Outer Membrane Vesicle Vaccines from Biosafe Surrogates Prevent Acute Lethal Glanders in Mice
Abstract
1. Introduction
2. Materials and Methods
2.1. Bacterial Strains and Culture Conditions
2.2. Stains, Western Blots and ELISA
2.3. Purification of OMVs
2.4. Transmission Electron Microscopy of OMVs
2.5. MALDI-TOF Scans of Purified Lipid A
2.6. Animal Experiments and Ethical Statement
2.7. Characterization of Antibody Responses
2.8. Opsonophagocytosis Assay
2.9. Statistical Analysis
3. Results
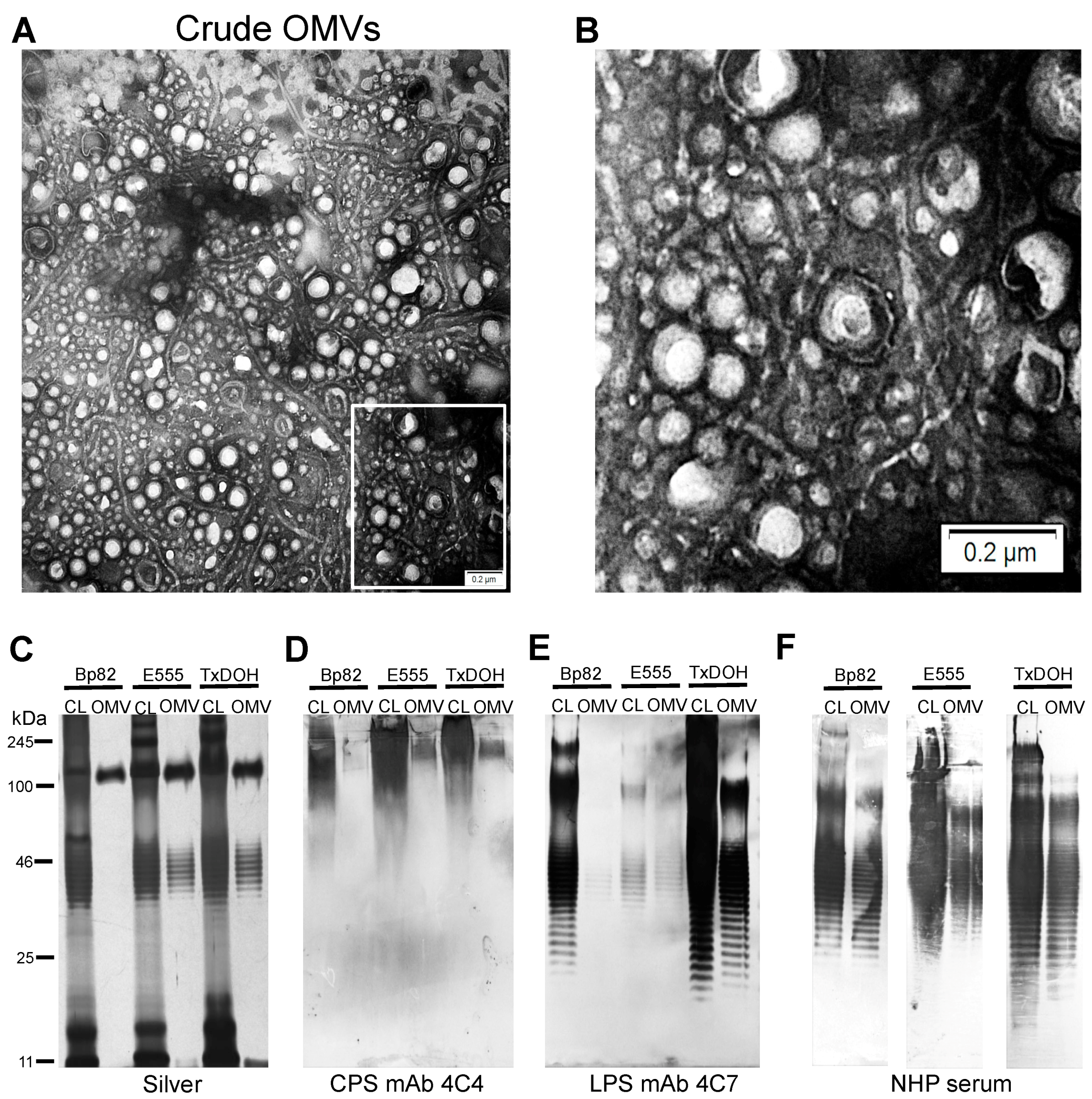
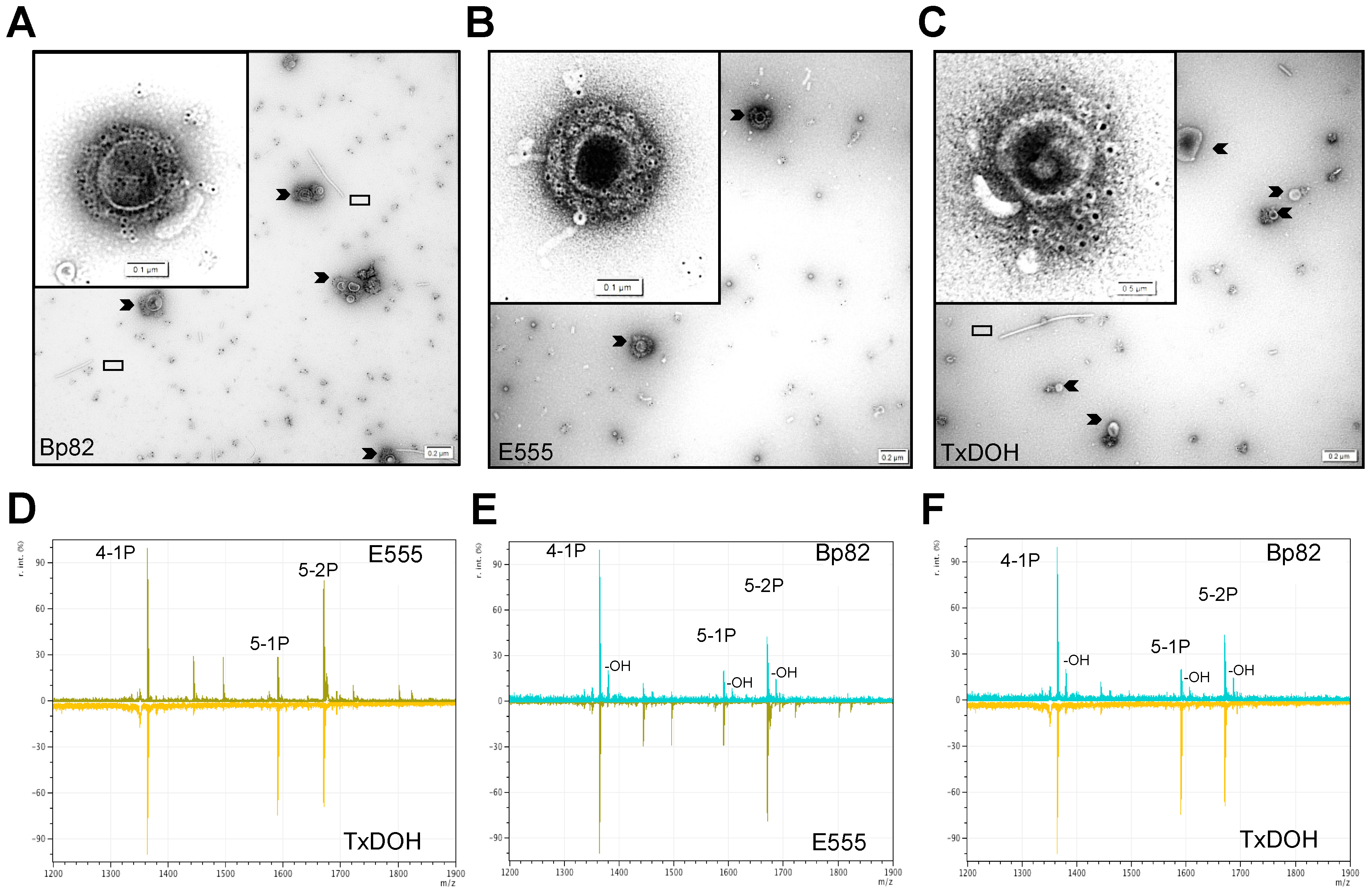
3.1. Purification and Characterization of OMVs
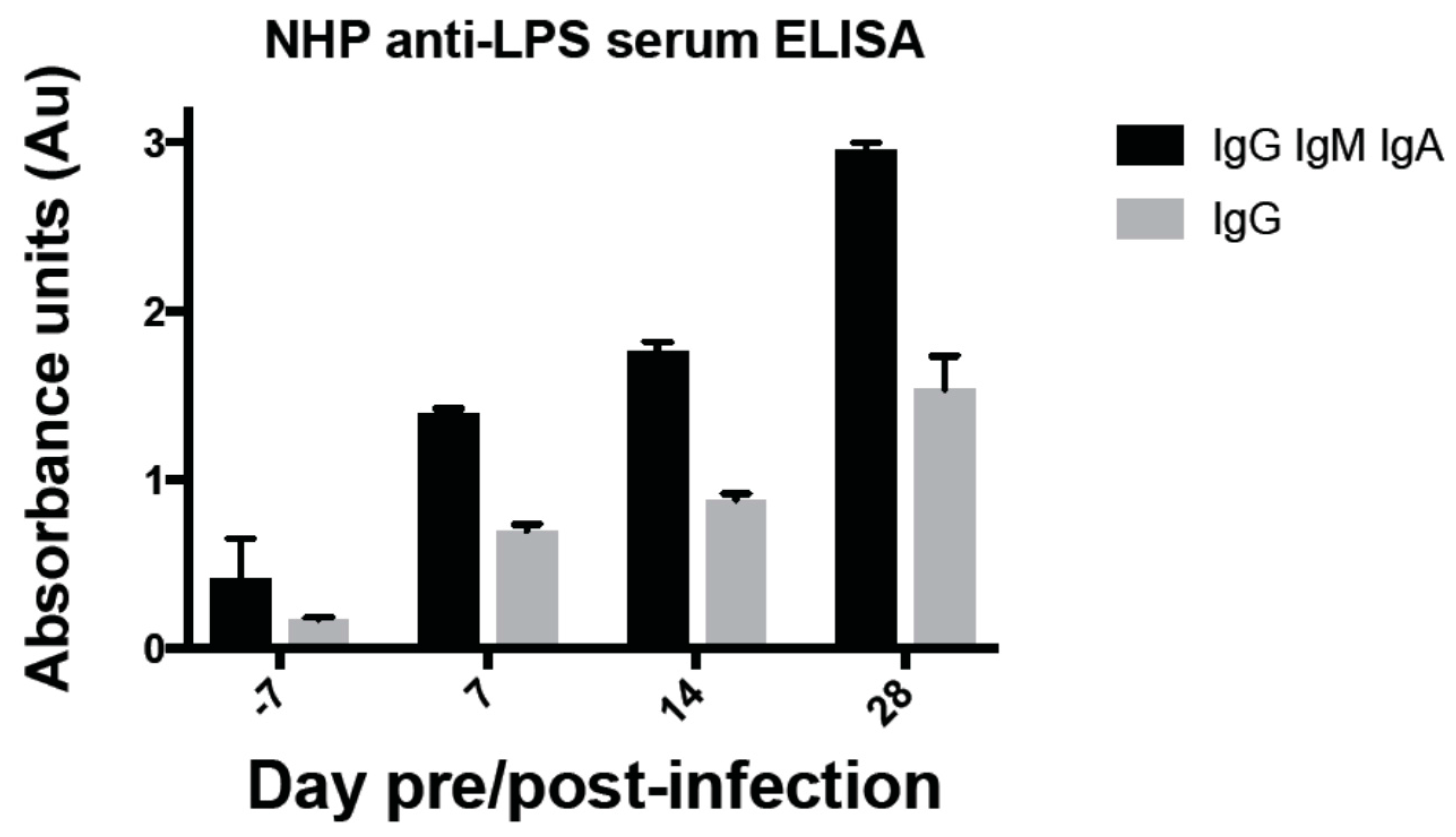
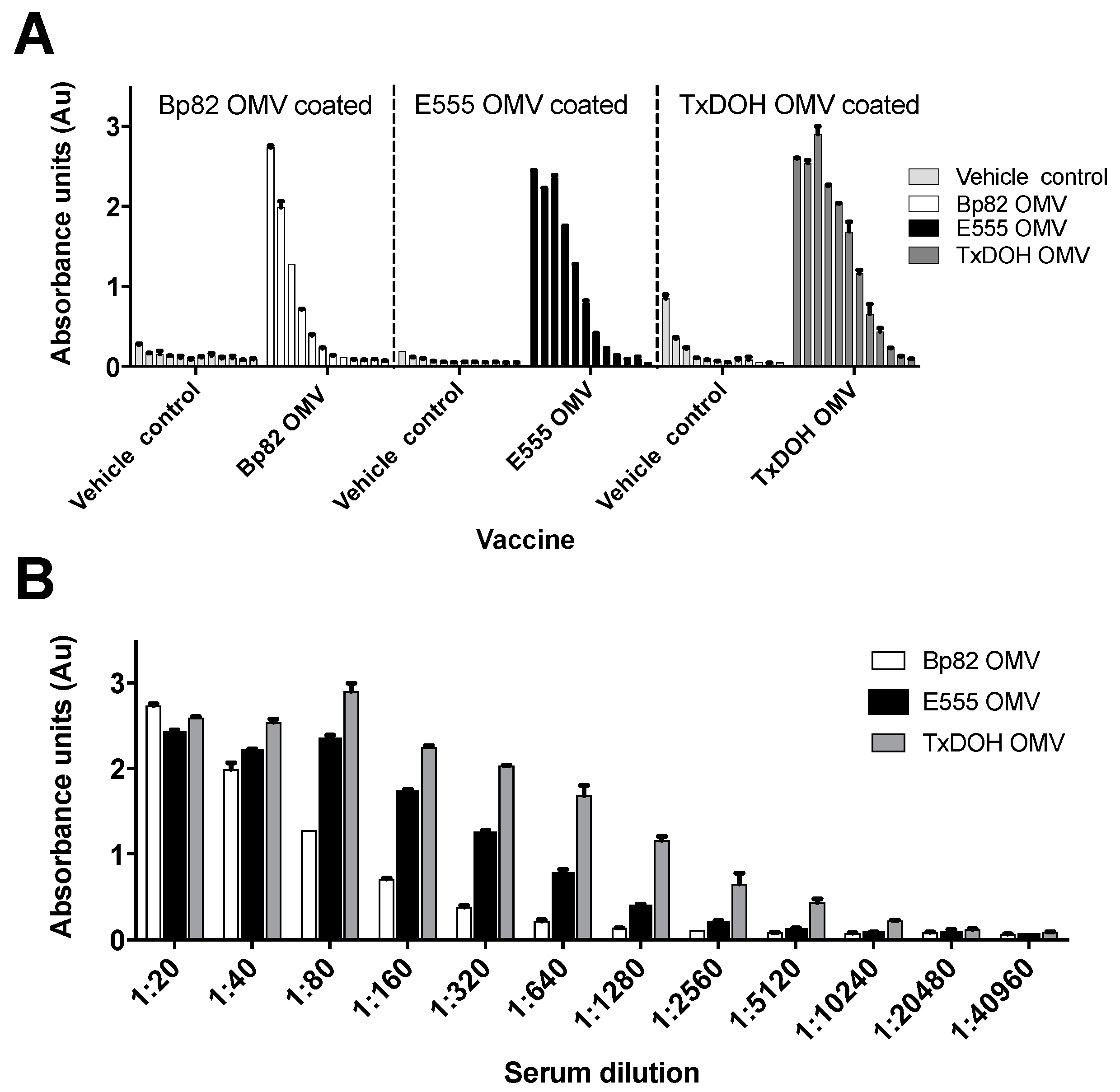
3.2. Strong Antibody Responses Are Generated by OMV Vaccination
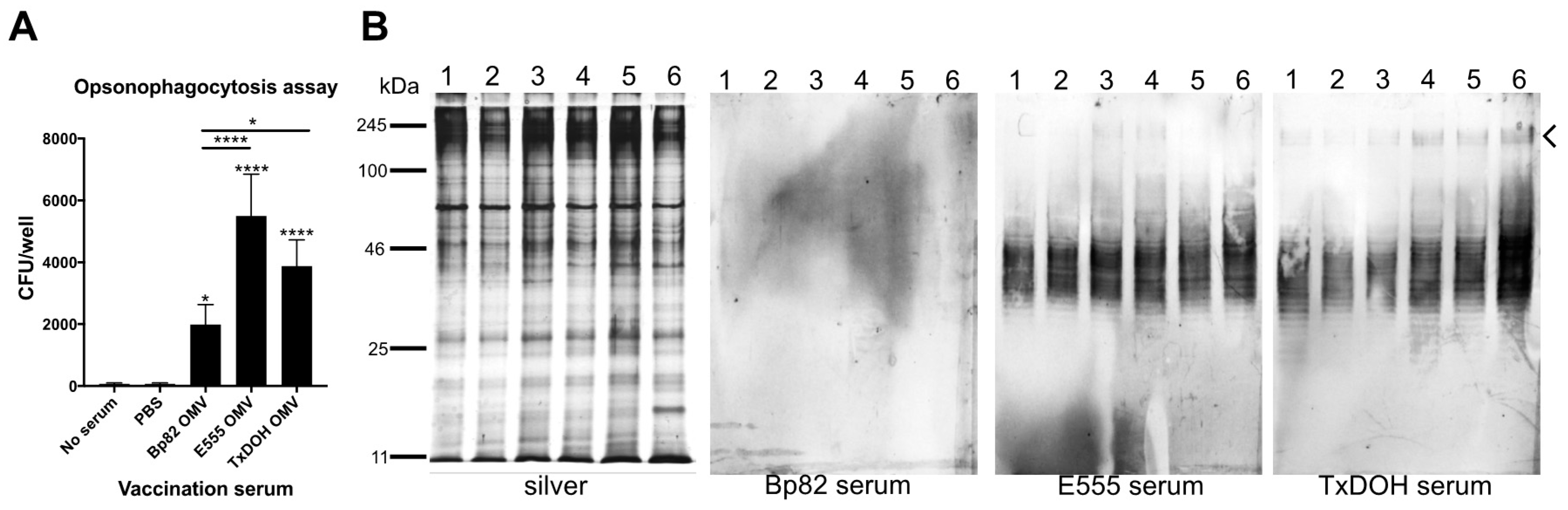
3.3. Characterization of B. mallei Specific Antibody Responses to OMVs
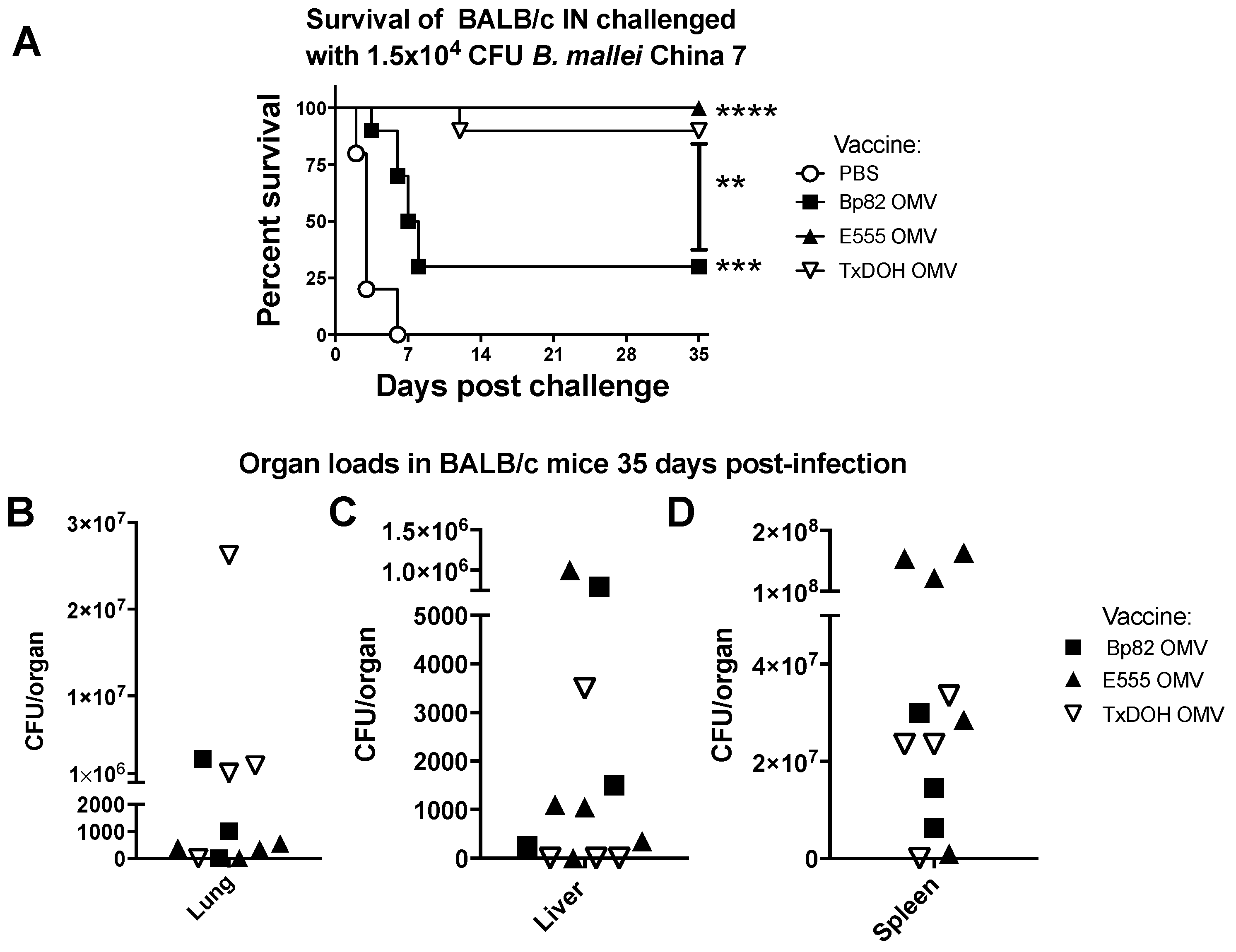
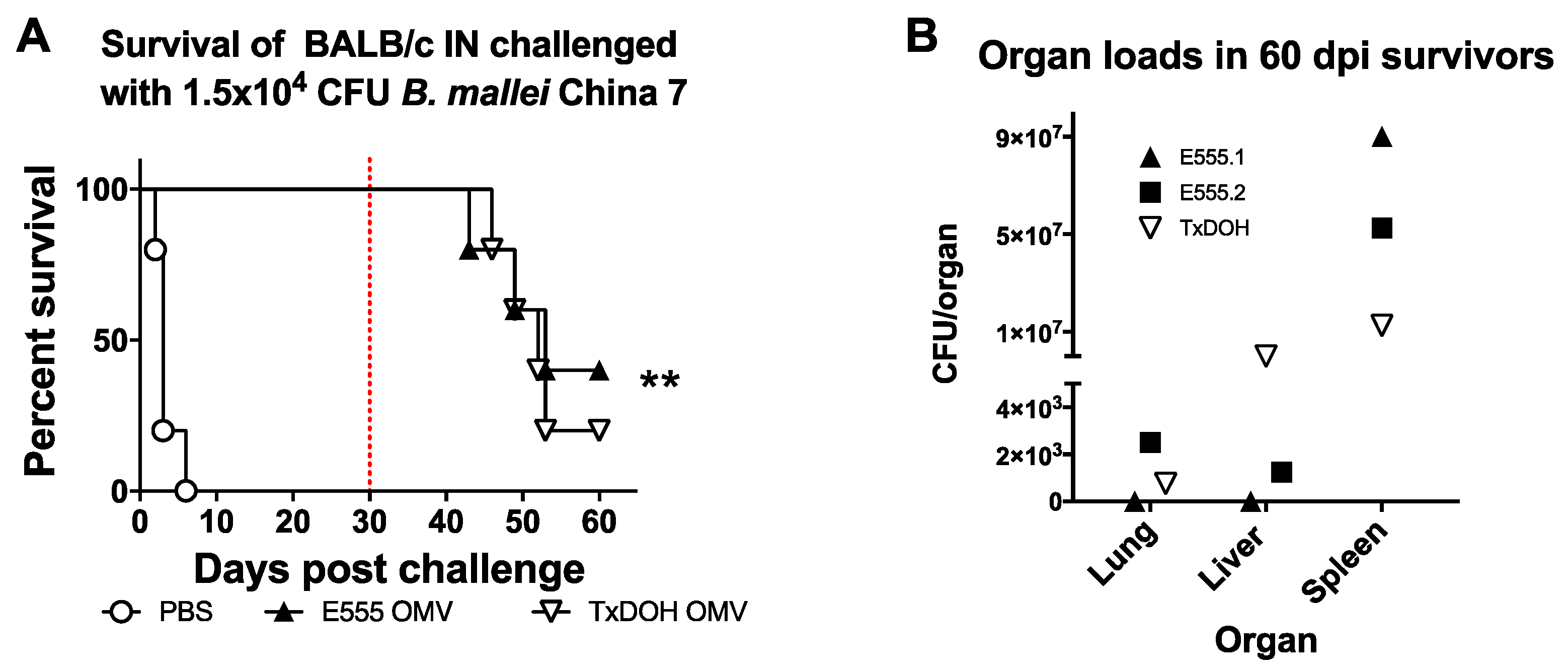
3.4. Ability of OMV Vaccines to Protect from Acute and Chronic Inhalational Glanders in BALB/c Mice
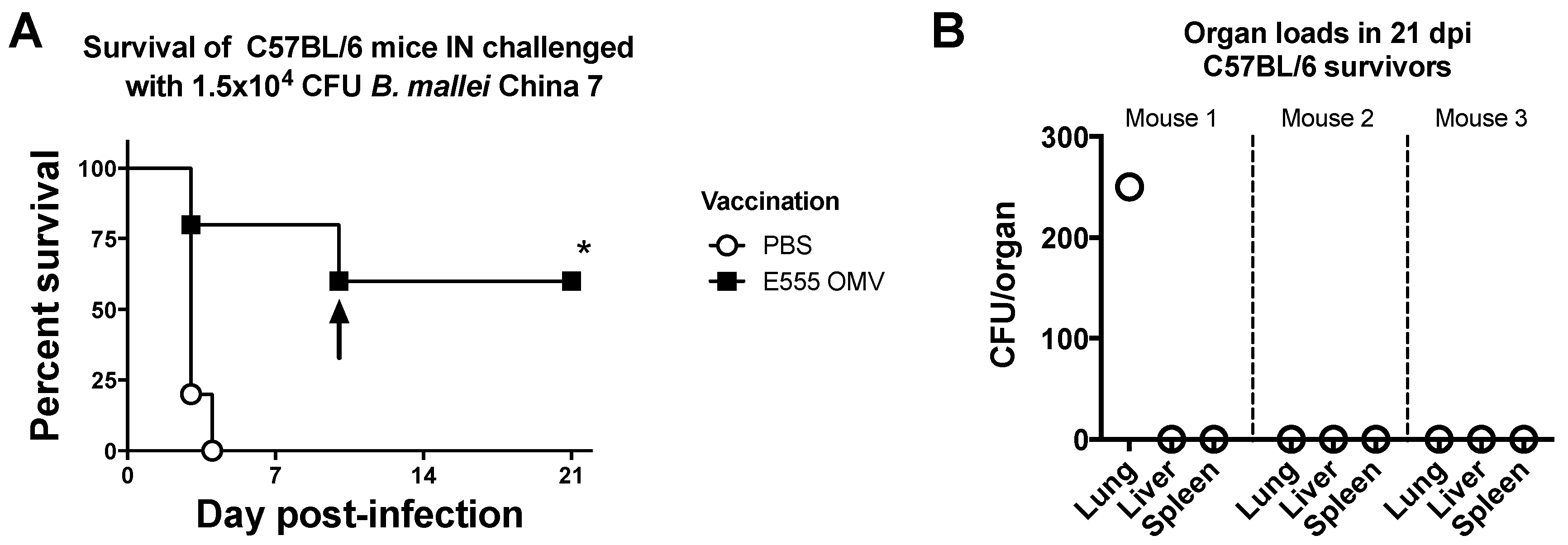
3.5. Ability of B. thailandensis E555 OMV Vaccine to Protect from Acute Lethal Glanders in C57BL/6 Mice
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Appendix A

References
- Sharrer, G.T. The great glanders epizootic, 1861–1866: A civil war legacy. Agric. Hist. 1995, 69, 79–97. [Google Scholar] [PubMed]
- Galyov, E.E.; Brett, P.J.; DeShazer, D. Molecular insights into Burkholderia pseudomallei and Burkholderia mallei pathogenesis. Annu. Rev. Microbiol. 2010, 64, 495–517. [Google Scholar] [CrossRef] [PubMed]
- Khan, I.; Wieler, L.H.; Melzer, F.; Elschner, M.C.; Muhammad, G.; Ali, S.; Sprague, L.D.; Neubauer, H.; Saqib, M. Glanders in animals: A review on epidemiology, clinical presentation, diagnosis and countermeasures. Transbound. Emerg. Dis. 2013, 60, 204–221. [Google Scholar] [CrossRef] [PubMed]
- Van Zandt, K.E.; Greer, M.T.; Gelhaus, H.C. Glanders: An overview of infection in humans. Orphanet J. Rare Dis. 2013, 8. [Google Scholar] [CrossRef] [PubMed]
- Wheelis, M. First shots fired in biological warfare. Nature 1998, 395. [Google Scholar] [CrossRef] [PubMed]
- Dance, D.A. Melioidosis and glanders as possible biological weapons. In Bioterrorism and Infectious Agents; Alibek, F.A., Ed.; Springer Science+Business Media Inc.: New York, NY, USA, 2005; pp. 99–145. [Google Scholar]
- Srinivasan, A.; Kraus, C.N.; DeShazer, D.; Becker, P.M.; Dick, J.D.; Spacek, L.; Bartlett, J.G.; Byrne, W.R.; Thomas, D.L. Glanders in a military research microbiologist. N. Engl. J. Med. 2001, 345, 256–258. [Google Scholar] [CrossRef] [PubMed]
- Miller, W.R.; Pannell, L.; Cravitz, L.; Tanner, W.A.; Ingalls, M.S. Studies on certain biological characteristics of malleomyces mallei and malleomyces pseudomallei: I. Morphology, cultivation, viability, and isolation from contaminated specimens. J. Bacteriol. 1948, 55, 115–126. [Google Scholar] [PubMed]
- Miller, W.R.; Pannell, L.; Cravitz, L.; Tanner, W.A.; Rosebury, T. Studies on certain biological characteristics of malleomyces mallei and malleomyces pseudomallei: II. Virulence and infectivity for animals. J. Bacteriol. 1948, 55, 127–135. [Google Scholar] [PubMed]
- Wittig, M.B.; Wohlsein, P.; Hagen, R.M.; Al Dahouk, S.; Tomaso, H.; Scholz, H.C.; Nikolaou, K.; Wernery, R.; Wernery, U.; Kinne, J.; et al. Glanders—A comprehensive review. DTW. Dtsch. Tierarztliche Wochenschr. 2006, 113, 323–330. [Google Scholar]
- Withers, M.R. Bacterial agents: Glanders and melioidosis. In Usamriid’s Medical Management of Biological Casualties Handbook, 8th ed.; U.S. Army Medical Research Institute of Infectious Diseases: Frederick, MD, USA, 2014; pp. 51–58. [Google Scholar]
- Goodyear, A.; Kellihan, L.; Bielefeldt-Ohmann, H.; Troyer, R.; Propst, K.; Dow, S. Protection from pneumonic infection with burkholderia species by inhalational immunotherapy. Infect. Immun. 2009, 77, 1579–1588. [Google Scholar] [CrossRef] [PubMed]
- Massey, S.; Johnston, K.; Mott, T.M.; Judy, B.M.; Kvitko, B.H.; Schweizer, H.P.; Estes, D.M.; Torres, A.G. In vivo bioluminescence imaging of Burkholderia mallei respiratory infection and treatment in the mouse model. Front. Microbiol. 2011, 2. [Google Scholar] [CrossRef] [PubMed]
- Mott, T.M.; Vijayakumar, S.; Sbrana, E.; Endsley, J.J.; Torres, A.G. Characterization of the Burkholderia mallei tonb mutant and its potential as a backbone strain for vaccine development. PLoS Negl. Trop. Dis. 2015, 9, e0003863. [Google Scholar] [CrossRef] [PubMed]
- Nierman, W.C.; DeShazer, D.; Kim, H.S.; Tettelin, H.; Nelson, K.E.; Feldblyum, T.; Ulrich, R.L.; Ronning, C.M.; Brinkac, L.M.; Daugherty, S.C.; et al. Structural flexibility in the Burkholderia mallei genome. Proc. Natl. Acad. Sci. USA 2004, 101, 14246–14251. [Google Scholar] [CrossRef] [PubMed]
- Ong, C.; Ooi, C.H.; Wang, D.; Chong, H.; Ng, K.C.; Rodrigues, F.; Lee, M.A.; Tan, P. Patterns of large-scale genomic variation in virulent and avirulent burkholderia species. Genome Res. 2004, 14, 2295–2307. [Google Scholar] [CrossRef] [PubMed]
- Brett, P.J.; Deshazer, D.; Woods, D.E. Characterization of Burkholderia pseudomallei and Burkholderia pseudomallei-like strains. Epidemiol. Infect. 1997, 118, 137–148. [Google Scholar] [CrossRef] [PubMed]
- Deshazer, D. Virulence of clinical and environmental isolates of burkholderia oklahomensis and Burkholderia thailandensis in hamsters and mice. FEMS Microbiol. Lett. 2007, 277, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Haraga, A.; West, T.E.; Brittnacher, M.J.; Skerrett, S.J.; Miller, S.I. Burkholderia thailandensis as a model system for the study of the virulence-associated type iii secretion system of Burkholderia pseudomallei. Infect. Immun. 2008, 76, 5402–5411. [Google Scholar] [CrossRef] [PubMed]
- Schell, M.A.; Ulrich, R.L.; Ribot, W.J.; Brueggemann, E.E.; Hines, H.B.; Chen, D.; Lipscomb, L.; Kim, H.S.; Mrazek, J.; Nierman, W.C.; et al. Type vi secretion is a major virulence determinant in Burkholderia mallei. Mol. Microbiol. 2007, 64, 1466–1485. [Google Scholar] [CrossRef] [PubMed]
- Burtnick, M.N.; Brett, P.J.; Harding, S.V.; Ngugi, S.A.; Ribot, W.J.; Chantratita, N.; Scorpio, A.; Milne, T.S.; Dean, R.E.; Fritz, D.L.; et al. The cluster 1 type vi secretion system is a major virulence determinant in Burkholderia pseudomallei. Infect. Immun. 2011, 79, 1512–1525. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, S.; Singh, P.; Robertson, J.D.; LeRoux, M.; Skerrett, S.J.; Goodlett, D.R.; West, T.E.; Mougous, J.D. Vgrg-5 is a burkholderia type vi secretion system-exported protein required for multinucleated giant cell formation and virulence. Infect. Immun. 2014, 82, 1445–1452. [Google Scholar] [CrossRef] [PubMed]
- Stevens, J.M.; Ulrich, R.L.; Taylor, L.A.; Wood, M.W.; Deshazer, D.; Stevens, M.P.; Galyov, E.E. Actin-binding proteins from Burkholderia mallei and Burkholderia thailandensis can functionally compensate for the actin-based motility defect of a Burkholderia pseudomallei bima mutant. J. Bacteriol. 2005, 187, 7857–7862. [Google Scholar] [CrossRef] [PubMed]
- Stone, J.K.; Mayo, M.; Grasso, S.A.; Ginther, J.L.; Warrington, S.D.; Allender, C.J.; Doyle, A.; Georgia, S.; Kaestli, M.; Broomall, S.M.; et al. Detection of Burkholderia pseudomallei O-antigen serotypes in near-neighbor species. BMC Microbiol. 2012, 12. [Google Scholar] [CrossRef] [PubMed]
- Qazi, O.; Prior, J.L.; Judy, B.M.; Whitlock, G.C.; Kitto, G.B.; Torres, A.G.; Estes, D.M.; Brown, K.A. Sero-characterization of lipopolysaccharide from Burkholderia thailandensis. Trans. R. Soc. Trop. Med. Hyg. 2008, 102, S58–S60. [Google Scholar] [CrossRef]
- Brett, P.J.; Burtnick, M.N.; Heiss, C.; Azadi, P.; DeShazer, D.; Woods, D.E.; Gherardini, F.C. Burkholderia thailandensis oaca mutants facilitate the expression of Burkholderia mallei-like o polysaccharides. Infect. Immun. 2011, 79, 961–969. [Google Scholar] [CrossRef] [PubMed]
- Tuanyok, A.; Stone, J.K.; Mayo, M.; Kaestli, M.; Gruendike, J.; Georgia, S.; Warrington, S.; Mullins, T.; Allender, C.J.; Wagner, D.M.; et al. The genetic and molecular basis of O-antigenic diversity in Burkholderia pseudomallei lipopolysaccharide. PLoS Negl. Trop. Dis. 2012, 6, e1453. [Google Scholar] [CrossRef] [PubMed]
- Reckseidler-Zenteno, S.L.; De Vinney, R.; Woods, D.E. The capsular polysacharride of Burkholderia pseudomallei contributes to survival in the serum by reducing complement factor c3b deposition. Infect. Immun. 2005, 73, 1106–1115. [Google Scholar] [CrossRef] [PubMed]
- Sim, B.M.; Chantratita, N.; Ooi, W.F.; Nandi, T.; Tewhey, R.; Wuthiekanun, V.; Thaipadungpanit, J.; Tumapa, S.; Ariyaratne, P.; Sung, W.K.; et al. Genomic acquisition of a capsular polysaccharide virulence cluster by non-pathogenic burkholderia isolates. Genome Biol. 2010, 11. [Google Scholar] [CrossRef] [PubMed]
- Bayliss, M.; Donaldson, M.I.; Nepogodiev, S.A.; Pergolizzi, G.; Scott, A.E.; Harmer, N.J.; Field, R.A.; Prior, J.L. Structural characterisation of the capsular polysaccharide expressed by Burkholderia thailandensis strain e555:: Wbii (pknock-kmr) and assessment of the significance of the 2-O-acetyl group in immune protection. Carbohydr. Res. 2017, 452, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Scott, A.E.; Laws, T.R.; D’Elia, R.V.; Stokes, M.G.; Nandi, T.; Williamson, E.D.; Tan, P.; Prior, J.L.; Atkins, T.P. Protection against experimental melioidosis following immunization with live Burkholderia thailandensis expressing a manno-heptose capsule. Clin. Vaccine Immunol. CVI 2013, 20, 1041–1047. [Google Scholar] [CrossRef] [PubMed]
- Moustafa, D.A.; Scarff, J.M.; Garcia, P.P.; Cassidy, S.K.; DiGiandomenico, A.; Waag, D.M.; Inzana, T.J.; Goldberg, J.B. Recombinant salmonella expressing Burkholderia mallei lps o antigen provides protection in a murine model of melioidosis and glanders. PLoS ONE 2015, 10, e0132032. [Google Scholar] [CrossRef] [PubMed]
- Hatcher, C.L.; Mott, T.M.; Muruato, L.A.; Sbrana, E.; Torres, A.G. Burkholderia mallei clh001 attenuated vaccine strain is immunogenic and protects against acute respiratory glanders. Infect. Immun. 2016, 84, 2345–2354. [Google Scholar] [CrossRef] [PubMed]
- Ulrich, R.L.; Amemiya, K.; Waag, D.M.; Roy, C.J.; DeShazer, D. Aerogenic vaccination with a Burkholderia mallei auxothroph protects against aerosol-initiated glanders in mice. Vaccine 2005, 23, 1986–1992. [Google Scholar] [CrossRef] [PubMed]
- Gregory, A.E.; Judy, B.M.; Qazi, O.; Blumentritt, C.A.; Brown, K.A.; Shaw, A.M.; Torres, A.G.; Titball, R.W. A gold nanoparticle-linked glycoconjugate vaccine against Burkholderia mallei. Nanomed. Nanotechnol. Biol. Med. 2015, 11, 447–456. [Google Scholar] [CrossRef] [PubMed]
- Torres, A.G.; Gregory, A.E.; Hatcher, C.L.; Vinet-Oliphant, H.; Morici, L.A.; Titball, R.W.; Roy, C.J. Protection of non-human primates against glanders with a gold nanoparticle glycoconjugate vaccine. Vaccine 2015, 33, 686–692. [Google Scholar] [CrossRef] [PubMed]
- Scott, A.E.; Burtnick, M.N.; Stokes, M.G.; Whelan, A.O.; Williamson, E.D.; Atkins, T.P.; Prior, J.L.; Brett, P.J. Burkholderia pseudomallei capsular polysaccharide conjugates provide protection against acute melioidosis. Infect. Immun. 2014, 82, 3206–3213. [Google Scholar] [CrossRef] [PubMed]
- Burtnick, M.N.; Heiss, C.; Roberts, R.A.; Schweizer, H.P.; Azadi, P.; Brett, P.J. Development of capsular polysaccharide-based glycoconjugates for immunization against melioidosis and glanders. Front. Cell. Infect. Microbiol. 2012, 2. [Google Scholar] [CrossRef] [PubMed]
- McBroom, A.J.; Kuehn, M.J. Release of outer membrane vesicles by gram-negative bacteria is a novel envelope stress response. Mol. Microbiol. 2007, 63, 545–558. [Google Scholar] [CrossRef] [PubMed]
- Choi, D.S.; Kim, D.K.; Choi, S.J.; Lee, J.; Choi, J.P.; Rho, S.; Park, S.H.; Kim, Y.K.; Hwang, D.; Gho, Y.S. Proteomic analysis of outer membrane vesicles derived from pseudomonas aeruginosa. Proteomics 2011, 11, 3424–3429. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.Y.; Bang, J.Y.; Park, G.W.; Choi, D.S.; Kang, J.S.; Kim, H.J.; Park, K.S.; Lee, J.O.; Kim, Y.K.; Kwon, K.H.; et al. Global proteomic profiling of native outer membrane vesicles derived from Escherichia coli. Proteomics 2007, 7, 3143–3153. [Google Scholar] [CrossRef] [PubMed]
- Van der Pol, L.; Stork, M.; van der Ley, P. Outer membrane vesicles as platform vaccine technology. Biotechnol. J. 2015, 10, 1689–1706. [Google Scholar] [CrossRef] [PubMed]
- Nieves, W.; Petersen, H.; Judy, B.M.; Blumentritt, C.A.; Russell-Lodrigue, K.; Roy, C.J.; Torres, A.G.; Morici, L.A. A Burkholderia pseudomallei outer membrane vesicle vaccine provides protection against lethal sepsis. Clin. Vaccine Immunol. CVI 2014, 21, 747–754. [Google Scholar] [CrossRef] [PubMed]
- Nieves, W.; Asakrah, S.; Qazi, O.; Brown, K.A.; Kurtz, J.; Aucoin, D.P.; McLachlan, J.B.; Roy, C.J.; Morici, L.A. A naturally derived outer-membrane vesicle vaccine protects against lethal pulmonary Burkholderia pseudomallei infection. Vaccine 2011, 29, 8381–8389. [Google Scholar] [CrossRef] [PubMed]
- Propst, K.L.; Mima, T.; Choi, K.H.; Dow, S.W.; Schweizer, H.P. A Burkholderia pseudomallei δpurm mutant is avirulent in immunocompetent and immunodeficient animals: Candidate strain for exclusion from select-agent lists. Infect. Immun. 2010, 78, 3136–3143. [Google Scholar] [CrossRef] [PubMed]
- Norris, M.H.; Kang, Y.; Lu, D.; Wilcox, B.A.; Hoang, T.T. Glyphosate resistance as a novel select-agent-compliant, non-antibiotic selectable-marker in chromosomal mutagenesis of the essential genes asd and dapb of Burkholderia pseudomallei. Appl. Environ. Microbiol. 2009, 75, 6062–6075. [Google Scholar] [CrossRef] [PubMed]
- Norris, M.H.; Kang, Y.; Wilcox, B.; Hoang, T.T. Stable, site-specific fluorescent tagging constructs optimized for burkholderia species. Appl. Environ. Microbiol. 2010, 76, 7635–7640. [Google Scholar] [CrossRef] [PubMed]
- Norris, M.H.; Propst, K.L.; Kang, Y.; Dow, S.W.; Schweizer, H.P.; Hoang, T.T. The Burkholderia pseudomallei δasd mutant exhibits attenuated intracellular infectivity and imparts protection against acute inhalation melioidosis in mice. Infect. Immun. 2011, 79, 4010–4018. [Google Scholar] [CrossRef] [PubMed]
- Norris, M.H. Identifying Virulence Factors and Regulators Contributing to Pathogenesis by the Select-Agent Bacterium Burkholderia pseudomallei. Docotral Thesis, University of Hawaii at Manoa, Honolulu, HI, USA, 2014. [Google Scholar]
- Norris, M.H.; Rahman Khan, M.S.; Schweizer, H.P.; Tuanyok, A. An avirulent Burkholderia pseudomallei ∆purm strain with atypical type b lps: Expansion of the toolkit for biosafe studies of melioidosis. BMC Microbiol. 2017, 17, 132. [Google Scholar] [CrossRef] [PubMed]
- Norris, M.H.; Schweizer, H.P.; Tuanyok, A. Structural diversity of Burkholderia pseudomallei lipopolysaccharides affects innate immune signaling. PLoS Negl. Trop. Dis. 2017, 11, e0005571. [Google Scholar] [CrossRef] [PubMed]
- Kulp, A.; Kuehn, M.J. Biological functions and biogenesis of secreted bacterial outer membrane vesicles. Annu. Rev. Microbiol. 2010, 64, 163–184. [Google Scholar] [CrossRef] [PubMed]
- Lam, J.S.; Anderson, E.M.; Hao, Y. Lps quantitation procedures. Methods Mol. Biol. 2014, 1149, 375–402. [Google Scholar] [PubMed]
- Lindner, B. Matrix-assisted laser desorption/ionization time-of-flight mass spectrometry of lipopolysaccharides. In Bacterial Toxins: Methods and Protocols; Holst, O., Ed.; Humana Press: Totowa, NJ, USA, 2000; pp. 311–325. [Google Scholar]
- Brett, P.J.; Burtnick, M.N.; Snyder, D.S.; Shannon, J.G.; Azadi, P.; Gherardini, F.C. Burkholderia mallei expresses a unique lipopolysaccharide mixture that is a potent activator of human toll-like receptor 4 complexes. Mol. Microbiol. 2007, 63, 379–390. [Google Scholar] [CrossRef] [PubMed]
- Goodyear, A.; Troyer, R.; Bielefeldt-Ohmann, H.; Dow, S. Myd88-dependent recruitment of monocytes and dendritic cells required for protection from pulmonary Burkholderia mallei infection. Infect. Immun. 2012, 80, 110–120. [Google Scholar] [CrossRef] [PubMed]
- Anuntagool, N.; Naigowit, P.; Petkanchanapong, V.; Aramsri, P.; Panichakul, T.; Sirisinha, S. Monoclonal antibody-based rapid identification of Burkholderia pseudomallei in blood culture fluid from patients with community-acquired septicaemia. J. Med. Microbiol. 2000, 49, 1075–1078. [Google Scholar] [CrossRef] [PubMed]
- Samosornsuk, N.; Lulitanond, A.; Saenla, N.; Anuntagool, N.; Wongratanacheewin, S.; Sirisinha, S. Short report: Evaluation of a monoclonal antibody-based latex agglutination test for rapid diagnosis of septicemic melioidosis. Am. J. Trop. Med. Hyg. 1999, 61, 735–737. [Google Scholar] [CrossRef] [PubMed]
- Kenfack, M.T.; Mazur, M.; Nualnoi, T.; Shaffer, T.L.; Ngassimou, A.; Bleriot, Y.; Marrot, J.; Marchetti, R.; Sintiprungrat, K.; Chantratita, N.; et al. Deciphering minimal antigenic epitopes associated with Burkholderia pseudomallei and Burkholderia mallei lipopolysaccharide O-antigens. Nat. Commun. 2017, 8. [Google Scholar] [CrossRef]
- Marchetti, R.; Dillon, M.J.; Burtnick, M.N.; Hubbard, M.A.; Kenfack, M.T.; Bleriot, Y.; Gauthier, C.; Brett, P.J.; AuCoin, D.P.; Lanzetta, R.; et al. Burkholderia pseudomallei capsular polysaccharide recognition by a monoclonal antibody reveals key details toward a biodefense vaccine and diagnostics against melioidosis. ACS Chem. Biol. 2015, 10, 2295–2302. [Google Scholar] [CrossRef] [PubMed]
- Novem, V.; Shui, G.; Wang, D.; Bendt, A.K.; Sim, S.H.; Liu, Y.; Thong, T.W.; Sivalingam, S.P.; Ooi, E.E.; Wenk, M.R.; et al. Structural and biological diversity of lipopolysaccharides from Burkholderia pseudomallei and Burkholderia thailandensis. Clin. Vaccine Immunol. CVI 2009, 16, 1420–1428. [Google Scholar] [CrossRef] [PubMed]
- Weehuizen, T.A.; Prior, J.L.; van der Vaart, T.W.; Ngugi, S.A.; Nepogodiev, S.A.; Field, R.A.; Kager, L.M.; van’t Veer, C.; de Vos, A.F.; Wiersinga, W.J. Differential toll-like receptor-signalling of Burkholderia pseudomallei lipopolysaccharide in murine and human models. PLoS ONE 2015, 10, e0145397. [Google Scholar] [CrossRef] [PubMed]
- Finkelman, F.D.; Holmes, J.; Katona, I.M.; Urban, J.F., Jr.; Beckmann, M.P.; Park, L.S.; Schooley, K.A.; Coffman, R.L.; Mosmann, T.R.; Paul, W.E. Lymphokine control of in vivo immunoglobulin isotype selection. Annu. Rev. Immunol. 1990, 8, 303–333. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, P.J.; Guo, Q.; Waag, D.M.; Donnenberg, M.S. The type iv pilin of Burkholderia mallei is highly immunogenic but fails to protect against lethal aerosol challenge in a murine model. Infect. Immun. 2007, 75, 3027–3032. [Google Scholar] [CrossRef] [PubMed]
- Bishop, A.L.; Schild, S.; Patimalla, B.; Klein, B.; Camilli, A. Mucosal immunization with vibrio cholerae outer membrane vesicles provides maternal protection mediated by antilipopolysaccharide antibodies that inhibit bacterial motility. Infect. Immun. 2010, 78, 4402–4420. [Google Scholar] [CrossRef] [PubMed]
- Holst, J.; Martin, D.; Arnold, R.; Huergo, C.C.; Oster, P.; O’Hallahan, J.; Rosenqvist, E. Properties and clinical performance of vaccines containing outer membrane vesicles from neisseria meningitidis. Vaccine 2009, 27, B3–B12. [Google Scholar] [CrossRef] [PubMed]
- Alving, C.R.; Rao, M. Lipid a and liposomes containing lipid a as antigens and adjuvants. Vaccine 2008, 26, 3036–3045. [Google Scholar] [CrossRef] [PubMed]
- Alving, C.R. Vaccine Adjuvants. In Vaccines for Biodefense and Emerging and Neglected Diseases; Stanberry, L.R., Ed.; Academic Press: London, UK, 2009; pp. 115–129. [Google Scholar]
- Warawa, J.M. Evaluation of surrogate animal models of melioidosis. Front. Microbiol. 2010, 1, 141. [Google Scholar] [CrossRef] [PubMed]
- Leakey, A.K.; Ulett, G.C.; Hirst, R.G. Balb/c and c57bl/6 mice infected with virulent Burkholderia pseudomallei provide contrasting animal models for the acute and chronic forms of human melioidosis. Microb. Pathog. 1998, 24, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Locksley, R.M.; Heinzel, F.P.; Sadick, M.D.; Holaday, B.J.; Gardner, K.D., Jr. Murine cutaneous leishmaniasis: Susceptibility correlates with differential expansion of helper t-cell subsets. Ann. Inst. Pasteur. Immunol. 1987, 138, 744–749. [Google Scholar] [CrossRef]
- Mills, C.D.; Kincaid, K.; Alt, J.M.; Heilman, M.J.; Hill, A.M. M-1/m-2 macrophages and the th1/th2 paradigm. J. Immunol. 2000, 164, 6166–6173. [Google Scholar] [CrossRef] [PubMed]
- Mattner, F.; Magram, J.; Ferrante, J.; Launois, P.; Di Padova, K.; Behin, R.; Gately, M.K.; Louis, J.A.; Alber, G. Genetically resistant mice lacking interleukin-12 are susceptible to infection with Leishmania major and mount a polarized th2 cell response. Eur. J. Immunol. 1996, 26, 1553–1559. [Google Scholar] [CrossRef] [PubMed]
- Elkins, K.L.; Cooper, A.; Colombini, S.M.; Cowley, S.C.; Kieffer, T.L. In vivo clearance of an intracellular bacterium, francisella tularensis lvs, is dependent on the p40 subunit of interleukin-12 (il-12) but not on il-12 p70. Infect. Immun. 2002, 70, 1936–1948. [Google Scholar] [CrossRef] [PubMed]
- Alves, N.J.; Turner, K.B.; Medintz, I.L.; Walper, S.A. Protecting enzymatic function through directed packaging into bacterial outer membrane vesicles. Sci. Rep. 2016, 6, 24866. [Google Scholar] [CrossRef] [PubMed]

| Antigen | Group | Geometric Mean Titer 1 | ||
|---|---|---|---|---|
| IgG1 | IgG2a | IgG1/IgG2a Ratio | ||
| B. mallei China 7 lysate | PBS | 100 | 100 | 1.00 |
| Bp82 OMV | 984 | 100 | 9.84 | |
| E555 OMV | 13718 | 400 | 34.30 | |
| TxDOH OMV | 23702 | 5796 | 4.09 | |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Norris, M.H.; Khan, M.S.R.; Chirakul, S.; Schweizer, H.P.; Tuanyok, A. Outer Membrane Vesicle Vaccines from Biosafe Surrogates Prevent Acute Lethal Glanders in Mice. Vaccines 2018, 6, 5. https://doi.org/10.3390/vaccines6010005
Norris MH, Khan MSR, Chirakul S, Schweizer HP, Tuanyok A. Outer Membrane Vesicle Vaccines from Biosafe Surrogates Prevent Acute Lethal Glanders in Mice. Vaccines. 2018; 6(1):5. https://doi.org/10.3390/vaccines6010005
Chicago/Turabian StyleNorris, Michael H., Mohammad S. R. Khan, Sunisa Chirakul, Herbert P. Schweizer, and Apichai Tuanyok. 2018. "Outer Membrane Vesicle Vaccines from Biosafe Surrogates Prevent Acute Lethal Glanders in Mice" Vaccines 6, no. 1: 5. https://doi.org/10.3390/vaccines6010005
APA StyleNorris, M. H., Khan, M. S. R., Chirakul, S., Schweizer, H. P., & Tuanyok, A. (2018). Outer Membrane Vesicle Vaccines from Biosafe Surrogates Prevent Acute Lethal Glanders in Mice. Vaccines, 6(1), 5. https://doi.org/10.3390/vaccines6010005






