The Experience of an Accelerated COVID-19 Immunization Campaign in Oman: A Review Within the WHO Health System Building Blocks Framework
Abstract
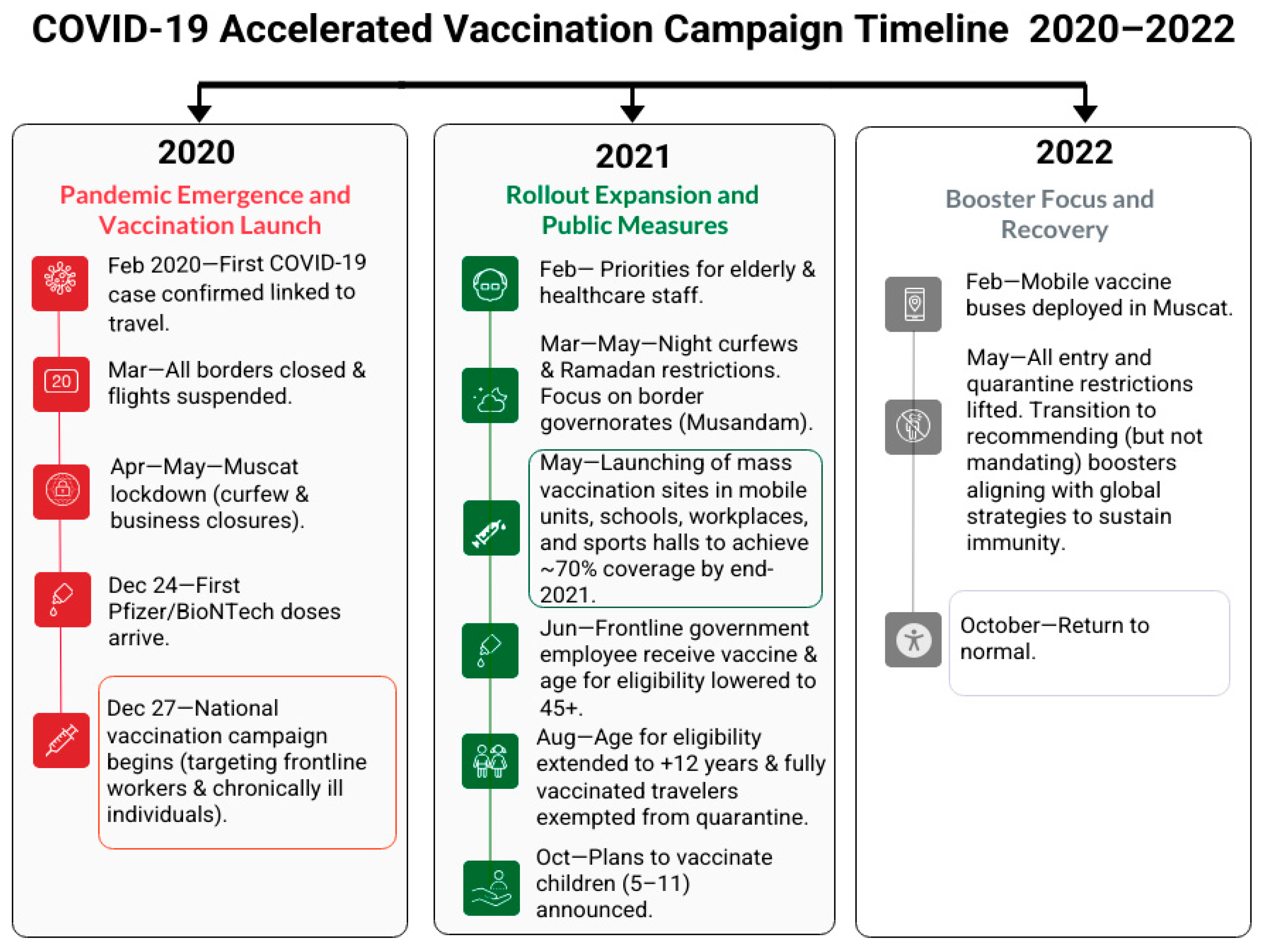
1. Introduction
2. The Objective of the Review
3. The WHO Health System Building Blocks Framework
4. Assessing the Accelerated COVID-19 Vaccination Campaign in Oman in Relation to the WHO Health System Building Blocks
4.1. Leadership and Governance
4.1.1. Roles of Other Core Government Sectors
4.1.2. Integrating Public–Private Partnership
4.1.3. Role of the Community and Volunteers
4.2. Service Delivery and Healthcare Responsiveness
4.2.1. Evidence for COVID-19 Vaccination
4.2.2. Reporting of Reactions to COVID-19 Vaccination
4.2.3. Reaching out to Non-Arabic Speakers
4.3. The Health Workforce
4.4. Health Information Systems
4.5. Access to Essential Medicines
4.6. Financing
5. Strengths, Challenges, and Lessons Learned
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| WHO | World Health Organization |
| EVM | Effective Vaccine Management |
| MoH | Ministry of Health |
| PHC | Primary Healthcare |
| HCWs | Healthcare Workers |
References
- Moghadas, S.M.; Vilches, T.N.; Zhang, K.; Nourbakhsh, S.; Sah, P.; Fitzpatrick, M.C.; Galvani, A.P. Evaluation of COVID-19 vaccination strategies with a delayed second dose. PLoS Biol. 2021, 19, e3001211. [Google Scholar] [PubMed]
- Henry, D.A.; Jones, M.A.; Stehlik, P.; Glasziou, P.P. Effectiveness of COVID-19 vaccines: Findings from real world studies. Med. J. Aust. 2021, 215, 149–151.e1. [Google Scholar]
- Al-Abri, S.S.; Al-Rawahi, B.; Abdelhady, D.; Al-Abaidani, I. Effective vaccine management and Oman’s healthcare system’s challenge to maintain high global standards. J. Infect. Public Health 2018, 11, 742–744. [Google Scholar] [CrossRef]
- Al Wahaibi, A.; Al Rawahi, B.; Patel, P.K.; Al Khalili, S.; Al Maani, A.; Al-Abri, S. COVID-19 disease severity and mortality determinants: A large population-based analysis in Oman. Travel Med. Infect. Dis. 2021, 39, 101923. [Google Scholar] [CrossRef]
- Medical Xpress. Oman Launches COVID-19 Vaccination Campaign. 2020. Available online: https://medicalxpress.com/news/2020-12-oman-covid-vaccination-campaign.html#google_vignette (accessed on 25 June 2025).
- Al Khalili, S.; Al Maani, A.; Al Wahaibi, A.; Al Yaquobi, F.; Al-Jardani, A.; Al Harthi, K.; Alqayoudhi, A.; Al Manji, A.; Al Rawahi, B.; Al-Abri, S. Challenges and Opportunities for Public Health Service in Oman from the COVID-19 Pandemic: Learning Lessons for a Better Future. Front. Public. Health 2021, 9, 770946. [Google Scholar] [CrossRef]
- Al Ghafri, T.; Al Ajmi, F.; Anwar, H.; Al Balushi, L.; Al Balushi, Z.; Al Fahdi, F.; Al Lawati, A.; Al Hashmi, S.; Al Ghamari, A.; Al Harthi, M.; et al. The Experiences and Perceptions of Health-Care Workers During the COVID-19 Pandemic in Muscat, Oman: A Qualitative Study. J. Prim. Care Community Health 2020, 11, 2150132720967514. [Google Scholar] [CrossRef]
- Al Lamki, S.; Aal Jumaa, I.; Al Ghafri, M.; Al Abri, Z.; World Health Organization 2024. Oman: A Primary Health Care Case Study in the Context of the COVID-19 Pandemic. Available online: https://iris.who.int/bitstream/handle/10665/376136/9789240088603-eng.pdf?sequence=1 (accessed on 25 July 2025).
- Al Rawahi, B.; Al Wahaibi, A.; Al Khalili, S.; Al Balushi, A.Y.M.; Al-Shehi, N.; Al Harthi, K.; Al-Abri, S. The impact of the acceleration of COVID-19 vaccine deployment in two border regions in Oman. IJID Reg. 2022, 3, 265–267. [Google Scholar] [CrossRef]
- Reuters research. Reuters COVID-19 Tracker 2022. COVID-19 Tracker. Available online: https://www.reuters.com/world-coronavirus-tracker-and-maps/graphics/world-coronavirus-tracker-and-maps/countries-and-territories/oman/ (accessed on 22 May 2025).
- National Centre for Statestics and Information. Ecensus Portal. 2025. Available online: https://portal.ecensus.gov.om/web/ (accessed on 13 September 2025).
- Chen, S.; Guo, L.; Xie, Y.; Dong, D.; Saber, R.; Alluhidan, M.; Alamri, A.; Alfaisal, A.; Alazemi, N.; Al-Farsi, Y.M.; et al. Government responses to the COVID-19 pandemic of the Gulf Cooperation Council countries: Good practices and lessons for future preparedness. Glob. Health Res. Policy 2024, 9, 10. [Google Scholar] [CrossRef] [PubMed]
- Naik, S.; Vr, S.; Mohakud, S.; Tripathy, T. Analysis of COVID-19 Vaccine Adverse Drug Reactions Reported Among Sultan Qaboos University Hospital Staff. Sultan Qaboos Univ. Med. J. 2024, 24, 216–220. [Google Scholar] [CrossRef]
- Sannathimmappa, M.B.; Nambiar, V.; Aravindakshan, R.; Baig, M.F.; Hassan, A.K.; Al-Balushi, M.S.M. Effectiveness and Adverse Effects of Astrazeneca and Pfizer COVID-19 Vaccines Among Medical Students in Oman: A Comparative Study. Biomed. Biotechnol. Res. J. (BBRJ) 2023, 7, 101–105. [Google Scholar] [CrossRef]
- Statista. Vaccines Administrated in the Gulf Cooperation Council Countries in February 2021, by Country. 2021. Available online: https://www.statista.com/statistics/1257344/gcc-vaccines-administered-by-country/#statisticContainer (accessed on 22 May 2025).
- Althobaity, Y.; Wu, J.; Tildesley, M.J. Non-pharmaceutical interventions and their relevance in the COVID-19 vaccine rollout in Saudi Arabia and Arab Gulf countries. Infect. Dis. Model. 2022, 7, 545–560. [Google Scholar] [CrossRef]
- Al Wahaibi, A.; Al-Maani, A.; Alyaquobi, F.; Al Harthy, K.; Al-Jardani, A.; Al Rawahi, B.; Al-Abri, S. Effects of COVID-19 on mortality: A 5-year population-based study in Oman. Int. J. Infect. Dis. 2021, 104, 102–107. [Google Scholar] [CrossRef]
- Khamis, F.; Al Rashidi, B.; Al-Zakwani, I.; Al Wahaibi, A.H.; Al Awaidy, S.T. Epidemiology of COVID-19 Infection in Oman: Analysis of the First 1304 Cases. Oman Med. J. 2020, 35, e145. [Google Scholar] [CrossRef] [PubMed]
- Mansour, S.; Alahmadi, M.; Mahmoud, A.; Al-Shamli, K.; Alhabsi, M.; Ali, W. Geospatial modelling of COVID-19 mortality in Oman using geographically weighted Poisson regression GWPR. Sci. Rep. 2025, 15, 8138. [Google Scholar] [CrossRef]
- Alsalloum, M.A.; Garwan, Y.M.; Jose, J.; Thabit, A.K.; Baghdady, N. COVID-19 vaccine hesitancy and acceptance among the public in the Gulf Cooperation Council countries: A review of the literature. Hum. Vaccines Immunother. 2022, 18, 2091898. [Google Scholar] [CrossRef] [PubMed]
- Algabbani, A.; AlOmeir, O.; Algabbani, F. Vaccine hesitancy in the Gulf Cooperation Council countries. East. Mediterr. Health J. 2023, 29, 402–411. [Google Scholar] [CrossRef]
- Teerawattananon, Y.; Anothaisintawee, T.; Pheerapanyawaranun, C.; Botwright, S.; Akksilp, K.; Sirichumroonwit, N.; Budtarad, N.; Isaranuwatchai, W. A systematic review of methodological approaches for evaluating real-world effectiveness of COVID-19 vaccines: Advising resource-constrained settings. PLoS ONE 2022, 17, e0261930. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, S.A.; Callaway, D.; Resnick-Ault, D.; Mandavia, S.; Martinez, R.; Bass, M.; Goralnick, E. Critical Concepts for COVID-19 Mass Vaccination Site Operations. Disaster Med. Public. Health Prep. 2023, 17, e60. [Google Scholar] [CrossRef]
- World Health Organization. World Health Organization 2007. Everybody’s Business: Strengthening Health Systems to Improve Health Outcomes-WHO’s Framework for Action. Available online: https://www.who.int/publications/i/item/everybody-s-business----strengthening-health-systems-to-improve-health-outcomes (accessed on 22 May 2025).
- Frenk, J. The Global Health System: Strengthening National Health Systems as the Next Step for Global Progress. PLoS Med. 2010, 7, e1000089. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. World Health Organization 2020. Monitoring the Building Blocks of Health Systems: A Handbook of Indicators and Their Measurement StrategiesMonitoring the Building Blocks of Health Systems: A Handbook of Indicators and Their Measurement Strategies. Available online: https://iris.who.int/bitstream/handle/10665/258734/9789241564052-eng.pdf (accessed on 25 July 2025).
- Al Ghafri, T.S.; Al Balushi, L.; Al Balushi, Z.; Al Hinai, F.; Al Hasani, S.; Anwar, H.; Al Lawati, M.; Al Harthi, S. Reporting at Least One Adverse Effect Post-COVID-19 Vaccination from Primary Health Care in Muscat. Cureus 2021, 13, e17055. Available online: https://www.cureus.com/articles/61637-reporting-at-least-one-adverse-effect-post-covid-19-vaccination-from-primary-health-care-in-muscat (accessed on 22 May 2025). [CrossRef]
- Al Hasani, S.; Al Ghafri, T.; Al Lawati, H.; Mohammed, J.; Al Mukhainai, A.; Al Ajmi, F.; Anwar, H. The Use of Telephone Consultation in Primary Health Care During COVID-19 Pandemic, Oman: Perceptions from Physicians. J. Prim. Care Community Health 2020, 11, 2150132720976480. [Google Scholar] [CrossRef] [PubMed]
- Hasan, T.; Beardsley, J.; Marais, B.J.; Nguyen, T.A.; Fox, G.J. The Implementation of Mass-Vaccination against SARS-CoV-2: A Systematic Review of Existing Strategies and Guidelines. Vaccines 2021, 9, 326. [Google Scholar] [CrossRef]
- Roser, M. What Is the COVID-19 Stringency Index? 2021. Available online: https://ourworldindata.org/metrics-explained-covid19-stringency-index (accessed on 11 September 2025).
- World Health Organization. WHO Collaboration in Oman’s Response to COVID-19. 2025. Available online: https://www.emro.who.int/omn/oman-news/who-collaboration-on-omans-response-to-covid-19.html (accessed on 25 July 2025).
- Badr Al Samaa Group of Hospitals & Medical Centres. Badr Al Samaa Completes COVID-19 Vaccination Drive at National Museum. 2021. Available online: https://al-khoud.badralsamaahospitals.com/news-and-event/67/badr-al-samaa-completes-covid-19-vaccination-drive-at-national-museum?page=9 (accessed on 25 July 2025).
- The Arabian Stories. COVID-19 Vaccine: Private Sector Firms in Oman Encourage Staff to Get Jab. 2021. Available online: https://www.thearabianstories.com/2021/05/18/covid-19-vaccine-private-sector-firms-in-oman-encourage-staff-to-get-jab/ (accessed on 25 July 2025).
- Arabnews. Oman Vaccinates Almost 2 Million People Against COVID-19. 2021. Available online: https://www.arabnews.com/node/1900826/middle-east (accessed on 25 July 2025).
- OERLive. Occidental Oman Contributes $2.5 Million Towards COVID Vaccine Procurement. 2021. Available online: https://oerlive.com/news/occidental-oman-contributes-2-5-million-towards-covid-vaccine-procurement/ (accessed on 25 July 2025).
- Observer Oman Daily. Oman LNG Earmarks RO6 Million for COVID-19, Job Security. 2020. Available online: https://www.omanobserver.om/article/14165/Business/oman-lng-earmarks-ro-6m-for-covid-19-job-security (accessed on 25 July 2025).
- Observer Oman Daily. OCCI Donates RO 2 Million for Job Fund, COVID-19. 2020. Available online: https://www.omanobserver.om/article/14399/Local/occi-donates-ro-2-million-for-job-fund-covid-19 (accessed on 25 July 2025).
- Al Awaidy, S.T.; Khatiwada, M.; Castillo, S.; Al Siyabi, H.; Al Siyabi, A.; Al Mukhaini, S.; Dochez, C. Knowledge, Attitude, and Acceptability of COVID-19 Vaccine in Oman: A Cross-sectional Study. Oman Med. J. 2022, 37, e380. [Google Scholar] [CrossRef]
- Al Awaidy, S.; Khamis, F.; Al Ghafri, T.; Badahdah, A. Support for Mandatory COVID-19 Vaccines for 5- to 11-Year-Old Children: Cross-sectional study of Omani mothers. Sultan Qaboos Univ. Med. J. 2024, 24, 229–234. [Google Scholar]
- Samhouri, D.; Aynsley, T.R.; Hanna, P.; Frost, M.; Houssiere, V. Risk communication and community engagement capacity in the Eastern Mediterranean Region: A call for action. BMJ Glob. Health 2024, 7 (Suppl. S3), e008652. [Google Scholar] [CrossRef]
- Al Manji, A.; Tahoun, M.; Amabo, F.C.; Alabri, M.; Mahmoud, L.; Al Abri, B.; Aboushady, A.T.; Jabbour, J.; Nabeth, P.; Sadek, M. Contact tracing in the context of COVID-19: A case study from Oman. BMJ Glob. Health 2022, 7 (Suppl. S3), e008724. [Google Scholar] [CrossRef] [PubMed]
- Al Siyabi, H.; Al Mukhaini, S.; Kanaan, M.; Al Hatmi, S.; Al Anqoudi, Z.; Al Kalbani, A.; Al Bahri, Z.; Wannous, C.; Al Awaidy, S.T. Community Participation Approaches for Effective National COVID-19 Pandemic Preparedness and Response: An Experience From Oman. Front. Public. Health 2021, 8, 616763. [Google Scholar] [CrossRef]
- Khamis, F.; Al Mahyijari, N.; Al Lawati, F.; Badahdah, A.M. The Mental Health of Female Physicians and Nurses in Oman during the COVID-19 Pandemic. Oman Med. J. 2020, 35, e203. [Google Scholar] [CrossRef]
- Large Turnout as Mass Vaccination Gets Underway at OCEC. Vaccination Campaign at OCEC. 2021. Available online: https://timesofoman.com/article/103010-large-turnout-as-mass-vaccination-gets-underway-at-ocec (accessed on 22 May 2025).
- Mughal, F.; Khunti, K.; Mallen, C.D. The impact of COVID-19 on primary care: Insights from the National Health Service (NHS) and future recommendations. J. Fam. Med. Prim. Care 2021, 10, 4345–4349. [Google Scholar]
- Said, E.A.; Al-Rubkhi, A.; Jaju, S.; Koh, C.Y.; Al-Balushi, M.S.; Al-Naamani, K.; Al-Sinani, S.; Al-Busaidi, J.Z.; Al-Jabri, A.A. Association of the Magnitude of Anti-SARS-CoV-2 Vaccine Side Effects with Sex, Allergy History, Chronic Diseases, Medication Intake, and SARS-CoV-2 Infection. Vaccines 2024, 12, 104. [Google Scholar] [CrossRef] [PubMed]
- Jose, J.; Rubaie, M.H.A.; Ramimy, H.A.; Varughese, S.S. Pharmacovigilance. Sultan Qaboos Univ. Med. J. 2021, 21, e161–e163. [Google Scholar] [CrossRef] [PubMed]
- Rudolph, A.; Mitchell, J.; Barrett, J.; Sköld, H.; Taavola, H.; Erlanson, N.; Melgarejo-González, C.; Yue, Q.-Y. Global safety monitoring of COVID-19 vaccines: How pharmacovigilance rose to the challenge. Ther. Adv. Drug Saf. 2022, 13, 20420986221118972. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Framework for Decision-Making: Implementation of Mass Vaccination Campaigns in the Context of COVD-19. 2020. Available online: https://iris.who.int/bitstream/handle/10665/332159/WHO-2019-nCoV-Framework_Mass_Vaccination-2020.1-eng.pdf (accessed on 15 August 2025).
- Helldén, D.; Tesfaye, S.; Gachen, C.; Lindstrand, A.; Källander, K. Digital health funding for COVID-19 vaccine deployment across four major donor agencies. Lancet Digit. Health 2023, 5, e627–e631. [Google Scholar] [CrossRef] [PubMed]
- Saxenian, H.; Alkenbrack, S.; Attaran, M.F.; Barcarolo, J.; Brenzel, L.; Brooks, A.; Ekeman, E.; Griffiths, U.; Rozario, S.; Maele, N.V.; et al. Sustainable financing for Immunization Agenda 2030. Vaccine 2024, 42, S73–S81. [Google Scholar] [CrossRef]
| WHO Building Block | Strengths | Challenges | Lessons Learned |
|---|---|---|---|
| 1. Leadership and Governance |
|
|
|
| 2. Service Delivery |
|
|
|
| 3. Health Workforce |
|
|
|
| 4. Health Information Systems |
|
|
|
| 5. Access to Essential Medicines (Vaccines and Supplies) |
|
|
|
| 6. Financing |
|
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al Ghafri, T.; Al Balushi, L.; Al Balushi, Z.; Al Kiyumi, L.; Bait Ishaq, A.; Al Harthi, J. The Experience of an Accelerated COVID-19 Immunization Campaign in Oman: A Review Within the WHO Health System Building Blocks Framework. Vaccines 2025, 13, 1002. https://doi.org/10.3390/vaccines13101002
Al Ghafri T, Al Balushi L, Al Balushi Z, Al Kiyumi L, Bait Ishaq A, Al Harthi J. The Experience of an Accelerated COVID-19 Immunization Campaign in Oman: A Review Within the WHO Health System Building Blocks Framework. Vaccines. 2025; 13(10):1002. https://doi.org/10.3390/vaccines13101002
Chicago/Turabian StyleAl Ghafri, Thamra, Lamya Al Balushi, Zainab Al Balushi, Lamees Al Kiyumi, Asma Bait Ishaq, and Jannat Al Harthi. 2025. "The Experience of an Accelerated COVID-19 Immunization Campaign in Oman: A Review Within the WHO Health System Building Blocks Framework" Vaccines 13, no. 10: 1002. https://doi.org/10.3390/vaccines13101002
APA StyleAl Ghafri, T., Al Balushi, L., Al Balushi, Z., Al Kiyumi, L., Bait Ishaq, A., & Al Harthi, J. (2025). The Experience of an Accelerated COVID-19 Immunization Campaign in Oman: A Review Within the WHO Health System Building Blocks Framework. Vaccines, 13(10), 1002. https://doi.org/10.3390/vaccines13101002






