MDCK-Adaptive Mutation of A169S Changes Glycosylation Pattern of Hemagglutinin and Enhances MDCK-Based H7N9 Vaccine Virus Production without Loss of Antigenicity and Immunogenicity
Abstract
1. Introduction
2. Materials and Methods
2.1. Passage Vaccine Virus in the MDCK Serum-Free System
2.2. Gene Sequencing
2.3. Plaque Assay
2.4. Generation of Recombinant Viruses
2.5. Virus Digestion Procedure
2.6. Deglycosylation of Virus Digested with PNGase F
2.7. Mass Spectrometry Characterization
2.8. Flow Cytometry Analysis
2.9. Real-Time Polymerase Chain Reaction
2.10. Mouse Immunization
2.11. Hemagglutination Inhibition Assay
2.12. Neutralization Assay
2.13. Statistical Analysis
3. Results
3.1. Characteration of the MDCK-Adapted Vaccine Virus
3.2. A169S Substitution Improved the Growth Property of the Recombinant Virus in MDCK
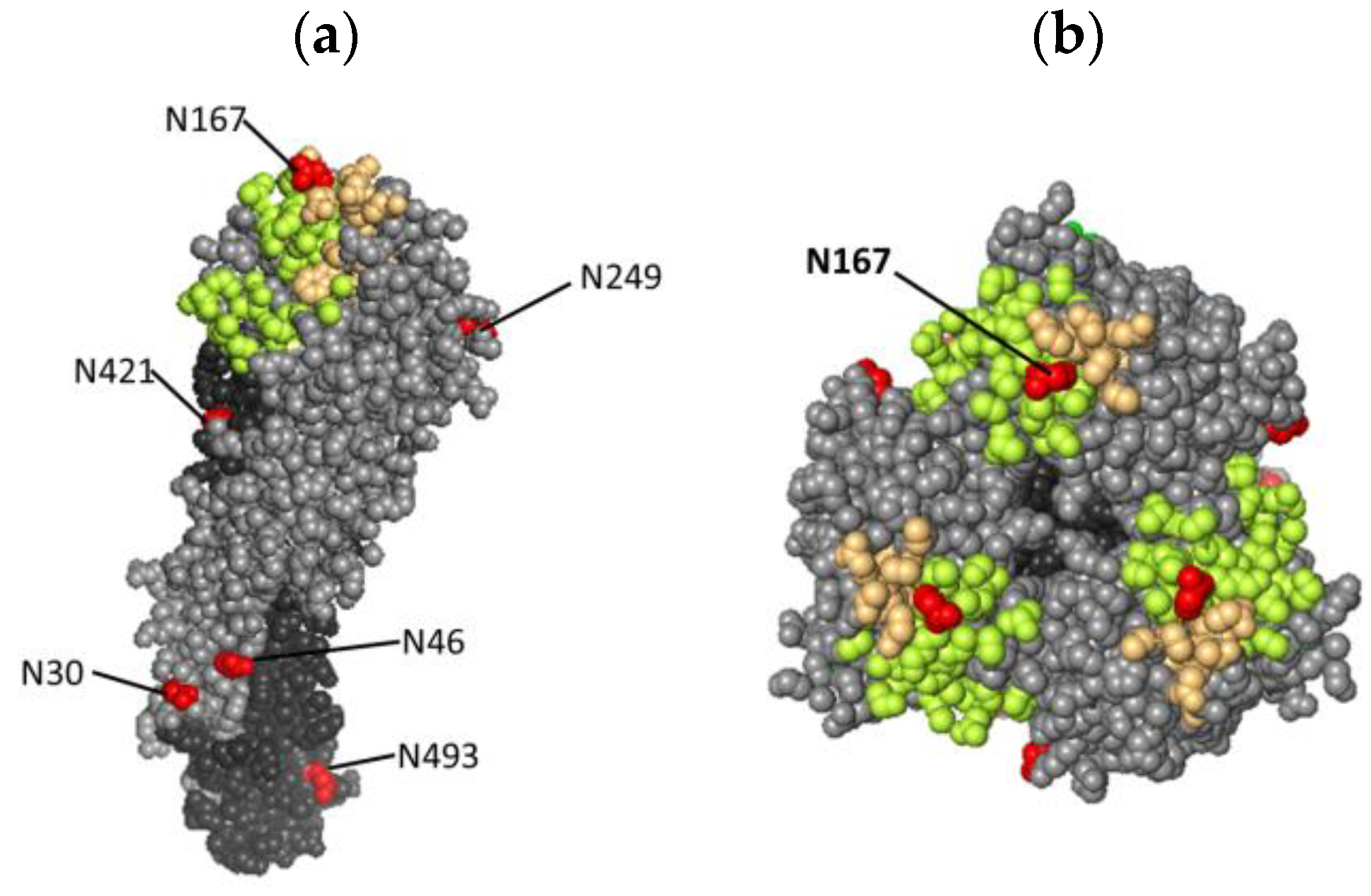
3.3. The A169S Substition Results in a New Glycosylation Site at N167 in Viral HA Protein
3.4. Analysis of the Effect of N167 Glycan on Virus Infection to MDCK Cells
3.5. Evaluating the Antigenicity and Immunogenicity of Vaccine Viruses
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- Parry, J. H7N9 avian flu infects humans for the first time. BMJ 2013, 346, f2151. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; Lam, T.T.; Smith, D.K.; Guan, Y. Emergence and development of H7N9 influenza viruses in China. Curr. Opin. Virol. 2016, 16, 106–113. [Google Scholar] [CrossRef] [PubMed]
- Food and Agriculture Organization. Available online: https://www.fao.org/ag/againfo/programmes/en/empres/h7n9/situation_update.html (accessed on 1 June 2022).
- Quan, C.; Shi, W.; Yang, Y.; Yang, Y.; Liu, X.; Xu, W.; Li, H.; Li, J.; Wang, Q.; Tong, Z.; et al. New Threats from H7N9 Influenza Virus: Spread and Evolution of High- and Low-Pathogenicity Variants with High Genomic Diversity in Wave Five. J. Virol. 2018, 92, e00301-18. [Google Scholar] [CrossRef] [PubMed]
- Parrish, C.R.; Murcia, P.R.; Holmes, E.C. Influenza virus reservoirs and intermediate hosts: Dogs, horses, and new possibilities for influenza virus exposure of humans. J. Virol. 2015, 89, 2990–2994. [Google Scholar] [CrossRef] [PubMed]
- Trock, S.C.; Burke, S.A.; Cox, N.J. Development of Framework for Assessing Influenza Virus Pandemic Risk. Emerg. Infect. Dis. 2015, 21, 1372–1378. [Google Scholar] [CrossRef] [PubMed]
- Rappuoli, R.; Pizza, M.; Del Giudice, G.; De Gregorio, E. Vaccines, new opportunities for a new society. Proc. Natl. Acad. Sci. USA 2014, 111, 12288–12293. [Google Scholar] [CrossRef] [PubMed]
- Pérez Rubio, A.; Eiros, J.M. Cell culture-derived flu vaccine: Present and future. Hum. Vaccines Immunother. 2018, 14, 1874–1882. [Google Scholar] [CrossRef] [PubMed]
- Lubiniecki, A.S. Historical reflections on cell culture engineering. Cytotechnology 1998, 28, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Merten, O.W.; Hannoun, C.; Manuguerra, J.C.; Ventre, F.; Petres, S. Production of influenza virus in cell cultures for vaccine preparation. Adv. Exp. Med. Biol. 1996, 397, 141–151. [Google Scholar]
- Onions, D.; Egan, W.; Jarrett, R.; Novicki, D.; Gregersen, J.P. Validation of the safety of MDCK cells as a substrate for the production of a cell-derived influenza vaccine. Biologicals 2010, 38, 544–551. [Google Scholar] [CrossRef]
- Montomoli, E.; Khadang, B.; Piccirella, S.; Trombetta, C.; Mennitto, E.; Manini, I.; Stanzani, V.; Lapini, G. Cell culture-derived influenza vaccines from Vero cells: A new horizon for vaccine production. Expert Rev. Vaccines 2012, 11, 587–594. [Google Scholar] [CrossRef]
- Donis, R.O.; Davis, C.T.; Foust, A.; Hossain, M.J.; Johnson, A.; Klimov, A.; Loughlin, R.; Xu, X.; Tsai, T.; Blayer, S.; et al. Performance characteristics of qualified cell lines for isolation and propagation of influenza viruses for vaccine manufacturing. Vaccine 2014, 32, 6583–6590. [Google Scholar] [CrossRef]
- Kistner, O.; Barrett, P.N.; Mundt, W.; Reiter, M.; Schober-Bendixen, S.; Eder, G.; Dorner, F. Development of a Vero cell-derived influenza whole virus vaccine. Dev. Biol. Stand. 1999, 98, 101–110. [Google Scholar]
- de Graaf, M.; Fouchier, R.A. Role of receptor binding specificity in influenza A virus transmission and pathogenesis. EMBO J. 2014, 33, 823–841. [Google Scholar] [CrossRef]
- Tseng, Y.F.; Hu, A.Y.; Huang, M.L.; Yeh, W.Z.; Weng, T.C.; Chen, Y.S.; Chong, P.; Lee, M.S. Adaptation of high-growth influenza H5N1 vaccine virus in Vero cells: Implications for pandemic preparedness. PLoS ONE 2011, 6, e24057. [Google Scholar] [CrossRef]
- Chang, P.; Sealy, J.E.; Sadeyen, J.R.; Bhat, S.; Lukosaityte, D.; Sun, Y.; Iqbal, M. Immune Escape Adaptive Mutations in the H7N9 Avian Influenza Hemagglutinin Protein Increase Virus Replication Fitness and Decrease Pandemic Potential. J. Virol. 2020, 94, e00216-20. [Google Scholar] [CrossRef] [PubMed]
- Wagner, R.; Wolff, T.; Herwig, A.; Pleschka, S.; Klenk, H.D. Interdependence of hemagglutinin glycosylation and neuraminidase as regulators of influenza virus growth: A study by reverse genetics. J. Virol. 2000, 74, 6316–6323. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Kong, D.; Hu, X.; Gao, Y.; Lin, S.; Liao, M.; Fan, H. Influenza H7N9 Virus Hemagglutinin with T169A Mutation Possesses Enhanced Thermostability and Provides Effective Immune Protection against Lethal H7N9 Virus Challenge in Chickens. Vaccines 2023, 11, 1318. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Baz, M.; Lu, J.; Paskel, M.; Santos, C.; Subbarao, K.; Jin, H.; Matsuoka, Y. Development of a high-yield live attenuated H7N9 influenza virus vaccine that provides protection against homologous and heterologous H7 wild-type viruses in ferrets. J. Virol. 2014, 88, 7016–7023. [Google Scholar] [CrossRef] [PubMed]
- Zhao, D.; Liang, L.; Wang, S.; Nakao, T.; Li, Y.; Liu, L.; Guan, Y.; Fukuyama, S.; Bu, Z.; Kawaoka, Y.; et al. Glycosylation of the Hemagglutinin Protein of H5N1 Influenza Virus Increases Its Virulence in Mice by Exacerbating the Host Immune Response. J. Virol. 2017, 91, e02215-16. [Google Scholar] [CrossRef]
- Chia, M.Y.; Hu, A.Y.; Tseng, Y.F.; Weng, T.C.; Lai, C.C.; Lin, J.Y.; Chen, P.L.; Wang, Y.F.; Chao, S.R.; Chang, J.Y.; et al. Evaluation of MDCK cell-derived influenza H7N9 vaccine candidates in ferrets. PLoS ONE 2015, 10, e0120793. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO Manual on Animal Influenza Diagnosis and Surveillance; WHO: Geneva, Switzerland, 2002. [Google Scholar]
- Hoffmann, E.; Stech, J.; Guan, Y.; Webster, R.G.; Perez, D.R. Universal primer set for the full-length amplification of all influenza A viruses. Arch. Virol. 2001, 146, 2275–2289. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.L.; Tzeng, T.T.; Hu, A.Y.; Wang, L.H.; Lee, M.S. Development and Evaluation of Vero Cell-Derived Master Donor Viruses for Influenza Pandemic Preparedness. Vaccines 2020, 8, 626. [Google Scholar] [CrossRef]
- Khatri, K.; Klein, J.A.; White, M.R.; Grant, O.C.; Leymarie, N.; Woods, R.J.; Hartshorn, K.L.; Zaia, J. Integrated Omics and Computational Glycobiology Reveal Structural Basis for Influenza A Virus Glycan Microheterogeneity and Host Interactions. Mol. Cell Proteom. 2016, 15, 1895–1912. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.J.; Wu, S.L.; Love, K.R.; Hancock, W.S. Characterization of Site-Specific Glycosylation in Influenza A Virus Hemagglutinin Produced by Spodoptera frugiperda Insect Cell Line. Anal. Chem. 2017, 89, 11036–11043. [Google Scholar] [CrossRef]
- Huang, H.W.; Liu, B.S.; Chien, K.Y.; Chiang, L.C.; Huang, S.Y.; Sung, W.C.; Wu, W.G. Cobra venom proteome and glycome determined from individual snakes of Naja atra reveal medically important dynamic range and systematic geographic variation. J. Proteom. 2015, 128, 92–104. [Google Scholar] [CrossRef]
- Schulze-Horsel, J.; Genzel, Y.; Reichl, U. Flow cytometric monitoring of influenza A virus infection in MDCK cells during vaccine production. BMC Biotechnol. 2008, 8, 45. [Google Scholar] [CrossRef]
- Kawakami, E.; Watanabe, T.; Fujii, K.; Goto, H.; Watanabe, S.; Noda, T.; Kawaoka, Y. Strand-specific real-time RT-PCR for distinguishing influenza vRNA, cRNA, and mRNA. J. Virol. Methods 2011, 173, 1–6. [Google Scholar] [CrossRef]
- Wood, J.M.; Schild, G.C.; Newman, R.W.; Seagroatt, V. An improved single-radial-immunodiffusion technique for the assay of influenza haemagglutinin antigen: Application for potency determinations of inactivated whole virus and subunit vaccines. J. Biol. Stand. 1977, 5, 237–247. [Google Scholar] [CrossRef] [PubMed]
- Dou, D.; Revol, R.; Östbye, H.; Wang, H.; Daniels, R. Influenza A Virus Cell Entry, Replication, Virion Assembly and Movement. Front. Immunol. 2018, 20, 1581. [Google Scholar] [CrossRef] [PubMed]
- Ohuchi, M.; Ohuchi, R.; Feldmann, A.; Klenk, H.D. Regulation of receptor binding affinity of influenza virus hemagglutinin by its carbohydrate moiety. J. Virol. 1997, 71, 8377–8384. [Google Scholar] [CrossRef] [PubMed]
- Chang, P.; Sealy, J.E.; Sadeyen, J.R.; Iqbal, M. Amino Acid Residue 217 in the Hemagglutinin Glycoprotein Is a Key Mediator of Avian Influenza H7N9 Virus Antigenicity. J. Virol. 2019, 93, e01627-18. [Google Scholar] [CrossRef] [PubMed]
- Tzeng, T.T.; Chen, P.L.; Weng, T.C.; Tsai, S.Y.; Lai, C.C.; Chou, H.I.; Chen, P.W.; Lu, C.C.; Liu, M.T.; Sung, W.C.; et al. Development of high-growth influenza H7N9 prepandemic candidate vaccine viruses in suspension MDCK cells. J. Biomed. Sci. 2020, 27, 4737. [Google Scholar] [CrossRef] [PubMed]
- Jang, H.; Ross, T.M. Hemagglutination Inhibition (HAI) antibody landscapes after vaccination with H7Nx virus like particles. PLoS ONE 2021, 16, e0246613. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Ye, H.; Li, H.; Ma, K.; Qiu, W.; Chen, Y.; Qiu, Z.; Li, B.; Jia, W.; Liang, Z.; et al. Evolution and Antigenic Drift of Influenza A (H7N9) Viruses, China, 2017–2019. Emerg. Infect. Dis. 2020, 26, 1906–1911. [Google Scholar] [CrossRef]
- Tzeng, T.T.; Chai, K.M.; Chen, I.H.; Chang, R.Y.; Chiang, J.R.; Liu, S.J. A TLR9 agonist synergistically enhances protective immunity induced by an Alum-adjuvanted H7N9 inactivated whole-virion vaccine. Emerg. Microbes Infect. 2023, 12, 2249130. [Google Scholar] [CrossRef]
- WHO. Antigenic and genetic characteristics of zoonotic influenza A viruses and development of candidate vaccine viruses for pandemic preparedness. Wkly. Epidemiol. Rec. 2019, 94, 485–495. [Google Scholar]
- Bahl, K.; Senn, J.J.; Yuzhakov, O.; Bulychev, A.; Brito, L.A.; Hassett, K.J.; Laska, M.E.; Smith, M.; Almarsson, Ö.; Thompson, J.; et al. Preclinical and Clinical Demonstration of Immunogenicity by mRNA Vaccines against H10N8 and H7N9 Influenza Viruses. Mol. Ther. 2017, 25, 1316–1327. [Google Scholar] [CrossRef]



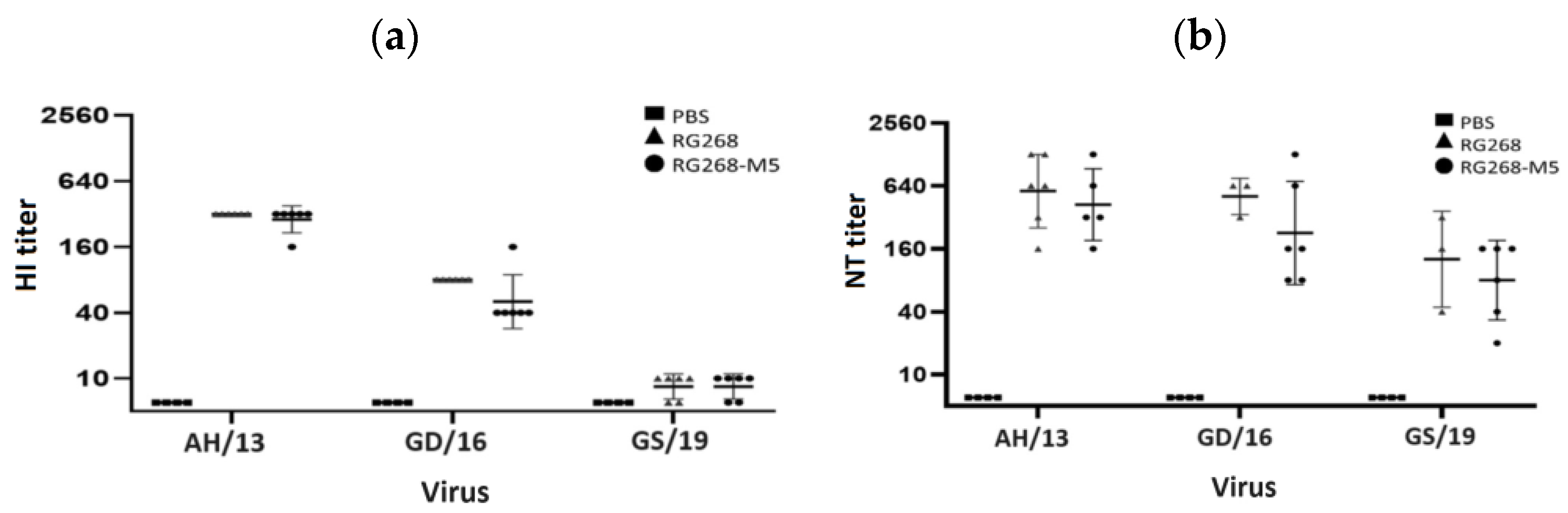
| CVV | HA Mutation Site (aa 167–169) a | Glycosylation (aa 167) | HI Titer Antiserum | |
|---|---|---|---|---|
| 13/180 | 15/248 | |||
| RG268 | NAA | No | 640 | 1280 |
| RG268-M5 | NAS | Yes | 640 | 1280 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, P.-L.; Weng, T.-C.; Lai, C.-C.; Tzeng, T.-T.; Lin, M.-H.; Hu, K.-C.; Hu, A.Y.-C.; Lee, M.-S.; Sung, W.-C. MDCK-Adaptive Mutation of A169S Changes Glycosylation Pattern of Hemagglutinin and Enhances MDCK-Based H7N9 Vaccine Virus Production without Loss of Antigenicity and Immunogenicity. Vaccines 2024, 12, 291. https://doi.org/10.3390/vaccines12030291
Chen P-L, Weng T-C, Lai C-C, Tzeng T-T, Lin M-H, Hu K-C, Hu AY-C, Lee M-S, Sung W-C. MDCK-Adaptive Mutation of A169S Changes Glycosylation Pattern of Hemagglutinin and Enhances MDCK-Based H7N9 Vaccine Virus Production without Loss of Antigenicity and Immunogenicity. Vaccines. 2024; 12(3):291. https://doi.org/10.3390/vaccines12030291
Chicago/Turabian StyleChen, Po-Ling, Tsai-Chuan Weng, Chia-Chun Lai, Tsai-Teng Tzeng, Min-Han Lin, Kai-Chieh Hu, Alan Yung-Chih Hu, Min-Shi Lee, and Wang-Chou Sung. 2024. "MDCK-Adaptive Mutation of A169S Changes Glycosylation Pattern of Hemagglutinin and Enhances MDCK-Based H7N9 Vaccine Virus Production without Loss of Antigenicity and Immunogenicity" Vaccines 12, no. 3: 291. https://doi.org/10.3390/vaccines12030291
APA StyleChen, P.-L., Weng, T.-C., Lai, C.-C., Tzeng, T.-T., Lin, M.-H., Hu, K.-C., Hu, A. Y.-C., Lee, M.-S., & Sung, W.-C. (2024). MDCK-Adaptive Mutation of A169S Changes Glycosylation Pattern of Hemagglutinin and Enhances MDCK-Based H7N9 Vaccine Virus Production without Loss of Antigenicity and Immunogenicity. Vaccines, 12(3), 291. https://doi.org/10.3390/vaccines12030291






