Biological Characterization and DIVA Potential of Three Rough Brucella melitensis Vaccine Strains
Abstract
1. Introduction
2. Materials and Methods
2.1. Strains and Cell Lines
2.2. Primers and PCR Conditions
2.3. Flow Diagram of Experiment
2.4. Construction of Gene Deletion Mutants
2.5. Agglutination Tests
2.6. Western Blotting
2.7. Bacterial Growth Curves
2.8. Polymyxin B Sensitivity Assay
2.9. Adhesion, Invasion, and Intracellular Survival Assay
2.10. Macrophage Cytotoxicity Assay
2.11. RNA Extraction and qPCR
2.12. Evaluation of Residual Virulence
2.13. Enzyme-Linked Immunosorbent Assay (ELISA)
2.14. Virulence Challenge
2.15. Statistical Analysis
3. Results
3.1. Three Spontaneous Rough-Type Mutants of B. melitensis Exhibit Attenuated Virulence
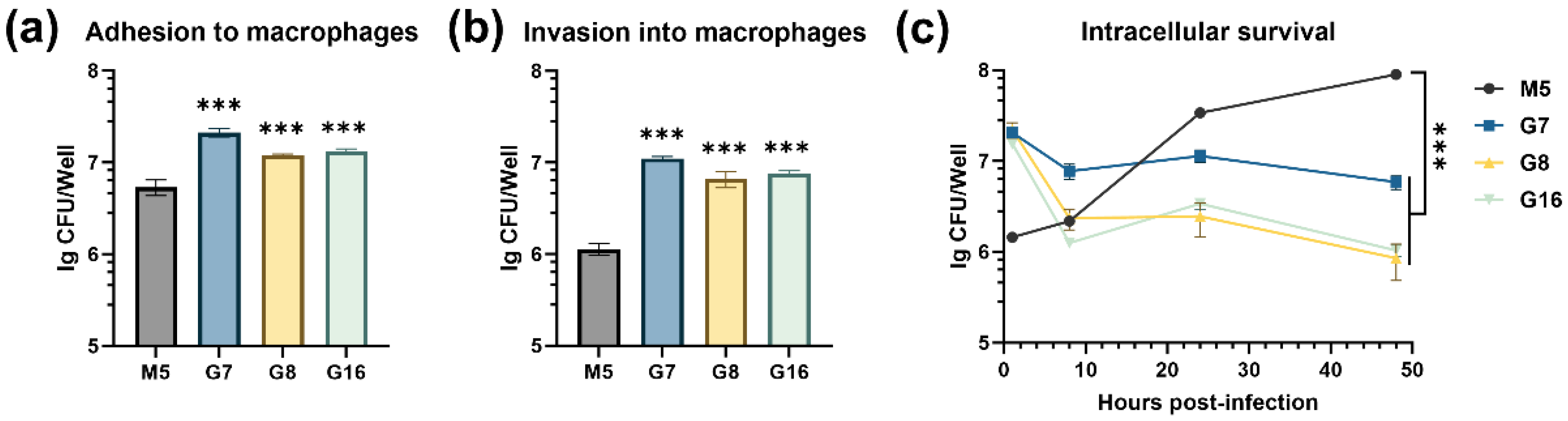
3.2. Rough Brucella Strains Show Enhanced Adhesion and Invasion but Impaired Intracellular Survival
3.3. Rough Brucella Strains Induce Macrophage Death and Significantly Activate Inflammatory Responses
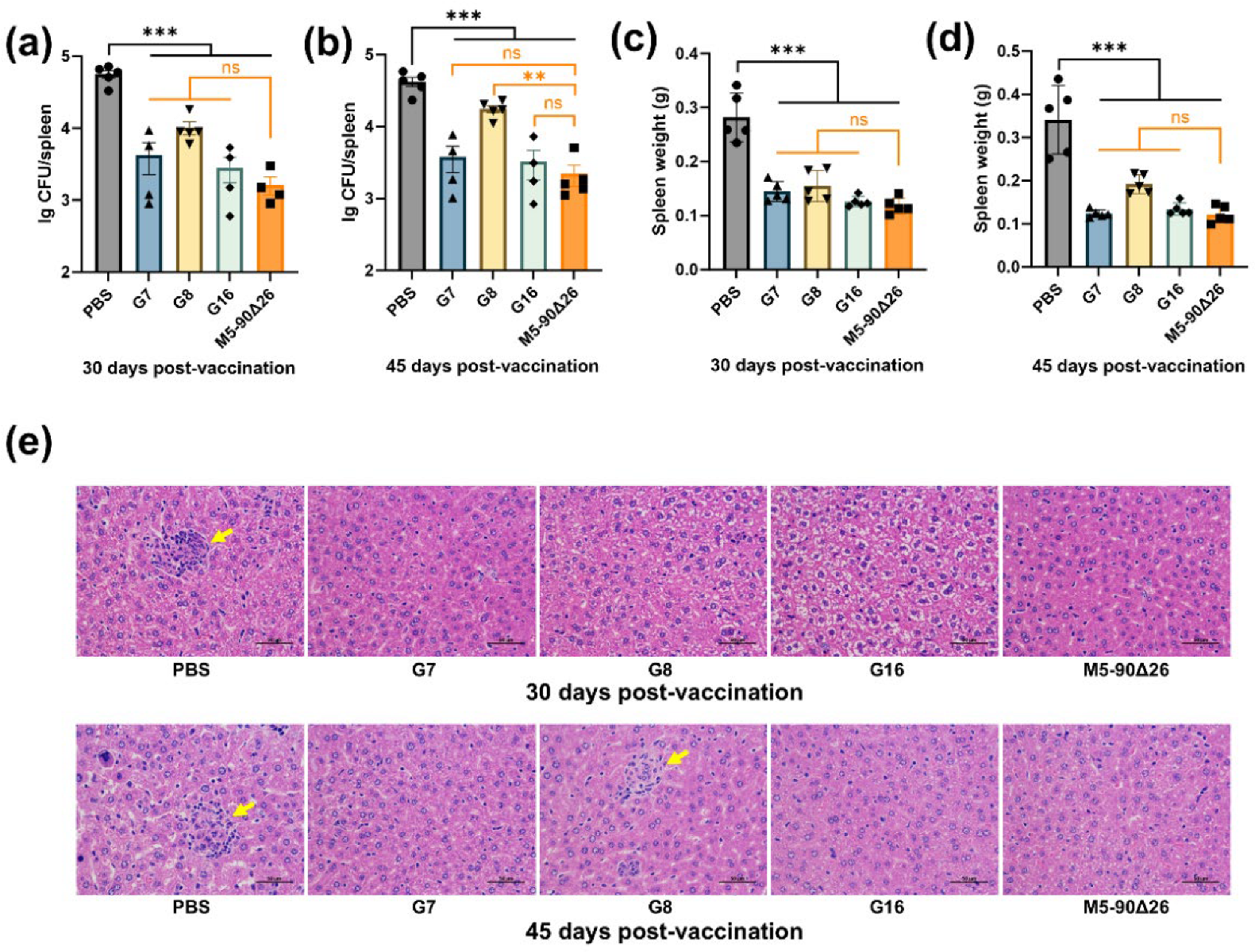
3.4. Rough Brucella Strains Exhibit Significantly Attenuated Virulence in Mice
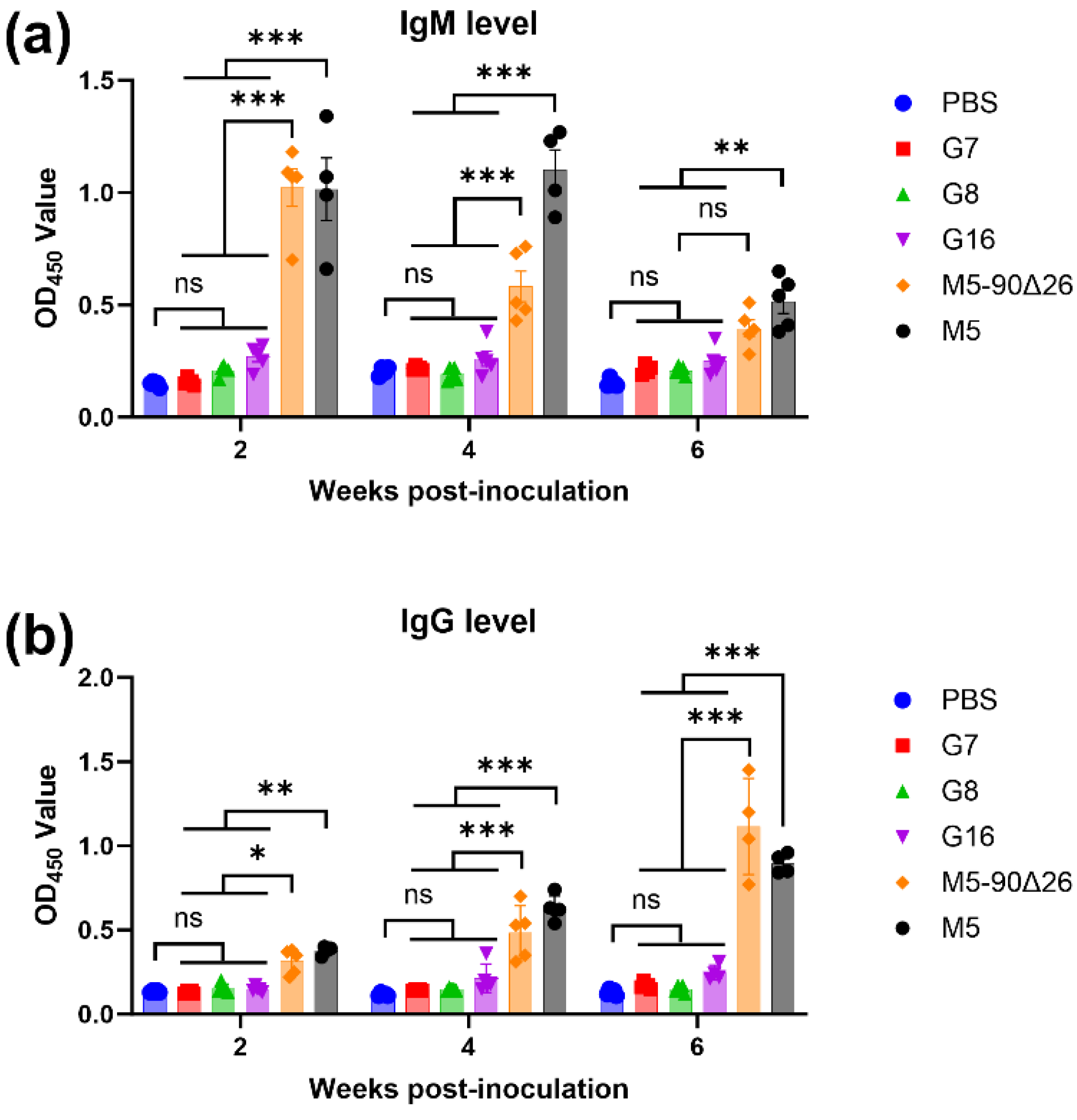
3.5. Rough Brucella Strains Induce a Th1-Biased Cellular Immune Response in Vaccinated Mice
3.6. Rough Brucella Strains G7 and G16 Provide Effective Immunoprotection in Mice
3.7. Rough Brucella Strains Can Be Differentially Diagnosed Using the LPS-ELISA Method
4. Discussion
4.1. Three Rough-Type Brucella Strains with Spontaneous O-Antigen Loss Exhibit Attenuation and Vaccine Potential
4.2. Attenuated Rough Brucella Strains G7/G8/G16 Show Hyper-Adhesion, Cytotoxicity, and Immune Activation
4.3. G16, a Semi-Rough Brucella Mutant, Induces Robust Th1 Immunity and Memory Response, Outperforming Other Vaccine Candidates
4.4. G16’s Semi-Rough Phenotype Confers Robust Protection, Outperforming Fully Rough Brucella Vaccine Strains
4.5. All Three Rough Brucella Vaccine Candidates Enable Reliable DIVA Discrimination via LPS-ELISA
4.6. Translational Challenges and Safety Considerations for Rough Brucella DIVA Vaccines
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| DIVA | Differentiating Infected from Vaccinated Animals |
| LDH | Lactate dehydrogenase |
| qPCR | Quantitative polymerase chain reaction |
| ELISA | Enzyme-linked immunosorbent assay |
| LPS | Lipopolysaccharide |
| CFU | Colony-forming unit |
References
- Boschiroli, M.L.; Foulongne, V.; O’Callaghan, D. Brucellosis: A worldwide zoonosis. Curr. Opin. Microbiol. 2001, 4, 58–64. [Google Scholar] [CrossRef]
- Qureshi, K.A.; Parvez, A.; Fahmy, N.A.; Abdel Hady, B.H.; Kumar, S.; Ganguly, A.; Atiya, A.; Elhassan, G.O.; Alfadly, S.O.; Parkkila, S.; et al. Brucellosis: Epidemiology, pathogenesis, diagnosis and treatment-a comprehensive review. Ann. Med. 2023, 55, 2295398. [Google Scholar] [CrossRef] [PubMed]
- de Figueiredo, P.; Ficht, T.A.; Rice-Ficht, A.; Rossetti, C.A.; Adams, L.G. Pathogenesis and immunobiology of brucellosis: Review of Brucella-host interactions. Am. J. Pathol. 2015, 185, 1505–1517. [Google Scholar] [CrossRef]
- von Bargen, K.; Gorvel, J.P.; Salcedo, S.P. Internal affairs: Investigating the Brucella intracellular lifestyle. FEMS Microbiol. Rev. 2012, 36, 533–562. [Google Scholar] [CrossRef]
- Seleem, M.N.; Boyle, S.M.; Sriranganathan, N. Brucella: A pathogen without classic virulence genes. Vet. Microbiol. 2008, 129, 1–14. [Google Scholar] [CrossRef]
- Stranahan, L.W.; Arenas-Gamboa, A.M. When the going gets rough: The significance of Brucella lipopolysaccharide phenotype in host-pathogen interactions. Front. Microbiol. 2021, 12, 713157. [Google Scholar] [CrossRef]
- Abdelgawad, H.A.; Lian, Z.; Yin, Y.; Fang, T.; Tian, M.; Yu, S. Characterization of Brucella abortus mutant A19mut2, a potential DIVA vaccine candidate with a modification on lipopolysaccharide. Vaccines 2023, 11, 1273. [Google Scholar] [CrossRef]
- Lalsiamthara, J.; Gogia, N.; Goswami, T.K.; Singh, R.K.; Chaudhuri, P. Intermediate rough Brucella abortus S19Δper mutant is DIVA enable, safe to pregnant guinea pigs and confers protection to mice. Vaccine 2015, 33, 2577–2583. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.Q.; Shi, J.X.; Fu, W.D.; Zhang, Y.; Zhang, J.; Wang, Z.; Li, T.S.; Chen, C.F.; Guo, F.; Zhang, H. A Brucella melitensis M5–90 wboA deletion strain is attenuated and enhances vaccine efficacy. Mol. Immunol. 2015, 66, 276–283. [Google Scholar] [CrossRef] [PubMed]
- Heidary, M.; Dashtbin, S.; Ghanavati, R.; Mahdizade Ari, M.; Bostanghadiri, N.; Darbandi, A.; Navidifar, T.; Talebi, M. Evaluation of Brucellosis Vaccines: A Comprehensive Review. Front. Vet. Sci. 2022, 9, 925773. [Google Scholar] [CrossRef]
- Haine, V.; Sinon, A.; Van Steen, F.; Rousseau, S.; Dozot, M.; Lestrate, P.; Lambert, C.; Letesson, J.J.; De Bolle, X. Systematic Targeted Mutagenesis of Brucella melitensis 16M Reveals a Major Role for GntR Regulators in the Control of Virulence. Infect. Immun. 2005, 73, 5578–5586. [Google Scholar] [CrossRef] [PubMed]
- Tian, M.; Lian, Z.; Bao, Y.; Bao, S.; Yin, Y.; Li, P.; Ding, C.; Wang, S.; Li, T.; Qi, J.; et al. Identification of a novel, small, conserved hypothetical protein involved in Brucella abortus virulence by modifying the expression of multiple genes. Transbound. Emerg. Dis. 2019, 66, 349–362. [Google Scholar] [CrossRef]
- Han, W.; Wei, D.; Sun, Z.; Qu, D. Investigating the mechanism of rough phenotype in a naturally attenuated Brucella strain: Insights from whole genome sequencing. Front. Med. 2024, 11, 1363785. [Google Scholar] [CrossRef]
- Cheng, Z.; Li, Z.; Yin, Y.; Lian, Z.; Abdelgawad, H.A.; Hu, H.; Guan, X.; Zuo, D.; Cai, Y.; Ding, C.; et al. Characteristics of Brucella abortus vaccine strain A19 reveals its potential mechanism of attenuated virulence. Vet. Microbiol. 2021, 254, 109007. [Google Scholar] [CrossRef]
- Li, P.; Tian, M.; Bao, Y.; Hu, H.; Liu, J.; Yin, Y.; Ding, C.; Wang, S.; Yu, S. Brucella Rough Mutant Induce Macrophage Death via Activating IRE1α Pathway of Endoplasmic Reticulum Stress by Enhanced T4SS Secretion. Front. Cell Infect. Microbiol. 2017, 7, 422. [Google Scholar] [CrossRef]
- Sun, P.; Yang, X.; Liu, J.; Bao, Y.; Qi, J.; Han, X.; Liu, G.; Wang, S.; Tian, M. Development and Application of Colloidal Gold Test Strips for the Rapid Detection of Canine Brucellosis. Biosensors 2024, 14, 388. [Google Scholar] [CrossRef]
- Feng, Y.; Peng, X.; Jiang, H.; Peng, Y.; Zhu, L.; Ding, J. Rough Brucella strain RM57 is attenuated and confers protection against Brucella melitensis. Microb. Pathog. 2017, 107, 270–275. [Google Scholar] [CrossRef]
- Zhang, M.; Han, X.; Liu, H.; Tian, M.; Ding, C.; Song, J.; Sun, X.; Liu, Z.; Yu, S. Inactivation of the ABC transporter ATPase gene in Brucella abortus strain 2308 attenuated the virulence of the bacteria. Vet. Microbiol. 2013, 164, 322–329. [Google Scholar] [CrossRef] [PubMed]
- Pei, J.; Ficht, T.A. Brucella abortus Rough Mutants Are Cytopathic for Macrophages in Culture. Infect. Immun. 2004, 72, 440–450. [Google Scholar] [CrossRef]
- Nandini, P.; Jakka, P.; Murugan, S.; Mazumdar, V.; Kumar, D.; Prakash, R.; Barbuddhe, S.B.; Radhakrishnan, G. Immuno-profiling of Brucella proteins for developing improved vaccines and DIVA capable serodiagnostic assays for brucellosis. Front. Microbiol. 2023, 14, 1253349. [Google Scholar] [CrossRef] [PubMed]
- Lapaque, N.; Moriyon, I.; Moreno, E.; Gorvel, J.P. Brucella lipopolysaccharide acts as a virulence factor. Curr. Opin. Microbiol. 2005, 8, 60–66. [Google Scholar] [CrossRef]
- Turse, J.E.; Pei, J.; Ficht, T.A. Lipopolysaccharide-Deficient Brucella Variants Arise Spontaneously during Infection. Front. Microbiol. 2011, 2, 54. [Google Scholar] [CrossRef] [PubMed]
- Stevens, M.G.; Hennager, S.G.; Olsen, S.C.; Cheville, N.F. Serologic responses in diagnostic tests for brucellosis in cattle vaccinated with Brucella abortus 19 or RB51. J. Clin. Microbiol. 1994, 32, 1065–1066. [Google Scholar] [CrossRef] [PubMed]
- Pei, J.; Turse, J.E.; Ficht, T.A. Evidence of Brucella abortus OPS dictating uptake and restricting NF-kappaB activation in murine macrophages. Microbes Infect. 2008, 10, 582–590. [Google Scholar] [CrossRef] [PubMed]
- Porte, F.; Naroeni, A.; Ouahrani-Bettache, S.; Liautard, J.P. Role of the Brucella suis Lipopolysaccharide O Antigen in Phagosomal Genesis and in Inhibition of Phagosome-Lysosome Fusion in Murine Macrophages. Infect. Immun. 2003, 71, 1481–1490. [Google Scholar] [CrossRef] [PubMed]
- Masjedian Jezi, F.; Razavi, S.; Mirnejad, R.; Zamani, K. Immunogenic and protective antigens of Brucella as vaccine candidates. Comp. Immunol. Microbiol. Infect. Dis. 2019, 65, 29–36. [Google Scholar] [CrossRef]
- Stevens, T.L.; Bossie, A.; Sanders, V.M.; Fernandez-Botran, R.; Coffman, R.L.; Mosmann, T.R.; Vitetta, E.S. Regulation of antibody isotype secretion by subsets of antigen-specific helper T cells. Nature 1988, 334, 255–258. [Google Scholar] [CrossRef]
- Vemulapalli, R.; He, Y.; Sriranganathan, N.; Boyle, S.M.; Schurig, G.G. Brucella abortus RB51: Enhancing vaccine efficacy and developing multivalent vaccines. Vet. Microbiol. 2002, 90, 521–532. [Google Scholar] [CrossRef]
- Jindan, R.A.; Saleem, N.; Shafi, A.; Amjad, S.M. Clinical Interpretation of Detection of IgM Anti-Brucella Antibody in the Absence of IgG and Vice Versa; a Diagnostic Challenge for Clinicians. Pol. J. Microbiol. 2019, 68, 51–57. [Google Scholar] [CrossRef]
- Vemulapalli, R.; He, Y.; Buccolo, L.S.; Boyle, S.M.; Sriranganathan, N.; Schurig, G.G. Complementation of Brucella abortus RB51 with a functional wboA gene results in O-antigen synthesis and enhanced vaccine efficacy but no change in rough phenotype and attenuation. Infect. Immun. 2000, 68, 3927–3932. [Google Scholar] [CrossRef]
- Dorneles, E.M.; Sriranganathan, N.; Lage, A.P. Recent advances in Brucella abortus vaccines. Vet. Res. 2015, 46, 76. [Google Scholar] [CrossRef] [PubMed]
- Blasco, J.M.; Moreno, E.; Munoz, P.M.; Conde-Alvarez, R.; Moriyon, I. A review of three decades of use of the cattle brucellosis rough vaccine Brucella abortus RB51: Myths and facts. BMC Vet. Res. 2023, 19, 211. [Google Scholar] [CrossRef] [PubMed]






| Names | Description | Source |
|---|---|---|
| Bacterial strains | ||
| M5 | B. melitensis parental strain; low virulence; smooth phenotype | CVCC |
| M5–90Δ26 | B. melitensis vaccine strain; smooth phenotype | CVCC |
| G7 | gntR7 deletion mutant derived from M5; rough phenotype | This study |
| G8 | gntR8 deletion mutant derived from M5; rough phenotype | This study |
| G16 | gntR16 deletion mutant derived from M5; semi-rough phenotype | This study |
| E. coli DH5α | F−, φ80dlacZ ΔM15, Δ (lacZYA-argF) U169, recA1, endA1, hsdR17 (rk−, mk+), phoA, supE44, thi−1, gyrA96, relA1, λ− | TIANGEN |
| Plasmids | ||
| pKB | pUC19-derived suicide plasmid containing sacB gene; KanR; | [12] |
| pKB-ΔgntR7 | pKB containing the upstream and downstream fragments of the gntR7 gene | This study |
| pKB-ΔgntR8 | pKB containing the upstream and downstream fragments of the gntR8 gene | This study |
| pKB-ΔgntR16 | pKB containing the upstream and downstream fragments of the gntR16 gene | This study |
| Primers | Sequence (5′-3′) | Function |
|---|---|---|
| GntR7-UF | GGTACCCGGGGATCCGCGGCATTGGGGCTGAAGCG | PCR amplification of the homologous fragments of the gntR7 gene |
| GntR7-UR | TGACGGGTTTTGCTAGTCATTCCTCCTCGACTTCA | |
| GntR7-DF | TCGAGGAGGAATGACTAGCAAAACCCGTCAGGCCG | |
| GntR7-DR | TGCCTGCAGGTCGACAGAGCGCGGTCAAGGTGGCG | |
| inG7-F | GCCTGAAGAAATTGCTCGAC | PCR identification of the G7 strain |
| inG7-R | GCGCGTTTGATCTGCTTCAG | |
| outG7-F | GTCTGGTTGACTTGTTTGAC | |
| outG7-R | TGGCTGATCGGGCTTATCTC | |
| GntR8-UF | GGTACCCGGGGATCCAGGCCGCAAGCTCCGCCTCG | PCR amplification of the homologous fragments of the gntR8 gene |
| GntR8-UR | AGTACCGAAAATGTTGCTGCTTCTTGCTTTGTGAC | |
| GntR8-DF | AAAGCAAGAAGCAGCAACATTTTCGGTACTGGCCA | |
| GntR8-DR | TGCCTGCAGGTCGACCACTGGAATCGCGTCAGGTG | |
| inG8-F | GTTAAAGCGCACGAAACATC | PCR identification of the G8 strain |
| inG8-R | GCTTCGAGCCTCTCGTAATC | |
| outG8-F | CGTGTGGAATGTCTATCGAT | |
| outG8-R | GATGTGCGTGAAGATCTGCT | |
| GntR16-UF | GGTACCCGGGGATCCACCCAGCCCCTGAATAATGC | PCR amplification of the homologous fragments of the gntR16 gene |
| GntR16-UR | AAAGTGGCACGAAGGCAATAGGAAAGCCTCCCAAC | |
| GntR16-DF | GAGGCTTTCCTATTGCCTTCGTGCCACTTTTACGC | |
| GntR16-DR | TGCCTGCAGGTCGACCAAGGCTGCGGCCCAGAATC | |
| inG16-F | GATTTATGCGGGCGATTATG | PCR identification of the G16 strain |
| inG16-R | ATCACCGCCATGTGAAAATC | |
| outG16-F | GTAGATATTCCGGTCGTTTT | |
| outG16-R | CCCCATCTTATTTTCTTGCG | |
| RT-IL1B-F | TGGACCTTCCAGGATGAGGACA | qPCR for the IL−1β gene |
| RT-IL1B-R | GTTCATCTCGGAGCCTGTAGTG | |
| RT-IL6-F | TACCACTTCACAAGTCGGAGGC | qPCR for the IL−6 gene |
| RT-IL6-R | CTGCAAGTGCATCATCGTTGTTC | |
| RT-MCP1-F | GCTACAAGAGGATCACCAGCAG | qPCR for the MCP1 gene |
| RT-MCP1-R | GTCTGGACCCATTCCTTCTTGG | |
| RT-MIP1B-F | ACCCTCCCACTTCCTGCTGTTT | qPCR for the MIP1β gene |
| RT-MIP1B-R | CTGTCTGCCTCTTTTGGTCAGG | |
| RT-iNOS-F | GAGACAGGGAAGTCTGAAGCAC | qPCR for the iNOS gene |
| RT-iNOS-R | CCAGCAGTAGTTGCTCCTCTTC | |
| RT-ActB-F | CATTGCTGACAGGATGCAGAAGG | qPCR for the β-actin gene |
| RT-ActB-R | TGCTGGAAGGTGGACAGTGAGG |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, J.; Yin, Y.; Yang, X.; Li, M.; Qu, J.; Wang, S.; Bao, Y.; Qi, J.; Wu, T.; Tian, M. Biological Characterization and DIVA Potential of Three Rough Brucella melitensis Vaccine Strains. Vaccines 2025, 13, 857. https://doi.org/10.3390/vaccines13080857
Liu J, Yin Y, Yang X, Li M, Qu J, Wang S, Bao Y, Qi J, Wu T, Tian M. Biological Characterization and DIVA Potential of Three Rough Brucella melitensis Vaccine Strains. Vaccines. 2025; 13(8):857. https://doi.org/10.3390/vaccines13080857
Chicago/Turabian StyleLiu, Jinyue, Yi Yin, Xinmei Yang, Mengsi Li, Jing Qu, Shaohui Wang, Yanqing Bao, Jingjing Qi, Tonglei Wu, and Mingxing Tian. 2025. "Biological Characterization and DIVA Potential of Three Rough Brucella melitensis Vaccine Strains" Vaccines 13, no. 8: 857. https://doi.org/10.3390/vaccines13080857
APA StyleLiu, J., Yin, Y., Yang, X., Li, M., Qu, J., Wang, S., Bao, Y., Qi, J., Wu, T., & Tian, M. (2025). Biological Characterization and DIVA Potential of Three Rough Brucella melitensis Vaccine Strains. Vaccines, 13(8), 857. https://doi.org/10.3390/vaccines13080857








