Investigating Beliefs in Anti-Vax Conspiracy Theories among Medical Students
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Research Tool
2.3. Participants and Setting
2.4. Data Collection
2.5. Ethical Issues
2.6. Data Analysis
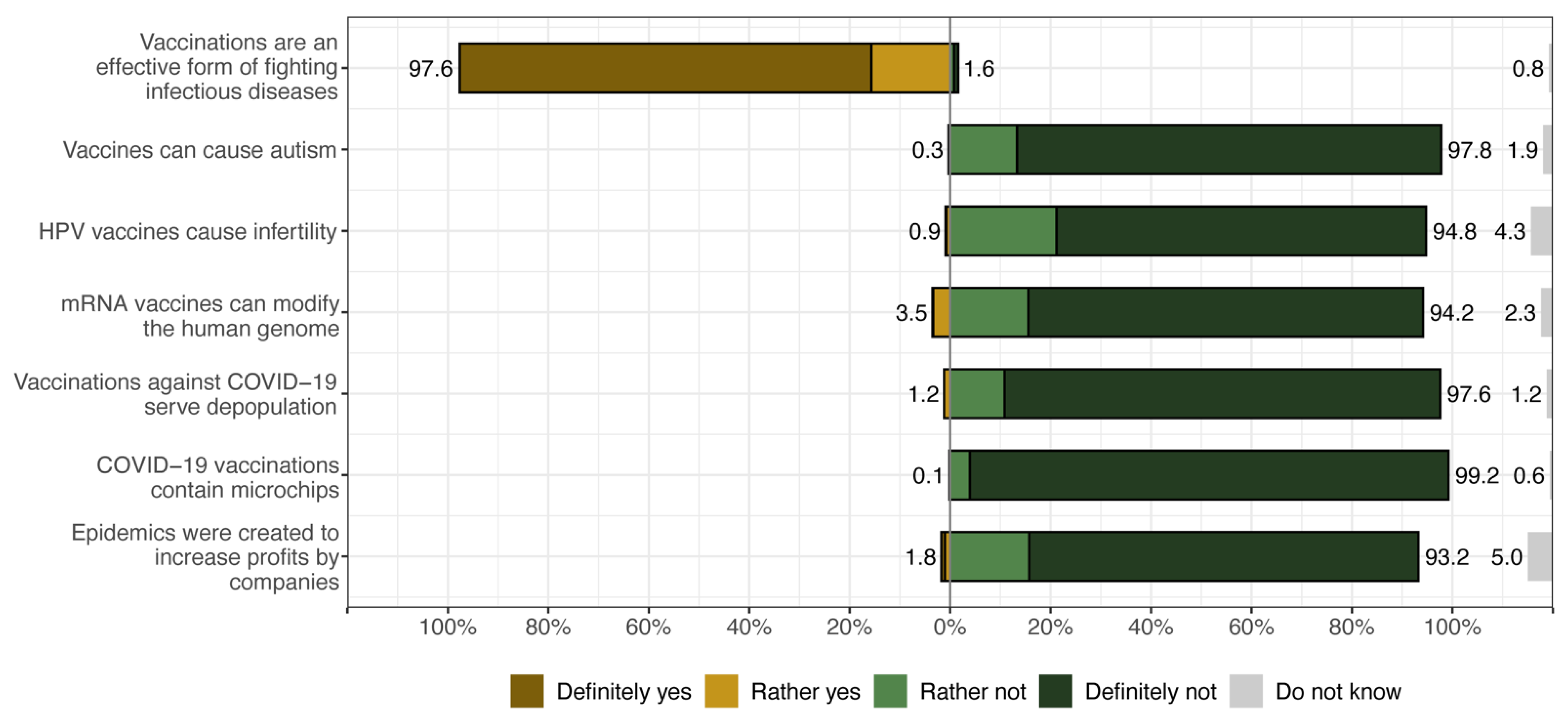
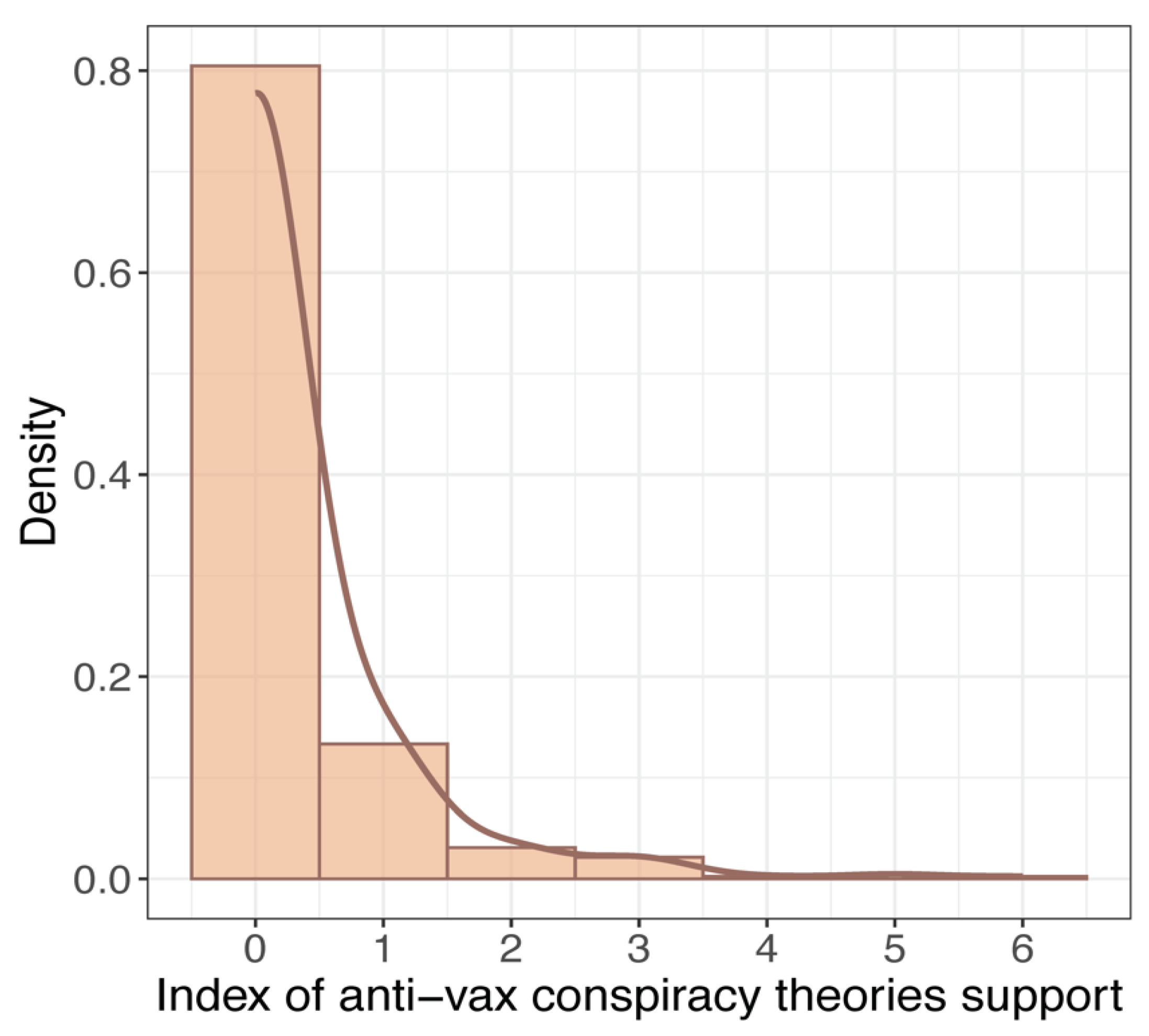
3. Results
| Predictors | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR (SE) | p | OR (SE) | p | OR (SE) | p | OR (SE) | p | OR (SE) | p | |
| Intercept | 0.30 (0.05) | <0.001 | 0.54 (0.12) | 0.004 | 0.30 (0.07) | <0.001 | 0.88 (0.15) | 0.448 | 0.41 (0.06) | <0.001 |
| Gender: Male [vs. Female] | 1.25 (0.17) | 0.110 | 1.12 (0.16) | 0.418 | 1.10 (0.17) | 0.189 | 1.17 (0.16) | 0.267 | 1.04 (0.15) | 0.798 |
| Year of study 3–5 [vs. 1–2] | 0.48 (0.10) | 0.001 | 0.44 (0.06) | <0.001 | 0.52 (0.07) | <0.001 | 0.43 (0.06) | <0.001 | 0.40 (0.05) | <0.001 |
| Domicile: 10–100 k [vs. Up to 10 k] inhabitants | 0.56 (0.10) | 0.001 | 0.52 (0.09) | <0.001 | 0.53 (0.09) | <0.001 | 0.48 (0.09) | <0.001 | 0.50 (0.09) | <0.001 |
| Domicile: 100–500 k [vs. Up to 10k] inhabitants | 0.67 (0.14) | 0.058 | 0.62 (0.13) | 0.026 | 0.65 (0.14) | 0.039 | 0.73 (0.15) | 0.131 | 0.70 (0.15) | 0.085 |
| Domicile: <500 k [vs. Up to 10 k] inhabitants | 0.38 (0.06) | <0.001 | 0.36 (0.06) | <0.001 | 0.38 (0.06) | <0.001 | 0.39 (0.06) | <0.001 | 0.39 (0.07) | <0.001 |
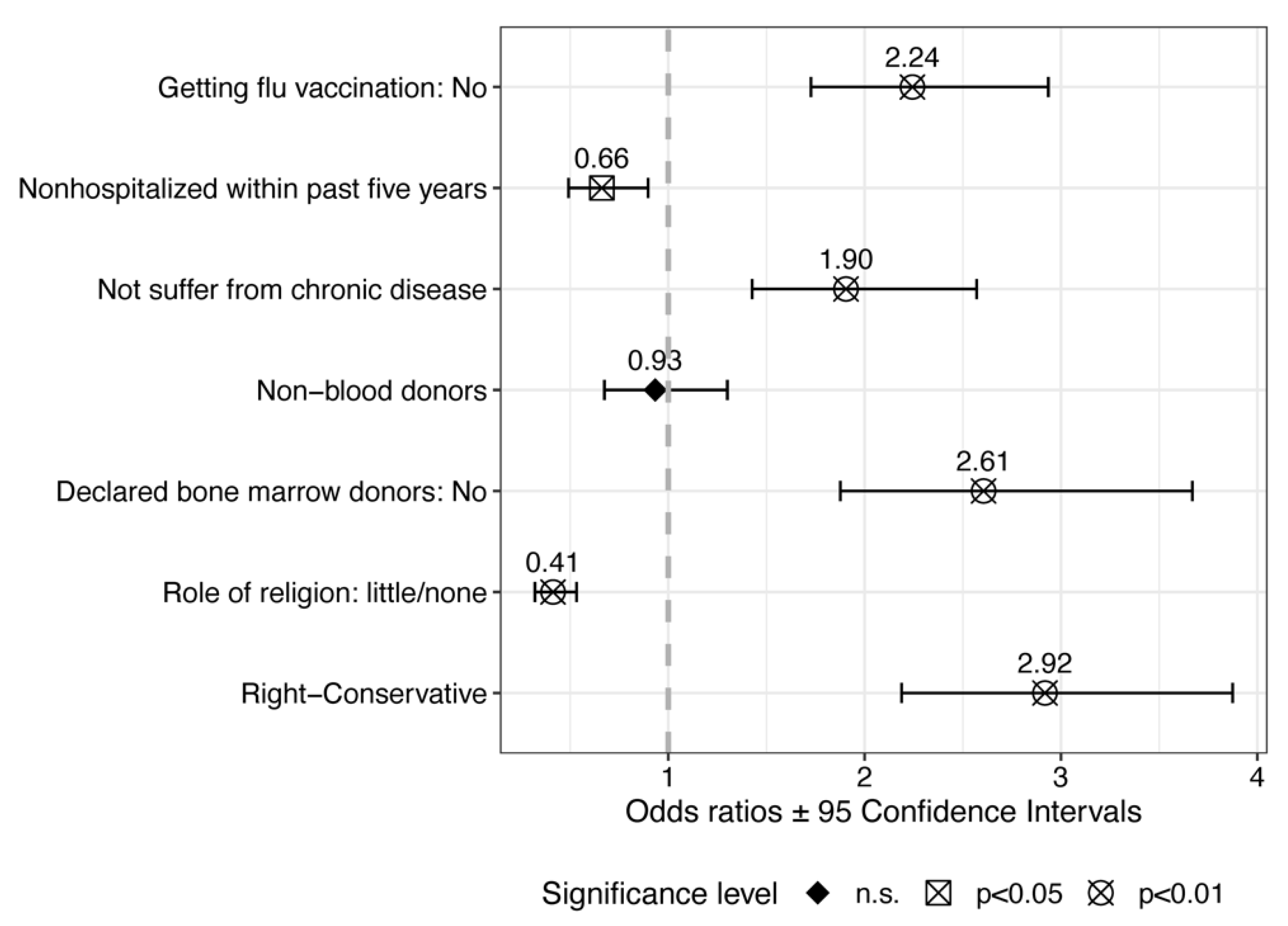
| Received flu vaccination: No [vs. Yes] | 1.93 (0.27) | <0.001 | ||||||||
| Hospitalized within past five years: No [vs. Yes] | 0.59 (0.09) | 0.001 | ||||||||
| Suffering from chronic disease: No [vs. Yes] | 1.61 (0.25) | 0.002 | ||||||||
| Blood donor: No [vs. Yes] | 0.84 (0.14) | 0.322 | ||||||||
| Declared bone marrow donor: No [vs. Yes] | 1.99 (0.36) | <0.001 | ||||||||
| Role of religion: Little/none [vs. Important] | 0.41 (0.06) | <0.001 | ||||||||
| Right–conservative [vs. Left–liberal] | 3.06 (0.47) | <0.001 | ||||||||
| Observations | 401 | 401 | 401 | 401 | 401 | |||||
| Likelihood Ratio Test (p-values) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| AIC | 1574.322 | 1582.870 | 1583.939 | 1555.988 | 1548.729 | |||||
| log-Likelihood | −780.161 | −783.435 | −783.969 | −770.994 | −767.364 | |||||
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- André, F.E. Vaccinology: Past achievements, present roadblocks and future promises. Vaccine 2003, 21, 593–595. [Google Scholar] [CrossRef] [PubMed]
- Andre, F.E.; Booy, R.; Bock, H.L.; Clemens, J.; Datta, S.K.; John, T.J.; Lee, B.W.; Lolekha, S.; Peltola, H.; Ruff, T.A.; et al. Vaccination greatly reduces disease, disability, death and inequity worldwide. Bull. World Health Organ. 2008, 86, 140–146. [Google Scholar] [CrossRef]
- Greenwood, B. The contribution of vaccination to global health: Past, present and future. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2014, 369, 20130433. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention (CDC). Ten great public health achievements—United States, 1900–1999. MMWR Morb. Mortal. Wkly. Rep. 1999, 48, 241–243. [Google Scholar]
- Centers for Disease Control and Prevention (CDC). Ten great public health achievements—Worldwide, 2001–2010. MMWR Morb. Mortal. Wkly. Rep. 2011, 60, 814–818. [Google Scholar]
- Norrby, E. Yellow fever and Max Theiler: The only Nobel Prize for a virus vaccine. J. Exp. Med. 2007, 204, 2779–2784. [Google Scholar] [CrossRef] [PubMed]
- The Nobel Prize. Available online: https://www.nobelprize.org/prizes/medicine/2023/press-release/ (accessed on 31 January 2024).
- Wolfe, R.M.; Sharp, L.K. Anti-vaccinationists past and present. BMJ 2002, 325, 430–432. [Google Scholar] [CrossRef]
- Hussain, A.; Ali, S.; Ahmed, M.; Hussain, S. The anti-vaccination movement: A regression in modern medicine. Cureus 2018, 10, e2919. [Google Scholar] [CrossRef] [PubMed]
- Grignolio, A. A brief history of anti-vaccination movements. In Vaccines: Are They Worth a Shot? Copernicus: Cham, Switzerland, 2018; pp. 25–40. [Google Scholar] [CrossRef]
- Gallegos, M.; de Castro Pecanha, V.; Caycho-Rodríguez, T. Anti-vax: The history of a scientific problem. J. Public Health 2023, 45, e140–e141. [Google Scholar] [CrossRef] [PubMed]
- Andrade, G. Medical conspiracy theories: Cognitive science and implications for ethics. Med. Health Care Philos. 2020, 23, 505–518. [Google Scholar] [CrossRef] [PubMed]
- Wakefield, A.J.; Murch, S.H.; Anthony, A.; Linnell, J.; Casson, D.M.; Malik, M.; Berelowitz, M.; Dhillon, A.P.; Thomson, M.A.; Harvey, P.; et al. Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. Lancet 1998, 351, 637–641. [Google Scholar] [CrossRef] [PubMed]
- Allan, G.M.; Ivers, N. The autism-vaccine story: Fiction and deception? Can. Fam. Physician 2010, 56, 1013. [Google Scholar] [PubMed]
- Davidson, M. Vaccination as a cause of autism—Myths and controversies. Dialogues Clin. Neurosci. 2017, 19, 403–407. [Google Scholar] [CrossRef] [PubMed]
- Andrade, G.E.; Hussain, A. Polio in Pakistan: Political, sociological, and epidemiological factors. Cureus 2018, 10, e3502. [Google Scholar] [CrossRef] [PubMed]
- Alsuwaidi, A.R.; Hammad, H.A.A.; Elbarazi, I.; Sheek-Hussein, M. Vaccine hesitancy within the Muslim community: Islamic faith and public health perspectives. Hum. Vaccin. Immunother. 2023, 19, 2190716. [Google Scholar] [CrossRef] [PubMed]
- Jegede, A.S. What Led to the Nigerian Boycott of the Polio Vaccination Campaign? PLoS Med. 2007, 4, e73. [Google Scholar] [CrossRef] [PubMed]
- Kapp, C. Nigerian states again boycott polio-vaccination drive. Muslim officials have rejected assurances that the polio vaccine is safe—Leaving Africa on the brink of reinfection. Lancet 2004, 363, 709. [Google Scholar] [CrossRef] [PubMed]
- Ghinai, I.; Willott, C.; Dadari, I.; Larson, H.J. Listening to the rumours: What the northern Nigeria polio vaccine boycott can tell us ten years on. Glob. Public Health 2013, 8, 1138–1150. [Google Scholar] [CrossRef]
- Karafillakis, E.; Simas, C.; Jarrett, C.; Verger, P.; Peretti-Watel, P.; Dib, F.; De Angelis, S.; Takacs, J.; Ali, K.A.; Pastore Celentano, L.; et al. HPV vaccination in a context of public mistrust and uncertainty: A systematic literature review of determinants of HPV vaccine hesitancy in Europe. Hum. Vaccines Immunother. 2019, 15, 1615–1627. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Zhang, Y.; Young, R.; Wu, X.; Zhu, G. Effects of vaccine-related conspiracy theories on Chinese young adults’ perceptions of the HPV vaccine: An experimental study. Health Commun. 2021, 36, 1343–1353. [Google Scholar] [CrossRef]
- Pertwee, E.; Simas, C.; Larson, H.J. An epidemic of uncertainty: Rumors, conspiracy theories and vaccine hesitancy. Nat. Med. 2022, 28, 456–459. [Google Scholar] [CrossRef] [PubMed]
- Karafillakis, E.; Van Damme, P.; Hendrickx, G.; Larson, H.J. COVID-19 in Europe: New challenges for addressing vaccine hesitancy. Lancet 2022, 399, 699–701. [Google Scholar] [CrossRef] [PubMed]
- Kalichman, S.C.; Eaton, L.A.; Earnshaw, V.A.; Brousseau, N. Faster than warp speed: Early attention to COVD-19 by anti-vaccine groups on Facebook. J. Public Health 2022, 44, e96–e105. [Google Scholar] [CrossRef]
- Islam, M.S.; Kamal, A.M.; Kabir, A.; Southern, D.L.; Khan, S.H.; Hasan, S.M.M.; Sarkar, T.; Sharmin, S.; Das, S.; Roy, T.; et al. COVID-19 vaccine rumors and conspiracy theories: The need for cognitive inoculation against misinformation to improve vaccine adherence. PLoS ONE 2021, 16, e0251605. [Google Scholar] [CrossRef] [PubMed]
- Shahsavari, S.; Holur, P.; Wang, T.; Tangherlini, T.R.; Roychowdhury, V. Conspiracy in the time of corona: Automatic detection of emerging COVID-19 conspiracy theories in social media and the news. J. Comput. Soc. Sci. 2020, 3, 279–317. [Google Scholar] [CrossRef]
- Kaadan, M.I.; Abdulkarim, J.; Chaar, M.; Zayegh, O.; Keblawi, M.A. Determinants of COVID-19 vaccine acceptance in the Arab world: A cross-sectional study. Glob. Health Res. Policy 2021, 6, 23. [Google Scholar] [CrossRef]
- Walkowiak, M.P.; Domaradzki, J.; Walkowiak, D. Better late than never: Predictors of delayed COVID-19 vaccine uptake in Poland. Vaccines 2022, 10, 528. [Google Scholar] [CrossRef] [PubMed]
- Jabkowski, P.; Domaradzki, J.; Baranowski, M. Exploring COVID-19 conspiracy theories: Education, religiosity, trust in scientists, and political orientation in 26 European countries. Sci. Rep. 2023, 13, 18116. [Google Scholar] [CrossRef]
- Dzieciolowska, S.; Hamel, D.; Gadio, S.; Dionne, M.; Gagnon, D.; Robitaille, L.; Cook, E.; Caron, I.; Talib, A.; Parkes, L.; et al. COVID-19 vaccine acceptance, hesitancy, and refusal among Canadian healthcare workers: A multicenter survey. Am. J. Infect. Control 2021, 49, 1152–1157. [Google Scholar] [CrossRef] [PubMed]
- Lindner-Pawłowicz, K.; Mydlikowska-Śmigórska, A.; Łampika, K.; Sobieszczańska, M. COVID-19 vaccination acceptance among healthcare workers and general population at the very beginning of the National Vaccination Program in Poland: A cross-sectional, exploratory study. Vaccines 2021, 10, 66. [Google Scholar] [CrossRef] [PubMed]
- Peterson, C.J.; Lee, B.; Nugent, K. COVID-19 Vaccination hesitancy among healthcare workers—A review. Vaccines 2022, 10, 948. [Google Scholar] [CrossRef] [PubMed]
- Tavolacci, M.P.; Dechelotte, P.; Ladner, J. COVID-19 Vaccine acceptance, hesitancy, and resistancy among university students in France. Vaccines 2021, 9, 654. [Google Scholar] [CrossRef]
- Gautier, S.; Luyt, D.; Davido, B.; Herr, M.; Cardot, T.; Rousseau, A.; Annane, D.; Delarocque-Astagneau, E.; Josseran, L. Cross-sectional study on COVID-19 vaccine hesitancy and determinants in healthcare students: Interdisciplinary trainings on vaccination are needed. BMC Med. Educ. 2022, 22, 299. [Google Scholar] [CrossRef]
- McCready, J.L.; Nichol, B.; Steen, M.; Unsworth, J.; Comparcini, D.; Tomietto, M. Understanding the barriers and facilitators of vaccine hesitancy towards the COVID-19 vaccine in healthcare workers and healthcare students worldwide: An Umbrella Review. PLoS ONE 2023, 18, e0280439. [Google Scholar] [CrossRef] [PubMed]
- Lielsvagere-Endele, S.; Kolesnikova, J.; Puzanova, E.; Timofejeva, S.; Millere, I. Motivators and Barriers to COVID-19 Vaccination of Healthcare Workers in Latvia. Front. Psychol. 2022, 13, 903506. [Google Scholar] [CrossRef] [PubMed]
- Walker, L.; Newall, A.; Heywood, A.E. Knowledge, Attitudes and Practices of Australian Medical Students towards Influenza Vaccination. Vaccine 2016, 34, 6193–6199. [Google Scholar] [CrossRef] [PubMed]
- Rostkowska, O.M.; Peters, A.; Montvidas, J.; Magdas, T.M.; Rensen, L.; Zgliczyński, W.S.; Durlik, M.; Pelzer, B.W. Attitudes and Knowledge of European Medical Students and Early Graduates about Vaccination and Self-Reported Vaccination Coverage-Multinational Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2021, 18, 3595. [Google Scholar] [CrossRef] [PubMed]
- Kimberly, M.D.B. Medical Student Knowledge, Attitudes, and Practices Regarding Immunization. J. Vaccines Vaccin. 2012, 6, 268. [Google Scholar] [CrossRef]
- Sanftenberg, L.; Roggendorf, H.; Babucke, M.; Breckwoldt, J.; Gaertner, B.; Hetzer, B.; Lendeckel, A.; Riemenschneider, H.; Voigt, K.; Keplinger, A.; et al. Medical Students’ Knowledge and Attitudes Regarding Vaccination against Measles, Influenza and HPV. An International Multicenter Study. J. Prev. Med. Hyg. 2020, 61, E181–E185. [Google Scholar] [CrossRef] [PubMed]
- Daniel, C.L.; McLendon, L.; Green, C.L.; Anderson, K.J.; Pierce, J.Y.; Perkins, A.; Beasley, M. HPV and HPV Vaccination Knowledge and Attitudes among Medical Students in Alabama. J. Cancer Educ. Off. J. Am. Assoc. Cancer Educ. 2021, 36, 168–177. [Google Scholar] [CrossRef]
- Jolley, D.; Douglas, K.M. The effects of anti-vaccine conspiracy theories on vaccination intentions. PLoS ONE 2014, 9, e89177. [Google Scholar] [CrossRef]
- Romer, D.; Jamieson, K.H. Conspiracy theories as barriers to controlling the spread of COVID-19 in the U.S. Soc. Sci. Med. 2020, 263, 113356. [Google Scholar] [CrossRef] [PubMed]
- Soveri, A.; Karlsson, L.C.; Antfolk, J.; Lindfelt, M.; Lewandowsky, S. Unwillingness to engage in behaviors that protect against COVID-19: The role of conspiracy beliefs, trust, and endorsement of complementary and alternative medicine. BMC Public Health 2021, 21, 684. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, J.V.; Wyka, K.; White, T.M.; Picchio, C.A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Ratzan, S.C.; Kamarulzaman, A.; El-Mohandes, A. A survey of COVID-19 vaccine acceptance across 23 countries in 2022. Nat. Med. 2023, 29, 366–375. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control. Seasonal Influenza Vaccination and Antiviral Use in EU/EEA Member States—Overview of Vaccine Recommendations for 2017–2018 and Vaccination Coverage Rates for 2015–2016 and 2016–2017 Influenza Seasons; ECDC: Stockholm, Sweden, 2018; Available online: https://www.ecdc.europa.eu/sites/default/files/documents/seasonal-influenza-antiviral-use-2018.pdf (accessed on 21 February 2024).
- Jankowski, M.; Grudziąż-Sękowska, J.; Wrześniewska-Wal, I.; Tyszko, P.; Sękowski, K.; Ostrowski, J.; Gujski, M.; Pinkas, J. National HPV Vaccination Program in Poland-Public Awareness, Sources of Knowledge, and Willingness to Vaccinate Children against HPV. Vaccines 2023, 11, 1371. [Google Scholar] [CrossRef] [PubMed]
- Marques, M.D.; Douglas, K.M.; Jolley, D. Practical recommendations to communicate with patients about health-related conspiracy theories. Med. J. Aust. 2022, 216, 381–384. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, E.; Wright, M.; Oliphant, C.; Cleveland, K.; Holmes, J.; Nies, M.; Robinson, R. Patient-guided talking points to address COVID-19 and general vaccine hesitancy. Pharmacy 2022, 10, 137. [Google Scholar] [CrossRef] [PubMed]
- Alderotti, G.; Corvo, M.F.; Buscemi, P.; Stacchini, L.; Giorgetti, D.; Lorini, C.; Bonaccorsi, G.; Pinilla, M.J.C.; Lastrucci, V. Communicating with patients about COVID-19 vaccination: A qualitative study on vaccinators in Tuscany region, Italy. Vaccines 2023, 11, 223. [Google Scholar] [CrossRef] [PubMed]
- Zarobkiewicz, M.K.; Zimecka, A.; Zuzak, T.; Cieślak, D.; Roliński, J.; Grywalska, E. Vaccination among Polish University Students. Knowledge, Beliefs and Anti-Vaccination Attitudes. Hum. Vaccines Immunother. 2017, 13, 2654–2658. [Google Scholar] [CrossRef]
- Jankowska-Polańska, B.; Sarzyńska, K.; Czwojdziński, E.; Świątoniowska-Lonc, N.; Dudek, K.; Piwowar, A. Attitude of Health Care Workers and Medical Students towards Vaccination against COVID-19. Vaccines 2022, 10, 535. [Google Scholar] [CrossRef]
- Jastrzẹbska, A.; Saden, G.; Knysz, B.; Pondel, M.; Siennicka, A. The Relationship between Knowledge about the Pandemic and Willingness to Get Vaccinated against SARS-CoV-2 in Medical Students in Poland: A Cross-Sectional Survey. Front. Public Health 2022, 10, 914462. [Google Scholar] [CrossRef] [PubMed]
- University Ranking 2023. Available online: https://2023.ranking.perspektywy.org/ranking/university-ranking (accessed on 3 February 2024).
- Bruder, M.; Haffke, P.; Neave, N.; Nouripanah, N.; Imhoff, R. Measuring individual differences in generic beliefs in conspiracy theories across cultures: Conspiracy mentality questionnaire. Front. Psychol. 2013, 4, 225. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, G.K.; Holding, A.; Perez, S.; Amsel, R.; Rosberger, Z. Validation of the vaccine conspiracy beliefs scale. Papillomavirus Res. 2016, 2, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Eurostat; Brancato, G.; Macchia, S.; Murgia, M.; Signore, M.; Simeoni, G.; Blanke, K.; Körner, T.; Nimmergut, A.; Lima, P.; et al. The Handbook of Recommended Practices for Questionnaire Development and Testing in the European Statistical System. 2005. Available online: https://www.istat.it/it/files/2013/12/Handbook_questionnaire_development_2006.pdf (accessed on 24 January 2024).
- Sawicka-Gutaj, N.; Gruszczyński, D.; Guzik, P.; Mostowska, A.; Walkowiak, J. Publication ethics of human studies in the light of the Declaration of Helsinki—A mini-review. J. Med. Sci. 2022, 91, e700. [Google Scholar] [CrossRef]
- Agresti, A.; Franklin, C. The Art and Science of Learning from Data; Prentice Hall: Upper Saddle River, NJ, USA, 2007; Volume 2. [Google Scholar]
- Midi, H.; Sarkar, S.K.; Rana, S. Collinearity diagnostics of binary logistic regression model. J. Interdiscip. Math. 2010, 13, 253–267. [Google Scholar] [CrossRef]
- R_Core_Team. R: A language and environment for statistical computing. In R Foundation for Statistical Computing; The R Foundation: Vienna, Austria, 2021. [Google Scholar]
- Wickham, H.; Averick, M.; Bryan, J.; Chang, W.; McGowan, L.D.A.; François, R.; Grolemund, G.; Hayes, A.; Henry, L.; Hester, J. Welcome to the Tidyverse. J. Open Source Softw. 2019, 4, 1686. [Google Scholar] [CrossRef]
- Wickham, H.; Miller, E. haven: Import and Export ‘SPSS’, ‘Stata’ and ‘SAS’ Files. R Package Version 2.4.3. 2021. Available online: https://CRAN.R-project.org/package=haven (accessed on 4 February 2024).
- Wickham, H. ggplot2: Elegant Graphics for Data Analysis; Springer: New York, NY, USA, 2016. [Google Scholar]
- Ludecke, D. sjPlot: Data Visualization for Statistics in Social Science. R Package Version 2.8.9. 2021. Available online: https://CRAN.R-project.org/package=sjPlot (accessed on 4 February 2024).
- Gohel, D. Flextable: Functions for Tabular Reporting. R Package Version 0.6.10. 2021. Available online: https://CRAN.R-project.org/package=flextabl (accessed on 4 February 2024).
- Szmyd, B.; Bartoszek, A.; Karuga, F.F.; Staniecka, K.; Błaszczyk, M.; Radek, M. Medical Students and SARS-CoV-2 Vaccination: Attitude and Behaviors. Vaccines 2021, 9, 128. [Google Scholar] [CrossRef] [PubMed]
- Mavros, M.N.; Mitsikostas, P.K.; Kontopidis, I.G.; Moris, D.N.; Dimopoulos, G.; Falagas, M.E. H1N1v Influenza Vaccine in Greek Medical Students. Eur. J. Public Health 2011, 21, 329–332. [Google Scholar] [CrossRef] [PubMed]
- Depoux, A.; Martin, S.; Karafillakis, E.; Preet, R.; Wilder-Smith, A.; Larson, H. The pandemic of social media panic travels faster than the COVID-19 outbreak. J. Travel Med. 2020, 27, taaa031. [Google Scholar] [CrossRef] [PubMed]
- Cinelli, M.; Quattrociocchi, W.; Galeazzi, A.; Valensise, C.M.; Brugnoli, E.; Schmidt, A.L.; Zola, P.; Zollo, F.; Scala, A. The COVID-19 social media infodemic. Sci. Rep. 2020, 10, 16598. [Google Scholar] [CrossRef]
- Rosenberg, H.; Syed, S.; Rezaie, S. The Twitter pandemic: The critical role of Twitter in the dissemination of medical information and misinformation during the COVID-19 pandemic. CJEM 2020, 22, 418–421. [Google Scholar] [CrossRef] [PubMed]
- The Lancet Infectious Diseases. The COVID-19 infodemic. Lancet Infect. 2020, 20, 875. [Google Scholar] [CrossRef] [PubMed]
- Seddig, D.; Maskileyson, D.; Davidov, E.; Ajzen, I.; Schmidt, P. Correlates of COVID-19 Vaccination Intentions: Attitudes, Institutional Trust, Fear, Conspiracy Beliefs, and Vaccine Skepticism. Soc. Sci. Med. 2022, 302, 114981. [Google Scholar] [CrossRef] [PubMed]
- van Prooijen, J.-W.; Etienne, T.W.; Kutiyski, Y.; Krouwel, A.P.M. Conspiracy Beliefs Prospectively Predict Health Behavior and Well-Being during a Pandemic. Psychol. Med. 2023, 53, 2514–2521. [Google Scholar] [CrossRef] [PubMed]
- Simione, L.; Vagni, M.; Gnagnarella, C.; Bersani, G.; Pajardi, D. Mistrust and Beliefs in Conspiracy Theories Differently Mediate the Effects of Psychological Factors on Propensity for COVID-19 Vaccine. Front. Psychol. 2021, 12, 683684. [Google Scholar] [CrossRef] [PubMed]
- Roozenbeek, J.; Schneider, C.R.; Dryhurst, S.; Kerr, J.; Freeman, A.L.J.; Recchia, G.; van der Bles, A.M.; van der Linden, S. Susceptibility to Misinformation about COVID-19 around the World. R. Soc. Open Sci. 2020, 7, 201199. [Google Scholar] [CrossRef]
- Sule, S.; DaCosta, M.C.; DeCou, E.; Gilson, C.; Wallace, K.; Goff, S.L. Communication of COVID-19 Misinformation on Social Media by Physicians in the US. JAMA Netw. Open 2023, 6, e2328928. [Google Scholar] [CrossRef] [PubMed]
- Walkowiak, M.P.; Walkowiak, J.B.; Walkowiak, D. More Time, Carrot-and-Stick, or Piling Coffins? Estimating the Role of Factors Overcoming COVID-19 Vaccine Hesitancy in Poland and Lithuania in the Years 2021–2022. Vaccines 2022, 10, 1523. [Google Scholar] [CrossRef] [PubMed]
- Kowalska-Duplaga, K.; Duplaga, M. The Association of Conspiracy Beliefs and the Uptake of COVID-19 Vaccination: A Cross-Sectional Study. BMC Public Health 2023, 23, 672. [Google Scholar] [CrossRef] [PubMed]
- Oleksy, T.; Wnuk, A.; Gambin, M.; Łyś, A.; Bargiel-Matusiewicz, K.; Pisula, E. Barriers and Facilitators of Willingness to Vaccinate against COVID-19: Role of Prosociality, Authoritarianism and Conspiracy Mentality. A Four-Wave Longitudinal Study. Personal. Individ. Differ. 2022, 190, 111524. [Google Scholar] [CrossRef]
- Regazzi, L.; Lontano, A.; Cadeddu, C.; Di Padova, P.; Rosano, A. Conspiracy Beliefs, COVID-19 Vaccine Uptake and Adherence to Public Health Interventions during the Pandemic in Europe. Eur. J. Public Health 2023, 33, 717–724. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, J.B.; Bell, R.A. Predictors of Intention to Vaccinate against COVID-19: Results of a Nationwide Survey. Vaccine 2021, 39, 1080–1086. [Google Scholar] [CrossRef] [PubMed]
- Haakonsen, J.M.F.; Furnham, A. COVID-19 Vaccination: Conspiracy Theories, Demography, Ideology, and Personality Disorders. Health Psychol. Off. J. Div. Health Psychol. Am. Psychol. Assoc. 2023, 42, 205–212. [Google Scholar] [CrossRef]
- Lo Moro, G.; Cugudda, E.; Bert, F.; Raco, I.; Siliquini, R. Vaccine Hesitancy and Fear of COVID-19 Among Italian Medical Students: A Cross-Sectional Study. J. Community Health 2022, 47, 475–483. [Google Scholar] [CrossRef] [PubMed]
- Jamison, A.M.; Broniatowski, D.A.; Dredze, M.; Sangraula, A.; Smith, M.C.; Quinn, S.C. Not Just Conspiracy Theories: Vaccine Opponents and Proponents Add to the COVID-19 “infodemic” on Twitter. Harv. Kennedy Sch. Misinf. Rev. 2020, 1, 10.37016/mr-2020-38. [Google Scholar] [CrossRef]
- Broniatowski, D.A.; Jamison, A.M.; Qi, S.; AlKulaib, L.; Chen, T.; Benton, A.; Quinn, S.C.; Dredze, M. Weaponized Health Communication: Twitter Bots and Russian Trolls Amplify the Vaccine Debate. Am. J. Public Health 2018, 108, 1378–1384. [Google Scholar] [CrossRef] [PubMed]
- Walter, D.; Ophir, Y.; Jamieson, K.H. Russian Twitter Accounts and the Partisan Polarization of Vaccine Discourse, 2015–2017. Am. J. Public Health 2020, 110, 718–724. [Google Scholar] [CrossRef] [PubMed]
- Karami, A.; Lundy, M.; Webb, F.; Turner-McGrievy, G.; McKeever, B.W.; McKeever, R. Identifying and Analyzing Health-related themes in disinformation shared by conservative and liberal Russian trolls on Twitter. Int. J. Environ. Res. Public Health 2021, 18, 2159. [Google Scholar] [CrossRef]
- Warner, E.L.; Barbati, J.L.; Duncan, K.L.; Yan, K.; Rains, S.A. Vaccine misinformation types and properties in Russian troll tweets. Vaccine 2022, 40, 953–960. [Google Scholar] [CrossRef]
- Yan, K.; Barbati, J.L.; Duncan, K.L.; Warner, E.L.; Rains, S.A. Russian troll vaccine misinformation dissemination on Twitter: The role of political partisanship. Health Commun. 2023, 38, 1591–1600. [Google Scholar] [CrossRef]
- Habib, S.S.; Alamri, M.S.; Alkhedr, M.M.; Alkhorijah, M.A.; Jabaan, R.D.; Alanzi, M.K. Knowledge and Attitudes of Medical Students toward COVID-19 Vaccine in Saudi Arabia. Vaccines 2022, 10, 541. [Google Scholar] [CrossRef] [PubMed]
- Kondo, A.; Abuliezi, R.; Ota, E.; Oki, T.; Naruse, K. Cross-Sectional Study of Factors Related to COVID-19 Vaccination Uptake among University Healthcare Students. Front. Public Health 2023, 11, 1325942. [Google Scholar] [CrossRef] [PubMed]
- Baessler, F.; Zafar, A.; Mengler, K.; Natus, R.N.; Dutt, A.J.; Kuhlmann, M.; Çinkaya, E.; Hennes, S. A Needs-Based Analysis of Teaching on Vaccinations and COVID-19 in German Medical Schools. Vaccines 2022, 10, 975. [Google Scholar] [CrossRef] [PubMed]
- Lo Moro, G.; Scaioli, G.; Bert, F.; Zacchero, A.L.; Minutiello, E.; Siliquini, R. Exploring the Relationship between COVID-19 Vaccine Refusal and Belief in Fake News and Conspiracy Theories: A Nationwide Cross-Sectional Study in Italy. Int. J. Environ. Res. Public Health 2022, 19, 9350. [Google Scholar] [CrossRef] [PubMed]
- Jamil, O.B.K.; Muhib, M.; Abbal, M.A.; Ahmed, A.M.; Khan, H.H.; Khan, N.Y. Medical Students in Karachi and COVID-19: Myths and Facts. SAGE Open Med. 2022, 10, 20503121221094208. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, A.; Catalan-Matamoros, D. Anti-vaccine discourse on social media: An exploratory audit of negative tweets about vaccines and their posters. Vaccines 2022, 10, 2067. [Google Scholar] [CrossRef] [PubMed]
- Wilson, S.L.; Wiysonge, C. Social media and vaccine hesitancy. BMJ Glob. Health 2020, 5, e004206. [Google Scholar] [CrossRef]
- Jennings, W.; Stoker, G.; Bunting, H.; Valgarðsson, V.O.; Gaskell, J.; Devine, D.; McKay, L.; Mills, M.C. Lack of trust, conspiracy beliefs, and social media use predict COVID-19 vaccine hesitancy. Vaccines 2021, 9, 593. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Total (n = 411) |
|---|---|
| Sex: | |
| Female | 270 (65.7%) |
| Male | 139 (33.8%) |
| Did not answer | 2 (0.5%) |
| Year of study | |
| 1st–2nd year | 235 (57.2%) |
| 3rd–5th year | 176 (42.8%) |
| Domicile: | |
| Up to 10,000 inhabitants | 90 (21.9%) |
| 10,000–100,000 inhabitants | 95 (23.1%) |
| 100,000–500,000 inhabitants | 58 (14.1%) |
| More than 500,000 inhabitants | 168 (40.9%) |
| Role of religion in life | |
| Important | 115 (28.0%) |
| Few | 122 (29.7%) |
| None | 174 (42.3%) |
| Being hospitalized within the past five years | |
| Yes | 89 (21.7%) |
| No | 322 (78.3%) |
| Suffering from any kind of chronic disease | |
| Yes | 137 (33.3%) |
| No | 274 (66.7%) |
| Blood donation | |
| Yes | 96 (23.4%) |
| No | 315 (76.6%) |
| Declaration of marrow donation | |
| Yes | 114 (27.7%) |
| No | 297 (72.3%) |
| Vaccination against COVID-19 | |
| Yes | 402 (97.8%) |
| No | 9 (2.2%) |
| Getting the flu vaccination | |
| Yes | 172 (41.8%) |
| No | 239 (58.2%) |
| Left–right orientation (political attitudes) | |
| Left | 211 (51.3%) |
| Centre | 147 (35.8%) |
| Right | 53 (12.9%) |
| Liberal–conservative orientation (worldview beliefs) | |
| Liberal | 283 (68.9%) |
| Centre | 80 (19.5%) |
| Conservative | 48 (11.7%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Domaradzki, J.; Jabkowski, P.; Walkowiak, D. Investigating Beliefs in Anti-Vax Conspiracy Theories among Medical Students. Vaccines 2024, 12, 359. https://doi.org/10.3390/vaccines12040359
Domaradzki J, Jabkowski P, Walkowiak D. Investigating Beliefs in Anti-Vax Conspiracy Theories among Medical Students. Vaccines. 2024; 12(4):359. https://doi.org/10.3390/vaccines12040359
Chicago/Turabian StyleDomaradzki, Jan, Piotr Jabkowski, and Dariusz Walkowiak. 2024. "Investigating Beliefs in Anti-Vax Conspiracy Theories among Medical Students" Vaccines 12, no. 4: 359. https://doi.org/10.3390/vaccines12040359
APA StyleDomaradzki, J., Jabkowski, P., & Walkowiak, D. (2024). Investigating Beliefs in Anti-Vax Conspiracy Theories among Medical Students. Vaccines, 12(4), 359. https://doi.org/10.3390/vaccines12040359






