Trends Towards Enhanced Rates and Sex Parity in HPV Vaccination in Croatia (2016–2023)
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection and Categorization
2.2. Data Analysis
3. Results
4. Discussion
4.1. Lessons Learned
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| HPV | Human papillomavirus |
| WHO | World Health Organization |
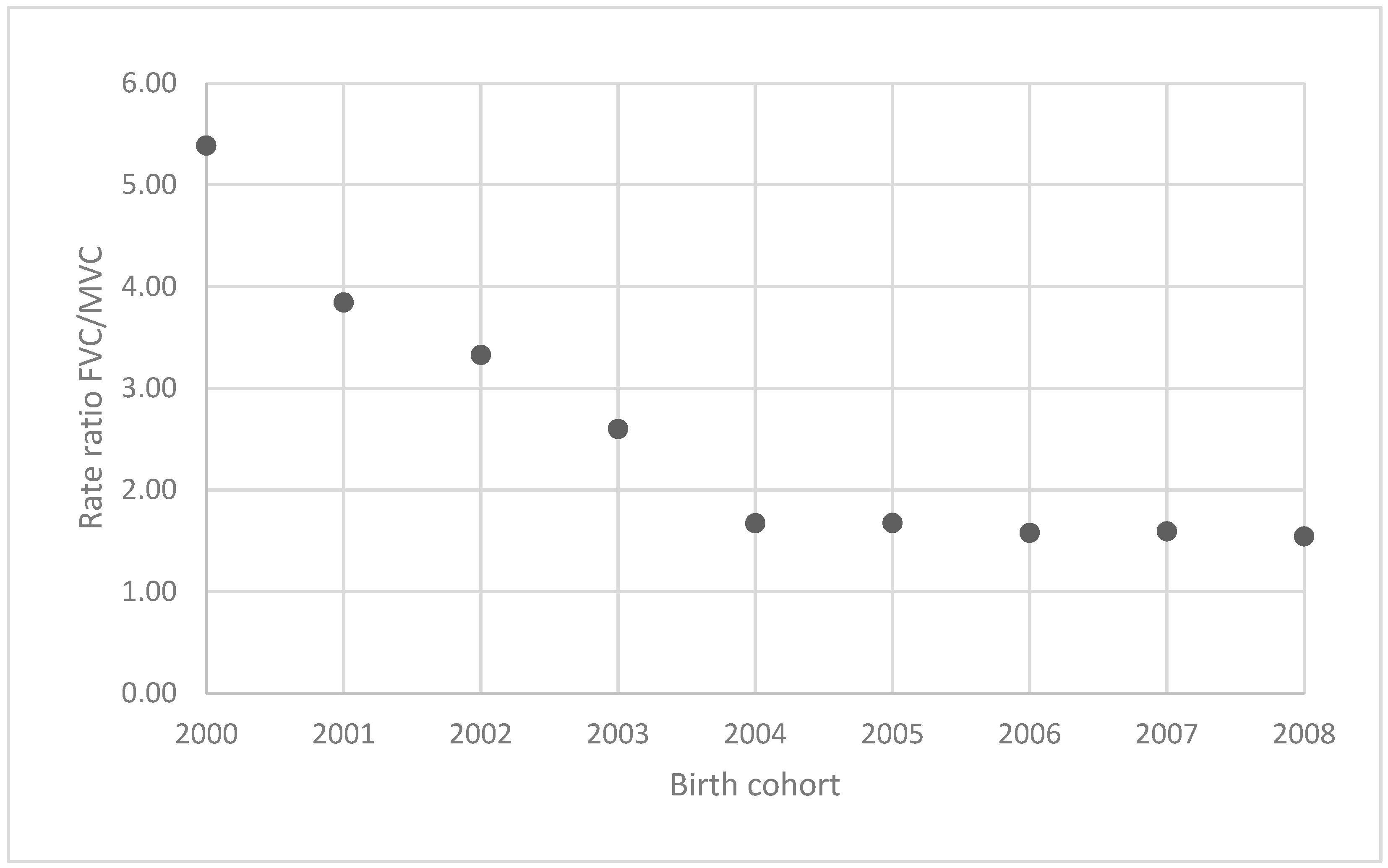
| FVC | Female vaccination coverage |
| MVC | Male vaccination coverage |
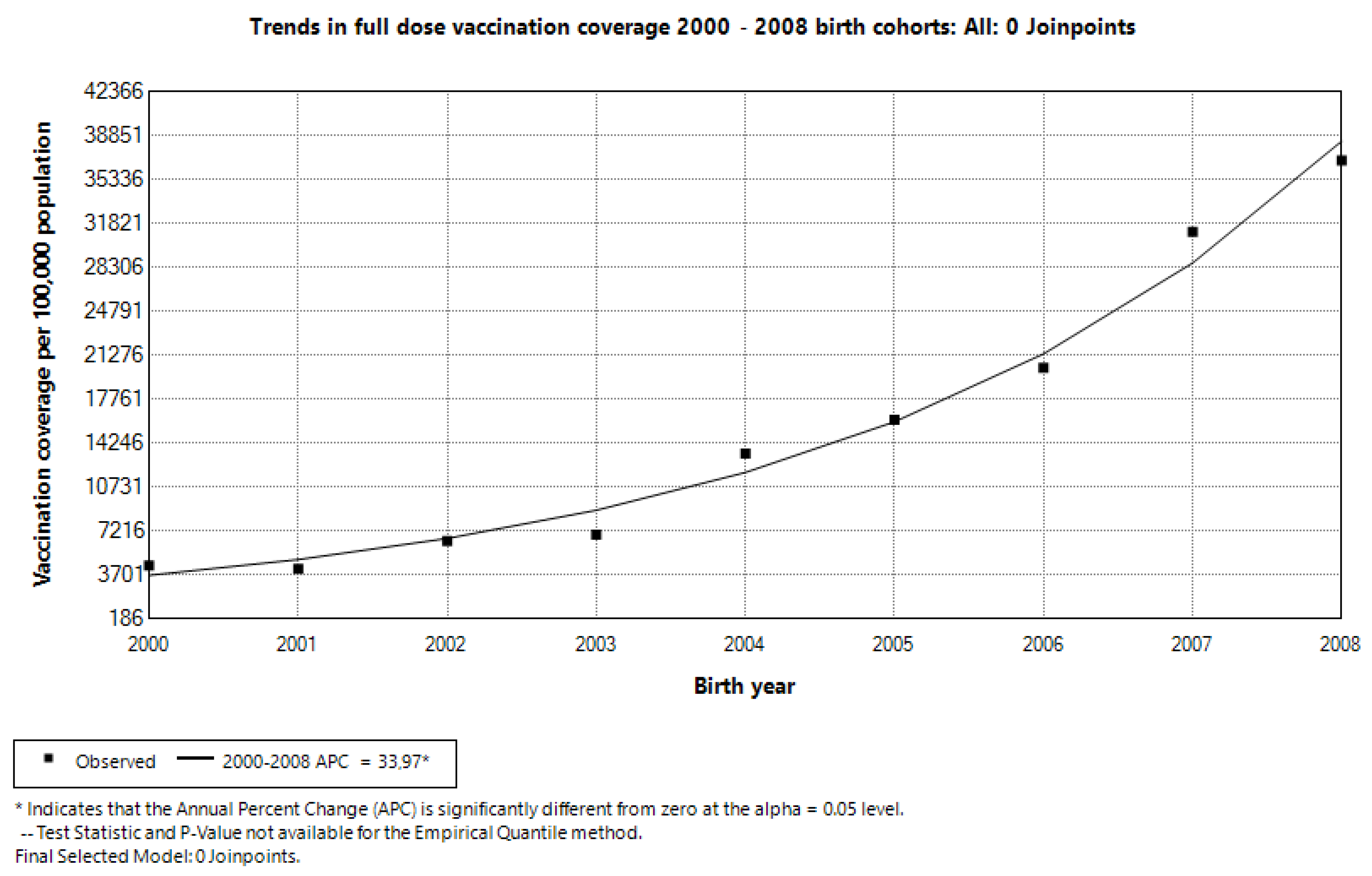
| APC | Annual Percent Change |
References
- Seong, J.; Ryou, S.M. Overview of the Efficacy of Human Papillomavirus Virus Vaccines. J. Bacteriol. Virol. 2020, 50, 158–167. [Google Scholar] [CrossRef]
- Lacey, C.J.N.; Lowndes, C.M.; Shah, K.V. Chapter 4: Burden and management of non-cancerous HPV-related conditions: HPV-6/11 disease. Vaccine 2006, 24, S35–S41. Available online: https://www.sciencedirect.com/science/article/pii/S0264410X06007274 (accessed on 29 January 2024). [CrossRef] [PubMed]
- de Martel, C.; Plummer, M.; Vignat, J.; Franceschi, S. Worldwide Burden of Cancer Attributable to HPV by Site, Country and HPV Type. Int. J. Cancer 2017, 141, 664–670. [Google Scholar] [PubMed]
- Factsheet about Human Papillomavirus. Available online: https://www.ecdc.europa.eu/en/human-papillomavirus/factsheet (accessed on 30 January 2024).
- Bruni, L.; Albero, G.; Serrano, B.; Mena, M.; Collado, J.J.; Gómez, D.; Muñoz, J.; Bosch, F.X.; de Sanjosé, S. Human Papillomavirus and Related Diseases Report WORLD 2023 March. Available online: https://hpvcentre.net/statistics/reports/XWX.pdf (accessed on 30 January 2024).
- Nacionalni dan Borbe Protiv Raka Vrata Maternice—Epidemiološki Podaci|Hrvatski Zavod za Javno Zdravstvo. Available online: https://www.hzjz.hr/sluzba-epidemiologija-prevencija-nezaraznih-bolesti/nacionalni-dan-borbe-protiv-raka-vrata-maternice-epidemioloski-podaci/ (accessed on 5 February 2024).
- Bilten Incidencija raka u Hrvatskoj 2020. Godine|Hrvatski Zavod za Javno Zdravstvo. Available online: https://www.hzjz.hr/aktualnosti/bilten-incidencija-raka-u-hrvatskoj-2020-godine/ (accessed on 1 February 2024).
- Bruni, L.; Albero, G.; Serrano, B.; Mena, M.; Collado, J.J.; Gómez, D.; Muñoz, J.; Bosch, F.X.; de Sanjosé, S. Human Papillomavirus and Related Diseases Report CROATIA. Available online: https://hpvcentre.net/datastatistics.php (accessed on 3 July 2024).
- World Health Organization. Global Strategy to Accelerate the Elimination of Cervical Cancer as a Public Health Problem; World Health Organization: Geneva, Switzerland, 2020; pp. 1–56. Available online: https://www.who.int/publications/i/item/9789240014107 (accessed on 1 February 2024).
- European Commission. Europe’s Beating Cancer Plan: Communication from the Commission to the European Parliament and the Council; European Commission: Brussels, Belgium, 2022. [Google Scholar]
- Nemeth Blažić, T.; Božičević, I.; Kosanović Ličina, M.L.; Štulhofer, A.; Nola, I.A. Self-reported HPV vaccination status and HPV vaccine hesitancy in a nationally representative sample of emerging adults in Croatia. Front. Public Health. 2023, 11, 1182582. [Google Scholar]
- Provedbeni Program Cijepljenja za 2024. Godinu|Hrvatski Zavod za Javno Zdravstvo. Available online: https://www.hzjz.hr/sluzba-epidemiologija-zarazne-bolesti/provedbeni-program-cijepljenja-za-2024-godinu/ (accessed on 5 April 2024).
- Cijepljenje Protiv Humanog Papiloma Virusa (HPV)|Hrvatski Zavod za Javno Zdravstvo. Available online: https://www.hzjz.hr/aktualnosti/cijepljenje-protiv-humanog-papiloma-virusa-hpv/ (accessed on 5 February 2024).
- Hrvatski Zdravstveno-Statistički Ljetopis za 2020.—Tablični Podaci|Hrvatski Zavod za Javno Zdravstvo. Available online: https://www.hzjz.hr/periodicne-publikacije/hrvatski-zdravstveno-statisticki-ljetopis-za-2020-tablicni-podaci/ (accessed on 5 April 2024).
- HRVATSKI ZDRAVSTVENO-STATISTIČKI LJETOPIS ZA 2021. GODINU. Available online: https://www.hzjz.hr/cat/hrvatski-zdravstveno-statisticki-ljetopis/ (accessed on 19 March 2024).
- HRVATSKI ZDRAVSTVENO-STATISTIČKI LJETOPIS ZA 2022. GODINU. Available online: https://www.hzjz.hr/cat/hrvatski-zdravstveno-statisticki-ljetopis/ (accessed on 5 April 2024).
- Hrvatsko društvo za školsku i sveučiličnu medicinu. Preporuke Hrvatskog društva za školsku i sveučilišnu medicinu HLZ o organizaciji cijepljenja protiv HPV infekcije. 19 January 2023, Volume 2023. Available online: https://zzjzpgz.hr/wp-content/uploads/2023/02/Preporuke-HDSSM-za-HPV-2023.pdf (accessed on 19 March 2024).
- HPV Vaccine Administration|CDC. Available online: https://www.cdc.gov/vaccines/vpd/hpv/hcp/administration.html (accessed on 30 January 2024).
- Meeting of the Strategic Advisory Group of Experts on Immunization, April 2022: Conclusions and Recommendations. Available online: https://www.who.int/publications/i/item/who-wer9724-261-276 (accessed on 30 January 2024).
- Joinpoint Regression Program. Available online: https://surveillance.cancer.gov/joinpoint/ (accessed on 22 March 2025).
- Kim, H.J.; Fay, M.P.; Feuer, E.J.; Midthune, D.N. Permutation tests for joinpoint regression with applications to cancer rates. Stat. Med. 2000, 19, 335–351. [Google Scholar] [CrossRef]
- OpenEpi-Dose Response: Chi Square for Trend. Available online: https://www.openepi.com/DoseResponse/DoseResponse.htm (accessed on 8 February 2024).
- Immunization, Vaccines and Biologicals. Available online: https://www.who.int/teams/immunization-vaccines-and-biologicals/diseases/human-papillomavirus-vaccines-(HPV)/hpv-clearing-house/hpv-dashboard (accessed on 6 February 2024).
- Human Papillomavirus (HPV) Vaccination Coverage. Available online: https://immunizationdata.who.int/global/wiise-detail-page/human-papillomavirus-(hpv)-vaccination-coverage (accessed on 23 March 2025).
- Bruni, L.; Saura-Lázaro, A.; Montoliu, A.; Brotons, M.; Alemany, L.; Diallo, M.S.; Afsar, O.Z.; LaMontagne, D.S.; Mosina, L.; Contreras, M.; et al. HPV vaccination introduction worldwide and WHO and UNICEF estimates of national HPV immunization coverage 2010–2019. Prev. Med. 2021, 144, 106399. [Google Scholar] [CrossRef] [PubMed]
- Budi mRAK! Izbjegni Rak! Sve o HPV-u i Prevenciji. Available online: https://budi-mrak.com/ (accessed on 19 March 2024).
- Spolno Zdravlje. Available online: https://spolnozdravlje.hr/ (accessed on 19 March 2024).
- Kaul, S.; Do, T.Q.N.; Hsu, E.; Schmeler, K.M.; Montealegre, J.R.; Rodriguez, A.M. School-Based Human Papillomavirus Vaccination Program for Increasing Vaccine Uptake in an Underserved Area in Texas. Papillomavirus Res. 2019, 8, 100189. [Google Scholar] [CrossRef] [PubMed]
- Borowska, M.; Koczkodaj, P.; Mańczuk, M. HPV vaccination coverage in the European Region. Nowotw. J. Oncol. 2024, 74, 191–196. [Google Scholar] [CrossRef]
- Nguyen-Huu, N.H.; Thilly, N.; Derrough, T.; Sdona, E.; Claudot, F.; Pulcini, C.; Agriner, N.; HPV Policy Working Group. Human papillomavirus vaccination coverage, policies, and practical implementation across Europe. Vaccine 2020, 38, 1315–1331. Available online: https://www.sciencedirect.com/science/article/pii/S0264410X19316354. [CrossRef] [PubMed]
- Rejza, M.; Rylewicz, K.; Lewandowska, M.; Gross-Tyrkin, K.; Łopiński, G.; Barwińska, J.; Majcherek, E.; Szymuś, K.; Klein, P.; Plagens-Rotman, K.; et al. HPV Vaccination among Polish Adolescents—Results from POLKA 18 Study. Healthcare 2022, 10, 2385. [Google Scholar] [CrossRef] [PubMed]
- Karafillakis, E.; Simas, C.; Jarrett, C.; Verger, P.; Peretti-Watel, P.; Dib, F.; Ali, K.A.; Celentano, L.P.; Larson, H. HPV vaccination in a context of public mistrust and uncertainty: A systematic literature review of determinants of HPV vaccine hesitancy in Europe. Hum. Vaccin Immunother. 2019, 15, 1615–1627. [Google Scholar] [CrossRef] [PubMed]
- Alarcão, V.; Zdravkova, B. Attitudes and Practices towards HPV Vaccination and Its Social Processes in Europe: An Equity-Focused Scoping Review. Societies 2022, 12, 131. [Google Scholar] [CrossRef]
- Posavec, M. HPV vaccination in the Republic of Croatia. Paediatr. Croatiaca 2018, 62, 48–51. [Google Scholar]
- Belavic, A.; Pavic Simetin, I. Educational intervention for increasing knowledge of human papillomavirus and vaccination amongst parents of first year high school students in Croatia. J. Public Health 2022, 44, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Khozin, S.; Blumenthal, G.M.; Pazdur, R. Real-world Data for Clinical Evidence Generation in Oncology. J. Natl. Cancer Inst. 2017, 109, djx187. Available online: https://academic.oup.com/jnci/article-pdf/109/11/djx187/23699015/djx187.pdf (accessed on 22 March 2025). [CrossRef] [PubMed]
- Liu, F.; Panagiotakos, D. Real-world data: A brief review of the methods, applications, challenges and opportunities. BMC Med. Res. Methodol. 2022, 22, 287. [Google Scholar] [CrossRef]
- Derrough, T.; Olsson, K.; Gianfredi, V.; Simondon, F.; Heijbel, H.; Danielsson, N.; Kramarz, P.; Pastore-Celentano, L. Immunisation Information Systems—Useful tools for monitoring vaccination programmes in EU/EEA countries, 2016. Eurosurveillance 2017, 22, 30519. [Google Scholar] [CrossRef] [PubMed]
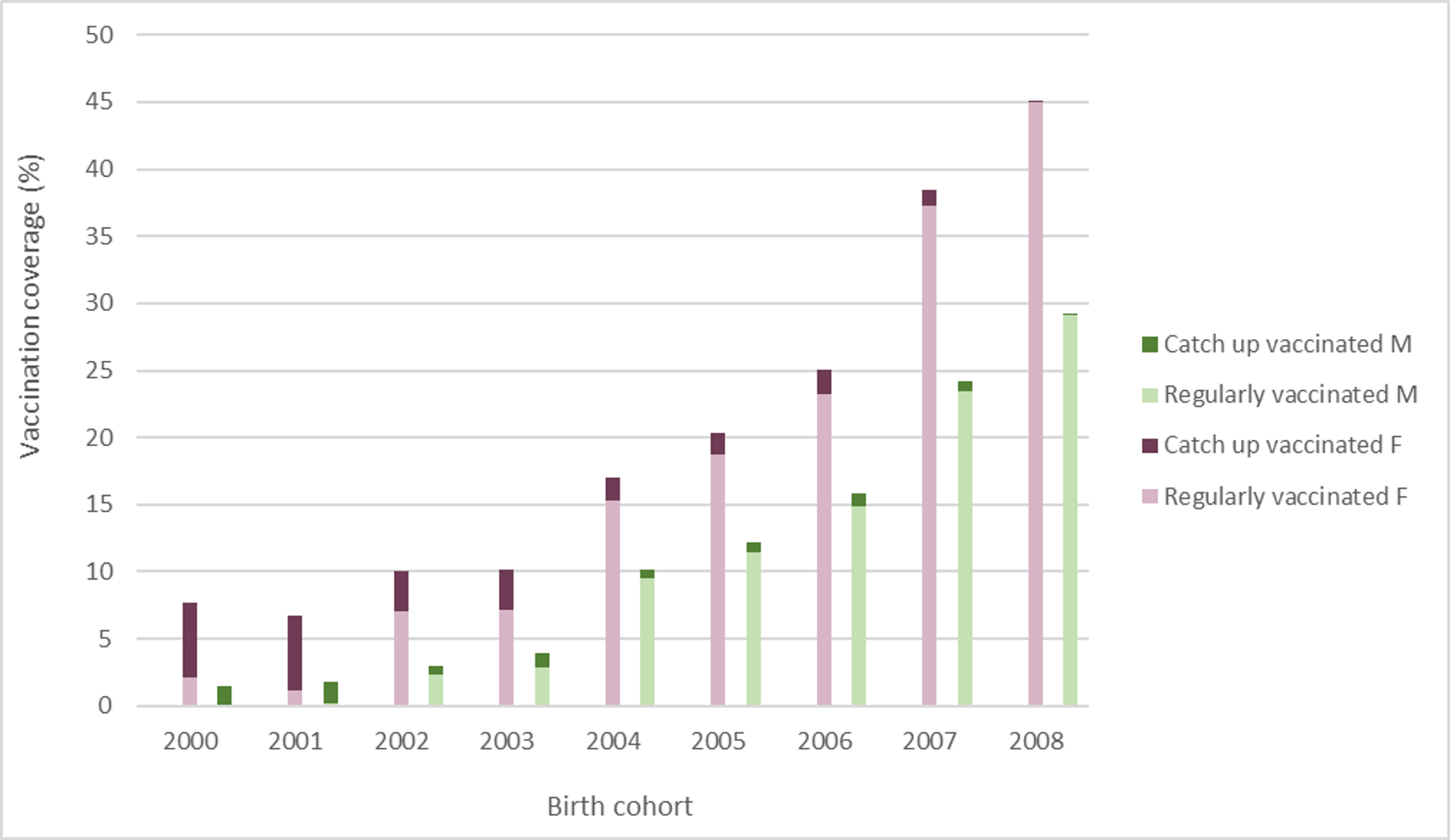
| Categories | Subcategories | Sex | Age of Recipient | Number of Doses |
|---|---|---|---|---|
| Full dose | Regularly vaccinated (organized) | Both F and M | ≤15 | 2 |
| Catch-up vaccinated (opportunistic) | Both F and M | 16–25 | 3 | |
| One dose | Both | Both F and M | <25 | At least 1 |
| Birth | Full Dose | One Dose | ||||
|---|---|---|---|---|---|---|
| Cohort | Total | F | M | Total | F | M |
| 2000 | 4.49 | 7.74 | 1.44 | 6.44 | 10.67 | 2.47 |
| 2001 | 4.20 | 6.77 | 1.76 | 7.94 | 12.20 | 3.90 |
| 2002 | 6.44 | 10.06 | 3.02 | 9.33 | 14.15 | 4.78 |
| 2003 | 6.93 | 10.14 | 3.90 | 10.86 | 15.47 | 6.50 |
| 2004 | 13.43 | 16.96 | 10.15 | 20.20 | 25.11 | 15.65 |
| 2005 | 16.13 | 20.32 | 12.14 | 25.05 | 30.41 | 19.96 |
| 2006 | 20.27 | 25.02 | 15.87 | 34.67 | 41.55 | 28.29 |
| 2007 | 31.15 | 38.49 | 24.18 | 39.84 | 48.81 | 31.31 |
| 2008 | 36.88 | 44.98 | 29.14 | 44.22 | 52.78 | 36.05 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raic, L.; Pavic Simetin, I.; Bradasevic, E.; Jezidzic, A.; Nemeth Blazic, T.; Poljicanin, T. Trends Towards Enhanced Rates and Sex Parity in HPV Vaccination in Croatia (2016–2023). Vaccines 2025, 13, 410. https://doi.org/10.3390/vaccines13040410
Raic L, Pavic Simetin I, Bradasevic E, Jezidzic A, Nemeth Blazic T, Poljicanin T. Trends Towards Enhanced Rates and Sex Parity in HPV Vaccination in Croatia (2016–2023). Vaccines. 2025; 13(4):410. https://doi.org/10.3390/vaccines13040410
Chicago/Turabian StyleRaic, Lucija, Ivana Pavic Simetin, Emanuel Bradasevic, Antea Jezidzic, Tatjana Nemeth Blazic, and Tamara Poljicanin. 2025. "Trends Towards Enhanced Rates and Sex Parity in HPV Vaccination in Croatia (2016–2023)" Vaccines 13, no. 4: 410. https://doi.org/10.3390/vaccines13040410
APA StyleRaic, L., Pavic Simetin, I., Bradasevic, E., Jezidzic, A., Nemeth Blazic, T., & Poljicanin, T. (2025). Trends Towards Enhanced Rates and Sex Parity in HPV Vaccination in Croatia (2016–2023). Vaccines, 13(4), 410. https://doi.org/10.3390/vaccines13040410






