Microbiome–Immune Interaction and Harnessing for Next-Generation Vaccines Against Highly Pathogenic Avian Influenza in Poultry
Abstract
1. Introduction: The Global HPAI Crisis and Microbiome–Immune Interplay
2. Microbiome–Immune Crosstalk: Implications for HPAI Vaccinology
2.1. Cross-Species Microbiome–Immune Lessons
2.2. Gut Microbiota as Immunomodulators in Poultry
2.3. Synthesis and Forward Vision
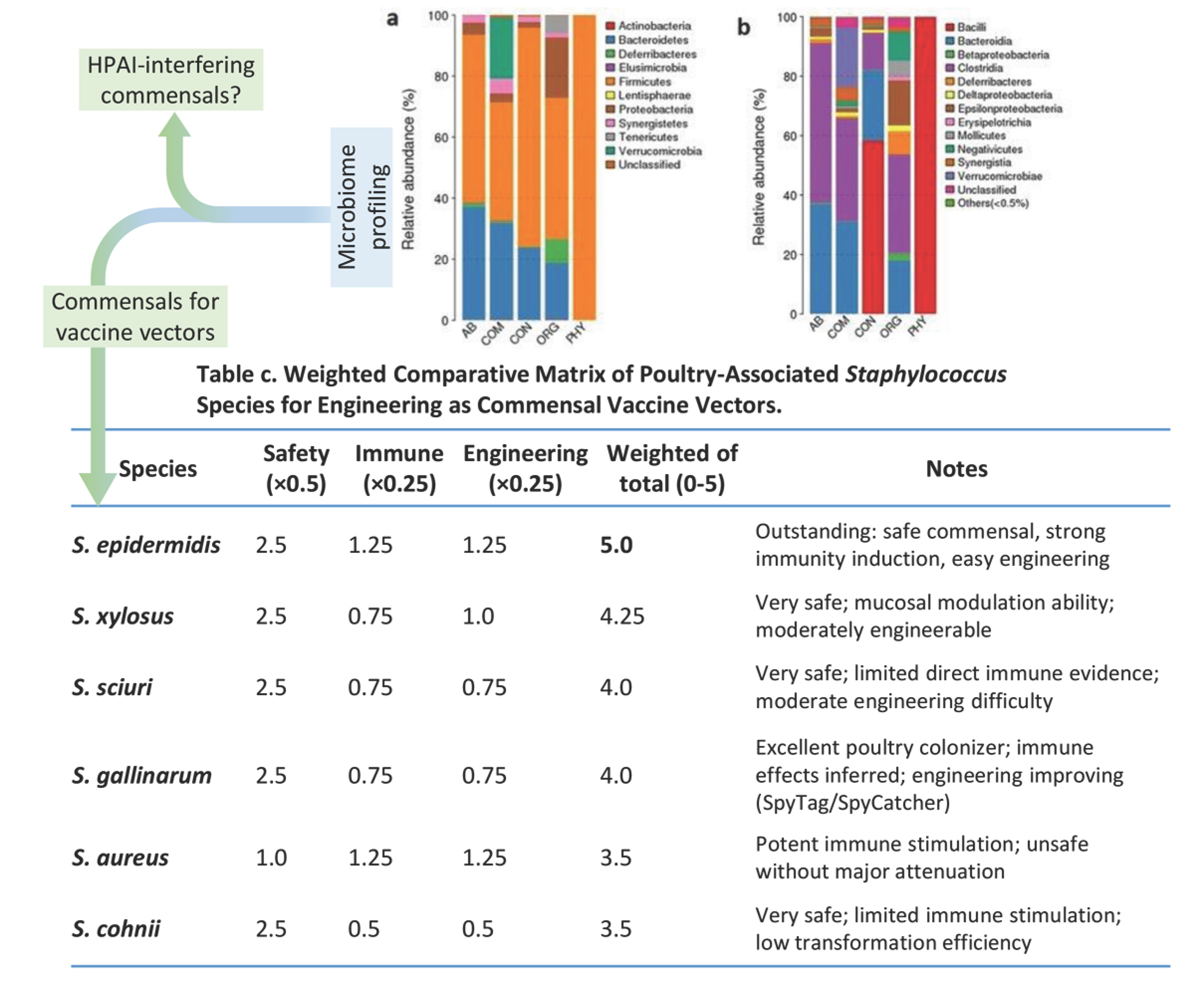
3. Commensal Bacteria as Novel Vaccine Vectors: Emerging Platforms for HPAI Control
3.1. Engineered Probiotic or Commensal Vectors
3.2. Microbiome-Targeted Adjuvants: Synbiotics and Postbiotics
3.3. Challenges and Translational Considerations
4. AI-Driven Microbiome Engineering for Vaccine Refinement and Viral Surveillance
5. Future Perspectives and One Health Integration
Author Contributions
Funding
Conflicts of Interest
References
- Niu, Q.; Jiang, Z.; Wang, L.; Ji, X.; Baele, G.; Qin, Y.; Lin, L.; Lai, A.; Chen, Y.; Veit, M.; et al. Prevention and control of avian influenza virus: Recent advances in diagnostic technologies and surveillance strategies. Nat. Commun. 2025, 16, 3558. [Google Scholar] [CrossRef]
- Xie, R.; Edwards, K.M.; Wille, M.; Wei, X.; Wong, S.S.; Zanin, M.; El-Shesheny, R.; Ducatez, M.; Poon, L.L.M.; Kayali, G.; et al. The episodic resurgence of highly pathogenic avian influenza H5 virus. Nature 2023, 622, 810–817. [Google Scholar] [CrossRef] [PubMed]
- Kovács, L.; Farkas, M.; Dobra, P.F.; Lennon, G.; Könyves, L.P.; Rusvai, M. Avian Influenza Clade 2.3.4.4b: Global Impact and Summary Analysis of Vaccine Trials. Vaccines 2025, 13, 453. [Google Scholar] [CrossRef]
- Webby, R.J.; Uyeki, T.M. An Update on Highly Pathogenic Avian Influenza A(H5N1) Virus, Clade 2.3.4.4b. J. Infect Dis. 2024, 230, 533–542. [Google Scholar] [CrossRef] [PubMed]
- Xie, Z.; Yang, J.; Jiao, W.; Li, X.; Iqbal, M.; Liao, M.; Dai, M. 2025. Clade 2.3.4.4b highly pathogenic avian influenza H5N1 viruses: Knowns, unknowns, and challenges. J. Virol. 2025, 99, e0042425. [Google Scholar] [CrossRef] [PubMed]
- Sacristán, C.; Ewbank, A.C.; Ibáñez Porras, P.; Pérez-Ramírez, E.; de la Torre, A.; Briones, V.; Iglesias, I. Novel Epidemiologic Features of High Pathogenicity Avian Influenza Virus A H5N1 2.3.3.4b Panzootic: A Review. Transbound. Emerg. Dis. 2024, 5322378. [Google Scholar] [CrossRef]
- Piesche, R.; Cazaban, C.; Frizzo da Silva, L.; Ramírez-Martínez, L.; Hufen, H.; Beer, M.; Harder, T.; Grund, C. Immunogenicity and Protective Efficacy of Five Vaccines Against Highly Pathogenic Avian Influenza Virus H5N1, Clade 2.3.4.4b, in Fattening Geese. Vaccines 2025, 13, 399. [Google Scholar] [CrossRef] [PubMed]
- Sajjadi, N.C.; Abolnik, C.; Baldinelli, F.; Brown, I.; Cameron, A.; de Wit, S.; Dhingra, M.; Espeisse, O.; Guerin, J.-L.; Harder, T.; et al. Vaccination and surveillance for high pathogenicity avian influenza in poultry-current situation and perspectives. Biologicals 2025, 91, 101840. [Google Scholar] [CrossRef]
- Sheta, B.; Waheed, O.; Ayad, E.; Habbak, L.; Hyder, A. Constitutive immunity is influenced by avian influenza virus-induced modification of gut microbiota in Eurasian teal (Anas crecca). Comp. Biochem. Physiol. C Toxicol. Pharmacol. 2024, 278, 109867. [Google Scholar] [CrossRef]
- Alwin, A.; Karst, S.M. The influence of microbiota-derived metabolites on viral infections. Curr. Opin. Virol. 2021, 49, 151–156. [Google Scholar] [CrossRef]
- Abd El-Hack, M.E.; El-Saadony, M.T.; Alqhtani, A.H.; Swelum, A.A.; Salem, H.M.; Elbestawy, A.R.; Noreldin, A.E.; Babalghith, A.O.; Khafaga, A.F.; Hassan, M.I.; et al. The relationship among avian influenza, gut microbiota and chicken immunity: An updated overview. Poult. Sci. 2022, 101, 102021. [Google Scholar] [CrossRef]
- Feng, Y.; de Jong, S.E.; Oliveira, A.P.B.N.; Samaha, H.; Yang, F.; Hu, M.; Wang, Y.; Beydoun, N.; Xie, X.; Zhang, H.; et al. Antibiotic-induced gut microbiome perturbation alters the immune responses to the rabies vaccine. Cell Host Microbe. 2025, 33, 705–718.e5. [Google Scholar] [CrossRef]
- Alqazlan, N.; Astill, J.; Raj, S.; Sharif, S. Strategies for enhancing immunity against avian influenza virus in chickens: A review. Avian Pathol. 2022, 51, 211–235. [Google Scholar] [CrossRef]
- Raj, S.; Alizadeh, M.; Shoojadoost, B.; Hodgins, D.; Nagy, É.; Mubareka, S.; Karimi, K.; Behboudi, S.; Sharif, S. Determining the Protective Efficacy of Toll-Like Receptor Ligands to Minimize H9N2 Avian Influenza Virus Transmission in Chickens. Viruses 2023, 15, 238. [Google Scholar] [CrossRef]
- Plaza, P.I.; Gamarra-Toledo, V.; Euguí, J.R.; Lambertucci, S.A. Recent Changes in Patterns of Mammal Infection with Highly Pathogenic Avian Influenza A(H5N1) Virus Worldwide. Emerg. Infect Dis. 2024, 30, 444–452. [Google Scholar] [CrossRef] [PubMed]
- Gilbertson, B.; Subbarao, K. Mammalian infections with highly pathogenic avian influenza viruses renew concerns of pandemic potential. J. Exp. Med. 2023, 220, e20230447. [Google Scholar] [CrossRef]
- Peacock, T.P.; Moncla, L.; Dudas, G.; VanInsberghe, D.; Sukhova, K.; Lloyd-Smith, J.O.; Worobey, M.; Lowen, A.C.; Nelson, M.I. The global H5N1 influenza panzootic in mammals. Nature 2025, 637, 304–313. [Google Scholar] [CrossRef] [PubMed]
- Zheng, D.; Liwinski, T.; Elinav, E. Interaction between microbiota and immunity in health and disease. Cell Res. 2020, 30, 492–506. [Google Scholar] [CrossRef]
- Li, K.; Ly, K.; Mehta, S.; Braithwaite, A. Importance of crosstalk between the microbiota and the neuroimmune system for tissue homeostasis. Clin. Transl. Immunol. 2022, 11, e1394. [Google Scholar] [CrossRef]
- Ngo, V.L.; Wang, Y.; Wang, Y.; Shi, Z.; Britton, R.; Zou, J.; Ramani, S.; Jiang, B.; Gewirtz, A.T. Select Gut Microbiota Impede Rotavirus Vaccine Efficacy. Cell Mol. Gastroenterol. Hepatol. 2024, 18, 101393. [Google Scholar] [CrossRef] [PubMed]
- Song, L.; Huang, Y.; Liu, G.; Li, X.; Xiao, Y.; Liu, C.; Zhang, Y.; Li, J.; Xu, J.; Lu, S.; et al. A Novel Immunobiotics Bacteroides dorei Ameliorates Influenza Virus Infection in Mice. Front. Immunol. 2022, 12, 828887. [Google Scholar] [CrossRef] [PubMed]
- Oh, J.Z.; Ravindran, R.; Chassaing, B.; Carvalho, F.A.; Maddur, M.S.; Bower, M.; Hakimpour, P.; Gill, K.P.; Nakaya, H.I.; Yarovinsky, F.; et al. TLR5-mediated sensing of gut microbiota is necessary for antibody responses to seasonal influenza vaccination. Immunity 2014, 41, 478–492. [Google Scholar] [CrossRef]
- Dasgupta, S.; Erturk-Hasdemir, D.; Ochoa-Reparaz, J.; Reinecker, H.C.; Kasper, D.L. Plasmacytoid dendritic cells mediate anti-inflammatory responses to a gut commensal molecule via both innate and adaptive mechanisms. Cell Host Microbe. 2014, 15, 413–423. [Google Scholar] [CrossRef]
- Ramakrishna, C.; Kujawski, M.; Chu, H.; Li, L.; Mazmanian, S.K.; Cantin, E.M. Bacteroides fragilis polysaccharide A induces IL-10 secreting B and T cells that prevent viral encephalitis. Nat. Commun. 2019, 10, 2153. [Google Scholar] [CrossRef]
- Chauhan, A.; Kumar, R.; Sharma, S.; Mahanta, M.; Vayuuru, S.K.; Nayak, B.; Kumar, S.; Shalimar. Fecal Microbiota Transplantation in Hepatitis B e Antigen-Positive Chronic Hepatitis B Patients: A Pilot Study. Dig. Dis. Sci. 2021, 66, 873–880. [Google Scholar] [CrossRef]
- Liu, Y.; Zhou, J.; Yang, Y.; Chen, X.; Chen, L.; Wu, Y. Intestinal Microbiota and Its Effect on Vaccine-Induced Immune Amplification and Tolerance. Vaccines 2024, 12, 868. [Google Scholar] [CrossRef]
- Hagan, T.; Cortese, M.; Rouphael, N.; Boudreau, C.; Linde, C.; Maddur, M.S.; Das, J.; Wang, H.; Guthmiller, J.; Zheng, N.Y.; et al. Antibiotics-Driven Gut Microbiome Perturbation Alters Immunity to Vaccines in Humans. Cell 2019, 178, 1313–1328.e13. [Google Scholar] [CrossRef]
- Garcia-Vello, P.; Tytgat, H.L.P.; Elzinga, J.; Van Hul, M.; Plovier, H.; Tiemblo-Martin, M.; Cani, P.D.; Nicolardi, S.; Fragai, M.; De Castro, C.; et al. The lipooligosaccharide of the gut symbiont Akkermansia muciniphila exhibits a remarkable structure and TLR signaling capacity. Nat. Commun. 2024, 15, 8411. [Google Scholar] [CrossRef]
- Ryan, F.J.; Clarke, M.; Lynn, M.A.; Benson, S.C.; McAlister, S.; Giles, L.C.; Choo, J.M.; Rossouw, C.; Ng, Y.Y.; Semchenko, E.A.; et al. Bifidobacteria support optimal infant vaccine responses. Nature 2025, 641, 456–464. [Google Scholar] [CrossRef] [PubMed]
- Wagner, J.; Handley, A.; Donato, C.M.; Lyons, E.A.; Pavlic, D.; Ong, D.S.; Bonnici, R.; Bogdanovic-Sakran, N.; Parker, E.P.K.; Bronowski, C.; et al. Early-life gut microbiome associates with positive vaccine take and shedding in neonatal schedule of the human neonatal rotavirus vaccine RV3-BB. Nat. Commun. 2025, 16, 3432. [Google Scholar] [CrossRef] [PubMed]
- Jordan, A.; Carding, S.R.; Hall, L.J. The early-life gut microbiome and vaccine efficacy. Lancet Microbe. 2022, 3, e787–e794. [Google Scholar] [CrossRef] [PubMed]
- Palinauskas, V.; Mateos-Hernandez, L.; Wu-Chuang, A.; de la Fuente, J.; Aželytė, J.; Obregon, D.; Cabezas-Cruz, A. Exploring the Ecological Implications of Microbiota Diversity in Birds: Natural Barriers Against Avian Malaria. Front. Immunol. 2022, 13, 807682. [Google Scholar] [CrossRef]
- Yilmaz, B.; Portugal, S.; Tran, T.M.; Gozzelino, R.; Ramos, S.; Gomes, J.; Regalado, A.; Cowan, P.J.; d’Apice, A.J.; Chong, A.S.; et al. Gut microbiota elicits a protective immune response against malaria transmission. Cell 2014, 159, 1277–1289. [Google Scholar] [CrossRef] [PubMed]
- Cao, J.; Hu, Y.; Liu, F.; Wang, Y.; Bi, Y.; Lv, N.; Li, J.; Zhu, B.; Gao, G.F. Metagenomic analysis reveals the microbiome and resistome in migratory birds. Microbiome 2020, 8, 26. [Google Scholar] [CrossRef] [PubMed]
- Gul, S.; Shi, Y.; Hu, J.; Song, S. The Influence of Microbiota on Wild Birds’ Parental Coprophagy Behavior: Current Advances and Future Research Directions. Microorganisms 2024, 12, 2468. [Google Scholar] [CrossRef]
- Abaidullah, M.; Peng, S.; Kamran, M.; Song, X.; Yin, Z. Current Findings on Gut Microbiota Mediated Immune Modulation against Viral Diseases in Chicken. Viruses 2019, 11, 681. [Google Scholar] [CrossRef]
- Alavi, S.; Mitchell, J.D.; Cho, J.Y.; Liu, R.; Macbeth, J.C.; Hsiao, A. Interpersonal Gut Microbiome Variation Drives Susceptibility and Resistance to Cholera Infection. Cell 2020, 181, 1533–1546.e13. [Google Scholar] [CrossRef]
- Jin, W.B.; Xiao, L.; Jeong, M.; Han, S.J.; Zhang, W.; Yano, H.; Shi, H.; Arifuzzaman, M.; Lyu, M.; Wang, D.; et al. Microbiota-derived bile acids antagonize the host androgen receptor and drive anti-tumor immunity. Cell 2025, 188, 2336–2353.e38. [Google Scholar] [CrossRef]
- Ullah, H.; Arbab, S.; Tian, Y.; Chen, Y.; Liu, C.Q.; Li, Q.; Li, K. Crosstalk between gut microbiota and host immune system and its response to traumatic injury. Front. Immunol. 2024, 15, 1413485. [Google Scholar] [CrossRef]
- Paradowska, M.; Dunislawska, A.; Siwek, M.; Slawinska, A. Avian Cell Culture Models to Study Immunomodulatory Properties of Bioactive Products. Animals 2022, 12, 670. [Google Scholar] [CrossRef]
- Idowu, P.A.; Mpofu, T.J.; Magoro, A.M.; Modiba, M.C.; Nephawe, K.A.; Mtileni, B. Impact of probiotics on chicken gut microbiota, immunity, behavior, and productive performance—A systematic review. Front. Anim. Sci. 2025, 6, 1562527. [Google Scholar] [CrossRef]
- Sultan, A.; Murtaza, S.; Naz, S.; Islam, Z.; Alrefaei, A.F.; Khan, R.U.; HAbdelrahman, S.; Chandrasekaran, A. Live performance, nutrient digestibility, immune response and fecal microbial load modulation in Japanese quails fed a Bacillus-based probiotic alone or combination with xylanase. Vet. Q. 2024, 44, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Stanley, D.; Hughes, R.J.; Moore, R.J. Microbiota of the chicken gastrointestinal tract. Appl. Microbiol. Biotechnol. 2014, 98, 4301–4310. [Google Scholar] [CrossRef] [PubMed]
- Waite, D.W.; Taylor, M.W. Characterizing the avian gut microbiota: Membership, driving influences, and potential function. Front. Microbiol. 2014, 5, 223. [Google Scholar] [CrossRef]
- Pantin-Jackwood, M.J.; Swayne, D.E. Pathogenesis and pathobiology of avian influenza virus infection in birds. Rev. Sci. Tech. 2009, 28, 113–136. [Google Scholar] [CrossRef] [PubMed]
- Brisbin, J.T.; Gong, J.; Sharif, S. Interactions between commensal bacteria and the gut-associated immune system of the chicken. Anim. Health Res. Rev. 2008, 9, 101–110. [Google Scholar] [CrossRef]
- Crhanova, M.; Hradecka, H.; Faldynova, M.; Matulova, M.; Havlickova, H.; Sisak, F.; Rychlik, I. Immune response of chicken gut to natural colonization by gut microflora. Infect. Immun. 2011, 79, 2755–2763. [Google Scholar] [CrossRef]
- Wang, W.C.; Sayedahmed, E.E.; Sambhara, S.; Mittal, S.K. Progress towards the Development of a Universal Influenza Vaccine. Viruses 2022, 14, 1684. [Google Scholar] [CrossRef]
- Lloren, K.K.S.; Senevirathne, A.; Lee, J.H. Advancing vaccine technology through the manipulation of pathogenic and commensal bacteria. Mater. Today Bio 2024, 29, 101349. [Google Scholar] [CrossRef]
- Xu, C.; Aqib, A.I.; Fatima, M.; Muneer, S.; Zaheer, T.; Peng, S.; Ibrahim, E.H.; Li, K. Deciphering the Potential of Probiotics in Vaccines. Vaccines 2024, 12, 711. [Google Scholar] [CrossRef]
- LeCureux, J.S.; Dean, G.A. Lactobacillus Mucosal Vaccine Vectors: Immune Responses against Bacterial and Viral Antigens. mSphere 2018, 3, e00061-18. [Google Scholar] [CrossRef]
- Wang, Z.S.; Yu, Q.H.; Gao, J.K.; Yang, Q. Mucosal and systemic immune responses induced by recombinant Lactobacillus spp. expressing the hemagglutinin of the avian influenza virus H5N1. Clin. Vaccine Immunol. 2012, 19, 174–179. [Google Scholar] [CrossRef] [PubMed]
- Shi, S.H.; Yang, W.T.; Yang, G.L.; Cong, Y.L.; Huang, H.B.; Wang, Q.; Cai, R.P.; Ye, L.P.; Hu, J.T.; Zhou, J.Y.; et al. Immunoprotection against influenza virus H9N2 by the oral administration of recombinant Lactobacillus plantarumNC8 expressing hemagglutinin in BALB/c mice. Virology 2014, 464–465, 166–176. [Google Scholar] [CrossRef] [PubMed]
- Shi, S.H.; Yang, W.T.; Yang, G.L.; Zhang, X.K.; Liu, Y.Y.; Zhang, L.J.; Ye, L.P.; Hu, J.T.; Xing, X.; Qi, C.; et al. Lactobacillus plantarum vaccine vector expressing hemagglutinin provides protection against H9N2 challenge infection. Virus Res. 2016, 211, 46–57. [Google Scholar] [CrossRef] [PubMed]
- Levit, R.; Cortes-Perez, N.G.; de Moreno de Leblanc, A.; Loiseau, J.; Aucouturier, A.; Langella, P.; LeBlanc, J.G.; Bermúdez-Humarán, L.G. Use of genetically modified lactic acid bacteria and bifidobacteria as live delivery vectors for human and animal health. Gut Microbes. 2022, 14, 2110821. [Google Scholar] [CrossRef]
- Wang, Z.; Yu, Q.; Fu, J.; Liang, J.; Yang, Q. Immune responses of chickens inoculated with recombinant Lactobacillus expressing the haemagglutinin of the avian influenza virus. J. Appl. Microbiol. 2013, 115, 1269–1277. [Google Scholar] [CrossRef]
- Yang, W.T.; Shi, S.H.; Yang, G.L.; Jiang, Y.L.; Zhao, L.; Li, Y.; Wang, C.F. Cross-protective efficacy of dendritic cells targeting conserved influenza virus antigen expressed by Lactobacillus plantarum. Sci. Rep. 2016, 6, 39665. [Google Scholar] [CrossRef]
- Tan, T.S.; Syed Hassan, S.; Yap, W.B. Expression of surface-bound nonstructural 1 (NS1) protein of influenza virus A H5N1 on Lactobacillus casei strain C1. Lett. Appl. Microbiol. 2017, 64, 446–451. [Google Scholar] [CrossRef]
- Zhang, R.; Xu, T.; Li, Z.; Li, L.; Li, C.; Li, X.; Wang, Z.; Wang, S.; Wang, X.; Zhang, H. Vaccination with recombinant Lactococcus lactis expressing HA1-IgY Fc fusion protein provides protective mucosal immunity against H9N2 avian influenza virus in chickens. Virol. J. 2023, 20, 76. [Google Scholar] [CrossRef]
- Ogbuewu, I.P.; Mabelebele, M.; Sebola, N.A.; Mbajiorgu, C. Bacillus Probiotics as Alternatives to In-feed Antibiotics and Its Influence on Growth, Serum Chemistry, Antioxidant Status, Intestinal Histomorphology, and Lesion Scores in Disease-Challenged Broiler Chickens. Front. Vet. Sci. 2022, 9, 876725. [Google Scholar] [CrossRef]
- Mou, C.; Zhu, L.; Yang, J.; Xu, W.; Cheng, X.; Yang, Q. Immune Responses Induced by Recombinant Bacillus Subtilis Expressing the Hemagglutinin Protein of H5N1 in chickens. Sci. Rep. 2016, 6, 38403. [Google Scholar] [CrossRef]
- Rudometova, N.B.; Fando, A.A.; Kisakova, L.A.; Kisakov, D.N.; Borgoyakova, M.B.; Litvinova, V.R.; Yakovlev, V.A.; Tigeeva, E.V.; Vahitov, D.I.; Sharabrin, S.V.; et al. Immunogenic and Protective Properties of Recombinant Hemagglutinin of Influenza A (H5N8) Virus. Vaccines 2024, 12, 143. [Google Scholar] [CrossRef]
- Lv, P.; Zhang, X.; Song, M.; Hao, G.; Wang, F.; Sun, S. Oral administration of recombinant Bacillus subtilis expressing a multi-epitope protein induces strong immune responses against Salmonella Enteritidis. Vet. Microbiol. 2023, 276, 109632. [Google Scholar] [CrossRef] [PubMed]
- EFSA Panel on Additives and Products or Substances used in Animal Feed (FEEDAP); Rychen, G.; Aquilina, G.; Azimonti, G.; Bampidis, V.; Bastos, M.L.; Bories, G.; Chesson, A.; Cocconcelli, P.S.; Flachowsky, G.; et al. Safety and efficacy of Alterion NE® (Bacillus subtilis DSM 29784) as a feed additive for chickens for fattening and chickens reared for laying. EFSA J. 2017, 15, e04933. [Google Scholar] [CrossRef]
- Gribonika, I.; Band, V.I.; Chi, L.; Perez-Chaparro, P.J.; Link, V.M.; Ansaldo, E.; Oguz, C.; Bousbaine, D.; Fischbach, M.A.; Belkaid, Y. Skin autonomous antibody production regulates host-microbiota interactions. Nature 2025, 638, 1043–1053. [Google Scholar] [CrossRef] [PubMed]
- Bousbaine, D.; Bauman, K.D.; Chen, Y.E.; Lalgudi, P.V.; Nguyen, T.T.D.; Swenson, J.M.; Yu, V.K.; Tsang, E.; Conlan, S.; Li, D.B.; et al. Discovery and engineering of the antibody response to a prominent skin commensal. Nature 2025, 638, 1054–1064. [Google Scholar] [CrossRef] [PubMed]
- EFSA Panel on Animal Health and Animal Welfare (AHAW); European Union Reference Laboratory for Avian Influenza; Nielsen, S.S.; Alvarez, J.; Bicout, D.J.; Calistri, P.; Canali, E.; Drewe, J.A.; Garin-Bastuji, B.; Gonzales Rojas, J.L.; et al. Vaccination of poultry against highly pathogenic avian influenza—Part 1. Available vaccines and vaccination strategies. EFSA J. 2023, 21, e08271. [Google Scholar] [CrossRef]
- Ziogas, A.; Novakovic, B.; Ventriglia, L.; Galang, N.; Tran, K.A.; Li, W.; Matzaraki, V.; van Unen, N.; Schlüter, T.; Ferreira, A.V.; et al. Long-term histone lactylation connects metabolic and epigenetic rewiring in innate immune memory. Cell 2025, 188, 2992–3012. [Google Scholar] [CrossRef]
- He, Y.; Fu, L.; Li, Y.; Wang, W.; Gong, M.; Zhang, J.; Dong, X.; Huang, J.; Wang, Q.; Mackay, C.R.; et al. Gut microbial metabolites facilitate anticancer therapy efficacy by modulating cytotoxic CD8+ T cell immunity. Cell Metab. 2021, 33, 988–1000.e7. [Google Scholar] [CrossRef]
- Bodman-Harris, O.; Rollier, C.S.; Iqbal, M. Approaches to Enhance the Potency of Vaccines in Chickens. Vaccines 2024, 12, 1337. [Google Scholar] [CrossRef]
- Cohen, D.; Melamed, S.; Millman, A.; Shulman, G.; Oppenheimer-Shaanan, Y.; Kacen, A.; Doron, S.; Amitai, G.; Sorek, R. Cyclic GMP-AMP signalling protects bacteria against viral infection. Nature 2019, 574, 691–695. [Google Scholar] [CrossRef] [PubMed]
- Luo, J.; Liu, X.; Xiong, F.; Gao, F.; Yi, Y.; Zhang, M.; Chen, Z.; Tan, W. Enhancing Immune Response and Heterosubtypic Protection Ability of Inactivated H7N9 Vaccine by Using STING Agonist as a Mucosal Adjuvant. Front. Immunol. 2019, 10, 2274. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Hong, H.; Wang, J.; Huang, J.; Li, J.; Tao, Y.; Liu, M.; Pang, H.; Li, J.; Bo, R. Mucosal immune responses and protective efficacy elicited by oral administration AMP-ZnONPs-adjuvanted inactivated H9N2 virus in chickens. Poult. Sci. 2024, 103, 103496. [Google Scholar] [CrossRef] [PubMed]
- Khosravi, A.; Boldaji, F.; Dastar, B.; Torshizi, M.A.K.; Alemi, M.; Hoseinifar, S.H. A synbiotic improves performance and gut health in broiler chickens. Sci. Rep. 2025, 15, 19164. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.Z.; Li, F.; Huang, X.; Nouman, M.; Bibi, R.; Fan, X.; Zhou, H.; Shan, Z.; Wang, L.; Jiang, Y.; et al. Oral Immunization of Chickens with Probiotic Lactobacillus crispatus Constitutively Expressing the α-β2-ε-β1 Toxoids to Induce Protective Immunity. Vaccines 2022, 10, 698. [Google Scholar] [CrossRef]
- Dunislawska, A.; Slawinska, A.; Siwek, M. Hepatic DNA Methylation in Response to Early Stimulation of Microbiota with Lactobacillus Synbiotics in Broiler Chickens. Genes 2020, 11, 579. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Torres, L.; Krüger, A.; Csibra, E.; Gianni, E.; Pinheiro, V.B. Synthetic biology approaches to biological containment: Pre-emptively tackling potential risks. Essays Biochem. 2016, 60, 393–410. [Google Scholar] [CrossRef]
- Forti, A.M.; Jones, M.A.; Elbeyli, D.N.; Butler, N.D.; Kunjapur, A.M. Engineered orthogonal and obligate bacterial commensalism mediated by a non-standard amino acid. Nat. Microbiol. 2025, 10, 1404–1416. [Google Scholar] [CrossRef] [PubMed]
- EFSA (European Food Safety Authority). Guidance on the assessment of genetically modified microorganisms and their products intended for food and feed use. EFSA J. 2011, 9, 2193. [Google Scholar] [CrossRef]
- EFSA Panel on Biological Hazards (BIOHAZ); Koutsoumanis, K.; Allende, A.; Alvarez-Ordóñez, A.; Bolton, D.; Bover-Cid, S.; Chemaly, M.; De Cesare, A.; Hilbert, F.; Lindqvist, R.; et al. Update of the list of qualified presumption of safety (QPS) recommended microbiological agents intentionally added to food or feed as notified to EFSA 20: Suitability of taxonomic units notified to EFSA until March 2024. EFSA J. 2024, 22, e8882. [Google Scholar] [CrossRef]
- Maraci, Ö.; Antonatou-Papaioannou, A.; Jünemann, S.; Castillo-Gutiérrez, O.; Busche, T.; Kalinowski, J.; Caspers, B.A. The Gut Microbial Composition Is Species-Specific and Individual-Specific in Two Species of Estrildid Finches, the Bengalese Finch and the Zebra Finch. Front. Microbiol. 2021, 12, 619141. [Google Scholar] [CrossRef] [PubMed]
- Bodawatta, K.H.; Koane, B.; Maiah, G.; Sam, K.; Poulsen, M.; Jønsson, K.A. Species-specific but not phylosymbiotic gut microbiomes of New Guinean passerine birds are shaped by diet and flight-associated gut modifications. Proc. Biol. Sci. 2021, 288, 20210446. [Google Scholar] [CrossRef]
- Qin, C.; Gong, L.; Zhang, X.; Wang, Y.; Wang, Y.; Wang, B.; Li, Y.; Li, W. Effect of Saccharomyces boulardii and Bacillus subtilis B10 on gut microbiota modulation in broilers. Anim. Nutr. 2018, 4, 358–366. [Google Scholar] [CrossRef]
- Liu, Y.; Zhao, D.; Zhang, J.; Huang, X.; Han, K.; Liu, Q.; Yang, J.; Zhang, L.; Li, Y. Development of an Inactivated Avian Influenza Virus Vaccine against Circulating H9N2 in Chickens and Ducks. Vaccines 2023, 11, 596. [Google Scholar] [CrossRef]
- Chen, T.H.; Yang, Y.L.; Jan, J.T.; Chen, C.C.; Wu, S.C. Site-Specific Glycan-Masking/Unmasking Hemagglutinin Antigen Design to Elicit Broadly Neutralizing and Stem-Binding Antibodies Against Highly Pathogenic Avian Influenza H5N1 Virus Infections. Front. Immunol. 2021, 12, 692700. [Google Scholar] [CrossRef]
- Todorov, S.D.; Ivanova, I.V.; Popov, I.; Weeks, R.; Chikindas, M.L. Bacillus spore-forming probiotics: Benefits with concerns? Crit. Rev. Microbiol. 2022, 48, 513–530. [Google Scholar] [CrossRef]
- Li, L.; Yang, L.; Zhang, L.; He, F.; Xia, Z.; Xiang, B. Multi-omic analysis reveals that Bacillus licheniformis enhances pekin ducks growth performance via lipid metabolism regulation. Front. Pharmacol. 2024, 15, 1412231. [Google Scholar] [CrossRef]
- Cargnin Faccin, F.; Perez, D.R. Pandemic preparedness through vaccine development for avian influenza viruses. Hum. Vaccin. Immunother. 2024, 20, 2347019. [Google Scholar] [CrossRef] [PubMed]
- Mohamadzadeh, M.; Pfeiler, E.A.; Brown, J.B.; Zadeh, M.; Gramarossa, M.; Managlia, E.; Bere, P.; Sarraj, B.; Khan, M.W.; Pakanati, K.C.; et al. Regulation of induced colonic inflammation by Lactobacillus acidophilus deficient in lipoteichoic acid. Proc. Natl. Acad. Sci. USA 2011, 108 (Suppl. 1), 4623–4630. [Google Scholar] [CrossRef] [PubMed]
- Swayne, D.E.; Kapczynski, D. Strategies and challenges for eliciting immunity against avian influenza virus in birds. Immunol. Rev. 2008, 225, 314–331. [Google Scholar] [CrossRef] [PubMed]
- Capua, I.; Alexander, D.J. Avian influenza infection in birds: A challenge and opportunity for the poultry veterinarian. Poult. Sci. 2009, 88, 842–846. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Gao, G.F. A brief history of human infections with H5Ny avian influenza viruses. Cell Host Microbe. 2025, 33, 176–181. [Google Scholar] [CrossRef]
- Thadani, N.N.; Gurev, S.; Notin, P.; Youssef, N.; Rollins, N.J.; Ritter, D.; Sander, C.; Gal, Y.; Marks, D.S. Learning from prepandemic data to forecast viral escape. Nature 2023, 622, 818–825. [Google Scholar] [CrossRef]
- Jumper, J.; Evans, R.; Pritzel, A.; Green, T.; Figurnov, M.; Ronneberger, O.; Tunyasuvunakool, K.; Bates, R.; Žídek, A.; Potapenko, A.; et al. Highly accurate protein structure prediction with AlphaFold. Nature 2021, 596, 583–589. [Google Scholar] [CrossRef]
- Notin, P.; Marks, D.S.; Weitzman, R.; Gal, Y. ProteinNPT: Improving Protein Property Prediction and Design with Non-Parametric Transformers. bioRxiv 2023. [Google Scholar] [CrossRef]
- Hayes, T.; Rao, R.; Akin, H.; Sofroniew, N.J.; Oktay, D.; Lin, Z.; Verkuil, R.; Tran, V.Q.; Deaton, J.; Wiggert, M.; et al. Simulating 500 million years of evolution with a language model. Science 2025, 387, 850–858. [Google Scholar] [CrossRef]
- Bukhari, S.N.H.; Jain, A.; Haq, E.; Mehbodniya, A.; Webber, J. Machine Learning Techniques for the Prediction of B-Cell and T-Cell Epitopes as Potential Vaccine Targets with a Specific Focus on SARS-CoV-2 Pathogen: A Review. Pathogens 2022, 11, 146. [Google Scholar] [CrossRef] [PubMed]
- Patronov, A.; Doytchinova, I. T-cell epitope vaccine design by immunoinformatics. Open Biol. 2013, 3, 120139. [Google Scholar] [CrossRef]
- Cia, G.; Pucci, F.; Rooman, M. Critical review of conformational B-cell epitope prediction methods. Brief. Bioinform. 2023, 24, bbac567. [Google Scholar] [CrossRef]
- Reiman, D.; Metwally, A.A.; Sun, J.; Dai, Y. PopPhy-CNN: A phylogenetic tree embedded architecture for convolutional neural networks to predict host phenotype from metagenomic data. IEEE J. Biomed. Health Inform. 2017, 24, 2993–3001. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.; Haiminen, N.; Carrieri, A.P.; Hu, R.; Jiang, L.; Parida, L.; Russell, B.; Allaband, C.; Zarrinpar, A.; Vázquez-Baeza, Y.; et al. Human Skin, Oral, and Gut Microbiomes Predict Chronological Age. mSystems 2020, 5, e00630-19. [Google Scholar] [CrossRef]
- Thaiss, C.A.; Zmora, N.; Levy, M.; Elinav, E. The microbiome and innate immunity. Nature 2016, 535, 65–74. [Google Scholar] [CrossRef]
- Lynch, S.V.; Pedersen, O. The human intestinal microbiome in health and disease. N. Engl. J. Med. 2016, 375, 2369–2379. [Google Scholar] [CrossRef]
- Khare, S.; Gurry, C.; Freitas, L.; Schultz, M.B.; Bach, G.; Diallo, A.; Akite, N.; Ho, J.; Lee, R.T.; Yeo, W.; et al. GISAID’s Role in Pandemic Response. China CDC Wkly. 2021, 3, 1049–1051. [Google Scholar] [CrossRef] [PubMed]
- Hadfield, J.; Megill, C.; Bell, S.M.; Huddleston, J.; Potter, B.; Callender, C.; Sagulenko, P.; Bedford, T.; Neher, R.A. Nextstrain: Real-time tracking of pathogen evolution. Bioinformatics 2018, 34, 4121–4123. [Google Scholar] [CrossRef] [PubMed]
- Viboud, C.; Sun, K.; Gaffey, R.; Ajelli, M.; Fumanelli, L.; Merler, S.; Zhang, Q.; Chowell, G.; Simonsen, L.; Vespignani, A.; et al. The RAPIDD Ebola forecasting challenge: Synthesis and lessons learnt. Epidemics 2018, 22, 13–21. [Google Scholar] [CrossRef]
- Shah, S.A.W.; Palomar, D.P.; Barr, I.; Poon, L.L.M.; Quadeer, A.A.; McKay, M.R. Seasonal antigenic prediction of influenza A H3N2 using machine learning. Nat. Commun. 2024, 15, 3833. [Google Scholar] [CrossRef] [PubMed]
- Ching, T.; Himmelstein, D.S.; Beaulieu-Jones, B.K.; Kalinin, A.A.; Do, B.T.; Way, G.P.; Ferrero, E.; Agapow, P.-M.; Zietz, M.; Hoffman, M.M.; et al. Opportunities and obstacles for deep learning in biology and medicine. J. R. Soc. Interface 2018, 15, 20170387. [Google Scholar] [CrossRef]
- Wang, S.; Sun, S.; Li, Z.; Zhang, R.; Xu, J. Accurate De Novo Prediction of Protein Contact Map by Ultra-Deep Learning Model. PLoS Comput. Biol. 2017, 13, e1005324. [Google Scholar] [CrossRef]
- Zamani, O.; Bittmann, T.; Ortega, D.L. The effect of avian influenza outbreaks on retail price premiums in the United States poultry market. Poult. Sci. 2024, 103, 104102. [Google Scholar] [CrossRef]
- van Dijk, J.G.; Hoye, B.J.; Verhagen, J.H.; Nolet, B.A.; Fouchier, R.A.; Klaassen, M. Juveniles and migrants as drivers for seasonal epizootics of avian influenza virus. J. Anim. Ecol. 2014, 83, 266–275. [Google Scholar] [CrossRef] [PubMed]
- Verhagen, J.H.; van der Jeugd, H.P.; Nolet, B.A.; Slaterus, R.; Kharitonov, S.P.; de Vries, P.P.; Vuong, O.; Majoor, F.; Kuiken, T.; Fouchier, R.A. Wild bird surveillance around outbreaks of highly pathogenic avian influenza A(H5N8) virus in the Netherlands, 2014, within the context of global flyways. Euro. Surveill. 2015, 20, 21069. [Google Scholar] [CrossRef]
- Dupas, M.-C.; Vincenti-Gonzalez, M.F.; Dhingra, M.; Guinat, C.; Vergne, T.; Wint, W.; Hendrickx, G.; Marsboom, C.; Gilbert, M.; Dellicour, S. Global risk mapping of highly pathogenic avian influenza H5N1 and H5Nx in the light of epidemic episodes occurring from 2020 onward. Epidemiol. Glob. Health 2025, 14, RP104748. [Google Scholar] [CrossRef]
- Rabinowitz, P.; Kock, R.; Kachani, M.; Kunkel, R.; Thomas, J.; Gilbert, J.; Wallace, R.; Blackmore, C.; Wong, D.; Karesh, W.; et al. Toward proof of concept of a One Health approach to disease prediction and control. Emerg. Infect. Dis. 2013, 19, e130265. [Google Scholar] [CrossRef] [PubMed]
- Hemarajata, P.; Versalovic, J. Effects of probiotics on gut microbiota: Mechanisms of intestinal immunomodulation and neuromodulation. Ther. Adv. Gastroenterol. 2013, 6, 39–51. [Google Scholar] [CrossRef]
- Jones, K.E.; Patel, N.G.; Levy, M.A.; Storeygard, A.; Balk, D.; Gittleman, J.L.; Daszak, P. Global trends in emerging infectious diseases. Nature 2008, 451, 990–993. [Google Scholar] [CrossRef]
- Atarashi, K.; Tanoue, T.; Oshima, K.; Suda, W.; Nagano, Y.; Nishikawa, H.; Fukuda, S.; Saito, T.; Narushima, S.; Hase, K.; et al. Treg induction by a rationally selected mixture of Clostridia strains from the human microbiota. Nature 2013, 500, 232–236. [Google Scholar] [CrossRef]
- Riglar, D.T.; Giessen, T.W.; Baym, M.; Kerns, S.J.; Niederhuber, M.J.; Bronson, R.T.; Kotula, J.W.; Gerber, G.K.; Way, J.C. Engineered bacteria can function in the mammalian gut long-term as live diagnostics of inflammation. Nat. Biotechnol. 2017, 35, 653–658. [Google Scholar] [CrossRef]
- Mackenzie, J.S.; Jeggo, M. The One Health approach—why is it so important? Trop. Med. Infect. Dis. 2019, 4, 88. [Google Scholar] [CrossRef]
- Lerner, H.; Berg, C. The concept of health in One Health and some practical implications for research and education: What is One Health? Infect. Ecol. Epidemiol. 2015, 5, 25300. [Google Scholar] [CrossRef]
- Zinsstag, J.; Schelling, E.; Waltner-Toews, D.; Tanner, M. From “one medicine” to “one health” and systemic approaches to health and well-being. Prev. Vet. Med. 2011, 101, 148–156. [Google Scholar] [CrossRef] [PubMed]
- Lewis, N.S.; Russell, C.A.; Langat, P.; Anderson, T.K.; Berger, K.; Bielejec, F.; Burke, D.F.; Dudas, G.; Fonville, J.M.; Fouchier, R.A.; et al. The global antigenic diversity of swine influenza A viruses. Elife 2016, 5, e12217. [Google Scholar] [CrossRef] [PubMed]
| Mechanism | Key Microbes/Metabolites | Immunological Outcome | Species |
|---|---|---|---|
| Increase anti-HA1-specific IgA and IgG levels | Lactobacillus spp. | ↑ HI titers post-HA1 vaccination | Mouse/ Chicken |
| Reg3γ lectin production | Segmented filamentous bacteria | ↑ IFN and Th17 response, ↓ rotavirus shedding | Mouse/ Pigs |
| Secondary bile acid synthesis | Clostridium scindens | ↑ Tfh cell differentiation | Human |
| SCFA such as Butyrate induction | Faecalibacterium | ↑ CD8+ cytotoxicity vs. H5N1 | Duck/ Chicken |
| α-Gal epitope presentation | Escherichia coli O86:B7 | Complement-mediated sporozoite neutralization | Eurasian teal |
| PSA-TLR2 signaling | Bacteroides fragilis | Correction of Th1/Th2 imbalance | Mouse |
| Virome-IL-12 axis | Caudovirales bacteriophages | Enhanced plasmablast differentiation | Human |
| Commensal Strain | Host Species | Vaccine Platform | Immune Outcome | Key Mechanism |
|---|---|---|---|---|
| Lactobacillus crispatus | Chicken | H5N2 inactivated | ↑ HI titers | TLR2-dependent B-cell activation |
| Bacteroides uniformis | Turkey | rHVT-H5 vectored | ↑ mucosal IgA | IL-22 induction in GALT |
| Faecalibacterium prausnitzii | Chicken | DNA vaccine (H5) | ↓ viral load | Butyrate-enhanced CD8+ cytotoxicity |
| Bifidobacterium animalis | Duck | H5 mRNA-LNP | ↑ neutralizing IgG | HDAC inhibition in germinal centers |
| Clostridium Cluster XIVa | Quail | H7 VLP | ↑ Treg/Th17 balance | SCFA-GPR43 signaling |
| Bacillus subtilis + GOS | Chicken | rNDV-H5 vectored | ↑ heterosubtypic protection | Galectin-9-mediated T-cell memory |
| Akkermansia muciniphila | Duck | Oral vector vaccine | ↑ antigen uptake | Mucin layer modulation |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sang, Y.; Nahashon, S.N.; Webby, R.J. Microbiome–Immune Interaction and Harnessing for Next-Generation Vaccines Against Highly Pathogenic Avian Influenza in Poultry. Vaccines 2025, 13, 837. https://doi.org/10.3390/vaccines13080837
Sang Y, Nahashon SN, Webby RJ. Microbiome–Immune Interaction and Harnessing for Next-Generation Vaccines Against Highly Pathogenic Avian Influenza in Poultry. Vaccines. 2025; 13(8):837. https://doi.org/10.3390/vaccines13080837
Chicago/Turabian StyleSang, Yongming, Samuel N. Nahashon, and Richard J. Webby. 2025. "Microbiome–Immune Interaction and Harnessing for Next-Generation Vaccines Against Highly Pathogenic Avian Influenza in Poultry" Vaccines 13, no. 8: 837. https://doi.org/10.3390/vaccines13080837
APA StyleSang, Y., Nahashon, S. N., & Webby, R. J. (2025). Microbiome–Immune Interaction and Harnessing for Next-Generation Vaccines Against Highly Pathogenic Avian Influenza in Poultry. Vaccines, 13(8), 837. https://doi.org/10.3390/vaccines13080837







