2. Materials and Methods
2.1. Study Participants
This cross-sectional study was conducted at the Translational and Experimental Clinical Research Center in Oral Health, within the Clinic of Preventive, Community Dentistry, and Oral Health at the University of Medicine and Pharmacy “Victor Babes,” Timișoara, Romania. The study took place between February and March 2024 and included 199 young adults, all dental medicine students enrolled in the second, fifth, and sixth years of study. Dental education in Romania is a 6-year integrated undergraduate program aligned with EU directives, combining preclinical coursework and clinical training. Upon graduation, students earn a Doctor of Dental Medicine (DMD) degree, qualifying them to practice general dentistry. Postgraduate specialization, regulated by the Ministry of Health, is available through competitive national residency programs lasting three years. Independent practice requires registration with the Romanian College of Dentists, the national regulatory authority.
To ensure adequate representation of the target population, a sample size calculation was performed prior to data collection. Using the finite population correction formula for proportions and considering an estimated total of 600 dental students enrolled in the Romanian section of the faculty, the minimum required sample size was calculated to be 234 participants. The parameters applied included a 95% confidence level, a 5% margin of error, and an assumed response distribution of 50% to account for maximum variability. Although the final sample comprised 199 students, this number represents over 85% of the estimated target and remains within an acceptable range for a cross-sectional observational study conducted under voluntary participation conditions [
34,
35].
Participants completed a 15-item questionnaire assessing their knowledge about human papillomavirus (HPV), vaccination status, systemic conditions, chronic inflammatory diseases, and smoking habits. Information regarding HPV vaccination status was self-reported by participants through the questionnaire, indicating whether they had received the vaccine or not. The questionnaire was adapted from previously validated tools used in similar studies assessing HPV knowledge among medical and dental students [
8,
36]. It was reviewed by three dental public health experts for clarity, content validity, and cultural relevance. A pilot version was tested on 15 students to ensure understanding and face validity. Minor linguistic and structural adjustments were made based on this feedback.
Students were divided into three main groups: 58 second-year students, 59 fifth-year students, and 82 sixth-year students. These specific year groups were selected using a convenience sampling approach to ensure a representative mix of junior and senior students. This selection was deliberate to reflect the progression through distinct stages of dental education. Second-year students represent the preclinical phase, primarily focused on theoretical foundations. Fifth-year students are typically immersed in clinical rotations, while sixth-year students are transitioning toward graduation and independent professional practice. This academic stratification enabled a comparative analysis of HPV-related knowledge and attitudes across different levels of training.
Recruitment was conducted during scheduled university sessions, and all eligible students present were invited to participate on a voluntary basis.
Information about the study was provided in person by trained members of the research team during regular academic courses. Participation was entirely voluntary, and no financial or academic incentives were offered. Students who agreed to participate signed a written informed consent form and were included only if they completed both the questionnaire and the saliva sample collection.
The primary variables of the study were HPV vaccination status and knowledge about HPV. The independent variables included the year of study and immunization status. For the purpose of this study, junior dental students were defined as those in the second year, while senior students included those in the fifth and sixth years. Additionally, the study aimed to assess students’ opinions and attitudes toward HPV prevention measures, as well as their confidence in clinical examinations for cancer detection.
For the purpose of age-based comparisons, participants were classified into two groups: those under the age of 25 (152 students, 76.4%) and those aged 25 or older (47 students, 23.6%). This categorization aligns with the structure of Romanian dental education, where students aged 25 and above are generally in the final years of their undergraduate program or are preparing for postgraduate specialization examinations. Although the average age of respondents was 23.5 years, those in the older age group are more likely to exhibit higher levels of clinical maturity and autonomy in health-related decision-making. These factors may influence their perspectives and behaviors concerning HPV prevention and vaccination.
This study complied with the ethical guidelines set forth in the World Medical Association’s Declaration of Helsinki (1964). Approval was granted by the Ethical Committee of the University of Medicine and Pharmacy “Victor Babes”, Timisoara, Romania (No. 15/15.01.2024). Participation was entirely voluntary, and all participants provided informed consent by reading and signing the consent form. Inclusion criteria comprised dental students enrolled in the 2nd, 5th, or 6th year who provided informed consent. Exclusion criteria included refusal to provide saliva samples or incomplete questionnaire responses.
In addition to assessing HPV-related knowledge, attitudes, and vaccination behaviors through a structured questionnaire, the study included a complementary biological investigation component. Specifically, participants were also subjected to salivary screening aimed at detecting HPV genotypes. This methodological integration allowed for a more robust and multidimensional analysis, facilitating the correlation between self-reported awareness and actual infection status. The inclusion of molecular testing reflects the study’s broader objective of bridging the gap between perceived and biological risk among future dental professionals.
2.2. Saliva Collection
Saliva samples were collected from consenting participants using a small, pre-labeled sterile Eppendorf collection tube. To standardize conditions and minimize contamination, participants were instructed to refrain from consuming food and beverages (except water) for at least two hours prior to sample collection. Additionally, smokers were advised to abstain from smoking for at least one hour before sampling, and oral hygiene procedures were avoided during the same period [
37].
To prevent DNA degradation, all samples were stored at low temperatures immediately after collection. Samples were immediately stored at 4 °C and subsequently frozen at −80 °C until DNA extraction. All samples were coded anonymously, and data were matched to questionnaires using unique IDs to preserve confidentiality. Each sample was assigned a unique, randomly generated identification number to eliminate analysis bias. Simultaneously, questionnaire data corresponding to each participant were recorded. The samples were then centrifuged at 4000×
g for 8 min at 4 °C. Following centrifugation, the resulting pellet was resuspended in 10 mL of sterile normal saline buffer and stored at −80 °C for subsequent DNA purification [
18].
2.3. Salivary DNA Isolation and HPV Genotyping Protocol
Before nucleic acid extraction, the samples (1 mL each) were centrifuged for 15 min at 15,000×
g. The resulting pellet was resuspended in 200 µL of lysis buffer. Nucleic acid isolation was performed using the Applied Biosystems MagMAX™ Viral/Pathogen II kit for automated extraction with the KingFisher™ Flex instrument (Applied Biosystems, Waltham, MA, USA). Following nucleic acid extraction, DNA concentration was quantified using a NanoDrop One spectrophotometer (Thermo Scientific, Waltham, MA, USA), and 50 ng of salivary DNA was used per PCR reaction. For genotyping, sample amplification was carried out by RT-PCR using the Allplex™ HPV28 kit (Seegene Inc., Seoul, South Korea), according to the manufacturer’s instructions. This multiplex assay allows the simultaneous amplification of target DNA from 14 high-risk human papillomavirus (HPV) types (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68, 26, 53, 69, 73, 82) and 9 low-risk HPV types (6, 11, 40, 42, 43, 44, 54, 61, 70). DNA purity was assessed by measuring the absorbance ratio at 260/280 nm using a NanoDrop One spectrophotometer (Thermo Scientific), with acceptable values ranging between 1.8 and 2.2. β-actin was used as an internal control to verify amplification integrity. All reactions were performed in an Eppendorf thermal cycler under the following conditions: initial denaturation at 95 °C for 8 min, followed by 35 cycles of 95 °C for 45 s, 56 °C for 30 s, and 72 °C for 30 s, with a final extension at 72 °C for 7 min [
38,
39].
2.4. Statistical Analysis
A structured statistical approach was utilized to assess the relationship between demographic characteristics, lifestyle factors, and awareness levels in relation to HPV vaccination status. Descriptive statistical methods were initially applied to summarize the dataset, including frequency distributions, means, and standard deviations. Correlation analysis was conducted to examine potential associations between key variables, while categorical variables were analyzed using cross-tabulations. The correlation coefficient “r” refers to Pearson correlation. As recommended, we performed a Shapiro–Wilk normality test on the numerical variables prior to applying Pearson correlation. The results confirmed a normal distribution (p > 0.05), supporting the use of parametric correlation methods. Percentages were calculated to identify patterns related to smoking status, awareness levels, and HPV vaccination uptake.
The data were initially entered and organized using Microsoft Excel, which served as the primary platform for data entry and preliminary formatting. This step ensured a clean and structured dataset that could be seamlessly imported into statistical software for further analysis.
To determine the predictors of HPV vaccination, a logistic regression model was implemented, incorporating independent variables such as age, sex, smoking status, and awareness of HPV-related risks. The regression model outputs, including coefficients, standard errors, p-values, and confidence intervals, were examined to assess statistical significance.
To facilitate data interpretation, graphical representations such as histograms, stacked bar charts, and a correlation heatmap were generated. All statistical analyses and tests were conducted using Python (version 3.11), employing libraries for data processing, visualization, and regression modeling, including Matplotlib (version 3.7.1). Additionally, MedCalc Statistical Software (version 22.013) was used for result validation, ensuring both accuracy and reproducibility. All statistical tests were two-tailed, with a significance threshold set at p < 0.05. No adjustments for multiple comparisons were made, given the exploratory nature of the study.
This rigorous statistical approach provided a robust analytical framework for evaluating factors associated with HPV vaccination status, enabling a comprehensive understanding of the variables influencing vaccination uptake.
3. Results
3.1. Participant Demographics and Health Status
The study included 199 participants, with an average age of 23.5 (±2.6) years. The majority of respondents were female, accounting for 79.4% of the sample, while males represented 20.6%. The distribution of ages was concentrated primarily in the early-to-mid-twenties, with some variability among participants. A small proportion (4%) of participants reported experiencing current health issues. Chronic conditions such as heart disease, lung disease, kidney disease, diabetes, anemia, or neurological disorders were noted in 5% of cases. Additionally, 10.6% of participants reported known allergies to food or medication, while 2.5% indicated previous severe adverse reactions to vaccinations (
Table 1).
3.2. Smoking Behavior and Medical Background
Among the participants, 31.2% reported current smoking behavior. When analyzed by gender, smoking was more prevalent among male students (45.7%) compared to female students (25.4%), indicating a gender-related difference in tobacco use patterns within the study population.
The use of immunosuppressive therapy was absent among all participants, as no individuals reported taking medications such as cortisone, prednisone, or other steroids within the past three months. Additionally, no respondents had received a blood transfusion in the past year. None of the female participants were pregnant or breastfeeding at the time of the survey.
3.3. HPV Vaccination Rates and Awareness
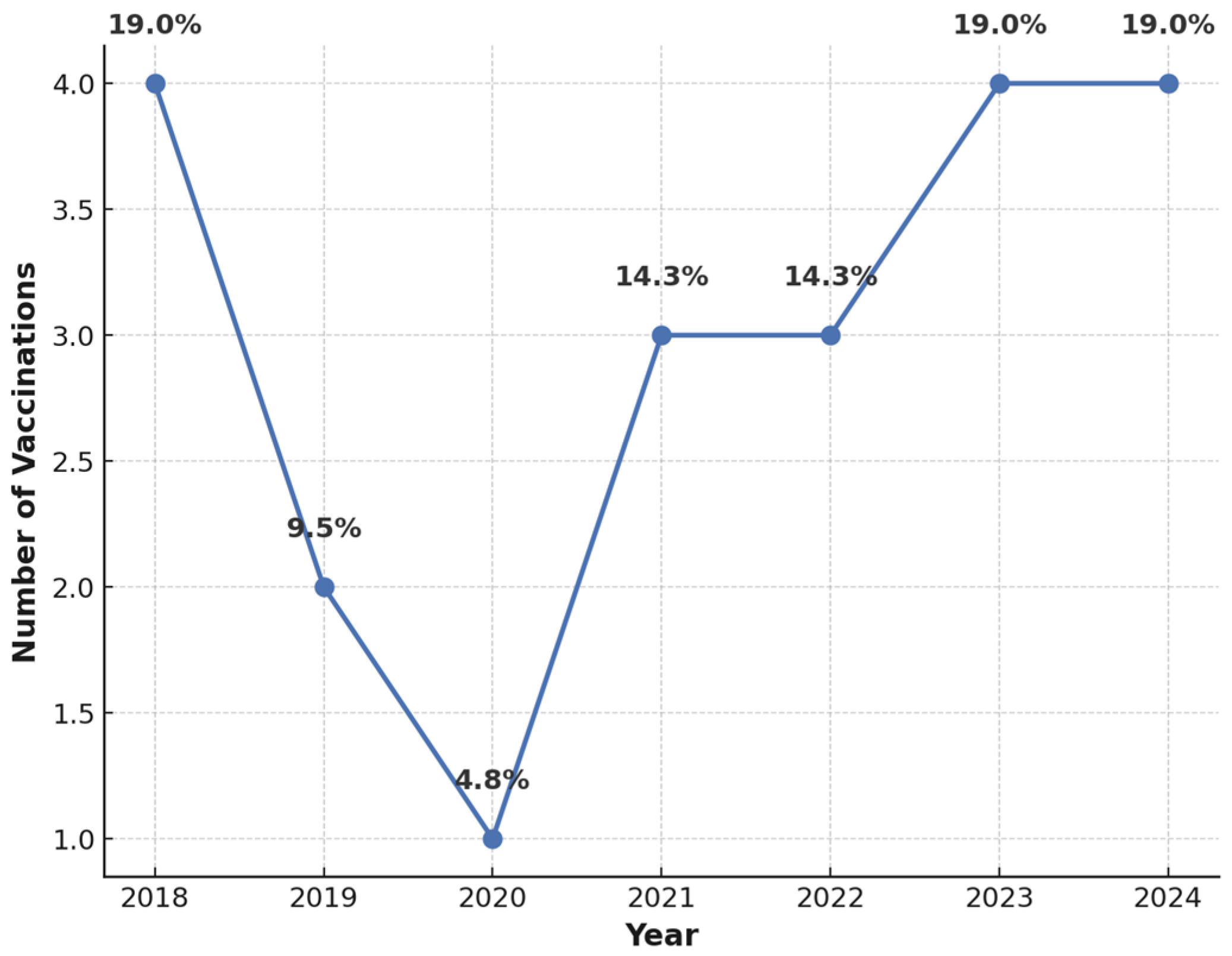
The analysis of HPV vaccination rates revealed a relatively low uptake, with only 10.6% of participants having received the HPV vaccine. Among vaccinated individuals, immunization predominantly took place in 2023 and 2024, suggesting increased awareness in recent years (
Figure 1). Despite low vaccination rates, 96.9% of participants acknowledged the safety and efficacy of HPV vaccination in cancer prevention. Furthermore, 94.5% believed that vaccinated individuals could no longer transmit the virus within the community.
3.4. Age and Gender Differences in Awareness and Vaccination
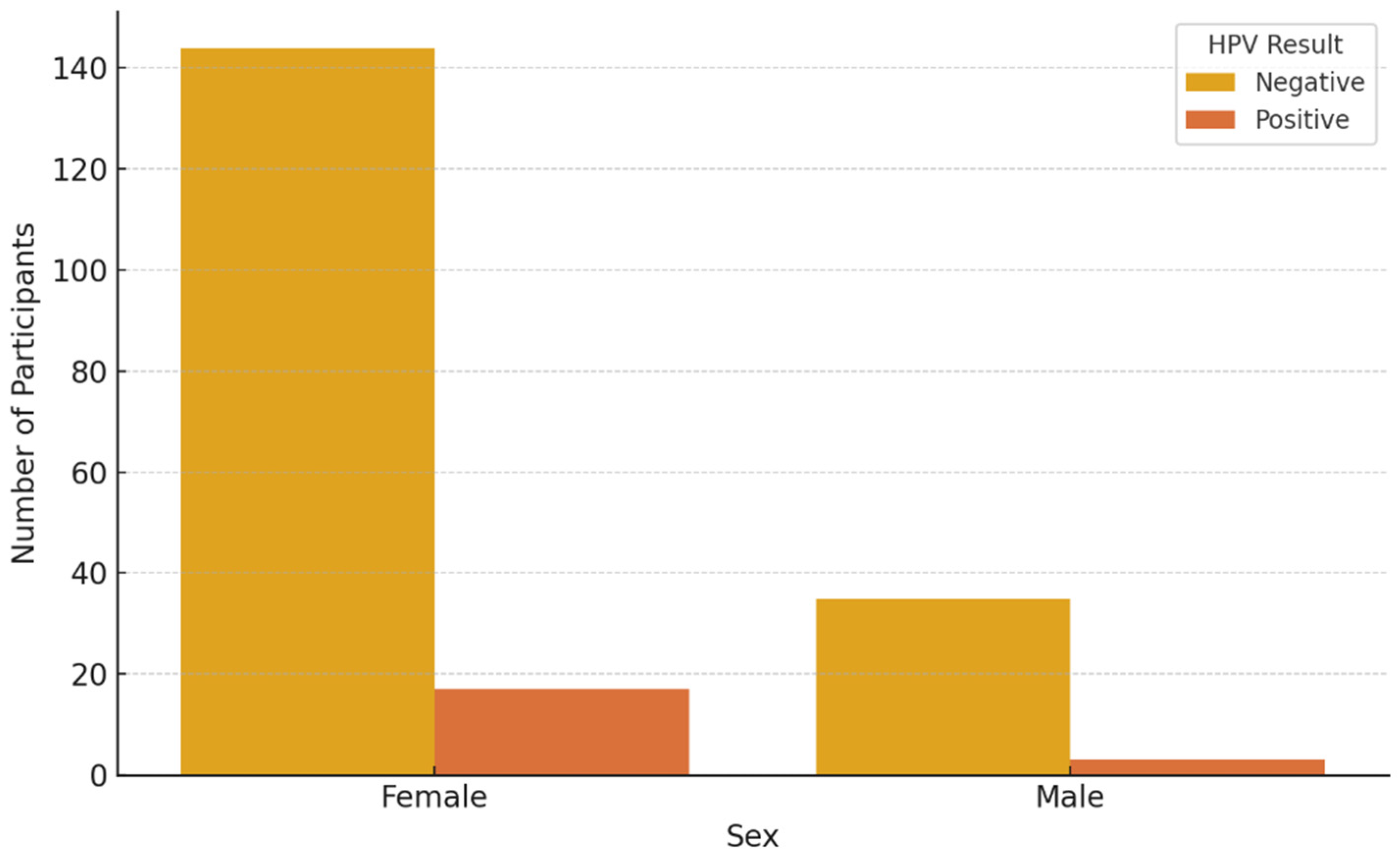
Salivary screening revealed that 10% of the participants tested positive for HPV types, underscoring the potential utility of saliva-based diagnostics as a non-invasive tool for early detection of HPV infections among asymptomatic young adults.
Among the participants, HPV vaccination uptake was low, with only 10.6% reporting having received the vaccine. When disaggregated by gender, 8.5% of the total sample were vaccinated females, while only 2.0% were vaccinated males. This gender-based difference was statistically significant (p = 0.0123), indicating that female students were more likely to be vaccinated.
Regarding smoking habits, a significant difference was observed (
p = 0.0456), with the smoking rate among males (45.7%) being significantly higher than that recorded among females (25.4%). HPV awareness, however, did not differ significantly between genders (
p = 0.0789), although slightly more females (88.1%) were aware of HPV vaccination compared to males (84.3%) (
Table 2).
When analyzing vaccination rates by age, participants were categorized into two groups: those under 25 years old and those 25 years or older. A significant association was found between age group and vaccination status (p = 0.0312), with younger students (<25 years) having a higher vaccination rate (68.4%) compared to 50.0% among older students. Smoking rates did not differ significantly between age groups (p = 0.0678), with younger students reporting a 29.5% smoking rate compared to 34.8% among older students.
A statistically significant difference in HPV awareness levels was observed between age groups (
p = 0.0234), with 89.6% of younger students demonstrating awareness compared to 72.4% of older students (
Table 3).
3.5. Family History and Wart Incidence
Among the surveyed participants, 31.7% reported having a family history of cancer. Of these, various cancer types were identified, including breast, colon, cervical, and pulmonary cancers, among others. Among participants with a family history of cancer (representing 31.7% of the sample), only 15.9% of this subgroup reported having received the HPV vaccine. This indicates that an elevated familial cancer risk did not translate into increased vaccination uptake. Clarifying this distinction, we note that the 15.9% refers specifically to those with a family history of cancer, not the entire study population. Notably, just 15.9% of those with a family history of cancer were vaccinated, indicating no increase in uptake among higher-risk individuals. When analyzed by sex, 12.0% of female participants were vaccinated, compared to only 4.9% of males. This disparity highlights a potential gap in targeted preventive strategies, especially among men, and emphasizes the importance of tailored health education and vaccination efforts across gender lines.
A total of 16.6% of participants reported the presence of papillomas or warts, highlighting the relevance of early screening and preventive vaccination efforts. Among these individuals, the majority were female (78.8%), while males accounted for 21.2% of cases.
Among the 199 participants, 20 individuals (10%) tested positive for high-risk HPV strains (types 16 or 18) via salivary PCR analysis. Of these 20 HPV-positive individuals, 18 had not received any dose of the HPV vaccine. The remaining two positive cases were among vaccinated individuals, both of whom had received only one dose of the vaccine, administered within six months prior to sample collection.
Figure 2 and
Figure 3 present HPV PCR test results stratified by age and sex, respectively, showing demographic variation in viral detection rates.
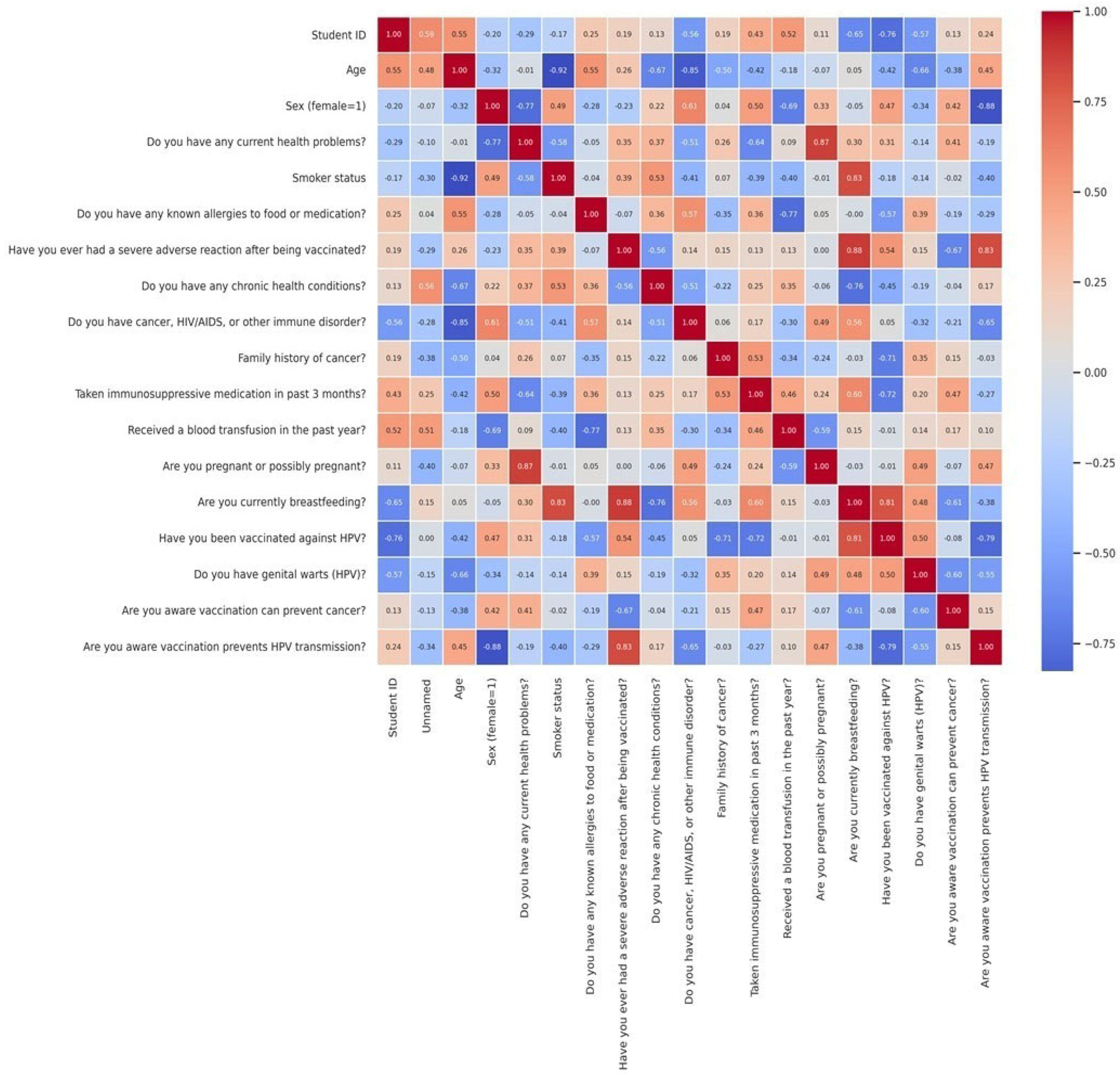
The correlation matrix provided insights into the degree of association between various factors influencing HPV vaccination status. While most variables exhibited weak correlations, notable patterns emerged in terms of lifestyle factors and vaccine uptake. A cross-tabulation analysis of smoking status and HPV vaccination suggested potential differences in vaccine uptake between smokers and non-smokers, likely reflecting variations in health awareness, risk perception, or healthcare-seeking behaviors. The correlation analysis revealed predominantly weak to moderate relationships among the investigated variables related to health status and HPV vaccination knowledge. A moderate positive correlation was identified between awareness that HPV vaccination can prevent cancer and the understanding that it reduces viral transmission (r = 0.52). Furthermore, the presence of chronic health conditions was moderately associated with recent use of immunosuppressive medication (r = 0.47) and with a history of blood transfusion (r = 0.43), indicating that these variables co-occurred more frequently within the same individuals. Conversely, demographic variables such as age and sex demonstrated weak correlations with key outcome variables, including HPV vaccination status (r = 0.12 for age, r = −0.08 for sex), indicating limited predictive value in this sample. The correlation between having been vaccinated against HPV and the presence of genital warts was also low (r = −0.15) (
Figure 4).
While the correlation matrix provides insight into potential associations, it is important to note that most correlations were weak and did not reach statistical significance. The matrix was included as an exploratory tool to visualize overall trends, not to infer causality.
The logistic regression analysis identified several significant predictors of HPV vaccination status. Smoking status was the strongest positive predictor (β = 1.49, OR = 4.44, p = 0.0045), indicating that smokers were over four times more likely to be vaccinated compared to non-smokers. Belief in the safety and cancer-preventive efficacy of the HPV vaccine was also positively associated with vaccine uptake (β = 1.29, OR = 3.63, p < 0.05). Female sex showed a moderate association (β = 1.01, OR = 2.74), suggesting a trend toward higher vaccination rates among women, though this did not reach statistical significance. Age demonstrated a minimal effect (β = 0.07, OR = 1.07, p > 0.05), indicating that it was not a meaningful predictor in this model. Interestingly, belief that HPV vaccination reduces community-level viral transmission was negatively associated with vaccination status (β = −0.82, OR = 0.44). The model intercept was negative (β = −2.12), reflecting a generally low baseline probability of vaccination in the absence of these influencing factors.
Participant perceptions of HPV vaccination were examined in relation to three key domains: beliefs about vaccine safety and efficacy, perceptions regarding the vaccine’s impact on viral transmission, and intentions for future vaccination.
When asked whether they believed that HPV vaccination was safe and effective in preventing cancer, 76.2% of participants responded affirmatively, while 13.2% disagreed and 10.6% were uncertain. Stratified by sex, 81.0% of female respondents believed in the vaccine’s safety and efficacy, compared to 61.0% of males. Meanwhile, 10.1% of females and 24.4% of males responded “no”, and 8.9% of females versus 14.6% of males indicated uncertainty. These findings suggest greater confidence in HPV vaccination among women, whereas male participants exhibited a higher degree of skepticism or lack of awareness.
A similar pattern emerged when participants were asked whether they believed that vaccinated individuals could no longer transmit HPV within the community. In total, 79.4% responded “yes”, 13.1% said “no”, and 7.5% were unsure. Among females, 82.9% believed vaccination prevents transmission, compared to 65.9% of males. Conversely, 10.8% of females and 22.0% of males disagreed, while 6.3% and 12.2%, respectively, were unsure. Although general awareness of HPV vaccine benefits was high, these results underscore persistent sex-based differences in perception, with men showing more doubt or misinformation.
Regarding future vaccination intent, 49.2% of all participants expressed willingness to receive the HPV vaccine, 12.6% reported no intention, and 27.1% were uncertain. Additionally, 10.6% stated that they had already been vaccinated. Among women, 48.1% intended to receive the vaccine, 11.4% did not, and 27.8% were unsure. Among men, 53.7% expressed intent, 17.1% declined, and 24.4% were undecided. While intention to vaccinate appears relatively strong—especially among men—the considerable proportion of undecided participants, together with the observed inconsistencies, highlights the need for clearer communication and targeted educational efforts to support informed decision-making.
These results are summarized in
Table 4, which presents HPV PCR results, vaccination status, and perceptions regarding vaccine safety, efficacy, and transmission prevention stratified by gender.
4. Discussion
The rising prevalence of HPV-positive oral cancers, along with the shifting demographic patterns of affected individuals, highlights the growing importance of preventive measures within dental practice. Dentists are uniquely positioned to contribute to the early identification and prevention of HPV-related oral malignancies through patient education, risk assessment, and routine screening for (pre)malignant lesions. Addressing topics such as HPV transmission and safe sexual practices can play a key role in curbing the increasing trend of HPV-associated oral cancers.
Given their evolving role as future oral health professionals, dental students represent a strategically significant population for targeted HPV prevention initiatives. Their academic training extends beyond the oral cavity to encompass broader medical knowledge, including systemic diseases, immune status, and behavioral risk factors. This positions them uniquely to provide holistic health education, addressing HPV transmission, vaccine benefits, and its association with both oropharyngeal and other HPV-related malignancies. As emphasized by Lipsky et al., dental professionals are increasingly recognized as key stakeholders in HPV-related cancer prevention—not only through clinical screenings, but also via routine patient interactions that offer opportunities for counseling and public health guidance [
40]. Assessing students during their formative academic years underscores the urgency of integrating comprehensive HPV education and communication training into dental curricula, empowering them to become proactive advocates for vaccination and early detection across healthcare settings.
However, multiple studies have shown that healthcare students, including those in dental and medical fields, often possess limited knowledge regarding oral cancer and its risk factors, indicating a clear need for improved educational strategies in this area.
Our study focused on screening the saliva of healthy dental students aged 18–25 from the Victor Babeș University of Medicine and Pharmacy in Timișoara for the presence of HPV. Additionally, it aimed to raise awareness among participants regarding the role of HPV 16 and 18 subtypes in oral cancers, as well as the benefits of vaccination, which is strongly recommended for this age group. In our study, the vast majority of dental students (96.9%) acknowledged the safety and efficacy of the HPV vaccine, and 94.5% believed that vaccinated individuals could no longer transmit the virus. Despite this high level of awareness, actual vaccination uptake remained low, with only 10.6% of participants reporting having received the HPV vaccine. Notably, vaccination rates were significantly higher among younger students and females.
Although general awareness regarding HPV and its link to cancer was relatively high, the gap between knowledge and preventive behavior underscores the presence of external barriers, such as accessibility, vaccine hesitancy, or insufficient emphasis on vaccination in the dental curriculum. These findings align with prior research highlighting poor vaccination rates among dental students despite moderate to high levels of awareness [
41].
Additionally, the moderate associations between chronic health conditions, recent use of immunosuppressive medications, and history of blood transfusions may reflect a clustering of health vulnerability indicators. These overlaps suggest the presence of a medically at-risk subgroup within the student population, warranting closer attention in preventive strategies and health education programs.
Reducing tobacco and alcohol consumption, along with maintaining a healthy diet, may lower the risk of oral HPV infections [
36,
42]. The development of HPV vaccines has brought significant hope for the prevention of related cancers. However, there is still a concerning lack of awareness, even among medical students. The level of awareness regarding HPV infection and vaccination among dental students in our study, although relatively high in terms of general knowledge, did not translate into equally high vaccination uptake. Only 10.6% of participants had received the HPV vaccine, a rate comparable to previous findings among healthcare students in regions such as Malaysia (3.6%) and Hong Kong (13.3%) [
36,
42]. Despite nearly all students acknowledging the efficacy and safety of the vaccine, a notable gap persists between knowledge and behavior, suggesting that informational awareness alone is not sufficient to drive vaccination. This may reflect structural or perceptual barriers such as limited access to vaccination services, concerns about side effects, or sociocultural hesitation related to HPV’s transmission route. Similarly to findings from other studies [
13,
43], our results demonstrated a significant association between academic year and HPV awareness, with senior students displaying higher levels of knowledge, likely due to greater exposure to clinical training and curricula addressing cancer prevention, reflect a consistent pattern of health literacy in this subgroup, particularly regarding the understanding of HPV vaccination as a preventive measure against both viral transmission and cancer development.
Interestingly, while no significant gender-based difference was observed in HPV knowledge, female students showed higher vaccination rates, echoing trends reported in other populations [
44]. Beyond vaccination uptake observed among female participants, the data also indicated a greater frequency of self-reported wart presence in this subgroup. While this may suggest potential biological differences in HPV manifestation between sexes, it is equally plausible that the disparity reflects gender-specific patterns in symptom perception, health literacy, or the propensity to seek medical evaluation [
45]. The results of the current study resonate with prior multinational data indicating that while knowledge of HPV and its link to oropharyngeal cancers is variable, many dental students express a willingness to receive training and expand their understanding. In the study by Lingam et al., Indian students displayed the highest awareness levels, likely due to their increased clinical exposure to HPV-related conditions, as India holds one of the highest global burdens of oral cancers. Notably, female students across all surveyed countries demonstrated more favorable attitudes toward HPV vaccination and were more comfortable discussing HPV-related topics with patients compared to males, a finding attributed in part to greater awareness about HPV’s role in cervical cancer and the influence of gendered communication dynamics in healthcare [
10]. Despite a generally high level of awareness regarding the benefits of HPV vaccination, our findings highlight persistent sex-based disparities in perception and confidence, with male participants demonstrating higher levels of uncertainty or susceptibility to misinformation.
Previous studies from countries such as Saudi Arabia and Malaysia have shown that students commonly receive information about HPV through formal education, the internet, and media sources—highlighting the influence of multiple channels in shaping awareness [
36,
44].
Our study findings align with previous Romanian research in recognizing a strong correlation between students’ academic level and their awareness of HPV and related health risks. For instance, Murariu et al. [
46] reported that fifth-year dental students and residents had significantly greater knowledge of oral cancer and HPV infection compared to fourth-year students, primarily due to curriculum exposure during the clinical years. Similarly, our results show that senior dental students had higher awareness and vaccination rates than junior students, reinforcing the importance of curricular timing in shaping preventive health knowledge. Consistent with our findings, previous research among Spanish dental students showed that clinical-level students demonstrated significantly higher levels of knowledge regarding the HPV–oropharyngeal cancer link and HPV vaccination compared to preclinical peers. In that study, clinical students outperformed in 12 out of 16 knowledge items related to oral HPV, and in all vaccination-related items, with statistically significant differences across the board. This reinforces the argument that exposure to clinical disciplines like oral pathology and public health is critical for building competent future practitioners who are capable of promoting HPV prevention [
12].
While Murariu et al. [
46] found that 81.8% to 82.5% of students acknowledged the existence of the HPV vaccine, only 23.4% to 34.9% believed it could prevent oral cancer, indicating a significant knowledge gap regarding HPV’s oncogenic potential beyond cervical cancer. In our study, despite high levels of general awareness (over 96% recognized the cancer-preventive benefit of the vaccine), actual vaccination uptake was notably lower (10.6%). This mismatch between knowledge and action reflects similar challenges in translating awareness into preventive behavior and may be influenced by accessibility, cultural perceptions, or lack of institutional emphasis on vaccination. The progressive development and approval of HPV vaccines have played a critical role in reducing the global burden of HPV-related diseases, particularly cervical cancer. Since 2007, bivalent and quadrivalent vaccines have been available in Europe, targeting HPV types 16 and 18, which are responsible for approximately 70% of cervical cancer cases [
47,
48]. These formulations also provide partial cross-protection against other high-risk types such as HPV 31, 33, and 45. Moreover, the quadrivalent vaccine extends protection to low-risk HPV types 6 and 11, which are linked to 90% of benign genital warts and cases of recurrent respiratory papillomatosis. In an effort to increase vaccine uptake and compliance, the originally recommended three-dose schedule was reduced to two doses for adolescents in 2014. The approval of the nonavalent vaccine by the European Medicines Agency in 2015, which covers five additional oncogenic HPV types (31, 33, 45, 52, and 58), has further expanded protection, raising the potential prevention of cervical cancer from approximately 70% to 90% [
17].
Moreover, this discrepancy between high knowledge and low vaccine uptake may also reflect the influence of misinformation or insufficient confidence in specific vaccine benefits, particularly in relation to oropharyngeal cancer prevention.
Despite being future healthcare providers, many medical students in Romania exhibit incomplete knowledge and varying degrees of HPV vaccine hesitancy. Prior studies have shown that awareness alone may not translate into vaccine acceptance. Psychological and motivational factors often override factual understanding. For example, while Voidăzan et al. (2016) found relatively high awareness of HPV among Romanian medical students, actual understanding and vaccine uptake remained low [
27]. Similarly, Grigore et al. (2018) reported that fewer than 40% of surveyed Romanian women had been vaccinated, citing low awareness and limited confidence in vaccine efficacy [
49]. These findings highlight a crucial need for tailored educational and behavioral strategies that address not only informational gaps but also emotional and trust-related barriers.
Comparatively, the study by Dincă et al. (2024) [
50] emphasized dental students’ gaps in understanding vaccine-preventable diseases (VPDs), with only 45.1% correctly identifying HPV as vaccine-preventable. Our cohort showed higher HPV awareness, suggesting potential differences in institutional focus or educational strategies. However, similar to Dincă et al. [
50], we observed that younger students and those earlier in their education demonstrated less accurate knowledge about HPV, underlining a systemic need for earlier and more comprehensive integration of HPV-related content in dental curricula. Furthermore, while Dincă et al. noted reluctance among students to treat patients with chronic viral infections like HIV due to high perceived risk. This indicates that, despite theoretical knowledge, there may be a lack of preparedness for patient communication on sensitive topics—an area requiring attention through practical training and role-play scenarios during clinical education. One limitation of this study is the low representation of male participants, who accounted for only 20.6% of the sample. This gender imbalance reflects the actual demographic composition of the dental student population at our institution during the time of data collection, where female enrollment was substantially higher. However, it may limit the generalizability of findings related to sex-based differences in HPV knowledge, attitudes, and vaccine uptake. The underrepresentation of male perspectives could introduce bias, especially when interpreting male-specific barriers to vaccination or health communication patterns. Future research should aim to include more balanced samples to validate and expand these findings. This underlines the critical role of universities in structuring effective educational interventions. However, the relatively low self-reported intention to vaccinate among students, despite high awareness, signals a need for targeted educational programs that not only inform but also actively address misconceptions and barriers to vaccine uptake. Moreover, although the overall intention to vaccinate appeared relatively favorable, particularly among male participants, a substantial proportion of respondents remained undecided. This hesitation, when viewed alongside the observed discrepancies between HPV-related knowledge and actual vaccination behavior, underscores the necessity for more nuanced communication strategies and the development of evidence-informed educational interventions to support informed and autonomous decision-making among future dental professionals. Reinforcing HPV-related content in the preclinical dental curriculum, coupled with stronger recommendations from healthcare providers, may enhance students’ readiness to both receive and advocate for vaccination. This is especially relevant as dental professionals increasingly become key figures in the early detection and prevention of HPV-related oropharyngeal cancers.
However, the contrast between high awareness and low vaccination uptake suggests the presence of external barriers such as limited accessibility, concerns about potential side effects, or misinformation contributing to vaccine hesitancy.
An important aspect that emerged from our findings is the potential role dental professionals can play in HPV-related cancer prevention, particularly through patient education and early detection strategies. However, despite the acknowledged importance of HPV prevention, students’ confidence in discussing HPV-related topics with patients remains an area requiring further development. This hesitancy, often observed in culturally conservative contexts, may be influenced by discomfort in addressing sexually transmitted infections or fear of being perceived as overstepping professional boundaries. Previous studies have reported similar trends, where dental students expressed reluctance in recommending HPV vaccination, especially to patients of the opposite sex [
13,
51]. Despite growing evidence of the preventive role that dentists can play in HPV-related cancer control, substantial gaps remain in formal education on this topic. A national survey of U.S. dental schools revealed that while 85% include HPV-related content in required courses, only 10% address prevention strategies and a mere 11% provide training in patient education on HPV. This suggests that educational efforts are still largely theoretical and may not equip students with the practical skills necessary for effective HPV prevention in clinical settings [
8]. While most dental students agree that educating patients about the HPV–oropharyngeal cancer link falls within their professional responsibilities, many lack the confidence to engage in such conversations. In a recent U.S. study, 44% of students reported anticipating discomfort when recommending the HPV vaccine, and only 33.9% felt “very confident” discussing HPV risk factors with patients [
8]. These findings underscore a critical need for communication training, particularly in discussing sexually transmitted infections in culturally sensitive environments [
8]. Participant hesitations toward HPV vaccination, as reflected in their uncertainty or misconceptions regarding vaccine safety and transmission prevention, highlight the need for targeted educational interventions. While outright refusal was rare, approximately 27.1% of participants reported indecision about future vaccination, and 13.2% expressed doubts about vaccine safety or efficacy. Moreover, a lower proportion (79.4%) believed that the vaccine prevents HPV transmission, despite widespread acknowledgment of its cancer-preventive role. Gender-based differences were also notable—male students were more likely to express hesitation, with 24.4% either disagreeing or unsure about the vaccine’s safety, compared to 10.1% of female respondents. These findings suggest that hesitancy may be driven more by informational gaps and trust issues than by active opposition and point to the importance of addressing these perceptual barriers through targeted, gender-sensitive communication strategies. The absence of clear clinical protocols for oral cancer screening was also identified as a significant barrier among dental students. A Dutch study found that students strongly supported the development of standardized screening procedures and emphasized the need for additional training in clinical oral examinations [
13]. The establishment of such protocols could enhance consistency and confidence in early detection practices [
13]. Similarly to findings in Romania, Dutch dental students reported low self-confidence in conducting oral cancer examinations. When asked to rate their confidence, visual inspection received an average score of 3.2 out of 4 (where 4 indicates “not confident”), and manual palpation scored even lower. These self-assessments highlight a universal need for improved clinical training and early exposure to head and neck cancer diagnostics during dental education [
13].
Given the increasing burden of HPV-related oropharyngeal cancers and the regular patient contact dentists have, it is essential to integrate structured communication training within the dental curriculum to improve future professionals’ confidence and competence in addressing sensitive health topics.
In parallel, our study supports the emerging role of saliva as a non-invasive diagnostic tool for HPV detection. The ease of collection, patient comfort, and the molecular content of saliva—ranging from DNA to exosomes—make it an appealing medium for early identification of high-risk HPV strains associated with oropharyngeal cancers. Our protocol, which involved pre-analytical standardization and PCR-based genotyping, highlights the feasibility of integrating salivary diagnostics into clinical and educational settings. As such, future dental professionals should be made aware of these advancements, which not only support preventive oncology but also align with the broader move toward personalized and minimally invasive medicine. Expanding the role of dentists in HPV surveillance and prevention, through both education and clinical screening, could significantly contribute to global efforts in reducing HPV-related cancer incidence. While most HPV-related research in Romania has focused on cervical cancer, our findings highlight the growing need to address oropharyngeal cancers within dental medicine. Dentists, due to their regular contact with patients, are well-positioned to contribute to HPV education and early detection. Romanian dental education should therefore include targeted communication training and practical prevention strategies. As emphasized by Diaconescu et al. (2021), psychological factors—such as health beliefs and stage of academic training—play a significant role in vaccination intent, reinforcing the value of tailored interventions during dental education [
28]. Future research should investigate the integration of salivary HPV screening into dental practice, particularly for high-risk groups. Since the participating dental students were still in training and not yet practicing independently, the main objective of our study was to evaluate their opinions and attitudes toward discussing HPV-related topics with future patients. This focus allowed us to explore their perceived role in HPV prevention, even in the absence of direct clinical responsibility.
In our study, salivary screening was performed on a subset of participants who consented to molecular testing for HPV. The results revealed a low prevalence of detectable HPV DNA in saliva samples, aligning with the self-reported low rate of HPV-related oral lesions and limited vaccination uptake. These findings are consistent with those of Fakhry et al. (2011), who reported that the detection of oral HPV DNA in asymptomatic individuals using salivary samples remains relatively rare, particularly in young populations with no known risk factors [
52]. Despite its low sensitivity in general populations, salivary screening remains a promising non-invasive tool for early detection, especially in high-risk groups or clinical settings where visual inspection alone may be insufficient.
Since our study had a small sample size of 199 participants, specifically dental students from the Victor Babeș University of Medicine and Pharmacy in Timișoara, it may reflect a sampling bias and may not provide a complete picture of HPV infection among the general population. However, this research has undoubtedly contributed to raising awareness among the participants, as reflected in our findings. The increased knowledge about HPV and its associated health risks has led to a greater understanding among these young adults of the importance of timely vaccination and its acceptance. This represents a crucial step in the right direction, especially considering that a previous questionnaire-based study in Romania indicated a low acceptance rate of the HPV vaccine. Given the significance of HPV-related diseases, enhancing awareness and promoting vaccination among future healthcare professionals is both an urgent necessity and a long-term investment in public health. In our study, all data regarding HPV awareness, vaccination status, and sexual health perceptions were self-reported, which introduces the potential for social desirability bias and underreporting of sensitive behaviors. The cross-sectional design does not allow for establishing causal relationships between variables such as awareness and vaccine uptake. Finally, although saliva-based HPV detection provides a non-invasive screening approach, the study did not assess participants’ oral health status or correlate positivity with clinical symptoms, which could have further validated the findings.
One of the key takeaways from this study is the use of a non-invasive screening method to detect the presence of HPV 16 and 18, making early identification more accessible. The study specifically focuses on young adults, a demographic that needs increased awareness regarding timely protection against HPV-related diseases. Furthermore, this research highlights the necessity of incorporating HPV immunization into public healthcare policies to mitigate the long-term burden of HPV-related illnesses. Future research should include larger, multicentric samples across Romanian universities, assess long-term behavior change following educational interventions, and explore patient perspectives on receiving HPV-related advice from dentists. A crucial message conveyed is that there is a significant gap in knowledge regarding HPV-related oral cancer and its vaccine, an issue that also applies to Romania. This underlines the need for increased awareness campaigns and improved vaccination strategies to enhance public health outcomes.