Influenza Vaccination in the Elderly in Three Cities in China: Current Status and Influencing Factors Under Different Funding Policies
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
- (1)
- residents aged 60 and above who had lived locally for ≥6 months.
- (1)
- individuals who did not agree to participate in the survey;
- (2)
- individuals with contraindications to the influenza vaccine; and
- (3)
- individuals who were unable to comprehend a simple, standardized screening question used to assess cognitive eligibility (e.g., “Do you plan to get a flu shot next year?”). Participants providing an irrelevant or incomprehensible response were excluded.
2.2. Sample Size
- (1)
- Full-subsidy region: p0 = 10%, p1 = 57.5%, B = 0.3 → Initial n ≈ 140
- (2)
- Partial reimbursement region: p0 = 5%, p1 = 39%, B = 0.2 → Initial n ≈ 160
- (3)
- Full self-payment region: p0 = 3%, p1 = 27.4%, B = 0.1 → Initial n ≈ 385
2.3. Survey Methods and Content
2.4. Statistical Analysis
3. Results
3.1. Demographic Characteristics
3.2. Vaccination Status and Influenza Vaccination Intention
3.3. Health Belief Model Scores
3.4. Multivariate Logistic Regression Analysis
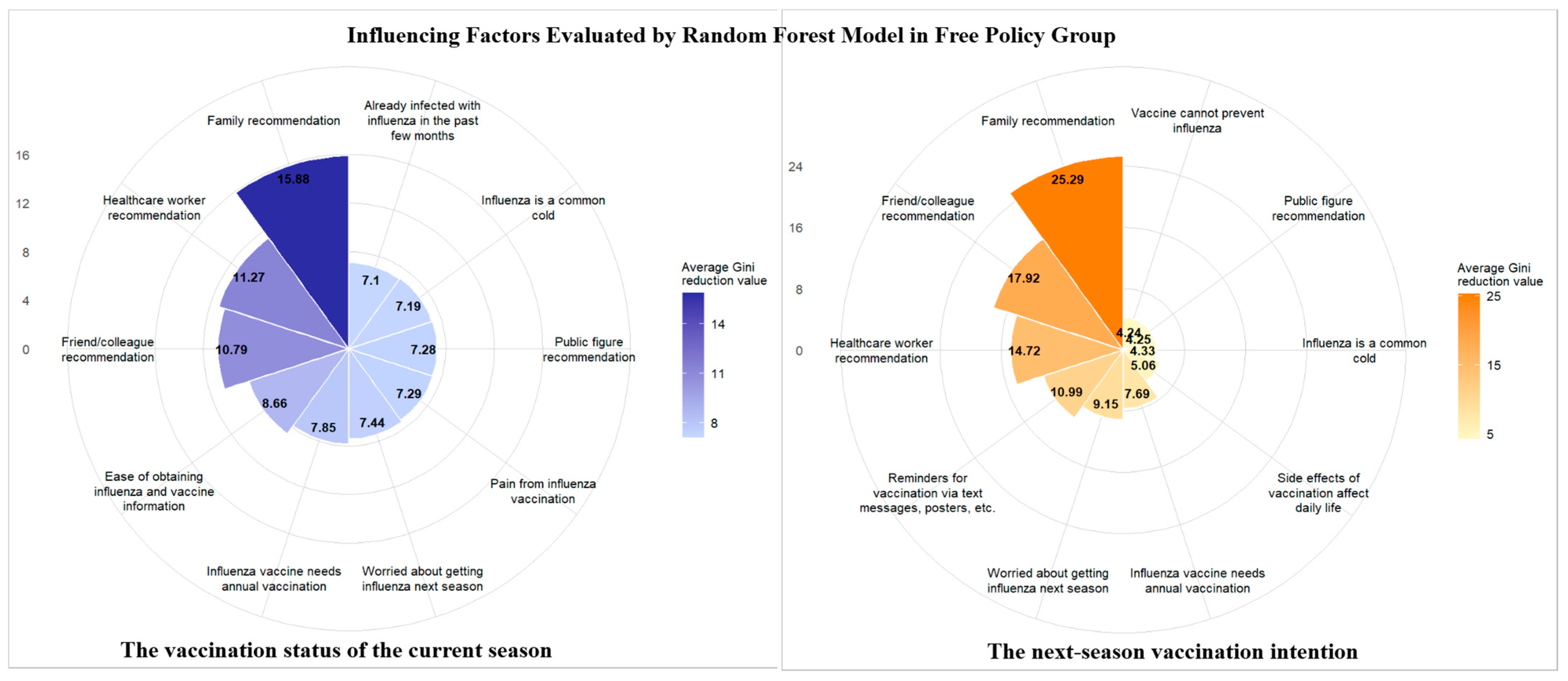
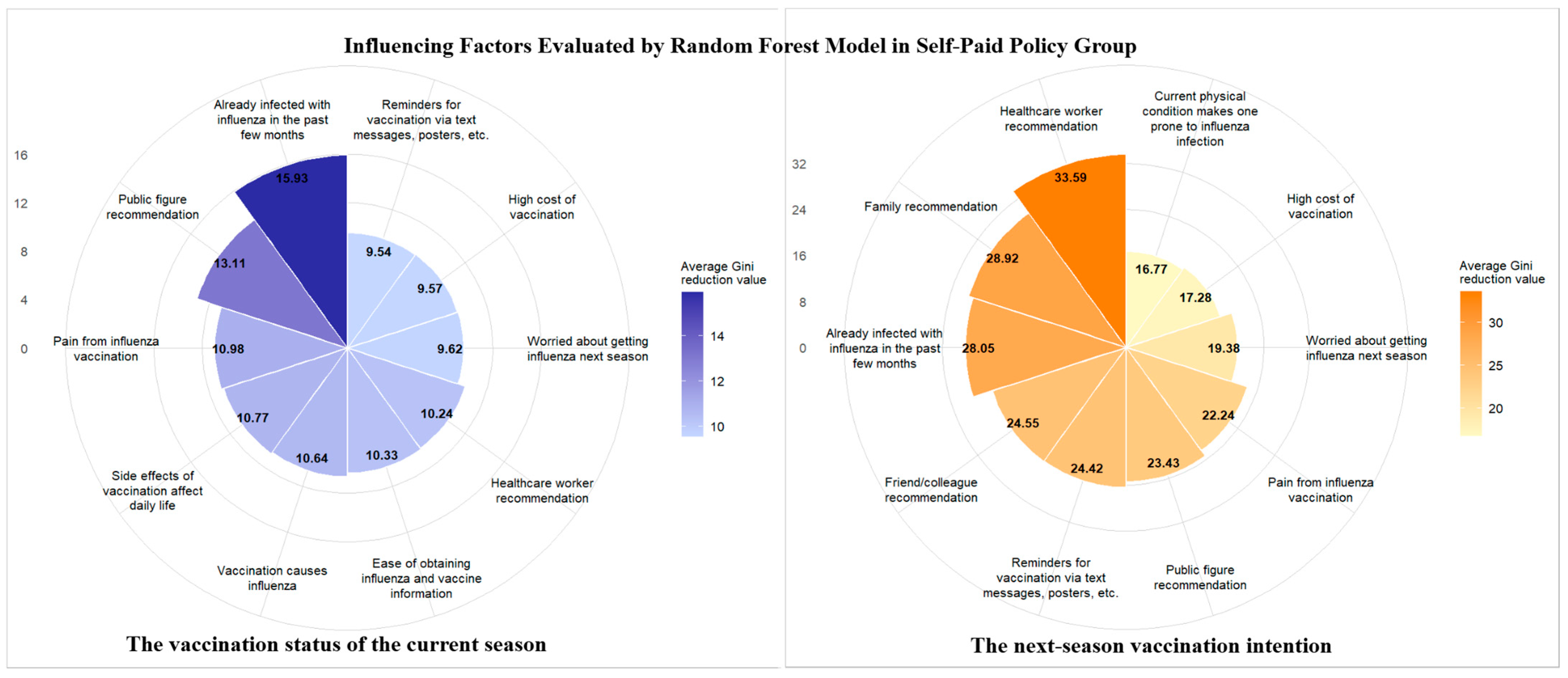
3.5. Random Forest Model Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Correction Statement
References
- Iuliano, A.D.; Roguski, K.M.; Chang, H.H.; Muscatello, D.J.; Palekar, R.; Tempia, S.; Cohen, C.; Gran, J.M.; Schanzer, D.; Cowling, B.J.; et al. Estimates of global seasonal influenza-associated respiratory mortality: A modelling study. Lancet 2018, 391, 1285–1300. [Google Scholar] [CrossRef]
- Somes, M.P.; Turner, R.M.; Dwyer, L.J.; Newall, A.T. Estimating the annual attack rate of seasonal influenza among unvaccinated individuals: A systematic review and meta-analysis. Vaccine 2018, 36, 3199–3207. [Google Scholar] [CrossRef] [PubMed]
- Katz, M.; Palekar, R.S.; Rolfes, M.A.; Arriola, C.S.; Acosta, B.O.; Guidos, P.A.; Vargas, X.B.; Bancej, C.; Ramirez, J.B.; Baumeister, E.; et al. Burden of influenza-associated respiratory hospitalizations in the Americas, 2010–2015. PLoS ONE 2019, 14, e0221479. [Google Scholar] [CrossRef]
- Wu, P.; Presanis, A.M.; Bond, H.S.; Lau, E.H.Y.; Fang, V.J.; Cowling, B.J. A joint analysis of influenza-associated hospitalizations and mortality in Hong Kong, 1998-2013. Sci. Rep. 2017, 7, 929. [Google Scholar] [CrossRef]
- Zhang, Y.; Muscatello, D.J.; Wang, Q.; Yang, P.; Pan, Y.; Huo, D.; Liu, Z.; Zhao, X.; Tang, Y.; Li, C.; et al. Hospitalizations for Influenza-Associated Severe Acute Respiratory Infection, Beijing, China, 2014-2016. Emerg. Infect. Dis. 2018, 24, 2098–2102. [Google Scholar] [CrossRef]
- Li, L.; Liu, Y.; Wu, P.; Peng, Z.; Wang, X.; Chen, T.; Wong, J.Y.T.; Yang, J.; Bond, H.S.; Wang, L.; et al. Influenza-associated excess respiratory mortality in China, 2010–15: A population-based study. Lancet Public Health 2019, 4, e473–e481. [Google Scholar] [CrossRef]
- Smetana, J.; Chlibek, R.; Shaw, J.; Splino, M.; Prymula, R. Influenza vaccination in the elderly. Hum. Vaccin. Immunother. 2018, 14, 540–549. [Google Scholar] [CrossRef]
- Cheng, L.X.; Li, L.; Cao, L.; Song, Y.F.; Zhang, Z.N.; Yin, Z.D. Analysis of vaccination status of three non-immunization program vaccines among people aged ≥60 in China from 2019 to 2023. Chin. J. Prev. Med. 2024, 25, 592–597, (In Chinese with English Abstract). [Google Scholar] [CrossRef]
- Healthy China Action Promotion Committee. Healthy China Action (2019–2030). Updated 15 July 2019. Available online: http://www.gov.cn/xinwen/2019-07/15/content_5409694.htm (accessed on 20 November 2024).
- Feng, Z.J. Strengthen operational researches on influenza polices, and promote influenza vaccination in China. Chin. J. Prev. Med. 2019, 53, 961–963, (In Chinese with English Abstract). [Google Scholar] [CrossRef]
- Xue, J.F.; Han, X.; Qi, Z.W.; Li, J.G.; Su, F.H.; Dai, W.; Zhou, G.Y. Effect of influenza vaccine literacy on influenza vaccine willingness in the elderly. Cap. J. Public Health 2025, 19, 165–168. [Google Scholar]
- Liang, J.; Liu, G.; Zhang, J.J.; Fang, Q.; Huang, Z.L.; Liu, C. Vaccination status and influencing factors of free influenza vaccine among the elderly in Futian District, Shenzhen. J. Trop. Med. 2020, 20, 706–710. [Google Scholar] [CrossRef]
- Xie, Y.Y.; Feng, D.Q.; Chen, S.Y.; Wu, B.; Chen, Y.F.; Fu, C.W. Vaccination behavior, willingness and influencing factors of free influenza vaccine among the elderly in Deqing County, Zhejiang Province. Fudan Univ. J. Med. Sci. 2025, 52, 686–693. [Google Scholar] [CrossRef]
- Yao, X.; Yu, M.K.; Wu, J.; Lv, M.; Xie, Z. Qualitative study on the influence of healthcare workers on influenza vaccination among the elderly in Beijing. Chin. Gen. Pract. 2020, 23, 2203–2206. [Google Scholar] [CrossRef]
- Yang, J.; Atkins, K.E.; Feng, L.; Pang, M.; Zheng, Y.; Liu, X.; Cowling, B.J.; Yu, H. Seasonal influenza vaccination in China: Landscape of diverse regional reimbursement policy, and budget impact analysis. Vaccine 2016, 34, 5724–5735. [Google Scholar] [CrossRef]
- Gao, Y.X.; Zhang, J.X. Determination of sample size for logistic regression analysis. J. Evid. Based Med. 2018, 18, 122–124. [Google Scholar] [CrossRef]
- Kwong, E.W.; Lam, I.O.; Chan, T.M. What factors affect influenza vaccine uptake among community-dwelling older Chinese people in Hong Kong general outpatient clinics? J. Clin. Nurs. 2009, 18, 960–971. [Google Scholar] [CrossRef]
- The People’s Bank of China. Exchange Rate on 25 August 2025 (In Chinese). Available online: http://www.pbc.gov.cn/zhengcehuobisi/125207/125217/125925/5816932/index.html (accessed on 25 August 2025).
- Wang, F.H.; Xie, Z.; Lü, M.; Deng, Y.; Zhang, T.H. Analysis of free influenza vaccination status and urban-rural disparities among elderly residents with Beijing household registration. J. Peking Univ. Health Sci. 2013, 45, 432–436, (In Chinese with English Abstract). [Google Scholar] [CrossRef]
- Fang, R.F.; Ma, Y.; Wu, J.; Lv, M.; Tian, L.J.; Xie, Z. Free Influenza Vaccination Coverage and Its Influencing Factors about Cognition among Elderly Population in Beijing. Chin. Gen. Pract. 2014, 1403–1406, (In Chinese with English Abstract). [Google Scholar] [CrossRef]
- Thomas, R.E.; Lorenzetti, D.L. Interventions to increase influenza vaccination rates of those 60 years and older in the community. Cochrane Database Syst. Rev. 2018, 5, CD005188. [Google Scholar] [CrossRef]
- Jiang, M.; Li, P.; Yao, X.; Hayat, K.; Gong, Y.; Zhu, S.; Peng, J.; Shi, X.; Pu, Z.; Huang, Y.; et al. Preference of influenza vaccination among the elderly population in Shaanxi province, China. Hum. Vaccin. Immunother. 2021, 17, 3119–3125. [Google Scholar] [CrossRef]
- Zhu, X.F.; Huang, T.; Zhu, X.P.; Tang, X.F.; Xu, H.J.; Xu, Z.; Feng, A.; Liu, L.; Luan, R.S. Impact of Community Healthcare Workers’ Knowledge, Attitude and Practice on the Influenza Vaccination among Elderly People. Chin. J. Evid. Based Med. 2013, 13, 543–547. [Google Scholar] [CrossRef]
- Kroneman, M.; van Essen, G.A.; John Paget, W. Influenza vaccination coverage and reasons to refrain among high-risk persons in four European countries. Vaccine 2006, 24, 622–628. [Google Scholar] [CrossRef]
- Suolang, D.J.; Ci, Z.; Ciren, W.L.; Zhang, L.J. Survey on influenza vaccination rate and influencing factors among the elderly in Chengguan District, Lhasa Prefecture, 2017–2018. Int. J. Epidemiol. Infect. Dis. 2019, 46, 340–344. [Google Scholar] [CrossRef]
- Chen, Q.X.; Nie, Y.Z.; Zhang, J.X.; Qiu, X.S.; Zhang, X.; Xue, Y.L.; Wang, X.; Li, Q.B. Investigation on influencing factors of influenza vaccination among the elderly in Foshan City. Mod. Prev. Med. 2010, 37, 2047–2051. [Google Scholar]
- Zhang, X.P.; Xu, E.P.; Liu, Y.; Wang, J.; Liu, S.J.; Du, J.; Che, X.R. Study on Influenza Vaccination and Its Influence Factors among the Old People in the Urban Area of Hangzhou City. Zhejiang J. Prev. Med. 2011, 23, 31–32. [Google Scholar] [CrossRef]
- Wang, Z.; Tsang, T.H.; Yu, F.Y.; Fang, Y.; Chen, S.; Sun, F.; Mo, P.K.H.; Wong, K.-C. Effectiveness, Usability, and Acceptability of ChatGPT With Retrieval-Augmented Generation (SIV-ChatGPT) in Increasing Seasonal Influenza Vaccination Uptake Among Older Adults: Quasi-Experimental Study. J. Med. Internet Res. 2025, 27, e76849. [Google Scholar] [CrossRef] [PubMed]

| Variable | Free Policy Region (n = 426) | Partial Reimbursement Region (n = 633) | Self-Paid Policy Region (n = 1206) | χ2 Value | p Value |
|---|---|---|---|---|---|
| Region | 0.026 | 0.999 | |||
| Urban | 145 (34.04%) | 214 (33.81%) | 406 (33.67%) | ||
| Urban–rural fringe | 141 (33.10%) | 209 (33.02%) | 400 (33.17%) | ||
| Rural | 140 (32.86%) | 210 (33.18%) | 400 (33.17%) | ||
| Gender | 6.966 | 0.031 | |||
| Male | 208 (48.83%) | 288 (45.50%) | 504 (41.79%) | ||
| Female | 218 (51.27%) | 345 (54.50%) | 702 (58.21%) | ||
| Age (years) | 74.530 | <0.001 | |||
| 60–69 | 145 (34.04%) | 224 (35.36%) | 482 (39.97%) | ||
| 70–79 | 192 (45.07%) | 258 (40.76%) | 449 (37.23%) | ||
| ≥80 | 89 (20.89%) | 151 (23.88%) | 275 (22.80%) | ||
| Living situation | 29.604 | <0.001 | |||
| Living alone | 37 (8.69%) | 59 (9.32%) | 143 (11.86%) | ||
| Living only with spouse | 208 (48.83%) | 283 (44.71%) | 632 (52.40%) | ||
| Living only with children | 76 (17.84%) | 117 (18.48%) | 151 (12.52%) | ||
| Living with spouse and children | 103 (24.18%) | 173 (27.33%) | 280 (23.22%) | ||
| Living in nursing home | 2 (0.47%) | 1 (0.16%) | 0 (0.00%) | ||
| Education level | 275.510 | <0.001 | |||
| No schooling | 149 (34.98%) | 140 (22.12%) | 90 (7.46%) | ||
| Primary school | 166 (38.97%) | 235 (37.12%) | 393 (32.59%) | ||
| Junior high school | 76 (17.84%) | 138 (21.80%) | 441 (36.57%) | ||
| Technical secondary/high school | 24 (5.63%) | 74 (11.69%) | 233 (19.32%) | ||
| College | 7 (1.64%) | 30 (4.74%) | 31 (2.57%) | ||
| University (and above) | 4 (0.94%) | 16 (2.53%) | 18 (1.49%) | ||
| Medical insurance status | 65.785 | <0.001 | |||
| Basic Social Medical Insurance for Urban Employees | 246 (57.75%) | 381 (60.19%) | 520 (43.12%) | ||
| Basic Social Medical Insurance for Urban and Rural Residents | 178 (41.78%) | 243 (38.39%) | 664 (55.06%) | ||
| Government Medical Scheme | 0 (0.00%) | 0 (0.00%) | 5 (0.41%) | ||
| No medical insurance | 2 (0.47%) | 8 (1.26%) | 12 (1.00%) | ||
| Other | 0 (0.00%) | 1 (0.16%) | 5 (0.41%) | ||
| Average monthly family income * | 151.140 | <0.001 | |||
| <$138/month | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | ||
| $138–$414/month | 27 (6.34%) | 77 (12.16%) | 234 (19.40%) | ||
| $414–$690/month | 114 (26.76%) | 275 (43.44%) | 467 (37.56%) | ||
| $690–$1379/month | 114 (26.76%) | 128 (20.22%) | 237 (19.65%) | ||
| ≥$1.379/month | 88 (20.66%) | 64 (10.11%) | 50 (4.15%) | ||
| Presence of chronic diseases (excluding simple hypertension) | 5.270 | 0.072 | |||
| Yes | 193 (45.31%) | 255 (40.28%) | 470 (38.97%) | ||
| No | 233 (54.69%) | 378 (59.72%) | 736 (61.03%) | ||
| Co-resident family members with illnesses(excluding simple hypertension) | 7.394 | 0.025 | |||
| Yes | 125 (29.34%) | 148 (23.38%) | 279 (23.13%) | ||
| No | 301 (70.66%) | 485 (76.62%) | 927 (76.87%) |
| Variable | Free Policy Region (n = 426) | Partial Reimbursement Region (n = 633) | Self-Paid Policy Region (n = 1206) | χ2 Value | p Value |
|---|---|---|---|---|---|
| Influenza vaccination status | 283.673 | <0.001 | |||
| Yes | 227 (53.29%) | 132 (20.85%) | 164 (13.60%) | ||
| No | 188 (44.13%) | 483 (76.30%) | 989 (82.01%) | ||
| Not sure | 11 (2.58%) | 18 (2.84%) | 53 (4.39%) | ||
| Next-season influenza vaccination intention | 127.759 | <0.001 | |||
| Yes | 293 (68.78%) | 302 (47.71%) | 448 (37.15%) | ||
| No | 133 (31.22%) | 331 (52.29%) | 758 (62.85%) | ||
| Pneumococcal vaccination status | 593.806 | <0.001 | |||
| Yes | 9 (2.11%) | 313 (49.45%) | 90 (7.46%) | ||
| No | 380 (89.20%) | 295 (46.60%) | 1062 (88.06%) | ||
| Not sure | 37 (8.69%) | 25 (3.95%) | 54 (4.48%) | ||
| COVID-19 vaccination status | 1.942 | 0.767 | |||
| Yes | 392 (92.02%) | 587 (92.73%) | 1129 (93.62%) | ||
| No | 22 (5.16%) | 32 (5.06%) | 55 (4.56%) | ||
| Not sure | 12 (2.82%) | 14 (2.21%) | 22 (1.82%) |
| Dimension | Free Policy Region (n = 426) | Partial Reimbursement Region (n = 633) | Self-Paid Policy Region (n = 206) | F Value | p Value | |||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |||
| Basic influenza knowledge | 11.28 | 1.86 | 9.99 | 1.74 | 10.52 | 1.99 | 57.862 | <0.001 |
| Perceived susceptibility | 16.70 | 3.84 | 15.37 | 3.25 | 15.85 | 3.61 | 17.923 | <0.001 |
| Perceived severity | 17.35 | 4.06 | 17.06 | 3.65 | 18.18 | 3.65 | 21.223 | <0.001 |
| Perceived vaccination benefit | 20.23 | 3.41 | 18.69 | 3.04 | 19.30 | 3.55 | 26.155 | <0.001 |
| Perceived vaccination barriers | 21.72 | 6.20 | 24.38 | 4.79 | 25.26 | 5.25 | 69.604 | <0.001 |
| Action cues | 23.07 | 4.85 | 20.48 | 3.88 | 19.52 | 4.49 | 102.520 | <0.001 |
| Free Policy Region (n = 426) | Partial Reimbursement Region (n = 633) | Self-Paid Policy Region (n = 1206) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dependent Variable | Independent Variable | β | Wald χ2 Value | Adjusted OR (95% CI) | p Value | β | Wald χ2 Value | Adjusted OR (95% CI) | p Value | β | Wald χ2 Value | Adjusted OR (95% CI) | p Value |
| Current-season vaccination behavior | Basic influenza knowledge | 0.080 | 1.468 | 1.083 (0.953–1.235) | 0.226 | 0.025 | 0.138 | 1.026 (0.898–1.172) | 0.710 | 0.043 | 0.748 | 1.044 (0.948–1.150) | 0.387 |
| Perceived susceptibility | −0.014 | 0.135 | 0.986 (0.917–1.060) | 0.713 | 0.121 | 8.676 | 1.128 (1.043–1.225) | 0.003 | 0.064 | 4.797 | 1.066 (1.007–1.129) | 0.029 | |
| Perceived severity | −0.089 | 5.442 | 0.914 (0.847–0.985) | 0.020 | −0.052 | 1.827 | 0.949 (0.880–1.024) | 0.177 | 0.010 | 0.108 | 1.010 (0.952–1.072) | 0.742 | |
| Perceived vaccination benefit | 0.081 | 2.725 | 1.084 (0.985–1.194) | 0.099 | 0.094 | 3.044 | 1.099 (0.989–1.223) | 0.081 | −0.003 | 0.009 | 0.997 (0.935–1.063) | 0.923 | |
| Perceived vaccination barriers | −0.006 | 0.082 | 0.994 (0.957–1.034) | 0.774 | −0.033 | 1.955 | 0.968 (0.924–1.013) | 0.162 | −0.057 | 10.416 | 0.944 (0.911–0.977) | 0.001 | |
| Action cues | 0.195 | 33.975 | 1.215 (1.140–1.300) | <0.001 | 0.192 | 21.984 | 1.211 (1.120~1.315) | <0.001 | 0.133 | 26.461 | 1.142 (1.087–1.202) | <0.001 | |
| Next-season vaccination intention | Basic influenza knowledge | −0.044 | 0.306 | 0.957 (0.818–1.119) | 0.580 | −0.107 | 2.885 | 0.898 (0.793–1.016) | 0.089 | 0.074 | 3.460 | 1.077 (0.996–1.165) | 0.063 |
| Perceived susceptibility | 0.165 | 13.278 | 1.180 (1.081–1.292) | <0.001 | 0.180 | 22.936 | 1.197 (1.113–1.290) | <0.001 | 0.075 | 10.123 | 1.078 (1.029–1.129) | 0.001 | |
| Perceived severity | −0.065 | 2.014 | 0.937 (0.855–1.024) | 0.156 | −0.016 | 0.215 | 0.984 (0.917–1.054) | 0.643 | −0.035 | 2.083 | 0.966 (0.921–1.012) | 0.149 | |
| Perceived vaccination benefit | 0.047 | 0.668 | 1.048 (0.937–1.174) | 0.414 | 0.105 | 5.083 | 1.111 (1.015–1.218) | 0.024 | 0.031 | 1.511 | 1.032 (0.982–1.085) | 0.219 | |
| Perceived vaccination barriers | −0.020 | 0.580 | 0.980 (0.932–1.033) | 0.446 | −0.024 | 1.233 | 0.976 (0.935–1.019) | 0.267 | −0.042 | 9.286 | 0.958 (0.932–0.985) | 0.002 | |
| Action cues | 0.266 | 45.504 | 1.305 (1.212–1.415) | <0.001 | 0.221 | 42.155 | 1.247 (1.169–1.336) | <0.001 | 0.230 | 117.971 | 1.258 (1.208–1.313) | <0.001 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Su, R.; Zhao, H.; Yang, X.; Qin, Y.; Zheng, J.; Liu, X.; Du, X.; Peng, Z. Influenza Vaccination in the Elderly in Three Cities in China: Current Status and Influencing Factors Under Different Funding Policies. Vaccines 2025, 13, 1158. https://doi.org/10.3390/vaccines13111158
Su R, Zhao H, Yang X, Qin Y, Zheng J, Liu X, Du X, Peng Z. Influenza Vaccination in the Elderly in Three Cities in China: Current Status and Influencing Factors Under Different Funding Policies. Vaccines. 2025; 13(11):1158. https://doi.org/10.3390/vaccines13111158
Chicago/Turabian StyleSu, Rina, Hongting Zhao, Xiaokun Yang, Ying Qin, Jiandong Zheng, Xinyi Liu, Xinwei Du, and Zhibin Peng. 2025. "Influenza Vaccination in the Elderly in Three Cities in China: Current Status and Influencing Factors Under Different Funding Policies" Vaccines 13, no. 11: 1158. https://doi.org/10.3390/vaccines13111158
APA StyleSu, R., Zhao, H., Yang, X., Qin, Y., Zheng, J., Liu, X., Du, X., & Peng, Z. (2025). Influenza Vaccination in the Elderly in Three Cities in China: Current Status and Influencing Factors Under Different Funding Policies. Vaccines, 13(11), 1158. https://doi.org/10.3390/vaccines13111158






