Generation of a Transgenic Plasmodium cynomolgi Parasite Expressing Plasmodium vivax Circumsporozoite Protein for Testing P. vivax CSP-Based Malaria Vaccines in Non-Human Primates
Abstract
1. Introduction
2. Materials and Methods
2.1. Optimization of In Vitro Parasite Culturing Conditions
2.2. In Vitro Culturing of Pcy Berok K2 Parasites
2.3. Parasite Synchronization
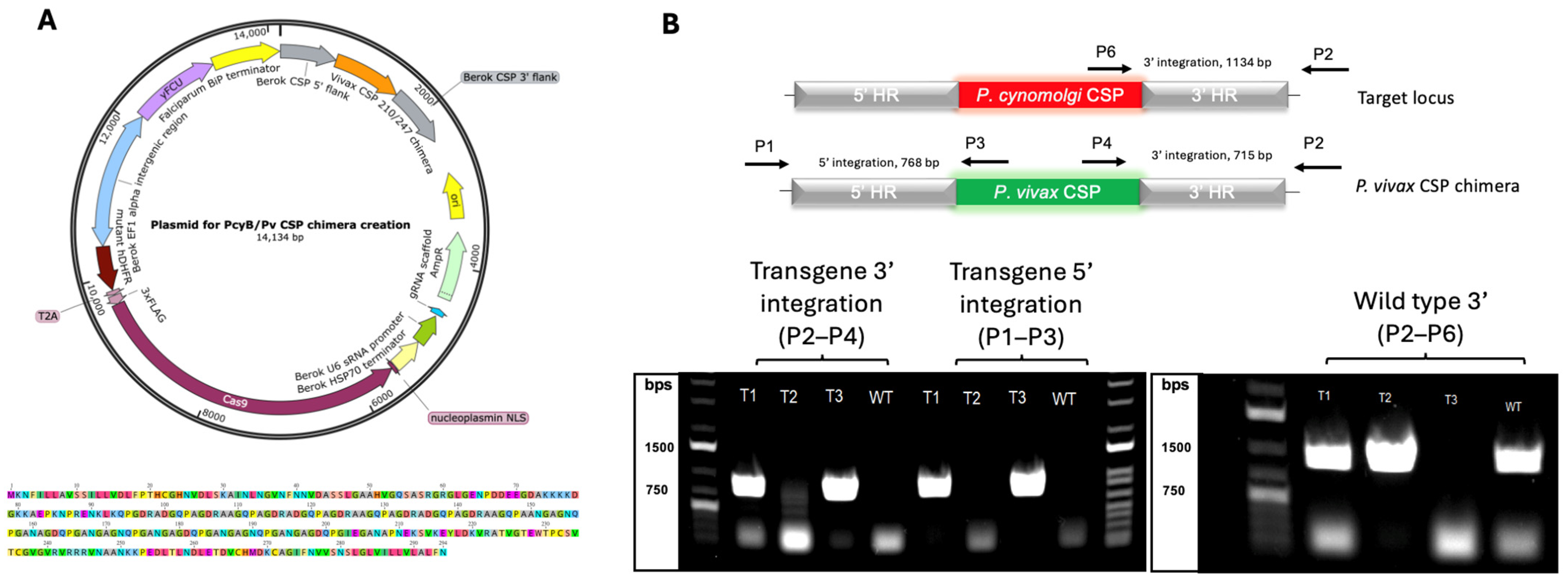
2.4. The Generation of a Cas9 Plasmid for the Editing of P. cynomolgi
2.5. The Generation of a Chimeric Pv CSP Cassette to Replace Pcy Berok CSP
2.6. Nucleofection of Pcy Berok K2 Parasites
2.7. Genotyping and Sequencing of Pcy Transgenic Parasites
2.8. Mosquito Infections
2.9. Immunofluorescence Assay Demonstration of Sporozoite Specificity for P. cynomolgi CSP Antibodies
2.10. Infection of NHPs
2.11. Quantification of Parasites in NHP Blood
3. Results
3.1. The Generation of a P. cynomolgi Parasite Expressing the P. vivax Circumsporozoite Protein
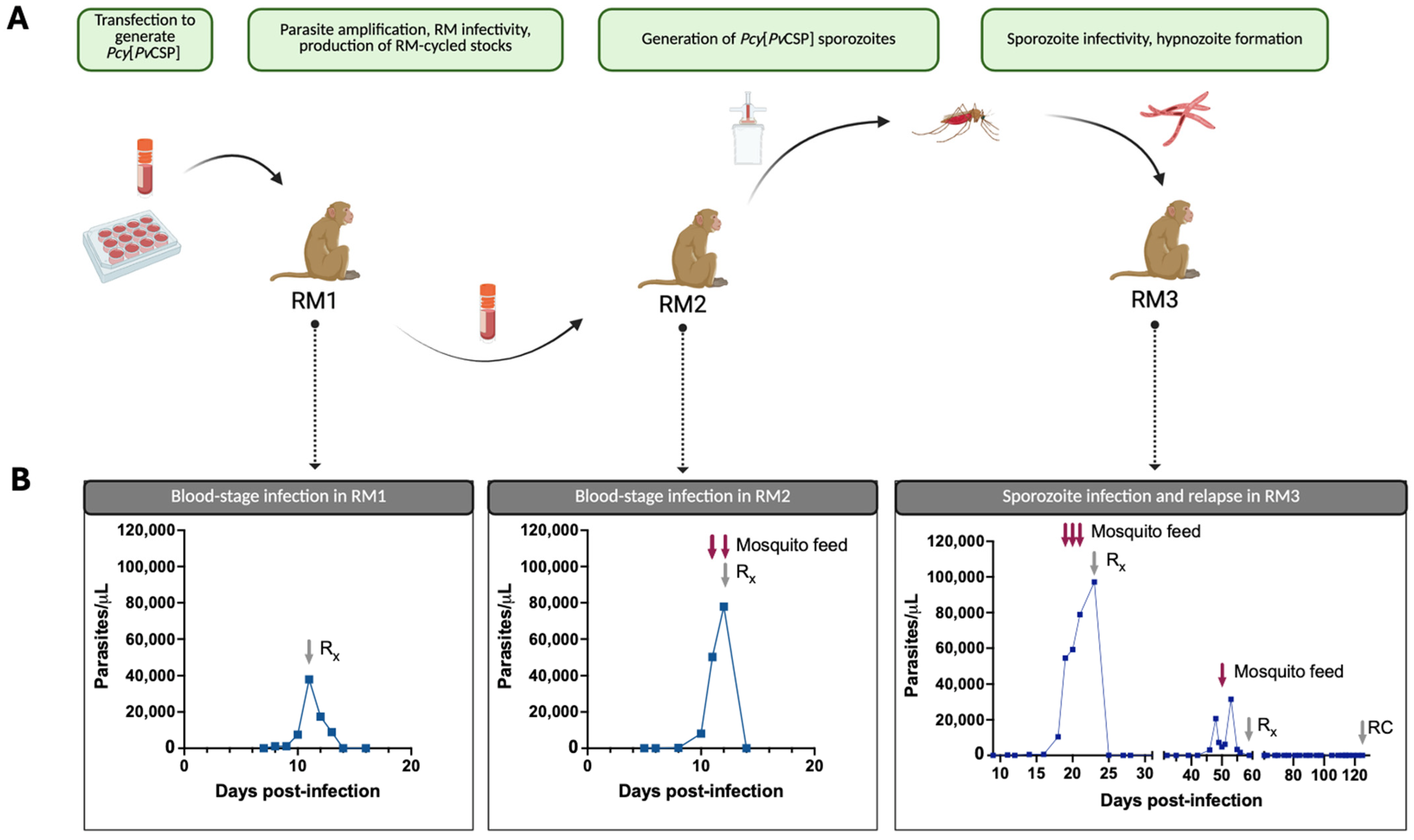
3.2. The Pcy[PvCSP] Transgenic Parasite Completes the Life Cycle Between Rhesus Macaques and Anopheles Mosquitoes
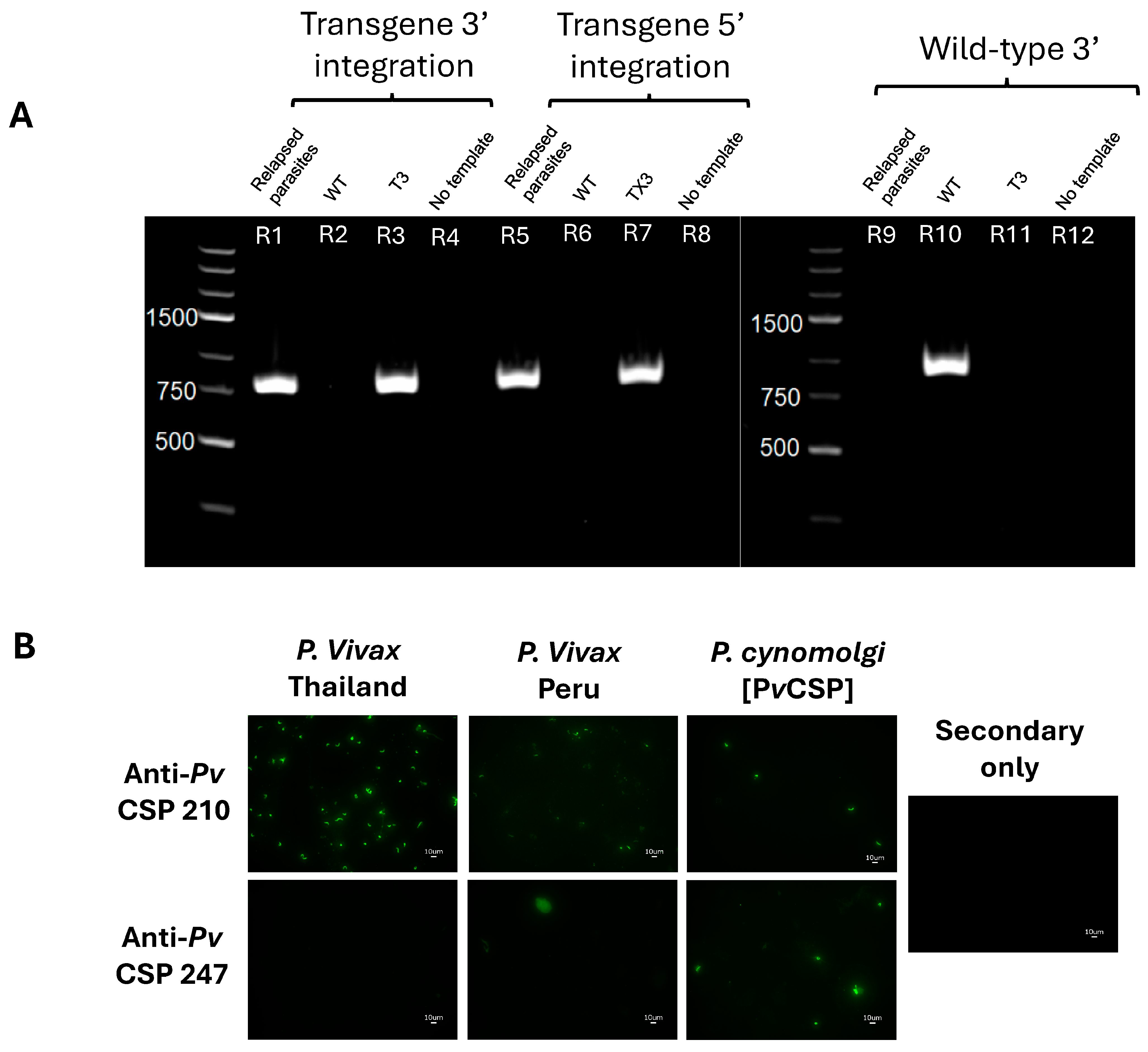
3.3. Transgenic Parasites Maintain Transgene Integrity and Protein Expression In Vivo
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AMA1 | Apical Membrane Antigen 1 |
| BSA | bovine serum albumin |
| DAPI | 4′,6-Diamidino-2-phenylindole |
| CSP | circumsporozoite protein |
| FcR | Fc (fragment crystallizable) receptor |
| IACUC | Institutional Animal Care and Use Committee |
| IFA | immunofluorescent assay |
| mAb | monoclonal antibody |
| NHP | non-human primate |
| OHSU | Oregon Health and Science University |
| PBS | phosphate-buffered saline |
| PCR/qRT-PCR | polymerase chain reaction/quantitative reverse transcriptase polymerase chain reaction |
| Pcy/Pf/Pv | Plasmodium cynomolgi/falciparum/vivax |
| Pcy[PvCSP] | Plasmodium cynomolgi expressing Plasmodium vivax circumsporozoite protein |
| RBC | red blood cell |
| RM | rhesus macaque |
| UTR | untranslated region |
| WT | wild-type |
References
- WHO. World Malaria Report 2024; World Health Organization: Geneva, Switzerland, 2024.
- World Health Organization. World Malaria Report 2022. Available online: https://www.who.int/teams/global-malaria-programme (accessed on 26 February 2023).
- Simwela, N.V.; Waters, A.P. Current status of experimental models for the study of malaria. Parasitology 2022, 149, 729–750. [Google Scholar] [CrossRef]
- Reyes-Sandoval, A. Plasmodium vivax pre-erythrocytic vaccines. Parasitol. Int. 2021, 84, 102411. [Google Scholar] [CrossRef] [PubMed]
- Adekunle, A.I.; Pinkevych, M.; McGready, R.; Luxemburger, C.; White, L.J.; Nosten, F.; Cromer, D.; Davenport, M.P. Modeling the dynamics of Plasmodium vivax infection and hypnozoite reactivation in vivo. PLoS Negl. Trop. Dis. 2015, 9, e0003595. [Google Scholar] [CrossRef]
- Anwar, M.N.; Hickson, R.I.; Mehra, S.; McCaw, J.M.; Flegg, J.A. A Multiscale Mathematical Model of Plasmodium Vivax Transmission. Bull. Math. Biol. 2022, 84, 81. [Google Scholar] [CrossRef] [PubMed]
- Duffy, P.E.; Patrick Gorres, J. Malaria vaccines since 2000: Progress, priorities, products. npj Vaccines. 2020, 5, 48. [Google Scholar] [CrossRef]
- Smith, R.C.; Vega-Rodríguez, J.; Jacobs-Lorena, M. The Plasmodium bottleneck: Malaria parasite losses in the mosquito vector. Mem. Do Inst. Oswaldo Cruz 2014, 109, 644–661. [Google Scholar] [CrossRef]
- Duffy, P.E. Current approaches to malaria vaccines. Curr. Opin. Microbiol. 2022, 70, 102227. [Google Scholar] [CrossRef]
- Cohen, J.; Nussenzweig, V.; Vekemans, J.; Leach, A. From the circumsporozoite protein to the RTS, S/AS candidate vaccine. Hum. Vaccin. 2010, 6, 90–96. [Google Scholar] [CrossRef]
- Ménard, R.; Sultan, A.A.; Cortes, C.; Altszuler, R.; van Dijk, M.R.; Janse, C.J.; Waters, A.P.; Nussenzweig, R.S.; Nussenzweig, V. Circumsporozoite protein is required for development of malaria sporozoites in mosquitoes. Nature 1997, 385, 336–339. [Google Scholar] [CrossRef]
- Zhu, F.; Zheng, H.; Chen, S.; Zhang, K.; Qin, X.; Zhang, J.; Liu, T.; Fan, Y.; Wang, L.; Li, X.; et al. Malaria oocysts require circumsporozoite protein to evade mosquito immunity. Nat. Commun. 2022, 13, 3208. [Google Scholar] [CrossRef]
- Hopp, C.S.; Chiou, K.; Ragheb, D.R.T.; Salman, A.M.; Khan, S.M.; Liu, A.J.; Sinnis, P. Longitudinal analysis of Plasmodium sporozoite motility in the dermis reveals component of blood vessel recognition. Elife 2015, 4, e07789. [Google Scholar] [CrossRef] [PubMed]
- Steward, M.J.; Vanderberg, J.P. Malaria Sporozoites Release Circumsporozoite Protein from Their Apical End and Translocate It along Their Surface. J. Protozool. 1991, 38, 411–421. [Google Scholar] [CrossRef]
- Zhao, J.; Bhanot, P.; Hu, J.; Wang, Q. A Comprehensive Analysis of Plasmodium Circumsporozoite Protein Binding to Hepatocytes. PLoS ONE 2016, 11, e0161607. [Google Scholar] [CrossRef]
- Arun Kumar, K.; Sano, G.I.; Boscardin, S.; Nussenzweig, R.S.; Nussenzweig, M.C.; Zavala, F.; Nussenzweig, V. The circumsporozoite protein is an immunodominant protective antigen in irradiated sporozoites. Nature 2006, 444, 937–940. [Google Scholar] [CrossRef]
- Davies, H.M.; Nofal, S.D.; McLaughlin, E.J.; Osborne, A.R. Repetitive sequences in malaria parasite proteins. FEMS Microbiol. Rev. 2017, 41, 923. [Google Scholar] [CrossRef]
- Kisalu, N.K.; Idris, A.H.; Weidle, C.; Flores-Garcia, Y.; Flynn, B.J.; Sack, B.K.; Murphy, S.; Schon, A.; Freire, E.; Francica, J.R.; et al. A human monoclonal antibody prevents malaria infection by targeting a new site of vulnerability on the parasite. Nat. Med. 2018, 24, 408–416. [Google Scholar] [CrossRef] [PubMed]
- Kisalu, N.K.; Pereira, L.D.; Ernste, K.; Flores-Garcia, Y.; Idris, A.H.; Asokan, M.; Dillon, M.; MacDonald, S.; Shi, W.; Chen, X.; et al. Enhancing durability of CIS43 monoclonal antibody by Fc mutation or AAV delivery for malaria prevention. J. Clin. Investig. 2021, 6, e143958. [Google Scholar] [CrossRef]
- Kayentao, K.; Ongoiba, A.; Preston, A.C.; Healy, S.A.; Hu, Z.; Skinner, J.; Doumbo, S.; Wang, J.; Cisse, H.; Doumtabe, D.; et al. Subcutaneous Administration of a Monoclonal Antibody to Prevent Malaria. N. Engl. J. Med. 2024, 390, 1549–1559. [Google Scholar] [CrossRef]
- da Veiga, G.T.S.; Moriggi, M.R.; Vettorazzi, J.F.; Müller-Santos, M.; Albrecht, L. Plasmodium vivax vaccine: What is the best way to go? Front. Immunol. 2022, 13, 910236. [Google Scholar] [CrossRef]
- Roobsoong, W.; Yadava, A.; Draper, S.J.; Minassian, A.M.; Sattabongkot, J. The challenges of Plasmodium vivax human malaria infection models for vaccine development. Front. Immunol. 2022, 13, 1006954. [Google Scholar] [CrossRef]
- Collins, K.A.; Wang, C.Y.T.; Adams, M.; Mitchell, H.; Robinson, G.J.; Rampton, M.; Elliott, S.; Odedra, A.; Khoury, D.; Ballard, E.; et al. A Plasmodium vivax experimental human infection model for evaluating efficacy of interventions. J. Clin. Investig. 2020, 130, 2920–2927. [Google Scholar] [CrossRef]
- González, J.M.; Hurtado, S.; Arévalo-Herrera, M.; Herrera, S. Variants of the Plasmodium vivax circumsporozoite protein (VK210 and VK247) in Colombian isolates. Mem. Do Inst. Oswaldo Cruz 2001, 96, 709–712. [Google Scholar] [CrossRef]
- Langhorne, J.; Buffet, P.; Galinski, M.; Good, M.; Harty, J.; Leroy, D.; Mota, M.M.; Pasini, E.; Renia, L.; Riley, E.; et al. The relevance of non-human primate and rodent malaria models for humans. Malar. J. 2011, 10, 23. [Google Scholar] [CrossRef] [PubMed]
- Schäfer, C.; Dambrauskas, N.; Reynolds, L.M.; Trakhimets, O.; Raappana, A.; Flannery, E.L.; Roobsoong, W.; Sattabongkot, J.; Mikolajczak, S.A.; Kappe, S.H.; et al. Partial protection against P. vivax infection diminishes hypnozoite burden and blood-stage relapses. Cell Host Microbe 2021, 29, 752–756.e4. [Google Scholar] [CrossRef]
- Voorberg-van der Wel, A.; Kocken, C.H.M.; Zeeman, A.M. Modeling Relapsing Malaria: Emerging Technologies to Study Parasite-Host Interactions in the Liver. Front. Cell. Infect. Microbiol. 2020, 10, 606033. [Google Scholar] [CrossRef]
- Stanisic, D.I.; McCarthy, J.S.; Good, M.F. Controlled Human Malaria Infection: Applications, Advances, and Challenges. Infect. Immun. 2018, 86, e00479-17. [Google Scholar] [CrossRef]
- Payne, R.O.; Griffin, P.M.; McCarthy, J.S.; Draper, S.J. Plasmodium vivax Controlled Human Malaria Infection—Progress and Prospects. Trends Parasitol. 2017, 33, 141. [Google Scholar] [CrossRef] [PubMed]
- Galen, S.C.; Borner, J.; Martinsen, E.S.; Schaer, J.; Austin, C.C.; West, C.J.; Perkins, S.L. The polyphyly of Plasmodium: Comprehensive phylogenetic analyses of the malaria parasites (order Haemosporida) reveal widespread taxonomic conflict. R. Soc. Open Sci. 2018, 5, 171780. [Google Scholar] [CrossRef]
- Galinski, M.R. Systems biology of malaria explored with nonhuman primates. Malar. J. 2022, 21, 177. [Google Scholar] [CrossRef]
- Muh, F.; Erwina, A.; Fitriana, F.; Syahada, J.H.; Cahya, A.D.; Choe, S.; Jun, H.; Garjito, T.A.; Siregar, J.E.; Han, J.-H. Plasmodium cynomolgi: What Should We Know? Microorganisms 2024, 12, 1607. [Google Scholar] [CrossRef]
- Collins, W.E.; Coatney, G.R.; Warren, M.; Contacos, P. The Primate Malarias; original book published 1971; National Institutes of Health: Bethesda, MD, USA, 2003. Available online: https://stacks.cdc.gov/view/cdc/6538/cdc_6538_DS1.pdf (accessed on 26 February 2023).
- Krotoski, W.A.; Krotoski, D.M.; Garnham, P.C.C.; Bray, R.S.; Killick-Kendrick, R.; Draper, C.C.; Targett, A.G.; Guy, M.W. Relapses in primate malaria: Discovery of two populations of exoerythrocytic stages. Preliminary note. BMJ 1980, 280, 153. [Google Scholar] [CrossRef] [PubMed]
- Bykersma, A. The New Zoonotic Malaria: Plasmodium cynomolgi. Trop. Med. Infect. Dis. 2021, 6, 46. [Google Scholar] [CrossRef]
- Zhong, H.; Cao, C.; Li, P.; Zhang, Y.H.; Shi, Y.L.; Ma, Q.J. Induction of protective immune responses in rhesus monkey by immunization with recombinant plasmids of polyvalent epitopes of Plasmodium falciparum using cholera toxin B as adjuvant. Acta Genet. Sin. 2000, 27, 966–971. [Google Scholar] [PubMed]
- Li, P.; Zhong, H.; Shi, C.H.; Cao, C.; Shi, Y.L.; Li, J.Z.; Ma, Q.J. Induction of protective immunity in rhesus monkey by inoculation with recombinant fusion protein of cholera toxin B subunit-multivalent epitopes of Plasmodium falciparum. Chin. J. Biotechnol. 2004, 20, 516–519. [Google Scholar]
- Cao, C.; Li, P.; Shi, C.H.; Zhong, H.; Li, J.Z.; Shi, Y.L.; Ma, Q.J. Induction of protective immune response in mice and rhesus monkeys by immunization with fusion protein of cholera toxin B subunit and multiples of Plasmodium falciparum. Chin. J. Biotechnol. 2000, 16, 333–336. [Google Scholar]
- Bhardwaj, D.; Kushwaha, A.; Puri, S.K.; Herrera, A.; Singh, N.; Chauhan, V.S. DNA prime-protein boost immunization in monkeys: Efficacy of a novel construct containing functional domains of Plasmodium cynomolgi CS and TRAP. FEMS Immunol. Med Microbiol. 2003, 39, 241–250. [Google Scholar] [CrossRef]
- Bhardwaj, D.; Hora, B.; Singh, N.; Puri, S.K.; Lalitha, P.; Rupa, P.; Chauhan, V.S. Immunogenicity and protective efficacy of three DNA vaccines encoding pre-erythrocytic- and erythrocytic-stage antigens of Plasmodium cynomolgi in rhesus monkeys. FEMS Immunol. Med Microbiol. 2002, 34, 33–43. [Google Scholar] [CrossRef]
- Kaushal, D.C.; Kaushal, N.A.; Narula, A.; Kumar, N.; Puri, S.K.; Dutta, S.; Lanar, E.D. Biochemical and immunological characterization of E. coli expressed 42 kDa fragment of Plasmodium vivax and P. cynomolgi bastianelli merozoite surface protein-1. Indian J. Biochem. Biophys. 2007, 44, 429–436. [Google Scholar]
- Dutta, S.; Kaushal, D.C.; Ware, L.A.; Puri, S.K.; Kaushal, N.A.; Narula, A.; Upadhyaya, D.S.; Lanar, D.E. Merozoite surface protein 1 of Plasmodium vivax induces a protective response against Plasmodium cynomolgi challenge in rhesus monkeys. Infect. Immun. 2005, 73, 5936–5944. [Google Scholar] [CrossRef]
- Kocken, C.H.M.; Dubbeld, M.A.; Van Der Wel, A.; Pronk, J.T.; Waters, A.P.; Langermans, J.A.M.; Thomas, A.W. High-level expression of Plasmodium vivax apical membrane antigen 1 (AMA-1) in Pichia pastoris: Strong immunogenicity in Macaca mulatta immunized with P. vivax AMA-1 and adjuvant SBAS2. Infect. Immun. 1999, 67, 43–49. [Google Scholar] [CrossRef]
- Pasini, E.M.; van der Wel, A.V.; Heijmans, N.; Klop, O.; Zeeman, A.-M.; Oostermeijer, H.; Nieuwenhuis, I.; Garcia, R.R.; van der Werff, N.O.; Hofman, S.O.; et al. Sterile protection against relapsing malaria with a single-shot vaccine. npj Vaccines 2022, 7, 126. [Google Scholar] [CrossRef] [PubMed]
- Yongvanitchit, K.; Kum-Arb, U.; Limsalakpetch, A.; Im-Erbsin, R.; Ubalee, R.; Spring, M.D.; Vesely, B.A.; Waters, N.; Pichyangkul, S. Superior protection in a relapsing Plasmodium cynomolgi rhesus macaque model by a chemoprophylaxis with sporozoite immunization regimen with atovaquone-proguanil followed by primaquine. Malar. J. 2024, 23, 106. [Google Scholar] [CrossRef]
- Verra, F.; Hughes, A.L. Biased Amino Acid Composition in Repeat Regions of Plasmodium Antigens. Mol. Biol. Evol. 1999, 16, 627–633. [Google Scholar] [CrossRef]
- Chua, A.C.Y.; Ong, J.J.Y.; Malleret, B.; Suwanarusk, R.; Kosaisavee, V.; Zeeman, A.-M.; Cooper, C.A.; Tan, K.S.W.; Zhang, R.; Tan, B.H.; et al. Robust continuous in vitro culture of the Plasmodium cynomolgi erythrocytic stages. Nat. Commun. 2019, 10, 3635. [Google Scholar] [CrossRef]
- Ward, K.E.; Christensen, P.; Racklyeft, A.; Dhingra, S.K.; Chua, A.C.Y.; Remmert, C.; Suwanarusk, R.; Matheson, J.; Blackman, M.J.; Kaneko, O.; et al. Integrative Genetic Manipulation of Plasmodium cynomolgi Reveals Multidrug Resistance-1 Y976F Associated with Increased in Vitro Susceptibility to Mefloquine. J. Infect. Dis. 2023, 227, 1121–1126. [Google Scholar] [CrossRef] [PubMed]
- Mohring, F.; Hart, M.N.; Patel, A.; Baker, D.A.; Moon, R.W. CRISPR-Cas9 Genome Editing of Plasmodium knowlesi. Bio. Protoc. 2020, 10, e3522. [Google Scholar] [CrossRef]
- Zhang, C.; Xiao, B.; Jiang, Y.; Zhao, Y.; Li, Z.; Gao, H.; Ling, Y.; Wei, J.; Li, S.; Lu, M.; et al. Efficient editing of malaria parasite genome using the CRISPR/Cas9 system. mBio. 2014, 5, mbio.01414-14. [Google Scholar] [CrossRef] [PubMed]
- Jennison, C.; Armstrong, J.M.; Dankwa, D.A.; Hertoghs, N.; Kumar, S.; Abatiyow, B.A.; Naung, M.; Minkah, N.K.; Swearingen, K.E.; Moritz, R.; et al. Plasmodium GPI-anchored micronemal antigen is essential for parasite transmission through the mosquito host. Mol. Microbiol. 2024, 121, 394–412. [Google Scholar] [CrossRef]
- Pasini, E.M.; Böhme, U.; Rutledge, G.G.; Voorberg-Van Der Wel, A.; Sanders, M.; Berriman, M.; Kocken, C.H.; Otto, T.D. An improved Plasmodium cynomolgi genome assembly reveals an unexpected methyltransferase gene expansion. Wellcome Open Res. 2017, 2, 42. [Google Scholar] [CrossRef]
- Tachibana, S.I.; Sullivan, S.A.; Kawai, S.; Nakamura, S.; Kim, H.R.; Goto, N.; Arisue, N.; Palacpac, N.M.Q.; Honma, H.; Yagi, M.; et al. Plasmodium cynomolgi genome sequences provide insight into Plasmodium vivax and the monkey malaria clade. Nat. Genet. 2012, 44, 1051–1055. [Google Scholar] [CrossRef]
- Miyazaki, Y.; Marin-Mogollon, C.; Imai, T.; Mendes, A.M.; van der Laak, R.; Sturm, A.; Geurten, F.J.A.; Miyazaki, S.; Chevalley-Maurel, S.; Ramesar, J.; et al. Generation of a Genetically Modified Chimeric Plasmodium falciparum Parasite Expressing Plasmodium vivax Circumsporozoite Protein for Malaria Vaccine Development. Front. Cell. Infect. Microbiol. 2020, 10, 591046. [Google Scholar] [CrossRef] [PubMed]
- Labun, K.; Montague, T.G.; Krause, M.; Torres Cleuren, Y.N.; Tjeldnes, H.; Valen, E. CHOPCHOP v3: Expanding the CRISPR web toolbox beyond genome editing. Nucleic Acids Res. 2019, 47, W171–W174. [Google Scholar] [CrossRef]
- Mohring, F.; Hart, M.N.; Rawlinson, T.A.; Henrici, R.; Charleston, A.J.; Benavente, E.D.; Patel, A.; Hall, J.; Almond, N.; Campino, S.; et al. Rapid and iterative genome editing in the malaria parasite Plasmodium knowlesi provides new tools for P. vivax research. eLife 2019, 8, e45829. [Google Scholar] [CrossRef]
- Habtewold, T.; Sharma, A.A.; Wyer, C.A.S.; Masters, E.K.G.; Windbichler, N.; Christophides, G.K. Plasmodium oocysts respond with dormancy to crowding and nutritional stress. Sci. Rep. 2021, 11, 3090. [Google Scholar] [CrossRef]
- Stanisic, D.I.; Liu, X.Q.; De, S.L.; Batzloff, M.R.; Forbes, T.; Davis, C.B.; Sekuloski, S.; Chavchich, M.; Chung, W.; Trenholme, K.; et al. Development of cultured Plasmodium falciparum blood-stage malaria cell banks for early phase in vivo clinical trial assessment of anti-malaria drugs and vaccines. Malar. J. 2015, 14, 143. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, R.; Wirtz, R.A.; Lanar, D.E.; Sattabongkot, J.; Hall, T.; Waters, A.P.; Prasittisuk, C. Circumsporozoite Protein Heterogeneity in the Human Malaria Parasite Plasmodium vivax. Science 1989, 245, 973–976. [Google Scholar] [CrossRef] [PubMed]
- Kain, K.C.; Brown, A.E.; Lanar, D.E.; Ballou, W.P.; Webster, H.K. Response of Plasmodium vivax variants to chloroquine as determined by microscopy and quantitative polymerase chain reaction. Am. J. Trop. Med. Hyg. 1993, 49, 478–484. [Google Scholar] [CrossRef] [PubMed]
- Voorberg-van der Wel, A.M.; Zeeman, A.M.; Nieuwenhuis, I.G.; van der Werff, N.M.; Klooster, E.J.; Klop, O.; Vermaat, L.C.; Gupta, D.K.; Dembele, L.; Diagana, T.T.; et al. A dual fluorescent Plasmodium cynomolgi reporter line reveals in vitro malaria hypnozoite reactivation. Commun. Biol. 2020, 3, 7. [Google Scholar] [CrossRef]
- Voorberg-van der Wel, A.; Zeeman, A.M.; van Amsterdam, S.M.; Voorberg-Van Berg, A.; Klooster, E.J.; Iwanaga, S.; Janse, C.J.; Van Gemert, G.-J.; Sauerwein, R.; Beenhakker, N.; et al. Transgenic fluorescent Plasmodium cynomolgi liver stages enable live imaging and purification of Malaria hypnozoite-forms. PLoS ONE 2013, 8, e54888. [Google Scholar] [CrossRef]
- Watson, Q.D.; Carias, L.L.; Malachin, A.; Redinger, K.R.; Bosch, J.; Bardelli, M.; Baldor, L.; Feufack-Donfack, L.B.; Popovici, J.; Moon, R.W.; et al. Human monoclonal antibodies inhibit invasion of transgenic Plasmodium knowlesi expressing Plasmodium vivax Duffy binding protein. Malar. J. 2023, 22, 369. [Google Scholar] [CrossRef]
- Mertens, J.E.; Rigby, C.A.; Bardelli, M.; Quinkert, D.; Hou, M.M.; Diouf, A.; Silk, S.E.; Chitnis, C.E.; Minassian, A.M.; Moon, R.W.; et al. Evaluation of the precision of the Plasmodium knowlesi growth inhibition assay for Plasmodium vivax Duffy-binding protein-based malaria vaccine development. Vaccine 2024, 42, 3621–3629. [Google Scholar] [CrossRef] [PubMed]
- Kocken, C.H.M.; Ozwara, H.; Van der Wel, A.; Beetsma, A.L.; Mwenda, J.M.; Thomas, A.W. Plasmodium knowlesi provides a rapid in vitro and in vivo transfection system that enables double-crossover gene knockout studies. Infect. Immun. 2002, 70, 655–660. [Google Scholar] [CrossRef]
- Othman, A.S.; Marin-Mogollon, C.; Salman, A.M.; Franke-Fayard, B.M.; Janse, C.J.; Khan, S.M. The use of transgenic parasites in malaria vaccine research. Expert Rev. Vaccines 2017, 16, 685–697. [Google Scholar] [CrossRef] [PubMed]
- Flores-Garcia, Y.; Wang, L.T.; Park, M.; Asady, B.; Idris, A.H.; Kisalu, N.K.; Muñoz, C.; Pereira, L.S.; Francica, J.R.; Seder, R.A.; et al. The P. falciparum CSP repeat region contains three distinct epitopes required for protection by antibodies in vivo. PLoS Pathog. 2021, 17, e1010042. [Google Scholar] [CrossRef]
- Marin-Mogollon, C.; Van Pul, F.J.A.; Miyazaki, S.; Imai, T.; Ramesar, J.; Salman, A.M.; Winkel, B.M.F.; Othman, A.S.; Kroeze, H.; Chevalley-Maurel, S.; et al. Chimeric Plasmodium falciparum parasites expressing Plasmodium vivax circumsporozoite protein fail to produce salivary gland sporozoites. Malar. J. 2018, 17, 288. [Google Scholar] [CrossRef]
- Bassat, Q.; Velarde, M.; Mueller, I.; Lin, J.; Leslie, T.; Wongsrichanalai, C.; Baird, J.K. Key Knowledge Gaps for Plasmodium vivax Control and Elimination. Am. J. Trop. Med. Hyg. 2016, 95 (Suppl. 6), 62. [Google Scholar] [CrossRef]
- Schäfer, C.; Roobsoong, W.; Kangwanrangsan, N.; Bardelli, M.; Rawlinson, T.A.; Dambrauskas, N.; Trakhimets, O.; Parthiban, C.; Goswami, D.; Reynolds, L.M.; et al. A Humanized Mouse Model for Plasmodium vivax to Test Interventions that Block Liver Stage to Blood Stage Transition and Blood Stage Infection. iScience 2020, 23, 101381. [Google Scholar] [CrossRef] [PubMed]
- Salman, A.M.; Montoya-DIáz, E.; West, H.; Lall, A.; Atcheson, E.; Lopez-Camacho, C.; Ramesar, J.; Bauza, K.; Collins, K.A.; Brod, F.; et al. Rational development of a protective P. vivax vaccine evaluated with transgenic rodent parasite challenge models. Sci. Rep. 2017, 7, srep46482. [Google Scholar] [CrossRef]
- White, M.T.; Karl, S.; Battle, K.E.; Hay, S.I.; Mueller, I.; Ghani, A.C. Modelling the contribution of the hypnozoite reservoir to Plasmodium vivax transmission. eLife 2014, 3, e04692. [Google Scholar] [CrossRef]
- White, M.; Amino, R.; Mueller, I. Theoretical Implications of a Pre-Erythrocytic Plasmodium vivax Vaccine for Preventing Relapses. Trends Parasitol. 2017, 33, 260–263. [Google Scholar] [CrossRef]
- Kim, Y.C.; Dema, B.; Rodriguez-Garcia, R.; López-Camacho, C.; Leoratti, F.M.S.; Lall, A.; Remarque, E.J.; Kocken, C.H.M.; Reyes-Sandoval, A. Evaluation of chimpanzee adenovirus and MVA expressing TRAP and CSP from plasmodium cynomolgi to prevent malaria relapse in Nonhuman Primates. Vaccines 2020, 8, 363. [Google Scholar] [CrossRef] [PubMed]
- Winnicki, A.C.; Dietrich, M.H.; Yeoh, L.M.; Carias, L.L.; Roobsoong, W.; Drago, C.L.; Malachin, A.N.; Redinger, K.R.; Feufack-Donfack, L.B.; Baldor, L.; et al. Potent AMA1-specific human monoclonal antibody against Plasmodium vivax Pre-erythrocytic and Blood Stages. Nat. Commun. 2024, 15, 10556. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aleshnick, M.; Hegde, S.; Jennison, C.; Mikolajczak, S.A.; Vaughan, A.M.; Haumpy, D.; Martinson, T.; Straimer, J.; Wilder, B.K. Generation of a Transgenic Plasmodium cynomolgi Parasite Expressing Plasmodium vivax Circumsporozoite Protein for Testing P. vivax CSP-Based Malaria Vaccines in Non-Human Primates. Vaccines 2025, 13, 536. https://doi.org/10.3390/vaccines13050536
Aleshnick M, Hegde S, Jennison C, Mikolajczak SA, Vaughan AM, Haumpy D, Martinson T, Straimer J, Wilder BK. Generation of a Transgenic Plasmodium cynomolgi Parasite Expressing Plasmodium vivax Circumsporozoite Protein for Testing P. vivax CSP-Based Malaria Vaccines in Non-Human Primates. Vaccines. 2025; 13(5):536. https://doi.org/10.3390/vaccines13050536
Chicago/Turabian StyleAleshnick, Maya, Shreeya Hegde, Charlie Jennison, Sebastian A. Mikolajczak, Ashley M. Vaughan, Derek Haumpy, Thomas Martinson, Judith Straimer, and Brandon K. Wilder. 2025. "Generation of a Transgenic Plasmodium cynomolgi Parasite Expressing Plasmodium vivax Circumsporozoite Protein for Testing P. vivax CSP-Based Malaria Vaccines in Non-Human Primates" Vaccines 13, no. 5: 536. https://doi.org/10.3390/vaccines13050536
APA StyleAleshnick, M., Hegde, S., Jennison, C., Mikolajczak, S. A., Vaughan, A. M., Haumpy, D., Martinson, T., Straimer, J., & Wilder, B. K. (2025). Generation of a Transgenic Plasmodium cynomolgi Parasite Expressing Plasmodium vivax Circumsporozoite Protein for Testing P. vivax CSP-Based Malaria Vaccines in Non-Human Primates. Vaccines, 13(5), 536. https://doi.org/10.3390/vaccines13050536





