Mapping Behavioral and Social Drivers of Influenza Vaccine Uptake in Older Adults: A Scoping Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Conceptual Framework
2.2. Research Questions
- (i)
- What behavioral and social drivers influence influenza vaccine uptake among those aged 60 years and older?
- (ii)
- What facilitators and barriers to influenza vaccination among older adults have been considered through the four domains of the BeSD framework?
- (iii)
- What knowledge deficiencies exist in the current research addressing this population’s behavioral and social drivers of influenza vaccination?
2.3. Search Strategy and Selection Criteria
2.4. Study Selection
2.5. Quality Appraisal
2.6. Data Extraction, Charting, and Analysis
3. Results
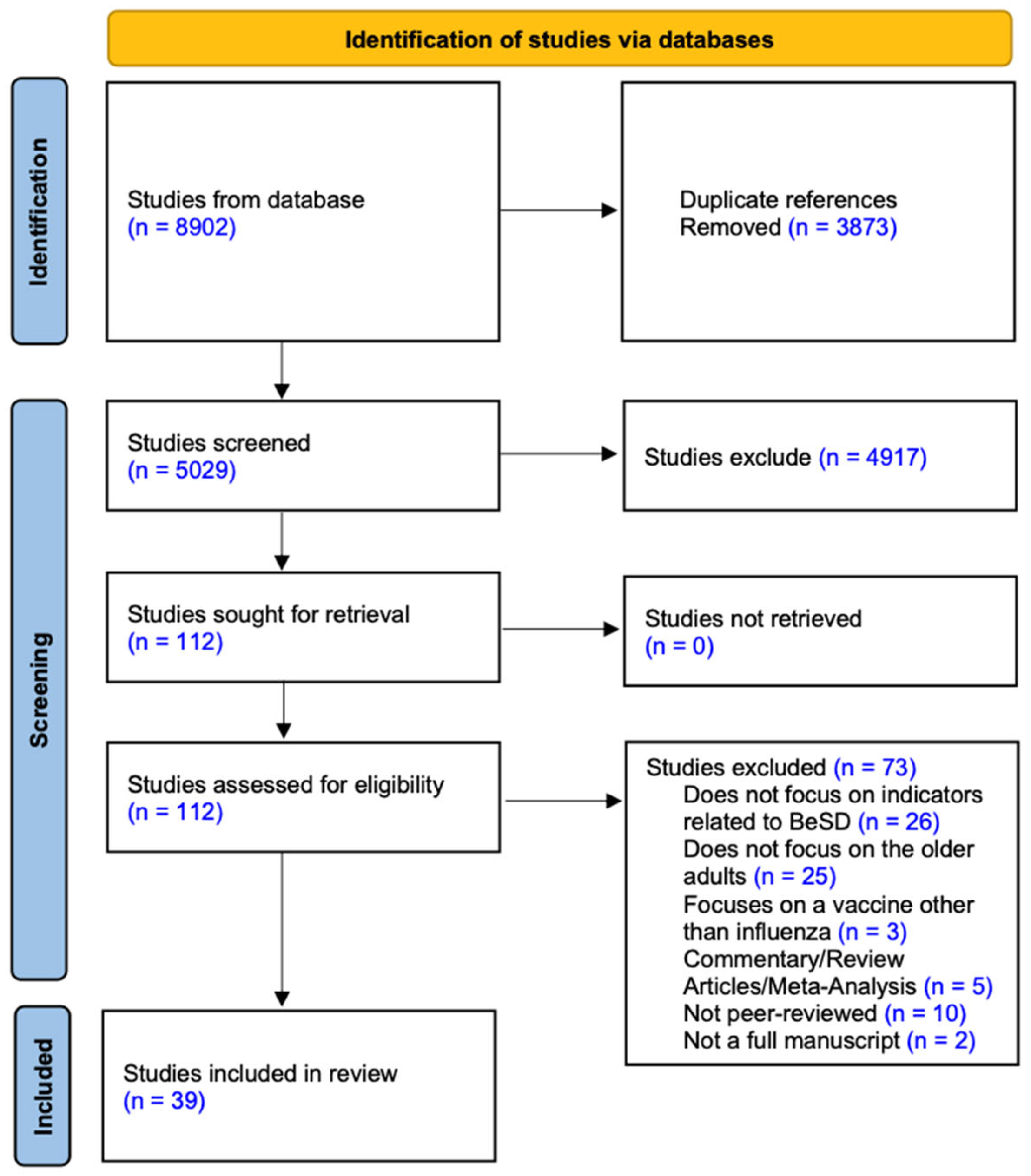
3.1. Selection of Sources of Evidence
3.2. Characteristics of Included Studies
3.3. Summary of Behavioral and Social Drivers by BeSD Domains
3.3.1. Thinking and Feeling
3.3.2. Social Processes
3.3.3. Motivation
3.3.4. Practical Issues
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
Appendix A.1. Understanding Behavioural and Social Drivers in Influenza Vaccination in Older Adults—Protocol
- -
- Population: The population of interest is older adults aged 60 years and older. Studies with mixed-age populations will be included if results for the older adult subgroup are reported separately.
- -
- Concept: The review will focus on behavioral and social drivers related to influenza vaccination. Eligible studies must address at least one domain of the BeSD framework, namely Thinking and Feeling, Social Processes, Motivation, or Practical Issues.
- -
- Context: There are no restrictions on geographic location or healthcare setting. Studies conducted in community, clinical, or institutional settings will be eligible.
- -
- Research detail:
- (a)
- Language: only studies published in English will be included;
- (b)
- Published Time: studies published up to 31 December 2024 will be considered;
- (c)
- Study method: all study designs, including qualitative, quantitative, and mixed methods studies, will be included;
- (d)
- Study Type Exclusion: Clinical reports, guidelines, position papers, study protocols, book chapters, conference abstracts, editorials, duplicate studies, and studies without full text will be excluded;
- (e)
- Topical Exclusion: Studies focusing solely on vaccine properties (e.g., efficacy, safety, immunogenicity), cost-effectiveness analyses, modeling studies, or budget impact analyses will be excluded. Studies focusing on vaccines unrelated to influenza vaccination will also be excluded.
- -
- Database
- -
- Search keyword
- (a)
- Population: “older adults”, “elderly”, “aged 60 years and older”
- (b)
- Intervention: “influenza vaccination”, “flu shot”, “immunization”
- (c)
- Behavioral and social drivers: “perception”, “acceptance”, “motivation”, “willingness”, “intention”, “hesitancy”, “social norms”, “recommendations”, “trust”, “barriers”, “facilitators”
- -
- Search steps
Appendix A.2. PRISMA-ScR Checklist
| SECTION | ITEM | PRISMA-ScR CHECKLIST ITEM | REPORTED ON PAGE # |
| TITLE | |||
| Title | 1 | Identify the report as a scoping review. | 1 |
| ABSTRACT | |||
| Structured summary | 2 | Provide a structured summary that includes (as applicable) the following: background, objectives, eligibility criteria, sources of evidence, charting methods, results, and conclusions that relate to the review questions and objectives. | 1 |
| INTRODUCTION | |||
| Rationale | 3 | Describe the rationale for the review in the context of what is already known. Explain why the review questions/objectives lend themselves to a scoping review approach. | 1–2 |
| Objectives | 4 | Provide an explicit statement of the questions and objectives being addressed with reference to their key elements (e.g., population or participants, concepts, and context) or other relevant key elements used to conceptualize the review questions and/or objectives. | 2 |
| METHODS | |||
| Protocol and registration | 5 | Indicate whether a review protocol exists; state if and where it can be accessed (e.g., a Web address); and, if available, provide registration information, including the registration number. | 2 and Appendix A.1 |
| Eligibility criteria | 6 | Specify characteristics of the sources of evidence used as eligibility criteria (e.g., years considered, language, and publication status) and provide a rationale. | 3 |
| Information sources | 7 | Describe all information sources in the search (e.g., databases with dates of coverage and contact with authors to identify additional sources), as well as the date the most recent search was executed. | 3 and Appendix A.3 |
| Search | 8 | Present the full electronic search strategy for at least one database, including any limits used, such that it could be repeated. | 3 and Appendix A.3 |
| Selection of sources of evidence | 9 | State the process for selecting sources of evidence (i.e., screening and eligibility) included in the scoping review. | 3 |
| Data charting process | 10 | Describe the methods of charting data from the included sources of evidence (e.g., calibrated forms or forms that have been tested by the team before their use and whether data charting was conducted independently or in duplicate) and any processes for obtaining and confirming data from investigators. | 3 |
| Data items | 11 | List and define all variables for which data were sought and any assumptions and simplifications made. | 3 |
| Critical appraisal of individual sources of evidence | 12 | If conducted, provide a rationale for conducting a critical appraisal of included sources of evidence; describe the methods used and how this information was used in any data synthesis (if appropriate). | 3-4 and Appendix A.4 |
| Synthesis of results | 13 | Describe the methods of handling and summarizing the data that were charted. | 4 |
| RESULTS | |||
| Selection of sources of evidence | 14 | Give the number of sources of evidence screened, assessed for eligibility, and included in the review, with reasons for exclusions at each stage, ideally using a flow diagram. | 4 and Figure 1 |
| Characteristics of sources of evidence | 15 | For each source of evidence, present characteristics for which data were charted and provide the citations. | 4–5 and Table 1 |
| Critical appraisal within sources of evidence | 16 | If conducted, present data on critical appraisal of included sources of evidence (see item 12). | Appendix A.4 |
| Results of individual sources of evidence | 17 | For each included source of evidence, present the relevant data that were charted that relate to the review questions and objectives. | 5 and Table 2 |
| Synthesis of results | 18 | Summarize and/or present the charting results as they relate to the review questions and objectives. | 13–14 |
| DISCUSSION | |||
| Summary of evidence | 19 | Summarize the main results (including an overview of concepts, themes, and types of evidence available), link to the review questions and objectives, and consider the relevance to key groups. | 14 |
| Limitations | 20 | Discuss the limitations of the scoping review process. | 17 |
| Conclusions | 21 | Provide a general interpretation of the results with respect to the review questions and objectives, as well as potential implications and/or next steps. | 17–18 |
| FUNDING | |||
| Funding | 22 | Describe sources of funding for the included sources of evidence, as well as sources of funding for the scoping review. Describe the role of the funders of the scoping review. | 18 |
Appendix A.3. Search Strategy and Results
| # | Searches | Results |
| 1 | ‘Influenza, Human’ [Mesh] OR flu[Title/Abstract] OR influenza[Title/Abstract] OR grippe[Title/Abstract] | 142,111 |
| 2 | Vaccines[Mesh] OR vaccin*[Title/Abstract] OR immuniz*[Title/Abstract] OR immunis*[Title/Abstract] OR inoculat*[Title/Abstract] OR shot*[Title/Abstract] | 748,464 |
| 3 | aged[Mesh] OR ‘old people’[Title/Abstract] OR ‘older people’[Title/Abstract] OR ‘old adults’[Title/Abstract] OR ‘old age’[Title/Abstract] OR aging[Title/Abstract] OR elder[Title/Abstract] OR elderly[Title/Abstract] OR senior[Title/Abstract] OR seniors[Title/Abstract] OR geriatric[Title/Abstract] | 3,987,173 |
| 4 | percept*[Title/Abstract] OR accept*[Title/Abstract] OR motivat*[Title/Abstract] OR refus*[Title/Abstract] OR decision*[Title/Abstract] OR attitude[Title/Abstract] OR intention*[Title/Abstract] OR uptake [Title/Abstract] OR knowledge[Title/Abstract] OR willingness[Title/Abstract] OR unwilling*[Title/Abstract] OR adherence[Title/Abstract] OR compliance[Title/Abstract] obedience[Title/Abstract] OR support[Title/Abstract] OR motivation[Title/Abstract] OR consideration[Title/Abstract] | 1,693,779 |
| 1 AND 2 AND 3 AND 4 | 569 | |
| Filters: Humans, English, from the database set—2024 | 525 | |
| * Truncation symbol used in search strings to substitute for zero or more characters at the end of a word. | ||
| # | Searches | Results |
| 1 | ‘influenza‘/exp OR influenza*:ab,ti OR flu:ab,ti OR grippe:ab,ti | 245,497 |
| 2 | ‘vaccine‘/exp OR ‘vaccination‘/exp OR vaccin*:ab,ti OR immuniz*:ab,ti OR immunis*:ab,ti OR incoculat*:ab,ti OR shot*:ab,ti | 845,190 |
| 3 | ‘aged‘/exp OR ‘old people‘:ab,ti OR ‘older people‘:ab,ti OR ‘older adults‘:ab,ti OR ‘old age‘:ab,ti OR aging:ab,ti OR elder:ab,ti OR elderly:ab,ti OR senior:ab,ti OR seniors:ab,ti OR geriatric:ab,ti | 4,617,288 |
| 4 | percept*:ab,ti OR accept*:ab,ti OR motivat*:ab,ti OR refus*:ab,ti OR decision*:ab,ti OR attitude:ab,ti OR intention*:ab,ti OR uptake:ab,ti OR knowledge:ab,ti OR willingness:ab,ti OR unwilling*:ab,ti OR adherence:ab,ti OR compliance:ab,ti OR obedience:ab,ti OR support:ab,ti OR motivation:ab,ti OR consideration:ab,ti | 6,016,676 |
| 1 AND 2 AND 3 AND 4 | 3476 | |
| AND [article]/lim AND [english]/lim AND ‘human’/de AND [embase]/lim AND (2014:py OR 2015:py OR 2016:py OR 2017:py OR 2018:py OR 2019:py OR 2020:py OR 2021:py OR 2022:py OR 2023:py OR 2024:py) | 2353 | |
| * Truncation symbol used in search strings to substitute for zero or more characters at the end of a word. | ||
| # | Search | Results |
| 1 | TS = (‘influenza, human’ OR ‘influenza*’ OR ‘flu’ OR ‘grippe’) | 198,337 |
| 2 | TS = (‘vaccin*’ OR ‘immuniz*’ OR ‘immunis*’ OR ‘incoculat*’ OR ‘shot*) | 750,003 |
| 3 | TS = (‘aged’ OR ‘old people’ OR ‘older people’ OR ‘older adults’ OR ‘old age’ OR ‘aging’ OR ‘elder’ OR ‘elderly’ OR ‘senior’ OR ‘seniors’ OR ‘geriatric’) | 6,579,376 |
| 4 | TS = (‘percept*’ OR ‘accept*’ OR ‘motivat*’ OR ‘refus*’ OR ‘decision’ OR ‘attitude’ OR ‘intention’ OR ‘uptake’ OR ‘knowledge’ OR ‘willingness’ OR ‘unwilling’ OR ‘adherence’ OR ‘compliance’ OR ‘obedience’ OR ‘support’ OR ‘motivation’ OR ‘consideration’) | 11,812,077 |
| 1 AND 2 AND 3 AND 4 | 6590 | |
| AND 2025 (Exclude—Publication Years) and Article (Document Types) and English (Languages) and Article (Document Types) and Proceeding Paper or Early Access or Book Chapters (Exclude—Document Types) | 4760 | |
| * Truncation symbol used in search strings to substitute for zero or more characters at the end of a word. | ||
| # | Search | Results |
| 1 | MH influenza, human OR TI influenza OR AB influenza OR TI flu OR AB flu OR TI grippe OR AB grippe | 29,051 |
| 2 | MH vaccines+ OR MH immunization+ OR TI vaccin* OR AB vaccin* OR TI immuniz* OR AB immuniz* OR TI immunis* OR AB immunis* OR TI inoculat* OR AB inoculat* OR TI shot* OR AB shot* | 115,737 |
| 3 | MH aged OR TI old people OR AB old people OR TI older people OR AB older people OR TI old adults OR AB old adults OR TI old age OR AB old age OR TI aging OR AB aging OR TI elder OR AB elder OR TI elderly OR AB elderly OR TI senior OR AB senior OR TI seniors OR AB seniors OR TI geriatric OR AB geriatric | 1,066,273 |
| 4 | TI (percept* OR accept* OR motivat* OR refus* OR decision OR attitude OR intention OR uptake OR knowledge OR willingness OR unwilling OR adherence OR compliance OR obedience OR support OR motivation OR consideration) OR AB (percept* OR accept* OR motivat* OR refus* OR decision OR attitude OR intention OR uptake OR knowledge OR willingness OR unwilling OR adherence OR compliance OR obedience OR support OR motivation OR consideration) | 1,344,905 |
| 1 AND 2 AND 3 AND 4 | 880 | |
| Limiters—Date Published: 20241231; English Language; Research Article; Human | 658 | |
| * Truncation symbol used in search strings to substitute for zero or more characters at the end of a word. | ||
| # | Search | Results |
| 1 | MeSH descriptor: [Influenza, Human] explode all trees | 3703 |
| 2 | (influenza* OR flu OR grippe):ti,ab,kw | 13,659 |
| 3 | 1 OR 2 | 13,659 |
| 4 | MeSH descriptor: [Vaccines] in all MeSH products | 17,900 |
| 5 | (vaccin* OR immuniz* OR immunis* OR incoculat* OR shot*):ti,ab,kw | 39,909 |
| 6 | 4 OR 5 | 39,931 |
| 7 | MeSH descriptor: [Aged] in all MeSH products | 285,395 |
| 8 | (‘old people’ OR ‘older people’ OR ‘old adults’ OR ‘old age’ OR ‘aging’ OR ‘elder’ OR ‘elderly’ OR ‘senior’ OR ‘seniors’ OR ‘geriatric’):ti,ab,kw | 185,408 |
| 9 | #7 OR #8 | 425,146 |
| 10 | (percept* OR accept* OR motivat* OR refus* OR decision OR attitude OR intention OR uptake OR knowledge OR willingness OR unwilling OR adherence OR compliance OR obedience OR support OR motivation OR consideration):ti,ab,kw | 464,591 |
| 11 | #3 AND #6 AND #9 AND #10 | 620 |
| with Publication Year to 2024, with Cochrane Library publication date to Dec 2024, in Trials | 606 | |
| * Truncation symbol used in search strings to substitute for zero or more characters at the end of a word. | ||
Appendix A.4. Critical Appraisal Checklist
| Studies | Were the Criteria for Inclusion in the Sample Clearly Defined? | Were the Study Subjects and the Setting Described in Detail? | Was the Exposure Measured in a Valid and Reliable Way? | Were Objective and Standard Criteria Used for Measurement of the Condition? | Were Confounding Factors Identified? | Were Strategies to Deal with Confounding Factors Stated? | Were the Outcomes Measured in a Valid and Reliable Way? | Was Appropriate Statistical Analysis Used? |
|---|---|---|---|---|---|---|---|---|
| Anne-Laure B et al. [26] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Bodekers B et al. [27] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Bosompra K et al. [23] | Yes | Yes | Yes | Unclear | No | No | Yes | Yes |
| Dardalas I et al. [34] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Dyda A et al. [28] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Fuller R et al. [8] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Ganczak M et al. [30] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Kaijikawa N et al. [32] | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Yes |
| Klett-Tammen J et al. [29] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Nexøe J et al. [22] | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Yes |
| Nicholls B et al. [9] | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Yes |
| Pietraszek A et al. [35] | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Yes |
| Zimmerman K et al. [24] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Che X et al. [52] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Gazibara T et al. [45] | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | Yes |
| Hou Z et al. [53] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Jiang X et al. [46] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Kharroubi G et al. [49] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Kizmaz M et al. [47] | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Yes |
| Kwong Y. et al. [38] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Mo H et al. [41] | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Yes |
| Praphasiri P et al. [42] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Shen Y et al. [55] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Victor F et al. [39] | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | Yes |
| Wu S et al. [43] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Ye C et al. [44] | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Yes |
| You Y et al. [54] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Yu S et al. [40] | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Yes |
| Zhang F et al. [48] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Zhao Z et al. [56] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Zhou Y et al. [51] | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | Yes |
| Schulz J et al. [58] | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Yes |
| Studies | Is There Congruity Between the Stated Philosophical Perspective and the Research Methodology? | Is There Congruity Between the Research Methodology and the Research Question or Objectives? | Is There Congruity Between the Research Methodology and the Methods Used to Collect Data? | Is There Congruity Between the Research Methodology and the Representation and Analysis of Data? | Is There Congruity Between the Research Methodology and the Interpretation of Results? | Are Participants and Their Voices Adequately Represented? | Is the Research Ethical According to Current Criteria or for Recent Studies, and Is There Evidence of Ethical Approval by an Appropriate Body? | Were the Conclusions Drawn in the Research Report Flow from the Analysis or Interpretation of the Data? |
|---|---|---|---|---|---|---|---|---|
| Adonis-Rizzo T et al. [25] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Teo M et al. [33] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Siu Y et al. [50] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Kwong Y et al. [57] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Studies | Are There Clear Research Questions? | Do the Collected Data Allow Addressing the Research Questions? | Is There an Adequate Rationale for Using a Mixed Methods Design to Address the Research Question? | Are the Different Components of the Study Effectively Integrated to Answer the Research Question? | Are the Outputs of Integration of Qualitative and Quantitative Components Adequately Interpreted? | Are Divergences and Inconsistencies Between Quantitative and Qualitative Results Adequately Addressed? | Do the Different Components of the Study Adhere to the Quality Criteria of Each Tradition of the Methods Involved? |
|---|---|---|---|---|---|---|---|
| Music M. et al. [36] | Yes | Yes | Yes | Yes | Yes | Cannot tell | Yes |
| Rikin S et al. [31] | Yes | Yes | Yes | Yes | Yes | Cannot tell | Yes |
| Xu Y et al. [37] | Yes | Yes | Yes | Yes | Yes | Cannot tell | Yes |
References
- World Health Organization Global Influenza Programme. Available online: https://www.who.int/teams/global-influenza-programme/surveillance-and-monitoring/burden-of-disease#:~:text=Influenza%2520economics%26text=WHO%2520estimates%2520that%2520seasonal%2520influenza,which%2520can%2520be%2520influenza%252Drelated (accessed on 12 February 2024).
- Allen, J.C.; Toapanta, F.R.; Chen, W.; Tennant, S.M. Understanding Immunosenescence and Its Impact on Vaccination of Older Adults. Vaccine 2020, 38, 8264–8272. [Google Scholar] [CrossRef] [PubMed]
- Tanner, A.R.; Dorey, R.B.; Brendish, N.J.; Clark, T.W. Influenza Vaccination: Protecting the Most Vulnerable. Eur. Respir. Rev. 2021, 30, 200258. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Influenza Strategy 2019–2030; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- OECD. Health at a Glance. 2023. Available online: https://www.oecd.org/en/publications/health-at-a-glance-2023_7a7afb35-en/full-report/routine-vaccinations_ee5003aa.html#:~:text=Unlike%20childhood%20immunisation%2C%20influenza%20vaccination,by%20around%C2%A05%C2%A0percentage%20points%20in%20recent%C2%A0years (accessed on 12 February 2024).
- Bonner, K.E.; Vashist, K.; Abad, N.S.; Kriss, J.L.; Meng, L.; Lee, J.T.; Wilhelm, E.; Lu, P.-J.; Carter, R.J.; Boone, K.; et al. Behavioral and Social Drivers of COVID-19 Vaccination in the United States, August–November 2021. Am. J. Prev. Med. 2023, 64, 865–876. [Google Scholar] [CrossRef] [PubMed]
- Thomas, R.E.; Lorenzetti, D.L. Interventions to Increase Influenza Vaccination Rates of Those 60 Years and Older in the Community. Cochrane Database Syst. Rev. 2018, 5, CD005188. [Google Scholar] [CrossRef]
- Fuller, H.R.; Huseth-Zosel, A.; Van Vleet, B.; Carson, P.J. Barriers to Vaccination among Older Adults: Demographic Variation and Links to Vaccine Acceptance. Aging Health Res. 2024, 4, 100176. [Google Scholar] [CrossRef]
- Nicholls, L.A.B.; Gallant, A.J.; Cogan, N.; Rasmussen, S.; Young, D.; Williams, L. Older Adults’ Vaccine Hesitancy: Psychosocial Factors Associated with Influenza, Pneumococcal, and Shingles Vaccine Uptake. Vaccine 2021, 39, 3520–3527. [Google Scholar] [CrossRef]
- Okoli, G.N.; Lam, O.L.T.; Racovitan, F.; Reddy, V.K.; Righolt, C.H.; Neilson, C.; Chit, A.; Thommes, E.; Abou-Setta, A.M.; Mahmud, S.M. Seasonal Influenza Vaccination in Older People: A Systematic Review and Meta-Analysis of the Determining Factors. PLoS ONE 2020, 15, e0234702. [Google Scholar] [CrossRef]
- Nicholls, L.B.; Gallant, A.; Cogan, N.; Rasmussen, S.; Young, D.; Williams, L. Older Adults’ Vaccine Hesitancy: Psychosocial Predictors of Influenza, Pneumococcal, & Shingles Vaccine Uptake. Innov. Aging 2020, 4, 913–914. [Google Scholar]
- Brewer, N.T.; Chapman, G.B.; Rothman, A.J.; Leask, J.; Kempe, A. Increasing Vaccination: Putting Psychological Science into Action. Psychol. Sci. Public Interest 2017, 18, 149–207. [Google Scholar] [CrossRef]
- Privor-Dumm, L.A.; Poland, G.A.; Barratt, J.; Durrheim, D.N.; Knoll, M.D.; Vasudevan, P.; Jit, M.; Bonvehí, P.E.; Bonanni, P.; on behalf of the International Council on Adult Immunization. A Global Agenda for Older Adult Immunization in the COVID-19 Era: A Roadmap for Action. Vaccine 2021, 39, 5240–5250. [Google Scholar] [CrossRef]
- WHO. Behavioural and Social Drivers of Vaccination: Tools and Practical Guidance for Achieving High Uptake; WHO: Geneva, Switzerland, 2022. [Google Scholar]
- Roller-Wirnsberger, R.; Lindner, S.; Kolosovski, L.; Platzer, E.; Dovjak, P.; Flick, H.; Tziraki, C.; Illario, M. The Role of Health Determinants in the Influenza Vaccination Uptake among Older Adults (65+): A Scope Review. Aging Clin. Exp. Res. 2021, 33, 2123–2132. [Google Scholar] [CrossRef] [PubMed]
- Kan, T.; Zhang, J. Factors Influencing Seasonal Influenza Vaccination Behaviour among Elderly People: A Systematic Review. Public Health 2018, 156, 67–78. [Google Scholar] [CrossRef] [PubMed]
- Okoli, G.N.; Abou-Setta, A.M.; Neilson, C.J.; Chit, A.; Thommes, E.; Mahmud, S.M. Determinants of Seasonal Influenza Vaccine Uptake Among the Elderly in the United States: A Systematic Review and Meta-Analysis. Gerontol. Geriatr. Med. 2019, 5, 233372141987034. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping Studies: Towards a Methodological Framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Porritt, K.; Gomersall, J.; Lockwood, C. JBI’s Systematic Reviews: Study Selection and Critical Appraisal. AJN Am. J. Nurs. 2014, 114, 47–52. [Google Scholar] [CrossRef]
- Hong, Q.N.; Pluye, P.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.-P.; Griffiths, F.; Nicolau, B.; et al. Mixed Methods Appraisal Tool (MMAT), Version 2018. Regist. Copyr. 2018, 1148552, 1–7. [Google Scholar]
- Nexøe, J.; Kragstrup, J.; Søgaard, J. Decision on Influenza Vaccination among the Elderly: A Questionnaire Study Based on the Health Belief Model and the Multidimensional Locus of Control Theory. Scand. J. Prim. Health Care 1999, 17, 105–110. [Google Scholar] [CrossRef]
- Bosompra, K.; Ashikaga, T.; Ruby, A. Attitudes, Perceived Norms, and Intentions: A Needs Assessment Study of the Influenza Immunization Intentions of Eldery Citizens in Vermont. J. Rural Health 2004, 20, 125–130. [Google Scholar] [CrossRef]
- Zimmerman, R.K.; Nowalk, M.P.; Bardella, I.J.; Fine, M.J.; Janosky, J.E.; Santibanez, T.A.; Wilson, S.A.; Raymund, M. Physician and Practice Factors Related to Influenza Vaccination among the Elderly. Am. J. Prev. Med. 2004, 26, 1–10. [Google Scholar] [CrossRef]
- Tamara Adonis-Rizzo, M.; Jett, K.F. Health Beliefs of Haitian Elders Related to Influenza Prevention. Public Health Nurs. 2007, 24, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Anne-Laure, C.-B.; Jocelyn, R.; Nathanaël, L.; De-Lambal, X.; Fabrice, C.; Michel, S. Predictors of IV Behaviors during and after the 2009 Influenza Pandemic in France. Vaccine 2014, 32, 2007–2015. [Google Scholar] [CrossRef] [PubMed]
- Bödeker, B.; Remschmidt, C.; Schmich, P.; Wichmann, O. Why Are Older Adults and Individuals with Underlying Chronic Diseases in Germany Not Vaccinated against Flu? A Population-Based Study. BMC Public Health 2015, 15, 618. [Google Scholar] [CrossRef]
- Dyda, A.; MacIntyre, C.R.; McIntyre, P.; Newall, A.T.; Banks, E.; Kaldor, J.; Liu, B. Factors Associated with Influenza Vaccination in Middle and Older Aged Australian Adults According to Eligibility for the National Vaccination Program. Vaccine 2015, 33, 3299–3305. [Google Scholar] [CrossRef] [PubMed]
- Klett-Tammen, C.J.; Krause, G.; Seefeld, L.; Ott, J.J. Determinants of Tetanus, Pneumococcal and Influenza Vaccination in the Elderly: A Representative Cross-Sectional Study on Knowledge, Attitude and Practice (KAP). BMC Public Health 2016, 16, 121. [Google Scholar] [CrossRef]
- Ganczak, M.; Gil, K.; Korzeń, M.; Bażydło, M. Coverage and Influencing Determinants of Influenza Vaccination in Elderly Patients in a Country with a Poor Vaccination Implementation. Int. J. Environ. Res. Public Health 2017, 14, 665. [Google Scholar] [CrossRef]
- Rikin, S.; Scott, V.; Shea, S.; LaRussa, P.; Stockwell, M.S. Influenza Vaccination Beliefs and Practices in Elderly Primary Care Patients. J. Community Health 2018, 43, 201–206. [Google Scholar] [CrossRef]
- Kajikawa, N.; Kataoka, Y.; Goto, R.; Maeno, T.; Yokoya, S.; Umeyama, S.; Takahashi, S.; Maeno, T. Factors Associated with Influenza Vaccination in Japanese Elderly Outpatients. Infect. Dis. Health 2019, 24, 212–221. [Google Scholar] [CrossRef]
- Teo, L.M.; Smith, H.E.; Lwin, M.O.; Tang, W.E. Attitudes and Perception of Influenza Vaccines among Older People in Singapore: A Qualitative Study. Vaccine 2019, 37, 6665–6672. [Google Scholar] [CrossRef]
- Dardalas, I.; Pourzitaki, C.; Manomenidis, G.; Malliou, F.; Galanis, P.; Papazisis, G.; Kouvelas, D.; Bellali, T. Predictors of Influenza Vaccination among Elderly: A Cross-Sectional Survey in Greece. Aging Clin. Exp. Res. 2020, 32, 1821–1828. [Google Scholar] [CrossRef]
- Pietraszek, A.; Sobieszczańska, M.; Makuch, S.; Dróżdż, M.; Mazur, G.; Agrawal, S. Identification of Barriers Limiting the Use of Preventive Vaccinations against Influenza among the Elderly Population: A Cross-Sectional Analysis. Vaccines 2022, 10, 651. [Google Scholar] [CrossRef] [PubMed]
- Music, M.; Taylor, N.; McChesney, C.; Krustev, C.; Chirila, A.; Ji, C. Perspectives of Older Adults on COVID-19 and Influenza Vaccination in Ontario, Canada. J. Prim. Care Community Health 2023, 14, 21501319231214127. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; See, M.T.A.; Aloweni, F.; Koh, C.H.F.; Tan, C.G.I.; Xin, X.H.; Gan, W.H.; Low, L.L.; Lim, S.F. Factors Influencing the Uptake of Seasonal Influenza Vaccination among Community-Dwelling Older Adults during COVID-19: A Mixed Methods Study. Vaccines 2023, 11, 641. [Google Scholar] [CrossRef] [PubMed]
- Kwong, E.W.Y.; Lam, I.O.Y.; Chan, T.M.F. What Factors Affect Influenza Vaccine Uptake among Community-Dwelling Older Chinese People in Hong Kong General Outpatient Clinics? J. Clin. Nurs. 2009, 18, 960–971. [Google Scholar] [CrossRef]
- Victor, J.F.; Gomes, G.D.; Sarmento, L.R.; Soares, A.M.D.; Mota, F.R.D.; Leite, B.M.B.; Soares, E.S.; da Silva, M.J. Factors Associated with Vaccination against Influenza A (H1N1) in the Elderly. Rev. Esc. Enferm. Usp. 2014, 48, 57–64. [Google Scholar] [CrossRef]
- Yu, D.S.F.; Low, L.P.L.; Lee, I.F.K.; Lee, D.T.F.; Ng, W.M. Predicting Influenza Vaccination Intent among At-Risk Chinese Older Adults in Hong Kong. Nurs. Res. 2014, 63, 270–277. [Google Scholar] [CrossRef]
- Mo, P.K.H.; Lau, J.T.F. Influenza Vaccination Uptake and Associated Factors among Elderly Population in Hong Kong: The Application of the Health Belief Model. Health Educ. Res. 2015, 30, 706–718. [Google Scholar] [CrossRef]
- Praphasiri, P.; Ditsungnoen, D.; Sirilak, S.; Rattanayot, J.; Areerat, P.; Dawood, F.S.; Lindblade, K.A. Predictors of Seasonal Influenza Vaccination among Older Adults in Thailand. PLoS ONE 2017, 12, e0188422. [Google Scholar] [CrossRef]
- Wu, S.; Su, J.; Yang, P.; Zhang, H.; Li, H.; Chu, Y.; Hua, W.; Li, C.; Tang, Y.; Wang, Q. Factors Associated with the Uptake of Seasonal Influenza Vaccination in Older and Younger Adults: A Large, Population-Based Survey in Beijing, China. BMJ Open 2017, 7, e017459. [Google Scholar] [CrossRef]
- Ye, C.; Zhu, W.; Yu, J.; Li, Z.; Hu, W.; Hao, L.; Wang, Y.; Xu, H.; Sun, Q.; Zhao, G. Low Coverage Rate and Awareness of Influenza Vaccine among Older People in Shanghai, China: A Cross-Sectional Study. Hum. Vaccin. Immunother. 2018, 14, 2715–2721. [Google Scholar] [CrossRef]
- Gazibara, T.; Kovacevic, N.; Kisic-Tepavcevic, D.; Nurkovic, S.; Kurtagic, I.; Gazibara, T.; Pekmezovic, T. Flu Vaccination among Older Persons: Study of Knowledge and Practices. J. Health Popul. Nutr. 2019, 38, 2. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Shang, X.; Lin, J.; Zhao, Y.; Wang, W.; Qiu, Y. Impacts of Free Vaccination Policy and Associated Factors on Influenza Vaccination Behavior of the Elderly in China: A Quasi-Experimental Study. Vaccine 2021, 39, 846–852. [Google Scholar] [CrossRef] [PubMed]
- Kizmaz, M.; Kumtepe Kurt, B.; Çetin Kargin, N.; Döner, E. Influenza, Pneumococcal and Herpes Zoster Vaccination Rates among Patients over 65 Years of Age, Related Factors, and Their Knowledge and Attitudes. Aging Clin. Exp. Res. 2020, 32, 2383–2391. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Or, P.P.L.; Chung, J.W.Y. The Effects of Health Literacy in Influenza Vaccination Competencies among Community-Dwelling Older Adults in Hong Kong. BMC Geriatr. 2020, 20, 103. [Google Scholar] [CrossRef]
- Kharroubi, G.; Cherif, I.; Bouabid, L.; Gharbi, A.; Boukthir, A.; Ben Alaya, N.; Ben Salah, A.; Bettaieb, J. Influenza Vaccination Knowledge, Attitudes, and Practices among Tunisian Elderly with Chronic Diseases. BMC Geriatr. 2021, 21, 700. [Google Scholar] [CrossRef]
- Siu, J.Y. Perceptions of Seasonal Influenza and Pneumococcal Vaccines Among Older Chinese Adults. Gerontologist 2021, 61, 439–448. [Google Scholar] [CrossRef]
- Zhou, Y.; Tang, J.; Zhang, J.; Wu, Q. Impact of the Coronavirus Disease 2019 Epidemic and a Free Influenza Vaccine Strategy on the Willingness of Residents to Receive Influenza Vaccines in Shanghai, China. Hum. Vaccin. Immunother. 2021, 17, 2289–2292. [Google Scholar] [CrossRef]
- Che, X.; Liu, Y.; Gu, W.; Wang, F.; Wang, J.; Jiang, W.; Du, J.; Zhang, X.; Xu, Y.; Zhang, X.; et al. Analysis on the Intention and Influencing Factors of Free Influenza Vaccination among the Elderly People Aged 70 and above in Hangzhou in 2022. Front. Public Health 2022, 10, 1052500. [Google Scholar] [CrossRef]
- Hou, Z.; Guo, J.; Lai, X.; Zhang, H.; Wang, J.; Hu, S.; Du, F.; Francis, M.R.; Fang, H. Influenza Vaccination Hesitancy and Its Determinants among Elderly in China: A National Cross-Sectional Study. Vaccine 2022, 40, 4806–4815. [Google Scholar] [CrossRef]
- You, Y.; Li, X.; Chen, B.; Zou, X.; Liu, G.; Han, X. Knowledge, Attitude, and Practice towards Influenza Vaccination among Older Adults in Southern China during the COVID-19 Pandemic. Vaccines 2023, 11, 1197. [Google Scholar] [CrossRef]
- Shen, Y.; Wang, J.; Zhao, Q.; Lv, M.; Wu, J.; Nicholas, S.; Maitland, E.; He, P.; Zhu, D. Predicting Future Vaccination Habits: The Link between Influenza Vaccination Patterns and Future Vaccination Decisions among Old Aged Adults in China. J. Infect. Public Health 2024, 17, 1079–1085. [Google Scholar] [CrossRef] [PubMed]
- Zhao, P.Z.; Xu, W.Q.; Wang, J.S.; Liang, P.; Li, H.Y.; Wang, C. Uptake and Correlates of Influenza Vaccine among Older Adults Residing in Rural Regions of South China: A Cross-Sectional Study. Front. Public Health 2024, 12, 1383293. [Google Scholar] [CrossRef]
- Kwong, E.W.Y.; Pang, S.M.C.; Choi, P.P.; Wong, T.K.S. Influenza Vaccine Preference and Uptake among Older People in Nine Countries. J. Adv. Nurs. 2010, 66, 2297–2308. [Google Scholar] [CrossRef] [PubMed]
- Schulz, P.J.; Wu, Y.-C.; An, S.; Chen, F.-L. Social Influences on Influenza Vaccination Decision Among Senior Citizens in Taiwan, South Korea, and Switzerland. Front. Commun. 2019, 4, 74. [Google Scholar] [CrossRef]
- Larson, H.J.; Cooper, L.Z.; Eskola, J.; Katz, S.L.; Ratzan, S. Addressing the Vaccine Confidence Gap. Lancet 2011, 378, 526–535. [Google Scholar] [CrossRef]
- Larson, H.J.; de Figueiredo, A.; Xiahong, Z.; Schulz, W.S.; Verger, P.; Johnston, I.G.; Cook, A.R.; Jones, N.S. The State of Vaccine Confidence 2016: Global Insights Through a 67-Country Survey. eBioMedicine 2016, 12, 295–301. [Google Scholar] [CrossRef]
- Harrison, E.A.; Wu, J.W. Vaccine Confidence in the Time of COVID-19. Eur. J. Epidemiol. 2020, 35, 325–330. [Google Scholar] [CrossRef]
- Majid, U.; Wasim, A.; Bakshi, S.; Truong, J. Knowledge, (Mis-)Conceptions, Risk Perception, and Behavior Change during Pandemics: A Scoping Review of 149 Studies. Public Underst. Sci. 2020, 29, 777–799. [Google Scholar] [CrossRef]
- Oboka, I.O. Studying the Evolution of Pandemic Preparedness on Influenza and COVID-19: The Role of Risk Communication. Master’s Thesis, UIS, Stavanger, Norway, 2024. [Google Scholar]
- Nypaver, C.; Dehlinger, C.; Carter, C. Influenza and Influenza Vaccine: A Review. J. Midwifery Women’s Health 2021, 66, 45–53. [Google Scholar] [CrossRef]
- Betsch, C.; Böhm, R.; Chapman, G.B. Using Behavioral Insights to Increase Vaccination Policy Effectiveness. Policy Insights Behav. Brain Sci. 2015, 2, 61–73. [Google Scholar] [CrossRef]
- Ni, L.; Chen, Y.; De Brujin, O. Towards Understanding Socially Influenced Vaccination Decision Making: An Integrated Model of Multiple Criteria Belief Modelling and Social Network Analysis. Eur. J. Oper. Res. 2021, 293, 276–289. [Google Scholar] [CrossRef]
- Mirza, R.; Hull, J.; Peng, S.; Mousavi, Y.; Mustafa, M.I.; Papageorgiou, P.; Rotgaus, E.; Hsieh, J. Going Viral: Understanding Medical Misinformation and Older Adults’ Vaccine Hesitancy. Innov. Aging 2020, 4, 377–378. [Google Scholar] [CrossRef]
- Pakalniškienė, V.; Kairys, A.; Jurkuvėnas, V.; Mikuličiūtė, V.; Ivleva, V. Could Belief in Fake News Predict Vaccination Behavior in the Elderly? Int. J. Environ. Res. Public Health 2022, 19, 14901. [Google Scholar] [CrossRef] [PubMed]
- Jiang, M.; Chen, S.; Yan, X.; Ying, X.; Tang, S. The Coverage and Challenges of Increasing Uptake of Non-National Immunization Program Vaccines in China: A Scoping Review. Infect. Dis. Poverty 2023, 12, 114. [Google Scholar] [CrossRef]
- Chen, S.; Rodewald, L.E.; Du, A.H.; Tang, S. Advancing the National Immunization Program in an Era of Achieving Universal Vaccine Coverage in China and Beyond. Infect. Dis. Poverty 2024, 13, 25. [Google Scholar] [CrossRef]
- Welch, V.L.; Metcalf, T.; Macey, R.; Markus, K.; Sears, A.J.; Enstone, A.; Langer, J.; Srivastava, A.; Cane, A.; Wiemken, T.L. Understanding the Barriers and Attitudes toward Influenza Vaccine Uptake in the Adult General Population: A Rapid Review. Vaccines 2023, 11, 180. [Google Scholar] [CrossRef]
- Yue, M.; Wang, Y.; Low, C.K.; Yoong, J.S.; Cook, A.R. Optimal Design of Population-Level Financial Incentives of Influenza Vaccination for the Elderly. Value Health 2020, 23, 200–208. [Google Scholar] [CrossRef]
- Wu, D.; Jin, C.; Bessame, K.; Tang, F.F.-Y.; Ong, J.J.; Wang, Z.; Xie, Y.; Jit, M.; Larson, H.J.; Chantler, T.; et al. Effectiveness of a Pay-It-Forward Intervention Compared with User-Paid Vaccination to Improve Influenza Vaccine Uptake and Community Engagement among Children and Older Adults in China: A Quasi-Experimental Pragmatic Trial. Lancet Infect. Dis. 2022, 22, 1484–1492. [Google Scholar] [CrossRef]
- Yoo, B.-K.; Kasajima, M.; Phelps, C.E.; Fiscella, K.; Bennett, N.M.; Szilagyi, P.G. Influenza Vaccine Supply and Racial/Ethnic Disparities in Vaccination among the Elderly. Am. J. Prev. Med. 2011, 40, 1–10. [Google Scholar] [CrossRef]
- Brewer, L.I.; Ommerborn, M.J.; Nguyen, A.L.; Clark, C.R. Structural Inequities in Seasonal Influenza Vaccination Rates. BMC Public Health 2021, 21, 1166. [Google Scholar] [CrossRef]
- Fayaz Farkhad, B.; Karan, A.; Albarracín, D. Longitudinal Pathways to Influenza Vaccination Vary with Socio-Structural Disadvantages. Ann. Behav. Med. 2022, 56, 472–483. [Google Scholar] [CrossRef] [PubMed]
- Bhanu, C.; Gopal, D.P.; Walters, K.; Chaudhry, U.A. Vaccination Uptake amongst Older Adults from Minority Ethnic Backgrounds: A Systematic Review. PLoS Med. 2021, 18, e1003826. [Google Scholar] [CrossRef] [PubMed]
- Bazargan, M.; Martinez-Hollingsworth, A.; Cobb, S.; Kibe, L.W. Correlates of Influenza Vaccination among Underserved Latinx Middle-Aged and Older Adults: A Cross-Sectional Survey. BMC Public Health 2022, 22, 907. [Google Scholar] [CrossRef] [PubMed]
- Bianconi, A.; Zanutto, G.; Castagna, G.; Coa, A.A.; De Gioia, E.R.; Longo, G.; Sicari, G.; Tomaiuolo, G.; Todeschini, R.; Pandolfi, P.; et al. Language Barriers during Vaccination Practice, the Point of View of Healthcare Providers. Ann. Ig. 2024, 36, 462–475. [Google Scholar] [CrossRef]
- Browne, M.; Thomson, P.; Rockloff, M.J.; Pennycook, G. Going against the Herd: Psychological and Cultural Factors Underlying the “Vaccination Confidence Gap”. PLoS ONE 2015, 10, e0132562. [Google Scholar] [CrossRef]
- Kisa, S.; Kisa, A. Religious Beliefs and Practices toward HPV Vaccine Acceptance in Islamic Countries: A Scoping Review. PLoS ONE 2024, 19, e0309597. [Google Scholar] [CrossRef]
- Ma, M.Z.; Chen, S.X.; Wang, X. Looking beyond Vaccines: Cultural Tightness–Looseness Moderates the Relationship between Immunization Coverage and Disease Prevention Vigilance. Appl. Psych Health Amp. Well 2024, 16, 1046–1072. [Google Scholar] [CrossRef]
- Doherty, T.M.; Ecarnot, F.; Gaillat, J.; Privor-Dumm, L. Nonstructural Barriers to Adult Vaccination. Hum. Vaccines Immunother. 2024, 20, 2334475. [Google Scholar] [CrossRef]
- Walsh, M.M.; Parker, A.M.; Vardavas, R.; Nowak, S.A.; Kennedy, D.P.; Gidengil, C.A. The Stability of Influenza Vaccination Behavior over Time: A Longitudinal Analysis of Individuals across 8 Years. Ann. Behav. Med. 2020, 54, 783–793. [Google Scholar] [CrossRef]
| Study | Year Country (Region) | Study Type | Study Population and Sample Size | Study Timeline |
|---|---|---|---|---|
| High Income Countries (HIC) | ||||
| Nexøe J et al. [22] | 1999 Demark (National) | Quantitative | 1775 individuals aged ≥ 65 years | 1996 to 1997 |
| Bosompra K et al. [23] | 2004 USA (Vermont) | Quantitative | 799 individuals aged ≥ 65 years | 2000 |
| Zimmerman K et al. [24] | 2004 USA (Pennsylvania) | Quantitative | 925 individuals aged ≥ 65 years | 2000 |
| Adonis-Rizzo T et al. [25] | 2007 USA (Florida) | Qualitative | 10 individuals aged ≥ 60 years | 2005 to 2006 |
| Anne-Laure B et al. [26] | 2014 France (National) | Quantitative | 269 individuals aged ≥ 65 years | 2009 to 2010 |
| Bodekers B et al. [27] | 2015 Germany (National) | Quantitative | 760 individuals aged ≥ 65 years | 2014 |
| Dyda A et al. [28] | 2015 Australia (New South Wales) | Quantitative | 7332 individuals aged ≥ 65 years | 2006 to 2008 |
| Klett-Tammen J et al. [29] | 2016 Germany (National) | Quantitative | 1223 individuals aged ≥ 60 years | 2012 to 2015 |
| Ganczak M et al. [30] | 2017 Poland (Szczecin) | Quantitative | 230 individuals aged ≥ 65 years | 2015 to 2016 |
| Rikin S et al. [31] | 2018 USA (New York) | Mixed-Methods | 200 Hispanic individuals aged ≥ 65 years | 2016 |
| Kajikawa N et al. [32] | 2019 Japan (Ibaraki) | Quantitative | 316 persons aged above 65 years | 2018 |
| Teo M et al. [33] | 2019 Singapore (National) | Qualitative | 15 individuals aged ≥ 65 years | 2017 |
| Dardalas I et al. [34] | 2020 Greece (4 Regions) | Quantitative | 318 individuals aged ≥ 60 years | 2018 |
| Nicholls B et al. [9] | 2021 UK (National) | Quantitative | 372 individuals aged ≥ 65 years | 2020 |
| Pietraszek A et al. [35] | 2022 Poland (National) | Quantitative | 500 individuals aged ≥ 60 years | 2020 |
| Music M et al. [36] | 2023 Canada (Ontrario) | Mixed-Methods | 33 individuals aged ≥ 65 years | 2021 to 2022 |
| Xu Y et al. [37] | 2023 Singapore (National) | Mixed-Methods | 235 individuals aged ≥ 65 years | 2020 to 2021 |
| Fuller R et al. [8] | 2024 USA (North Dakota) | Quantitative | 901 individuals aged ≥ 65 years | 2022 |
| Middle Income Countries (MIC) | ||||
| Kwong Y et al. [38] | 2009 China (Hongkong) | Quantitative | 197 individuals aged ≥ 65 years | 2005 |
| Victor F et al. [39] | 2014 Brazil (Fortaleza) | Quantitative | 286 individuals aged ≥ 60 years | 2010 to 2011 |
| Yu S et al. [40] | 2014 China (Hongkong) | Quantitative | 306 individuals aged ≥ 65 years | 2011 |
| Mo H et al. [41] | 2015 China (Hongkong) | Quantitative | 1101 individuals aged ≥ 65 years | 2009 |
| Praphasiri P et al. [42] | 2017 Thailand (Nakhon Phano) | Quantitative | 581 individuals aged ≥ 65 years | 2014 |
| Wu S et al. [43] | 2017 China (Beijing) | Quantitative | 1362 individuals aged ≥ 60 years | 2015 |
| Ye C et al. [44] | 2018 China (Shanghai) | Quantitative | 4417 individuals aged ≥ 60 years | 2016 to 2017 |
| Gazibara T et al. [45] | 2019 Serbia (Belgrade) | Quantitative | 480 individuals aged ≥ 65 years | 2012 to 2013 |
| Jiang X et al. [46] | 2020 China (Zhejiang) | Quantitative | 1210 individuals aged ≥ 60 years | 2019 |
| Kizmaz M et al. [47] | 2020 Turkey (Gemerek) | Quantitative | 326 individuals aged ≥ 65 years | 2019 |
| Zhang F et al. [48] | 2020 China (Hongkong) | Quantitative | 486 individuals aged ≥ 65 years | 2016 |
| Kharroubi G et al. [49] | 2021 Tunisia (National) | Quantitative | 1191 individuals aged ≥ 60 years with chronic disease | 2019 |
| Siu Y et al. [50] | 2021 China (Hongkong) | Qualitative | 40 individuals aged ≥ 65 years | 2016 |
| Zhou Y et al. [51] | 2021 China (Shanghai) | Quantitative | 445 individuals aged ≥ 60 years | 2020 |
| Che X et al. [52] | 2022 China (Hangzhou) | Quantitative | 11,663 individuals aged ≥ 70 years | 2022 |
| Hou Z et al. [53] | 2022 China (National) | Quantitative | 3849 individuals aged ≥ 60 years | 2019 |
| You Y et al. [54] | 2023 China (Shenzhen) | Quantitative | 975 individuals aged ≥ 60 years | 2021 |
| Shen Y et al. [55] | 2024 China (Beijing) | Quantitative | 540 individuals aged ≥ 65 years | 2016 to 2020 |
| Zhao Z et al. [56] | 2024 China (Guangdong) | Quantitative | 423 individuals aged ≥ 60 years | 2023 |
| Mixed | ||||
| Kwong Y et al. [57] | 2010 Multiple | Qualitative | 208 individuals aged ≥ 65 years | 2006 to 2007 |
| Schulz J et al. [58] | 2019 Multiple | Quantitative | 627 individuals aged ≥ 65 years | 2017 |
| Study | BeSD Domains | Theoretical Model | Sociodemographic Characteristics | Health-Related Factors | Outcomes | |||
|---|---|---|---|---|---|---|---|---|
| Thinking and Feeling | Social Process | Motivation | Practical Issues | |||||
| High Income Countries (HIC) | ||||||||
| Nexøe J et al., 1999 [22] | * Perceived benefits, Perceived severity # Perceived barriers | Health belief model, Multidimensional health locus of control | Age, Living status, Residence | Influenza vaccination history | Influenza vaccination behavior | |||
| Bosompra K et al., 2004 [23] | * Perceived benefits, Normative beliefs about vaccination | The theory of reasoned action | Influenza vaccination behavior | |||||
| Zimmerman K et al., 2004 [24] | * Risk perception | * Recommendation from HCWs | * Vaccination intention | The theory of reasoned action | Residence | Cancer screening history | Influenza vaccination behavior | |
| Adonis-Rizzo T et al., 2007 [25] | * Fear of illness | * Recommendation from HCWs | # Lack of insurance, Transportation and geographic barriers, Language barriers ^ | Health belief model | Influenza vaccination behavior or intention | |||
| Anne-Laure B et al., 2014 [26] | * Social trust | Influenza vaccination behavior | ||||||
| Bodekers B et al., 2015 [27] | * Risk Perception, Positive vaccine attitude # Fear of side effects | * Recommendation from HCWs | Gender, Age | Chronic diseases | Influenza vaccination behavior | |||
| Dyda A et al., 2015 [28] | * Free cost # Language and cultural barriers ^ | Age, Sex, Income, Education level, Country, Region, Career status | Obesity, Physical assistance need, Chronic diseases | Influenza vaccination behavior | ||||
| Klett-Tammen J et al., 2016 [29] | * Vaccine confidence | * Recommendation from HCWs | Influenza vaccination behavior | |||||
| Ganczak M et al., 2017 [30] | * Family influence, Information provision | * Vaccination intention | Age | Health status, Comorbidities | Influenza vaccination behavior | |||
| Rikin S et al., 2018 [31] | # Fear of side effects | Influenza vaccination behavior | ||||||
| Kajikawa N et al., 2019 [32] | * Vaccine confidence | * Recommendation from HCWs | Age | Influenza vaccination behavior | ||||
| Teo M et al., 2019 [33] | # Fear of side effects, Perceived low risk | * Recommendation from HCWs, Recommendation from Family, Recommendation from Friends | Influenza vaccination intention | |||||
| Dardalas I et al., 2020 [34] | * Behavioral beliefs, Control beliefs | * Family influence, Peer influence | * Vaccination intention | Theory of planned behavior | Gender | Influenza vaccination behavior and intention | ||
| Nicholls B et al., 2021 [9] | * Risk perception, Preference for natural immunity ^ | * Collective Responsibility | Influenza vaccination behavior | |||||
| Pietraszek A et al., 2022 [35] | * Risk Perception (Context: COVID-19 pandemic) | Income | Chronic disease | Influenza vaccination behavior | ||||
| Music M et al., 2023 [36] | * Vaccine confidence | * Social trust, Information provision # Misinformation | # Vaccine hesitancy | Influenza vaccination behavior | ||||
| Xu Y et al., 2023 [37] | * Risk perception (Context: COVID-19 pandemic) # Fear of side effects, Lack of vaccine confidence | * Collective responsibility | # High cost | Living status | Influenza vaccination behavior | |||
| Fuller R et al., 2024 [8] | # Fear of injections | # Lack of recommendation from HCWs | # High costs, Accessibility barriers | Residence, Educational level, Ethnicity, Living conditions | Influenza vaccination behavior within the previous 5 years | |||
| Middle Income Countries (MIC) | ||||||||
| Kwong Y et al., 2009 [38] | * Perceived susceptibility, Perceived severity, Perceived benefits # Perceived barriers | * Recommendation from HCWs, Recommendation from family | Health belief model | Influenza vaccination behavior | ||||
| Victor F et al., 2014 [39] | * Perceived benefits | * Recommendation from HCWs | * Information accessibility | Age | Chronic disease, Medication use, Regular health monitoring, Frequency of visits to FHCs, Participation in FHC groups | Influenza vaccination behavior | ||
| Yu S et al., 2014 [40] | * Perceived susceptibility | # Postvaccination discomfort | Influenza vaccination intention | |||||
| Mo H et al., 2015 [41] | * Risk perception, Fear of side effects | * Recommendation from HCWs, Community engagement | * Low cost | Age | Chronic diseases | Past influenza vaccination behavior, Influenza vaccination intention | ||
| Praphasiri P et al., 2017 [42] | * Vaccine confidence | * Recommendation from HCWs | # Accessibility barriers | Fragile | Influenza vaccination behavior | |||
| Wu S et al., 2017 [43] | * Risk perception # Fear of side effects | * Recommendation from HCWs | * Free cost | Education level | Chronic disease | Influenza vaccination behavior | ||
| Ye C et al., 2018 [44] | # Low vaccine literacy | Living status | Influenza vaccination behavior | |||||
| Gazibara T et al., 2019 [45] | * Vaccine literacy, Vaccine confidence # Fear of side effects, Perceived low risk | * Recommendation from HCWs, Family influence | Educational level | Influenza vaccination behavior | ||||
| Jiang X et al., 2020 [46] | * Vaccine literacy, Risk Perception, Vaccine confidence | * Free cost | Age, Education level, Income, Family construct | Health status | Influenza vaccination behavior | |||
| Kizmaz M et al., 2020 [47] | * Recommendation from HCWs | Influenza vaccination behavior | ||||||
| Zhang F et al., 2020 [48] | * Vaccine literacy # Cognitive overload, Decisional conflict | # Limited information access | Age, Education level | Health condition | Influenza vaccination behavior | |||
| Kharroubi G et al., 2021 [49] | * Vaccine literacy, Vaccine confidence # Fear of side effects | Past influenza vaccination behavior, Influenza vaccination intention | ||||||
| Siu Y et al., 2021 [50] | # Negative vaccine beliefs, low perceived susceptibility, Perceived risk posed by the vaccination locations ^, Stereotypes of hospitals and clinics ^ | # Misinformation, Limited provider engagement | Health belief model | Influenza vaccination decision-making processes | ||||
| Zhou Y et al., 2021 [51] | * Vaccination Intention (Context: COVID-19 pandemic) | * Free cost | Influenza vaccination behavior | |||||
| Che X et al., 2022 [52] | * Vaccine literacy | * Social trust | * Vaccination convenience | Age, Education level, Region | Influenza vaccination intention | |||
| Hou Z et al., 2022 [53] | * Risk perception, Vaccine confidence # Fear of side effects | # Vaccine hesitancy | * Free cost | 3Cs Model | Gender, Educational level, Residence | Influenza vaccination behavior | ||
| You Y et al., 2023 [54] | * Vaccine Confidence, Vaccine literacy | Age, Marital status, Education level, Income | COVID-19 vaccination history | Influenza vaccination behavior | ||||
| Shen Y et al., 2024 [55] | * Vaccine confidence # Perceived low risk | # Accessibility barriers | Age, Income, Residence | Chronic disease | Influenza vaccination behavior within 5 years | |||
| Zhao Z et al., 2024 [56] | * Positive vaccine attitude, Risk perception # Low vaccine literacy, Perceived cost barriers | * Social trust | # Vaccine hesitancy | Income, Rural area | Influenza vaccination behavior | |||
| Mixed | ||||||||
| Kwong Y et al., 2010 [57] | * Perceived risk, Vaccine confidence # Fear of side effects, Fear of injections, Preference for natural immunity ^ | * Recommendation from HCWs, Family influence, Peer influence, Community norms | * Vaccination intention, Moral motivation | # High cost, Accessibility issues, Vaccine availability shortages, Health system barriers (e.g., insurance coverage, ease of access) | Health belief model | Health condition, Chronic disease, Traditional health practices | Influenza vaccination behavior | |
| Schulz J et al., 2019 [58] | * Recommendation from HCWs, Recommendation from Family, Recommendation from Friends | Age, Sex | Influenza vaccination behavior | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, E.; Shang, S.; Xing, Y.; Cui, J.; Pan, C.; Seale, H.; Fang, Q. Mapping Behavioral and Social Drivers of Influenza Vaccine Uptake in Older Adults: A Scoping Review. Vaccines 2025, 13, 624. https://doi.org/10.3390/vaccines13060624
Zhang E, Shang S, Xing Y, Cui J, Pan C, Seale H, Fang Q. Mapping Behavioral and Social Drivers of Influenza Vaccine Uptake in Older Adults: A Scoping Review. Vaccines. 2025; 13(6):624. https://doi.org/10.3390/vaccines13060624
Chicago/Turabian StyleZhang, Enming, Shuhui Shang, Yufei Xing, Jiasong Cui, Chen Pan, Holly Seale, and Qiong Fang. 2025. "Mapping Behavioral and Social Drivers of Influenza Vaccine Uptake in Older Adults: A Scoping Review" Vaccines 13, no. 6: 624. https://doi.org/10.3390/vaccines13060624
APA StyleZhang, E., Shang, S., Xing, Y., Cui, J., Pan, C., Seale, H., & Fang, Q. (2025). Mapping Behavioral and Social Drivers of Influenza Vaccine Uptake in Older Adults: A Scoping Review. Vaccines, 13(6), 624. https://doi.org/10.3390/vaccines13060624






