Attitudes Toward General Vaccination Mediate the Association Between Influenza Vaccination History and Pneumococcal Vaccination Intention Among Older Adults in China
Abstract
1. Introduction
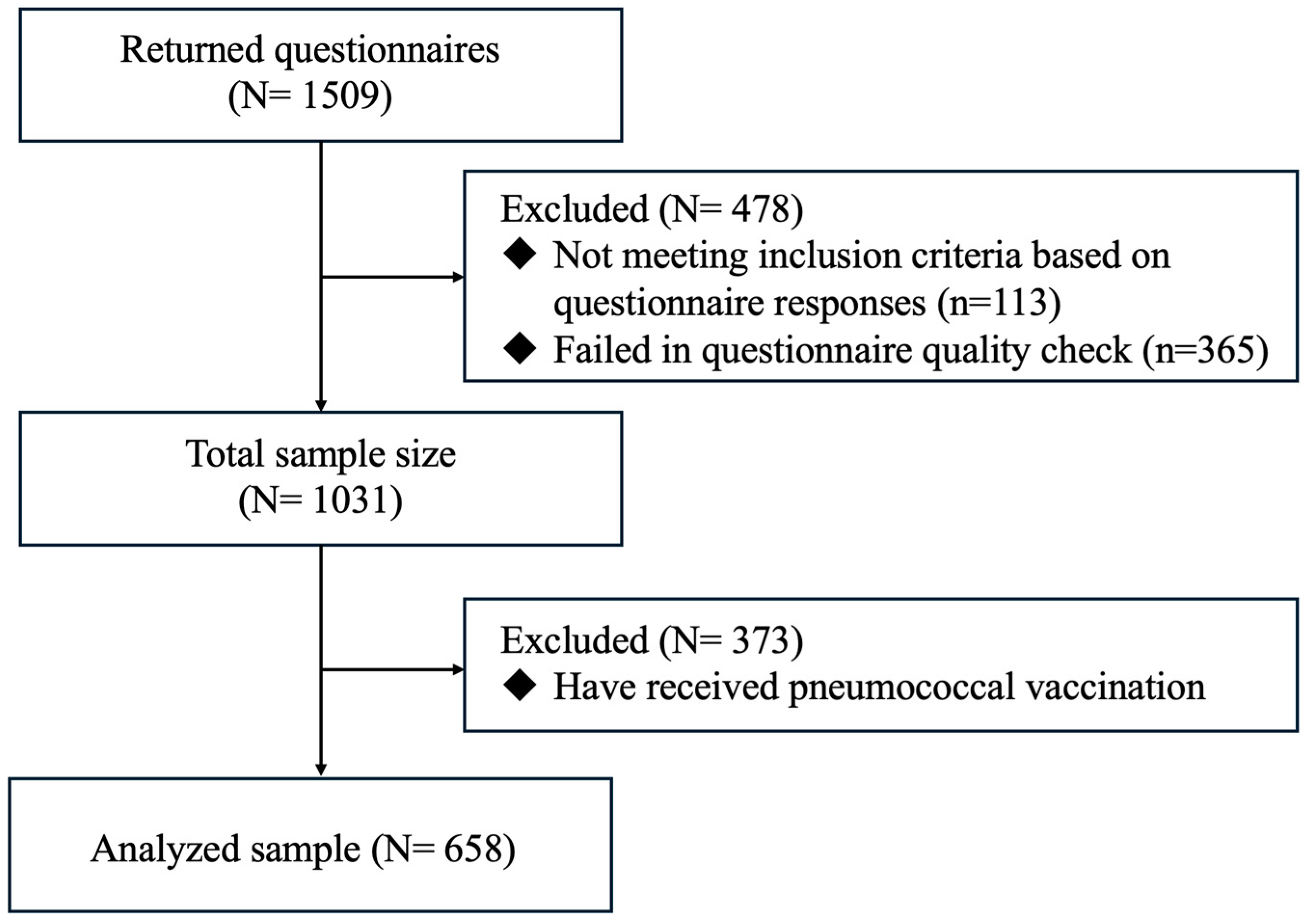
2. Methods
2.1. Study Design
2.2. Sample Size Planning
2.3. Participant Recruitment
2.4. Data Collection
2.5. Measures
2.5.1. Influenza Vaccination History (Independent Variable)
2.5.2. Negative Attitudes Toward General Vaccination (Mediators)
2.5.3. Pneumococcal Vaccination Intention (Dependent Variable)
2.5.4. Background Information
2.6. Statistical Analysis
3. Results
3.1. Background Information, Vaccination-Related Behavior, Intention, and Perceptions
3.2. Factors Associated with Pneumococcal Vaccination Intention
3.3. Spearman Correlations of the Main Studied Variables
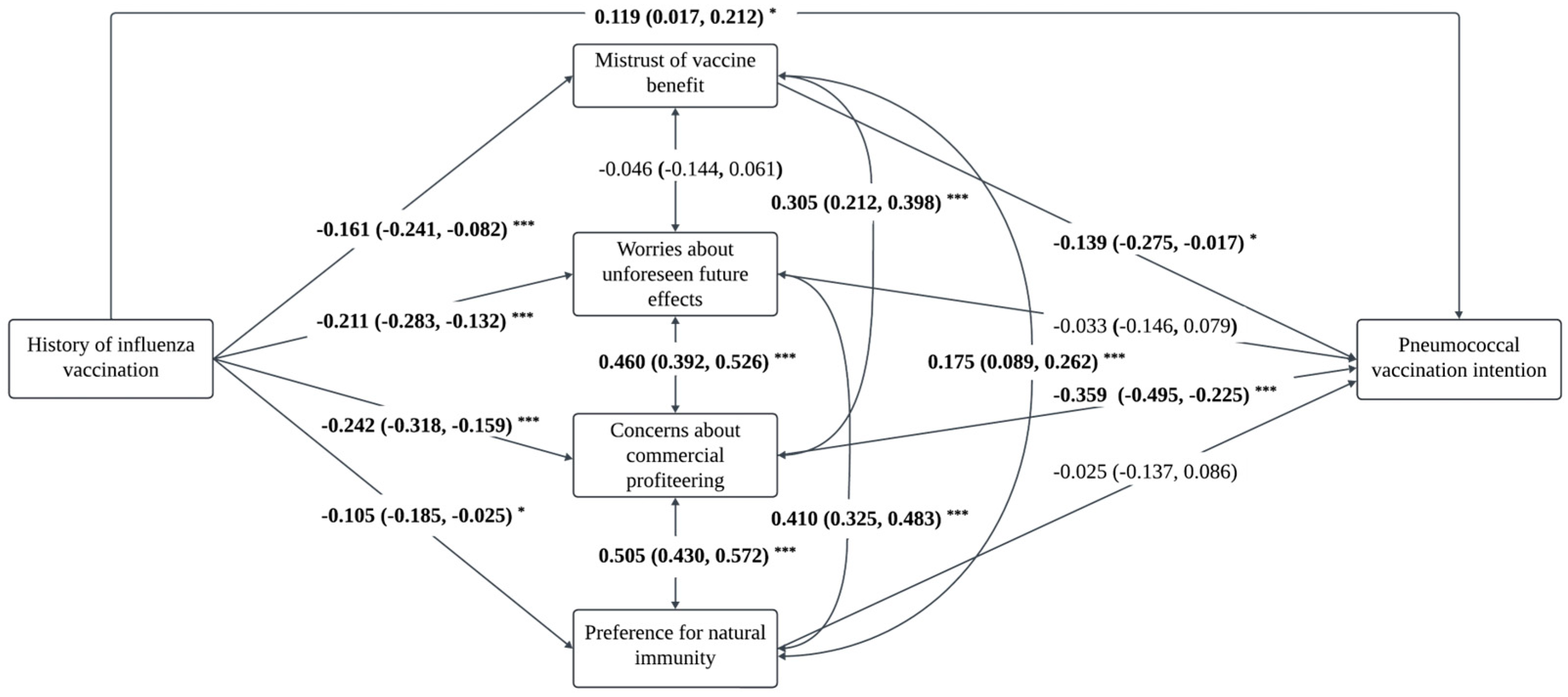
3.4. Mediations Between the History of Influenza Vaccination and Pneumococcal Vaccination Intention
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chen, X.; Giles, J.; Yao, Y.; Yip, W.; Meng, Q.; Berkman, L.; Chen, H.; Chen, X.; Feng, J.; Feng, Z.; et al. The path to healthy ageing in China: A Peking University–Lancet Commission. Lancet 2022, 400, 1967–2006. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Aging and health. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 16 September 2024).
- World Health Organization. Ageing and health in China. 2024. Available online: https://www.who.int/china/health-topics/ageing (accessed on 16 September 2024).
- The People’s Republic of China. China to Ramp up Elderly Care Services to Address Population Aging: Minister. 2024. Available online: https://english.www.gov.cn/news/202408/01/content_WS66aac459c6d0868f4e8e9a36.html (accessed on 16 September 2024).
- Chen, C.; Ding, S.; Wang, J. Digital health for aging populations. Nat. Med. 2023, 29, 1623–1630. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.; Wang, L.; Xie, M.; Li, X. Recommendations for Influenza, Streptococcus pneumoniae Vaccination in Elderly People in China Writing Group, Geriatric Respiratory Group and Chinese Society of Geriatrics. Recommendations for influenza and Streptococcus pneumoniae vaccination in elderly people in China. Aging Med. 2020, 3, 4–14. [Google Scholar]
- Beran, J.; Reynales, H.; Poder, A.; Yu, C.Y.; Pitisuttithum, P.; Yuan, L.L.; Vermeulen, W.; Verhoeven, C.; Leav, B.; Zhang, B.; et al. Prevention of influenza during mismatched seasons in older adults with an MF59-adjuvanted quadrivalent influenza vaccine: A randomised, controlled, multicentre, phase 3 efficacy study. Lancet Infect. Dis. 2021, 21, 1027–1037. [Google Scholar] [CrossRef]
- Sikjær, M.G.; Pedersen, A.A.; Wik, M.S.; Stensholt, S.S.; Hilberg, O.; Løkke, A. Vaccine effectiveness of the pneumococcal polysaccharide and conjugated vaccines in elderly and high-risk populations in preventing invasive pneumococcal disease: A systematic search and meta-analysis. Eur. Clin. Respir. J. 2023, 10, 2168354. [Google Scholar] [CrossRef]
- Jiang, Y.; Ye, Z.; Chen, D.; Shu, Y. Dual influenza and pneumococcal vaccination was associated with lower short-term risks of all-cause and acute respiratory hospitalizations among the elderly in Shenzhen, China: A retrospective cohort study. Emerg. Microbes Infect. 2020, 9, 2578–2587. [Google Scholar] [CrossRef] [PubMed]
- Lu, X.; Lu, J.; Zhang, L.; Mei, K.; Guan, B.; Lu, Y. Gap between willingness and behavior in the vaccination against influenza, pneumonia, and herpes zoster among Chinese aged 50–69 years. Expert Rev. Vaccines 2021, 20, 1147–1152. [Google Scholar] [CrossRef] [PubMed]
- Hou, Z.; Guo, J.; Lai, X.; Zhang, H.; Wang, J.; Hu, S.; Du, F.; Francis, M.R.; Fang, H. Influenza vaccination hesitancy and its determinants among elderly in China: A national cross-sectional study. Vaccine 2022, 40, 4806–4815. [Google Scholar] [CrossRef] [PubMed]
- Simione, L.; Vagni, M.; Maiorano, T.; Giostra, V.; Pajardi, D. How Implicit Attitudes toward Vaccination Affect Vaccine Hesitancy and Behaviour: Developing and Validating the V-IRAP. Int. J. Environ. Res. Public Health 2022, 19, 4205. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Zhang, Z.; Chen, X.; Wang, C.; Teng, C.; Wang, L.; Song, Y.; Shen, J.; Liu, L.; Pei, Y. Willingness and influencing factors to be vaccinated against herpes zoster and pneumococcus of people aged 50 years and over in Xicheng District parks, Beijing. Aging Res. 2024, 2, 9340027. [Google Scholar] [CrossRef]
- Yunhua, B.; Peng, B.; Shuping, L.; Zheng, Z. A narrative review on vaccination rate and factors associated with the willingness to receive pneumococcal vaccine in Chinese adult population. Hum. Vaccines Immunother. 2022, 18, 2139123. [Google Scholar] [CrossRef] [PubMed]
- Nicholls, L.A.B.; Gallant, A.J.; Cogan, N.; Rasmussen, S.; Young, D.; Williams, L. Older adults’ vaccine hesitancy: Psychosocial factors associated with influenza, pneumococcal, and shingles vaccine uptake. Vaccine 2021, 39, 3520–3527. [Google Scholar] [CrossRef]
- Henn, L.; Otto, S.; Kaiser, F.G. Positive spillover: The result of attitude change. J. Environ. Psychol. 2020, 69, 101429. [Google Scholar] [CrossRef]
- Nash, N.; Whitmarsh, L.; Capstick, S.; Hargreaves, T.; Poortinga, W.; Thomas, G.; Sautkina, E.; Xenias, D. Climate-relevant behavioral spillover and the potential contribution of social practice theory. Wiley Interdiscip. Rev. Clim. Change 2017, 8, e481. [Google Scholar] [CrossRef]
- Defra, A. Framework for Pro-Environmental Behaviours; Department for Environment, Food and Rural Affairs: London, UK, 2008.
- Deb, A.; Podmore, B.; Barnett, R.; Beier, D.; Galetzka, W.; Qizilbash, N.; Haeckl, D.; Boellinger, T.; Johnson, K.D.; Weiss, T. Pneumococcal vaccination coverage in individuals (16–59 years) with a newly diagnosed risk condition in Germany. BMC Infect. Dis. 2022, 22, 753. [Google Scholar] [CrossRef]
- Trent, M.J.; Salmon, D.A.; MacIntyre, C.R. Predictors of pneumococcal vaccination among Australian adults at high risk of pneumococcal disease. Vaccine 2022, 40, 1152–1161. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Dunham, L.S.; Johnson, K.D. Regional factors associated with pneumococcal vaccination coverage among US adults with underlying chronic or immunocompromising conditions. Hum. Vaccines Immunother. 2023, 19, 2194779. [Google Scholar] [CrossRef] [PubMed]
- Thomas, K.; Lazarini, A.; Kaltsonoudis, E.; Voulgari, P.V.; Drosos, A.A.; Repa, A.; Sali, A.M.I.; Sidiropoulos, P.; Tsatsani, P.; Gazi, S.; et al. Patterns and factors associated with pneumococcal vaccination in a prospective cohort of 1697 patients with rheumatoid arthritis. Front. Med. 2023, 9, 1039464. [Google Scholar] [CrossRef] [PubMed]
- Gilmour, H. Factors associated with shingles and pneumococcal vaccination among older Canadians. Health Rep. 2024, 35, 14–24. [Google Scholar] [PubMed]
- Zakhour, R.; Tamim, H.; Faytrouni, F.; Khoury, J.; Makki, M.; Charafeddine, L. Knowledge, attitude and practice of influenza vaccination among Lebanese parents: A cross-sectional survey from a developing country. PLoS ONE 2021, 16, e0258258. [Google Scholar] [CrossRef] [PubMed]
- Trujillo, K.L.; Green, J.; Safarpour, A.; Lazer, D.; Lin, J.; Motta, M. COVID-19 spillover effects onto general vaccine attitudes. Public Opin. Q. 2024, 88, 97–122. [Google Scholar] [CrossRef]
- Zhang, V.; Zhu, P.; Wagner, A.L. Spillover of vaccine hesitancy into adult COVID-19 and influenza: The role of race, religion, and political affiliation in the United States. Int. J. Environ. Res. Public Health 2023, 20, 3376. [Google Scholar] [CrossRef] [PubMed]
- Peretti-Watel, P.; Raude, J.; Sagaon-Teyssier, L.; Constant, A.; Verger, P.; Beck, F. Attitudes toward vaccination and the H1N1 vaccine: Poor people’s unfounded fears or legitimate concerns of the elite? Soc. Sci. Med. 2014, 109, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Municipal Bureau of Statistics. China Statistical Yearbook. 2023. Available online: https://www.stats.gov.cn/sj/ndsj/2023/indexeh.htm (accessed on 26 September 2024).
- Martin, L.R.; Petrie, K.J. Understanding the dimensions of anti-vaccination attitudes: The vaccination attitudes examination (VAX) scale. Ann. Behav. Med. 2017, 51, 652–660. [Google Scholar] [CrossRef]
- Ye, X.; Lee, H.-H.; Hui, K.-H.; Xin, M.; Mo, P.K.H. Effects of negative attitudes towards vaccination in general and trust in government on uptake of a booster dose of COVID-19 vaccine and the moderating role of psychological reactance: An observational prospective cohort study in Hong Kong. Vaccines 2023, 11, 393. [Google Scholar] [CrossRef]
- Bhatnagar, R.; Kim, J.; Many, J.E. Candidate surveys on program evaluation: Examining Instrument reliability, validity and program effectiveness. Am. J. Educ. Res. 2014, 2, 683–690. [Google Scholar] [CrossRef]
- Zhang, D.; Zhou, W.; Poon, P.K.-M.; Kwok, K.O.; Chui, T.W.-S.; Hung, P.H.Y.; Ting, B.Y.T.; Chan, D.C.-C.; Wong, S.Y.-S. Vaccine resistance and hesitancy among older adults who live alone or only with an older partner in community in the early stage of the fifth wave of COVID-19 in Hong Kong. Vaccines 2022, 10, 1118. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Ten Threats to Global Health in 2019. 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 16 September 2024).
- MacDonald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- Woolf, K.; Gogoi, M.; Martin, C.A.; Papineni, P.; Lagrata, S.; Nellums, L.B.; McManus, I.C.; Guyatt, A.L.; Melbourne, C.; Bryant, L.; et al. Healthcare workers’ views on mandatory SARS-CoV-2 vaccination in the UK: A cross-sectional, mixed-methods analysis from the UK-REACH study. EClinicalMedicine 2022, 46, 101346. [Google Scholar] [CrossRef]
- Huang, J.; Mak, F.-Y.; Wong, Y.-Y.; Ko, S.; Chong, M.K.C.; Wang, Z.; Hon, K.-L.; Wong, E.L.Y.; Yeoh, E.-K.; Wong, M.C.S. Enabling factors, barriers, and perceptions of pneumococcal vaccination strategy implementation: A qualitative study. Vaccines 2022, 10, 1164. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Guo, M.; Wang, Y.; Chen, R.; Wei, X. The relationship between influenza vaccine hesitancy and vaccine literacy among youth and adults in China. Front. Immunol. 2024, 15, 1444393. [Google Scholar] [CrossRef] [PubMed]
- Michel, J.-P.; Goldberg, J. Education, healthy ageing and vaccine literacy. J. Nutr. Health Aging 2021, 25, 698–701. [Google Scholar] [CrossRef] [PubMed]
- Reno, C.; Maietti, E.; Fantini, M.P.; Savoia, E.; Manzoli, L.; Montalti, M.; Gori, D. Enhancing COVID-19 vaccines acceptance: Results from a survey on vaccine hesitancy in Northern Italy. Vaccines 2021, 9, 378. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Fang, Y.; Ip, M.; Lau, M.; Lau, J.T. Facilitators and barriers to completing recommended doses of pneumococcal vaccination among community-living individuals aged ≥65 years in Hong Kong—A population-based study. Hum. Vaccines Immunother. 2021, 17, 527–536. [Google Scholar] [CrossRef] [PubMed]
- Siu, J.Y.-M.; Cao, Y.; Shum, D.H. Perceptions of and hesitancy toward COVID-19 vaccination in older Chinese adults in Hong Kong: A qualitative study. BMC Geriatr. 2022, 22, 288. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.; Yao, Y.; Wang, Y.; Gong, J.; Meng, Q.; Wang, H.; Wang, W.; Chen, X.; Zhao, Y. Determinants of COVID-19 vaccination status and hesitancy among older adults in China. Nat. Med. 2023, 29, 623–631. [Google Scholar] [CrossRef]
| Variables | n (%)/Median ± IQR | p-Value a | |||||
|---|---|---|---|---|---|---|---|
| Total (n = 658) | Province A (n = 175) | Province B (n = 81) | Province C (n = 128) | Province D (n = 84) | Province E (n = 190) | ||
| Background variables | |||||||
| Age (years), Median ± IQR | 65.0 ± 9.0 | 65.0 ± 11.0 | 63.0 ± 4.0 | 64.0 ± 6.0 | 64.0 ± 6.8 | 69.0 ± 11.0 | <0.001 |
| Gender | 0.061 | ||||||
| Male | 308 (46.8) | 70 (40.0) | 32 (39.5) | 62 (48.4) | 46 (54.8) | 98 (51.6) | |
| Female | 350 (53.2) | 105 (60.0) | 49 (60.5) | 66 (51.6) | 38 (45.2) | 92 (48.4) | |
| Education level | 0.004 | ||||||
| High school or below | 607 (92.2) | 157 (89.7) | 78 (96.3) | 112 (87.5) | 75 (89.3) | 185 (97.4) | |
| College and above | 51 (7.8) | 18 (10.3) | 3 (3.7) | 16 (12.5) | 9 (10.7) | 5 (2.6) | |
| Marital status | 0.054 | ||||||
| Married or living with a partner | 569 (86.5) | 151 (86.3) | 78 (96.3) | 112 (87.5) | 70 (83.3) | 158 (83.2) | |
| Unmarried/divorced/separated/widowed | 89 (13.5) | 24 (13.7) | 3 (3.7) | 16 (12.5) | 14 (16.7) | 32 (16.8) | |
| Employment status | <0.001 | ||||||
| Retired | 398 (60.5) | 75 (42.9) | 38 (46.9) | 85 (66.4) | 50 (59.5) | 150 (78.9) | |
| Unemployed | 224 (34.0) | 87 (49.7) | 42 (51.9) | 37 (28.9) | 30 (35.7) | 28 (14.7) | |
| Employed | 36 (5.5) | 13 (7.4) | 1 (1.2) | 6 (4.7) | 4 (4.8) | 12 (6.3) | |
| Monthly household income (CNY) | <0.001 | ||||||
| ≤3000 | 290 (44.1) | 103 (58.9) | 49 (60.5) | 58 (45.3) | 29 (34.5) | 51 (26.8) | |
| 3001–5000 | 193 (29.3) | 48 (27.4) | 15 (18.5) | 39 (30.5) | 23 (27.4) | 68 (35.8) | |
| >5000 | 175 (26.6) | 24 (13.7) | 17 (21.0) | 31 (24.2) | 32 (38.1) | 71 (37.4) | |
| Living alone b | 0.384 | ||||||
| Yes | 61 (9.3) | 22 (12.6) | 7 (8.6) | 10 (7.8) | 9 (10.7) | 13 (6.8) | |
| No | 597 (90.7) | 153 (87.4) | 74 (91.4) | 118 (92.2) | 75 (89.3) | 177 (93.2) | |
| Living with spouse | 493 (74.9) | 115 (65.7) | 66 (81.5) | 105 (82.0) | 59 (70.2) | 148 (77.9) | |
| Living with son/daughter | 216 (32.8) | 47 (26.9) | 19 (23.5) | 42 (32.8) | 25 (29.8) | 83 (43.7) | |
| Living with other family | 48 (7.3) | 19 (10.9) | 5 (6.2) | 7 (5.5) | 6 (7.1) | 11 (5.8) | |
| Medical insurance status | <0.001 | ||||||
| Yes | 558 (84.8) | 152 (86.9) | 75 (92.6) | 118 (92.2) | 75 (89.3) | 138 (72.6) | |
| No | 92 (14.0) | 20 (11.4) | 4 (4.9) | 9 (7.0) | 8 (9.5) | 51 (26.8) | |
| Unknown | 8 (1.2) | 3 (1.7) | 2 (2.5) | 1 (0.8) | 1 (1.2) | 1 (0.5) | |
| Chronic disease status | 0.006 | ||||||
| Yes | 517 (78.6) | 140 (80.0) | 64 (79.0) | 93 (72.7) | 57 (67.9) | 163 (85.8) | |
| One chronic disease | 273 (41.5) | 59 (33.7) | 44 (54.3) | 46 (35.9) | 25 (29.8) | 99 (52.1) | |
| Two or more chronic diseases | 244 (37.1) | 81 (46.3) | 20 (24.7) | 47 (36.7) | 32 (38.1) | 64 (33.7) | |
| No/unknown | 141 (21.4) | 35 (20.0) | 17 (21.0) | 35 (27.3) | 27 (32.1) | 27 (14.2) | |
| Vaccination-related behavior, intention, and perceptions | |||||||
| History of influenza vaccination c | <0.001 | ||||||
| Yes | 363 (55.2) | 79 (45.1) | 64 (79.0) | 44 (34.4) | 30 (35.7) | 146 (76.8) | |
| No | 295 (44.8) | 96 (54.9) | 17 (21.0) | 84 (65.6) | 54 (64.3) | 44 (23.2) | |
| Whether heard of pneumococcal vaccination | <0.001 | ||||||
| Yes | 220 (33.4) | 45 (25.7) | 36 (44.4) | 58 (45.3) | 37 (44.0) | 44 (23.2) | |
| No | 438 (66.6) | 130 (74.3) | 45 (55.6) | 70 (54.7) | 47 (56.0) | 146 (76.8) | |
| Pneumococcal vaccination intention | <0.001 | ||||||
| Very unlikely | 68 (10.3) | 13 (7.4) | 6 (7.4) | 17 (13.3) | 6 (7.1) | 26 (13.7) | |
| Unlikely | 111 (16.9) | 28 (16.0) | 7 (8.6) | 26 (20.3) | 9 (10.7) | 41 (21.6) | |
| Half and half | 295 (44.8) | 89 (50.9) | 25 (30.9) | 53 (41.4) | 44 (52.4) | 84 (44.2) | |
| Likely | 107 (16.3) | 35 (20.0) | 20 (24.7) | 15 (11.7) | 18 (21.4) | 19 (10.0) | |
| Very likely | 77 (11.7) | 10 (5.7) | 23 (28.4) | 17 (13.3) | 7 (8.3) | 20 (10.5) | |
| Negative attitudes toward general vaccination (range: 12–52), Median ± IQR | 28.5 ± 12.0 | 29.0 ± 10.0 | 24.0 ± 14.5 | 30.5 ± 9.0 | 31.5 ± 8.0 | 26.0 ± 11.3 | <0.001 |
| Mistrust of vaccine benefit (range: 3–15) | 6.0 ± 3.0 | 6.0 ± 3.0 | 3.0 ± 3.0 | 6.0 ± 3.0 | 6.0 ± 3.0 | 6.0 ± 3.0 | <0.001 |
| Worries about unforeseen future effects (range: 3–15) | 10.0 ± 4.0 | 10.0 ± 4.0 | 9.0 ± 3.0 | 10.5 ± 4.0 | 11.0 ± 2.8 | 8.0 ± 3.0 | <0.001 |
| Concerns about commercial profiteering (range: 3–15) | 6.0 ± 4.0 | 6.0 ± 4.0 | 4.0 ± 3.0 | 6.0 ± 5.0 | 6.0 ± 3.0 | 5.0 ± 3.0 | <0.001 |
| Preference for natural immunity (range: 3–11) | 7.5 ± 4.0 | 8.0 ± 3.0 | 6.0 ± 5.0 | 8.0 ± 5.8 | 9.0 ± 2.0 | 7.0 ± 4.0 | <0.001 |
| Variables | Pneumococcal Vaccination Intention | |
|---|---|---|
| OR (95%CI) a | AOR (95%CI) b | |
| Background variables | ||
| Age (years) | 0.972 (0.946, 0.999) * | 0.956 (0.924, 0.990) * |
| Gender | ||
| Male | Ref | Ref |
| Female | 1.542 (1.091, 2.181) * | 1.389 (0.938, 2.055) |
| Education level | ||
| High school or below | Ref | Ref |
| College and above | 0.872 (0.453, 1.678) | 1.322 (0.622, 2.810) |
| Marital status | ||
| Unmarried/divorced/separated/widowed | Ref | Ref |
| Married or living with a partner | 1.300 (0.771, 2.191) | 0.841 (0.421, 1.678) |
| Employment status | ||
| Unemployed | Ref | Ref |
| Employed/retired (with pension) | 1.109 (0.784, 1.569) | 1.215 (0.785, 1.882) |
| Monthly household income (CNY) | ||
| ≤3000 | Ref | Ref |
| >3000 | 0.675 (0.480, 0.950) * | 0.587 (0.388, 0.889) * |
| Living alone | ||
| No | Ref | Ref |
| Yes | 0.308 (0.137, 0.689) ** | 0.270 (0.103, 0.708) ** |
| Medical insurance | ||
| No/unknown | Ref | Ref |
| Yes | 1.059 (0.656, 1.708) | 1.393 (0.804, 2.414) |
| Chronic disease | ||
| No/unknown | Ref | Ref |
| Yes | 0.752 (0.503, 1.125) | 0.945 (0.589, 1.515) |
| Vaccination-related behavior and perceptions | ||
| History of influenza vaccination | ||
| No | Ref | Ref |
| Yes | 2.172 (1.517, 3.112) *** | 1.675 (1.110, 2.527) * |
| Negative attitudes toward general vaccination | ||
| Mistrust of vaccine benefit | 0.787 (0.720, 0.860) *** | 0.906 (0.828, 0.990) * |
| Worries about unforeseen future effects | 0.847 (0.791, 0.908) *** | 0.977 (0.895, 1.065) |
| Concerns about commercial profiteering | 0.673 (0.612, 0.741) *** | 0.715 (0.631, 0.809) *** |
| Preference for natural immunity | 0.814 (0.748, 0.887) *** | 0.967 (0.901, 1.039) |
| Variables | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| 1. History of influenza vaccination | - | ||||
| 2. Pneumococcal vaccination intention | 0.167 *** | - | |||
| 3. Mistrust of vaccine benefit | −0.210 *** | −0.253 *** | - | ||
| 4. Worries about unforeseen future effects | −0.236 *** | −0.180 *** | 0.131 *** | - | |
| 5. Concerns about commercial profiteering | −0.262 *** | −0.360 *** | 0.477 *** | 0.514 *** | - |
| 6. Preference for natural immunity | −0.118 ** | −0.212 *** | 0.305 *** | 0.433 *** | 0.519 *** |
| Paths | Standardized Estimate | 95% CI | % of the Total Effect |
|---|---|---|---|
| Outcome: pneumococcal vaccination intention | |||
| 1. Total effect | 0.238 | (0.138, 0.329) | \ |
| 2. Direct effect | 0.119 | (0.017, 0.212) | 50.0% |
| 3. Indirect effect | 0.119 | (0.077, 0.168) | 50.0% |
| (1) History of influenza vaccination → mistrust of vaccine benefit → outcome | 0.022 | (0.004, 0.054) | 9.2% |
| (2) History of influenza vaccination → worries about unforeseen future effects → outcome | 0.007 | (−0.017, 0.033) | 2.9% |
| (3) History of influenza vaccination → concerns about commercial profiteering → outcome | 0.087 | (0.049, 0.136) | 36.6% |
| (4) History of influenza vaccination → preference for natural immunity → outcome | 0.003 | (−0.008, 0.018) | 1.3% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, S.; Ruan, C.; Jiang, Y.; Song, Y.; Zhang, Y.; Qin, Z.; Shi, X.; Zhang, M.; Zhou, J.; Chen, D.; et al. Attitudes Toward General Vaccination Mediate the Association Between Influenza Vaccination History and Pneumococcal Vaccination Intention Among Older Adults in China. Vaccines 2025, 13, 20. https://doi.org/10.3390/vaccines13010020
Huang S, Ruan C, Jiang Y, Song Y, Zhang Y, Qin Z, Shi X, Zhang M, Zhou J, Chen D, et al. Attitudes Toward General Vaccination Mediate the Association Between Influenza Vaccination History and Pneumococcal Vaccination Intention Among Older Adults in China. Vaccines. 2025; 13(1):20. https://doi.org/10.3390/vaccines13010020
Chicago/Turabian StyleHuang, Siwen, Chi Ruan, Yan Jiang, Yudan Song, Yuhang Zhang, Zeying Qin, Xinyu Shi, Mengyue Zhang, Jingtao Zhou, Dingwan Chen, and et al. 2025. "Attitudes Toward General Vaccination Mediate the Association Between Influenza Vaccination History and Pneumococcal Vaccination Intention Among Older Adults in China" Vaccines 13, no. 1: 20. https://doi.org/10.3390/vaccines13010020
APA StyleHuang, S., Ruan, C., Jiang, Y., Song, Y., Zhang, Y., Qin, Z., Shi, X., Zhang, M., Zhou, J., Chen, D., Xiao, Y., Wang, L., Tian, L., Peng, R., Peng, Z., & Luo, S. (2025). Attitudes Toward General Vaccination Mediate the Association Between Influenza Vaccination History and Pneumococcal Vaccination Intention Among Older Adults in China. Vaccines, 13(1), 20. https://doi.org/10.3390/vaccines13010020






