The Attitude Toward Seasonal Influenza Vaccine Among Workers of Community Healthcare Centers in Zhejiang Province, China: Barriers and Facilitators
Abstract
1. Introduction
2. Methods
2.1. Study Areas
2.2. Study Design
2.3. Sampling
2.4. Questionnaire
2.5. Statistical Analysis
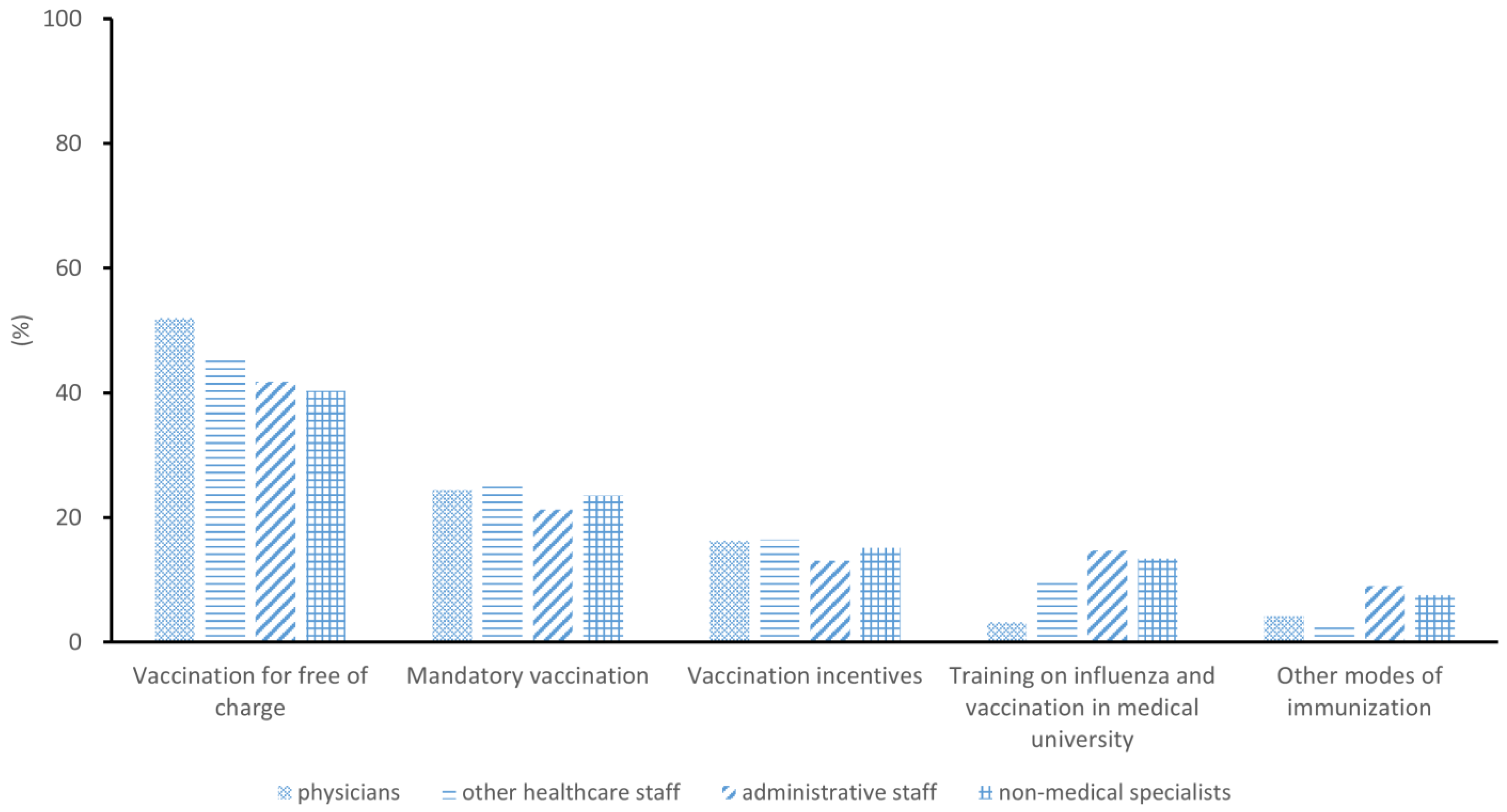
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Iuliano, A.D.; Roguski, K.M.; Chang, H.H.; Muscatello, D.J.; Palekar, R.; Tempia, S.; Cohen, C.; Gran, J.M.; Schanzer, D.; Cowling, B.J.; et al. Estimates of global seasonal influenza-associated respiratory mortality: A modelling study. Lancet 2018, 391, 1285–1300. [Google Scholar] [CrossRef]
- Molinari, N.A.; Ortega-Sanchez, I.R.; Messonnier, M.L.; Thompson, W.W.; Wortley, P.M.; Weintraub, E.; Bridges, C.B. The annual impact of seasonal influenza in the US: Measuring disease burden and costs. Vaccine 2007, 25, 5086–5096. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Yang, L.; Liu, C.; Jin, H.; Lin, L. Estimated Incidence of Seasonal Influenza in China from 2010 to 2020 Using a Multiplier Model. JAMA Netw. Open 2022, 5, e227423. [Google Scholar] [CrossRef]
- Li, J.; Zhang, Y.; Zhang, X.; Liu, L. Influenza and Universal Vaccine Research in China. Viruses 2022, 15, 116. [Google Scholar] [CrossRef]
- Gong, H.; Shen, X.; Yan, H.; Lu, W.Y.; Zhong, G.J.; Dong, K.G.; Yang, J.; Yu, H.J. Estimating the disease burden of seasonal influenza in China, 2006–2019. Zhonghua Yi Xue Za Zhi 2021, 101, 560–567. [Google Scholar] [CrossRef] [PubMed]
- Members of the Western Pacific Region Global Influenza Surveillance Response System; Dwyer, D.; Barr, I.; Hurt, A.; Kelso, A.; Reading, P.; Sullivan, S.; Buchy, P.; Yu, H.; Zheng, J.; et al. Seasonal influenza vaccine policies, recommendations and use in the World Health Organization’s Western Pacific Region. West. Pac. Surveill. Response J. 2013, 4, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Kuster, S.P.; Shah, P.S.; Coleman, B.L.; Lam, P.-P.; Tong, A.; Wormsbecker, A.; McGeer, A. Incidence of influenza in healthy adults and healthcare workers: A systematic review and meta-analysis. PLoS ONE 2011, 6, e26239. [Google Scholar] [CrossRef]
- Voirin, N.; Barret, B.; Metzger, M.H.; Vanhems, P. Hospital-acquired influenza: A synthesis using the Outbreak Reports and Intervention Studies of Nosocomial Infection (ORION) statement. J. Hosp. Infect. 2009, 71, 1–14. [Google Scholar] [CrossRef]
- Demicheli, V.; Jefferson, T.; Ferroni, E.; Rivetti, A.; Di Pietrantonj, C. Vaccines for preventing influenza in healthy adults. Cochrane Database Syst. Rev. 2018, 2, CD001269. [Google Scholar] [CrossRef]
- Thomas, R.E.; Jefferson, T.; Lasserson, T.J.; Earnshaw, S. Influenza vaccination for healthcare workers who care for people aged 60 or older living in long-term care institutions. Cochrane Database Syst. Rev. 2025, 2, CD005187. [Google Scholar] [CrossRef]
- De Serres, G.; Skowronski, D.M.; Ward, B.J.; Gardam, M.; Lemieux, C.; Yassi, A.; Patrick, D.M.; Krajden, M.; Loeb, M.; Collignon, P.; et al. Influenza Vaccination of Healthcare Workers: Critical Analysis of the Evidence for Patient Benefit Underpinning Policies of Enforcement. PLoS ONE 2017, 12, e0163586. [Google Scholar] [CrossRef] [PubMed]
- Vanhems, P.; Baghdadi, Y.; Roche, S.; Bénet, T.; Regis, C.; Lina, B.; Robert, O.; Voirin, N.; Ecochard, R.; Amour, S. Influenza vaccine effectiveness among healthcare workers in comparison to hospitalized patients: A 2004-2009 case-test, negative-control, prospective study. Hum. Vaccines Immunother. 2016, 12, 485–490. [Google Scholar] [CrossRef]
- Kassianos, G. Willingness of European healthcare workers to undergo vaccination against seasonal influenza: Current situation and suggestions for improvement. Drugs Context 2015, 4, 212268. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Schmid, P.; Rauber, D.; Betsch, C.; Lidolt, G.; Denker, M.L. Barriers of Influenza Vaccination Intention and Behavior—A Systematic Review of Influenza Vaccine Hesitancy, 2005–2016. PLoS ONE 2017, 12, e0170550. [Google Scholar] [CrossRef]
- Atamna, Z.; Chazan, B.; Nitzan, O.; Colodner, R.; Kfir, H.; Strauss, M.; Schwartz, N.; Markel, A. Seasonal Influenza Vaccination Effectiveness and Compliance among Hospital Health Care Workers. Isr. Med. Assoc. J. 2016, 18, 5–9. [Google Scholar] [PubMed]
- Tuckerman, J.L.; Collins, J.E.; Marshall, H.S. Factors affecting uptake of recommended immunizations among health care workers in South Australia. Hum. Vaccines Immunother. 2015, 11, 704–712. [Google Scholar] [CrossRef]
- Hollmeyer, H.; Hayden, F.; Mounts, A.; Buchholz, U. Review: Interventions to increase influenza vaccination among healthcare workers in hospitals. Influ. Other Respir. Viruses 2013, 7, 604–621. [Google Scholar] [CrossRef] [PubMed]
- Bellia, C.; Setbon, M.; Zylberman, P.; Flahault, A. Healthcare worker compliance with seasonal and pandemic influenza vaccination. Influ. Other Respir. Viruses 2013, 7 (Suppl. S2), 97–104. [Google Scholar] [CrossRef]
- FitzSimons, D.; Hendrickx, G.; Lernout, T.; Badur, S.; Vorsters, A.; Van Damme, P. Incentives and barriers regarding immunization against influenza and hepatitis of health care workers. Vaccine 2014, 32, 4849–4854. [Google Scholar] [CrossRef]
- Ip, D.K.M.; Lau, L.L.H.; Chan, K.H.; Fang, V.J.; Leung, G.M.; Peiris, M.J.S.; Cowling, B.J. The Dynamic Relationship Between Clinical Symptomatology and Viral Shedding in Naturally Acquired Seasonal and Pandemic Influenza Virus Infections. Clin. Infect. Dis. 2016, 62, 431–437. [Google Scholar] [CrossRef]
- Barbadoro, P.; Marigliano, A.; Di Tondo, E.; Chiatti, C.; Di Stanislao, F.; D’errico, M.M.; Prospero, E. Determinants of influenza vaccination uptake among Italian healthcare workers. Hum. Vaccines Immunother. 2013, 9, 911–916. [Google Scholar] [CrossRef] [PubMed]
- Lai, X.; Li, M.; Hou, Z.; Guo, J.; Zhang, H.; Wang, J.; Fang, H. Factors associated with caregivers’ hesitancy to vaccinate children against influenza: A cross-sectional survey in China. Vaccine 2022, 40, 3975–3983. [Google Scholar] [CrossRef]
- Fan, J.; Xu, S.; Liu, Y.; Ma, X.; Cao, J.; Fan, C.; Bao, S. Influenza vaccination rates among healthcare workers: A systematic review and meta-analysis investigating influencing factors. Front. Public Health 2023, 11, 1295464. [Google Scholar] [CrossRef] [PubMed]
- Bouadma, L.; Barbier, F.; Biard, L.; Esposito-Farèse, M.; Le Corre, B.; Macrez, A.; Salomon, L.; Bonnal, C.; Zanker, C.; Najem, C.; et al. Personal decision-making criteria related to seasonal and pandemic A(H1N1) influenza-vaccination acceptance among French healthcare workers. PLoS ONE 2012, 7, e38646. [Google Scholar] [CrossRef][Green Version]
- Jia, W.; Zhang, X.; Sun, R.; Li, P.; Wang, D.; Song, C. Effective measures to improve influenza vaccination coverage among healthcare workers during and after COVID-19. Hum Vaccines Immunother. 2023, 19, 2289243. [Google Scholar] [CrossRef] [PubMed]
- Yi, H.; Yang, Y.; Zhang, L.; Zhang, M.; Wang, Q.; Zhang, T.; Zhang, Y.; Qin, Y.; Peng, Z.; Leng, Z.; et al. Improved influenza vaccination coverage among health-care workers: Evidence from a web-based survey in China, 2019/2020 season. Hum Vaccines Immunother. 2021, 17, 2185–2189. [Google Scholar] [CrossRef]
- Ma, L.; Han, X.; Ma, Y.; Yang, Y.; Xu, Y.; Liu, D.; Yang, W.; Feng, L. Decreased influenza vaccination coverage among Chinese healthcare workers during the COVID-19 pandemic. Infect. Dis. Poverty 2022, 11, 105. [Google Scholar] [CrossRef]
- Bonaccorsi, G.; Lorini, C.; Santomauro, F.; Guarducci, S.; Pellegrino, E.; Puggelli, F.; Balli, M.; Bonanni, P. Predictive factors associated with the acceptance of pandemic and seasonal influenza vaccination in health care workers and students in Tuscany, Central Italy. Hum. Vaccines Immunother. 2013, 9, 2603–2612. [Google Scholar] [CrossRef] [PubMed]
- Abramson, Z.H.; Levi, O. Influenza vaccination among primary healthcare workers. Vaccine 2008, 26, 2482–2489. [Google Scholar] [CrossRef]
- Costantino, C.; Mazzucco, W.; Azzolini, E.; Baldini, C.; Bergomi, M.; Biafiore, A.D.; Bianco, M.; Borsari, L.; Cacciari, P.; Cadeddu, C.; et al. Influenza vaccination coverage among medical residents: An Italian multicenter survey. Hum. Vaccines Immunother. 2014, 10, 1204–1210. [Google Scholar] [CrossRef]
- Karafillakis, E.; Dinca, I.; Apfel, F.; Cecconi, S.; Wűrz, A.; Takacs, J.; Suk, J.; Celentano, L.P.; Kramarz, P.; Larson, H.J. Vaccine hesitancy among healthcare workers in Europe: A qualitative study. Vaccine 2016, 34, 5013–5020. [Google Scholar] [CrossRef] [PubMed]
- Betsch, C.; Renkewitz, F.; Betsch, T.; Ulshöfer, C. The influence of vaccine-critical websites on perceiving vaccination risks. J. Health Psychol. 2010, 15, 446–455. [Google Scholar] [CrossRef] [PubMed]
- Sato, A.P.; Antunes, J.L.; Moura, R.F.; de Andrade, F.B.; Duarte, Y.A.; Lebrão, M.L. Factors associated to vaccination against influenza among elderly in a large Brazilian metropolis. PLoS ONE 2015, 10, e0123840. [Google Scholar] [CrossRef] [PubMed]
- Dini, G.; Toletone, A.; Sticchi, L.; Orsi, A.; Bragazzi, N.L.; Durando, P. Influenza vaccination in healthcare workers: A comprehensive critical appraisal of the literature. Hum. Vaccines Immunother. 2018, 14, 772–789. [Google Scholar] [CrossRef]
- Prematunge, C.; Corace, K.; McCarthy, A.; Nair, R.C.; Roth, V.; Suh, K.N.; Garber, G. Qualitative motivators and barriers to pandemic vs. seasonal influenza vaccination among healthcare workers: A content analysis. Vaccine 2014, 32, 7128–7134. [Google Scholar] [CrossRef]
| Variable | Level | N | % | Vaccination Coverage (%, 95%CI) |
|---|---|---|---|---|
| Sex | Male | 1101 | 49.93 | 1.36 (1.18–1.57) |
| Female | 1104 | 50.07 | 1.36 (1.19–1.54) | |
| Civil status | Single | 538 | 24.40 | 1.11 (1.05–1.33) |
| Married | 1397 | 63.36 | 1.43 (1.26–1.63) | |
| Divorced | 239 | 10.84 | 1.25 (1.15–1.59) | |
| Widowed | 31 | 1.41 | 3.22 (1.80–5.48) | |
| Years of employment | 0–9 yrs | 486 | 22.04 | 1.23 (1.09–1.29) |
| 10–19 yrs | 1423 | 64.54 | 1.40 (1.20–1.59) | |
| ≥ 20 yrs | 296 | 13.42 | 1.35 (1.12–1.54) | |
| Profession | Physicians | 1102 | 49.98 | 1.45 (1.25–1.88) |
| Other healthcare workers | 862 | 39.09 | 1.39 (1.18–1.79) | |
| Administrative staff | 122 | 5.53 | 0.82 (0.45–1.05) | |
| Non-medical specialists | 119 | 5.40 | 0.84 (0.36–1.17) | |
| BMI | <18 | 752 | 34.10 | 1.19 (1.03–1.38) |
| 18–25 | 1106 | 50.16 | 1.35 (1.11–1.50) | |
| 26–30 | 239 | 10.84 | 1.67 (1.37–2.16) | |
| >30 | 108 | 4.90 | 1.85 (1.32–2.63) | |
| Have children | Yes | 1502 | 68.12 | 1.46 (1.17–1.79) |
| No | 703 | 31.88 | 1.13 (1.05–1.26) |
| Attitude | Physicians * | Other Healthcare Workers * | Administrative Staff * | Non-Medical Specialists * | Total * | p # |
|---|---|---|---|---|---|---|
| Acceptance | ||||||
| Consider themselves as a high-risk group | 3.32 (4, 3) | 2.82 (3, 4) | 2.70 (3, 4) | 3.05 (3, 4) | 3.07 (3, 4) | 0.04 |
| To avoid spreading influenza among family | 4.38 (5, 1) | 4.17 (5, 1) | 4.02 (5, 2) | 3.88 (5, 2) | 4.23 (5, 1) | 0.13 |
| To avoid spreading influenza among patients | 4.36 (5, 1) | 3.98 (5, 2) | 3.05 (3, 3) | 3.76 (5, 2) | 3.95 (5, 2) | 0.01 |
| To avoid influenza | 4.40 (5, 1) | 4.38 (5, 1) | 4.27 (5, 1) | 4.28 (5, 1) | 4.36 (5, 1) | 0.85 |
| Influenza vaccination was strongly recommended from own CHC | 2.86 (3, 3) | 2.75 (2, 2) | 2.75 (3, 3) | 2.07 (2, 2) | 2.65 (3, 3) | 0.33 |
| To avoid work absences | 3.91 (4, 2) | 3.47 (4, 3) | 3.72 (4, 2) | 3.09 (3, 2) | 3.88 (4, 2) | 0.08 |
| Scientific validity of the vaccine | 4.18 (5, 1) | 3.58 (4, 2) | 3.33 (3, 2) | 3.86 (5, 2) | 3.82 (4, 2) | 0.01 |
| Refusal | ||||||
| Does not consider influenza vaccine effective | 2.20 (4, 1) | 2.83 (4, 3) | 2.67 (3, 4) | 2.41 (3, 2) | 2.56 (3, 3) | 0.01 |
| Does not consider influenza vaccine safe | 1.97 (1, 3) | 2.57 (2, 3) | 2.67 (4, 3) | 2.32 (2, 3) | 2.68 (3, 3) | 0.01 |
| Influenza does not overweight the risk of vaccination | 2.28 (2, 2) | 2.92 (3, 2) | 2.85 (3, 1) | 2.57 (3, 3) | 2.88 (4, 3) | 0.01 |
| Not a high-risk group of influenza and possible complications | 3.38 (4, 2) | 3.69 (4, 2) | 4.11 (5, 2) | 4.04 (4, 2) | 3.72 (4, 1) | 0.01 |
| Not a high-risk group for spreading influenza in the general population | 2.61 (3, 3) | 3.07 (3, 1) | 3.53 (4, 2) | 3.38 (4, 2) | 3.16 (3, 2) | 0.01 |
| Not a high-risk group for spreading influenza in patients | 2.57 (3, 2) | 3.08 (3, 2) | 3.65 (4, 2) | 3.63 (5, 2) | 3.16 (3, 3) | 0.01 |
| Influenza vaccination was not recommended by own CHC | 1.76 (1, 2) | 1.97 (1, 2) | 2.28 (2, 2) | 2.03 (2, 2) | 1.95 (1, 2) | 0.01 |
| Personal conviction to take less medications | 2.70 (3, 3) | 3.72 (4, 2) | 3.77 (4, 2) | 3.47 (4, 2) | 3.55 (4, 3) | 0.01 |
| I’m against vaccination generally | 1.35 (1, 0) | 2.08 (1, 2) | 2.37 (2, 2) | 1.88 (1, 2) | 2.13 (1, 2) | 0.01 |
| I forgot it | 1.72 (2, 0) | 2.31 (3, 2) | 2.51 (3, 1) | 2.05 (2, 0) | 2.21 (3, 2) | 0.01 |
| I did not have time | 1.29 (2, 1) | 2.02 (1, 2) | 1.8 (2, 0) | 1.47 (2, 0) | 1.52 (2, 1) | 0.01 |
| Because of adverse reaction of previous influenza vaccinations | 1.13 (1, 0) | 1.88 (3, 1) | 2.17 (3, 2) | 1.59 (2, 1) | 1.90 (3, 1) | 0.01 |
| Variable | Level | N | Received Vaccination | p for χ2-Test |
|---|---|---|---|---|
| Socio-demographics | ||||
| Sex | Male | 1101 | 1.36 | 0.38 |
| Female | 1104 | 1.36 | ||
| Civil status | Single | 538 | 1.11 | 0.03 |
| Married | 1397 | 1.43 | ||
| Divorced | 239 | 1.25 | ||
| Widowed | 31 | 3.22 | ||
| Years of employment | 0–9 yrs | 486 | 1.23 | 0.27 |
| 10–19 yrs | 1423 | 1.4 | ||
| ≥20 yrs | 296 | 1.35 | ||
| Profession | Physicians | 1102 | 1.45 | 0.01 |
| Other healthcare workers | 862 | 1.39 | ||
| Administrative staff | 122 | 0.82 | ||
| Non-medical specialists | 119 | 0.84 | ||
| BMI | <18 | 752 | 1.19 | 0.02 |
| 18–25 | 1106 | 1.35 | ||
| 26–30 | 239 | 1.67 | ||
| >30 | 108 | 1.85 | ||
| Having children | Yes | 1502 | 1.46 | 0.01 |
| No | 703 | 1.13 | ||
| Regular exercise | Yes | 1222 | 1.59 | 0.01 |
| No | 983 | 1.15 | ||
| Stop smoking and limit alcohol consumption | Yes | 305 | 2.26 | 0.01 |
| No | 1900 | 1.29 | ||
| Vaccination for own child | Yes | 2102 | 1.38 | 0.01 |
| No | 103 | 1.02 | ||
| Sources of information | ||||
| Decree issued by the Ministry of Health | Yes | 133 | 1.73 | 0.01 |
| No | 2072 | 1.28 | ||
| Mass media | Yes | 384 | 1.78 | 0.01 |
| No | 1821 | 1.21 | ||
| Scientific publications | Yes | 201 | 1.79 | 0.01 |
| No | 2004 | 1.25 | ||
| Institutional websites | Yes | 152 | 1.86 | 0.01 |
| No | 2053 | 1.19 | ||
| Workmates | Yes | 299 | 1.37 | 0.48 |
| No | 1906 | 1.36 | ||
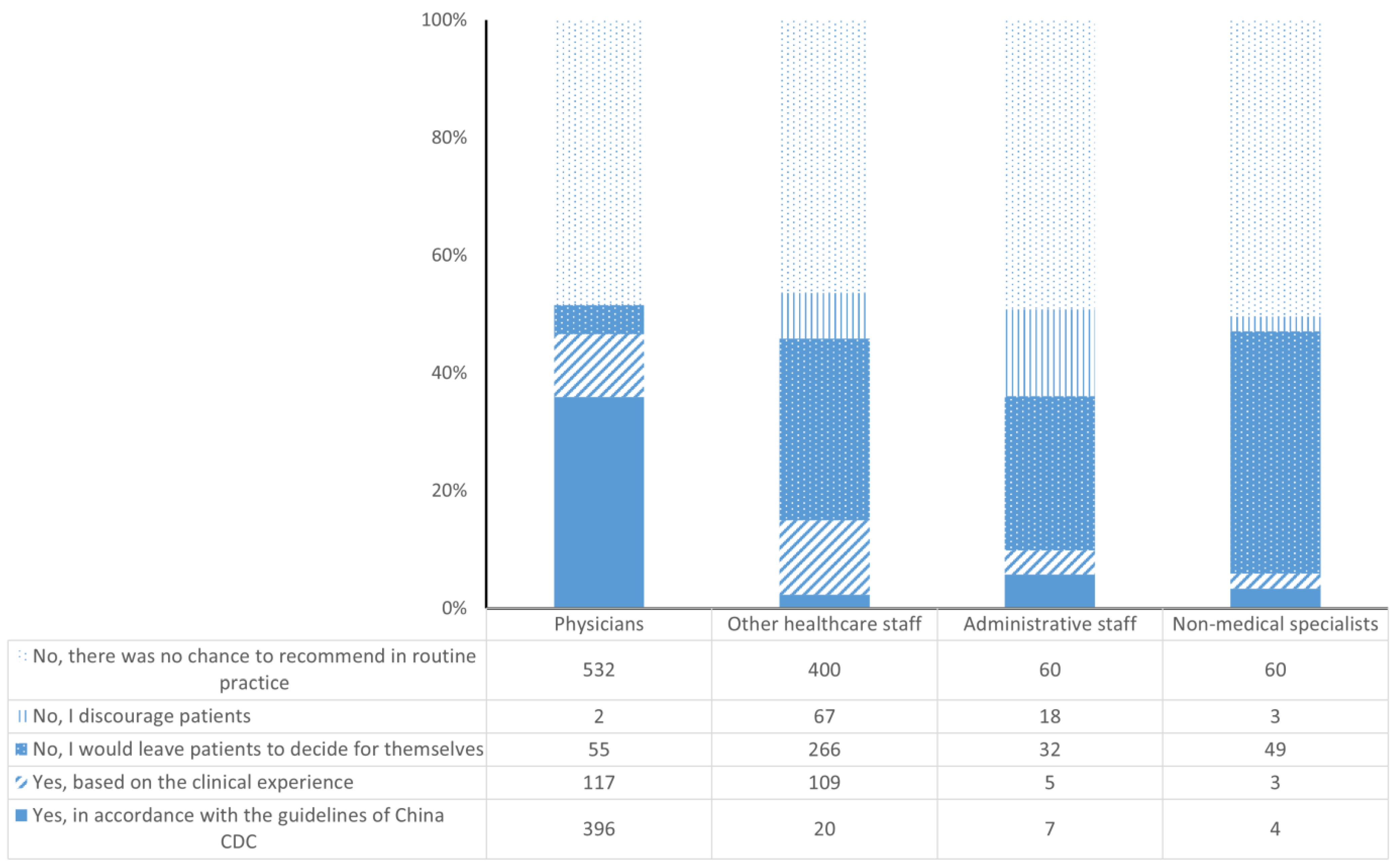
| Recommendation on influenza vaccination | Yes, in accordance with the guidelines of China CDC | 427 | 1.79 | 0.01 |
| Yes, based on the clinical experience | 234 | 1.41 | ||
| No, I would leave patients to decide for themselves | 402 | 1.37 | ||
| No, I discourage patients | 90 | 1.31 | ||
| No, there was no chance to recommend in routine practice | 1052 | 1.26 | ||
| Quality of information received | Nil | 113 | 1.02 | 0.02 |
| Inadequate | 187 | 1.05 | ||
| Adequate | 858 | 1.32 | ||
| Good | 917 | 1.37 | ||
| Excellent | 130 | 1.53 |
| Variable | Level | AOR | 95% CI | p |
|---|---|---|---|---|
| Socio-demographics | ||||
| Civil status | Single | Ref | - | - |
| Married | 1.12 | 0.53–1.35 | 0.24 | |
| Divorced | 0.82 | 0.45–1.16 | 0.31 | |
| Widowed | 1.32 | 0.43–3.93 | 0.18 | |
| Profession | Physicians | 2.68 | 1.33–5.47 | 0.01 |
| Other healthcare workers | 1.08 | 0.78–2.61 | 0.22 | |
| Administrative staff | Ref | - | - | |
| Non-medical specialists | 1.01 | 0.29–1.65 | 0.41 | |
| BMI | <18 | 1.02 | 0.61–4.22 | 0.37 |
| 18–25 | Ref | - | - | |
| 26–30 | 1.19 | 0.88–1.81 | 0.29 | |
| >30 | 1.77 | 1.19–3.02 | 0.01 | |
| Having children | Yes | 1.29 | 0.91–1.88 | 0.11 |
| No | Ref | - | - | |
| Regular exercise | Yes | 0.71 | 0.52–0.91 | 0.01 |
| No | Ref | - | - | |
| Stop smoking and limit alcohol consumption | Yes | 1.06 | 0.89–1.25 | 0.26 |
| No | Ref | - | - | |
| Vaccination for own child | Yes | 1.03 | 0.74–2.06 | 0.47 |
| No | Ref | - | - | |
| Sources of information | ||||
| Ministry of Health | Yes | 1.59 | 1.07–2.65 | 0.02 |
| No | Ref | - | - | |
| Mass media | Yes | 0.37 | 0.21–0.58 | 0.01 |
| No | Ref | - | - | |
| Scientific publications | Yes | 1.56 | 1.03–2.29 | 0.02 |
| No | Ref | - | - | |
| Institutional websites | Yes | 1.55 | 1.05–2.33 | 0.01 |
| No | Ref | - | - | |
| Recommendation on influenza vaccination | Yes, in accordance with the guidelines of China CDC | 4.02 | 2.71–6.50 | 0.01 |
| Yes, based on the clinical experience | 5.58 | 4.16–8.17 | 0.01 | |
| No, I would leave patients to decide for themselves | 1.37 | 0.95–2.27 | 0.38 | |
| No, I discourage patients | 0.42 | 0.11–0.75 | 0.01 | |
| No, there was no chance to recommend in routine practice | Ref | - | - | |
| Quality of information received | Nil | Ref | - | - |
| Inadequate | 0.88 | 0.31–1.82 | 0.52 | |
| Adequate | 1.02 | 0.42–2.22 | 0.38 | |
| Good | 1.04 | 0.47–1.89 | 0.51 | |
| Excellent | 1.22 | 0.32–2.17 | 0.62 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shen, J.; Han, S.; Zhang, C.; Lv, H.; Hu, Y. The Attitude Toward Seasonal Influenza Vaccine Among Workers of Community Healthcare Centers in Zhejiang Province, China: Barriers and Facilitators. Vaccines 2025, 13, 507. https://doi.org/10.3390/vaccines13050507
Shen J, Han S, Zhang C, Lv H, Hu Y. The Attitude Toward Seasonal Influenza Vaccine Among Workers of Community Healthcare Centers in Zhejiang Province, China: Barriers and Facilitators. Vaccines. 2025; 13(5):507. https://doi.org/10.3390/vaccines13050507
Chicago/Turabian StyleShen, Jianyong, Shangyan Han, Chao Zhang, Huakun Lv, and Yu Hu. 2025. "The Attitude Toward Seasonal Influenza Vaccine Among Workers of Community Healthcare Centers in Zhejiang Province, China: Barriers and Facilitators" Vaccines 13, no. 5: 507. https://doi.org/10.3390/vaccines13050507
APA StyleShen, J., Han, S., Zhang, C., Lv, H., & Hu, Y. (2025). The Attitude Toward Seasonal Influenza Vaccine Among Workers of Community Healthcare Centers in Zhejiang Province, China: Barriers and Facilitators. Vaccines, 13(5), 507. https://doi.org/10.3390/vaccines13050507




