Evaluation of Immunogenicity of an Orf Virus Vector-Based Vaccine Delivery Platform in Sheep
Abstract
1. Introduction
2. Materials and Methods
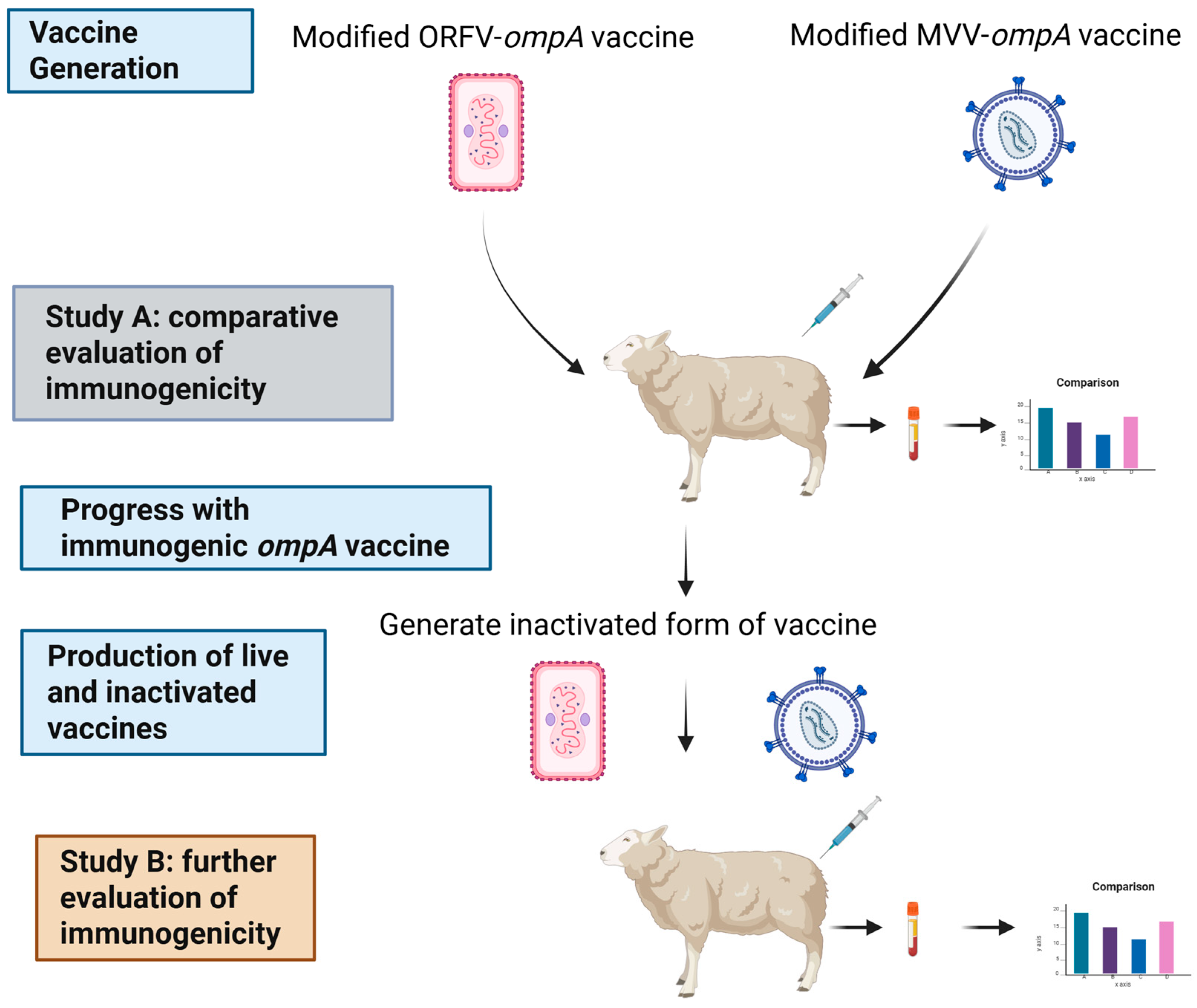
2.1. Project Overview
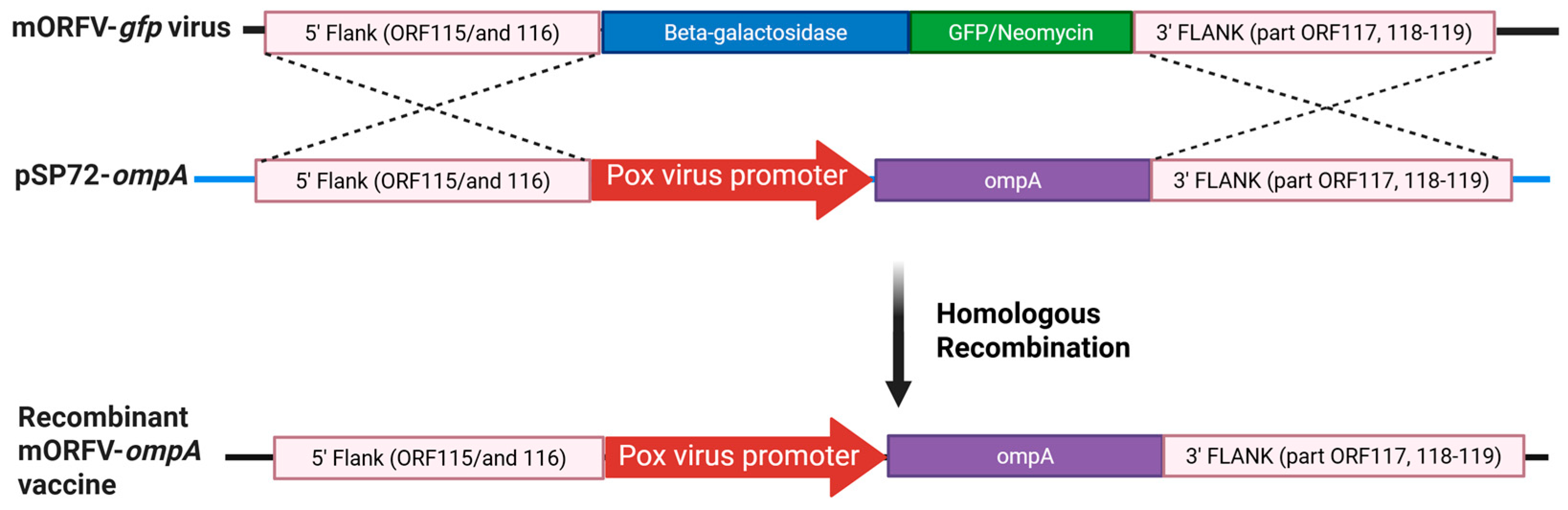
2.2. Production and Evaluation of the Recombinant Modified Orf Virus Encoding the ompA Gene of C. abortus (mORFV-ompA)
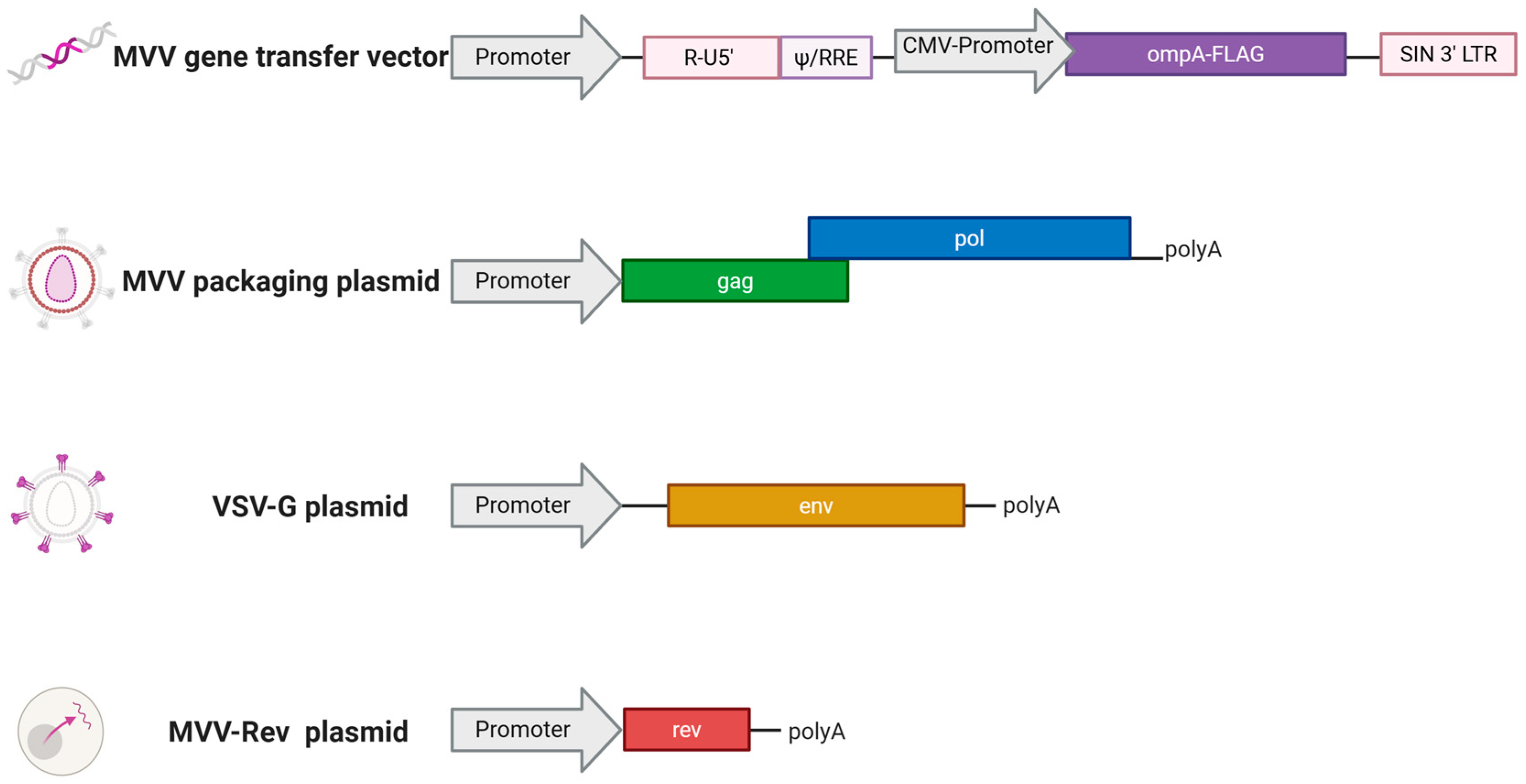
2.3. Production of the Recombinant Modified Maedi Visna Virus Encoding the ompA Gene of C. abortus (mMVV-ompA)
2.4. Evaluation of mMVV-ompA
2.4.1. Detection of Protein Expression
2.4.2. Determination of mMVV-ompA Vector Titre
2.5. Experimental Animals and Ethics Statement
2.6. Selection of Sheep for the Immunogenicity Studies
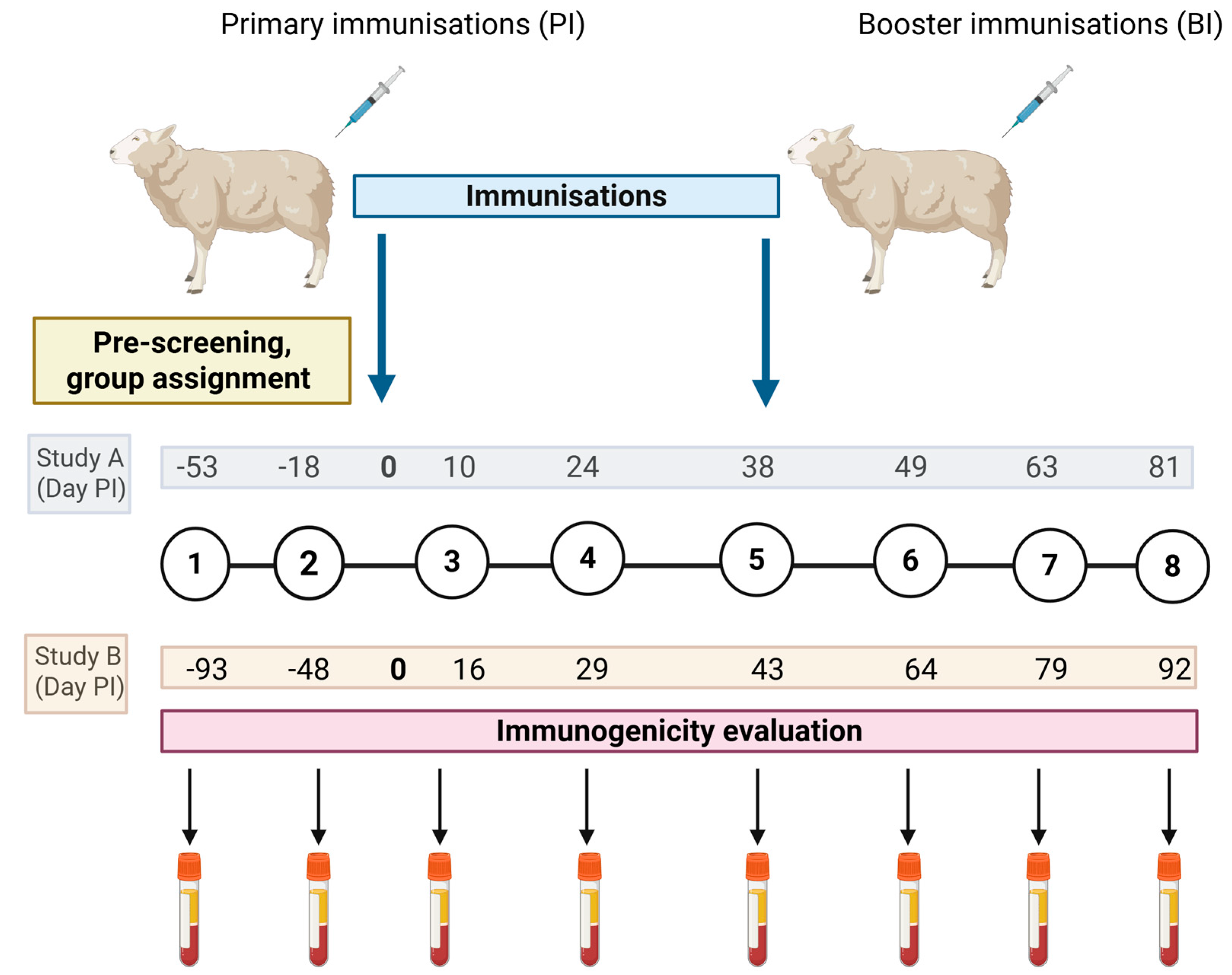
2.7. Preparation and Administration of the ompA Virus Vaccines and Blood Sample Schedules for Immunogenicity Studies A and B
2.8. Serological Responses to C. abortus MOMP
2.9. Cellular Analysis
2.10. Assessment of Humoral Responses to ORFV
2.11. Statistical Analyses
3. Results
3.1. Confirmation of ompA Gene mRNA/MOMP Protein from Vaccine Constructs In Vitro
3.2. Screening of Antigen Reactivity to MOMP in Sheep Cohort for Study A
3.2.1. Antibody Responses to MOMP
3.2.2. Screening of Sheep Cohort for Assignment of Vaccine and Control Groups by Evaluation of Cellular Baseline Responses to Concanavalin A and Recall Responses to Chlamydial Antigens
3.3. Humoral and Cellular Antigen-Driven Responses to MOMP Following Immunisation with ompA Vaccines
3.3.1. Anti-MOMP IgG Responses
3.3.2. Cellular IFN-γ Responses Following Vaccine-Delivered ompA
3.4. Evaluation of mORFV-ompA Inactivation
3.5. Comprehensive Immunogenicity Evaluation of Live and Inactivated mORFV-ompA In Vivo in Sheep
3.5.1. Screening of Sheep Cohort for the Comprehensive Immunogenicity Study B Comparing Live and Inactivated mORFV-ompA
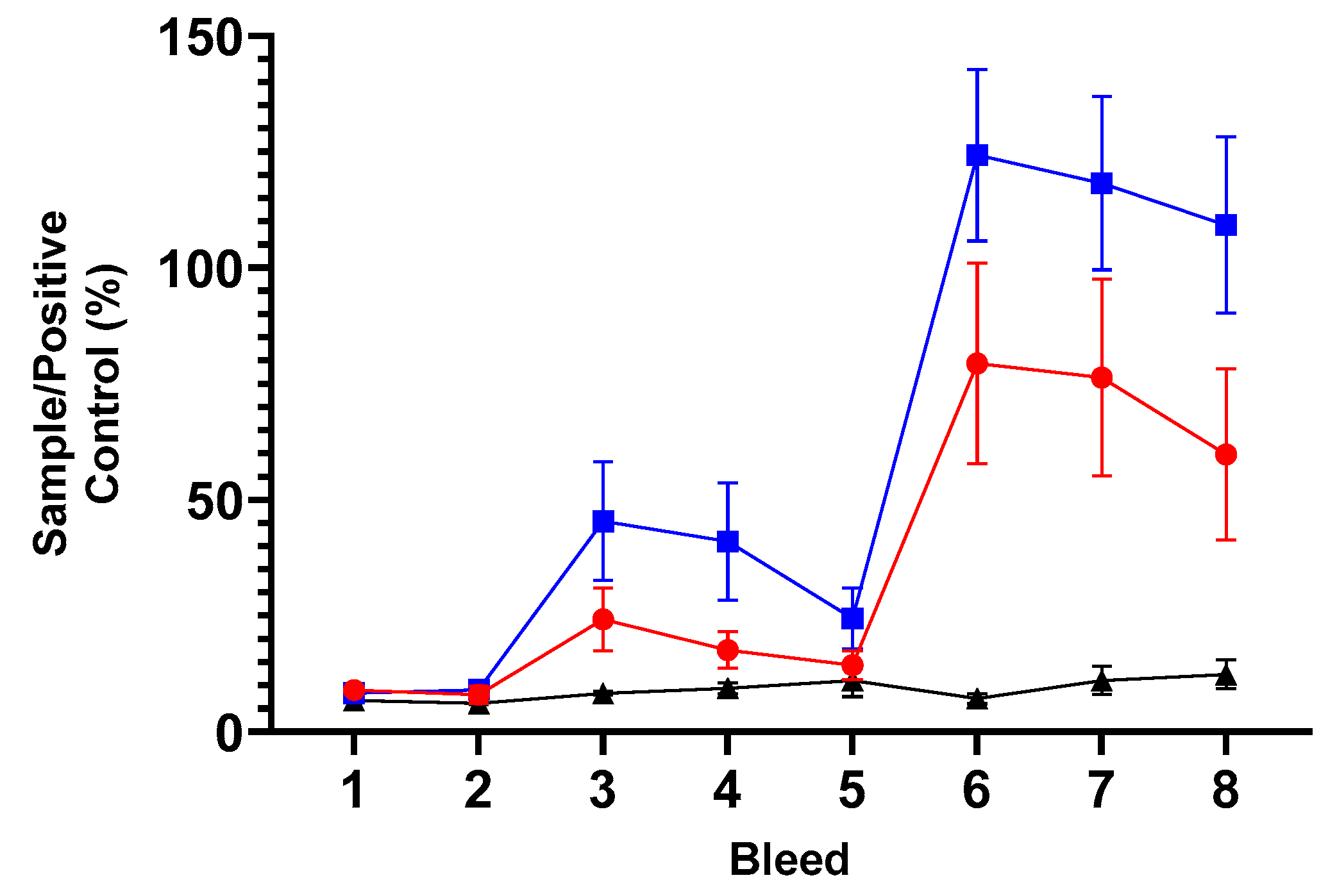
3.5.2. Humoral Responses to MOMP in ORFV-ompA Immunisation Study B
3.5.3. Cellular Immune Responses
3.5.4. Cellular Immune Responses to the MOMP Antigen in Sheep Following Immunisation with mORFV-ompA
3.5.5. Humoral Responses to the Vaccine Backbone, ORFV
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Draper, S.J.; Heeney, J.L. Viruses as vaccine vectors for infectious diseases and cancer. Nat. Rev. Microbiol. 2010, 8, 62–73. [Google Scholar] [CrossRef] [PubMed]
- Ghattas, M.; Dwivedi, G.; Lavertu, M.; Alameh, M.G. Vaccine Technologies and Platforms for Infectious Diseases: Current Progress, Challenges, and Opportunities. Vaccines 2021, 9, 1490. [Google Scholar] [CrossRef]
- Yong, L.; Hutchings, C.; Barnes, E.; Klenerman, P.; Provine, N.M. Distinct Requirements for CD4(+) T Cell Help for Immune Responses Induced by mRNA and Adenovirus-Vector SARS-CoV-2 Vaccines. Eur. J. Immunol. 2025, 55, e202451142. [Google Scholar] [CrossRef]
- Condit, R.C.; Williamson, A.-L.; Sheets, R.; Seligman, S.J.; Monath, T.P.; Excler, J.-L.; Gurwith, M.; Bok, K.; Robertson, J.S.; Kim, D.; et al. Unique safety issues associated with virus-vectored vaccines: Potential for and theoretical consequences of recombination with wild type virus strains. Vaccine 2016, 34, 6610–6616. [Google Scholar] [CrossRef]
- McCann, N.; O’Connor, D.; Lambe, T.; Pollard, A.J. Viral vector vaccines. Curr. Opin. Immunol. 2022, 77, 102210. [Google Scholar] [CrossRef]
- Wang, H.; Tian, J.; Zhao, J.; Zhao, Y.; Yang, H.; Zhang, G. Current Status of Poultry Recombinant Virus Vector Vaccine Development. Vaccines 2024, 12, 630. [Google Scholar] [CrossRef]
- Global Veterinary Vaccinology Research and Innovation Landscape Survey Report, January 2022. Available online: https://www.star-idaz.net/wp-content/uploads/2024/08/Star-Idaz-Veterinary-Vaccinology-report_Jan-2022.pdf (accessed on 30 May 2025).
- Confer, A.W.; Ayalew, S. The OmpA family of proteins: Roles in bacterial pathogenesis and immunity. Vet. Microbiol. 2013, 163, 207–222. [Google Scholar] [CrossRef] [PubMed]
- Olsen, A.W.; Rosenkrands, I.; Holland, M.J.; Andersen, P.; Follmann, F. A Chlamydia trachomatis VD1-MOMP vaccine elicits cross-neutralizing and protective antibodies against C/C-related complex serovars. NPJ Vaccines 2021, 6, 58. [Google Scholar] [CrossRef] [PubMed]
- Desclozeaux, M.; Robbins, A.; Jelocnik, M.; Khan, S.A.; Hanger, J.; Gerdts, V.; Potter, A.; Polkinghorne, A.; Timms, P. Immunization of a wild koala population with a recombinant Chlamydia pecorum Major Outer Membrane Protein (MOMP) or Polymorphic Membrane Protein (PMP) based vaccine: New insights into immune response, protection and clearance. PLoS ONE 2017, 12, e0178786. [Google Scholar] [CrossRef]
- Tan, T.W.; Herring, A.J.; Anderson, I.E.; Jones, G.E. Protection of sheep against Chlamydia psittaci infection with a subcellular vaccine containing the major outer membrane protein. Infect. Immun. 1990, 58, 3101–3108. [Google Scholar] [CrossRef]
- Mercer, A.A.; Norihito, U.A.; Sonja-Maria, F.B.; Hofmann, K.; Fraser, K.M.; Bateman, T.; Fleming, S.B. Comparative analysis of genome sequences of three isolates of Orf virus reveals unexpected sequence variation. Virus Res. 2006, 116, 146–158. [Google Scholar] [CrossRef]
- Haig, D.M. Orf virus infection and host immunity. Curr. Opin. Infect. Dis. 2006, 19, 127–131. [Google Scholar] [CrossRef]
- Travieso, T.; Li, J.; Mahesh, S.; Mello, J.; Blasi, M. The use of viral vectors in vaccine development. NPJ Vaccines 2022, 7, 75. [Google Scholar] [CrossRef] [PubMed]
- Moss, B. Poxvirus DNA replication. Cold Spring Harb. Perspect. Biol. 2013, 5, a010199. [Google Scholar] [CrossRef] [PubMed]
- Pincha, M.; Sundarasetty, B.S.; Stripecke, R. Lentiviral vectors for immunization: An inflammatory field. Expert Rev. Vaccines 2010, 9, 309–321. [Google Scholar] [CrossRef] [PubMed]
- Shaw, A.; Cornetta, K. Design and Potential of Non-Integrating Lentiviral Vectors. Biomedicines 2014, 2, 14–35. [Google Scholar] [CrossRef]
- Iglesias, M.C.; Frenkiel, M.P.; Mollier, K.; Souque, P.; Despres, P.; Charneau, P. A single immunization with a minute dose of a lentiviral vector-based vaccine is highly effective at eliciting protective humoral immunity against West Nile virus. J. Gene Med. 2006, 8, 265–274. [Google Scholar] [CrossRef]
- García-Nicolás, O.; Ricklin, M.E.; Liniger, M.; Vielle, N.J.; Python, S.; Souque, P.; Charneau, P.; Summerfield, A. A Japanese Encephalitis Virus Vaccine Inducing Antibodies Strongly Enhancing In Vitro Infection Is Protective in Pigs. Viruses 2017, 9, 124. [Google Scholar] [CrossRef]
- Gallinaro, A.; Borghi, M.; Bona, R.; Grasso, F.; Calzoletti, L.; Palladino, L.; Cecchetti, S.; Vescio, M.F.; Macchia, D.; Morante, V.; et al. Integrase Defective Lentiviral Vector as a Vaccine Platform for Delivering Influenza Antigens. Front. Immunol. 2018, 9, 171. [Google Scholar] [CrossRef]
- Grasso, F.; Negri, D.R.; Mochi, S.; Rossi, A.; Cesolini, A.; Giovannelli, A.; Chiantore, M.V.; Leone, P.; Giorgi, C.; Cara, A. Successful therapeutic vaccination with integrase defective lentiviral vector expressing nononcogenic human papillomavirus E7 protein. Int. J. Cancer 2013, 132, 335–344. [Google Scholar] [CrossRef]
- Coutant, F.; Sanchez David, R.Y.; Félix, T.; Boulay, A.; Caleechurn, L.; Souque, P.; Thouvenot, C.; Bourgouin, C.; Beignon, A.S.; Charneau, P. A nonintegrative lentiviral vector-based vaccine provides long-term sterile protection against malaria. PLoS ONE 2012, 7, e48644. [Google Scholar] [CrossRef]
- Kim, J.H.; Sohn, H.J.; Lee, J.; Yang, H.J.; Chwae, Y.J.; Kim, K.; Park, S.; Shin, H.J. Vaccination with lentiviral vector expressing the nfa1 gene confers a protective immune response to mice infected with Naegleria fowleri. Clin. Vaccine Immunol. 2013, 20, 1055–1060. [Google Scholar] [CrossRef] [PubMed]
- Karponi, G.; Kritas, S.; Petridou, E.; Papanikolaou, E. Efficient Transduction and Expansion of Ovine Macrophages for Gene Therapy Implementations. Vet. Sci. 2018, 5, 57. [Google Scholar] [CrossRef] [PubMed]
- McLean, R.K. Development of a Novel Lentiviral Vaccine Vector and Characterisation of In Vitro Immune Responses. Ph.D. Thesis, The University of Edinburgh, Edinburgh, UK, 2018. [Google Scholar]
- Longbottom, D.; Livingstone, M.; Aitchison, K.D.; Imrie, L.; Manson, E.; Wheelhouse, N.; Inglis, N.F. Proteomic characterisation of the Chlamydia abortus outer membrane complex (COMC) using combined rapid monolithic column liquid chromatography and fast MS/MS scanning. PLoS ONE 2019, 14, e0224070. [Google Scholar] [CrossRef]
- Livingstone, M.; Aitchison, K.; Palarea-Albaladejo, J.; Ciampi, F.; Underwood, C.; Paladino, A.; Chianini, F.; Entrican, G.; Wattegedera, S.R.; Longbottom, D. Protective Efficacy of Decreasing Antigen Doses of a Chlamydia abortus Subcellular Vaccine Against Ovine Enzootic Abortion in a Pregnant Sheep Challenge Model. Vaccines 2025, 13, 89. [Google Scholar] [CrossRef] [PubMed]
- Deane, D.; McInnes, C.J.; Percival, A.; Wood, A.; Thomson, J.; Lear, A.; Gilray, J.; Fleming, S.; Mercer, A.; Haig, D. Orf virus encodes a novel secreted protein inhibitor of granulocyte-macrophage colony-stimulating factor and interleukin-2. J. Virol. 2000, 74, 1313–1320. [Google Scholar] [CrossRef]
- Krieg, P.A.; Melton, D.A. In vitro RNA synthesis with SP6 RNA polymerase. Methods Enzymol. 1987, 155, 397–415. [Google Scholar] [CrossRef]
- Glover, D.M. DNA Cloning: A Practical Approach; IRL Press: Oxford, UK, 1985. [Google Scholar]
- Ballandras-Colas, A.; Chivukula, V.; Gruszka, D.T.; Shan, Z.; Singh, P.K.; Pye, V.E.; McLean, R.K.; Bedwell, G.J.; Li, W.; Nans, A.; et al. Multivalent interactions essential for lentiviral integrase function. Nat. Commun. 2022, 13, 2416. [Google Scholar] [CrossRef]
- Clapham, P.R.; McKnight, A.; Weiss, R.A. Human immunodeficiency virus type 2 infection and fusion of CD4-negative human cell lines: Induction and enhancement by soluble CD4. J. Virol. 1992, 66, 3531–3537. [Google Scholar] [CrossRef]
- Reed, L.J.; Muench, H. A simple method of estimating fifty per cent endpoints. Am. J. Epidemiol. 1938, 27, 493–497. [Google Scholar] [CrossRef]
- Percie du Sert, N.; Hurst, V.; Ahluwalia, A.; Alam, S.; Avey, M.T.; Baker, M.; Browne, W.J.; Clark, A.; Cuthill, I.C.; Dirnagl, U.; et al. The ARRIVE guidelines 2.0: Updated guidelines for reporting animal research. J. Physiol. 2020, 598, 3793–3801. [Google Scholar] [CrossRef] [PubMed]
- SRUC. Premium Sheep & Goat Health Scheme. Available online: https://www.sruc.ac.uk/business-services/veterinary-laboratory-services/premium-sheep-goat-health-scheme/ (accessed on 13 May 2025).
- Wilson, K.; Livingstone, M.; Longbottom, D. Comparative evaluation of eight serological assays for diagnosing Chlamydophila abortus infection in sheep. Vet. Microbiol. 2009, 135, 38–45. [Google Scholar] [CrossRef]
- Wattegedera, S.R.; Livingstone, M.; Maley, S.; Rocchi, M.; Lee, S.; Pang, Y.; Wheelhouse, N.M.; Aitchison, K.; Palarea-Albaladejo, J.; Buxton, D.; et al. Defining immune correlates during latent and active chlamydial infection in sheep. Vet. Res. 2020, 51, 75. [Google Scholar] [CrossRef] [PubMed]
- McKeever, D.J.; Reid, H.W.; Inglis, N.F.; Herring, A.J. A qualitative and quantitative assessment of the humoral antibody response of the sheep to orf virus infection. Vet. Microbiol. 1987, 15, 229–241. [Google Scholar] [CrossRef]
- Donachie, W.; Jones, G.E. The use of ELISA to detect antibodies to Pasteurella haemolytica A2 and Mycoplasma ovipneumoniae in sheep with experimental chronic pneumonia. In The ELISA: Enzyme Linked Immunosorbent Assay in Veterinary Research and Diagnosis; Wardley, R.C., Crowther, J.R., Eds.; Martinus Nijhoff: The Hague, The Netherlands, 1982; pp. 102–110. [Google Scholar]
- Benjamini, Y.; Hochberg, Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J. R. Stat. Soc. B 1995, 57, 289–300. [Google Scholar] [CrossRef]
- R Core Team. The R Project for Statistical Computing. Available online: https://www.r-project.org (accessed on 8 October 2024).
- Huang, H.S.; Tan, T.W.; Buxton, D.; Anderson, I.E.; Herring, A.J. Antibody response of the ovine lymph node to experimental infection with an ovine abortion strain of Chlamydia psittaci. Vet. Microbiol. 1990, 21, 345–351. [Google Scholar] [CrossRef]
- Livingstone, M.; Entrican, G.; Wattegedera, S.; Buxton, D.; McKendrick, I.J.; Longbottom, D. Antibody responses to recombinant protein fragments of the major outer membrane protein and polymorphic outer membrane protein POMP90 in Chlamydophila abortus-infected pregnant sheep. Clin. Diagn. Lab. Immunol. 2005, 12, 770–777. [Google Scholar] [CrossRef] [PubMed]
- Gorrell, M.D.; Brandon, M.R.; Sheffer, D.; Adams, R.J.; Narayan, O. Ovine lentivirus is macrophagetropic and does not replicate productively in T lymphocytes. J. Virol. 1992, 66, 2679–2688. [Google Scholar] [CrossRef]
- Ryan, S.; Tiley, L.; McConnell, I.; Blacklaws, B. Infection of dendritic cells by the Maedi-Visna lentivirus. J. Virol. 2000, 74, 10096–10103. [Google Scholar] [CrossRef]
- Amann, R.; Rohde, J.; Wulle, U.; Conlee, D.; Raue, R.; Martinon, O.; Rziha, H.J. A new rabies vaccine based on a recombinant ORF virus (parapoxvirus) expressing the rabies virus glycoprotein. J. Virol. 2013, 87, 1618–1630. [Google Scholar] [CrossRef]
- Jha, R.; Srivastava, P.; Salhan, S.; Finckh, A.; Gabay, C.; Mittal, A.; Bas, S. Spontaneous secretion of interleukin-17 and -22 by human cervical cells in Chlamydia trachomatis infection. Microbes Infect. 2011, 13, 167–178. [Google Scholar] [CrossRef] [PubMed]
- Mathew, M.; Waugh, C.; Beagley, K.W.; Timms, P.; Polkinghorne, A. Interleukin 17A is an immune marker for chlamydial disease severity and pathogenesis in the koala (Phascolarctos cinereus). Dev. Comp. Immunol. 2014, 46, 423–429. [Google Scholar] [CrossRef]
- Phillips, S.; Quigley, B.L.; Timms, P. Seventy Years of Chlamydia Vaccine Research—Limitations of the Past and Directions for the Future. Front. Microbiol. 2019, 10, 70. [Google Scholar] [CrossRef]
- Olsen, A.W.; Rosenkrands, I.; Jacobsen, C.S.; Cheeseman, H.M.; Kristiansen, M.P.; Dietrich, J.; Shattock, R.J.; Follmann, F. Immune signature of Chlamydia vaccine CTH522/CAF®01 translates from mouse-to-human and induces durable protection in mice. Nat. Commun. 2024, 15, 1665. [Google Scholar] [CrossRef] [PubMed]
- Proctor, J.; Stadler, M.; Cortes, L.M.; Brodsky, D.; Poisson, L.; Gerdts, V.; Smirnov, A.I.; Smirnova, T.I.; Barua, S.; Leahy, D.; et al. A TriAdj-Adjuvanted Chlamydia trachomatis CPAF Protein Vaccine Is Highly Immunogenic in Pigs. Vaccines 2024, 12, 423. [Google Scholar] [CrossRef]
- Entrican, G.; Francis, M.J. Applications of platform technologies in veterinary vaccinology and the benefits for one health. Vaccine 2022, 40, 2833–2840. [Google Scholar] [CrossRef] [PubMed]
- Reemers, S.; Peeters, L.; van Schijndel, J.; Bruton, B.; Sutton, D.; van der Waart, L.; van de Zande, S. Novel Trivalent Vectored Vaccine for Control of Myxomatosis and Disease Caused by Classical and a New Genotype of Rabbit Haemorrhagic Disease Virus. Vaccines 2020, 8, 441. [Google Scholar] [CrossRef]
- Pagallies, F.; Labisch, J.J.; Wronska, M.; Pflanz, K.; Amann, R. Efficient and scalable clarification of Orf virus from HEK suspension for vaccine development. Vaccine X 2024, 18, 100474. [Google Scholar] [CrossRef]
- Eilts, F.; Labisch, J.J.; Orbay, S.; Harsy, Y.M.J.; Steger, M.; Pagallies, F.; Amann, R.; Pflanz, K.; Wolff, M.W. Stability studies for the identification of critical process parameters for a pharmaceutical production of the Orf virus. Vaccine 2023, 41, 4731–4742. [Google Scholar] [CrossRef]
- Lothert, K.; Pagallies, F.; Eilts, F.; Sivanesapillai, A.; Hardt, M.; Moebus, A.; Feger, T.; Amann, R.; Wolff, M.W. A scalable downstream process for the purification of the cell culture-derived Orf virus for human or veterinary applications. J. Biotechnol. 2020, 323, 221–230. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wattegedera, S.R.; Thomson, J.; Coulter, L.; Wood, A.; McLean, R.K.; Hill, H.; Cunnea, C.; Snedden, K.; Percival, A.; Palarea-Albaladejo, J.; et al. Evaluation of Immunogenicity of an Orf Virus Vector-Based Vaccine Delivery Platform in Sheep. Vaccines 2025, 13, 631. https://doi.org/10.3390/vaccines13060631
Wattegedera SR, Thomson J, Coulter L, Wood A, McLean RK, Hill H, Cunnea C, Snedden K, Percival A, Palarea-Albaladejo J, et al. Evaluation of Immunogenicity of an Orf Virus Vector-Based Vaccine Delivery Platform in Sheep. Vaccines. 2025; 13(6):631. https://doi.org/10.3390/vaccines13060631
Chicago/Turabian StyleWattegedera, Sean R., Jackie Thomson, Lesley Coulter, Ann Wood, Rebecca K. McLean, Holly Hill, Cameron Cunnea, Karen Snedden, Ann Percival, Javier Palarea-Albaladejo, and et al. 2025. "Evaluation of Immunogenicity of an Orf Virus Vector-Based Vaccine Delivery Platform in Sheep" Vaccines 13, no. 6: 631. https://doi.org/10.3390/vaccines13060631
APA StyleWattegedera, S. R., Thomson, J., Coulter, L., Wood, A., McLean, R. K., Hill, H., Cunnea, C., Snedden, K., Percival, A., Palarea-Albaladejo, J., Entrican, G., Longbottom, D., Griffiths, D. J., & McInnes, C. J. (2025). Evaluation of Immunogenicity of an Orf Virus Vector-Based Vaccine Delivery Platform in Sheep. Vaccines, 13(6), 631. https://doi.org/10.3390/vaccines13060631







