Early IgG Response to Foot and Mouth Disease Vaccine Formulated with a Vegetable Oil Adjuvant
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Ethical Statement
2.3. Adjuvants and Antigen
2.4. Preparation of FMD Vaccine
2.5. Immunization and Sample Collection
2.6. Analysis of FMDV-Specific Antibody and Isotypes
2.7. Lymphocyte Proliferation
2.8. Cytokine Production by Splenocytes
2.9. Flow Cytometry Analysis of T Lymphocyte Subsets
2.10. Flow Cytometry Analysis of Bone Marrow Plasma Cells (Bmpcs)
2.11. Transcriptome Sequencing
2.12. Analysis of Differentially Expressed Genes (DEGs)
2.13. Validation of Gene Expression by RT-qPCR
2.14. Statistical Analysis
3. Results
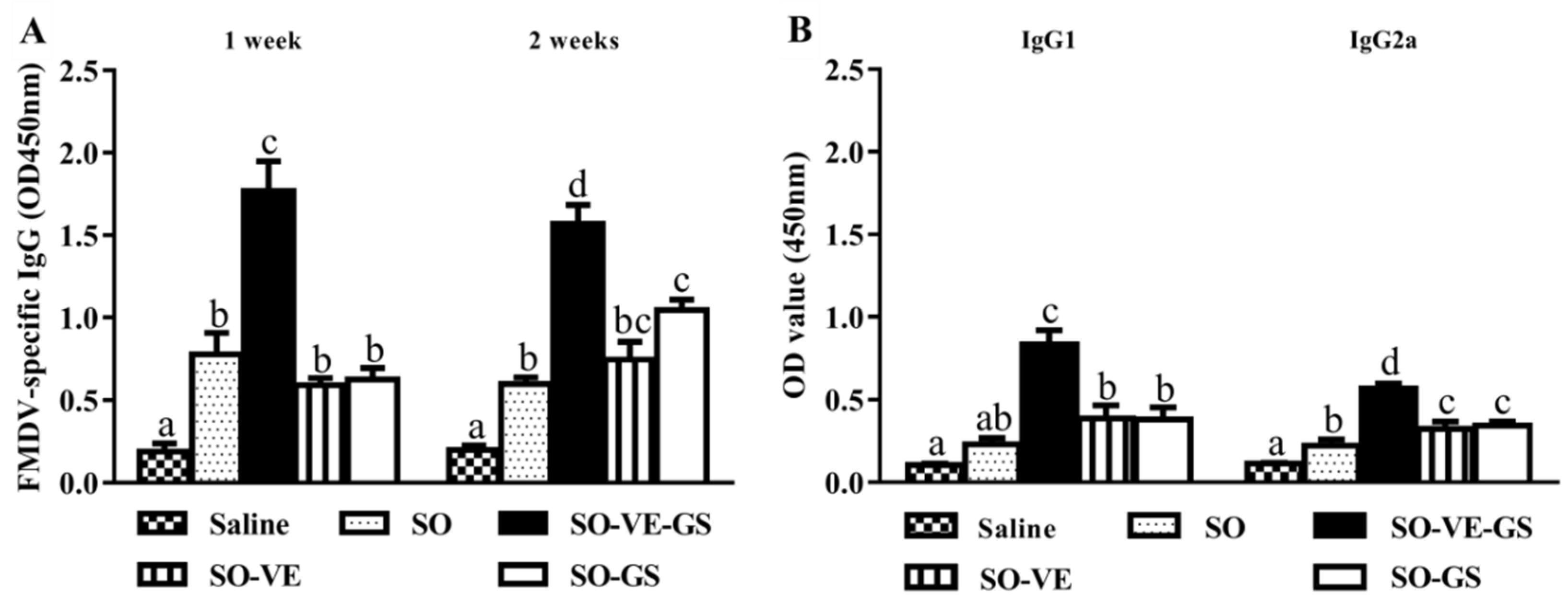
3.1. Synergistic Effect of Vitamin E and Ginseng Saponins on FMDV-Specific Antibody Response
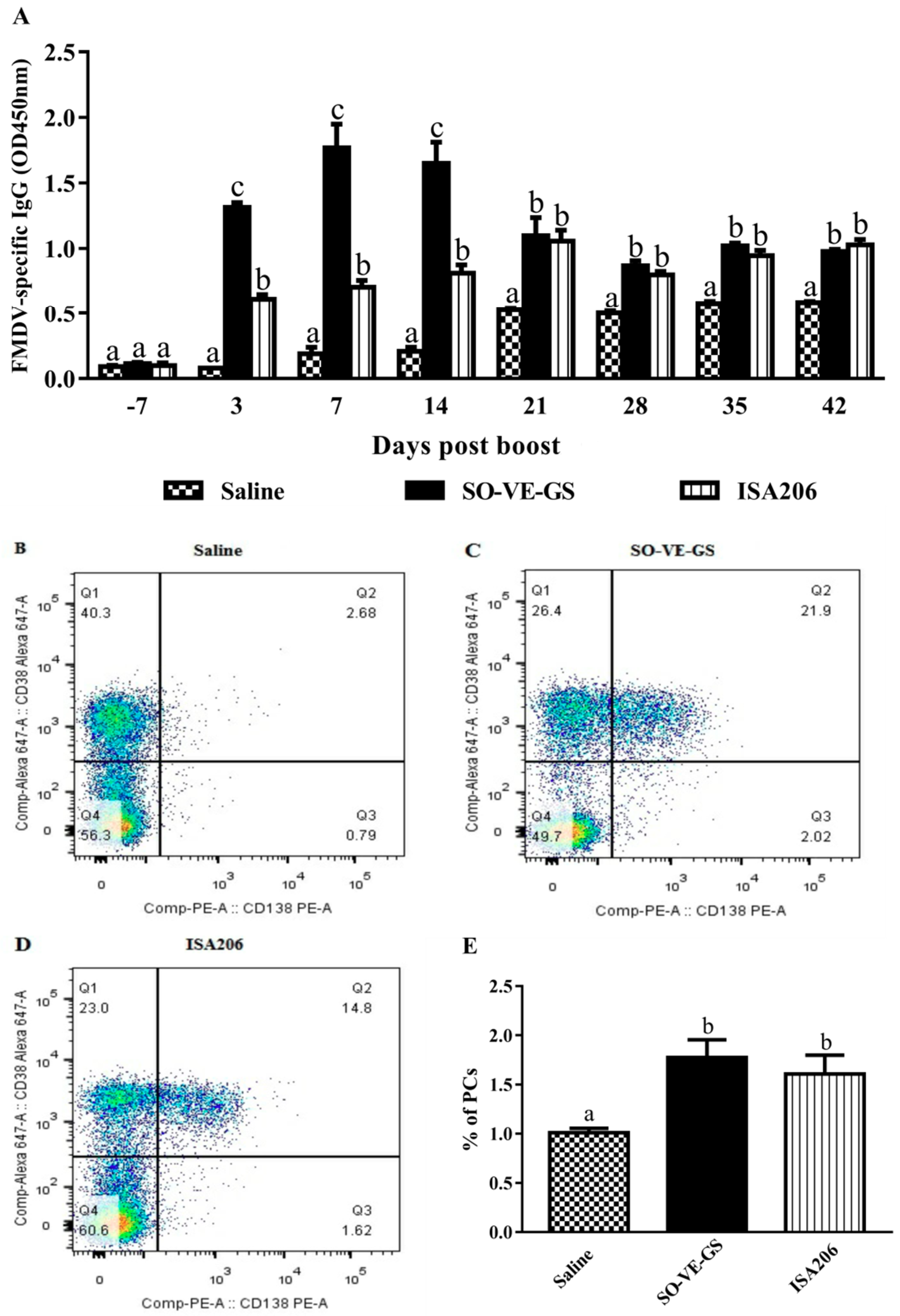
3.2. Effect of SO-VE-GS on the Duration and Early Production of Antibody Response
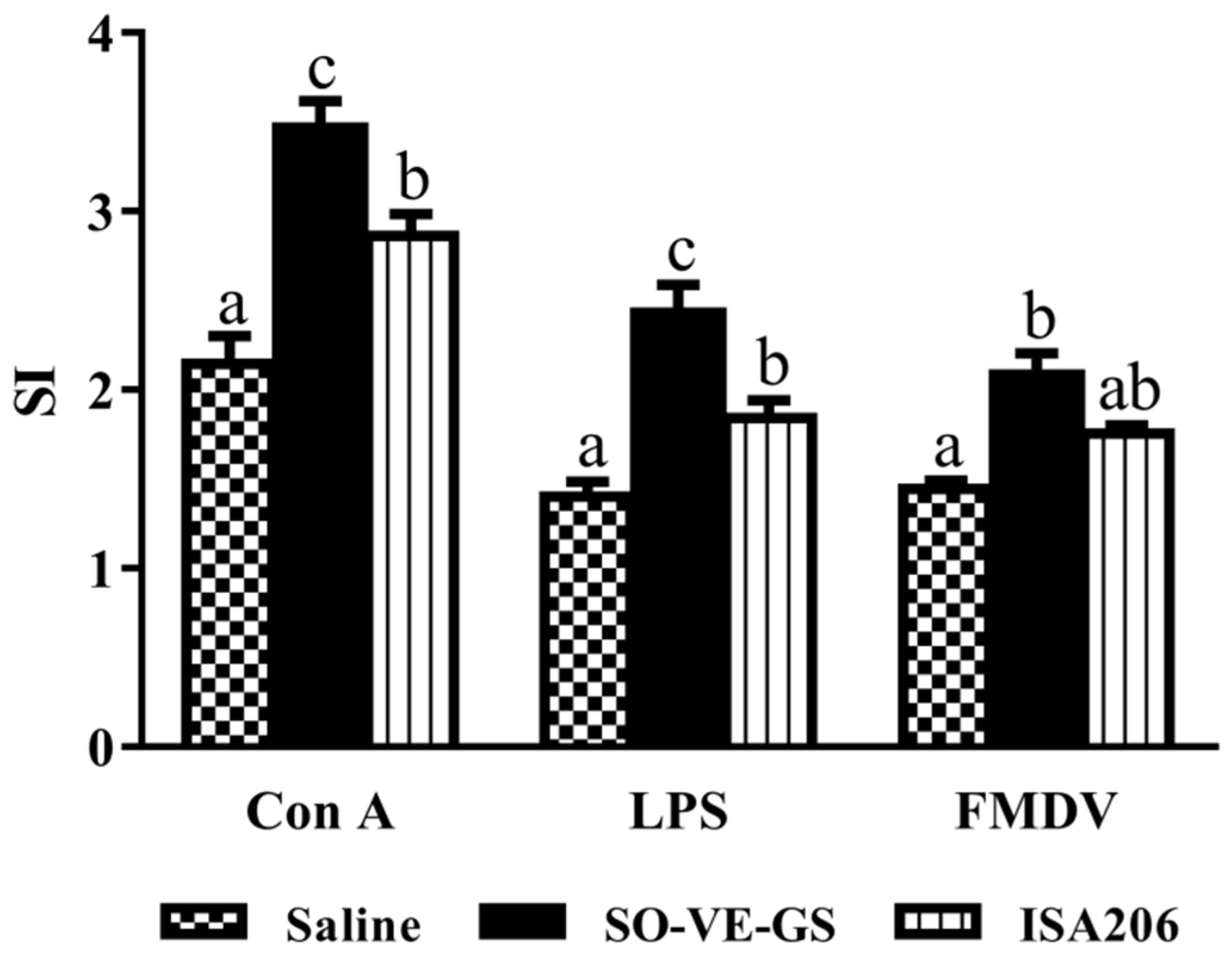
3.3. Effect of SO-VE-GS on Lymphocyte Proliferation
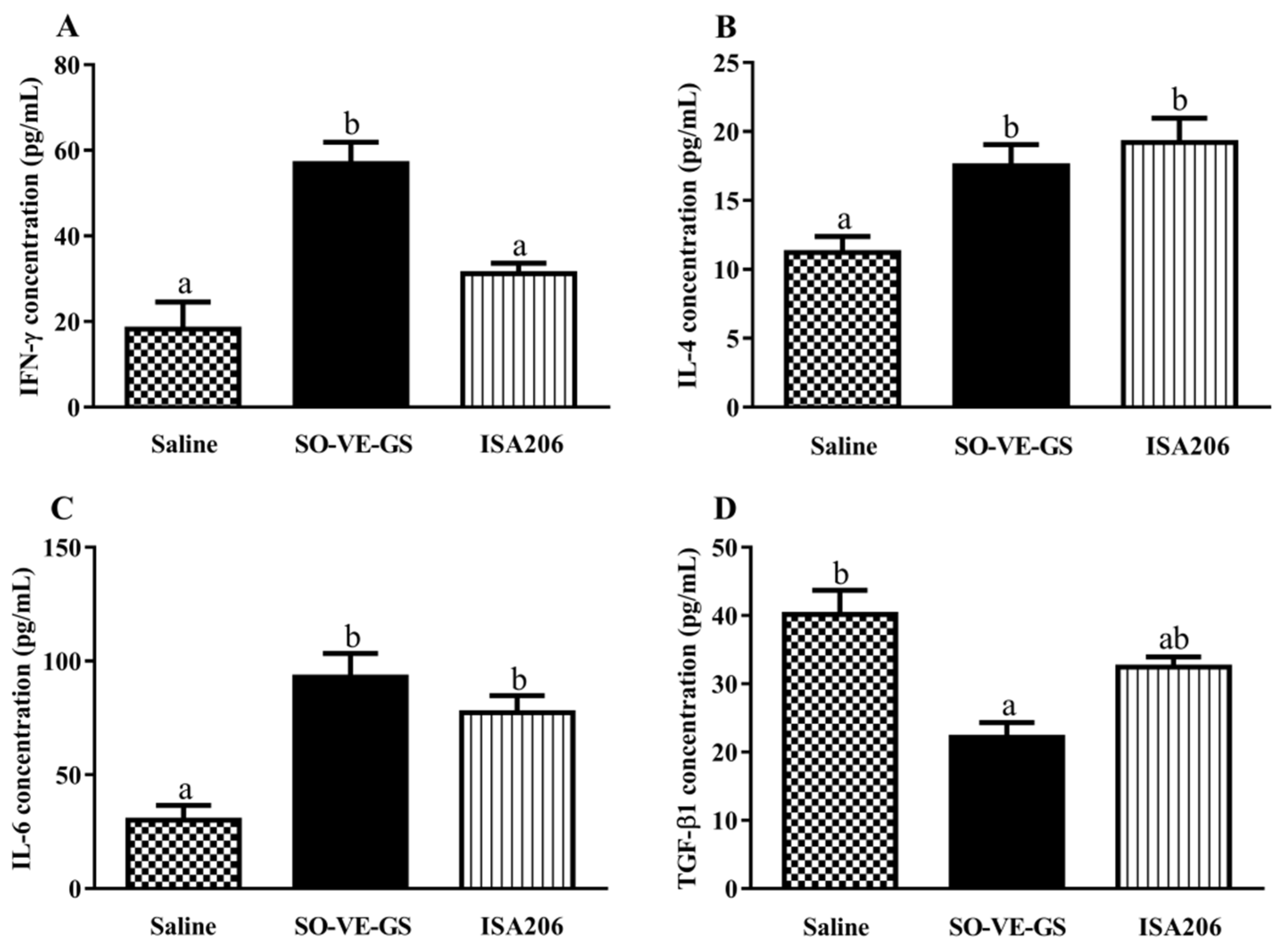
3.4. Effects of SO-VE-GS on Cytokine Production by Lymphocytes
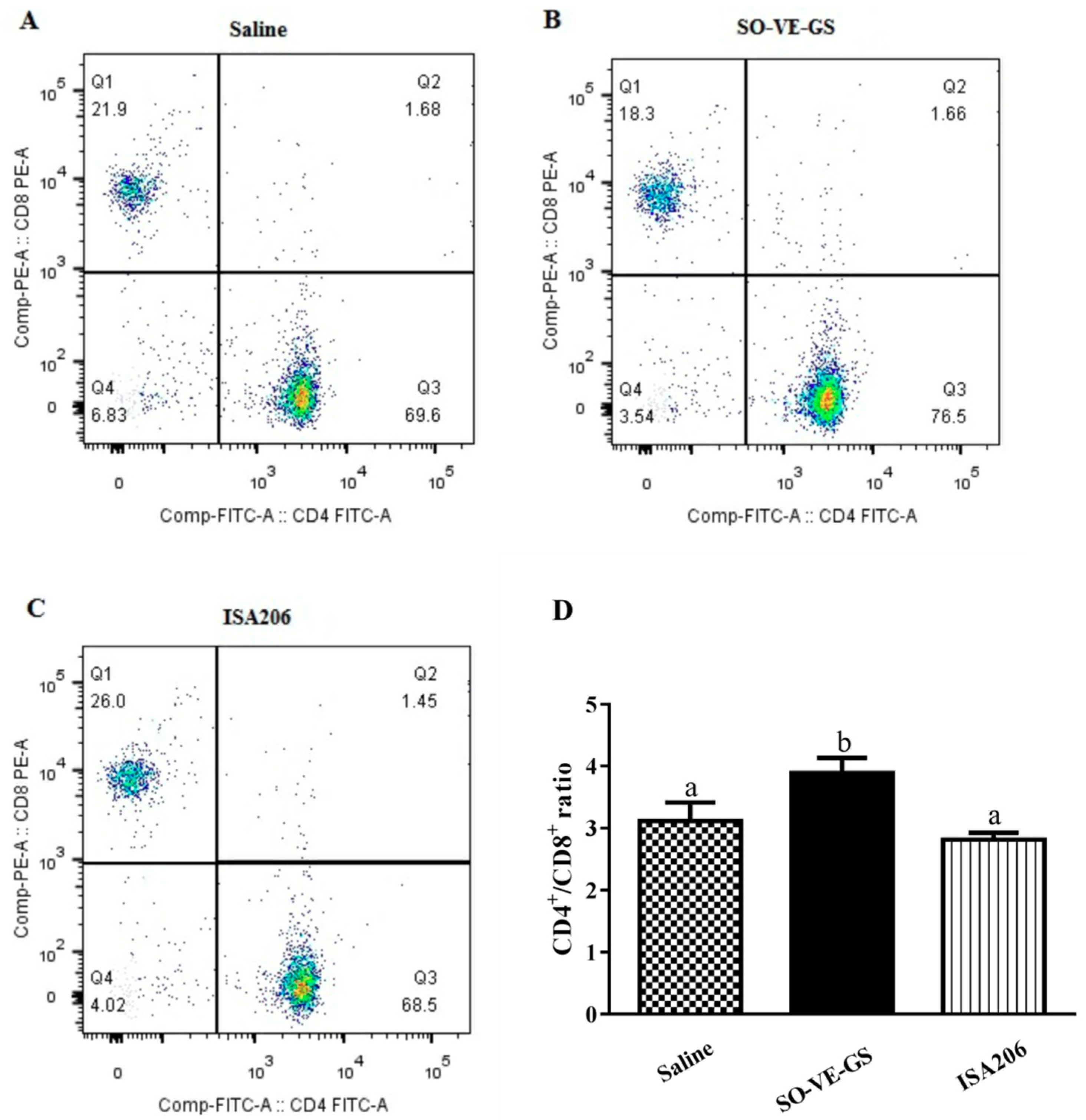
3.5. Effect of SO-VE-GS on CD4+/CD8+ T Cell Ratio
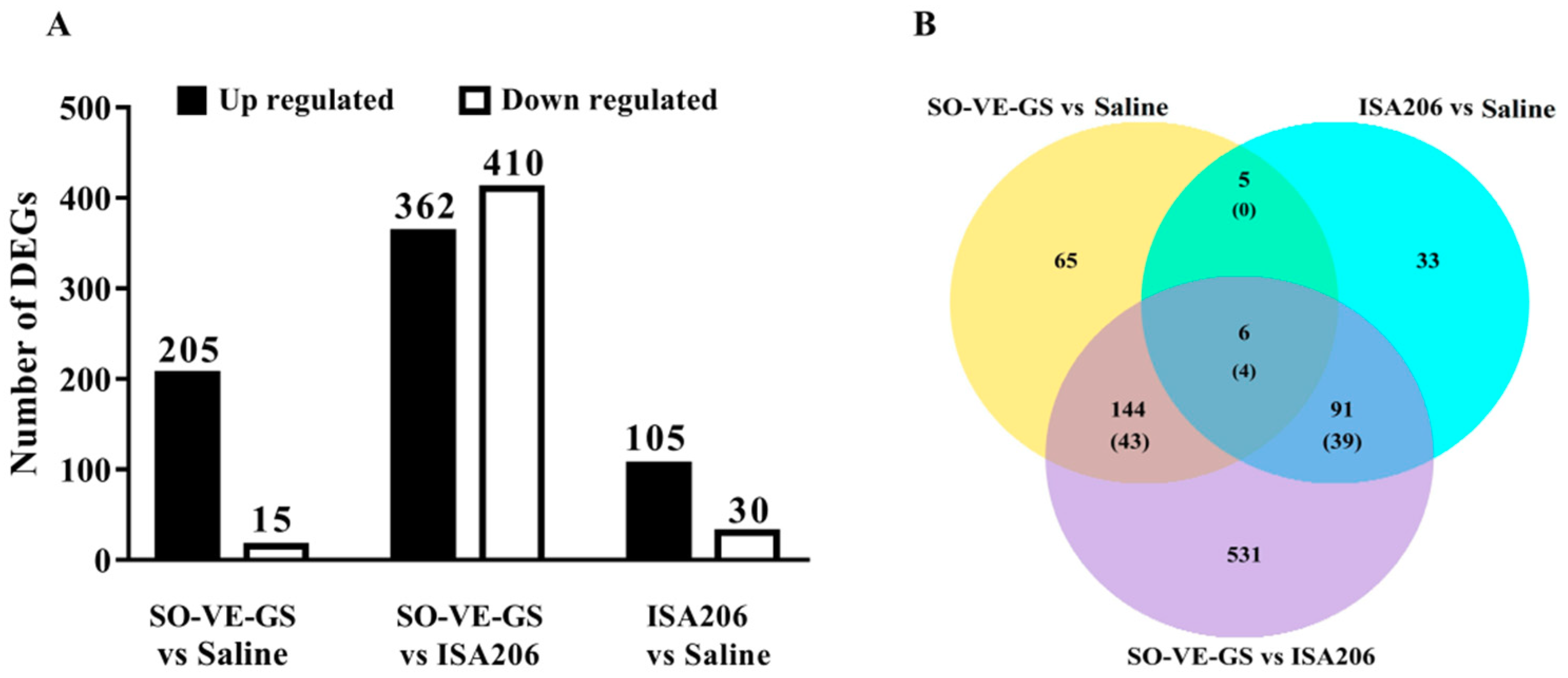
3.6. Analysis of DEGs
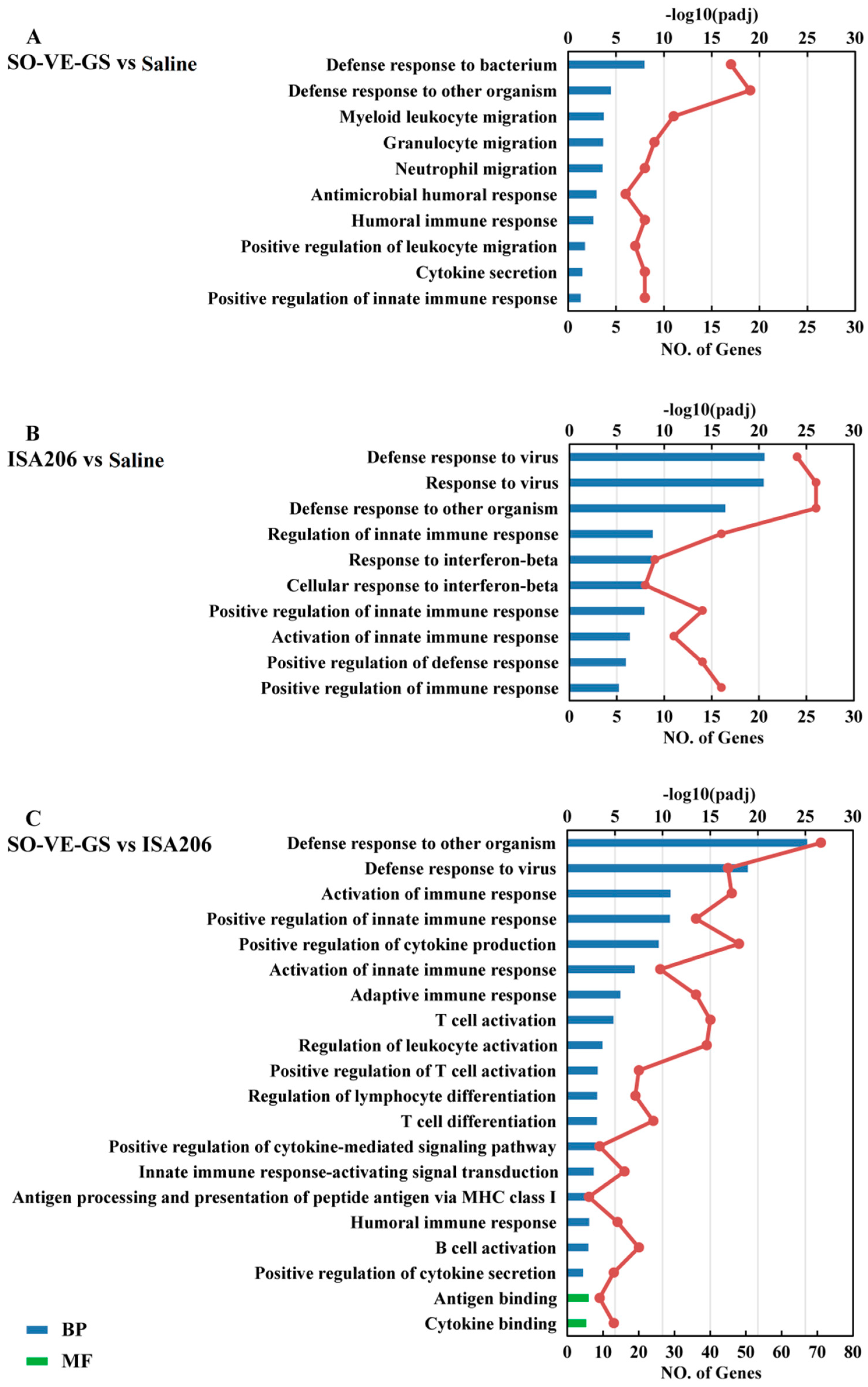
3.7. Gene Ontology Enrichment Analysis of DEGs
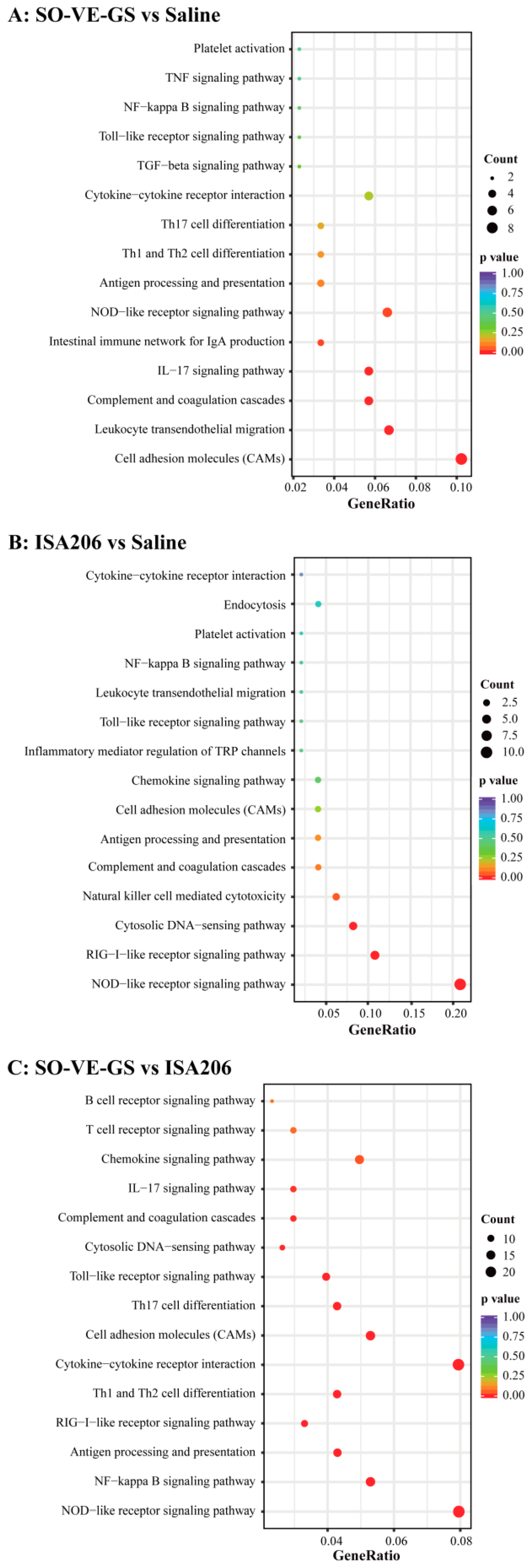
3.8. Kyoto Encyclopedia of Genes and Genomes Pathway Enrichment Analysis of DEGs
3.9. Validation of Gene Expression by Real Time-qPCR
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ibrahim, E.E.-S.; Gamal, W.M.; Hassan, A.I.; Mahdy, S.E.-D.; Hegazy, A.Z.; Abdel-Atty, M.M. Comparative study on the immunopotentiator effect of ISA 201, ISA 61, ISA 50, ISA 206 used in trivalent foot and mouth disease vaccine. Vet. World 2015, 8, 1189–1198. [Google Scholar] [CrossRef]
- Wiratsudakul, A.; Sekiguchi, S. The implementation of cattle market closure strategies to mitigate the foot-and-mouth disease epidemics: A contact modeling approach. Res. Vet. Sci. 2018, 121, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Puckette, M.; Clark, B.A.; Smith, J.D.; Turecek, T.; Martel, E.; Gabbert, L.; Pisano, M.; Hurtle, W.; Pacheco, J.M.; Barrera, J.; et al. Foot-and-Mouth Disease (FMD) Virus 3C Protease Mutant L127P: Implications for FMD Vaccine Development. J. Virol. 2017, 91, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Diaz-San Segundo, F.; Medina, G.N.; Grubman, M.J.; de los Santos, T. Animal Health: Foot-and-Mouth Disease. In Encyclopedia of Agriculture and Food Systems; Elsevier: Amsterdam, The Netherlands, 2014; Volume 1, pp. 327–345. ISBN 9780080931395. [Google Scholar]
- Diaz-San Segundo, F.; Medina, G.N.; Stenfeldt, C.; Arzt, J.; de los Santos, T. Foot-and-mouth disease vaccines. Vet. Microbiol. 2017, 206, 102–112. [Google Scholar] [CrossRef] [PubMed]
- Depa, P.M.; Dimri, U.; Sharma, M.C.; Tiwari, R. Update on epidemiology and control of foot and mouth disease-a menace to international trade and global animal enterprise. Vet. World 2012, 5, 694–704. [Google Scholar] [CrossRef]
- Li, D.; Zhou, C.; She, D.; Li, P.; Sun, P.; Bai, X.; Chen, Y.; Xie, B.; Liu, Z. The comparison of the efficacy of swine FMD vaccine emulsified with oil adjuvant of ISA 201 VG or ISA 206 VG. J. Biosci. Med. 2013, 01, 22–25. [Google Scholar] [CrossRef][Green Version]
- Jamal, S.M.; Belsham, G.J. Foot-and-mouth disease: Past, present and future. Vet. Res. 2013, 44, 116. [Google Scholar] [CrossRef]
- Park, M.-E.; Lee, S.-Y.; Kim, R.-H.; Ko, M.-K.; Park, J.-N.; Lee, K.-N.; Kim, S.-M.; Choi, J.-H.; You, S.-H.; Kim, B.; et al. Altered adjuvant of foot-and-mouth disease vaccine improves immune response and protection from virus challenge. Trials Vaccinol. 2016, 5, 97–104. [Google Scholar] [CrossRef]
- Coffman, R.L.; Sher, A.; Seder, R.A. Vaccine Adjuvants: Putting Innate Immunity to Work. Immunity 2010, 33, 492–503. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Xie, F.; Chen, J.; Fan, Q.; Zhai, L.; Hu, S. Increased Humoral Immune Responses of Pigs to Foot-and-Mouth Disease Vaccine Supplemented with Ginseng Stem and Leaf Saponins. Chem. Biodivers. 2012, 9, 2225–2235. [Google Scholar] [CrossRef] [PubMed]
- Song, X.; Bao, S.; Wu, L.; Hu, S. Ginseng stem-leaf saponins (GSLS) and mineral oil act synergistically to enhance the immune responses to vaccination against foot-and-mouth disease in mice. Vaccine 2009, 27, 51–55. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Xu, W.; Chen, J.; Guan, R.; Bi, S.; Jin, H.; Cui, X.; Shi, F.; Hu, S. Soybean oil containing ginseng saponins as adjuvants promotes production of cytokines and enhances immune responses to foot-and-mouth disease vaccine. Microbiol. Immunol. 2018, 62, 187–194. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Wang, Y.; Wang, M.; Su, X.; Lu, Y.; Su, F.; Hu, S. Rapeseed oil and ginseng saponins work synergistically to enhance Th1 and Th2 immune responses induced by the foot-and-mouth disease vaccine. Clin. Vaccine Immunol. 2014, 21, 113–1119. [Google Scholar] [CrossRef] [PubMed]
- Yu, M.; Vajdy, M. A novel retinoic acid, catechin hydrate and mustard oil-based emulsion for enhanced cytokine and antibody responses against multiple strains of HIV-1 following mucosal and systemic vaccinations. Vaccine 2011, 29, 2429–2436. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.; Akalkotkar, A.; Bivona, J.J.; Lee, J.Y.; Park, Y.K.; Yu, M.; Colpitts, S.L.; Vajdy, M. Vitamin A or E and a catechin synergize as vaccine adjuvant to enhance immune responses in mice by induction of early interleukin-15 but not interleukin-1β responses. Immunology 2016, 148, 352–362. [Google Scholar] [CrossRef] [PubMed]
- Quintilio, W.; de Freitas, F.A.; Rodriguez, D.; Kubrusly, F.S.; Yourtov, D.; Miyaki, C.; de Cerqueira Leite, L.C.; Raw, I. Vitamins as influenza vaccine adjuvant components. Arch. Virol. 2016, 161, 2787–2795. [Google Scholar] [CrossRef]
- Morel, S.; Didierlaurent, A.; Bourguignon, P.; Delhaye, S.; Baras, B.; Jacob, V.; Planty, C.; Elouahabi, A.; Harvengt, P.; Carlsen, H. Adjuvant System AS03 containing α-tocopherol modulates innate immune response and leads to improved adaptive immunity. Vaccine 2011, 29, 2461–2473. [Google Scholar] [CrossRef]
- Cao, Y. Adjuvants for foot-and-mouth disease virus vaccines: Recent progress. Expert Rev. Vaccines 2014, 13, 1377–1385. [Google Scholar] [CrossRef]
- Feng, H.; Fan, J.; Qiu, H.; Wang, Z.; Yan, Z.; Yuan, L.; Guan, L.; Du, X.; Song, Z.; Han, X.; et al. Chuanminshen violaceum polysaccharides improve the immune responses of foot-and-mouth disease vaccine in mice. Int. J. Biol. Macromol. 2015, 78, 405–416. [Google Scholar] [CrossRef]
- Szyszko, E.A.; Skarstein, K.; Jonsson, R.; Brokstad, K.A. Distinct phenotypes of plasma cells in spleen and bone marrow of autoimmune NOD.B10.H2b mice. Autoimmunity 2011, 44, 415–426. [Google Scholar] [CrossRef]
- Chu, V.T.; Fröhlich, A.; Steinhauser, G.; Scheel, T.; Roch, T.; Fillatreau, S.; Lee, J.J.; Löhning, M.; Berek, C. Eosinophils are required for the maintenance of plasma cells in the bone marrow. Nat. Immunol. 2011, 12, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.; Xu, B.; Huang, M.; He, Q. Effects of recombinant Agrocybe aegerita lectin as an immunoadjuvant on immune responses. Immunopharmacol. Immunotoxicol. 2018, 40, 6–12. [Google Scholar] [CrossRef] [PubMed]
- Buggisch, M.; Ateghang, B.; Ruhe, C.; Strobel, C.; Lange, S.; Wartenberg, M.; Sauer, H. Stimulation of ES-cell-derived cardiomyogenesis and neonatal cardiac cell proliferation by reactive oxygen species and NADPH oxidase. J. Cell Sci. 2007, 120, 885–894. [Google Scholar] [CrossRef] [PubMed]
- Livak, K.J.; Schmittgen, T.D. Analysis of Relative Gene Expression Data Using Real-Time Quantitative PCR and the 2−ΔΔCT Method. Methods 2001, 25, 402–408. [Google Scholar] [CrossRef] [PubMed]
- Yoshimura, T.; McLean, M.H.; Dzutsev, A.K.; Yao, X.; Chen, K.; Huang, J.; Gong, W.; Zhou, J.; Xiang, Y.; H. Badger, J.; et al. The antimicrobial peptide cramp is essential for colon homeostasis by maintaining microbiota balance. J. Immunol. 2018, 200, 2174–2185. [Google Scholar] [CrossRef]
- Hunold, K.; Weber-Steffens, D.; Runza, V.L.; Jensenius, J.C.; Männel, D.N. Functional analysis of mouse ficolin-B and detection in neutrophils. Immunobiology 2012, 217, 982–985. [Google Scholar] [CrossRef] [PubMed]
- Huang, D.W.; Sherman, B.T.; Lempicki, R.A. Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources. Nat. Protoc. 2009, 4, 44–57. [Google Scholar] [CrossRef] [PubMed]
- Hulsegge, I.; Kommadath, A.; Smits, M.A. Globaltest and GOEAST: Two different approaches for Gene Ontology analysis. BMC Proc. 2009, 3, S10. [Google Scholar] [CrossRef] [PubMed]
- Kanehisa, M.; Furumichi, M.; Tanabe, M.; Sato, Y.; Morishima, K. KEGG: New perspectives on genomes, pathways, diseases and drugs. Nucleic Acids Res. 2017, 45, D353–D361. [Google Scholar] [CrossRef] [PubMed]
- Xiao, C.; Rajput, Z.I.; Hu, S. Improvement of a commercial foot-and-mouth disease vaccine by supplement of Quil A. Vaccine 2007, 25, 4795–4800. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Li, H.; Qi, X.; Ma, Y.; Yang, B.; Zhang, S.; Chang, H.; Yin, X.; Li, Z. Immunogenicity and protective efficacy of a novel foot-and-mouth disease virus empty-capsid-like particle with improved acid stability. Vaccine 2019, 37, 2016–2025. [Google Scholar] [CrossRef]
- Ramírez-Carvajal, L.; Diaz-San Segundo, F.; Ramirez-Medina, E.; Rodríguez, L.L.; de los Santos, T. Constitutively Active IRF7/IRF3 Fusion Protein Completely Protects Swine against Foot-and-Mouth Disease. J. Virol. 2016, 90, 8809–8821. [Google Scholar] [CrossRef]
- Vohr, H.-W. (Ed.) Encyclopedia of Immunotoxicology; Springer: Berlin/Heidelberg, Germany, 2016; ISBN 978-3-642-54595-5. [Google Scholar]
- Ellyard, J.I. Antigen-selected, immunoglobulin-secreting cells persist in human spleen and bone marrow. Blood 2004, 103, 3805–3812. [Google Scholar] [CrossRef] [PubMed]
- Manz, R.A.; Radbruch, A. Plasma cells for a lifetime? Eur. J. Immunol. 2002, 32, 923–927. [Google Scholar] [CrossRef]
- Zhang, Y.; Dominguez-Medina, C.; Cumley, N.J.; Heath, J.N.; Essex, S.J.; Bobat, S.; Schager, A.; Goodall, M.; Kracker, S.; Buckley, C.D.; et al. IgG1 Is Required for Optimal Protection after Immunization with the Purified Porin OmpD from Salmonella Typhimurium. J. Immunol. 2017, 199, 4103–4109. [Google Scholar] [CrossRef] [PubMed]
- Feurino, L.W.; Zhang, Y.; Bharadwaj, U.; Zhang, R.; Li, F.; Fisher, W.E.; Brunicardi, F.C.; Chen, C.; Yao, Q.; Li, M. IL-6 stimulates Th2 type cytokine secretion and upregulates VEGF and NRP-1 expression in pancreatic cancer cells. Cancer Biol. Ther. 2007, 6, 1096–1100. [Google Scholar] [CrossRef] [PubMed]
- Ulusoy, C.; Kim, E.; Tüzün, E.; Huda, R.; Yılmaz, V.; Poulas, K.; Trakas, N.; Skriapa, L.; Niarchos, A.; Strait, R.T.; et al. Preferential production of IgG1, IL-4 and IL-10 in MuSK-immunized mice. Clin. Immunol. 2014, 151, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Turqueti-Neves, A.; Otte, M.; Schwartz, C.; Schmitt, M.E.R.; Lindner, C.; Pabst, O.; Yu, P.; Voehringer, D. The Extracellular Domains of IgG1 and T Cell-Derived IL-4/IL-13 Are Critical for the Polyclonal Memory IgE Response In Vivo. PLoS Biol. 2015, 13, e1002290. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Das, S.; Agrawal, A.; Mukhopadhyay, I.; Ghosh, B. Genetic association of key Th1/Th2 pathway candidate genes, IRF2, IL6, IFNGR2, STAT4 and IL4RA, with atopic asthma in the Indian population. J. Hum. Genet. 2015, 60, 443–448. [Google Scholar] [CrossRef] [PubMed]
- Hodgkin, P.D.; Tangye, S.G.; Ferguson, A.; Avery, D.T.; Ma, C.S. Isotype Switching by Human B Cells Is Division-Associated and Regulated by Cytokines. J. Immunol. 2014, 169, 4298–4306. [Google Scholar]
- Maeda, Y.; Ohtsuka, H.; Tomioka, M.; Oikawa, M. Effect of progesterone on Th1/Th2/Th17 and Regulatory T cell-related genes in peripheral blood mononuclear cells during pregnancy in cows. Vet. Res. Commun. 2013, 37, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.T.; Martin, S.L.; Xia, L.; Gorham, J.D. TGF-β1 Uses Distinct Mechanisms to Inhibit IFN-γ Expression in CD4+ T Cells at Priming and at Recall: Differential Involvement of Stat4 and T-bet. J. Immunol. 2005, 174, 5950–5958. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Alonso, C.; Coutinho, A. Immunoglobulin C-gene expression. III. Possible induction of specific genetic events in activated B lymphocytes by the polyclonal stimuli driving clonal expansion. Eur. J. Immunol. 1982, 12, 502–506. [Google Scholar] [PubMed]
- Muranski, P.; Restifo, N.P. Adoptive immunotherapy of cancer using CD4+T cells. Curr. Opin. Immunol. 2009, 21, 200–208. [Google Scholar]
- Fuster, F.; Vargas, J.I.; Jensen, D.; Sarmiento, V.; Acuña, P.; Peirano, F.; Fuster, F.; Arab, J.P.; Martínez, F.; Fuster, F.; et al. CD4/CD8 ratio as a predictor of the response to HBV vaccination in HIV-positive patients: A prospective cohort study. Vaccine 2016, 34, 1889–1895. [Google Scholar] [CrossRef]
- Sato, H.; Adachi, E.; Lim, L.A.; Koga, M.; Koibuchi, T.; Tsutsumi, T.; Yotsuyanagi, H. CD4/CD8 ratio predicts the cellular immune response to acute hepatitis C in HIV-coinfected adults. J. Infect. Chemother. 2019, 25, 646–648. [Google Scholar]
- Bohórquez, J.A.; Wang, M.; Pérez-Simó, M.; Vidal, E.; Rosell, R.; Ganges, L. Low CD4/CD8 ratio in classical swine fever postnatal persistent infection generated at 3 weeks after birth. Transbound. Emerg. Dis. 2019, 66, 752–762. [Google Scholar]
- Carr, B.V.; Lefevre, E.A.; Windsor, M.A.; Inghese, C.; Gubbins, S.; Prentice, H.; Juleff, N.D.; Charleston, B. CD4+ T-cell responses to foot-and-mouth disease virus in vaccinated cattle. J. Gen. Virol. 2013, 94, 97–107. [Google Scholar] [CrossRef]
- Jiang, L.; Yu, Z.; Lin, Y.; Cui, L.; Yao, S.; Lv, L.; Liu, J. Low-molecular-weight polysaccharides from Agaricus blazei Murrill modulate the Th1 response in cancer immunity. Oncol. Lett. 2018, 15, 3429–3436. [Google Scholar]
- Maekawa, S.; Wang, P.-C.; Chen, S.-C. Comparative Study of Immune Reaction Against Bacterial Infection from Transcriptome Analysis. Front. Immunol. 2019, 10, 153. [Google Scholar]
- Zhi, X.; Lv, J.; Wei, Y.; Du, P.; Chang, Y.; Zhang, Y.; Gao, Y.; Wu, R. Foot-and-mouth disease virus infection stimulates innate immune signaling in the mouse macrophage RAW 264.7 cells. Can. J. Microbiol. 2018, 64, 155–166. [Google Scholar] [CrossRef] [PubMed]
- Bi, S.; Ma, X.; Wang, Y.; Chi, X.; Zhang, Y.; Xu, W.; Hu, S. Protective Effect of Ginsenoside Rg1 on Oxidative Damage Induced by Hydrogen Peroxide in Chicken Splenic Lymphocytes. Oxid. Med. Cell. Longev. 2019, 2019, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Xu, W.; Du, A.; Hu, S. Transcriptome analysis of bovine lymphocytes stimulated by Atractylodis macrocephalae Koidz. polysaccharides in vitro. Vet. Immunol. Immunopathol. 2018, 196, 30–34. [Google Scholar] [CrossRef]
- Shi, W.; Kou, Y.; Xiao, J.; Zhang, L.; Gao, F.; Kong, W.; Su, W.; Jiang, C.; Zhang, Y. Comparison of immunogenicity, efficacy and transcriptome changes of inactivated rabies virus vaccine with different adjuvants. Vaccine 2018, 36, 5020–5029. [Google Scholar] [CrossRef] [PubMed]
- Peterson, A.D.; Ghosh, A.P.; Maitra, R. Merging K -means with hierarchical clustering for identifying general-shaped groups. Stat. 2018, 7, e172. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, A.; Medzhitov, R. Regulation of Adaptive Immunity by the Innate Immune System. Science (80-) 2010, 327, 291–295. [Google Scholar] [CrossRef] [PubMed]
- Berczi, I.; Szentivanyi, A. Antigen presentation. In NeuroImmune Biology; Elsevier: Amsterdam, The Netherlands, 2003; pp. 301–313. [Google Scholar]
- Davis, S.J.; Ikemizu, S.; Evans, E.J.; Fugger, L.; Bakker, T.R.; van der Merwe, P.A. The nature of molecular recognition by T cells. Nat. Immunol. 2003, 4, 217–224. [Google Scholar] [CrossRef] [PubMed]


| Gene | Primer Sequence |
|---|---|
| (a) GAPDH | Forward: 5-TCGTCCGGTAGACAA AATGG-3 Reverse: 5-GAG GTC AATGAAGGGGTCGT-3 |
| (b) Trem3 | Forward: 5-CTGATGCTCTGTGTCTCGGG-3 Reverse: 5-AGGACAAGTCAGGGTCAGGT-3 |
| (c) Gm11127 | Forward: 5-GCCTCTTCCATCCACCGACT-3 Reverse: 5-TCATCATAAAAGCCACCACAGC-3 |
| (d) H2-Eb1 | Forward: 5-ATAAATTCCTTGTGCGGCGG-3 Reverse: 5-CAGGAGGTTGTGGTGTTCCA-3 |
| (e) Epx | Forward: 5-TTAGCCACACTCATCCTCACC-3 Reverse: 5-TGCTATGCAGTCTCGAAGGAC-3 |
| (f) Prg2 | Forward: 5-TCGCCTCCATCCACAGTTTC-3 Reverse: 5-CCATCAACCCATCGAAAGCG-3 |
| (g) Ifi44 | Forward: 5-ATGGCATTCTGCATTTGGCT-3 Reverse: 5-AATGCCTCCAGCTTGGACTT-3 |
| (h) Oas1g | Forward: 5-AGCCTAATCCCTTAATCTACACC-3 Reverse: 5-GCAGGTAGAGAACTCGCCAT-3 |
| (i) Oas2 | Forward: 5-CCTTGGAAAGTGCCAGTACCT-3 Reverse: 5-TGCCACAAGATCCCTCCTGTA-3 |
| (j) Slc15a2 | Forward: 5-GCAGAGGCACGGACTAGATAC-3 Reverse: 5-GGGATCAACGGCTGTTCACAT-3 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cui, X.; Wang, Y.; Maqbool, B.; Yuan, L.; He, S.; Zhang, C.; Xu, W.; Hu, S. Early IgG Response to Foot and Mouth Disease Vaccine Formulated with a Vegetable Oil Adjuvant. Vaccines 2019, 7, 143. https://doi.org/10.3390/vaccines7040143
Cui X, Wang Y, Maqbool B, Yuan L, He S, Zhang C, Xu W, Hu S. Early IgG Response to Foot and Mouth Disease Vaccine Formulated with a Vegetable Oil Adjuvant. Vaccines. 2019; 7(4):143. https://doi.org/10.3390/vaccines7040143
Chicago/Turabian StyleCui, Xuemei, Yong Wang, Babar Maqbool, Lijia Yuan, Shanshan He, Cenrong Zhang, Wei Xu, and Songhua Hu. 2019. "Early IgG Response to Foot and Mouth Disease Vaccine Formulated with a Vegetable Oil Adjuvant" Vaccines 7, no. 4: 143. https://doi.org/10.3390/vaccines7040143
APA StyleCui, X., Wang, Y., Maqbool, B., Yuan, L., He, S., Zhang, C., Xu, W., & Hu, S. (2019). Early IgG Response to Foot and Mouth Disease Vaccine Formulated with a Vegetable Oil Adjuvant. Vaccines, 7(4), 143. https://doi.org/10.3390/vaccines7040143





