Abstract
Background: Vaccine hesitancy (VH) remains a major threat to global health that can reverse the progress in tackling vaccine-preventable diseases. Vaccine uptake among adolescent Girls and young women (AGYW) is often low. We assessed VH using a validated scale among AGYW in Uganda, Zambia, and South Africa. Methods: From June 2023 to February 2024, we recruited AGYW from fishing communities in Uganda, urban and peri-urban locations in Lusaka and Ndola, Zambia, and mining communities in Rustenburg, South Africa. Eligible participants were aged 15–24 years, sexually active, and HIV-negative but at risk for HIV acquisition. We collected demographic, HIV-related behavioral data, and vaccine hesitancy data using a structured questionnaire. Vaccine confidence was assessed using the 10-question Vaccine Hesitancy Scale that describes two factors, i.e., “vaccine confidence” and “risk tolerance”. Exploratory and Confirmatory Factor Analyses were performed to assess scale validity and internal consistency. Logistic regression was used to determine associations between demographics and vaccine confidence. Results: A total of 1213 AGYW participated in the study, with a mean age of 19.4 (SD ± 2.6) years. More than half (54%) were aged between 15 and 19 years. The majority of AGYW (94%) strongly believed that vaccines were important for their health and the community and that vaccination is a good way to protect them from diseases. About two-thirds of the AGYW (66%) indicated that they were concerned about the adverse effects of vaccines, while 30% responded that they did not need vaccines for diseases that were not common. We observed that 951 (78%) of the AGYW reported high vaccine confidence, while 494 (41%) reported low concerns over risks. Vaccine confidence varied across countries, with Zambia and Uganda showing lower vaccine confidence (adjusted odds ratios of 0.28 and 0.45, respectively, p < 0.005) in comparison to South Africa. Conclusions: A high level of vaccine confidence was observed among AGYW. Vaccine confidence among AGYW was driven more by the trust in vaccine safety and the need to protect communities against diseases. These findings suggest the potential for acceptance of vaccines, including future HIV vaccines, among AGYW. Despite high levels of vaccine confidence, concerns over vaccine risks remain substantial and must be addressed.
1. Introduction
Vaccine hesitancy (VH), defined as the delay in acceptance or refusal of vaccines despite the availability of vaccination services, remains a major threat to global immunization goals [1,2]. In East and Southern Africa, challenges in achieving high vaccination coverage rates persist, including VH, which undermines the effectiveness of vaccines critical for preventing high-burden diseases such as cervical cancer, hepatitis B, and COVID-19 [3,4,5]. Adolescent Girls and Young Women (AGYW) in this region face intersecting social, cultural, and informational vulnerabilities that shape their risk of VH [6]. These include limited autonomy in health decision-making, low levels of vaccine literacy, gender power dynamics that often prioritize community or parental and peer influence over individual agency [7,8], high exposure to misinformation, particularly through social media platforms [9,10,11], and low educational attainment and misconceptions about fertility and vaccine safety [12]. Additional influences include mistrust in health systems [13].
While VH is a global issue, its impact may be profound in vulnerable populations, particularly AGYW at risk of acquiring Human Immunodeficiency Virus (HIV). This is partly because they represent a crucial demographic at a high risk of vaccine-preventable diseases (VPDs), such as Human Papilloma Virus (HPV) and Hepatitis B and C [14]. VH may further hinder efforts to study, test, and deploy any future vaccines, including HIV vaccines.
The Strategic Advisory Group of Experts on Immunization (SAGE) acknowledges that many factors contribute to VH and that there is no unique group of determinants behind VH in all settings. According to the “3Cs” model, VH is linked to confidence, convenience, and complacency [2]. Confidence is defined as trust in the effectiveness and safety of vaccines; the system that delivers them, including the reliability and competence of health services and health professionals; and the motivations of policymakers who guide recommended vaccines. Convenience is defined as the perceived level of access to vaccinations. It depends on physical availability, affordability, geographical accessibility, ability to understand information (language and health literacy), and appeal of immunization services (the quality of the service). Complacency is defined as the perceived risk of contracting the disease; when the perceived risk is low, vaccination may be thought of as an unnecessary preventive action.
The long-term global goal is to develop a safe and effective HIV vaccine that protects people from acquiring HIV. Given the high vulnerability of AGYW, it is important to develop safe and effective HIV prevention products that could target this population. However, vaccine acceptance and confidence remain crucial barriers to the success of any vaccination program. Vaccine uptake among adolescents and young adults has been reported to be low [14], and this might impair the ability to study, test, and roll out any potential new HIV/AIDS vaccines.
Understanding the drivers of VH among AGYW in East and Southern Africa is essential to inform targeted, gender-responsive interventions to improve vaccine coverage. To understand VH among AGYW, the International AIDS Vaccine Initiative (IAVI) included a VH module in the Multisite study for AGYW for future HIV vaccines and antibodies for prevention of HIV (MAGY) study, conducted in Uganda, Zambia, and South Africa. The MAGY study partly aimed to establish cohorts of AGYW for the evaluation of HIV prevention products in sub-Saharan Africa. This publication presents findings from MAGY that focused on assessing vaccine confidence among AGYW.
2. Materials and Methods
2.1. Study Design
This cross-sectional survey was embedded within the MAGY study, a prospective observational cohort study. MAGY was a flagship study under the International AIDS Vaccine Initiative, Accelerate the Development of Vaccines and New Technologies to Combat the AIDS Epidemic (IAVI ADVANCE) program, enrolling AGYW (15–24 years old) between June 2023 and February 2024. Vaccine confidence data were collected from each participant as part of the baseline assessment at enrollment.
2.2. Study Setting
Participants were recruited from distinct communities in three countries: fishing communities around Lake Victoria (including islands Kimi and Nsazi, as well as landing sites Kasenyi, Kigungu, and Nakiwogo) in Uganda; urban and peri-urban areas in Lusaka and Ndola, Zambia, including primary healthcare settings serving single, sexually active mothers and known hotspots for female sex workers (FSWs); and various healthcare facilities, youth groups, and community outreach activities in Rustenburg, a mining town in South Africa’s North West Province. Before screening visits, community engagement was conducted to identify potential participants. Potential participants were invited to study clinics where screening and enrollment occurred. Additional recruitment strategies included peer referrals, participant recommendations, flyers and posters, and social media platforms such as Facebook and Twitter.
2.3. Study Participants
Eligible participants were HIV-negative, non-pregnant AGYW aged 15 to 24 years old, who reported sexual activity in the past three months, and met at least one criterion from a validated risk assessment questionnaire that adapted the VOICE risk assessment questionnaire [developed for adult women for Pre-exposure Prophylaxis (PrEP) trials in sub-Saharan Africa] [15], and the Ayton risk assessment (designed for AGYW in rural South Africa) [16]. HIV risk assessment was based on any one of the following: sexual intercourse in the past three months; use of contraception in the last year; perceived high HIV risk; ever having been pregnant; low HIV knowledge; financial dependence (relying on sexual partners for financial support); and any alcohol or illicit drug use in the past year. All participants who met the eligibility criteria were enrolled after providing informed consent.
2.4. Data Collection
Data collection took place in clinic rooms to ensure privacy and confidentiality. Trained study clinicians administered a face-to-face structured interview questionnaire (Supplementary File S1) to obtain social demographic data such as age, level of education, marital status, religion, source of income, and information about vaccines. Information about VH was obtained through administering the validated Vaccine Hesitancy Scale (VHS) [17], which included 10 Likert scale questions assessing thoughts on general vaccine confidence; responses were coded 1 for “strongly disagree”, 2 “disagree”, 3 “neither disagree nor agree”, 4 “agree”, or 5 “strongly agree”. The ten questions included; (1) Vaccines are important for my health; (2) Vaccines are effective; (3) Being vaccinated is important for the health of others in the community; (4) All routine vaccinations recommended by the local authority on vaccination (this varied by country) are beneficial; (5) New vaccines carry more risks than others; (6) The information I receive from the local authority on vaccination is reliable and trustworthy; (7) Getting vaccines is a good way to protect me from diseases; (8) Generally, I do what my doctor or healthcare provider recommends about vaccines for me; (9) I am concerned about serious adverse effects of vaccines; and (10) I don’t need vaccines for diseases that are not common anymore.
2.5. Statistical Analysis
The data were electronically captured in the REDCap (Westlake, TX, USA) software database, and data analysis was performed using STATA SE version 18 (Stata Corp, College Station, TX, USA). Participant characteristics were summarized overall and by study site.
To determine the latent traits or factors in the VHS, Exploratory Factor Analysis (EFA) was conducted on half of the sample (n = 606; randomly selected) using the Principal Component Factor method (PCF) and the maximum likelihood (ML) method for the factor loadings of the VHS with oblique rotation (Promax). Oblique rotation was chosen because the factors were expected to be correlated, allowing for a more accurate representation of the underlying structure. To examine model fit, Confirmatory Factor Analysis (CFA) was performed on the second half sample (n = 607). To determine the internal consistency, we used Cronbach’s alpha to determine scale reliability.
To determine the level of vaccine confidence for each item on the VHS, we constructed a 5-point scale of the class intervals for interpreting the VHS items’ average score. We reverse-coded items 1, 2, 3, 4, 6, 7, and 8 on the VHS to ensure that higher values consistently represent lower vaccine confidence. Scores (1–5) were grouped into class intervals to simplify analysis and interpretation. The interval width was calculated by dividing the score range (5 − 1 = 4) by the number of scores (5), resulting in a width of 0.8. Intervals were created by adding this width to the minimum score (1) (Table 1). Average scores, frequencies, and percentages were then calculated. This approach follows best practices by categorizing scores to improve interpretive clarity and facilitating comparisons [18].

Table 1.
The 5-point scale of the class intervals for interpreting the composite scores using averages (mean).
A composite score for each respective factor was calculated by taking the mean values of its respective component questions. These scores were then dichotomized: values less than or equal to 2 (representing “Strongly Agree” or “Agree” responses, with regard to confidence in vaccines or risk tolerance) were coded as 0, while values greater than 2 (representing “Neither Agree nor Disagree,” “Disagree,” or “Strongly Disagree” responses) were coded as 1.
Bivariate logistic regression analyses were performed between covariates and both hesitancy scores (confidence and risk tolerance). We analyzed individual associations between demographic characteristics (including country, age, relationship status, religious affiliation, education level, source of income, and school attendance) and each outcome and calculated crude odds ratios with 95% confidence intervals and p-values. Covariates that showed statistical significance (p < 0.2) were then included in multivariate logistic regression models to identify factors independently associated with vaccine confidence. To control potential confounding factors, adjusted odds ratios were calculated for significant predictors.
3. Results
3.1. Socio-Demographic Characteristics of Study Participants
A total of 1213 AGYW were interviewed, 656 (54%) were aged between 15 and 19 years. The mean age was 19.4 (SD ± 2.6) years. The majority of AGYW, 1197 (99%), previously attended school, while only 351 (29%) were still in school. Most, 1107 (91%) of the AGYW had never married, and 750 (62%) were single with steady sexual partners. Details of the demographic characteristics are depicted in Table 2.

Table 2.
Socio-demographic characteristics of AGYW in the MAGY cohort study in Uganda, Zambia, and South Africa.
3.2. Responses to Vaccine Hesitancy Scale Items
The MAGY cohort showed strong positive beliefs about vaccines, with favorable mean scores regarding vaccines’ importance for personal health (1.77) and community benefit (1.78). They strongly agreed that vaccination is effective for disease prevention (1.72). However, they expressed significant concerns about vaccine safety, with a high mean score of 3.56 regarding serious adverse effects. They also showed moderate confidence towards new vaccines, perceiving them as riskier than established vaccines (mean score 2.74).
Most AGYW agreed or strongly agreed that vaccines were important for their health (94%); vaccines were effective (87%); being vaccinated was important for the health of others in the community (93%); and all routine vaccinations recommended by national vaccination programs were beneficial (91%). About two-thirds (66%) of the AGYW agreed or strongly agreed that they were concerned about the serious adverse effects of vaccines, while 30% agreed or strongly agreed that they do not need vaccines for diseases that are not common anymore. Details of the responses and average scores to the VHS items are shown in Table 3 below.

Table 3.
Descriptive analysis of Vaccine Hesitancy Scale responses (n = 1213).
3.3. Structure, Model Fit, and Internal Consistency of the VHS
To examine the structure of our VHS items, we performed Exploratory Factor Analysis (EFA). Promax rotation was used in the EFA because it allows factors to correlate with each other, which is more realistic for behavioral constructs and helps identify a clearer factor structure. The Confirmatory Factor Analysis (CFA) remained unrotated since it tested a pre-specified factor structure based on theory, making rotation unnecessary. Details are shown in Table 4. The analysis revealed two distinct factors that describe the 10 VHS items, with Eigenvalues greater than 1. These two factors together accounted for 52% of the total variance in the items. We describe these two factors as “vaccine confidence” and “risk tolerance”. Vaccine confidence was dominant, explaining 40% of the variance, while risk tolerance explained 12%. Details are shown in Table 5. As shown in Table 4, 7 VHS items were loaded on vaccine confidence, and two items were loaded on risk tolerance. Only 9 of the 10 VHS items loaded on our factors. Item 9, “I am concerned about the serious adverse effects of vaccines,” didn’t load on either factor.

Table 4.
Exploratory Factor Analysis, showing rotated and unrotated factor loadings (n = 606).

Table 5.
Exploratory Factor Analysis of putative latent factors (n = 606).
We conducted a CFA on two sets of the VHS items: one with nine items, excluding item 9 (“I am concerned about the serious adverse effects of vaccines”), and another with all ten items included. Using data from 607 participants, the analysis revealed that item 9 had a very weak loading of 0.14 on the risk tolerance factor. The CFA results demonstrated that all the remaining nine items loaded strongly onto their respective factors, providing robust support for our two-factor model, as detailed in the test statistics presented in Table 6.

Table 6.
Confirmatory Factor Analysis Model Fit statistics for a 2-factor model.
To assess the internal consistency of both factors, we calculated Cronbach’s alpha based on data from 1213 participants. For vaccine confidence, Cronbach’s alpha was 0.85, indicating excellent scale reliability. However, for risk tolerance, Cronbach’s alpha was 0.44, which is considered poor. This low value is likely due to the small number of items on the risk tolerance factor, as scale reliability typically improves with more items. On including item 9 of our VHS on risk tolerance, our Cronbach’s alpha dropped to 0.34, implying that question 3 reduces the reliability of this factor. The correlation between the two factors was 0.26, suggesting a weak association and indicating that they represent separate dimensions of VH.
3.4. Relationship Between Demographic Characteristics and Vaccine Confidence
3.4.1. Correlates of Vaccine Confidence
As shown in Figure 1, 951 (78.4%) AGYW exhibited high vaccine confidence. We observed significant variations in vaccine confidence levels among countries, with AGYW in Zambia (adjusted odds ratios (aOR): 0.26, 95% CI: 0.18–0.39) showing a lower likelihood of vaccine confidence, followed by Uganda [aOR]: 0.44, 95% confidence interval (CI): 0.29–0.66) in comparison to South Africa. Participants not currently in school showed lower vaccine confidence compared to those who were in school (aOR 0.70, 95% CI: 0.50–0.97).
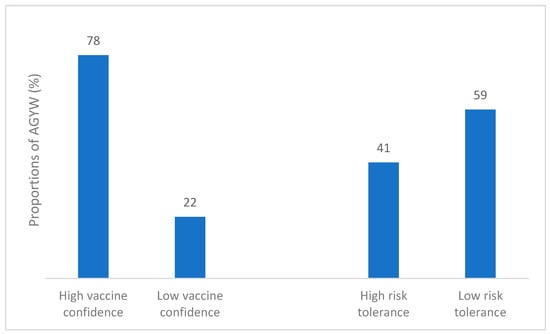
Figure 1.
Vaccine confidence and Risk tolerance of 1213 AGYW.
Participants with formal employment (aOR 0.55, 95% CI: 0.31–0.96) and those receiving Support/assistance (aOR 0.59, 95% CI: 0.40–0.87) showed lower vaccine confidence than the participants with no source of income. Table 7 shows the details of demographic characteristics and vaccine confidence.

Table 7.
Correlates of vaccine confidence.
3.4.2. Correlates of Risk Tolerance
As shown in Figure 1, 41% of respondents demonstrated high risk tolerance. There was a significant variation in risk tolerance levels across the three countries, with Zambia (aOR: 0.22, 95% CI: 0.16–0.31) showing the lowest risk tolerance, followed by Uganda (aOR: 0.53, 95% CI: 0.37–0.76) compared to South Africa.
Participants in formal employment (aOR 0.44, 95% CI: 0.26–0.73), informal employment (aOR: 0.55, 95% CI: 0.33–0.94), and those receiving support/assistance (aOR 0.39, 95% CI: 0.26–0.60) showed significantly lower risk tolerance than the participants with no source of income.
Participants who were not in school showed lower risk tolerance compared to those who were in school (OR 0.66, 95% CI: 0.48–0.91). Details are shown in Table 8 below.

Table 8.
Correlates of risk tolerance.
4. Discussion
Vaccination remains one of the most cost-effective strategies to reduce the global burden of infectious diseases. In this cohort of AGYW, we observed a high level of vaccine confidence coupled with a low risk tolerance for vaccines. Specifically, more than 90% of AGYW believed that vaccines were effective, safe, and that vaccination was important to protecting both themselves and their communities. These findings are promising from a public health perspective, as high vaccine confidence may lead to increased vaccine uptake and consequently reduce the burden of vaccine-preventable diseases. However, the low-risk tolerance noted could contribute to vaccine hesitancy, especially with the introduction of new vaccines.
A systematic review examining knowledge, attitudes, and practices towards adolescent vaccination in Africa reported high acceptability of vaccines among adolescents [19]. In contrast, Wang et al. reported lower levels of vaccine confidence among adolescents, who were less likely to believe in the benefits and safety of vaccines [20]. Notably, Wang et al.’s study included both adolescent males and females and found the males to be less confident about vaccines than the females. It also compared vaccine confidence among adolescents and adults, but never examined vaccine confidence among adolescents alone.
Despite ongoing vaccination promotion efforts, VH remains a significant issue [14,21] and was identified as one of the ten leading global health threats by the World Health Organization (WHO) [1]. To address this challenge, the WHO recommends regular monitoring of vaccine confidence, which remains understudied among adolescents [22,23]. Most of the recent studies have predominantly focused on vaccine confidence about COVID-19 vaccines [3,24], while others have targeted HPV vaccines [7,25,26,27,28]. Our study is among the first to assess vaccine confidence among AGYW at risk of HIV acquisition in sub-Saharan Africa using the VHS. The VHS has been widely used in different populations to assess VH and is more reliable in measuring “lack of confidence” than “risk tolerance” [29,30]. It demonstrated acceptable reliability and validity when applied to AGYW at risk of HIV, a finding similar to that of Shapiro et al. [17]. In our study, we found strong scale reliability for the “vaccine confidence” factor, with a high Cronbach’s alpha (0.85), while the “vaccine risk tolerance” factor showed poor reliability, with a Cronbach’s alpha of 0.44.
We observed several covariates correlating with vaccine confidence and tolerance for risk. AGYW living in Zambia were less likely to accept vaccines than those living in Uganda and South Africa. The AGYW from Zambia also demonstrated a lower risk tolerance for vaccines. This finding is not surprising, as vaccine confidence does vary by region and time [31,32]. Such geographical variation in vaccine confidence is expected, as it can be influenced by factors including healthcare accessibility, information availability, cultural beliefs, and trust in health systems [8,33]. Differences in vaccine information access are particularly relevant, as limited access may contribute to lower confidence [13,32].
While several studies have reported an association between the level of education and VH [34], we observed that there was no association between the level of education and vaccine confidence. For instance, Wegner et al. showed that Indian mothers with a high school education reported higher vaccine confidence than those with less [35]. The relationship between the level of education and VH is complex and influenced by various factors, including knowledge, perception, access to information, trust in healthcare systems, and sociocultural contexts [36]. AGYW with lower education levels may face challenges in accessing reliable health information or understanding and interpreting public health information. This could make them more susceptible to misinformation or confusion about vaccines, potentially contributing to VH. Furthermore, AGYW with no or less education might not fully understand the severity of vaccine-preventable diseases or may underestimate the potential risks of not vaccinating, leading to complacency [37]. This study, however, reported that AGYW who were not in school showed lower vaccine confidence compared to those who were in school. We did not observe any association between vaccine hesitancy (VH) and level of education, likely because more than three-fourths of the MAGY cohort were either currently in secondary school, had completed secondary school, or were enrolled in tertiary education. As a result, the educational status of participants was skewed toward AGYW with at least some high school education. Additionally, recruitment for the MAGY study began shortly after the peak of the COVID-19 pandemic, a period during which communities had experienced first-hand the life-saving impact of vaccines through the scale-up of COVID-19 vaccination efforts. This likely reduced the influence of formal education as the sole source of vaccine information, as community members were exposed to messaging on the benefits of vaccination from multiple sources beyond formal schooling. However, we did observe that AGYW who were currently in school had significantly higher vaccine confidence compared to those who were not. This may be attributed to the role that formal education played in vaccine education during the pandemic, reinforcing positive perceptions about vaccination.
We further report that the source of income was associated with vaccine confidence and risk tolerance. The AGYW who had no source of income were more likely to be vaccine-confident than those who were employed. AGYW with formal employment and those receiving support/assistance showed significantly lower vaccine confidence than the participants with informal or no source of income. The association between socioeconomic status and vaccine confidence is multifactorial [38]. Our finding that low socioeconomic status was associated with vaccine confidence could demonstrate the trust in healthcare systems, which in Africa often provide vaccines for free or at low cost, coupled with fewer resources to access alternative information sources that fuel VH (e.g., online misinformation) [39,40].
Limitations
This study had some limitations. First, our study population was restricted to AGYW at risk for HIV, excluding AGYW who were pregnant, those living with HIV, and lower risk (typically those who did not report sexual activity in the previous three months), limiting generalizability. While the study benefits from a relatively large sample of diverse AGYW across three countries, our study population should not be considered broadly representative of Ugandan, Zambian, and South African AGYW. Second, “vaccine confidence” items on the VHS were worded positively, and all “risk tolerance” items were worded negatively. Consequently, the focus and content of the items on the scale became intertwined. Therefore, the item that was eliminated for not loading on either factor could have been due to the intertwining. Third, only two items loaded on the second factor assessing “tolerance for risks”. Scales with factors that are composed of fewer than three items are considered unstable, and calculating Cronbach’s alpha for a two-item sub-scale has limitations. Fourth, this study assessed responses to the VHS for vaccines in general; thus, these findings do not represent confidence in specific vaccines. It is well known that vaccine confidence varies according to the type of vaccine. Finally, this study was cross-sectional, and it is therefore not advisable to draw causal conclusions between our covariates and the respective correlated elements of confidence.
5. Conclusions
Our study reports that the VHS consisted of two factors, including “vaccine confidence” and “tolerance for risks.” However, the few items on risk tolerance could affect the scale’s reliability in measuring concerns and risks associated with vaccines. Vaccine confidence among AGYW was driven more by the trust in vaccine safety and the need to protect communities against diseases. This highlights the importance of addressing the perceptions and attitudes that the AGYW may have about vaccines, particularly newer ones. Demographic factors such as being in school, socioeconomic status, and country of origin were associated with vaccine confidence levels among AGYW in our study. Therefore, future interventions aimed at increasing vaccine uptake among AGYW should focus on improving education about vaccine safety tailored to the audience (e.g., cultural background, education, and socio-economic status), addressing specific concerns related to side effects, and leveraging trusted community leaders to build confidence in vaccines. Additionally, health communication strategies should be tailored to address the unique concerns of AGYW who may be more vulnerable to vaccine misinformation. This is crucial for informing future interventions aimed at enhancing vaccine uptake in this population.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/vaccines13111083/s1, Supplementary File S1: Socio-demographic questionnaire. Vaccine Hesitancy module questionnaire.
Author Contributions
Conceptualization, N.K., A.N., A.S., M.O.K., J.M., V.E., P.M., W.K., B.O., K.O., S.C.F. and M.A.P.; methodology, N.K., M.A.P., G.B., M.O.K., P.M., W.K., J.M., B.O., V.E., G.B. and J.M.A.; software, N.K.; validation, G.B., and formal analysis, J.M.A. and M.A.P.; investigation, A.S., J.M. and B.O.; resources, K.O., M.O.K. and S.C.F.; data curation, M.I., C.K., K.M.-M. and N.K.; writing—original draft preparation, N.K. and J.M.A.; writing—review and editing, A.S., W.K., M.O.K., A.N., M.A.P., J.M., B.O., K.O., G.B., M.I., P.M. and V.E.; visualization, N.K., J.M.A. and A.S.; supervision, A.S., W.K., P.M. and M.O.K.; project administration, A.S., W.K., P.M. and K.O.; funding acquisition, M.O.K., P.M., B.O., K.O., S.C.F. and W.K. All authors have read and agreed to the published version of the manuscript.
Funding
This work was funded by IAVI, grant number: Agreement A11565, and made possible by the support of many donors, including the United States Agency for International Development (USAID). The full list of IAVI donors is available at http://www.iavi.org. The contents of this manuscript are the responsibility of the authors and do not necessarily reflect the views of USAID or the US Government.
Institutional Review Board Statement
Ethical approval was obtained from the Uganda Virus Research Institute Research and Ethics Committee (UVRI-REC) approval number GC/127/947, and the Uganda National Council for Science and Technology (UNCST) approval number HS2741ES, University of Zambia Biomedical Research Committee (Ref No. 3414-2022) and National Health Research Authority (Ref: NHREB0006/05/02/2023), in Zambia. In South Africa, the study was reviewed and approved by the University of Witwatersrand Human Research Ethics Committee (Ref No. 221114B) and the Research Committee of the Northwest Provincial Department of Health.
Informed Consent Statement
Written informed consent was sought from AGYW aged 18 years and above. Both parental consent and assent were sought for all minors, while emancipated minors assented to participate in the study. All participants’ data were anonymized to ensure confidentiality, and strict measures were taken to protect participant privacy throughout the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data is not publicly available due to ethical restrictions.
Acknowledgments
We are grateful to the study participants. We wish to acknowledge the support from the University of California, San Francisco’s International Traineeships in AIDS Prevention Studies (ITAPS), U.S. NIMH, R25MH123256. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. IAVI participated in data collection, data analysis, data interpretation, and writing of the report. The corresponding authors had full access to all the data in the study and had final responsibility for the decision to submit for publication. IAVI’s donors had no role in study design, data collection, data analysis, data interpretation, or writing of the report. We further acknowledge the research teams at UVRI-IAVI HIV vaccine program, the Center for Family Health Research in Zambia (CFHRZ), and the Aurum Institute for collecting the data from the research participants.
Conflicts of Interest
Author Nasimu Kyakuwa, Ali Ssetaala, Annet Nanvubya, Geofrey Basalirwa, Brenda Okech, Juliet Mpendo was employed by the company Uganda Virus Research Institute—International AIDS Vaccine Initiative (UVRI-IAVI) HIV Vaccine Program Ltd. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| OR | Odds Ratio |
| 95%CI | 95% Confidence Interval |
| HIV | Human Immunodeficiency Virus |
| UVRI | Uganda Virus Research Institute |
| IAVI | International AIDS Vaccine Initiative |
| UNCST | Uganda National council for science and Technology |
| USAID | United States Agency for International Development |
References
- WHO. Ten Threats to Global Health in 2019; WHO: Geneva, Switzerland, 2019. [Google Scholar]
- MacDonald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Wang, D.; Chukwu, A.; Mwanyika-Sando, M.; Abubakari, S.W.; Assefa, N.; Madzorera, I.; Hemler, E.C.; Ismail, A.; Lankoande, B.; Mapendo, F.; et al. COVID-19 vaccine hesitancy and its determinants among sub-Saharan African adolescents. PLoS Glob. Public Health 2022, 2, e0000611. [Google Scholar] [CrossRef]
- Duncan, J.; Harris, M.; Skyers, N.; Bailey, A.; Figueroa, J.P. A call for low-and middle-income countries to commit to the elimination of cervical cancer. Lancet Reg. Health–Am. 2021, 2, 100036. [Google Scholar] [CrossRef]
- Ochola, E.; Ocama, P.; Orach, C.G.; Nankinga, Z.K.; Kalyango, J.N.; McFarland, W.; Karamagi, C. High burden of hepatitis B infection in Northern Uganda: Results of a population-based survey. BMC Public Health 2013, 13, 727. [Google Scholar] [CrossRef] [PubMed]
- Adeyanju, G.C.; Betsch, C.; Adamu, A.A.; Gumbi, K.S.; Head, M.G.; Aplogan, A.; Tall, H.; Essoh, T.-A. Examining enablers of vaccine hesitancy toward routine childhood and adolescent vaccination in Malawi. Glob. Health Res. Policy 2022, 7, 28. [Google Scholar] [CrossRef]
- Rujumba, J.; Akugizibwe, M.; Basta, N.E.; Banura, C. Why don’t adolescent girls in a rural Uganda district initiate or complete routine 2-dose HPV vaccine series: Perspectives of adolescent girls, their caregivers, healthcare workers, community health workers and teachers. PLoS ONE 2021, 16, e0253735. [Google Scholar] [CrossRef]
- Sacre, A.; Bambra, C.; Wildman, J.M.; Thomson, K.; Bennett, N.; Sowden, S.; Todd, A. Socioeconomic inequalities in vaccine uptake: A global umbrella review. PLoS ONE 2023, 18, e0294688. [Google Scholar] [CrossRef]
- Zimet, G.D.; Rosberger, Z.; Fisher, W.A.; Perez, S.; Stupiansky, N.W. Beliefs, behaviors and HPV vaccine: Correcting the myths and the misinformation. Prev. Med. 2013, 57, 414–418. [Google Scholar] [CrossRef] [PubMed]
- Ortiz, R.R.; Smith, A.; Coyne-Beasley, T. A systematic literature review to examine the potential for social media to impact HPV vaccine uptake and awareness, knowledge, and attitudes about HPV and HPV vaccination. Hum. Vaccines Immunother. 2019, 15, 1465–1475. [Google Scholar] [CrossRef] [PubMed]
- Adeyanju, G.C.; Sprengholz, P.; Betsch, C.; Essoh, T.-A. Caregivers’ willingness to vaccinate their children against childhood diseases and human papillomavirus: A cross-sectional study on vaccine hesitancy in Malawi. Vaccines 2021, 9, 1231. [Google Scholar] [CrossRef]
- Essoh, T.-A.; Adeyanju, G.C.; Adamu, A.A.; Tall, H.; Aplogan, A.; Tabu, C. Exploring the factors contributing to low vaccination uptake for nationally recommended routine childhood and adolescent vaccines in Kenya. BMC Public Health 2023, 23, 912. [Google Scholar] [CrossRef]
- Unfried, K.; Priebe, J. Vaccine hesitancy and trust in sub-Saharan Africa. Sci. Rep. 2024, 14, 10860. [Google Scholar] [CrossRef]
- English, A.; Middleman, A.B. Adolescents, young adults, and vaccine hesitancy: Who and what drives the decision to vaccinate? Pediatr. Clin. 2023, 70, 283–295. [Google Scholar]
- Giovenco, D.; Pettifor, A.; MacPhail, C.; Kahn, K.; Wagner, R.; Piwowar-Manning, E.; Wang, J.; Hughes, J.P. Assessing risk for HIV infection among adolescent girls in South Africa: An evaluation of the VOICE risk score (HPTN 068). Afr. J. Reprod. Gynaecol. Endosc. 2019, 22, e25359. [Google Scholar] [CrossRef] [PubMed]
- Ayton, S.G.; Pavlicova, M.; Karim, Q.A. Identification of adolescent girls and young women for targeted HIV prevention: A new risk scoring tool in KwaZulu Natal, South Africa. Sci. Rep. 2020, 10, 13017. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, G.K.; Tatar, O.; Dube, E.; Amsel, R.; Knauper, B.; Naz, A.; Perez, S.; Rosberger, Z. The vaccine hesitancy scale: Psychometric properties and validation. Vaccine 2018, 36, 660–667. [Google Scholar] [CrossRef] [PubMed]
- Alkharusi, H. A descriptive analysis and interpretation of data from Likert scales in educational and psychological research. Indian J. Psychol. Educ. 2022, 12, 13–16. [Google Scholar]
- Abdullahi, L.H.; Kagina, B.M.; Cassidy, T.; Adebayo, E.F.; Wiysonge, C.S.; Hussey, G.D. Knowledge, attitudes and practices on adolescent vaccination among adolescents, parents and teachers in Africa: A systematic review. Vaccine 2016, 34, 3950–3960. [Google Scholar] [CrossRef]
- Wang, B.; Giles, L.; Afzali, H.H.A.; Clarke, M.; Ratcliffe, J.; Chen, G.; Marshall, H. Adolescent confidence in immunisation: Assessing and comparing attitudes of adolescents and adults. Vaccine 2016, 34, 5595–5603. [Google Scholar] [CrossRef]
- Szilagyi, P.G.; Albertin, C.S.; Gurfinkel, D.; Saville, A.W.; Vangala, S.; Rice, J.D.; Helmkamp, L.; Zimet, G.D.; Valderrama, R.; Breck, A.; et al. Prevalence and characteristics of HPV vaccine hesitancy among parents of adolescents across the US. Vaccine 2020, 38, 6027–6037. [Google Scholar] [CrossRef]
- Cadeddu, C.; Castagna, C.; Sapienza, M.; Lanza, T.E.; Messina, R.; Chiavarini, M.; Ricciardi, W.; de Waure, C. Understanding the determinants of vaccine hesitancy and vaccine confidence among adolescents: A systematic review. Hum. Vaccines Immunother. 2021, 17, 4470–4486. [Google Scholar] [CrossRef]
- Ren, J.; Wagner, A.L.; Zheng, A.; Sun, X.; Boulton, M.L.; Huang, Z.; Zikmund-Fisher, B.J. The demographics of vaccine hesitancy in Shanghai, China. PLoS ONE 2018, 13, e0209117. [Google Scholar] [CrossRef] [PubMed]
- Willis, D.E.; Presley, J.; Williams, M.; Zaller, N.; McElfish, P.A. COVID-19 vaccine hesitancy among youth. Hum. Vaccines Immunother. 2021, 17, 5013–5015. [Google Scholar] [CrossRef] [PubMed]
- Omayo, L.N.; Malande, O.O.; Musyoki, A.M.; Hoffman, P.X.; E Adamu, V. Determinants of human papillomavirus (HPV) vaccine hesitancy in sub-Saharan Africa: A systematic review. J. Afr. Soc. Paediatr. Infect. Dis. 2023, 2, 1–29. [Google Scholar] [CrossRef]
- Bitariho, G.K.; Tuhebwe, D.; Tigaiza, A.; Nalugya, A.; Ssekamatte, T.; Kiwanuka, S.N. Knowledge, perceptions and uptake of human papilloma virus vaccine among adolescent girls in Kampala, Uganda; a mixed-methods school-based study. BMC Pediatr. 2023, 23, 368. [Google Scholar] [CrossRef]
- Nakibuuka, V.; Muddu, M.; Kraehenbuhl, J.P.; Birungi, C.; Semitala, F.C.; Tusubira, A.K. Uptake of human papilloma virus vaccination among adolescent girls living with HIV in Uganda: A mixed methods study. PLoS ONE 2024, 19, e0300155. [Google Scholar] [CrossRef]
- Patrick, L.; Bakeera-Kitaka, S.; Rujumba, J.; Malande, O.O. Encouraging improvement in HPV vaccination coverage among adolescent girls in Kampala, Uganda. PLoS ONE 2022, 17, e0269655. [Google Scholar] [CrossRef]
- Luyten, J.; Bruyneel, L.; van Hoek, A.J. Assessing vaccine hesitancy in the UK population using a generalized vaccine hesitancy survey instrument. Vaccine 2019, 37, 2494–2501. [Google Scholar] [CrossRef]
- Domek, G.J.; O’LEary, S.T.; Bull, S.; Bronsert, M.; Contreras-Roldan, I.L.; Ventura, G.A.B.; Kempe, A.; Asturias, E.J. Measuring vaccine hesitancy: Field testing the WHO SAGE Working Group on Vaccine Hesitancy survey tool in Guatemala. Vaccine 2018, 36, 5273–5281. [Google Scholar] [CrossRef]
- Eagan, R.L.; Larson, H.J.; de Figueiredo, A. Recent trends in vaccine coverage and confidence: A cause for concern. Hum. Vaccines Immunother. 2023, 19, 2237374. [Google Scholar] [CrossRef] [PubMed]
- de Figueiredo, A.; Temfack, E.; Tajudeen, R.; Larson, H.J. Declining trends in vaccine confidence across sub-Saharan Africa: A large-scale cross-sectional modeling study. Hum. Vaccines Immunother. 2023, 19, 2213117. [Google Scholar] [CrossRef] [PubMed]
- Mwiinde, A.M.; Kaonga, P.; Jacobs, C.; Zulu, J.M.; Fwemba, I. Determinants of COVID-19 vaccine acceptance and hesitancy among adolescents and youths aged 10–35 years in sub-Saharan African countries: A systematic review and meta-analysis. PLoS ONE 2024, 19, e0310827. [Google Scholar] [CrossRef] [PubMed]
- Cao, M.; Zhao, J.; Huang, C.; Wang, X.; Ye, L.; Han, X.; Yu, W.; Yin, Z.; Zhang, J.; Liu, Y. Assessing vaccine hesitancy using the WHO scale for caregivers of children under 3 years old in China. Front. Public Health 2023, 11, 1090609. [Google Scholar] [CrossRef] [PubMed]
- Wagner, A.L.; Shotwell, A.R.; Boulton, M.L.; Carlson, B.F.; Mathew, J.L. Demographics of vaccine hesitancy in Chandigarh, India. Front. Med. 2021, 7, 585579. [Google Scholar] [CrossRef]
- Adamu, A.A.; Essoh, T.-A.; Adeyanju, G.C.; Jalo, R.I.; Saleh, Y.; Aplogan, A.; Wiysonge, C.S. Drivers of hesitancy towards recommended childhood vaccines in African settings: A scoping review of literature from Kenya, Malawi and Ethiopia. Expert Rev. Vaccines 2021, 20, 611–621. [Google Scholar] [CrossRef]
- Obohwemu, K.; Jong, F.C.-D.; Ling, J. Parental childhood vaccine hesitancy and predicting uptake of vaccinations: A systematic review. Prim. Health Care Res. Dev. 2022, 23, e68. [Google Scholar] [CrossRef]
- Mohd Azizi, F.S.; Kew, Y.; Moy, F.M. Vaccine hesitancy among parents in a multi-ethnic country, Malaysia. Vaccine 2017, 35, 2955–2961. [Google Scholar] [CrossRef]
- Alie, M.S.; Abebe, G.F.; Negesse, Y.; Adugna, A.; Girma, D. Vaccine hesitancy in context of COVID-19 in East Africa: Systematic review and meta-analysis. BMC Public Health 2024, 24, 2796. [Google Scholar] [CrossRef]
- Kulkarni, S.; Sengeh, P.; Eboh, V.; Jalloh, M.B.; Conteh, L.; Sesay, T.; Ibrahim, N.; Manneh, P.O.; Kaiser, R.; Jinnai, Y.; et al. Role of information sources in vaccination uptake: Insights from a cross-sectional household survey in Sierra Leone, 2019. Glob. Health Sci. Pract. 2022, 10, e2100237. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
