Bridging Gaps in Vaccine Access and Equity: A Middle Eastern Perspective
Abstract
1. Introduction
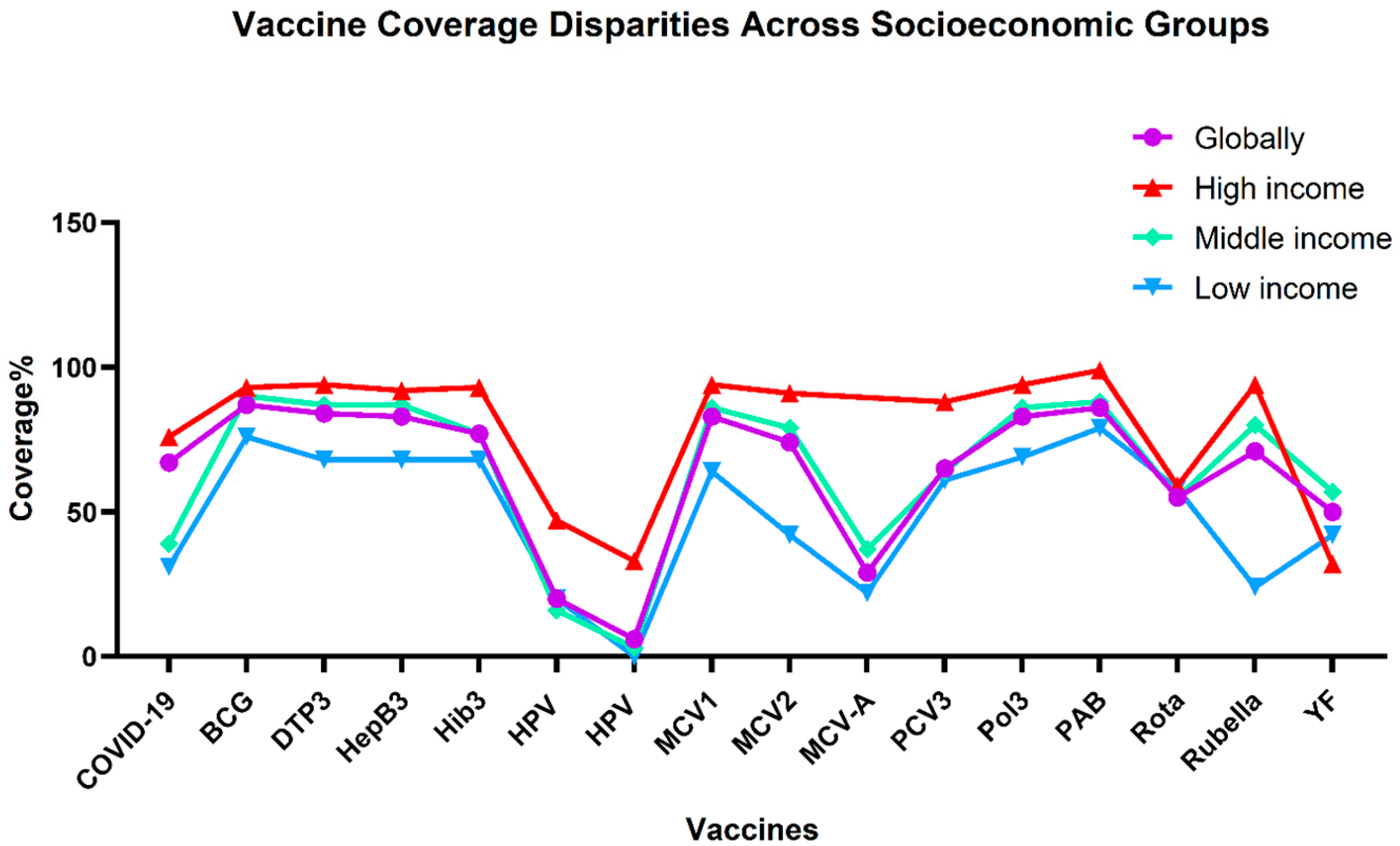
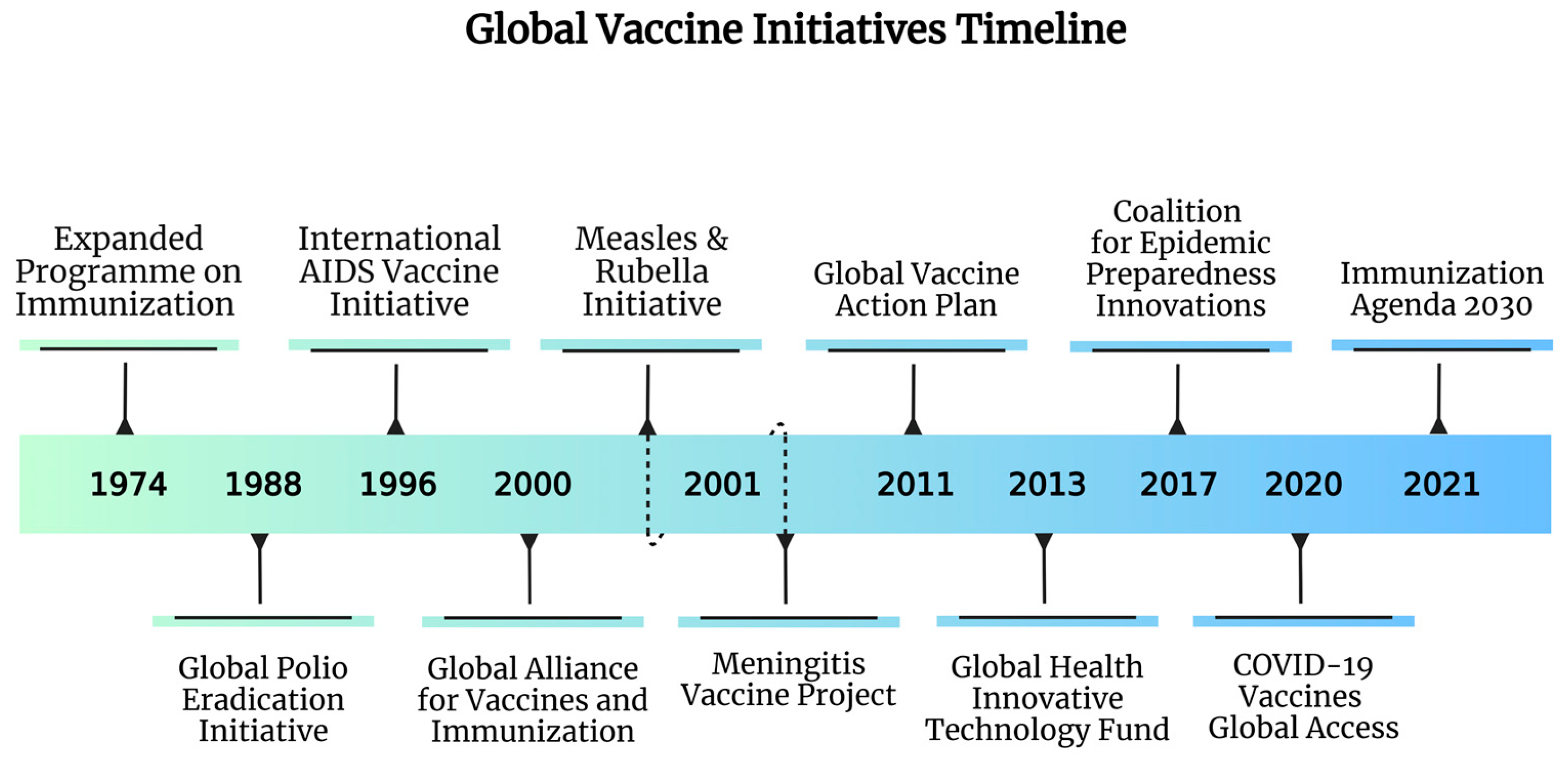
2. Global Overview of Vaccine Equity and Access
2.1. Vaccination Barriers in Developing Countries
2.2. Innovative Solutions for Vaccine Distribution in Developing Countries
2.3. International Organizations and Donor Support as Vaccination Facilitators
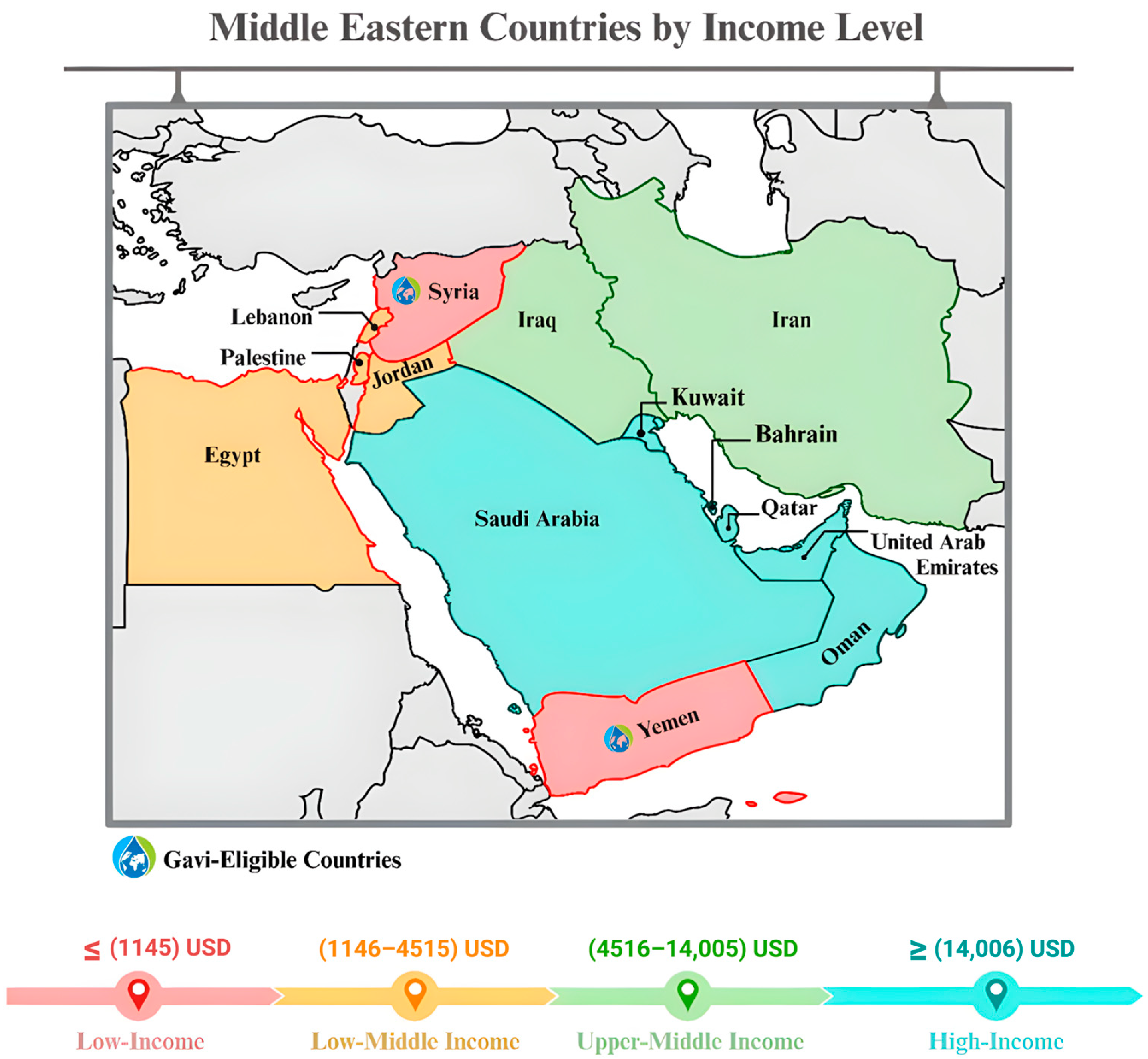
3. Overview of the Middle Eastern Region
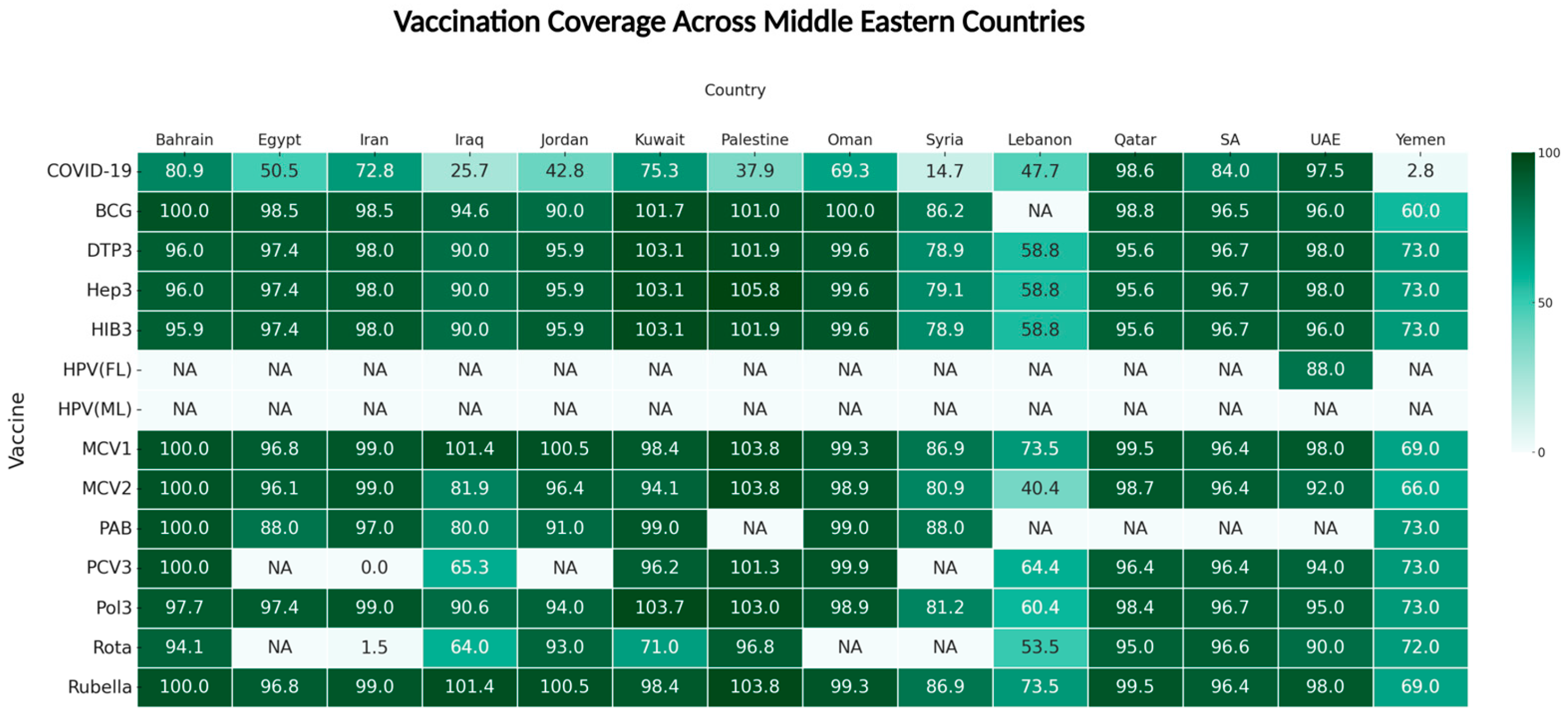
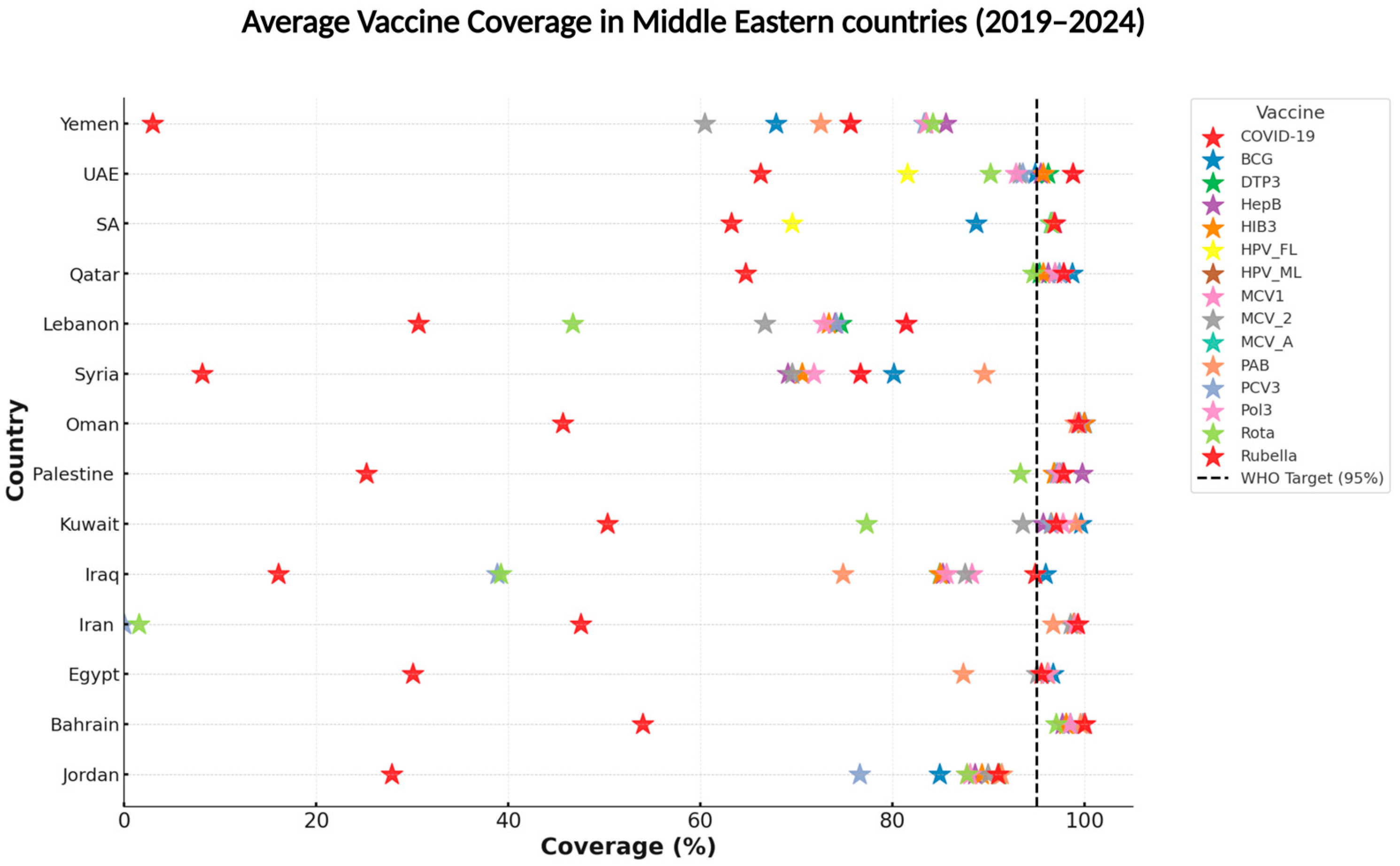
3.1. Vaccine Landscape in the Middle East
3.2. Innovative Solutions for Vaccine Distribution in the Middle East
4. Challenges and Disparities in Vaccine Access in the Middle East
4.1. Structural and Political Challenges
4.2. Regional and Social Disparities in Access
4.3. Opportunities and Initiatives to Improve Vaccine Equity
4.4. Actionable Strategies and Policy Recommendations
5. Bridging the Gaps for Improving Vaccine Access
6. Study Limitation
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CEPI | Coalition for Epidemic Preparedness Innovations |
| DTP3 | Diphtheria-Tetanus-Pertussis (3 doses) |
| EPI | Expanded Programme on Immunization |
| GCC | Gulf Cooperation Council |
| GPEI | Global Polio Eradication Initiative |
| GVAP | Global Vaccine Action Plan |
| HEPB3 | Hepatitis B (3 doses) |
| HPV | Human Papillomavirus |
| IA2030 | Immunization Agenda 2030 |
| IMD | Invasive Meningococcal Disease |
| LICs | Low-Income Countries |
| MCV1 | Measles-Containing Vaccine (1st dose) |
| MCV2 | Measles-Containing Vaccine (2nd dose) |
| MENA | Middle East and North Africa |
| MERS-CoV | Middle East Respiratory Syndrome Coronavirus |
| MICs | Middle-Income Countries |
| NIDs | National Immunization Days |
| PCV3 | Pneumococcal Conjugate Vaccine (3 doses) |
| ROTA | Rotavirus Vaccine |
| VPD | Vaccine-Preventable Disease |
| WHA | World Health Assembly |
| WUENIC | WHO/UNICEF Estimates of National Immunization Coverage |
| YF | Yellow Fever |
References
- Wolicki, S.B.; Nuzzo, J.B.; Blazes, D.L.; Pitts, D.L.; Iskander, J.K.; Tappero, J.W. Public Health Surveillance: At the Core of the Global Health Security Agenda. Health Secur. 2016, 14, 185–188. [Google Scholar] [CrossRef]
- McInnes, C. WHO’s next? Changing authority in global health governance after Ebola. Int. Aff. 2015, 91, 1299–1316. [Google Scholar] [CrossRef]
- Privor-Dumm, L.; Excler, J.L.; Gilbert, S.; Abdool Karim, S.S.; Hotez, P.J.; Thompson, D.; Kim, J.H. Vaccine access, equity and justice: COVID-19 vaccines and vaccination. BMJ Glob. Health 2023, 8, e011881. [Google Scholar] [CrossRef]
- Singh, B.; Chattu, V.K. Prioritizing ‘equity’ in COVID-19 vaccine distribution through Global Health Diplomacy. Health Promot. Perspect. 2021, 11, 281–287. [Google Scholar] [CrossRef]
- Nunes, C.; McKee, M.; Howard, N. The role of global health partnerships in vaccine equity: A scoping review. PLoS Glob. Public Health 2024, 4, e0002834. [Google Scholar] [CrossRef]
- Duan, Y.; Shi, J.; Wang, Z.; Zhou, S.; Jin, Y.; Zheng, Z.J. Disparities in COVID-19 Vaccination among Low-, Middle-, and High-Income Countries: The Mediating Role of Vaccination Policy. Vaccines 2021, 9, 905. [Google Scholar] [CrossRef]
- Sehovic, A.B.; Govender, K. Addressing COVID-19 vulnerabilities: How do we achieve global health security in an inequitable world. Glob. Public Health 2021, 16, 1198–1208. [Google Scholar] [CrossRef]
- Sadr-Azodi, N.; DeRoeck, D.; Senouci, K. Breaking the inertia in coverage: Mainstreaming under-utilized immunization strategies in the Middle East and North Africa region. Vaccine 2018, 36, 4425–4432. [Google Scholar] [CrossRef]
- World Health Organization (WHO) Regional Office for the Eastern Mediterranean. Expanded Programme on Immunization. Available online: https://www.emro.who.int/egy/programmes/expanded-programme-on-immunization.html (accessed on 17 July 2025).
- Saxenian, H.; Sadr-Azodi, N.; Kaddar, M.; Senouci, K. Immunisation financing and programme performance in the Middle East and North Africa, 2010 to 2017. BMJ Glob. Health 2019, 4, e001248. [Google Scholar] [CrossRef]
- Piot, P.; Larson, H.J.; O’Brien, K.L.; N’Kengasong, J.; Ng, E.; Sow, S.; Kampmann, B. Immunization: Vital progress, unfinished agenda. Nature 2019, 575, 119–129. [Google Scholar] [CrossRef]
- Rojas-Venegas, M.; Cano-Ibanez, N.; Khan, K.S. Vaccination coverage among migrants: A systematic review and meta-analysis. Semergen 2022, 48, 96–105. [Google Scholar] [CrossRef]
- Iqbal, M.S.; Khan, S.U.; Qamer, S.; Vohra, S. Vaccine Hesitancy of COVID-19 among Parents for Their Children in Middle Eastern Countries-A Systematic Review. Vaccines 2023, 11, 1556. [Google Scholar] [CrossRef]
- United Nations International Children’s Emergency Fund (UNICEF). Where We Work. Available online: https://www.unicef.org/mena/where-we-work (accessed on 17 July 2025).
- World Health Organization (WHO). Vaccines and Vaccination Against Yellow Fever: WHO Position Paper—June 2013. Wkly. Epidemiol. Rec. 2013, 88, 269–284. Available online: https://www.who.int/publications/i/item/who-wer8827 (accessed on 17 July 2025).
- Gavi, the Vaccine Alliance. Yellow Fever Vaccine Support. Available online: https://www.gavi.org/types-support/vaccine-support/yellow-fever (accessed on 17 July 2025).
- Kane, M.A.; Serrano, B.; de Sanjose, S.; Wittet, S. Implementation of human papillomavirus immunization in the developing world. Vaccine 2012, 30 (Suppl. S5), F192–F200. [Google Scholar] [CrossRef]
- Ali, H.A.; Hartner, A.M.; Echeverria-Londono, S.; Roth, J.; Li, X.; Abbas, K.; Portnoy, A.; Vynnycky, E.; Woodruff, K.; Ferguson, N.M.; et al. Vaccine equity in low and middle income countries: A systematic review and meta-analysis. Int. J. Equity Health 2022, 21, 82. [Google Scholar] [CrossRef]
- Bennett, A.; Bar-Zeev, N.; Cunliffe, N.A. Measuring indirect effects of rotavirus vaccine in low income countries. Vaccine 2016, 34, 4351–4353. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Immunization Data Portal—All Data. Available online: https://immunizationdata.who.int/global?topic=Vaccination-coverage&location= (accessed on 17 July 2025).
- World Health Organization (WHO). COVID-19 Vaccines | WHO COVID-19 Dashboard. Available online: https://data.who.int/dashboards/covid19/vaccines (accessed on 17 July 2025).
- Dumpa, N.; Goel, K.; Guo, Y.; McFall, H.; Pillai, A.R.; Shukla, A.; Repka, M.A.; Murthy, S.N. Stability of Vaccines. Am. Assoc. Pharm. Sci. PharmSciTech 2019, 20, 42. [Google Scholar] [CrossRef]
- Khatiwada, A.P.; Shrestha, S.; Dharel, D.; Sapkota, B. Immunization Practice in Low- and Middle-Income Countries; Springer International Publishing: Cham, Switzerland, 2023; pp. 851–866. [Google Scholar] [CrossRef]
- American Society of Health-System Pharmacists (ASHP). ASHP Executive Forum on Cold Chain Management: Pharmaceutical Cold Chain Management in Health Systems. Resource Guide #1. 2022. Available online: https://www.ashp.org/-/media/assets/innovation/docs/ASHP-Cold-Chain-Management-Resource-Guide-1.pdf (accessed on 17 July 2025).
- World Health Assembly, 71. Addressing the Global Shortage of, and Access to, Medicines and Vaccines: Report by the Director-General. World Health Organization. 2018. Available online: https://iris.who.int/handle/10665/276350 (accessed on 17 July 2025).
- Ergetie, F.S.; Kassaw, A.T.; Sendekie, A.K. Vaccine cold chain management practices in primary health centers providing an ex-panded immunization program in Northwest Ethiopia: Self-reported and actual practice observational study. Front. Public Health 2023, 11, 1194807. [Google Scholar] [CrossRef]
- Lennon, P.; Atuhaire, B.; Yavari, S.; Sampath, V.; Mvundura, M.; Ramanathan, N.; Robertson, J. Root cause analysis underscores the im-portance of understanding, addressing, and communicating cold chain equipment failures to improve equipment performance. Vaccine 2017, 35, 2198–2202. [Google Scholar] [CrossRef]
- De Boeck, K.; Decouttere, C.; Vandaele, N. Vaccine distribution chains in low- and middle-income countries: A literature review. Omega 2020, 97, 102097. [Google Scholar] [CrossRef]
- Acharya, K.P.; Ghimire, T.R.; Subramanya, S.H. Access to and equitable distribution of COVID-19 vaccine in low-income countries. NPJ Vaccines 2021, 6, 54. [Google Scholar] [CrossRef]
- Goldenberg, M.J. Vaccine Hesitancy: Public Trust, Expertise, and the War on Science; University of Pittsburgh Press: Pittsburgh, PA, USA, 2021. [Google Scholar] [CrossRef]
- Le, L.M.; Veettil, S.K.; Donaldson, D.; Kategeaw, W.; Hutubessy, R.; Lambach, P.; Chaiyakunapruk, N. The impact of pharmacist involvement on immunization uptake and other outcomes: An updated systematic review and meta-analysis. J. Am. Pharm. Assoc. 2022, 62, 1499–1513.e16. [Google Scholar] [CrossRef]
- Eiden, A.L.; Drakeley, S.; Modi, K.; Mackie, D.; Bhatti, A.; DiFranzo, A. Attitudes and beliefs of healthcare providers toward vac-cination in the United States: A cross-sectional online survey. Vaccine 2024, 42, 126437. [Google Scholar] [CrossRef]
- Lorini, C.; Santomauro, F.; Donzellini, M.; Capecchi, L.; Bechini, A.; Boccalini, S.; Bonanni, P.; Bonaccorsi, G. Health literacy and vaccination: A systematic review. Hum. Vaccines Immunother. 2018, 14, 478–488. [Google Scholar] [CrossRef]
- Ngo, N.V.; Pemunta, N.V.; Muluh, N.E.; Adedze, M.; Basil, N.; Agwale, S. Armed conflict, a neglected determinant of childhood vaccination: Some children are left behind. Hum. Vaccines Immunother. 2020, 16, 1454–1463. [Google Scholar] [CrossRef]
- Singh, S.K.; Gupta, G.K.; Agrawal, D.; Zaidi, S.H.N.; Batra, J.; Sharma, L.; Juneja, S.; Joshi, K.J.; Sethy, G.; Haile, D.A.; et al. Leveraging Resource Centers for Strengthening Immunization Supply Chain. Cureus 2024, 16, e58966. [Google Scholar] [CrossRef]
- Adhikari, B.B.; Goodson, J.L.; Chu, S.Y.; Rota, P.A.; Meltzer, M.I. Assessing the Potential Cost-Effectiveness of Microneedle Patches in Childhood Measles Vaccination Programs: The Case for Further Research and Development. Drugs R D 2016, 16, 327–338. [Google Scholar] [CrossRef]
- Kolluru, C.; Gomaa, Y.; Prausnitz, M.R. Development of a thermostable microneedle patch for polio vaccination. Drug Deliv. Transl. Res. 2019, 9, 192–203. [Google Scholar] [CrossRef]
- Gavi, the Vaccine Alliance. How Solar Power is Revolutionising Immunisation in the Most Remote Parts of the World. Available online: https://www.gavi.org/vaccineswork/how-solar-power-revolutionising-immunisation-most-remote-parts-world (accessed on 17 July 2025).
- World Health Organization. Introducing Solar-Powered Vaccine Refrigerator and Freezer Systems: A Guide for Managers in National Immunization Programmes; WHO: Geneva, Switzerland, 2015; Available online: https://apps.who.int/iris/bitstream/handle/10665/195778/9789241509862_eng.pdf (accessed on 17 July 2025)ISBN 9789241509862.
- Aggarwal, S.; Gupta, P.; Balaji, S.; Sharma, S.; Ghosh, A.K.; Simmy; Bhargava, B.; Panda, S. Assessing the Feasibility of Drone-Mediated Vaccine De-livery: An Exploratory Study. Health Sci. Rep. 2025, 8, e70208. [Google Scholar] [CrossRef]
- Alhothali, G.T.; Mavondo, F.T.; Alyoubi, B.A.; Algethami, H. Consumer Acceptance of Drones for Last-Mile Delivery in Jeddah, Saudi Arabia. Sustainability 2024, 16, 5621. [Google Scholar] [CrossRef]
- Civil Aviation Authority (Oman). Regulation Governing Unmanned Aircraft Systems (Drones). Decision No. 1412/2023, Issued 15 October 2023. Available online: https://www.caa.gov.om/files/publications/regulation-governing-unmanned-aircraft-systems-drones.pdf (accessed on 17 July 2025).
- Lexology. SA: New Vaccine-Related Regulations and Compliance Requirements. (14 March 2024). Available online: https://www.lexology.com/library/detail.aspx?g=a68af277-8311-468f-a14a-4183ddb7ee3c (accessed on 17 July 2025).
- Xie, Y.J.; Liao, X.; Lin, M.; Yang, L.; Cheung, K.; Zhang, Q.; Li, Y.; Hao, C.; Wang, H.H.; Gao, Y.; et al. Community Engagement in Vaccination Promotion: Systematic Review and Meta-Analysis. J. Med. Internet Res. Public Health Surveill. 2024, 10, e49695. [Google Scholar] [CrossRef]
- Gonah, L.; Kobie, A.G. Framework for Risk Communication and Community Engagement to Improve Vaccine Uptake for COVID-19 and other Vaccine-Preventable Diseases in Low- and Middle-Income Countries (LMIC). Ann. Glob. Health 2021, 87, 123. [Google Scholar] [CrossRef]
- Rago, L.; Sillo, H.; ‘t Hoen, E.; Zweygarth, M. Regulatory framework for access to safe, effective quality medicines. Antivir. Ther. 2014, 19 (Suppl. S3), 69–77. [Google Scholar] [CrossRef]
- World Health Organization. Egypt’s Regulatory System Reaches WHO Maturity Level 3 in Medicines Reg-Ulation. WHO News. (20 December 2024). Available online: https://www.who.int/news/item/20-12-2024-egypt-s-regulatory-system-reaches-who-maturity-level-3-in-medicines-regulation (accessed on 17 July 2025).
- World Health Organization. SA Regulatory System Becomes Third to Reach WHO Maturity Level 4. WHO News. (30 October 2023). Available online: https://www.who.int/news/item/30-10-2023-saudi-arabia-regulatory-system-becomes-third-to-reach-who-maturity-level-4 (accessed on 17 July 2025).
- Dureab, F.; Hussain, T.; Sheikh, R.; Al-Dheeb, N.; Al-Awlaqi, S.; Jahn, A. Forms of Health System Fragmentation During Conflict: The Case of Yemen. Front. Public Health 2021, 9, 659980. [Google Scholar] [CrossRef]
- World Health Organization, Regional Office for the Eastern Mediterranean. Statement for Regional Di-rector, WHO Eastern Mediterranean Region, on Occupied Palestinian Territory. (16 October 2023). Available online: https://www.emro.who.int/media/news/statement-for-regional-director-who-eastern-mediterranean-region-on-occupied-palestinian-territory.html (accessed on 17 July 2025).
- Alshammari, T.M.; Mendi, N.; Alenzi, K.A.; Alsowaida, Y. Pharmacovigilance Systems in Arab Countries: Overview of 22 Arab Countries. Drug Saf. 2019, 42, 849–868. [Google Scholar] [CrossRef]
- Hardon, A.; Blume, S. Shifts in global immunisation goals (1984–2004): Unfinished agendas and mixed results. Soc. Sci. Med. 2005, 60, 345–356. [Google Scholar] [CrossRef]
- Bustreo, F.; Okwo-Bele, J.M.; Kamara, L. World Health Organization perspectives on the contribution of the Global Alliance for Vaccines and Immunization on reducing child mortality. Arch. Dis. Child. 2015, 100 (Suppl. S1), S34–S37. [Google Scholar] [CrossRef]
- MacDonald, N.; Mohsni, E.; Al-Mazrou, Y.; Kim Andrus, J.; Arora, N.; Elden, S.; Madrid, M.Y.; Martin, R.; Mahmoud Mustafa, A.; Rees, H.; et al. Global vaccine action plan lessons learned I: Recommendations for the next decade. Vaccine 2020, 38, 5364–5371. [Google Scholar] [CrossRef]
- Carter, A.; Msemburi, W.; Sim, S.Y.; Gaythorpe, K.A.M.; Lambach, P.; Lindstrand, A.; Hutubessy, R. Modeling the impact of vaccination for the immunization Agenda 2030: Deaths averted due to vaccination against 14 pathogens in 194 countries from 2021 to 2030. Vaccine 2024, 42 (Suppl. S1), S28–S37. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Global Vaccine Action Plan 2011–2020. 2013. Available online: https://www.who.int/publications/i/item/global-vaccine-action-plan-2011-2020 (accessed on 17 July 2025).
- McAdams, D.; McDade, K.K.; Ogbuoji, O.; Johnson, M.; Dixit, S.; Yamey, G. Incentivising wealthy nations to participate in the COVID-19 Vaccine Global Access Facility (COVAX): A game theory perspective. BMJ Glob. Health 2020, 5, e003627. [Google Scholar] [CrossRef]
- Nagi, M.A.; Luangsinsiri, C.; Thavorncharoensap, M. A systematic review of economic evaluations of vaccines in Middle East and North Africa countries: Is existing evidence good enough to support policy decision-making? Expert Rev. Pharmacoecon. Outcomes Res. 2021, 21, 1159–1178. [Google Scholar] [CrossRef]
- Beaumont, P.; Blake, G.H.; Wagstaff, J.M. The Middle East: A Geographical Study, 2nd ed.; Routledge: London, UK, 1988; Available online: https://api.pageplace.de/preview/DT0400.9781317240303_A26682329/preview-9781317240303_A26682329.pdf (accessed on 17 July 2025).
- Almezaini, K.; Rickli, J.M. The Small Gulf States: Foreign and Security Policies Before and After the Arab Spring; Routledge: London, UK, 2016; Available online: https://books.google.jo/books?id=n2SuDQAAQBAJ&lpg=PA1966&hl=ar&pg=PA1966#v=onepage&q&f=false (accessed on 17 July 2025)ISBN 9781317214342.
- Bashir, F.A. The Behaviour of Muslim Foreign Aid Donors During the Coronavirus Pandemic: The Case of GCC States. Islam Civilisational Renew. 2022, 13, 11–30. [Google Scholar] [CrossRef]
- World Health Organization, Regional Office for the Eastern Mediterranean. Expanded Programme on Immunization in the Eastern Mediterranean Region. East. Mediterr. Health, J. 1996, 2, 151–154. Available online: https://www.emro.who.int/emhj-volume-2-1996/volume-2-issue-1/article22.html (accessed on 17 July 2025).
- World Health Organization; Ministry of Health, Bahrain. Bahrain COVID-19 Case Studies: Leveraging Digital Reminders to Increase Immunization Coverage. WHO EMRO. 2022. Available online: https://www.moh.gov.bh/Content/Upload/File/637933076434107917-WHOEMBAH001E-eng.pdf (accessed on 17 July 2025).
- World Health Organization, Regional Office for the Eastern Mediterranean. Eastern Mediterranean Vaccine Action Plan| VPI-infocus | Vaccine Preventable Diseases. Available online: https://www.emro.who.int/vpi/vpi-infocus/eastern-mediterranean-vaccine-action-plan.html (accessed on 17 July 2025).
- United Nations International Children’s Emergency Fund (UNICEF) Egypt. National Immunization Campaign Against Polio. UNICEF. Available online: https://www.unicef.org/egypt/stories/national-immunization-campaign-against-polio (accessed on 17 July 2025).
- Saleh, S.; Chedid, P. Knowledge, attitude and practice toward childhood immunization among mothers in Lebanon. PLoS ONE 2025, 20, e0322205. [Google Scholar] [CrossRef]
- Kaloti, R.; Fouad, F.M. The politics of COVID-19 vaccine equity among refugee populations in Lebanon. J. Glob. Health Econ. Policy 2022, 2, e2022003. [Google Scholar] [CrossRef]
- United Nations International Children’s Emergency Fund (UNICEF). Lebanon’s Crisis Threatening Children’s Health. (21 February 2023). Available online: https://www.unicef.org/press-releases/lebanons-crisis-threatening-childrens-health (accessed on 17 July 2025).
- World Bank. World Bank Country and Lending Groups. 2024. Available online: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (accessed on 17 July 2025).
- Binagwaho, A.; Farmer, P.E.; Nsanzimana, S.; Karema, C.; Gasana, M.; de Dieu Ngirabega, J.; Ngabo, F.; Wagner, C.M.; Nutt, C.T.; Nyatanyi, T.; et al. Rwanda 20 years on: Investing in life. Lancet 2014, 384, 371–375. [Google Scholar] [CrossRef]
- Program for Appropriate Technology in Health (PATH). Vietnam and ImmReg: Expanding Reach of the Immunization Registry in Vietnam. Seattle, WA: PATH. 2016. Available online: https://www.path.org/publications/files/ID_vietnam_unf_cs.pdf (accessed on 17 July 2025).
- Hester, K.A.; Sakas, Z.; Ellis, A.S.; Bose, A.S.; Darwar, R.; Gautam, J.; Jaishwal, C.; James, H.; Keskinocak, P.; Nazzal, D.; et al. Critical success factors for high routine immunization per-formance: A case study of Nepal. Vaccine X 2022, 12, 100214. [Google Scholar] [CrossRef]
- Abu-Odah, H.; Su, J.; Musa, S.S. Unwillingness or reluctance of Palestinians to get the COVID-19 vaccine: The reasons behind it and how to persuade them. Int. J. Infect. Dis. 2022, 119, 53–55. [Google Scholar] [CrossRef]
- Ritchie, H.; Mathieu, E.; Rodés-Guirao, L.; Appel, C.; Gavrilov, D.; Giattino, C.; Hasell, J.; Macdonald, B.; Dattani, S.; Beltekian, D.; et al. Coronavirus (COVID-19) Vaccinations. Our World in Data. 2024. Available online: https://ourworldindata.org/covid-vaccinations (accessed on 17 July 2025).
- Majer, J.; Elhissi, J.H.; Mousa, N.; Kostandova, N. COVID-19 vaccination in the Gaza Strip: A cross-sectional study of vaccine coverage, hesitancy, and associated risk factors among community members and healthcare workers. Confl. Health 2022, 16, 48. [Google Scholar] [CrossRef]
- Kapuria, B.; Sami Hamadeh, R.; Mazloum, F.; Korbane, J.A.; Aung, K.; Kamal, D.; Chamoun, N.; Syed, S. Achieving sustainable, environmentally viable, solarized vaccine cold chain system and vaccination program-an effort to move towards clean and green energy-driven pri-mary healthcare in Lebanon. Front. Health Serv. 2024, 4, 1386432. [Google Scholar] [CrossRef]
- Department of Health—Abu Dhabi. Abu Dhabi to Use Drone Technology for Medical Supply Transfer and Delivery. (6 July 2021). Available online: https://www.doh.gov.ae/en/news/Abu-Dhabi-to-Use-Drone-Technology-for-Medical-Supply-Transfer-and-Delivery (accessed on 17 July 2025).
- Abu Dhabi Global Healthcare Week. SA Announces $133M Vaccine Manufacturing Facility. (June 2022). Available online: https://www.adghw.com/articles/in-the-news/2022/june/saudi-arabia-announces-133m-vaccine-manufacturing-facility (accessed on 17 July 2025).
- Hayat Biotech. Hayat-Vax Becomes First COVID-19 Vaccine Produced in the Arab World. (29 March 2021). Available online: https://hayatbiotech.com/hayat-vax-becomes-first-covid-19-vaccine-produced-in-the-arab-world (accessed on 17 July 2025).
- Ministry of Health—Kingdom of Bahrain. E-Services. Available online: https://www.moh.gov.bh/eServices?lang=en&utm (accessed on 17 July 2025).
- Louw, G.E.; Hohlfeld, A.S.; Kalan, R.; Engel, M.E. Mobile Phone Text Message Reminders to Improve Vaccination Uptake: A Sys-tematic Review and Meta-Analysis. Vaccines 2024, 12, 1151. [Google Scholar] [CrossRef]
- Alvaredo, F.; Assouad, L.; Piketty, T. Measuring lnequality in the Middle East 1990–2016: The World’s Most Unequal Region? Rev. Income Wealth 2018, 65, 685–711. [Google Scholar] [CrossRef]
- Hanieh, A.; Ziadah, R. Pandemic Effects: COVID-19 and the Crisis of Development in the Middle East. Dev. Change 2022, 53, 1308–1334. [Google Scholar] [CrossRef] [PubMed]
- Fawcett, L. The Middle East and COVID-19: Time for collective action. Glob. Health 2021, 17, 133. [Google Scholar] [CrossRef] [PubMed]
- Dahdal, Y.; Davidovitch, N.; Gilmont, M.; Lezaun, J.; Negev, M.; Sandler, D.; Shaheen, M. Lessons of the Israeli-palestinian conflict for public health: The case of the COVID-19 vaccination gap. Int. J. Environ. Res. Public Health 2021, 18, 11292. [Google Scholar] [CrossRef]
- Grundy, J.; Biggs, B.A. The impact of conflict on immunisation coverage in 16 countries. Int. J. Health Policy Manag. 2019, 8, 211–221. [Google Scholar] [CrossRef]
- Ozaras, R.; Leblebicioglu, H.; Sunbul, M.; Tabak, F.; Balkan, I.I.; Yemisen, M.; Sencan, I.; Ozturk, R. The Syrian conflict and infectious diseases. Expert Rev. Anti-Infect. Ther. 2016, 14, 547–555. [Google Scholar] [CrossRef]
- Kaddar, M.; Saxenian, H.; Senouci, K.; Mohsni, E.; Sadr-Azodi, N. Vaccine procurement in the Middle East and North Africa region: Challenges and ways of improving program efficiency and fiscal space. Vaccine 2019, 37, 3520–3528. [Google Scholar] [CrossRef]
- Mishrif, A.; Al Balushi, Y. (Eds.) Economic Diversification in the Gulf Region: Comparing Global Challenges. In The Political Economy of the Middle East; Palgrave Macmillan: London, UK, 2018; Volume II, Available online: https://books.google.jo/books?id=5wdGDwAAQBAJ&lpg=PR5&dq=economic%20challenges%20%2B%20GULF%20countries&lr=lang_en&pg=PR7#v=onepage&q=economic%20challenges%20+%20GULF%20countries&f=true (accessed on 17 July 2025).
- Rahman, M.M.; Umar, S.; Awad Almarri, S.; Khan, H.T.A. Healthcare Provisions for Migrant Workers in Qatar. Health Soc. Care Community 2023, 2023, 1–13. [Google Scholar] [CrossRef]
- Rinaldi, A.L.; Lima, R.D.C.; Apolinário Júnior, L. The US–China Rivalry: Health Diplomacy and Vaccine Donations Strategies. J. Curr. Chin. Aff. 2024, 1–30. [Google Scholar] [CrossRef]
- Singh, B.; Kaur, J.; Chattu, V.K. Global vaccine inequities and multilateralism amid COVID-19: Reconnaissance of Global Health Diplomacy as a panacea? Health Promot. Perspect. 2022, 12, 315–324. [Google Scholar] [CrossRef] [PubMed]
- Kickbusch, I.; Liu, A. Global health diplomacy-reconstructing power and governance. Lancet 2022, 399, 2156–2166. [Google Scholar] [CrossRef] [PubMed]
- Siddiqui, A.; Priya; Adnan, A.; Abbas, S.; Qamar, K.; Islam, Z.; Rahmat, Z.S.; Essar, M.Y.; Farahat, R.A. COVID-19 vaccine hesitancy in conflict zones: A review of current literature. Front. Public Health 2022, 10, 1006271. [Google Scholar] [CrossRef] [PubMed]
- Blanchet, K.; Mallard, G.; Moret, E.; Sun, J. Sanctioned countries in the global COVID-19 vaccination campaign: The forgotten 70. Confl. Health 2021, 15, 69. [Google Scholar] [CrossRef]
- Katoue, M.G.; Cerda, A.A.; Garcia, L.Y.; Jakovljevic, M. Healthcare system development in the Middle East and North Africa region: Challenges, endeavors and prospective opportunities. Front. Public Health 2022, 10, 1045739. [Google Scholar] [CrossRef]
- United Nations Office for the Coordination of Humanitarian Affairs (OCHA). Humanitarian Situation Update #306: Gaza Strip. (30 June 2023). Available online: https://www.ochaopt.org/content/humanitarian-situation-update-306-gaza-strip (accessed on 17 July 2025).
- Médecins Sans Frontières (MSF). Israel and Palestine: The Despair of Vaccination Inequalities. Doctors Without Borders. (3 March 2021). Available online: https://www.doctorswithoutborders.ca/israel-and-palestine-the-despair-of-vaccination-inequalities (accessed on 17 July 2025).
- Swissinfo.ch. Yemen and the Challenge of COVID Vaccine Rollout in Conflict Countries. (4 June 2021). Available online: https://www.swissinfo.ch/eng/politics/yemen-and-the-challenge-of-covid-vaccine-rollout-in-conflict-countries/46651534 (accessed on 17 July 2025).
- Murshidi, M.M.; Hijjawi, M.Q.B.; Jeriesat, S.; Eltom, A. Syrian refugees and Jordan’s health sector. Lancet 2013, 382, 206–207. [Google Scholar] [CrossRef]
- Doshmangir, L.; Shirjang, A.; Assan, A.; Gordeev, V.S. Iranian primary health care network: Challenges and ways forward. Prim. Health Care Res. Dev. 2023, 24, e1. [Google Scholar] [CrossRef]
- World Bank. Stakeholder Engagement Plan (SEP): Supporting Lebanon’s COVID-19 Vaccination and Response for Vulnerable Groups (P176778); World Bank Group: Washington, DC, USA, 2021; Available online: https://documents.worldbank.org/en/publication/documents-reports/documentdetail/099715112072127444 (accessed on 17 July 2025).
- DeRoeck, D.; Bawazir, S.A.; Carrasco, P.; Kaddar, M.; Brooks, A.; Fitzsimmons, J.; Andrus, J. Regional group purchasing of vaccines: Review of the Pan American Health Organization EPI revolving fund and the Gulf Cooperation Council group purchasing program. Int. J. Heal. Plan. Manag. 2006, 21, 23–43. [Google Scholar] [CrossRef]
- Al-Tawfiq, J.A.; Lee, S.-S.; Memish, Z.A. Emergence of invasive meningococcal disease during Hajj pilgrimage—Vigilance and preparedness, in the post-pandemic year. Int. J. Infect. Dis. 2024, 145, 107092. [Google Scholar] [CrossRef]
- Khaleej Times. Free HPV Vaccine for Dubai Schoolgirls to Start in March. 2024. Available online: https://www.khaleejtimes.com/lifestyle/health/free-hpv-vaccine-for-dubai-schoolgirls-to-start-in-march (accessed on 17 July 2025).
- Mbaeyi, C.; Ryan, M.J.; Smith, P.; Mahamud, A.; Farag, N.; Haithami, S.; Sharaf, M.; Jorba, J.C.; Ehrhardt, D. Response to a Large Polio Outbreak in a Setting of Conflict—Middle East, 2013–2015. Materials 2017, 66, 227–231. [Google Scholar] [CrossRef]
- King Abdullah International Medical Research Center (KAIMRC). KAIMRC a Strong Player in Quest for a MERS-CoV Vaccine (Issue No. 6). Available online: https://innovations.kaimrc.med.sa/en/feature/387/kaimrc-a-strong-player-in-quest-for-a-mers-cov-vaccine%C2%A0.html (accessed on 17 July 2025).
- United Nations International Children’s Emergency Fund (UNICEF). Routine Childhood Immuniza-tions. 2023. Available online: https://www.unicef.org/jordan/stories/routine-childhood-immunizations (accessed on 17 July 2025).
- World Bank. Vaccinating Refugees: Lessons from the Inclusive Lebanon Vaccine Roll-Out Experience. 2021. Available online: https://www.worldbank.org/en/news/feature/2021/06/18/vaccinating-refugees-lessons-from-the-inclusive-lebanon-vaccine-roll-out-experience (accessed on 17 July 2025).
- Khaleej Times. Here’s How This Abu Dhabi Firm is Reshaping Global Pharma Supply Chain. 2023. Available online: https://www.khaleejtimes.com/uae/heres-how-this-abu-dhabi-firm-is-reshaping-global-pharma-supply-chain (accessed on 17 July 2025).
- Suliman, D.M.; Nawaz, F.A.; Mohanan, P.; Modber, M.A.K.A.; Musa, M.K.; Musa, M.B.; El Chbib, D.; Elhadi, Y.A.M.; Essar, M.Y.; Isa, M.A.; et al. UAE efforts in promoting COVID-19 vaccination and building vaccine confidence. Vaccine 2021, 39, 6341–6345. [Google Scholar] [CrossRef] [PubMed]
- Saudi Authority for Industrial Cities and Technology Zones (Modon). Modon signs Vaccine Deal for Plant in Sadeer City. Available online: https://www.zawya.com/en/business/healthcare/modon-vaccine-sign-deal-for-plant-in-sadeer-city-sulehjv7 (accessed on 17 July 2025).
- World Health Organization (WHO) Regional Office for the Eastern Mediterranean. Eastern Mediter-Ranean Vaccine Action Plan 2016–2020: A Framework for Implementation of the Global Vaccine Action Plan. WHO Regional Office for the Eastern Mediterranean. 2016. Available online: https://apps.who.int/iris/handle/10665/250375 (accessed on 17 July 2025).
- World Health Organization (WHO) Regional Office for the Eastern Mediterranean. Sixtieth Session of the WHO Regional Committee for the Eastern Mediterranean. 2013. Available online: https://www.emro.who.int/about-who/rc60/sixtieth-session.html (accessed on 17 July 2025).
- United Nations International Children’s Emergency Fund (UNICEF) Jordan. From Mafraq to Aqaba, Young Volunteers are Leading Efforts to Build Trust in COVID-19 Vaccines. 2022. Available online: https://www.unicef.org/jordan/stories/mafraq-aqaba-young-volunteers-are-leading-efforts-build-trust-covid-19-vaccines (accessed on 17 July 2025).
- Gavi, the Vaccine Alliance. Gulf Countries Unite to Support COVAX. 2021. Available online: https://www.gavi.org/news/media-room/gulf-countries-unite-support-covax#:~:text=Geneva%2C%206%20October%202021%20%E2%80%93%20Gulf,US%24%202.5%20million%20in%20funding (accessed on 17 July 2025).
- United Nations International Children’s Emergency Fund (UNICEF). Kingdom of SA Pledges US$ 50 Million to Protect Children Around the World from Polio and Measles. 2019. Available online: https://www.unicef.org/press-releases/kingdom-saudi-arabia-pledges-us-500-million-protect-children-around-world-polio-and (accessed on 17 July 2025).
- Gavi, the Vaccine Alliance. The Arab League Supports Gavi Efforts on Immunisation and Saving Children’s Lives with Vaccines. Available online: https://www.gavi.org/news/media-room/arab-league-supports-gavi-efforts-immunisation-and-saving-childrens-lives-vaccines (accessed on 17 July 2025).
- Lam, E.; Al-Tamimi, W.; Russell, S.P.; Butt, M.O.-U.I.; Blanton, C.; Musani, A.S.; Date, K. Oral Cholera Vaccine Coverage during an Outbreak and Humanitarian Crisis, Iraq, 2015. Emerg. Infect. Dis. 2017, 23, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Institute for Economics & Peace. Global Peace Index 2023: Measuring Peace in a Complex World, Sydney, June 2023. Available online: http://visionofhumanity.org/resources (accessed on 17 July 2025).
- Gavi, the Vaccine Alliance. Our Support: Guidelines. Available online: https://www.gavi.org/news/document-library/gavi-vaccine-funding-guidelines (accessed on 17 July 2025).
- World Health Organization. Report on Assessment of Public Health Core Capacities of the International Health Regulations (2005): Bahrain, 24–27 March 2014. WHO Regional Office for the Eastern Mediterranean. Available online: https://www.moh.gov.bh/Content/Files/IHR/documents/new/assessment/IHR%20Assessment%20Mission_Bahrain_%20Final%20Report_%202014.pdf (accessed on 17 July 2025).
- Government of Kuwait. “Basic Vaccinations in Kuwait.” e.gov.kw. Available online: https://e.gov.kw/sites/kgoenglish/Pages/CitizensResidents/Health/BasicVaccinationsInKuwait.aspx (accessed on 17 July 2025).
- Alshishtawy, M.M. Four Decades of Progress Evolution of the health system in Oman. Sultan Qaboos Univ. Med J. [SQUMJ] 2010, 10, 12–22. [Google Scholar] [CrossRef] [PubMed]
- Al-Dahshan, A.; Hammoud, H.; Chehab, M.; Osman, S.R.O. Vaccination coverage in Qatar: Benchmarking with global figures. Qatar Med J. 2019, 4. [Google Scholar] [CrossRef]
- World Health Organization. Expanded Programme on Immunization (EPI) Review. WHO Regional Office for the Eastern Mediterranean. 2011. Available online: https://iris.who.int/bitstream/handle/10665/205034/B4547.pdf (accessed on 17 July 2025).
- Emirates Health Services (n.d.). Child Health and Vaccinations. Emirates Health Services. Available online: https://www.ehs.gov.ae/en/services/services-directory/child-health-and-vaccinations (accessed on 17 July 2025).
- United Nations Children’s Fund (UNICEF). Yemen Vaccination Report. Vaccination in Yemen: Sav-ing lives, Protecting the Economy | UNICEF Yemen. 2022. Available online: https://www.unicef.org/yemen/media/9771/file/YemenVaccinationReport.pdf.pdf (accessed on 17 July 2025).
- World Health Organization. Immunization coverage of children aged 24–35 months in the Islamic Republic of Iran: A national cluster coverage survey. East. Mediterr. Health J. 2022, 28, 139–147. Available online: https://www.emro.who.int/emhj-volume-28-2022/volume-28-issue-2/immunization-coverage-of-children-aged-2435-months-in-the-islamic-republic-of-iran-a-national-cluster-coverage-survey.html (accessed on 17 July 2025).
- World Health Organization; Regional Office for the Eastern Mediterranean. Urgent routine immunization services to resume in Ninewa. (15 June 2020). East. Mediterr. Health J. 2022, 282, 121–129. Available online: https://www.emro.who.int/media/news/urgent-routine-immunization-services-to-resume-in-ninewa.html (accessed on 17 July 2025).
- ThinkWell. Sustainable Immunization Financing: Jordan Country Brief. (October 2023). Available online: https://thinkwell.global/wp-content/uploads/2023/11/Sustainable-Immunization-Financing-Jordan-Country-Brief-October-2023.pdf (accessed on 17 July 2025).
- Gavi, the Vaccine Alliance. Big Catch-Up: Syria Rolls out Initiative to Reach Millions of Children Missed During COVID-19. (12 June 2023). Available online: https://www.gavi.org/news/media-room/big-catch-syria-rolls-out-initiative-reach-millions-children-missed-during-covid-19 (accessed on 17 July 2025).
- World Health Organization, Regional Office for the Eastern Mediterranean. Kuwait Donates $4.6M for Measles Campaign Targeting over 900,000 Children. (15 March 2023). Available online: https://www.emro.who.int/lbn/lebanon-news/kuwait-donates-46m-for-measles-campaign-targeting-over-900000-children.html (accessed on 17 July 2025).
- United Nations Children’s Fund (UNICEF) Lebanon. Routine Immunization Campaign. 2023. Available online: https://www.unicef.org/lebanon/routine-immunization-campaign (accessed on 17 July 2025).
- Gavi, the Vaccine Alliance. Gavi, IFRC and UNICEF Collaborate on Emergency Response in Palestine. (1 November 2023). Available online: https://www.gavi.org/news/media-room/gavi-ifrc-and-unicef-collaborate-emergency-response-palestine (accessed on 17 July 2025).
- United Nations Children’s Fund (UNICEF). Routine Vaccines Are Saving Children’s Lives -in the Gaza Strip. 2023. Available online: https://www.unicef.org/sop/stories/routine-vaccines-are-saving-children-lives (accessed on 17 July 2025).
- Ozcirpici, B.; Aydin, N.; Coskun, F.; Tuzun, H.; Ozgur, S. Vaccination coverage of children aged 12-23 months in Gaziantep, Turkey: Comparative results of two studies carried out by lot quality technique: What changed after family medicine? BMC Public Health 2014, 14, 217. [Google Scholar] [CrossRef]
- Kisa, S.; Kisa, A. Religious beliefs and practices toward HPV vaccine acceptance in Islamic countries: A scoping review. PLoS ONE 2024, 19, e0309597. [Google Scholar] [CrossRef]
- Memish, Z.A.; Zumla, A.; Alhakeem, R.F.; Assiri, A.; Turkestani, A.; Al Harby, K.D.; Alyemni, M.; Dhafar, K.; Gautret, P.; Barbeschi, M.; et al. Hajj: Infectious disease surveillance and control. Lancet 2014, 383, 2073–2082. [Google Scholar] [CrossRef]
- Al-Tawfiq, J.A.; Memish, Z.A. The Hajj 2019 Vaccine Requirements and Possible New Challenges. J. Epidemiol. Glob. Health 2019, 9, 147–152. [Google Scholar] [CrossRef]
- Aemehdoust, Z.; Ahmadnia, S.; Nafici, N. The Experiences of Iranian Women Facing HPV. Soc. Welf. 2025, 25, 45–75. Available online: https://www.magiran.com/p2874255 (accessed on 17 July 2025). [CrossRef]
- Abdelhamed, W.; El-Kassas, M. Hepatitis B virus in Egypt: The whole story. Egypt. Liver J. 2024, 14, 56. [Google Scholar] [CrossRef]
- World Health Organization. Viral Hepatitis. WHO Regional Office for the Eastern Mediterranean. Available online: https://www.emro.who.int/egy/programmes/viral-hepatitis.html (accessed on 17 July 2025).
- Cai, C.-R.; Wu, Z.-X.; Guan, J.-Y. Effect of vaccination strategies on the dynamic behavior of epidemic spreading and vaccine coverage. Chaos Solitons Fractals 2014, 62, 36–43. [Google Scholar] [CrossRef]
- Islam, T.; Mandal, S.; Chouhan, P. Influence of socio-demographic factors on coverage of full vaccination among children aged 12–23 months: A study in Indian context (2015–2016). Hum. Vaccines Immunother. 2024, 17, 5226–5234. [Google Scholar] [CrossRef]
- Cellini, M.; Pecoraro, F.; Rigby, M.; Luzi, D. Comparative analysis of pre-Covid19 child immunization rates across 30 European countries and identification of underlying positive societal and system influences. PLoS ONE 2022, 17, e0271290. [Google Scholar] [CrossRef] [PubMed]
- Pickles, G. Overcoming Barriers to African Vaccine Manufacturing: How to Ensure Sustainable and Scalable Vaccine Production in Africa. MedAccess. 2023. Available online: https://medaccess.org/overcoming-barriers-to-african-vaccine-manufacturing/ (accessed on 17 July 2025).
- WHO Commission on Macroeconomics and Health; World Health Organization. Macroeconomics and Health: In-vesting in Health for Economic Development: Executive Summary/Report of the Commission on Macroeconomics and Health. 2001. Available online: https://iris.who.int/handle/10665/42463 (accessed on 17 July 2025).
- Nature Index. National Vaccine and Serum Institute. Available online: https://www.nature.com/nature-index/institution-outputs/china/national-vaccine-and-serum-institute/521c3621140ba0c63b000000 (accessed on 17 July 2025).
- Anonymous. Moderna feud with NIH over COVID vaccine. Nat. Biotechnol. 2021, 39, 1481. [Google Scholar] [CrossRef] [PubMed]
- Goodwin Law. Racing Against COVID-19: The Regulatory Landscape for Vaccine Development. 2020. Available online: https://www.goodwinlaw.com/en/insights/publications/2020/03/03_06-racing-against-covid19 (accessed on 17 July 2025).
- Lalani, H.S.; Nagar, S.; Sarpatwari, A.; Barenie, R.E.; Avorn, J.; Rome, B.N.; Kesselheim, A.S. US public investment in development of mRNA covid-19 vaccines: Retrospective cohort study. Br. Med. J. 2023, 380, e073747. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health & Human Services. Strategic National Stockpile (SNS). Available online: https://remm.hhs.gov/sns.htm (accessed on 17 July 2025).
- U.S. Food and Drug Administration (FDA). Fast Track. Available online: https://www.fda.gov/patients/fast-track-breakthrough-therapy-accelerated-approval-priority-review/fast-track (accessed on 17 July 2025).
- China Med Device. Fast-Track Channels Established by NMPA—China Med Device. Available online: https://chinameddevice.com/fast-track-channels (accessed on 17 July 2025).
- World Health Organization (WHO). Immunization Agenda 2030: A Global Strategy to Leave No One Behind. 2020. Available online: https://www.who.int/publications/m/item/immunization-agenda-2030-a-global-strategy-to-leave-no-one-behind (accessed on 17 July 2025).
- Ciccacci, F.; Ruggieri, E.; Scarcella, P.; Moramarco, S.; Carestia, M.; Di Giovanni, D.; Silaghi, L.A.; Doro Altan, A.M.; Orlando, S. Between war and pestilence: The impact of armed conflicts on vaccination efforts: A review of literature. Front. Public Health 2025, 13, 1604288. [Google Scholar] [CrossRef]
- Bou-Karroum, L.; Daher, N.; Jabbour, M.; Akhu-Zaheya, L.; Khater, W.; Alloubani, A.; Orach, C.G.; Komakech, H.; Bennett, S.; El-Jardali, F. Assessing the integration of refugee health data into national health information systems in Jordan, Lebanon, and Uganda. Confl Health 2024, 18 (Suppl. S1), 49. [Google Scholar] [CrossRef]
- Swed, S.; Baroudi, I.; Ezzdean, W.; Sawaf, B.; Bohsas, H.; Patwary, M.M. COVID-19 vaccine hesitancy among people in Syria: An incipient crisis. Ann. Med. Surg. (Lond.) 2022, 75, 103324. [Google Scholar] [CrossRef]
- United Nations International Children’s Emergency Fund (UNICEF). Yemen Ministry of Public Health and Population, Gavi, WHO and UNICEF Launch Oral Cholera Vaccination Campaign. 2023. Available online: https://www.unicef.org/yemen/press-releases/yemen-ministry-public-health-and-population-gavi-who-and-unicef-launch-oral-cholera (accessed on 17 July 2025).
- Matlin, S.A.; Smith, A.C.; Merone, J.; LeVoy, M.; Shah, J.; Vanbiervliet, F.; Vandentorren, S.; Vearey, J.; Saso, L. The Challenge of Reaching Undocumented Migrants with COVID-19 Vaccination. Int. J. Environ. Res. Public Health 2022, 19, 9973. [Google Scholar] [CrossRef]
- Harrison, K.; Rahimi, N.; Danovaro-Holliday, M.C. Factors limiting data quality in the expanded programme on immunization in low and middle-income countries: A scoping review. Vaccine 2020, 38, 4652–4663. [Google Scholar] [CrossRef]

| Initiative | Timeline | Countries Involved | Summary | Key Outcomes | Supporting Data/Statistics | Reference |
|---|---|---|---|---|---|---|
| Vaccine Group Purchasing Program | 1985—present | Bahrain, Kuwait, Oman, Qatar, SA, the United Arab Emirates, and Yemen (since 2004) | In 1978, the Gulf states initiated a joint drug tender, which evolved into a group purchasing system for medical products. The group purchasing of vaccines started in 1985 and required member countries to purchase at least 60% of their vaccine needs through the program. |
|
| [103] |
| Meningococcal Vaccination for Hajj and Umrah Pilgrims | 1987—present | SA | Following the 1987 MenA outbreaks, mandatory MenA-C vaccination was implemented for Hajj pilgrims and visitors. Despite this, invasive meningococcal disease (IMD) outbreaks persisted, with notable cases occurring between 1995 and 1999 and 2000 and 2001, mainly due to MenW. From 2002, MenACWY vaccination became mandatory, later switching to a conjugated vaccine. Immunization efforts also expanded to include Saudi residents and infants. |
|
| [104] |
| National Immunization Days (NIDs) | 2006—present | Egypt | Since Egypt was declared polio-free in 2006, two National Immunization Days (NIDs) are conducted annually as part of Egypt’s polio program. WHO, UNICEF, and USAID support the Egyptian Ministry of Health and Population (MoHP) to ensure that all children in Egypt, including vulnerable migrant populations, are protected against polio. |
|
| [9] |
| Introduction of HPV Vaccine | 2008—present | United Arab Emirates | In 2008, Abu Dhabi introduced the HPV vaccine into its immunization program, offering it free to girls aged 15–17 in public and private schools. By 2013, free immunization had been expanded to Emirati women aged 18–26. In 2019, the HPV vaccine was available to schoolgirls aged 13–14. |
|
| [105] |
| Middle East Polio Outbreak Response Plan | 2013–2015 | Egypt, Iran, Iraq, Jordan, Lebanon, Palestine, Syria, and Turkey | Eight national governments partnered with the Global Polio Eradication Initiative (GPEI) to develop a multiphase response plan. Supplementary immunization activities (SIAs) were implemented, including health facility vaccinations, house-to-house visits, transit-point vaccinations, and mobile teams reaching vulnerable and hard-to-reach populations. |
|
| [106] |
| MERS-COV Vaccine Development | 2015—present | SA and the UK | SA’s KAIMRC collaborated with the UK’s Oxford University in 2015 to develop the ChAdOX1 vaccine against MERS-COV, which was successful in mice and camels and can potentially protect humans and camels. Human phase 1 trials have begun in both countries. |
|
| [107] |
| Routine Childhood Immunizations | 1979—present | Jordan | Supported by UNICEF Jordan, the national immunization program, led by the Ministry of Health, routinely provides vaccinations for children residing in the country. |
|
| [108] |
| Inclusive COVID-19 Vaccination Program | 2021—present | Lebanon | In 2021, Lebanon’s COVID-19 vaccination campaign adopted an inclusive approach, covering all residents, including refugees, based on priority categories, such as morbidity and age, regardless of nationality or residency status. The initiative involved the Government of Lebanon, the private sector, the World Bank, UN agencies, and NGOs, with the World Bank reallocating USD 34 million from the Lebanon Health Resilience project and mobilizing additional funds for refugee vaccination. |
|
| [109] |
| Hayat Biotech Company | 2021—present | UAE and China | Hayat Biotech is a joint venture between Sinopharm CNBG and G42, a company based in Abu Dhabi. The company focuses on life sciences, biotechnology, and vaccine production, supporting global health security and sustainability. They produced the Hayat-Vax vaccine, the first COVID-19 vaccine in the Middle East, and maintained a strategic stockpile to ensure readiness for future needs. |
|
| [110,111] |
| Sadeer City Vaccine and Vital Medicines Factory | 2023—present | SA | The Saudi Authority for Industrial Cities and Technology Zones (Modon) has partnered with the Vaccine Industrial Company to establish a factory in Sadeer City for the manufacture of vaccines and vital medicines, with an investment of USD 133 million. This initiative aims to strengthen pharmaceutical security and localize vaccine production, including those for seasonal flu, COVID-19, chickenpox, pneumococcal, and meningitis. |
|
| [112] |
| Country | Income-Level | Global Peace Index (GDI) Ranking | Major Funding source | Gavi Eligibility | Reference |
|---|---|---|---|---|---|
| Bahrain | High Income | Medium 108 | Fully government-funded | Not Eligible | [69,120,121,122] |
| Kuwait | High Income | High 35 | Fully Government-Funded | Not Eligible | [69,120,121,123] |
| Oman | High Income | High 48 | Government-Funded | Not Eligible | [69,120,121,124] |
| Qatar | High Income | High 21 | Fully Government–Funded | Not Eligible | [69,120,121,125] |
| Saudi Arabia | High Income | Medium 119 | fully government-funded | Not Eligible | [69,120,121,126] |
| United Arab Emirate | High income | Medium 75 | fully government-funded | Not Eligible | [69,120,121,127] |
| Yemen | Low income | Very Low 162 | Gavi, The Vaccine Alliance | Eligible | [69,120,121,128] |
| Egypt | Low-Middle Income | Medium 121 | Government-Funded, excluding Campaigns which are funded by WHO, UNICEF and USAID | Not Eligible | [9,69,120,121] |
| Iran | High-Middle Income | Low 147 | Government-Funded | Not Eligible | [69,120,121,129] |
| Iraq | High-Middle income | Very Low 154 | Ministry of Health supported by the WHO and UNICEF | Not Eligible | [69,120,121,130] |
| Jordan | Low-Middle Income | High 62 | Government-Funded | Not Eligible | [69,120,121,131] |
| Syria | Low Income | Very Low 161 | Gavi, The Vaccine Alliance | Eligible | [69,120,121,132] |
| Lebanon | Low-Middle Income | Low 135 | Government-Funded, Campaign Support Kuwait Fund & humanitarian donors via MOPH + WHO/UNICEF | Not Eligible | [69,120,121,133,134] |
| Palestine | Low-Middle Income | Low 134 | Government-Funded, Campaign Support WHO, UNICEF, Gavi. | Not Eligible | [69,120,121,135,136] |
| Turkey | High-Middle Income | Low 147 | Government-Funded | Not Eligible | [69,120,121,137] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
AL-Eitan, L.N.; Almahdawi, D.L.; Abu Khiarah, R.A.; Alghamdi, M.A. Bridging Gaps in Vaccine Access and Equity: A Middle Eastern Perspective. Vaccines 2025, 13, 806. https://doi.org/10.3390/vaccines13080806
AL-Eitan LN, Almahdawi DL, Abu Khiarah RA, Alghamdi MA. Bridging Gaps in Vaccine Access and Equity: A Middle Eastern Perspective. Vaccines. 2025; 13(8):806. https://doi.org/10.3390/vaccines13080806
Chicago/Turabian StyleAL-Eitan, Laith N., Diana L. Almahdawi, Rabi A. Abu Khiarah, and Mansour A. Alghamdi. 2025. "Bridging Gaps in Vaccine Access and Equity: A Middle Eastern Perspective" Vaccines 13, no. 8: 806. https://doi.org/10.3390/vaccines13080806
APA StyleAL-Eitan, L. N., Almahdawi, D. L., Abu Khiarah, R. A., & Alghamdi, M. A. (2025). Bridging Gaps in Vaccine Access and Equity: A Middle Eastern Perspective. Vaccines, 13(8), 806. https://doi.org/10.3390/vaccines13080806






