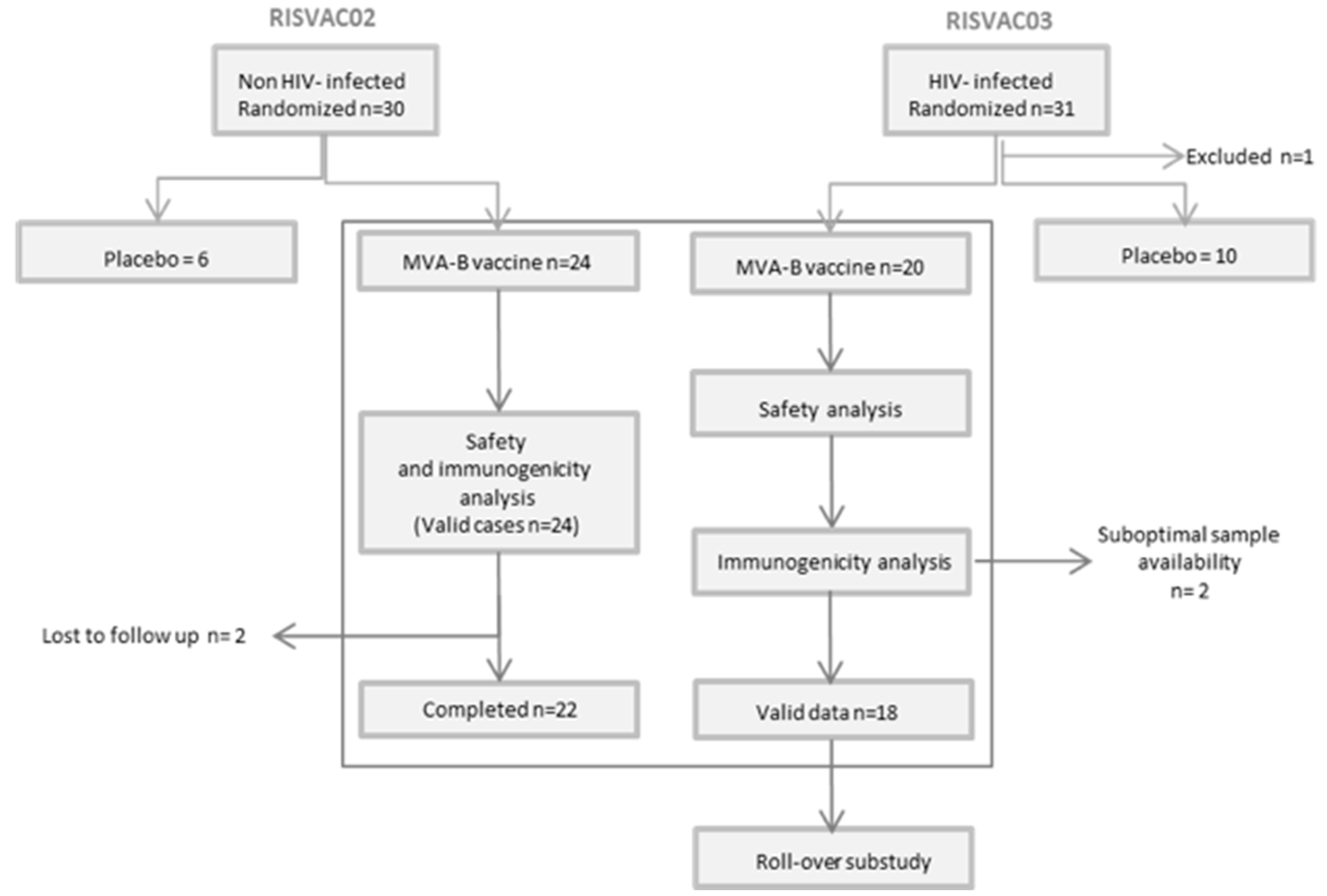
3.1. Clinical Characteristics of Participants
3.2. Safety
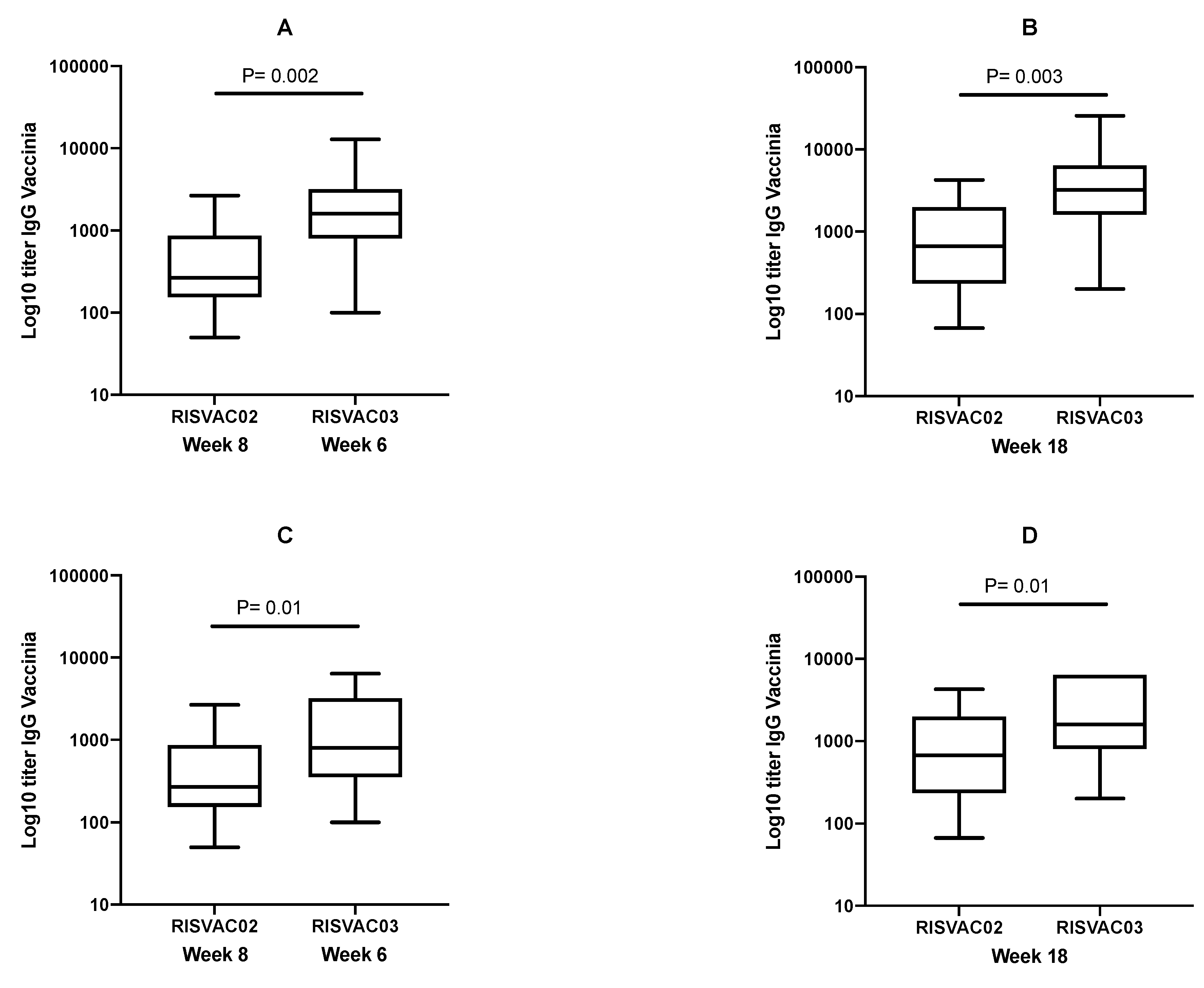
3.3. Immunogenicity
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Dorrell, L.; Yang, H.; Iversen, A.K.; Conlon, C.; Suttill, A.; Lancaster, M.; Dong, T.; Cebere, I.; Edwards, A.; Rowland-Jones, S.; et al. Therapeutic immunization of highly active antiretroviral therapy-treated HIV-1-infected patients: Safety and immunogenicity of an HIV-1 gag/poly-epitope DNA vaccine. Aids 2005, 19, 1321–1323. [Google Scholar] [CrossRef] [PubMed]
- Hanke, T.; Goonetilleke, N.; McMichael, A.J.; Dorrell, L. Clinical experience with plasmid DNA- and modified vaccinia virus Ankara-vectored human immunodeficiency virus type 1 clade A vaccine focusing on T-cell induction. J. Gen. Virol. 2007, 88, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Howles, S.; Guimarães-Walker, A.; Yang, H.; Hancock, G.; di Gleria, K.; Tarragona-Fiol, T.; Hayes, P.; Gilmour, J.; Bridgeman, A.; Hanke, T.; et al. Vaccination with a modified vaccinia virus Ankara (MVA)-vectored HIV-1 immunogen induces modest vector-specific T cell responses in human subjects. Vaccine 2010, 28, 7306–7312. [Google Scholar] [CrossRef] [PubMed]
- Bellino, S.; Francavilla, V.; Longo, O.; Tripiciano, A.; Paniccia, G.; Arancio, A.; Fiorelli, V.; Scoglio, A.; Collacchi, B.; Campagna, M.; et al. Parallel conduction of the phase I preventive and therapeutic trials based on the Tat vaccine candidate. Rev. Recent Clin. Trials 2009, 4, 195–204. [Google Scholar] [CrossRef] [PubMed]
- Adetokunboh, O.O.; Ndwandwe, D.; Awotiwon, A.; Uthman, O.A.; Wiysonge, C.S. Vaccination among HIV-infected, HIV-exposed uninfected and HIV-uninfected children: A systematic review and meta-analysis of evidence related to vaccine efficacy and effectiveness. Hum. Vaccin. Immunother. 2019, 22, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Mena, G.; Llupià, A.; García-Basteiro, A.L.; Díez, C.; León, A.; García, F.; Bayas, J.M. Assessing the immunological response to hepatitis B vaccination in HIV-infected patients in clinical practice. Vaccine 2012, 30, 3703–3709. [Google Scholar] [CrossRef]
- Mena, G.; García-Basteiro, A.L.; Llupià, A.; Díez, C.; Costa, J.; Gatell, J.M.; García, F.; Bayas, J.M. Factors associated with the immune response to hepatitis A vaccination in HIV-infected patients in the era of highly active antiretroviral therapy. Vaccine 2013, 31, 3668–3674. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Arriaza, J.; Esteban, M. Enhancing poxvirus vectors vaccine immunogenicity. Hum. Vaccine Immunother. 2014, 10, 2235–2244. [Google Scholar] [CrossRef] [PubMed]
- Gomez, C.E.; Perdiguero, B.; Garcia-Arriaza, J.; Esteban, M. Poxvirus vectors as HIV/AIDS vaccines in humans. Hum. Vaccine Immunother. 2012, 8, 1192–1207. [Google Scholar] [CrossRef] [PubMed]
- García, F.; de Quirós, J.C.L.B.; Gómez, C.E.; Perdiguero, B.; Nájera, J.L.; Jiménez, V.; García-Arriaza, J.; Guardo, A.C.; Pérez, I.; Díaz-Brito, V.; et al. Safety and immunogenicity of a modified pox vector-based HIV/AIDS vaccine candidate expressing Env, Gag, Pot and Nef proteins of HIV-1 subtype B (MVA-B) in healthy HIV-1-uninfected volunteers: A phase I clinical trial (RISVAC02). Vaccine 2011, 29, 8309–8316. [Google Scholar] [CrossRef] [PubMed]
- Mothe, B.; Climent, N.; Plana, M.; Rosàs, M.; Jiménez, J.L.; Muñoz-Fernández, M.Á.; Puertas, M.C.; Carrillo, J.; Gonzalez, N.; León, A.; et al. Safety and immunogenicity of a modified vaccinia Ankara-based HIV-1 vaccine (MVA-B) in HIV-1-infected patients alone or in combination with a drug to reactivate latent HIV-1. J. Antimicrob. Chemother. 2015, 70, 1833–1842. [Google Scholar] [CrossRef] [PubMed]
- Gómez, C.E.; Nájera, J.L.; Jiménez, E.P.; Jiménez, V.; Wagner, R.; Graf, M.; Frachette, M.J.; Liljeström, P.; Pantaleo, G.; Esteban, M. Head-to-head comparison on the immunogenicity of two HIV/AIDS vaccine candidates based on the attenuated poxvirus strains MVA and NYVAC co-expressing in a single locus the HIV-1BX08 gp120 and HIV-1(IIIB) Gag-Pol-Nef proteins of clade B. Vaccine 2007, 25, 2863–2885. [Google Scholar] [CrossRef] [PubMed]
- Buchbinder, S.P.; Mehrotra, D.V.; Duerr, A.; Fitzgerald, D.W.; Mogg, R.; Li, D.; Gilbert, P.B.; Lama, J.R.; Marmor, M.; del Rio, C.; et al. Efficacy assessment of a cell-mediated immunity HIV-1 vaccine (the Step Study): A double-blind, randomised, placebo-controlled, test-of-concept trial. Lancet 2008, 372, 1881–1893. [Google Scholar] [CrossRef]
| AEs in RISVAC02 | Related * | Non-related ** | Total |
| Grade 1 | 123 | 22 | 145 |
| Grade 2 | 4 | 4 | 8 |
| Grade ≥3 | - | 5 | 5 |
| Total | 127 | 31 | 158 |
| AEs in RISVAC03 | Related * | Non-related ** | Total |
| Grade 1 | 102 | 129 | 231 |
| Grade 2 | 13 | 8 | 21 |
| Grade ≥3 | - | 5 | 5 |
| Total | 115 | 142 | 257 |
| RISVAC02 | RISVAC03 | p | |
|---|---|---|---|
| LOCAL | |||
| Pain | 24 (100) | 18 (90) | 0.20 |
| Redness | 4 (17) | 8 (40) | 0.12 |
| Itching | 4 (17) | 6 (30) | 0.47 |
| SYSTEMIC | |||
| Headache | 10 (42) | 7 (35) | 0.76 |
| Malaise | 12 (50) | 13 (65) | 0.37 |
| Myalgia | 4 (17) | 9 (45) | 0.05 |
| Nausea/vomiting | 3 (13) | 2 (10) | 1 |
| Chills | 1 (4) | 7 (35) | 0.02 |
| Fever | 2 (8) | 0 (0) | 0.49 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Couto, E.; Diaz-Brito, V.; Mothe, B.; Guardo, A.C.; Fernandez, I.; Ugarte, A.; Etcheverry, F.; Gómez, C.E.; Esteban, M.; Pich, J.; et al. Comparison of Safety and Vector-Specific Immune Responses in Healthy and HIV-Infected Populations Vaccinated with MVA-B. Vaccines 2019, 7, 178. https://doi.org/10.3390/vaccines7040178
Couto E, Diaz-Brito V, Mothe B, Guardo AC, Fernandez I, Ugarte A, Etcheverry F, Gómez CE, Esteban M, Pich J, et al. Comparison of Safety and Vector-Specific Immune Responses in Healthy and HIV-Infected Populations Vaccinated with MVA-B. Vaccines. 2019; 7(4):178. https://doi.org/10.3390/vaccines7040178
Chicago/Turabian StyleCouto, Elvira, Vicenç Diaz-Brito, Beatriz Mothe, Alberto C. Guardo, Irene Fernandez, Ainoa Ugarte, Flor Etcheverry, Carmen E. Gómez, Mariano Esteban, Judit Pich, and et al. 2019. "Comparison of Safety and Vector-Specific Immune Responses in Healthy and HIV-Infected Populations Vaccinated with MVA-B" Vaccines 7, no. 4: 178. https://doi.org/10.3390/vaccines7040178
APA StyleCouto, E., Diaz-Brito, V., Mothe, B., Guardo, A. C., Fernandez, I., Ugarte, A., Etcheverry, F., Gómez, C. E., Esteban, M., Pich, J., Arnaiz, J. A., López Bernaldo de Quirós, J. C., Brander, C., Plana, M., García, F., & Leal, L. (2019). Comparison of Safety and Vector-Specific Immune Responses in Healthy and HIV-Infected Populations Vaccinated with MVA-B. Vaccines, 7(4), 178. https://doi.org/10.3390/vaccines7040178






