Abstract
Herpes zoster, induced by the reactivation of the varicella-zoster virus (VZV), is a unilaterally distributed vesicular rash that can cause multiple complications. VZV not only causes neurological problems, including postherpetic neuralgia and ocular zoster, but also causes inflammatory vasculopathy and increases the incidence of hemorrhagic or ischemic complications. Therefore, understanding the association between the development of herpes zoster and the subsequent occurrence of acute stroke or cardiovascular diseases, including myocardial infarction and heart failure, is of great interest. Conversely, many risk factors are involved in the development of herpes zoster. Recently, it has become clear that aging, insufficient immune function, and diseases related to lifestyle habits (for example, stroke and cardiovascular disease), can trigger the onset of herpes zoster. Preventing the onset of herpes zoster, which substantially reduces quality of life, will lead to lower medical costs for countries and extend healthy life expectancy for general populations. Thus, because herpes zoster is a vaccine-preventable disease, active vaccination is recommended for high-risk groups. This review summarizes the association between herpes zoster and cardiovascular disease and vaccination against herpes zoster as a useful disease management and prevention measure for cardiovascular disease.
1. Introduction
Varicella-zoster virus (VZV) causes chickenpox (varicella), usually in childhood, and becomes latent in the neurons of the cranial and spinal ganglia of nearly all individuals after the chickenpox resolves. Herpes zoster, commonly known as shingles, is a viral disease caused by the reactivation of latent VZV residing in the sensory ganglia and dorsal roots after primary infection, especially in older adults and immunocompromised individuals. It primarily manifests as a painful skin rash and blisters occurring in specific dermatomes (areas along nerves), which are called “zoster” herpes. Herpes zoster represents a significant health concern for the general population [1] because postherpetic neuralgia has a negative impact on quality of life [2]. The overall lifetime risk of herpes zoster is 32.2% [3], and postherpetic neuralgia affects 13–25% of patients with herpes zoster [4].
Recently, the global incidence of herpes zoster has increased; however, the cause remains unknown [4,5,6,7]. Furthermore, in Japan’s aging society, there is a high possibility that the incidence of not only herpes zoster but also chickenpox among older people will increase as cell-mediated immunity specific to VZV declines with age [4,5,8,9,10].
Humans are the only natural hosts for VZV, complicating efforts to understand the pathophysiology of VZV-associated vasculopathy [11]. In postmortem analyses, the cerebral arteries have been observed to contain VZV DNA and VZV-specific antigens, supporting the hypothesis that vasculitis is caused by VZV [12]. The incidence of herpes zoster is increasing with age; the incidence was found to be 10.9 cases per 1000 patient-years in people and was significantly higher in women than in men [13]. Several studies have unequivocally demonstrated that the occurrence of herpes zoster rises with advancing age [14].
The preferred site of herpes zoster is the intercostal nerves, with the next most common site being the ophthalmic division of the trigeminal nerve [15]. Additionally, the seventh cranial nerve may be the site of VZV reactivation. In this review, we summarize the association between herpes zoster and cardiovascular disease and the relevant disease management and prevention measures, including vaccination, for cardiovascular disease.
2. Risk Factors for Herpes Zoster
The risk factors that promote the reactivation of herpes zoster include a weakened immune system, advanced aging, and stress [16]. Because herpes zoster develops in immunocompromised patients or those with comorbid conditions or chronic diseases, insufficient immunological protection may increase the risk of severe complications [17].
2.1. Literature Search Results for Cardiovascular Disease and Herpes Zoster
The keywords “cardiovascular disease”, “herpes zoster”, “heart failure”, and “myocardial infarction” were searched in PubMed. The research time frame for the database was until December 2023. The language was limited to English. The titles and abstracts of all potentially relevant articles were read to determine their relevance. Full articles were also scrutinized if the titles and abstracts were unclear. Reference lists of identified articles were screened to ensure the completeness of the search.
As depicted in Figure 1, a total of 38 studies underwent title and abstract screening, with 5 studies excluded due to duplication. A total of 2 studies were excluded because they focused on COVID-19 vaccines, and 6 studies were associated with research on the differential diagnoses of chest pain. Subsequently, out of the 13 studies not meeting the eligibility criteria for a full-text review, 7 reports were excluded due to being review articles or guideline-related articles, while 9 reports were included in the review. Figure 1 illustrates a flowchart outlining the selection process.
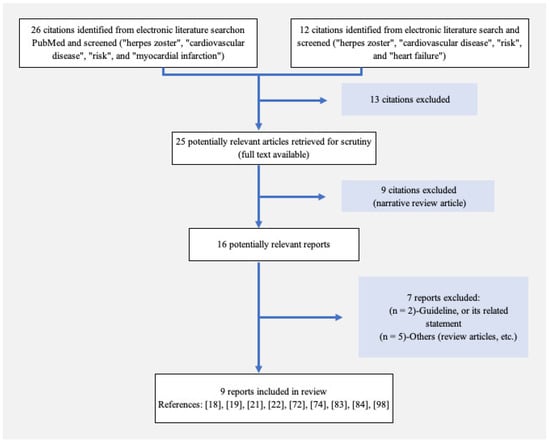
Figure 1.
A flowchart depicting the selection process. A total of 25 studies were imported for title and abstract screening after removing duplicates or determining ineligibility. Following a comprehensive full-text review, 16 studies were deemed eligible, and 9 reports were ultimately included in the review.
2.2. Cardiovascular Diseases as Risk Factors for Herpes Zoster
In a large cohort study involving 25,209 patients diagnosed with herpes zoster during the study period, dyslipidemia and prior myocardial infarction were significant risk factors, whereas diabetes mellitus, hypertension, prior stroke, and smoking were not [18]. In a Japanese cohort study using the Diagnosis Procedure Combination (DPC) database, age ≥ 75 years, diabetes mellitus, dyslipidemia, hyperuricemia, hypertension, heart failure, and glucocorticoid administration were associated with increased risks of herpes zoster onset in patients hospitalized for cerebrovascular and cardiovascular events [19]. In a Korean nationwide cohort study, comorbidities including hematologic malignancies, hypertension, diabetes mellitus, and chronic lung and liver disease increased the risk of herpes zoster in patients with rheumatic disease [20]. The risk factors for herpes zoster appear to vary across different populations and health conditions. While dyslipidemia and prior myocardial infarction stood out as significant contributors in one study, the Japanese and Korean cohorts highlighted the importance of age, various comorbidities, and medication administration. These nuanced insights emphasize the need for a comprehensive understanding of the diverse factors influencing herpes zoster risk, enabling more tailored preventive strategies in clinical practice.
A population-based study in Taiwan revealed that patients with heart failure, especially men, may have an increased risk of herpes zoster [21]. According to a nationwide population-based case–control study in Korea, patients with an episode of myocardial infarction (hazard ratio [HR] 1.625, 95% confidence interval [CI] 1.144–2.308), ischemic stroke (HR 1.518, 95% CI 1.177–1.957), or heart failure (HR 1.485, 95% CI 1.041–2.117) were at increased risk of hospitalization for herpes zoster [22]. These findings emphasize the complex relationship between cardiovascular events and the susceptibility to herpes zoster. Individuals with heart failure, ischemic heart disease, stroke, or other cardiovascular diseases, as well as those with a history of such conditions, not only face an elevated risk of developing herpes zoster but are also more likely to be hospitalized due to the exacerbation of either herpes zoster or cardiovascular diseases.
2.3. Diabetes
Diabetes mellitus was associated with an increased risk of herpes zoster in a multivariate analysis [23,24,25,26]. Patients with poor glycemic control, with a mean HbA1c of 10.7%, had a higher risk of developing herpes zoster (HR 1.44, 95% CI 1.26–1.64) [26]. However, even after experiencing hyperglycemia, the risk of developing shingles has been shown to be low if adequate blood sugar control is achieved through treatment. Therefore, the prompt initiation of hyperglycemic control is essential, and achieving optimal glycemic control early contributes to the prevention of shingles. Proactive measures, including regular monitoring and timely adjustments to treatment plans, may play a pivotal role in reducing the overall burden of herpes zoster in patients with diabetes.

Table 1.
Risk factors for herpes zoster.
Table 1.
Risk factors for herpes zoster.
| Risks [Reference] | Results (Country; Herpes Zoster Cases) | Subgroups | HR (95% CI) |
|---|---|---|---|
| Cardiovascular diseases [22] | Cardiovascular diseases increase the risk of herpes zoster hospitalization (Korea; 20,311) | Myocardial infarction | 1.625 (1.144–2.308) |
| Stroke | 1.518 (1.177–1.957) | ||
| Heart failure | 1.485 (1.041–2.117) | ||
| Rheumatoid arthritis [27] | RA increases the risk of herpes zoster (USA and UK; 1611) | USA | 1.91 (1.80–2.03) |
| UK | 1.65 (1.57–1.75) | ||
| Rheumatic diseases [20] | Compared with RA, SLE and BS are stronger risk factors for herpes zoster (Korea; 1869) | SLE | 4.29 (3.49–5.27) |
| Behçet’s syndrome | 4.54 (3.66–5.64) | ||
| Infliximab | 2.92 (1.72–4.89) | ||
| Glucocorticoids | 2.91 (1.72–4.89) | ||
| Heart failure [21] | Heart failure (Taiwan; 211) | All | 2.07 (1.54–2.78) |
| Men | 2.30 (1.51–3.50) | ||
| Respiratory diseases [28] | COPD, asthma, and lung cancer are related to a high risk of contracting herpes zoster (Spain; 31,765) | COPD | 1.16 (1.13–1.19) |
| Asthma | 1.67 (1.63–1.71) | ||
| Lung cancer | 1.68 (1.60–1.76) | ||
| UVR [29] | There is a higher risk of herpes zoster in men, especially those with a history of severe sunburn (US; 24,201) | Men | 1.14 (1.02–1.29) |
| Higher lifetime number of severe sunburn | 1.13 (1.00–1.28) |
HR, hazard ratio; CI, confidence interval; RA, rheumatoid arthritis; SLE, systemic lupus erythematosus; BS, Behçet’s syndrome; COPD, chronic obstructive pulmonary disease; UVR, ultraviolet radiation.
2.4. Respiratory Diseases
According to a study using German claims data, patients with asthma, coronary heart disease, chronic obstructive pulmonary disease (COPD), depression, and rheumatoid arthritis had an average of 30% increased risk of developing acute herpes zoster compared with patients without any chronic underlying conditions [30]. In a recent large population analysis using artificial intelligence, COPD, asthma, and lung cancer demonstrated a higher risk of developing herpes zoster [28] (Table 1). Regarding postherpetic neuralgia, an increased risk was only observed in patients with COPD (odd ratio (OR) 1.24 [95% CI 1.23–1.25]) and lung cancer (1.14 [1.13–1.16]). These insights underscore the intricate interplay between various chronic conditions and the susceptibility to herpes zoster, emphasizing the importance of comprehensive risk assessments and targeted preventive measures.
2.5. Malignancy
Profoundly compromised immune states, such as those seen in individuals with solid tumors, are strongly linked to an elevated susceptibility to herpes zoster due to a decline in VZV-specific cellular immunity [31,32]. In immunocompromised patients, particularly those with cancer, herpes zoster can lead to increased morbidity [33]. This is characterized by a prolonged phase of skin rash and an elevated risk of cutaneous dissemination, as well as involvement of the internal organs, including pneumonitis, hepatitis, and central nervous system disease [34]. Notably, the risk of developing herpes zoster is higher among patients undergoing chemotherapy [35] or immunotherapy [36] compared to individuals not currently undergoing active treatment.
2.6. Immunocompromised Conditions
Immune-compromised conditions, including acquired immunodeficiency syndrome (AIDS) [32], systemic lupus nephritis [37], rheumatoid arthritis [27,38], transplant recipients [39], lymphoma, leukemia, and cancer, are widely recognized as established risk factors for herpes zoster [40,41,42]. In contrast to the course of herpes zoster in immunocompetent patients, herpes zoster often recurs or is prolonged in immunocompromised patients, especially those with AIDS [43]. This heightened susceptibility underscores the need for vigilant monitoring and specialized care for immunocompromised individuals to mitigate the impact of herpes zoster and improve overall health outcomes.
2.7. Rheumatoid Arthritis
In a retrospective cohort study that encompassed 20,357 individuals with rheumatoid arthritis, factors contributing to the risk of herpes zoster encompassed advanced age, the use of prednisone, medications employed in the management of moderate and severe rheumatoid arthritis, as well as various comorbidities [44]. Among patients undergoing treatment with TNF-α antagonists, both etanercept (HR 0.62) and adalimumab (HR 0.53) were linked to a reduced likelihood of developing herpes zoster.
2.8. Inflammatory Bowel Disease
Patients with inflammatory bowel disease face a significantly elevated risk of herpes zoster [39,45]. Over an average follow-up period of 5.0 years, the likelihood of developing herpes zoster was notably higher in individuals with Crohn’s disease (adjusted HR 2.13, p < 0.001) and ulcerative colitis (adjusted HR 1.40, p < 0.001) compared to the control group. Particularly in young patients with Crohn’s disease, the incidence of herpes zoster significantly rises in those with metabolic comorbidities, such as diabetes mellitus, hypertension, or dyslipidemia.
2.9. Iatrogenic Risk Factors
Herpes zoster manifests in immunocompromised patients undergoing radiation therapy, bone marrow transplantation, immunosuppressive medication, or prolonged use of steroids [46]. Individuals with COPD face an elevated risk of developing herpes zoster compared to the general population. Moreover, the relative risk of herpes zoster is higher for patients with COPD using oral steroids (adjusted HR 3.00, 95% CI 2.40–3.75) [47]. Limited studies have explored the occurrence of herpes zoster during immunotherapy [36]. Immune checkpoint inhibitors can trigger herpes zoster in two ways: during the treatment of immune-related adverse events with high-dose steroids and in the context of immune reconstitution inflammatory syndrome [48]. Some Janus kinase inhibitors, particularly peficitinib, baricitinib, and tofacitinib, are linked with an increased risk of herpes zoster infection in patients with immune-mediated inflammatory diseases such as rheumatoid arthritis and inflammatory bowel disease [49].
2.10. Ultraviolet Radiation (UVR)
Exposure to ambient UVR was linked to an elevated risk of herpes zoster in men, but this association was not observed in women [29] (refer to Table 1). For men, a history of severe sunburn was modestly associated with an increased risk of herpes zoster, potentially due to immunosuppression resulting from excessive sun exposure.
3. Postherpetic Complications
Herpes zoster is typically benign, lasting between 4 and 7 days; however, severe complications may occur. VZV infects a wide variety of cell types in the central and peripheral nervous system, thereby expanding the diversity of clinical disorders associated with the virus. Although postherpetic neuralgia is the most debilitating complication, there are several other severe postherpetic complications (Figure 2). VZV infection can cause various neurological disorders, such as meningitis, encephalitis, transverse myelitis, radiculitis, and polyneuritis [50]. However, the exact mechanisms underlying the development of postherpetic complications remain unclear.
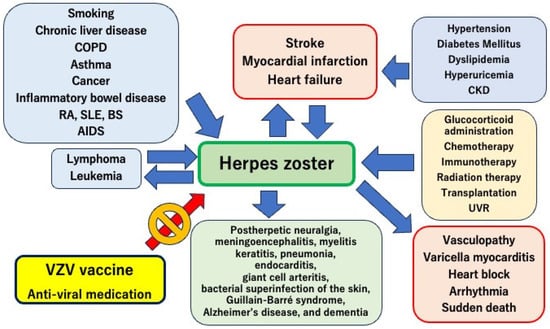
Figure 2.
Relationship between cardiovascular disease and herpes zoster. Cardiovascular diseases, including myocardial infarction, heart failure, and stroke, are closely related to the onset and worsening of herpes zoster. Furthermore, severe complications induced by herpes zoster are important for cardiovascular diseases, such as vasculopathy, myocarditis, arrhythmia, and sudden death. Aggressive vaccination against the varicella-zoster virus is essential for the prevention and management of cardiovascular diseases. COPD, chronic obstructive pulmonary disease; RA, rheumatoid arthritis; SLE, systemic lupus erythematosus; BS, Behçet’s syndrome; AIDS, acquired immunodeficiency syndrome; VZV, varicella zoster virus; CKD, chronic kidney disease; UVR, ultraviolet radiation.
3.1. Neuralgia
Postherpetic neuralgia is characterized by chronic strong pain in the area where the rash occurs. The pain is typically sharp, stabbing, or burning, and may persist for weeks to months or even years after the rash has healed. This pain can be severe and debilitating, affecting the patient’s quality of life. Postherpetic neuralgia is the leading cause of pain-related suicide among older adults [51]. Patients with advanced age and weakened immune systems, such as those with HIV or those undergoing immunosuppressive treatment, are at a higher risk. The inflammation caused by VZV during acute infection may damage or sensitize the nerves, resulting in prolonged pain signals. Early intervention for postherpetic neuralgia is often crucial to effectively manage this condition.
Furthermore, the risk of postherpetic neuralgia is higher in women and increases significantly with age and comorbidities such as diabetes mellitus, COPD, and heart failure [52]. The cumulative risk of developing herpes zoster between the ages of 50 and 90 years was found to be 31.7%. A comprehensive medical approach to improving the overall health of individuals susceptible to shingles and its complications is essential, necessitating the addressing of risk factors for postherpetic neuralgia.
3.2. Meningoencephalitis
Herpes zoster encephalitis induced by viral dissemination into the central nervous system is a potential complication that can lead to virus-induced cerebral angiitis [53]. The presentation is similar to most cases of viral encephalitis and includes confusion, headache, fever, and meningeal symptoms [14]. Recognizing these neurological complications is crucial for prompt diagnosis and intervention. In summary, herpes zoster can lead to encephalitis with associated cerebral angiitis, highlighting the importance of vigilance in identifying and managing these potential complications for better patient outcomes.
3.3. Myelitis
When VZV spreads centrally along peripheral nerves toward the spinal cord, it can enter the spinal cord at levels corresponding to the affected dorsal root ganglia and nerves, leading to myelitis [14]. If the cervical spinal cord is affected, individuals with zoster myelitis may experience weakness in all four extremities and impaired sphincter function. Herpes zoster with a sacral distribution can also result in bladder and bowel dysfunctions. Moreover, zoster myelitis with a cervical or thoracic distribution may induce diaphragmatic paralysis, which should be considered a potential cause of death in patients with VZV infection-induced cervical radiculitis or myelitis.
3.4. Cranial Nerve Damage
Ocular herpes zoster affects the ophthalmic branch of the trigeminal nerve, leading to significant local eye complications [15]. Moreover, the reactivation of the VZV along the seventh cranial nerve can result in the Ramsay Hunt syndrome, characterized by facial paralysis and otic zoster. Both ocular herpes zoster, which leads to significant eye complications, and Ramsay Hunt syndrome profoundly impact a patient’s quality of life. Healthcare professionals managing these conditions should prioritize early intervention whenever feasible. Increasing awareness about these illnesses is crucial as this can facilitate early treatment by ensuring that more people are informed about these conditions.
3.5. Keratitis
The reactivation of herpes zoster ophthalmicus has the potential to result in peripheral ulcerative keratitis. Concurrently, herpes zoster keratitis may manifest alongside other eye conditions, including blepharitis, conjunctivitis, scleritis, uveitis, and retinopathy [54]. VZV can trigger immune-mediated damage across all layers of the cornea, leading to scarring, thinning, and the development of new blood vessels (neovascularization) [55]. Ultimately, individuals with herpes zoster keratitis may experience visual impairment and, possibly, progression to blindness [56]. By recognizing these complications, early intervention and comprehensive eye care can be provided to individuals affected by herpes zoster.
3.6. Respiratory Complications
Primary VZV infection in adults tends to have a more severe manifestation, notably including interstitial pneumonia, compared to younger individuals. Varicella pneumonia, occurring as a complication of herpes zoster, is infrequent and is predominantly documented in immunocompromised individuals. Cases of varicella pneumonia linked to VZV infection are often associated with a high incidence of respiratory failure. Nevertheless, timely diagnosis and the prompt initiation of antiviral medications have the potential to enhance outcomes [57].
3.7. Subacute Endocarditis
An unusual occurrence of subacute bacterial endocarditis subsequent to herpes zoster has been documented [58]. It is important to highlight that herpes zoster has been linked to the onset of other significant infections, such as pneumonia and necrotizing fasciitis.
3.8. Giant Cell Arteritis
Giant cell arteritis, also recognized as temporal arteritis, is a chronic granulomatous inflammation affecting medium and large blood vessels, with the potential for severe, visual, and life-threatening consequences [59]. Although recent data indicate that herpes zoster might serve as an underlying immunological trigger for giant cell arteritis, the role of VZV in the development of giant cell arthritis remains a subject of controversy [14]. The prevalence of giant cell arteritis was notably higher among individuals with herpes zoster compared to the general population (0.340% vs. 0.143%, p < 0.0001) [60]. Conducting additional research to clarify the connection between herpes zoster and giant cell arteritis is anticipated to facilitate the early detection and proper management of this severe vascular disease.
3.9. Bacterial Superinfection of the Skin and Soft Tissue
Primarily caused by Group A Streptococcus, superinfection of the skin and soft tissue is induced by bacteria. Distinguishing herpes zoster skin rashes from bacterial epidermal and facial soft tissue infections can be challenging in clinical practice. Moreover, bacterial superinfection of herpes zoster may complicate diagnoses [61]. When the differential diagnosis is difficult, C-reactive protein and leukocyte counts should be determined, whereas parameters such as neutrophils or immature granulocytes do not add diagnostic value.
3.10. Guillain–Barré Syndrome
There appears to be an association between Guillain–Barré syndrome and preceding herpes zoster. Despite the availability of numerous case reports on this link, establishing a causal relationship remains challenging, given the common occurrence of both conditions among neurologists [14]. The time span between the initial zoster rash and the onset of inflammatory polyradiculitis varies widely, ranging from 2 days to several months. Clinical symptoms mirror those typically observed in Guillain–Barré syndrome, and a brief interval (less than 2 weeks) between the rash and Guillain–Barré syndrome is indicative of a poor prognosis. The treatment for this complication aligns with that employed for Guillain–Barré syndromes related to other causes.
3.11. Alzheimer’s Disease and Dementia
In a comprehensive population-based cohort study conducted in Korea, the presence of the herpes virus was linked to an elevated risk of dementia [62]. Conversely, the utilization of antiviral agents was associated with a reduced risk of dementia in individuals with herpes zoster. Herpes viruses, specifically herpes simplex virus type 1 and VZV, have been implicated in the development of Alzheimer’s disease. Antivirus treatment demonstrated an association with a decreased risk of dementia (adjusted HR 0.89, 95% CI 0.86–0.92), while herpes infection without antiviral medications increased the risk of dementia (adjusted HR 1.50, 95% CI 1.29–1.74) [63]. Consequently, antiviral treatment is linked to a diminished long-term risk of dementia in individuals displaying evident signs of herpes infection. Conversely, a meta-analysis comprising nine studies found no significant association between herpes zoster and the incidence of dementia or Alzheimer’s disease [64]. However, it did reveal a noteworthy association between herpes zoster opthalmicus and the incidence of dementia [64,65].
3.12. Subsequent Cancer Risk
The herpes zoster group exhibited a significantly increased risk of hematologic malignancies, including multiple myeloma (HR 1.63, 95% CI 1.37–1.95), leukemia (HR 1.20, 1.03–1.39), and lymphoma (HR 1.15, 11.02–1.30), compared with the non-herpes zoster group [66]. Conversely, the risk of liver (HR 0.87, 95% CI 0.82–0.93) and larynx (HR 0.73, 0.58–0.92) cancers was significantly decreased in the herpes zoster group compared to the non-herpes zoster group.
The herpes zoster with the postherpetic neuralgia group demonstrated a higher HR for specific cancer risk, such as lymphoid and hematopoietic systems (95% CI 1.27–2.39, p < 0.001). However, no significant increase in the HR for cancers of the lips, mouth, pharynx, digestive system, and respiratory system was observed [67].
5. Prevention of Herpes Zoster and Its Complications
The most efficient means to prevent postherpetic neuralgia is by mitigating the risk of developing herpes zoster through vaccination. Recognized as a vaccine-preventable ailment, herpes zoster vaccination is recommended for individuals aged > 50 years and has demonstrated efficacy in reducing the incidence of both herpes zoster and postherpetic neuralgia.
Vaccines targeting varicella-zoster, including Varivax for varicella and Shingrix and Zostavax for herpes zoster, are accessible options for preventing herpes zoster [74]. The recombinant zoster vaccine (RZV) has exhibited sustained high efficacy against herpes zoster, remaining effective approximately 10 years post-vaccination, with a clinically acceptable safety profile [75]. Studies have confirmed the effectiveness of the zoster vaccine in preventing incident herpes zoster in older individuals with chronic kidney disease [76]. Recent global vaccination guidelines have recently been revised to prioritize recombinant zoster vaccines for high-risk groups, such as patients with cancer [77]. The immunogenicity of the recombinant zoster vaccine has been explored in patients with cancer undergoing chemotherapy, revealing that both humoral and cell-mediated immune responses persisted 12 months post-vaccination [78]. Compared to the general population, older adults with immune senescence and those who are immunocompromised due to disease or immunosuppressive therapy face an elevated risk of herpes zoster and its complications, which can be severe and life-threatening. Vaccination emerges as an effective strategy against herpes zoster, with studies demonstrating that herpes zoster vaccination in immunocompromised individuals can induce immune responses and offer protection from infection [79].
6. Recurrence Rate of Herpes Zoster
Herpes zoster was traditionally thought to occur only once in a lifetime, with recurrences mainly observed in severely immunocompromised individuals. However, there is a growing trend in the recurrence rate, which is now reported as 12.0 per 1000 person-years. In a population-based study conducted in Korea, several notable risk factors for the recurrence of herpes zoster were identified. These included old age (51–70 years) (HR 1.447, 95% CI 1.311–1.598), female gender (HR 1.476, 95% CI 1.345–1.619), and zoster-related pain lasting longer than 90 days (HR 2.293, 95% CI 1.990–2.643) [80]. Additionally, concurrent conditions such as hematologic malignancies (HR 2.864, 95% CI 1.929–4.251), autoimmune diseases (HR 1.466, 95% CI 1.252–1.715), dyslipidemia (HR 1.390, 95% CI 1.263–1.530), and hypertension (HR 1.222, 95% CI 1.107–1.350) were identified as significant risk factors for the recurrence of herpes zoster.
7. Herpes Virus-Induced Vasculopathy
VZV vasculopathy encompasses instances of varicella or zoster that exhibit a temporal association with stroke, particularly when the zoster occurs within the ophthalmic division of the trigeminal nerve [81].
7.1. Vasculopathy-Related Diseases
VZV vasculopathy, which has the potential to trigger stroke, giant cell arteritis, and granulomatous aortitis, arises from productive viral infection of arteries [81]. The presence of VZV within the sensory ganglia allows for transaxonal travel to cerebral arteries, where the nerve terminates in the adventitia, as well as to coronary arteries [82,83]. This process is accompanied by an increased sympathetic tone, elevated blood pressure, and altered immunological status [84]. These mechanisms can initiate inflammation and pathological vascular remodeling [85], ultimately leading to vascular failure, atherosclerosis, microvascular angina, and heart failure induced by microvascular dysfunction.
7.2. Vasculopathy-Related Signaling
The inflammation induced by VZV in arteries plays a role in pathological vascular remodeling. This process involves the downregulation of programmed death ligand-1, contributing to persistent vasculitis [81]. Additionally, it involves major histocompatibility complex class-I, which leads to ineffective clearance of the virus.
7.3. Pathological Changes
Arteries infected with VZV exhibit a disrupted internal elastic lamina, a thickened intima composed of myofibroblasts expressing α-smooth muscle actin, and a deficiency of medial smooth muscle cells, resulting in the compromise of vessel wall integrity [86]. In the early stages of VZV vasculopathy, arteries contain a substantial number of neutrophils in the adventitia, a presence that diminishes in the later stages of VZV vasculopathy [87].
8. Mechanisms of Herpes Zoster-Induced Cardiovascular Diseases
Examinations of herpes zoster through pathological analyses have revealed diverse levels of ganglionic hemorrhage and inflammation [88]. Observations from reports have outlined the existence of hemorrhage, necrosis, and inflammation within the spinal ganglia affected by herpes zoster in patients [89,90]. The histological characteristics encompass mononuclear and lymphocytic inflammation, neuronal degeneration, phagocytosis of neurons by satellite cells, and vacant neuronal cell beds. This process ultimately leads to fibrous scarring of the ganglia [46].
8.1. Inflammation
The infection of herpes zoster initiates an inflammatory response within the body. The release of proinflammatory cytokines during herpes zoster infection triggers endovascular inflammation, leading to the rupture of atherosclerotic plaque [74]. Subsequently, thrombosis occurs, resulting in acute cardiovascular events such as acute myocardial infarction [91]. Cerebrospinal fluid obtained from virologically confirmed VZV vasculopathy patients exhibited significantly elevated levels of interleukin (IL)-8, proinflammatory cytokines (IL-6, IL-1β, TNF-α, IFN-γ, IL-2), anti-inflammatory cytokine IL-10, and matrix metalloproteinases-2 [92]. IL-8 serves as a chemoattractant for neutrophils, while IL-6 promotes macrophage differentiation, potentially contributing to inflammation and damage to the vascular wall-key features of VZV vasculopathy [81]. Therefore, the chronic inflammation induced by herpes zoster vasculopathy is linked to an elevated risk of cardiovascular diseases, including atherosclerosis.
8.2. Autonomic Nervous System Dysfunction
VZV infection seldom leads to orthostatic hypotension, characterized by widespread sympathetic dysfunction due to polyneuropathy [93]. In contrast, VZV infection results in dysfunction of the bladder and bowel, involving segmental dysfunction of the parasympathetic or sympathetic system due to dorsal root ganglionopathy. Recognizing autonomic dysfunction associated with VZV is crucial, particularly because individuals experiencing such symptoms may seek medical attention at gastroenterology or urology clinics. Autonomic dysfunction induced by herpes zoster may also contribute to cardiovascular complications, including arrhythmias and elevated blood pressure.
8.3. Vasculopathy
Herpes zoster is linked to various vasculopathies, encompassing ischemic stroke, aneurysm, cerebral and subarachnoid hemorrhage, mononuclear vision loss, arterial dissection, peripheral arterial disease, myocardial infarction, and transient ischemic stroke [81,85,94,95]. The complex relationship between herpes zoster and various vascular problems emphasizes the importance of thorough medical care and preventive measures for these patients. It is important to understand the potential impact on various vascular complications. Continued research is essential to uncover the underlying mechanisms and enhance strategies to manage these complex connections, ultimately leading to better outcomes for patients.
9. Herpes Zoster-Related Cardiovascular Diseases
Evidence suggesting the involvement of herpes zoster in the development of cardiovascular diseases has recently been reported [18]. Specifically, activation of the immune system during herpes zoster may cause vascular inflammation and heart failure. Understanding and managing this association is essential for the prevention of cardiovascular disease (Figure 2).
9.1. All Major Adverse Cardiac and Cerebrovascular Events (MACCEs)
A recent retrospective cohort study analyzing the association between herpes zoster and MACCEs showed that cumulative MACCE survival at the end of the follow-up period was 54.4% in patients with herpes zoster compared with 74.2% in the non-herpes zoster participants [18]. Although contracting herpes zoster has been shown to increase the risk of MACCEs within a year after infection, there is no relationship between the presence or absence of herpes zoster and the risk of cerebral infarction. The higher risk of MACCEs may be due to systemic unhealthy conditions, such as dehydration, insomnia, temporal hypertension, and mental stress induced by the strong pain of neuralgia. A study identified 29,054 cases of herpes zoster among 16,811,501 in-hospital cases registered from 1208 hospitals. Factors associated with a poor short-term prognosis in this group included age over 75 years (HR 2.18, 95% CI 1.55–3.05), liver cirrhosis or hepatic failure (HR 1.65, 95% CI 1.22–2.24), chronic kidney disease (HR 1.92, 95% CI 1.10–3.34), heart failure (HR 1.65, 95% CI 1.22–2.24), and old cerebrovascular events (HR 1.92, 95% CI 1.10–3.34) [19].
9.2. Stroke
Several studies and meta-analyses have demonstrated an increased risk of stroke following herpes zoster infection [18,70,71,72,83,84,91,96,97,98,99,100,101,102,103]. The stroke risk increases in the first week following herpes zoster infection and then decreases over the subsequent 6–12-month follow-up period [104]. The Taiwan National Health Research Institute records revealed a 4.5-fold increased risk of stroke if herpes zoster occurred in the ophthalmic division of the trigeminal nerve [105]. In patients aged < 40 years with herpes zoster, the risks of stroke and transient ischemic attacks were significantly higher (1.74- and 2.42-fold, respectively) [106].
In long-term analyses, the multivariable-adjusted HR for stroke was 1.38 (95% CI 1.19–1.74) in individuals 5–8 years after the herpes zoster occurrence compared with those with no history of herpes zoster [100] (Table 2). The risk of stroke associated with herpes zoster potentially varies depending on the focus and extent of the lesion and severity of pain.

Table 2.
Cardiovascular diseases and history of herpes zoster.
9.3. Myocardial Infarction
Numerous clinical studies have indicated that herpes zoster raises the likelihood of experiencing myocardial infarction [70,72,83,84,91,95,96,97,98,99,107]. Over a mean follow-up duration of 4.4 years, the cumulative survival rate for AMI was 68.7% in the herpes zoster group and 90.0% in the non-herpes zoster group [18]. Herpes zoster infection was linked to a 1.35-fold increased risk of myocardial infarction within the initial 30 days post-infection [74]. Factors such as history of prior myocardial infarction, male gender, age over 50 years, a history of heart failure, peripheral vascular disease, HIV infection, prior cerebrovascular accident, and renal disease heightened the odds of experiencing a myocardial infarction within 30 days after herpes zoster infection.
9.4. Coronary Heart Disease
As shown in Table 2, long-term analyses comparing individuals with no history of herpes zoster revealed that the multivariable-adjusted HR for coronary heart disease was 1.25 (95% CI 1.07–1.46) among individuals 9–12 years after the herpes zoster occurrence [100]. Infection-associated systemic inflammation and increased heart rate are known to increase the metabolic demands on systemic organs and tissues and decrease coronary perfusion. These conditions are crucial for the development of coronary artery disease.
9.5. Myocarditis
Direct damage to the myocardium caused by the virus and immunological abnormalities following infection are deemed to cause viral myocarditis. Varicella myocarditis is a serious form of VZV that causes cardiac complications [108,109,110]. Although myocarditis caused by VZV is rare, it is an important complication associated with high mortality.
9.6. Heart Failure
In a retrospective case–control study based on the National Health Insurance System claims database of Korea, of 20,311 patients with herpes zoster, severe herpes zoster requiring hospitalization independently increased the risk of subsequent heart failure (HR 2.034, 95% CI 1.615–2.562) [22]. Importantly, heart failure was also a major risk factor for herpes hospitalization (HR 1.485, 95% CI 1.041–2.117).
9.7. Arrhythmia
VZV has been documented to necessitate permanent pacemaker placement due to complete heart block [111,112,113] and lead to second-degree atrioventricular block [114]. The development of a complete heart block is believed to result directly from the reactivation of the virus within the cardiac sympathetic/parasympathetic ganglia [111]. Comprehending and consistently anticipating these cardiac complications is essential for timely intervention and the effective management of patients with shingles. Additional research is necessary to delve into the mechanisms underlying VZV-related cardiac issues and optimize prevention strategies for this specific group of patients.
10. Conclusions
Herpes zoster, a condition that significantly diminishes quality of life, is preventable through vaccination. Recent studies have unveiled associations with prolonged pain, severe cardiovascular disease, and stroke. Therefore, vaccination against VZV is strongly recommended, especially for individuals over the age of 50. In conclusion, recognizing herpes zoster as a substantial concern in cardiovascular disease management, a more proactive vaccination approach is crucial to mitigate its impact and enhance overall health outcomes.
Funding
This work was partially supported by JSPS KAKENHI, grant number JP19K11371.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Gnann, J.W., Jr.; Whitley, R.J. Clinical practice. Herpes zoster. N. Engl. J. Med. 2002, 347, 340–346. [Google Scholar] [CrossRef] [PubMed]
- Yawn, B.P.; Itzler, R.F.; Wollan, P.C.; Pellissier, J.M.; Sy, L.S.; Saddier, P. Health care utilization and cost burden of herpes zoster in a community population. Mayo Clin. Proc. 2009, 84, 787–794. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.H.; Huang, L.M.; Chang, I.S.; Tsai, F.Y.; Lu, C.Y.; Shao, P.L.; Chang, L.Y.; Varicella-Zoster Working Group, Advisory Committee on Immunization Practices, Taiwan. Disease burden and epidemiology of herpes zoster in pre-vaccine Taiwan. Vaccine 2010, 28, 1217–1220. [Google Scholar] [CrossRef] [PubMed]
- Yawn, B.P.; Saddier, P.; Wollan, P.C.; St Sauver, J.L.; Kurland, M.J.; Sy, L.S. A population-based study of the incidence and complication rates of herpes zoster before zoster vaccine introduction. Mayo Clin. Proc. 2007, 82, 1341–1349. [Google Scholar] [CrossRef] [PubMed]
- Kawai, K.; Gebremeskel, B.G.; Acosta, C.J. Systematic review of incidence and complications of herpes zoster: Towards a global perspective. BMJ Open 2014, 4, e004833. [Google Scholar] [CrossRef]
- Rimland, D.; Moanna, A. Increasing incidence of herpes zoster among Veterans. Clin. Infect. Dis. 2010, 50, 1000–1005. [Google Scholar] [CrossRef] [PubMed]
- Kawai, K.; Yawn, B.P.; Wollan, P.; Harpaz, R. Increasing Incidence of Herpes Zoster Over a 60-year Period From a Population-based Study. Clin. Infect. Dis. 2016, 63, 221–226. [Google Scholar] [CrossRef]
- Schmader, K. Herpes zoster in older adults. Clin. Infect. Dis. 2001, 32, 1481–1486. [Google Scholar] [CrossRef]
- Weinberg, A.; Lazar, A.A.; Zerbe, G.O.; Hayward, A.R.; Chan, I.S.; Vessey, R.; Silber, J.L.; MacGregor, R.R.; Chan, K.; Gershon, A.A.; et al. Influence of age and nature of primary infection on varicella-zoster virus-specific cell-mediated immune responses. J. Infect. Dis. 2010, 201, 1024–1030. [Google Scholar] [CrossRef]
- Burke, B.L.; Steele, R.W.; Beard, O.W.; Wood, J.S.; Cain, T.D.; Marmer, D.J. Immune responses to varicella-zoster in the aged. Arch. Intern. Med. 1982, 142, 291–293. [Google Scholar] [CrossRef]
- Bahouth, M.N.; Venkatesan, A. Acute Viral Illnesses and Ischemic Stroke: Pathophysiological Considerations in the Era of the COVID-19 Pandemic. Stroke 2021, 52, 1885–1894. [Google Scholar] [CrossRef] [PubMed]
- Gilden, D.H.; Kleinschmidt-DeMasters, B.K.; Wellish, M.; Hedley-Whyte, E.T.; Rentier, B.; Mahalingam, R. Varicella zoster virus, a cause of waxing and waning vasculitis: The New England Journal of Medicine case 5-1995 revisited. Neurology 1996, 47, 1441–1446. [Google Scholar] [CrossRef] [PubMed]
- Takao, Y.; Miyazaki, Y.; Okeda, M.; Onishi, F.; Yano, S.; Gomi, Y.; Ishikawa, T.; Okuno, Y.; Mori, Y.; Asada, H.; et al. Incidences of Herpes Zoster and Postherpetic Neuralgia in Japanese Adults Aged 50 Years and Older From a Community-based Prospective Cohort Study: The SHEZ Study. J. Epidemiol. 2015, 25, 617–625. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, P.G.E. The Spectrum of Neurological Manifestations of Varicella-Zoster Virus Reactivation. Viruses 2023, 15, 1663. [Google Scholar] [CrossRef]
- Wareham, D.W.; Breuer, J. Herpes zoster. BMJ 2007, 334, 1211–1215. [Google Scholar] [CrossRef]
- Tung, Y.C.; Tu, H.P.; Wu, M.K.; Kuo, K.L.; Su, Y.F.; Lu, Y.Y.; Lin, C.L.; Wu, C.H. Higher risk of herpes zoster in stroke patients. PLoS ONE 2020, 15, e0228409. [Google Scholar] [CrossRef]
- Thomas, S.L.; Hall, A.J. What does epidemiology tell us about risk factors for herpes zoster? Lancet Infect. Dis. 2004, 4, 26–33. [Google Scholar] [CrossRef]
- Horev, A.; Horev, A.; Gordon-Irshai, A.; Gordon, M.; Andre, N.; Ifergane, G. Herpes zoster and long-term vascular risk: A retrospective cohort study. Sci. Rep. 2023, 13, 2364. [Google Scholar] [CrossRef]
- Ishikawa, Y.; Nakano, K.; Tokutsu, K.; Nakayamada, S.; Matsuda, S.; Fushimi, K.; Tanaka, Y. Short-Term Prognostic Factors in Hospitalized Herpes Zoster Patients and Its Associated Cerebro-Cardiovascular Events: A Nationwide Retrospective Cohort in Japan. Front. Med. 2022, 9, 843809. [Google Scholar] [CrossRef]
- Ryu, H.J.; Han, J.O.; Lee, S.A.; Seo, M.R.; Choi, H.J.; Ko, K.P.; Baek, H.J. Risk factors for herpes zoster in patients with rheumatic diseases: A nationwide cohort study in Korea. Rheumatology 2021, 60, 2427–2433. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.H.; Lin, Y.T.; Lin, C.Y.; Huang, M.Y.; Chang, W.C.; Chang, W.P. A nationwide population-based cohort study to identify the correlation between heart failure and the subsequent risk of herpes zoster. BMC Infect. Dis. 2015, 15, 17. [Google Scholar] [CrossRef]
- Seo, H.M.; Cha, M.J.; Han, J.H.; Han, K.; Park, S.H.; Bang, C.H.; Lee, J.H.; Lee, J.Y.; Choi, E.K.; Park, Y.M. Reciprocal relationship between herpes zoster and cardiovascular diseases: A nationwide population-based case-control study in Korea. J. Dermatol. 2018, 45, 1312–1318. [Google Scholar] [CrossRef] [PubMed]
- Heymann, A.D.; Chodick, G.; Karpati, T.; Kamer, L.; Kremer, E.; Green, M.S.; Kokia, E.; Shalev, V. Diabetes as a risk factor for herpes zoster infection: Results of a population-based study in Israel. Infection 2008, 36, 226–230. [Google Scholar] [CrossRef]
- Munoz-Quiles, C.; Lopez-Lacort, M.; Ampudia-Blasco, F.J.; Diez-Domingo, J. Risk and impact of herpes zoster on patients with diabetes: A population-based study, 2009–2014. Hum. Vaccin. Immunother. 2017, 13, 2606–2611. [Google Scholar] [CrossRef]
- Lai, S.W.; Liu, C.S.; Kuo, Y.H.; Lin, C.L.; Hwang, B.F.; Liao, K.F. The incidence of herpes zoster in patients with diabetes mellitus: A meta-analysis of cohort studies. Medicine 2021, 100, e25292. [Google Scholar] [CrossRef] [PubMed]
- Poirrier, J.E.; Meyers, J.L.; Nagar, S.P.; Patterson, B.J.; Glasser, L.I.; Jabbour, S.A. Herpes Zoster Incidence and Burden in Adults With Type 2 Diabetes in the U.S.: A Retrospective Database Analysis. Diabetes Care 2022, 45, 2585–2593. [Google Scholar] [CrossRef]
- Smitten, A.L.; Choi, H.K.; Hochberg, M.C.; Suissa, S.; Simon, T.A.; Testa, M.A.; Chan, K.A. The risk of herpes zoster in patients with rheumatoid arthritis in the United States and the United Kingdom. Arthritis Rheum. 2007, 57, 1431–1438. [Google Scholar] [CrossRef] [PubMed]
- Morena, D.; Lumbreras, S.; Rodriguez, J.M.; Campos, C.; Castillo, M.; Benavent, M.; Izquierdo, J.L. Chronic Respiratory Diseases as a Risk Factor for Herpes Zoster Infection. Arch. Bronconeumol. 2023, 59, 797–804. [Google Scholar] [CrossRef]
- Kawai, K.; VoPham, T.; Drucker, A.; Curhan, S.G.; Curhan, G.C. Ultraviolet Radiation Exposure and the Risk of Herpes Zoster in Three Prospective Cohort Studies. Mayo Clin. Proc. 2020, 95, 283–292. [Google Scholar] [CrossRef]
- Batram, M.; Witte, J.; Schwarz, M.; Hain, J.; Ultsch, B.; Steinmann, M.; Bhavsar, A.; Wutzler, P.; Criee, C.P.; Hermann, C.; et al. Burden of Herpes Zoster in Adult Patients with Underlying Conditions: Analysis of German Claims Data, 2007–2018. Dermatol. Ther. 2021, 11, 1009–1026. [Google Scholar] [CrossRef]
- Lasagna, A.; Mele, D.; Bergami, F.; Alaimo, D.; Dauccia, C.; Alessio, N.; Comolli, G.; Pasi, F.; Muzzi, A.; Novelli, V.; et al. The immunogenicity and the safety of the adjuvanted glycoprotein E (gE)-based recombinant vaccine against herpes zoster (RZV) in cancer patients during immunotherapy. Hum. Vaccin. Immunother. 2023, 19, 2288282. [Google Scholar] [CrossRef]
- Marra, F.; Parhar, K.; Huang, B.; Vadlamudi, N. Risk Factors for Herpes Zoster Infection: A Meta-Analysis. Open Forum Infect. Dis. 2020, 7, ofaa005. [Google Scholar] [CrossRef] [PubMed]
- Kawai, K.; Yawn, B.P. Risk of Herpes Zoster in Cancer Patients and the Promise of New Vaccines. J. Infect. Dis. 2019, 220, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Tayyar, R.; Ho, D. Herpes Simplex Virus and Varicella Zoster Virus Infections in Cancer Patients. Viruses 2023, 15, 439. [Google Scholar] [CrossRef] [PubMed]
- Qian, J.; Heywood, A.E.; Karki, S.; Banks, E.; Macartney, K.; Chantrill, L.; Liu, B. Risk of Herpes Zoster Prior to and Following Cancer Diagnosis and Treatment: A Population-Based Prospective Cohort Study. J. Infect. Dis. 2019, 220, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Serra, F.; Cassaniti, I.; Lilleri, D.; Pedrazzoli, P.; Baldanti, F.; Lasagna, A. Herpes zoster in patients with solid tumors treated with immune checkpoint inhibitors. Immunotherapy 2022, 14, 389–393. [Google Scholar] [CrossRef]
- Chen, H.H.; Chen, Y.M.; Chen, T.J.; Lan, J.L.; Lin, C.H.; Chen, D.Y. Risk of herpes zoster in patients with systemic lupus erythematosus: A three-year follow-up study using a nationwide population-based cohort. Clinics 2011, 66, 1177–1182. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, F.; Michaud, K.; Chakravarty, E.F. Rates and predictors of herpes zoster in patients with rheumatoid arthritis and non-inflammatory musculoskeletal disorders. Rheumatology 2006, 45, 1370–1375. [Google Scholar] [CrossRef]
- Imafuku, S.; Dormal, G.; Goto, Y.; Jegou, C.; Rosillon, D.; Matsuki, T. Risk of herpes zoster in the Japanese population with immunocompromising and chronic disease conditions: Results from a claims database cohort study, from 2005 to 2014. J. Dermatol. 2020, 47, 236–244. [Google Scholar] [CrossRef]
- Gilden, D.H.; Cohrs, R.J.; Mahalingam, R. Clinical and molecular pathogenesis of varicella virus infection. Viral Immunol. 2003, 16, 243–258. [Google Scholar] [CrossRef]
- Mueller, N.H.; Gilden, D.H.; Cohrs, R.J.; Mahalingam, R.; Nagel, M.A. Varicella zoster virus infection: Clinical features, molecular pathogenesis of disease, and latency. Neurol. Clin. 2008, 26, 675–697. [Google Scholar] [CrossRef] [PubMed]
- Wung, P.K.; Holbrook, J.T.; Hoffman, G.S.; Tibbs, A.K.; Specks, U.; Min, Y.I.; Merkel, P.A.; Spiera, R.; Davis, J.C.; St Clair, E.W.; et al. Herpes zoster in immunocompromised patients: Incidence, timing, and risk factors. Am. J. Med. 2005, 118, 1416. [Google Scholar] [CrossRef] [PubMed]
- Gilden, D.H.; Kleinschmidt-DeMasters, B.K.; LaGuardia, J.J.; Mahalingam, R.; Cohrs, R.J. Neurologic complications of the reactivation of varicella-zoster virus. N. Engl. J. Med. 2000, 342, 635–645. [Google Scholar] [CrossRef] [PubMed]
- McDonald, J.R.; Zeringue, A.L.; Caplan, L.; Ranganathan, P.; Xian, H.; Burroughs, T.E.; Fraser, V.J.; Cunningham, F.; Eisen, S.A. Herpes zoster risk factors in a national cohort of veterans with rheumatoid arthritis. Clin. Infect. Dis. 2009, 48, 1364–1371. [Google Scholar] [CrossRef] [PubMed]
- Soh, H.; Chun, J.; Han, K.; Park, S.; Choi, G.; Kim, J.; Lee, J.; Im, J.P.; Kim, J.S. Increased Risk of Herpes Zoster in Young and Metabolically Healthy Patients with Inflammatory Bowel Disease: A Nationwide Population-Based Study. Gut Liver 2019, 13, 333–341. [Google Scholar] [CrossRef] [PubMed]
- Kleinschmidt-DeMasters, B.K.; Gilden, D.H. Varicella-Zoster virus infections of the nervous system: Clinical and pathologic correlates. Arch. Pathol. Lab. Med. 2001, 125, 770–780. [Google Scholar] [CrossRef]
- Yang, Y.W.; Chen, Y.H.; Wang, K.H.; Wang, C.Y.; Lin, H.W. Risk of herpes zoster among patients with chronic obstructive pulmonary disease: A population-based study. CMAJ 2011, 183, E275–E280. [Google Scholar] [CrossRef]
- Lasagna, A.; Cassaniti, I.; Sacchi, P.; Baldanti, F.; Bruno, R.; Pedrazzoli, P. Infectious complications and immunotherapy: Old pitfalls and new horizons. Future Oncol. 2022, 18, 2377–2381. [Google Scholar] [CrossRef]
- Xu, Q.; He, L.; Yin, Y. Risk of herpes zoster associated with JAK inhibitors in immune-mediated inflammatory diseases: A systematic review and network meta-analysis. Front. Pharmacol. 2023, 14, 1241954. [Google Scholar] [CrossRef]
- Patil, A.; Goldust, M.; Wollina, U. Herpes zoster: A Review of Clinical Manifestations and Management. Viruses 2022, 14, 192. [Google Scholar] [CrossRef]
- Schmader, K. Postherpetic neuralgia in immunocompetent elderly people. Vaccine 1998, 16, 1768–1770. [Google Scholar] [CrossRef] [PubMed]
- Munoz-Quiles, C.; Lopez-Lacort, M.; Orrico-Sanchez, A.; Diez-Domingo, J. Impact of postherpetic neuralgia: A six year population-based analysis on people aged 50 years or older. J. Infect. 2018, 77, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Lizzi, J.; Hill, T.; Jakubowski, J. Varicella Zoster Virus Encephalitis. Clin. Pract. Cases Emerg. Med. 2019, 3, 380–382. [Google Scholar] [CrossRef] [PubMed]
- Cohen, E.J.; Jeng, B.H. Herpes Zoster: A Brief Definitive Review. Cornea 2021, 40, 943–949. [Google Scholar] [CrossRef] [PubMed]
- Liao, X.; Li, C.Q.; Ge, Q.M.; Tang, L.Y.; Su, T.; Li, Q.Y.; Pan, Y.C.; Shu, H.Y.; Zhang, L.J.; Shao, Y. Investigation of Altered Spontaneous Brain Activity Patterns in Herpes Zoster Keratitis Using the Percent Amplitude of Fluctuation Method: A Resting-State Functional Magnetic Resonance Imaging Study. Neuropsychiatr. Dis. Treat. 2023, 19, 1781–1789. [Google Scholar] [CrossRef]
- Gallon, P.; Parekh, M.; Ferrari, S.; Fasolo, A.; Ponzin, D.; Borroni, D. Metagenomics in ophthalmology: Hypothesis or real prospective? Biotechnol. Rep. 2019, 23, e00355. [Google Scholar] [CrossRef]
- Yadav, P.S.; Adhikari, P.; Jha, N.M.; Khadka, S.; Kafle, S.; Singh, S.; Subedi, S.; Bhatta, M. Varicella pneumonia in an immunocompetent child: A case report. IDCases 2023, 33, e01870. [Google Scholar] [CrossRef]
- Agur Cohen, D.; Braun, E. Unusual subacute endocarditis following herpes zoster infection. a case report. Fam. Pract. 2023, cmad113. [Google Scholar] [CrossRef]
- Borchers, A.T.; Gershwin, M.E. Giant cell arteritis: A review of classification, pathophysiology, geoepidemiology and treatment. Autoimmun. Rev. 2012, 11, A544–A554. [Google Scholar] [CrossRef]
- Lee, D.H.; Iovieno, A.; Sheldon, C.A. Is There an Association between Herpetic Infections and Giant Cell Arteritis? A Population-Based Study. J. Clin. Med. 2020, 10, 63. [Google Scholar] [CrossRef] [PubMed]
- Drerup, C.; Eveslage, M.; Sunderkotter, C.; Ehrchen, J. Diagnostic Value of Laboratory Parameters for Distinguishing Between Herpes Zoster and Bacterial Superficial Skin and Soft Tissue Infections. Acta Derm. Venereol. 2020, 100, adv00009. [Google Scholar] [CrossRef]
- Bae, S.; Yun, S.C.; Kim, M.C.; Yoon, W.; Lim, J.S.; Lee, S.O.; Choi, S.H.; Kim, Y.S.; Woo, J.H.; Kim, S.Y.; et al. Association of herpes zoster with dementia and effect of antiviral therapy on dementia: A population-based cohort study. Eur. Arch. Psychiatry Clin. Neurosci. 2021, 271, 987–997. [Google Scholar] [CrossRef] [PubMed]
- Lopatko Lindman, K.; Hemmingsson, E.S.; Weidung, B.; Brannstrom, J.; Josefsson, M.; Olsson, J.; Elgh, F.; Nordstrom, P.; Lovheim, H. Herpesvirus infections, antiviral treatment, and the risk of dementia-a registry-based cohort study in Sweden. Alzheimers Dement. 2021, 7, e12119. [Google Scholar] [CrossRef] [PubMed]
- Elhalag, R.H.; Motawea, K.R.; Talat, N.E.; Rouzan, S.S.; Reyad, S.M.; Elsayed, S.M.; Chebl, P.; Abowafia, M.; Shah, J. Herpes Zoster virus infection and the risk of developing dementia: A systematic review and meta-analysis. Medicine 2023, 102, e34503. [Google Scholar] [CrossRef] [PubMed]
- Warren-Gash, C.; Breuer, J. Herpes zoster in people who are immunocompromised: What are the options for prevention? Lancet Infect. Dis. 2019, 19, 922–924. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Han, K.; Yoo, S.A.; Lee, J.H. Herpes Zoster and Subsequent Cancer Risk: A Nationwide Population-Based Cohort Study in Korea. Dermatology 2021, 237, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Sim, J.H.; Cho, H.S.; Kim, Y.D.; Mun, J.; Kim, S.B.; Lee, J.H.; Leem, J.G. The Association between Herpes Zoster and Increased Cancer Risk: A Nationwide Population-Based Matched Control Study. Curr. Oncol. 2021, 28, 2720–2730. [Google Scholar] [CrossRef] [PubMed]
- Sreenivasan, N.; Basit, S.; Wohlfahrt, J.; Pasternak, B.; Munch, T.N.; Nielsen, L.P.; Melbye, M. The short- and long-term risk of stroke after herpes zoster—A nationwide population-based cohort study. PLoS ONE 2013, 8, e69156. [Google Scholar] [CrossRef]
- Buturak, A.; Norgaz, T.; Gorgulu, S. Brivudine induced coronary vasospasm as a manifestation of Kounis syndrome: First report. Int. J. Cardiol. 2015, 185, 4–6. [Google Scholar] [CrossRef]
- Wu, P.H.; Chuang, Y.S.; Lin, Y.T. Does Herpes Zoster Increase the Risk of Stroke and Myocardial Infarction? A Comprehensive Review. J. Clin. Med. 2019, 8, 547. [Google Scholar] [CrossRef]
- Langan, S.M.; Minassian, C.; Smeeth, L.; Thomas, S.L. Risk of stroke following herpes zoster: A self-controlled case-series study. Clin. Infect. Dis. 2014, 58, 1497–1503. [Google Scholar] [CrossRef]
- Kim, J.; Jeon, J.; Lee, H.S.; Lee, K.Y. Association Between the Risk for Cardiovascular Events and Antiviral Treatment for Herpes Zoster. Clin. Infect. Dis. 2021, 73, 758–764. [Google Scholar] [CrossRef] [PubMed]
- Meyer, J.J.; Liu, K.; Danesh-Meyer, H.V.; Niederer, R.L. Prompt Antiviral Therapy Is Associated With Lower Risk of Cerebrovascular Accident Following Herpes Zoster Ophthalmicus. Am. J. Ophthalmol. 2022, 242, 215–220. [Google Scholar] [CrossRef]
- Parameswaran, G.I.; Drye, A.F.; Wattengel, B.A.; Carter, M.T.; Doyle, K.M.; Mergenhagen, K.A. Increased Myocardial Infarction Risk Following Herpes Zoster Infection. Open Forum Infect. Dis. 2023, 10, ofad137. [Google Scholar] [CrossRef]
- Strezova, A.; Diez-Domingo, J.; Al Shawafi, K.; Tinoco, J.C.; Shi, M.; Pirrotta, P.; Mwakingwe-Omari, A.; Zoster-049 Study Group. Long-term Protection Against Herpes Zoster by the Adjuvanted Recombinant Zoster Vaccine: Interim Efficacy, Immunogenicity, and Safety Results up to 10 Years After Initial Vaccination. Open Forum Infect. Dis. 2022, 9, ofac485. [Google Scholar] [CrossRef] [PubMed]
- Langan, S.M.; Thomas, S.L.; Smeeth, L.; Margolis, D.J.; Nitsch, D. Zoster vaccination is associated with a reduction of zoster in elderly patients with chronic kidney disease. Nephrol. Dial. Transplant. 2016, 31, 2095–2098. [Google Scholar] [CrossRef]
- Pedrazzoli, P.; Lasagna, A.; Cassaniti, I.; Ferrari, A.; Bergami, F.; Silvestris, N.; Sapuppo, E.; Di Maio, M.; Cinieri, S.; Baldanti, F. Vaccination for herpes zoster in patients with solid tumors: A position paper on the behalf of the Associazione Italiana di Oncologia Medica (AIOM). ESMO Open 2022, 7, 100548. [Google Scholar] [CrossRef]
- Vink, P.; Delgado Mingorance, I.; Maximiano Alonso, C.; Rubio-Viqueira, B.; Jung, K.H.; Rodriguez Moreno, J.F.; Grande, E.; Marrupe Gonzalez, D.; Lowndes, S.; Puente, J.; et al. Immunogenicity and safety of the adjuvanted recombinant zoster vaccine in patients with solid tumors, vaccinated before or during chemotherapy: A randomized trial. Cancer 2019, 125, 1301–1312. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, K.M.; Farraye, F.A.; Winthrop, K.L.; Willer, D.O.; Vink, P.; Tavares-Da-Silva, F. Safety and efficacy of recombinant and live herpes zoster vaccines for prevention in at-risk adults with chronic diseases and immunocompromising conditions. Vaccine 2023, 41, 36–48. [Google Scholar] [CrossRef]
- Kim, Y.J.; Lee, C.N.; Lee, M.S.; Lee, J.H.; Lee, J.Y.; Han, K.; Park, Y.M. Recurrence Rate of Herpes Zoster and Its Risk Factors: A Population-based Cohort Study. J. Korean Med. Sci. 2019, 34, e1. [Google Scholar] [CrossRef]
- Nagel, M.A.; Jones, D.; Wyborny, A. Varicella zoster virus vasculopathy: The expanding clinical spectrum and pathogenesis. J. Neuroimmunol. 2017, 308, 112–117. [Google Scholar] [CrossRef] [PubMed]
- Nagel, M.A.; Bubak, A.N. Varicella Zoster Virus Vasculopathy. J. Infect. Dis. 2018, 218, S107–S112. [Google Scholar] [CrossRef] [PubMed]
- Yawn, B.P.; Wollan, P.C.; Nagel, M.A.; Gilden, D. Risk of Stroke and Myocardial Infarction After Herpes Zoster in Older Adults in a US Community Population. Mayo Clin. Proc. 2016, 91, 33–44. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.C.; Yun, S.C.; Lee, H.B.; Lee, P.H.; Lee, S.W.; Choi, S.H.; Kim, Y.S.; Woo, J.H.; Kim, S.H.; Kwon, S.U. Herpes Zoster Increases the Risk of Stroke and Myocardial Infarction. J. Am. Coll. Cardiol. 2017, 70, 295–296. [Google Scholar] [CrossRef] [PubMed]
- Yawn, B.P.; Lindsay, A.C.; Yousefi, M.; Wang, C. Risk of, and risk factors for, vasculopathy associated with acute herpes zoster. J. Stroke Cerebrovasc. Dis. 2023, 32, 106891. [Google Scholar] [CrossRef] [PubMed]
- Nagel, M.A.; Forghani, B.; Mahalingam, R.; Wellish, M.C.; Cohrs, R.J.; Russman, A.N.; Katzan, I.; Lin, R.; Gardner, C.J.; Gilden, D.H. The value of detecting anti-VZV IgG antibody in CSF to diagnose VZV vasculopathy. Neurology 2007, 68, 1069–1073. [Google Scholar] [CrossRef]
- Nagel, M.A.; Traktinskiy, I.; Stenmark, K.R.; Frid, M.G.; Choe, A.; Gilden, D. Varicella-zoster virus vasculopathy: Immune characteristics of virus-infected arteries. Neurology 2013, 80, 62–68. [Google Scholar] [CrossRef]
- Oaklander, A.L. The pathology of shingles: Head and Campbell’s 1900 monograph. Arch. Neurol. 1999, 56, 1292–1294. [Google Scholar] [CrossRef]
- Nagashima, K.; Nakazawa, M.; Endo, H. Pathology of the human spinal ganglia in varicella-zoster virus infection. Acta Neuropathol. 1975, 33, 105–117. [Google Scholar] [CrossRef]
- Ghatak, N.R.; Zimmerman, H.M. Spinal ganglion in herpes zoster. A light and electron microscopic study. Arch. Pathol. 1973, 95, 411–415. [Google Scholar]
- Musher, D.M.; Abers, M.S.; Corrales-Medina, V.F. Acute Infection and Myocardial Infarction. N. Engl. J. Med. 2019, 380, 171–176. [Google Scholar] [CrossRef]
- Jones, D.; Alvarez, E.; Selva, S.; Gilden, D.; Nagel, M.A. Proinflammatory cytokines and matrix metalloproteinases in CSF of patients with VZV vasculopathy. Neurol. Neuroimmunol. Neuroinflamm 2016, 3, e246. [Google Scholar] [CrossRef]
- Sakakibara, R.; Sawai, S.; Ogata, T. Varicella-zoster virus infection and autonomic dysfunction. Auton. Neurosci. 2022, 242, 103018. [Google Scholar] [CrossRef]
- Gilden, D.; Cohrs, R.J.; Mahalingam, R.; Nagel, M.A. Varicella zoster virus vasculopathies: Diverse clinical manifestations, laboratory features, pathogenesis, and treatment. Lancet Neurol. 2009, 8, 731–740. [Google Scholar] [CrossRef]
- Warren-Gash, C. Herpes Zoster: Epidemiological Links With Stroke and Myocardial Infarction. J. Infect. Dis. 2018, 218, S102–S106. [Google Scholar] [CrossRef]
- Zhang, Y.; Luo, G.; Huang, Y.; Yu, Q.; Wang, L.; Li, K. Risk of Stroke/Transient Ischemic Attack or Myocardial Infarction with Herpes Zoster: A Systematic Review and Meta-Analysis. J. Stroke Cerebrovasc. Dis. 2017, 26, 1807–1816. [Google Scholar] [CrossRef] [PubMed]
- Erskine, N.; Tran, H.; Levin, L.; Ulbricht, C.; Fingeroth, J.; Kiefe, C.; Goldberg, R.J.; Singh, S. A systematic review and meta-analysis on herpes zoster and the risk of cardiac and cerebrovascular events. PLoS ONE 2017, 12, e0181565. [Google Scholar] [CrossRef] [PubMed]
- Minassian, C.; Thomas, S.L.; Smeeth, L.; Douglas, I.; Brauer, R.; Langan, S.M. Acute Cardiovascular Events after Herpes Zoster: A Self-Controlled Case Series Analysis in Vaccinated and Unvaccinated Older Residents of the United States. PLoS Med. 2015, 12, e1001919. [Google Scholar] [CrossRef] [PubMed]
- Wise, J. Shingles is linked to increased risk of cardiovascular events. BMJ 2015, 351, h6757. [Google Scholar] [CrossRef]
- Curhan, S.G.; Kawai, K.; Yawn, B.; Rexrode, K.M.; Rimm, E.B.; Curhan, G.C. Herpes Zoster and Long-Term Risk of Cardiovascular Disease. J. Am. Heart Assoc. 2022, 11, e027451. [Google Scholar] [CrossRef] [PubMed]
- Marra, F.; Ruckenstein, J.; Richardson, K. A meta-analysis of stroke risk following herpes zoster infection. BMC Infect. Dis. 2017, 17, 198. [Google Scholar] [CrossRef] [PubMed]
- Lian, Y.; Zhu, Y.; Tang, F.; Yang, B.; Duan, R. Herpes zoster and the risk of ischemic and hemorrhagic stroke: A systematic review and meta-analysis. PLoS ONE 2017, 12, e0171182. [Google Scholar] [CrossRef] [PubMed]
- Parameswaran, G.I.; Wattengel, B.A.; Chua, H.C.; Swiderek, J.; Fuchs, T.; Carter, M.T.; Goode, L.; Doyle, K.; Mergenhagen, K.A. Increased Stroke Risk Following Herpes Zoster Infection and Protection With Zoster Vaccine. Clin. Infect. Dis. 2023, 76, e1335–e1340. [Google Scholar] [CrossRef] [PubMed]
- Schink, T.; Behr, S.; Thone, K.; Bricout, H.; Garbe, E. Risk of Stroke after Herpes Zoster—Evidence from a German Self-Controlled Case-Series Study. PLoS ONE 2016, 11, e0166554. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.C.; Chien, C.W.; Ho, J.D. Herpes zoster ophthalmicus and the risk of stroke: A population-based follow-up study. Neurology 2010, 74, 792–797. [Google Scholar] [CrossRef] [PubMed]
- Breuer, J.; Pacou, M.; Gauthier, A.; Brown, M.M. Herpes zoster as a risk factor for stroke and TIA: A retrospective cohort study in the UK. Neurology 2014, 82, 206–212. [Google Scholar] [CrossRef] [PubMed]
- Wutzler, P. Stroke and myocardial infarction after herpes zoster. MMW Fortschr. Med. 2017, 159, 66–68. [Google Scholar] [CrossRef]
- Morales, A.R.; Adelman, S.; Fine, G. Varicella myocarditis. A case of sudden death. Arch. Pathol. 1971, 91, 29–31. [Google Scholar]
- Elikowski, W.; Marszalek, A.; Malek-Elikowska, M.; Ganowicz-Kaatz, T.; Mozer-Lisewska, I. Myopericarditis in a 23-year-old male with herpes zoster. Pol. Merkur. Lekarski 2016, 40, 97–101. [Google Scholar]
- Kelly, E.; Cullen, G.; McGurk, C. When an MI is not an MI: A case of varicella zoster myocarditis. Cardiology 2008, 109, 193–195. [Google Scholar] [CrossRef] [PubMed]
- Ma, T.S.; Collins, T.C.; Habib, G.; Bredikis, A.; Carabello, B.A. Herpes zoster and its cardiovascular complications in the elderly--another look at a dormant virus. Cardiology 2007, 107, 63–67. [Google Scholar] [CrossRef] [PubMed]
- Kalender, E.; Sensoy, B.; Cay, S. Heart block after herpes zoster reactivation. Int. J. Cardiol. 2016, 203, 549–550. [Google Scholar] [CrossRef] [PubMed]
- Singhal, R.; Jin, P.; Nassereddin, A.T.; Lopez, J.E.; Keeley, E.C. Varicella Zoster Virus-Induced Complete Heart Block. Am. J. Med. 2023, 136, e63–e64. [Google Scholar] [CrossRef] [PubMed]
- Kazemi, V.; Fernandez, M.C.; Zide, K. Herpes Zoster-induced Progressive Heart Block: A Case Report. Cureus 2018, 10, e3674. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).