Progress and Challenges in Measles and Rubella Elimination in the WHO European Region
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Measles
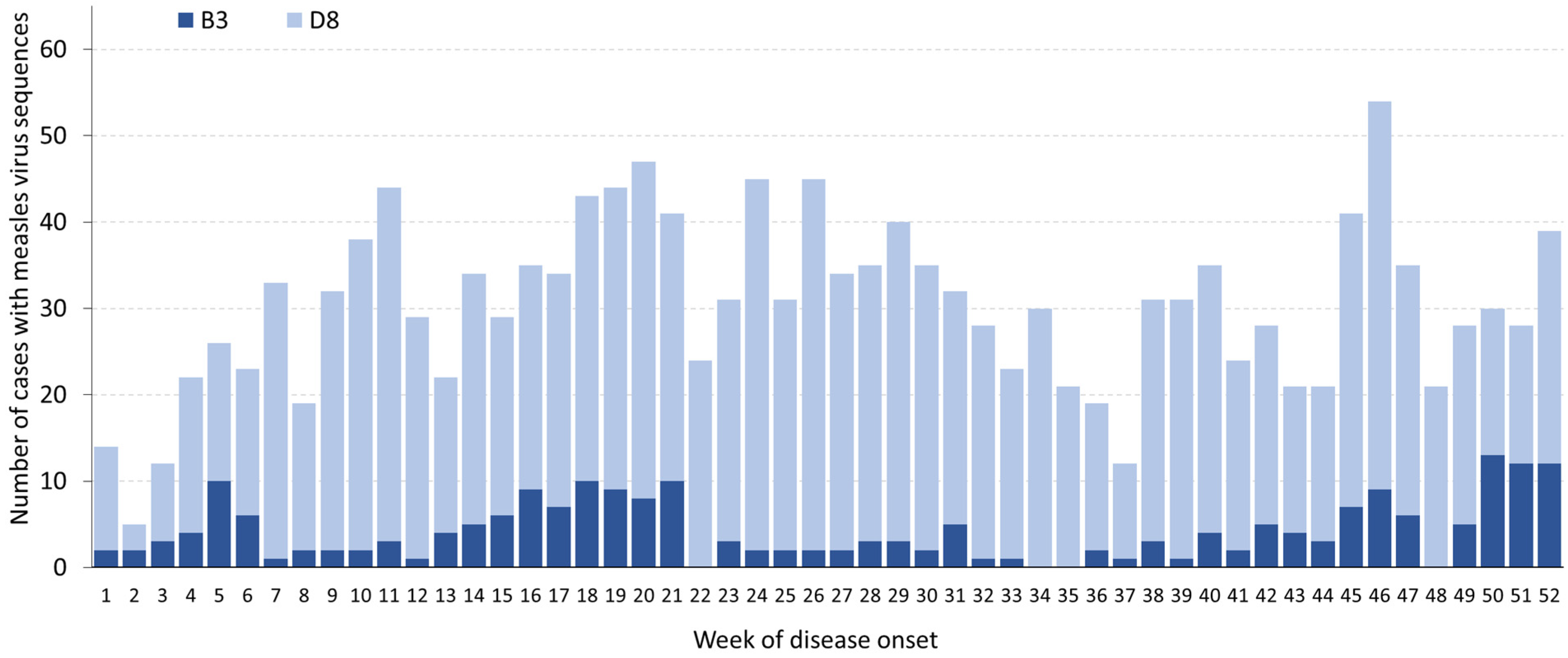
3.1.1. Incidence—Notifications and Laboratory Data
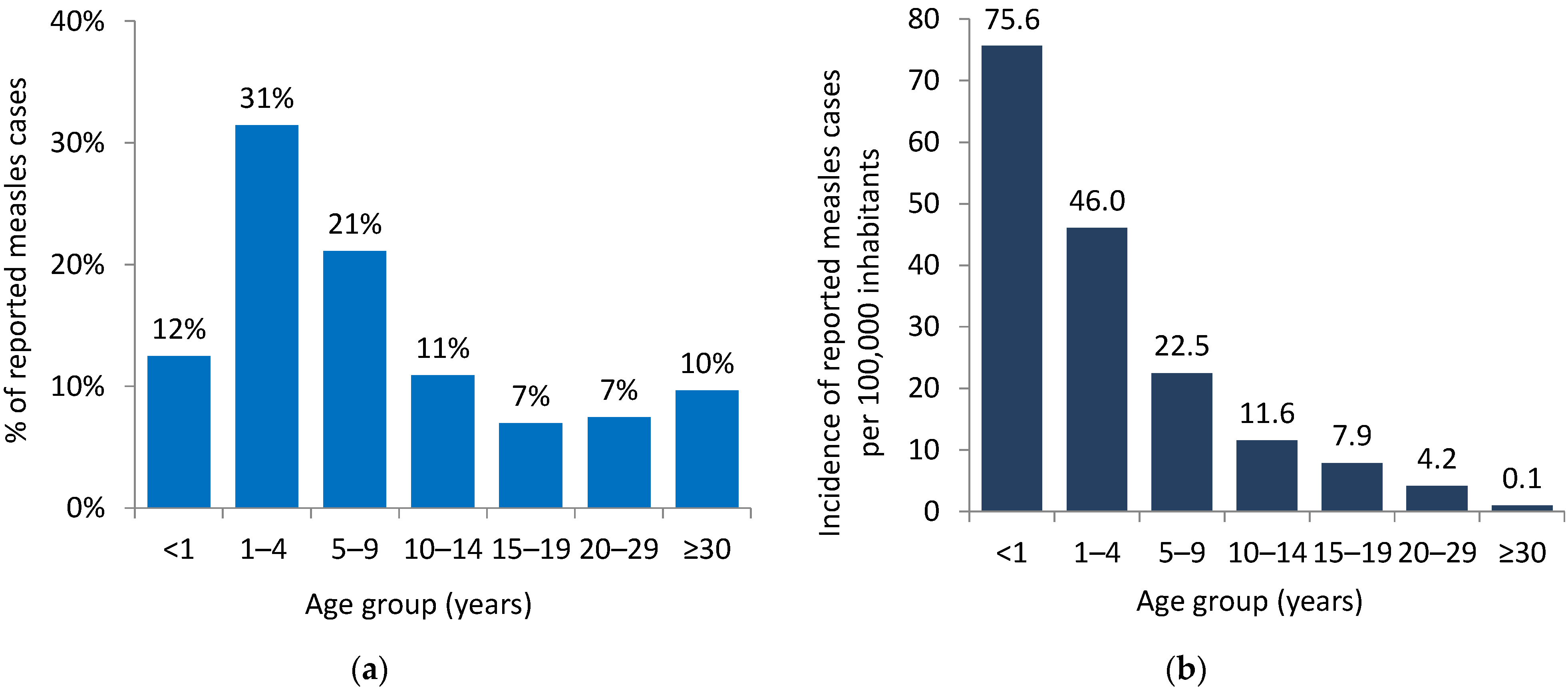
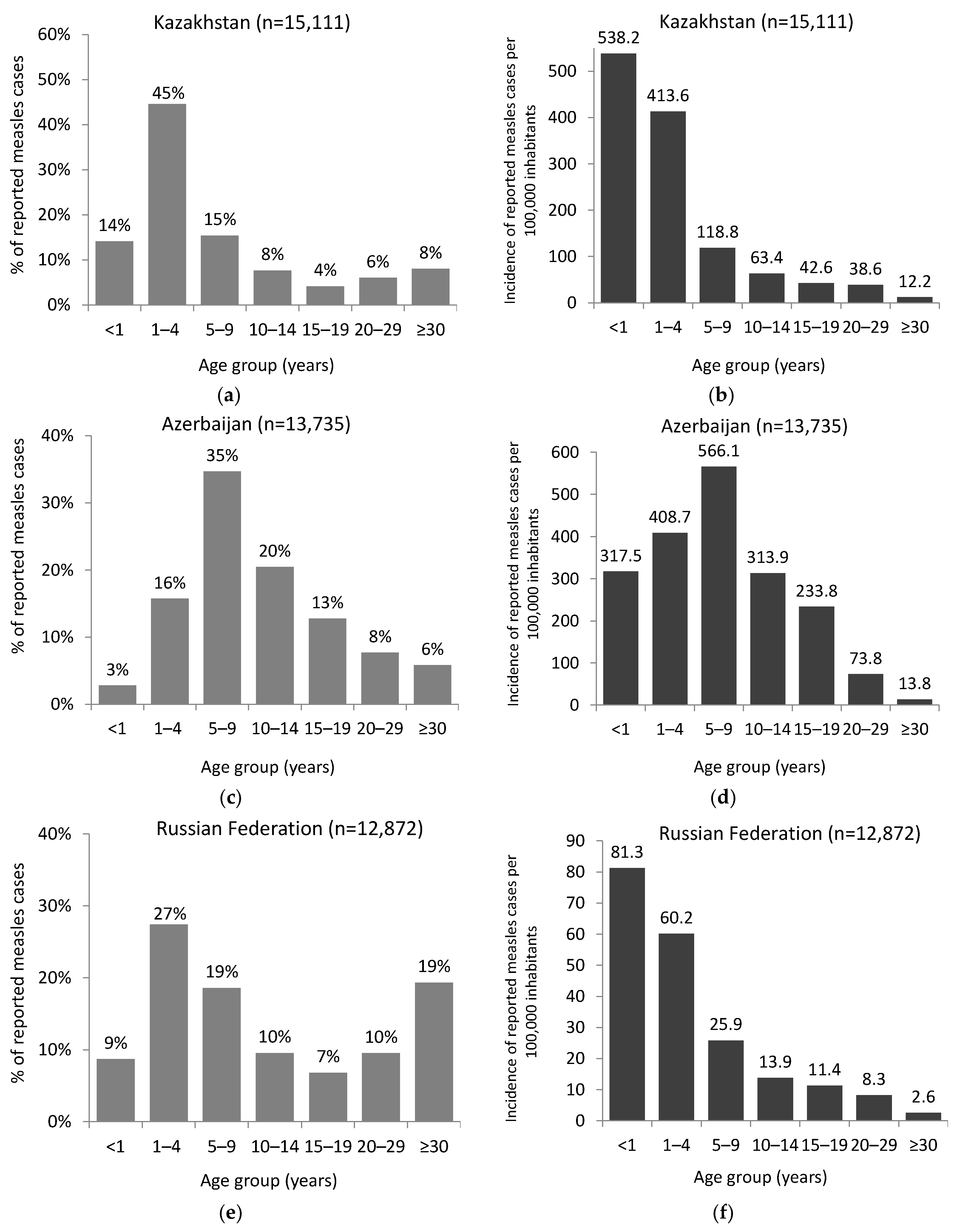
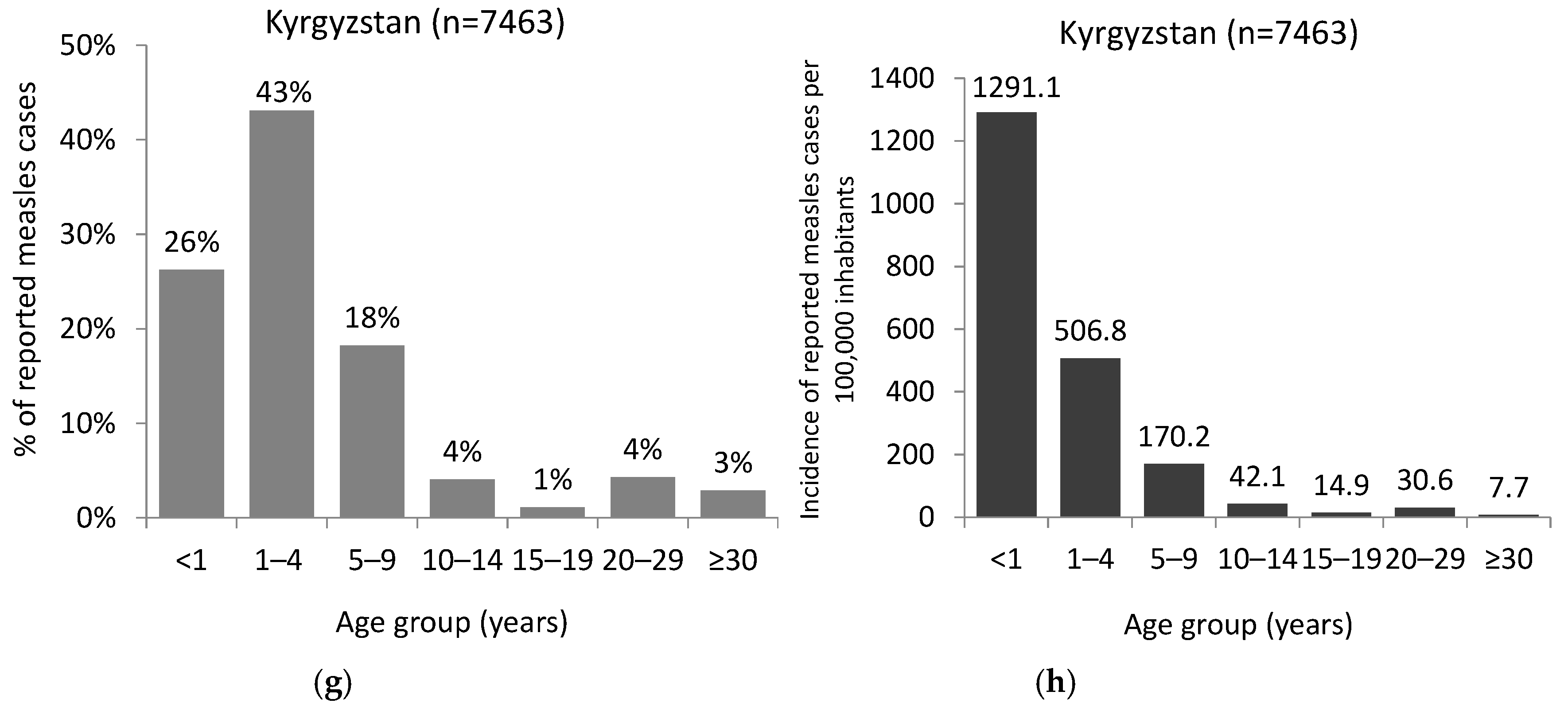
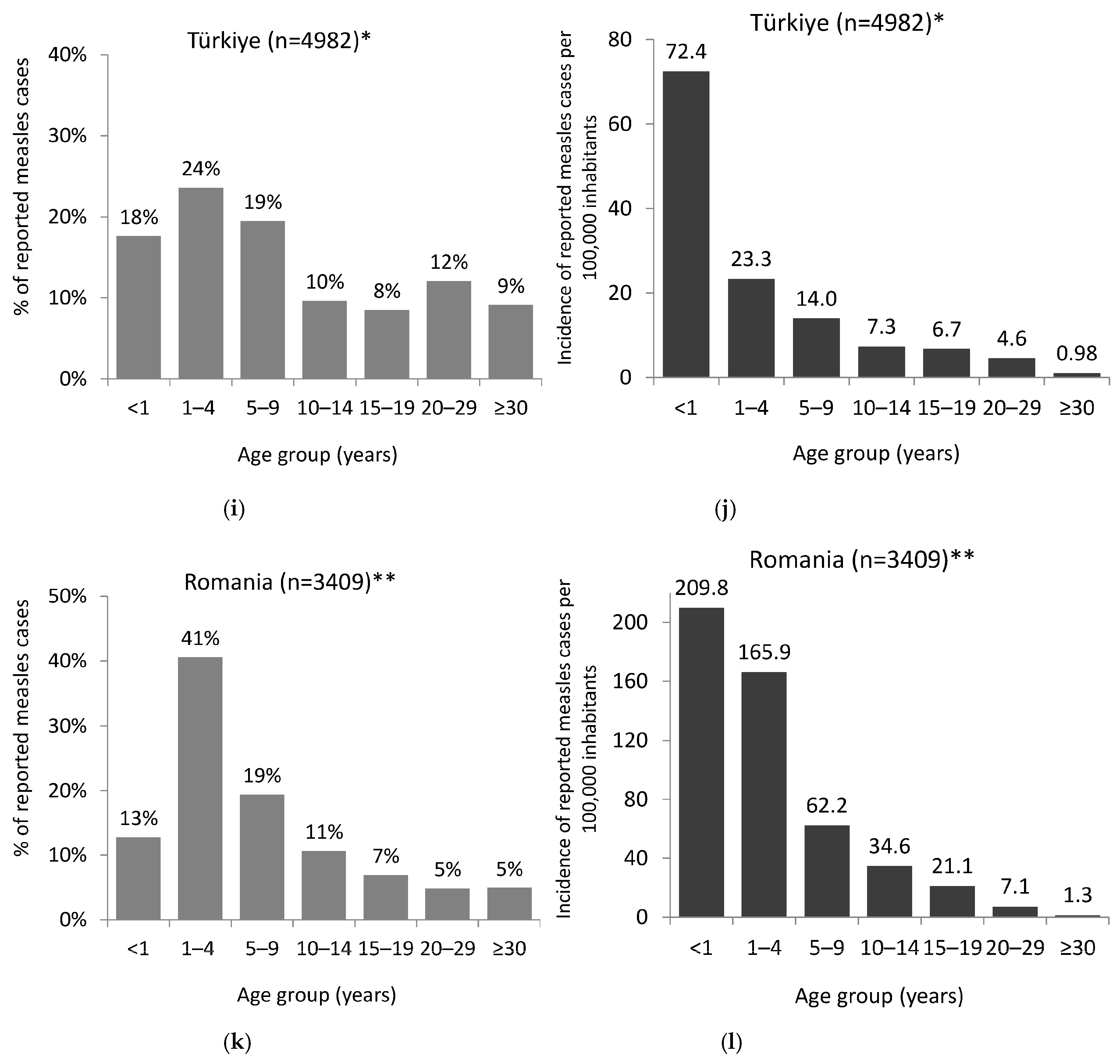
3.1.2. Age Distribution
3.1.3. Vaccination Status
3.1.4. Measles-Rrelated Deaths
3.1.5. Hospitalization
3.1.6. Imported Cases
3.2. Rubella
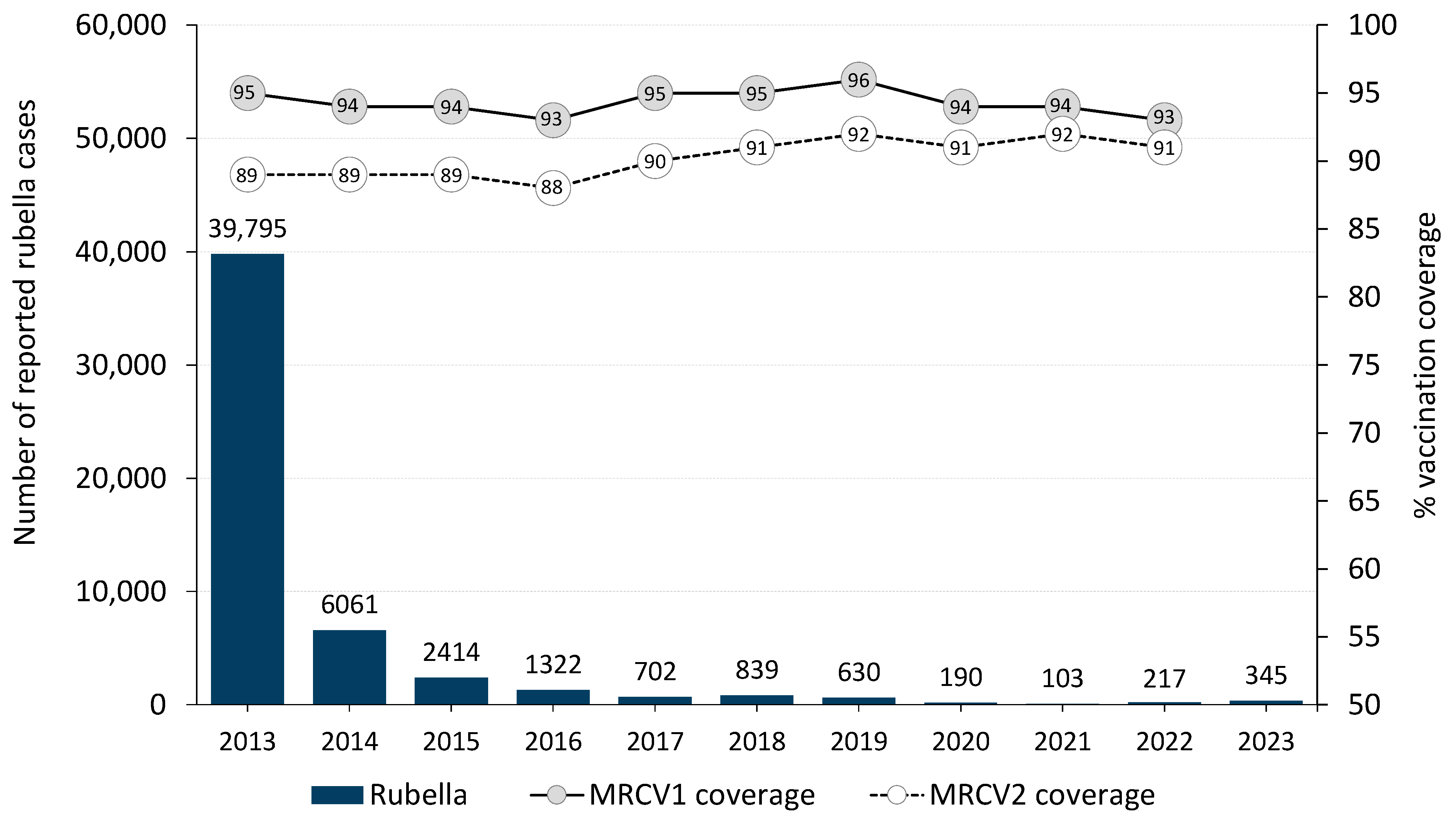
3.2.1. Incidence—Notifications and Laboratory Data
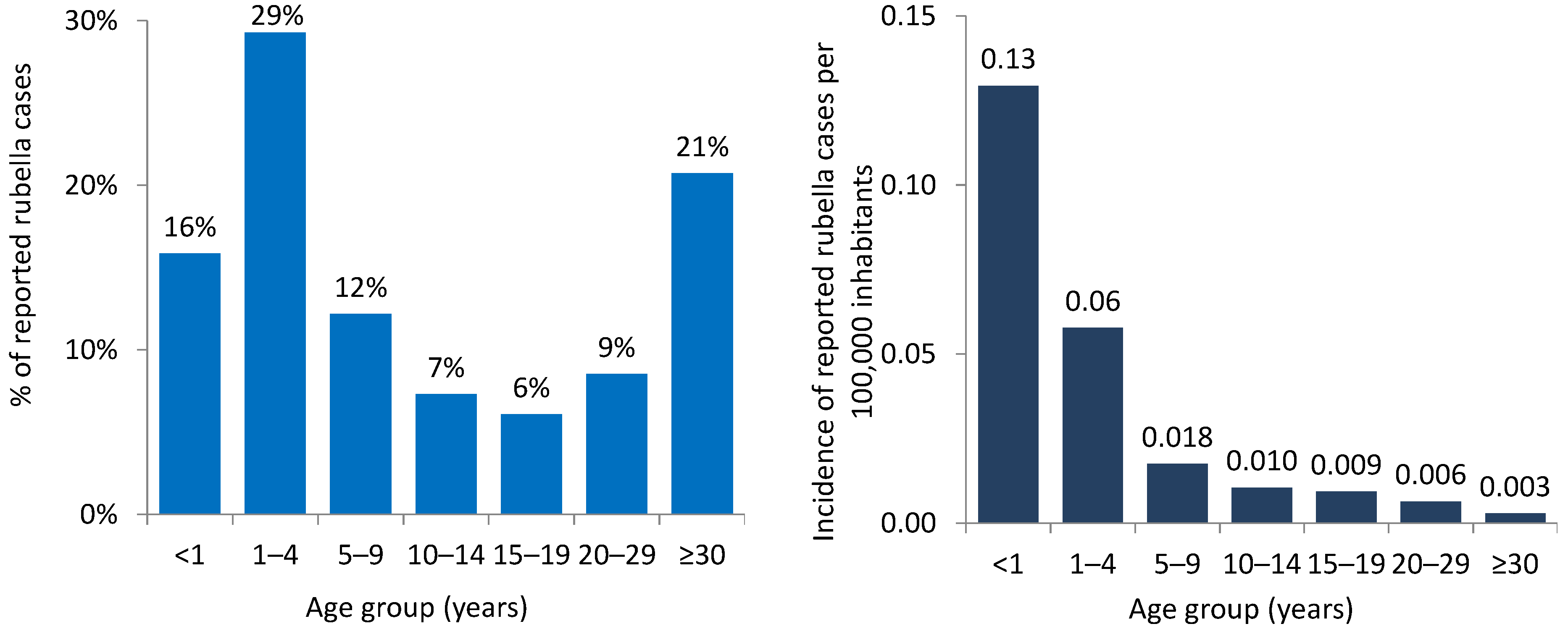
3.2.2. Age Distribution
3.2.3. Vaccination Status
3.2.4. Imported Cases
4. Discussion
4.1. Measles
4.2. Rubella
4.3. Limitations of Surveillance Data
4.4. Measles and Rubella Elimination Strategies
4.4.1. Achieving and Sustaining High Vaccination Coverage
4.4.2. Improving the Availability and Use of High-Quality, Evidence-based Information on Immunization
4.4.3. Strengthening Surveillance
4.4.4. Ensuring Adequate Outbreak Preparedness and Response
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Immunization Data Portal. Available online: https://immunizationdata.who.int/ (accessed on 9 April 2024).
- World Health Organization. Regional Office for Europe. HEALTH21—Health for All in the 21st Century: An Introduction; WHO Regional Office for Europe: Copenhagen, Denmark, 1998; Available online: https://iris.who.int/handle/10665/107327 (accessed on 16 April 2024).
- World Health Organization. Regional Office for Europe. Strategic Plan for Measles and Congenital Rubella Infection in the European Region of WHO; WHO Regional Office for Europe: Copenhagen, Denmark, 2003; Available online: https://iris.who.int/handle/10665/107526 (accessed on 16 April 2024).
- World Health Organization. Regional Office for Europe. Fifty-Fifth Regional Committee for Europe: Bucharest, 12–15 September 2005: Draft Resolution: Strengthening National Immunization Systems through Measles and Rubella Elimination and Prevention of Congenital Rubella Infection in WHO’s European Region; WHO Regional Office for Europe: Copenhagen, Denmark, 2005; Available online: https://iris.who.int/handle/10665/365068 (accessed on 16 April 2024).
- World Health Organization. Regional Office for Europe. Sixtieth Regional Committee for Europe: Moscow, 13–16 September 2010: Resolution: Renewed Commitment to Elimination of Measles and Rubella and Prevention of Congenital Rubella Syndrome by 2015 and Sustained Support for Polio-Free Status in the WHO European Region; WHO Regional Office for Europe: Copenhagen, Denmark, 2010; Available online: https://apps.who.int/iris/handle/10665/333436 (accessed on 29 September 2022).
- World Health Organization. Regional Office for Europe. Sixty-Fourth Regional Committee for Europe: Copenhagen, 15–18 September 2014: Resolution: European Vaccine Action Plan 2015–2020; WHO Regional Office for Europe: Copenhagen, Denmark, 2014; Available online: https://apps.who.int/iris/handle/10665/337429 (accessed on 1 August 2022).
- World Health Organization. Regional Office for Europe. European Vaccine Action Plan 2015–2020; WHO Regional Office for Europe: Copenhagen, Denmark, 2014; Available online: https://apps.who.int/iris/handle/10665/340400 (accessed on 29 September 2022).
- World Health Organization. Regional Office for Europe. The European Immunization Agenda 2030; WHO Regional Office for Europe: Copenhagen, Denmark, 2021; Available online: https://www.who.int/europe/initiatives/the-european-immunization-agenda-2030 (accessed on 24 January 2024).
- Measles Nucleotide Surveillance Database (MeaNs). Available online: https://who-gmrln.org/means2 (accessed on 5 March 2024).
- Rubella Nucleotide Surveillance database (RubeNS). Available online: https://who-gmrln.org/rubens2 (accessed on 5 March 2024).
- World Health Organization. Regional Office for Europe. Monitoring and Reporting of Routine Immunization-Related Data; WHO Regional Office for Europe: Copenhagen, Denmark, 2023; Available online: https://www.who.int/europe/activities/monitoring-and-reporting-of-routine-immunization-related-data (accessed on 30 April 2024).
- European Centre for Disease Prevention and Control. The European Surveillance System (TESSy). European Centre for Disease Prevention and Control: Stockholm, Sweden, 2017. Available online: https://www.ecdc.europa.eu/en/publications-data/european-surveillance-system-tessy (accessed on 5 March 2024).
- World Health Organization. Regional Office for Europe. Twelfth Meeting of the European Regional Verification Commission for Measles and Rubella Elimination: 8–11 September 2023 Copenhagen, Denmark: Meeting Report; Licence: CC BY-NC-SA 3.0 IGO; WHO Regional Office for Europe: Copenhagen, Denmark, 2024; Available online: https://www.who.int/europe/publications/i/item/WHO-EURO-2024-9722-49494-74055 (accessed on 30 April 2024).
- World Health Organization. Regional Office for Europe. Eliminating Measles and Rubella in the WHO European Region: Integrated Guidance for Surveillance, Outbreak Response and Verification of Elimination; WHO Regional Office for Europe: Copenhagen, Denmark, 2024; Available online: https://iris.who.int/handle/10665/375923 (accessed on 11 April 2024).
- United Nations, Department of Economic and Social Affairs, Population Division. World Population Prospects: The 2022 Revision; Online edition; Population Division: New York, NY, USA, 2022; Available online: https://population.un.org/wpp/ (accessed on 1 February 2024).
- World Health Organization. Regional Office for Europe. WHO EpiBrief no. 1/2020: A Report on the Epidemiology of Selected Vaccine-preventable Diseases in the European Region; WHO Regional Office for Europe: Copenhagen, Denmark, 2020; Available online: https://iris.who.int/handle/10665/360803 (accessed on 30 April 2024).
- World Health Organization. Regional Office for Europe. WHO EpiData 4/2024; WHO Regional Office for Europe: Copenhagen, Denmark, 2024; Available online: https://www.who.int/europe/publications/m/item/epidata-4-2024 (accessed on 30 April 2024).
- Akilbekova, D.; Yerdessov, S.; Gaipov, A. Urgent health update: Rising measles cases in Kazakhstan. Lancet Reg. Health 2024, 37, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Dubé, E.; Laberge, C.; Guay, M.; Bramadat, P.; Roy, R.; Bettinger, J.A. Vaccine hesitancy: An overview. Human Vaccin. Immunother. 2013, 9, 1763–1773. [Google Scholar] [CrossRef] [PubMed]
- Funk, S.; Knapp, J.K.; Lebo, E.; Reef, S.E.; Dabbagh, A.J.; Kretsinger, K.; Jit, M.; Edmunds, W.J.; Strebel, P.M. Combining serological and contact data to derive target immunity levels for achieving and maintaining measles elimination. BMC Med. 2019, 17, 180. [Google Scholar] [CrossRef] [PubMed]
- Pritt, B.S.; Hardin, N.J.; Richmond, J.A.; Shapiro, S.L. Death certification errors at an academic institution. Arch. Pathol. Lab. Med. 2005, 129, 1476–1479. [Google Scholar] [CrossRef] [PubMed]
- Armour, A.; Bharucha, H. Nosological inaccuracies in death certification in Northern Ireland. Ulster Med. J. 1997, 66, 13–17. [Google Scholar] [PubMed] [PubMed Central]
- Wendorf, K.A.; Winter, K.; Zipprich, J.; Schechter, R.; Hacker, J.K.; Preas, C.; Cherry, J.D.; Glaser, C.; Harriman, K. Subacute sclerosing panencephalitis: The devastating measles complication is more common than we think. Clin. Infect. Dis. 2017, 65, 226–232. [Google Scholar] [CrossRef] [PubMed]
- Muscat, M. Who gets measles in Europe? J. Infect. Dis. 2011, 204, S353–S365. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Regional Office for Europe. A practical guide to identifying, addressing and tracking inequities in immunization; WHO Regional Office for Europe: Copenhagen, Denmark, 2024; In Press. [Google Scholar]
- Shet, A.; Carr, K.; Danovaro-Holliday, M.C.; Sodha, S.V.; Prosperi, C.; Wunderlich, J.; Wonodi, C.; Reynolds, H.W.; Mirza, I.; Gacic-Dobo, M.; et al. Impact of the SARS-CoV-2 pandemic on routine immunisation services: Evidence of disruption and recovery from 170 countries and territories. Lancet Glob. Health 2022, 10, e186–e194. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Regional Office for Europe. Operational Considerations for Planning and Implementing Catch-Up Vaccination in the WHO European Region; WHO Regional Office for Europe: Copenhagen, Denmark, 2023; Available online: https://apps.who.int/iris/handle/10665/351183 (accessed on 12 April 2024).
- World Health Organization. Regional Office for Europe. Communicating with Health Workers about COVID-19 Vaccination; WHO Regional Office for Europe: Copenhagen, Denmark, 2021; Available online: https://iris.who.int/handle/10665/343962 (accessed on 25 April 2024).
- World Health Organization. Regional Office for Europe. Communicating with Patients about COVID-19 Vaccination: Evidence-Based Guidance for Effective Conversations to Promote COVID-19 Vaccine Uptake; WHO Regional Office for Europe: Copenhagen, Denmark, 2021; Available online: https://iris.who.int/handle/10665/340751 (accessed on 25 April 2024).
- World Health Organization. Regional Office for Europe. Communicating about Vaccination with Caregivers and Patients: A Communication Training Module for Health Workers; WHO Regional Office for Europe: Copenhagen, Denmark, 2023; Available online: https://iris.who.int/handle/10665/375090 (accessed on 25 April 2024).
- World Health Organization. Regional Office for Europe. Vaccination and Trust: How Concerns Arise and the Role of Communication in Mitigating Crises; WHO Regional Office for Europe: Copenhagen, Denmark, 2017; Available online: https://iris.who.int/handle/10665/343299 (accessed on 26 April 2024).
- Lahti, A.; Rosengren, B.E.; Nilsson, J.Å.; Karlsson, C.; Karlsson, M.K. Long-term effects of daily physical education throughout compulsory school on duration of physical activity in young adulthood: An 11-year prospective controlled study. BMJ Open Sport Exerc. Med. 2018, 4, e000360. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Goldfarb, E.S.; Lieberman, L.D. Three decades of research: The case for comprehensive sex education. J. Adolesc. Health 2021, 68, 13–27. [Google Scholar] [CrossRef] [PubMed]
- Berniell, L.; de la Mata, D.; Valdés, N. Spillovers of health education at school on parents’ physical activity. Health Econ. 2013, 22, 1004–1020. [Google Scholar] [CrossRef] [PubMed]
- Maisonneuve, A.R.; Witteman, H.O.; Brehaut, J.; Dubé, È.; Wilson, K. Educating children and adolescents about vaccines: A review of current literature. Expert Rev. Vaccines 2018, 17, 311–321. [Google Scholar] [CrossRef] [PubMed]
- Esposito, S.; Bianchini, S.; Tagliabue, C.; Umbrello, G.; Madini, B.; Di Pietro, G.; Principi, N. Impact of a website based educational program for increasing vaccination coverage among adolescents. Human Vaccin. Immunother. 2018, 14, 961–968. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Regional Office for Europe. Immune Patrol. 2022. Available online: https://www.who.int/europe/multi-media/item/immune-patrol---overview# (accessed on 25 April 2024).
- World Health Organization. Regional Office for Europe. European Immunization Week. Available online: https://www.who.int/europe/campaigns/european-immunization-week (accessed on 25 April 2024).
- Filia, A.; Brenna, A.; Panà, A.; Maggio Cavallaro, G.; Massari, M.; Ciofi degli Atti, M.L. Health burden and economic impact of measles-related hospitalizations in Italy in 2002–2003. BMC Public Health 2007, 7, 169. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Measles Outbreak Guide; WHO: Geneva, Switzerland, 2022; Available online: https://apps.who.int/iris/handle/10665/360891 (accessed on 30 April 2024).
- Botelho-Nevers, E.; Cassir, N.; Minodier, P.; Laporte, R.; Gautret, P.; Badiaga, S.; Thiberville, D.J.; Ninove, L.; Charrel, R.; Brouqui, P. Measles among healthcare workers: A potential for nosocomial outbreaks. Euro Surveill. 2011, 16, 19764. [Google Scholar] [CrossRef] [PubMed]

| Country | Number of Measles Cases | Incidence per Million Inhabitants * | Number of Measles Cases 2023 | |||||
|---|---|---|---|---|---|---|---|---|
| 2022 | 2023 | 2022 | 2023 | Laboratory-confirmed | Epidemiologically Linked | Clinically Compatible | Imported | |
| Albania | 1 | 3 | 0.4 | 1.1 | 3 | 0 | 0 | 0 |
| Andorra | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Armenia | 0 | 556 | 0 | 200.1 | 547 | 9 | 0 | 38 |
| Austria | 1 | 186 | 0.1 | 20.8 | 186 | 0 | 0 | 8 |
| Azerbaijan | 1 | 13,735 | 0.1 | 1319.1 | 1429 | 5466 | 6840 | 57 |
| Belarus | 0 | 188 | 0 | 19.8 | 188 | 0 | 0 | 0 |
| Belgium | 17 | 68 | 1.5 | 5.8 | 52 | 12 | 4 | - |
| Bosnia and Herzegovina | 6 | 10 | 1.9 | 3.1 | 8 | 0 | 2 | 0 |
| Bulgaria | 1 | 0 | 0.1 | 0 | 0 | 0 | 0 | - |
| Croatia | 0 | 3 | 0 | 0.7 | 3 | 0 | 0 | 3 |
| Cyprus | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Czechia | 0 | 1 | 0 | 0.1 | 1 | 0 | 0 | 0 |
| Denmark | 0 | 9 | 0 | 1.5 | 5 | 4 | 0 | 3 |
| Estonia | 0 | 4 | 0 | 3.0 | 4 | 0 | 0 | 4 |
| Finland | 1 | 1 | 0.2 | 0.2 | 1 | 0 | 0 | 1 |
| France | 19 | 117 | 0.3 | 1.8 | 102 | 7 | 8 | 31 |
| Georgia | 12 | 39 | 3.2 | 10.5 | 37 | 0 | 2 | 13 |
| Germany | 15 | 83 | 0.2 | 1.0 | 75 | 3 | 5 | 30 |
| Greece | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Hungary | 0 | 1 | 0 | 0.1 | 1 | 0 | 0 | 1 |
| Iceland | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Ireland | 2 | 4 | 0.4 | 0.8 | 1 | 3 | 0 | 2 |
| Israel | 0 | 18 | 0 | 2.0 | 15 | 1 | 2 | 3 |
| Italy | 15 | 44 | 0.3 | 0.7 | 39 | 1 | 4 | 17 |
| Kazakhstan | 4 | 15,111 | 0.2 | 770.7 | 14,087 | 688 | 336 | - |
| Kyrgyzstan | 23 | 7463 | 3.5 | 1108.0 | 2023 | 3373 | 2067 | 4 |
| Latvia | 0 | 1 | 0 | 0.5 | 1 | 0 | 0 | 1 |
| Lithuania | 0 | 4 | 0 | 1.5 | 4 | 0 | 0 | 1 |
| Luxembourg | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Malta | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Monaco | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Montenegro | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Netherlands (Kingdom of the) | 6 | 7 | 0.3 | 0.4 | 6 | 1 | 0 | 3 |
| North Macedonia | 0 | 1 | 0 | 0.5 | 1 | 0 | 0 | 0 |
| Norway | 1 | 2 | 0.2 | 0.4 | 2 | 0 | 0 | 1 |
| Poland | 41 | 29 | 1.0 | 0.7 | 16 | 0 | 13 | 1 |
| Portugal | 0 | 1 | 0 | 0.1 | 0 | 0 | 1 | 0 |
| Republic of Moldova | 0 | 3 | 0 | 0.9 | 3 | 0 | 0 | 2 |
| Romania | 9 | 3419 | 0.5 | 171.9 | 3018 | 281 | 120 | 17 |
| Russian Federation | 117 | 12,872 | 0.8 | 89.1 | 12,570 | 189 | 113 | 292 |
| San Marino | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Serbia | 0 | 52 | 0 | 7.3 | 47 | 1 | 4 | 0 |
| Slovakia | 0 | 6 | 0 | 1.0 | 6 | 0 | 0 | 2 |
| Slovenia | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Spain | 1 | 13 | 0.02 | 0.3 | 10 | 0 | 3 | 6 |
| Sweden | 4 | 11 | 0.4 | 1.0 | 11 | 0 | 0 | 6 |
| Switzerland | 1 | 37 | 0.1 | 4.2 | 34 | 3 | 0 | 13 |
| Tajikistan | 451 | 294 | 45.3 | 29.0 | 250 | 44 | 0 | 0 |
| Türkiye | 127 | 4984 | 1.5 | 58.1 | 4969 | 2 | 13 | 66 |
| Turkmenistan | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Ukraine | 11 | 66 | 0.3 | 1.8 | 57 | 0 | 9 | 0 |
| United Kingdom | 50 | 231 | 0.7 | 3.4 | 231 | 0 | 0 | 30 |
| Uzbekistan | 8 | 1183 | 0.2 | 33.6 | 1166 | 0 | 17 | 3 |
| WHO European Region | 945 | 60,860 | 1.0 | 65.3 | 41,209 | 10,088 | 9563 | 659 |
| <1 Years | 1–4 Years | 5–9 Years | 10–14 Years | 15–19 Years | 20–29 Years | ≥30 Years | Unknown Age | Total | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unvaccinated | 6804 | 90% | 14,652 | 77% | 7945 | 62% | 3515 | 53% | 2059 | 49% | 1848 | 41% | 2214 | 38% | 8 | 67% | 39,045 | 64% |
| Vaccinated with a single dose | 88 | 1% | 2220 | 12% | 1288 | 10% | 621 | 9% | 300 | 7% | 204 | 4% | 221 | 4% | 1 | 8% | 4943 | 8% |
| Vaccinated with at least two doses | 6 | 0% | 148 | 1% | 917 | 7% | 881 | 13% | 591 | 14% | 441 | 10% | 440 | 7% | 1 | 8% | 3425 | 6% |
| Unknown status | 699 | 9% | 2117 | 11% | 2688 | 21% | 1609 | 24% | 1288 | 30% | 2051 | 45% | 2993 | 51% | 2 | 17% | 13,447 | 22% |
| Total | 7597 | 100% | 19,137 | 100% | 12,838 | 100% | 6626 | 100% | 4238 | 100% | 4544 | 100% | 5868 | 100% | 12 | 100% | 60,860 | 100% |
| Country | Number of Rubella Cases | Incidence per Million Inhabitants * | Number of Rubella Cases 2023 | |||||
|---|---|---|---|---|---|---|---|---|
| 2022 | 2023 | 2022 | 2023 | Laboratory-confirmed | Epidemiologically Linked | Clinically Compatible | Imported | |
| Albania | 0 | 1 | 0 | 0.4 | 1 | 0 | 0 | 0 |
| Andorra | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Armenia | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Austria | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Azerbaijan | 4 | 0 | 0.4 | 0 | 0 | 0 | 0 | - |
| Belarus | - | 0 | - | 0 | 0 | 0 | 0 | - |
| Belgium 1 | - | - | - | - | - | - | - | - |
| Bosnia and Herzegovina | 0 | 2 | 0 | 0.6 | 1 | 0 | 1 | - |
| Bulgaria | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Croatia | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Cyprus | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Czechia | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Denmark 2 | - | - | - | - | - | - | - | - |
| Estonia | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Finland | 1 | 1 | 0.2 | 0.2 | 1 | 0 | 0 | 0 |
| France | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Georgia | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Germany | 8 | 8 | 0.1 | 0.1 | 5 | 0 | 3 | 0 |
| Greece | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Hungary | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Iceland | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Ireland | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Israel | 0 | 1 | 0 | 0.1 | 1 | 0 | 0 | 0 |
| Italy | 4 | 2 | 0.1 | 0.03 | 1 | 0 | 1 | 0 |
| Kazakhstan | 0 | 7 | 0 | 0.4 | 6 | 1 | 0 | - |
| Kyrgyzstan | 2 | 11 | 0.3 | 1.6 | 11 | 0 | 0 | 1 |
| Latvia | 1 | 0 | 0.5 | 0 | 0 | 0 | 0 | - |
| Lithuania | 1 | 1 | 0.4 | 0.4 | 1 | 0 | 0 | 0 |
| Luxembourg | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Malta | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Monaco | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Montenegro | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Netherlands (Kingdom of the) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| North Macedonia | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Norway | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Poland | 147 | 263 | 3.7 | 6.4 | 10 | 3 | 250 | - |
| Portugal | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Republic of Moldova | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Romania | 0 | 1 | 0 | 0.1 | 1 | 0 | 0 | 1 |
| Russian Federation | 0 | 3 | 0 | 0.02 | 3 | 0 | 0 | 0 |
| San Marino | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Serbia | - | 0 | - | 0 | 0 | 0 | 0 | - |
| Slovakia | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Slovenia | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Spain | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Sweden | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Switzerland | 0 | 1 | 0 | 0.1 | 0 | 0 | 1 | 0 |
| Tajikistan | 0 | 10 | 0 | 1.0 | 10 | 0 | 0 | 0 |
| Türkiye | 40 | 20 | 0.5 | 0.2 | 20 | 0 | 0 | 0 |
| Turkmenistan | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Ukraine | 9 | 11 | 0.2 | 0.3 | 5 | 0 | 6 | 0 |
| United Kingdom | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Uzbekistan | 0 | 2 | 0 | 0.1 | 2 | 0 | 0 | 0 |
| WHO European Region | 217 | 345 | 0.2 | 0.4 | 79 | 4 | 262 | 2 |
| <1 Years | 1–4 Years | 5–9 Years | 10–14 Years | 15–19 Years | 20–29 Years | ≥30 Years | Unknown Age | Total | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unvaccinated | 7 | 54% | 2 | 8% | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | 1 | 6% | 0 | 0% | 10 | 3% |
| Vaccinated with a single dose | 0 | 0% | 13 | 54% | 2 | 20% | 0 | 0% | 0 | 0% | 0 | 0% | 1 | 6% | 0 | 0% | 16 | 5% |
| Vaccinated with at least two doses | 0 | 0% | 1 | 4% | 3 | 30% | 2 | 33% | 0 | 0% | 1 | 14% | 0 | 0% | 0 | 0% | 7 | 2% |
| Unknown status | 6 | 46% | 8 | 33% | 5 | 50% | 4 | 67% | 5 | 100% | 6 | 86% | 15 | 88% | 263 | 100% | 312 | 90% |
| Total | 13 | 100% | 24 | 100% | 10 | 100% | 6 | 100% | 5 | 100% | 7 | 100% | 17 | 100% | 263 | 100% | 345 | 100% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Muscat, M.; Ben Mamou, M.; Reynen-de Kat, C.; Jankovic, D.; Hagan, J.; Singh, S.; Datta, S.S. Progress and Challenges in Measles and Rubella Elimination in the WHO European Region. Vaccines 2024, 12, 696. https://doi.org/10.3390/vaccines12060696
Muscat M, Ben Mamou M, Reynen-de Kat C, Jankovic D, Hagan J, Singh S, Datta SS. Progress and Challenges in Measles and Rubella Elimination in the WHO European Region. Vaccines. 2024; 12(6):696. https://doi.org/10.3390/vaccines12060696
Chicago/Turabian StyleMuscat, Mark, Myriam Ben Mamou, Catharina Reynen-de Kat, Dragan Jankovic, José Hagan, Simarjit Singh, and Siddhartha Sankar Datta. 2024. "Progress and Challenges in Measles and Rubella Elimination in the WHO European Region" Vaccines 12, no. 6: 696. https://doi.org/10.3390/vaccines12060696
APA StyleMuscat, M., Ben Mamou, M., Reynen-de Kat, C., Jankovic, D., Hagan, J., Singh, S., & Datta, S. S. (2024). Progress and Challenges in Measles and Rubella Elimination in the WHO European Region. Vaccines, 12(6), 696. https://doi.org/10.3390/vaccines12060696








