COVID-19 Vaccinations, Trust, and Vaccination Decisions within the Refugee Community of Calgary, Canada
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Sampling and Recruitment
2.3. Data Collection
2.4. Data Analysis
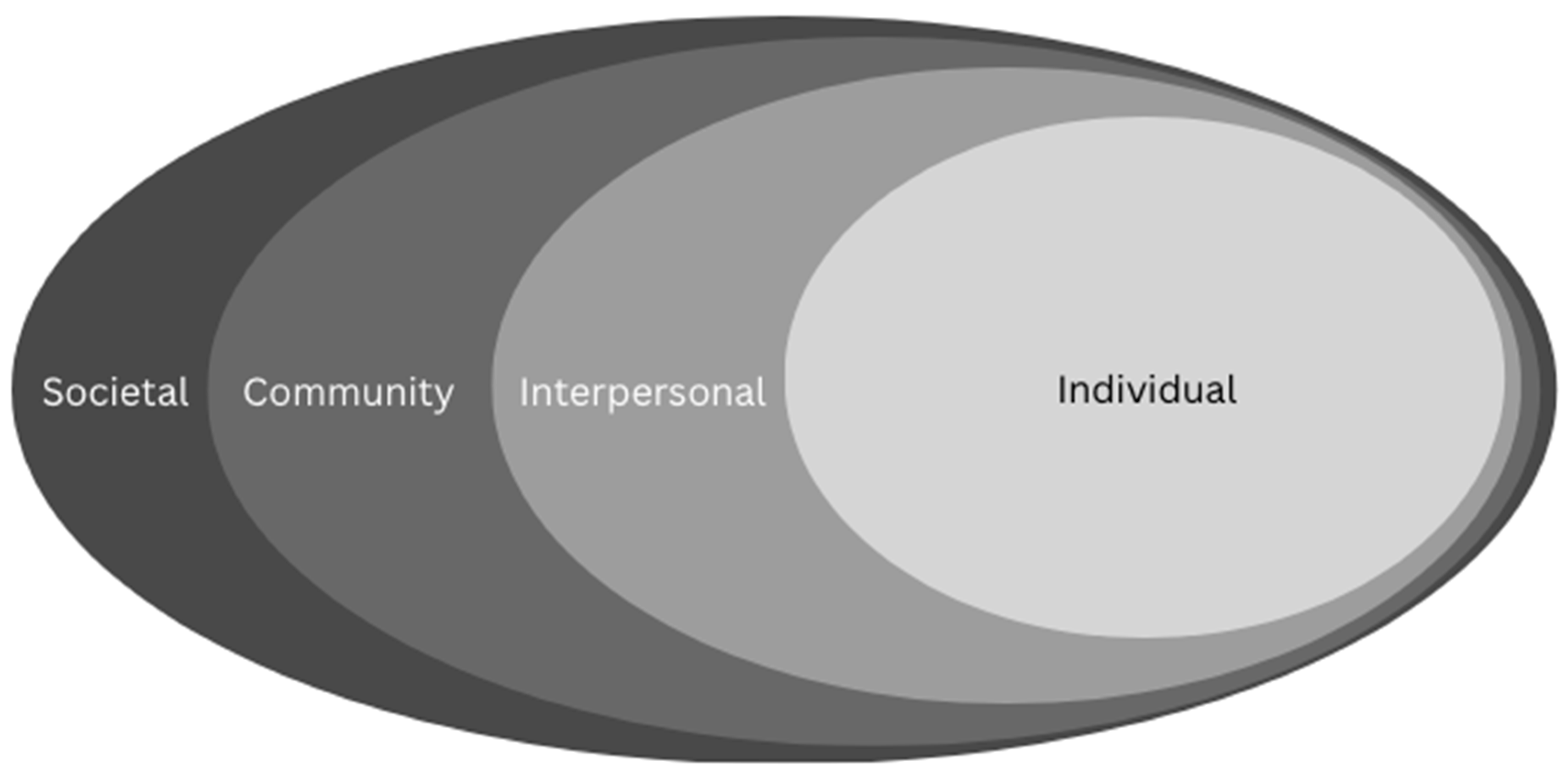
3. Results
3.1. Individual Factors
- Concerns about side effects: Concerns refugees had or held about the negative side effects of the vaccine and mortality rates were discussed by several refugees (n = 6) as a factor shaping their decisions. Concerns were for themselves or for their family members, and these sentiments tended to correspond with informal knowledge networks or broader community discourse. Such concerns were generally addressed when healthcare professionals took the time to ask about and address their concerns.
- Personal ‘disbelief’ in vaccine necessity or effectiveness and/or preference to avoid medical intervention: Another factor shared by refugees (n = 7) was a belief that the COVID-19 vaccine, or vaccines/medical intervention in general, is not effective or not a necessary form of defence against illness. This factor included the belief that their bodies are able to defend against diseases naturally and do not need additional assistance from vaccines.
- Concerns about risks to subpopulations: Individual refugees and all key informants involved in service provision spoke about vaccine safety concerns for specific subpopulations, such as children, youth, pregnant women, and persons with allergies or underlying health conditions. Similar to concerns about vaccine side effects, participants shared that concerns about specific subpopulations were addressed when healthcare professionals took the time to ask about and address such concerns.
- Fear of COVID-19: An important individual factor was the willingness and eagerness to be vaccinated. Refugees linked vaccine compliance to desires to mitigate physical health risks of COVID-19, including for healthy and at-risk persons. This motivation for health ultimately superseded any uncertainty about the vaccine or its safety, even in cases where refugees had remaining concerns, and key informants noted an ongoing desire to protect children with initial doses.
3.2. Interpersonal Factors
- (Mis)information: Information was a key factor in shaping decisions which could positively or negatively influence vaccine uptake. Refugees shared examples of multiple and competing sources of information and linked these to feelings of hesitancy and confidence with the vaccine. Sources of misinformation commonly cited included social media and stories from friends and family. Despite being immersed in multiple sources of information, the large majority of refugees interviewed shared they were able to navigate misinformation and were not opposed to vaccinations. However, refugees also feared the influence of misinformation on other people who may be hesitant to vaccinate.
- Desire to protect others: Interpersonal factors included desires to protect others through vaccination. For example, some refugees framed their decision to be vaccinated as being for the protection for others, especially family members, rather than themselves.
- Influence of family members: Similar to (mis)information, a key factor that refugees contended with was the influence of family members. Refugees expressed different levels of hesitancy and/or vaccine confidence among family members, which shaped their thoughts and feelings around vaccinations. There were also cases where refugees explicitly stated that pressure or preference from family members, such as spouses, was a deciding factor in being vaccinated.
3.3. Community Factors
- Information overload: While multiple and competing sources of information shaped vaccination decisions, according to participants, a key factor related to this was information overload. This factor had the potential to erode any positive gains in vaccine confidence that information from trusted and reliable sources could contribute to. For example, refugees linked the recurring changes in public health information to feelings of confusion, being overwhelmed, and uncertainty, especially with regards to information about the minutiae around risks and effectiveness of various brands of vaccines. While this wasn’t a factor in vaccine refusal per se, it added difficulty in determining personal vaccine confidence and participants highlighted desires to ‘shop around’ for specific vaccines.
- Access to evidence-based information: Evidence-based information was highlighted by refugees and key informants as key to gaining confidence. Access to such information was facilitated by multiple sources, including social media, primary sources, family members, and information sessions at vaccine clinics. While access could be facilitated through different sources, both refugees and key informants identified that evidence-based information helped increase confidence when it was delivered in a timely and trusted manner through personnel such as nurses or doctors prior to vaccination.
- Secondary information sources and personal networks: Another route to information was through secondary sources, such as social media, television, friends, and acquaintances. Refugees shared that these sources frequently delivered information related to the virus and the vaccine, whether they were actively seeking information (such as searching on the internet) or coming it across it more passively (such as hearsay). Family and friendship networks were also flagged as common sources of counsel and information about the vaccine.
- Pre-migration experiences: A more subtle factor in participant accounts was how refugees’ experience in Canada and their pre-migration experiences with vaccine access shaped their outlooks. This contributed to unique perceptions and concerns, such as whether patients perceived vaccination personnel to be open to questions, whether they had a choice in being vaccinated, or comparisons to other countries. Others noted that Canada had broad allowance for variations of personal preference in choosing the vaccine.
- Fatigue, indifference, and booster-specific hesitancy: The dose in question was a factor which influenced whether refugees pursued vaccinations or not. All participant groups shared cases where they, a family member, or a patient who conformed to or were even eager to get first and/or second doses refused subsequent boosters. Justifications for booster refusals varied, with examples of vaccine fatigue, indifference, or not wanting to go beyond the mandatory two doses. Key informants also reported that booster hesitancy trends followed the hesitancy patterns of early doses of the vaccine, with concerns around boosters’ side-effects and risks to subpopulations, with the added layer of fatigue and indifference.
3.4. Societal Factors
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Crawshaw, A.F.; Farah, Y.; Deal, A.; Rustage, K.; Hayward, S.E.; Carter, J.; Knights, F.; Goldsmith, L.P.; Campos-Matos, I.; Wurie, F.; et al. Defining the determinants of vaccine uptake and undervaccination in migrant populations in Europe to improve routine and COVID-19 vaccine uptake: A systematic review. Lancet Infect. Dis. 2022, 22, 254–266. [Google Scholar] [CrossRef]
- Institute for Clinical Evaluative Sciences (ICES). Vaccine Coverage by Neighbourhood COVID-19 Risk in Immigrants, Refugees, and Other Newcomers, up to 26 April 2021. Available online: https://www.ices.on.ca/wp-content/uploads/2023/04/ICES-Report-COVID-19-Vaccine-coverage-by-neighbourhood-risk-among-immigrants.pdf (accessed on 27 November 2022).
- Crawshaw, A.F.; Deal, A.; Rustage, K.; Forster, A.S.; Campos-Matos, I.; Vandrevala, T.; Würz, A.; Pharris, A.; Suk, J.E.; Kinsman, J.; et al. What must be done to tackle vaccine hesitancy and barriers to COVID-19 vaccination in migrants? J. Travel Med. 2021, 28, taab048. [Google Scholar] [CrossRef]
- Eissa, A.; Lofters, A.; Akor, N.; Prescod, C.; Nnorom, O. Increasing SARS-CoV-2 vaccination rates among Black people in Canada. CMAJ 2021, 193, E1220–E1221. [Google Scholar] [CrossRef]
- MacDonald, N.E. SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Tankwanchi, A.S.; Bowman, B.; Garrison, M.; Larson, H.; Wiysonge, C.S. Vaccine hesitancy in migrant communities: A rapid review of latest evidence. Curr. Opin. Immunol. 2021, 71, 62–68. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Ensuring the Integration of Refugees and Migrants in Immunization Policies, Planning and Service Delivery Globally. 2022. Available online: https://www.who.int/publications/i/item/9789240051843 (accessed on 21 November 2022).
- Abdi, I.; Menzies, R.; Seale, H. Barriers and facilitators of immunisation in refugees and migrants in Australia: An east-African case study. Vaccine 2019, 37, 6724–6729. [Google Scholar] [CrossRef]
- Abba-Aji, M.; Stuckler, D.; Galea, S.; McKee, M. Ethnic/racial minorities’ and migrants’ access to COVID-19 vaccines: A systematic review of barriers and facilitators. J. Migr. Health 2022, 5, 100086. [Google Scholar] [CrossRef]
- Kowal, S.P.; Jardine, C.G.; Bubela, T.M. “If they tell me to get it, I’ll get it. If they don’t….”: Immunization decision-making processes of immigrant mothers. Can. J. Public Health 2015, 106, e230–e235. [Google Scholar] [CrossRef] [PubMed]
- Demeke, J.; McFadden, S.M.; Dada, D.; Djiometio, J.N.; Vlahov, D.; Wilton, L.; Wang, M.; Nelson, L.E. Strategies that promote equity in COVID-19 vaccine uptake for undocumented immigrants: A review. J. Community Health 2022, 47, 554–562. [Google Scholar] [CrossRef] [PubMed]
- Wilson, L.; Rubens-Augustson, T.; Murphy, M.; Jardine, C.; Crowcroft, N.; Hui, C.; Wilson, K. Barriers to immunization among newcomers: A systematic review. Vaccine 2018, 36, 1055–1062. [Google Scholar] [CrossRef] [PubMed]
- Greenaway, C.; Hargreaves, S.; Barkati, S.; Coyle, C.M.; Gobbi, F.; Veizis, A.; Douglas, P. COVID-19: Exposing and addressing health disparities among ethnic minorities and migrants. J. Travel Med. 2020, 27, taaa113. [Google Scholar] [CrossRef]
- Mipatrini, D.; Stefanelli, P.; Severoni, S.; Rezza, G. Vaccinations in migrants and refugees: A challenge for European health systems. a systematic review of current scientific evidence. Pathog. Glob. Health 2017, 111, 59–68. [Google Scholar] [CrossRef]
- MacDonald, S.E.; Paudel, Y.R.; Du, C. COVID-19 vaccine coverage among immigrants and refugees in Alberta: A population-based cross-sectional study. J. Glob. Health 2022, 12, 05053. [Google Scholar] [CrossRef]
- National Academies of Sciences, Engineering, and Medicine. Framework for Equitable Allocation of COVID-19 Vaccine; The National Academies Press: Washington, DC, USA, 2020. [Google Scholar] [CrossRef]
- Thomas, C.M.; Osterholm, M.T.; Stauffer, W.M. Critical considerations for COVID-19 vaccination of refugees, immigrants, and migrants. Am. J. Trop. Med. Hyg. 2021, 104, 433–435. [Google Scholar] [CrossRef]
- World Health Organization (WHO) Regional Office for Europe. Delivery of Immunization Services for Refugees and Migrants: Technical Guidance on Refugee and Migrant Health. 2019. Available online: https://apps.who.int/iris/handle/10665/326924 (accessed on 23 November 2022).
- Denford, S.; Mowbray, F.; Towler, L.; Wehling, H.; Lasseter, G.; Amlôt, R.; Oliver, I.; Yardley, L.; Hickman, M. Exploration of attitudes regarding uptake of COVID-19 vaccines among vaccine hesitant adults in the UK: A qualitative analysis. BMC Infect. Dis. 2022, 22, 407. [Google Scholar] [CrossRef] [PubMed]
- Larson, H.; Leask, J.; Aggett, S.; Sevdalis, N.; Thomson, A. A multidisciplinary research agenda for understanding vaccine-related decisions. Vaccines 2013, 1, 293–304. [Google Scholar] [CrossRef] [PubMed]
- Amo-Adjei, J.; Nurzhynska, A.; Essuman, R.; Lohiniva, A.L. Trust and willingness towards COVID-19 vaccine uptake: A mixed-method study in Ghana. Arch. Public Health 2021, 80, 64. [Google Scholar] [CrossRef] [PubMed]
- Romer, D.; Jamieson, K.H. Conspiracy theories as barriers to controlling the spread of COVID-19 in the U.S. Soc. Sci. Med. 2020, 263, 113356. [Google Scholar] [CrossRef] [PubMed]
- Achangwa, C.; Lee, T.J.; Lee, M.S. Acceptance of the COVID-19 vaccine by foreigners in South Korea. Int. J. Environ. Public Health 2021, 18, 12035. [Google Scholar] [CrossRef] [PubMed]
- Aktürk, Z.; Linde, K.; Hapfelmeier, A.; Kunisch, R.; Schneider, A. COVID-19 vaccine hesitancy in people with migratory backgrounds: A cross-sectional study among Turkish- and German-speaking citizens in Munich. BMC Infect. Dis. 2021, 21, 1214. [Google Scholar] [CrossRef] [PubMed]
- Salibi, N.; Abdulrahim, S.; El Haddad, M.; Bassil, S.; El Khoury, Z.; Ghattas, H.; McCall, S.J. COVID-19 vaccine acceptance in older Syrian refugees: Preliminary findings from an ongoing study. Prev. Med. Rep. 2021, 24, 101606. [Google Scholar] [CrossRef] [PubMed]
- West, H.; Lawton, A.; Hossain, S.; Mustafa, G.; Razzaque, A.; Kuhn, R. COVID-19 vaccine hesitancy among Temporary Foreign Workers from Bangladesh. Health Syst. Reform 2021, 7, e1991550. [Google Scholar] [CrossRef] [PubMed]
- Jean Baptiste, A.E.; Wagai, J.; Luce, R.; Masresha, B.; Klinkenberg, D.; Veldhuijzen, I.; Oteri, J.; Dieng, B.; Ikeonu, O.C.; Meleh, S.; et al. Measles outbreak in complex emergency: Estimating vaccine effectiveness and evaluation of the vaccination campaign in Borno State, Nigeria, 2019. BMC Public Health 2021, 21, 437. [Google Scholar] [CrossRef]
- Stadnick, N.A.; Cain, K.L.; Oswald, W.; Watson, P.; Ibarra, M.; Lagoc, R.; Ayers, L.O.; Salgin, L.; Broyles, S.L.; Laurent, L.C.; et al. Co-creating a Theory of Change to advance COVID-19 testing and vaccine uptake in underserved communities. Health Serv. Res. 2022, 57, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Deal, A.; Hayward, S.E.; Huda, M.; Knights, F.; Crawshaw, A.F.; Carter, J.; Hassan, O.B.; Farah, Y.; Ciftci, Y.; Rowland-Pomp, M.; et al. Strategies and action points to ensure equitable uptake of COVID-19 vaccinations: A national qualitative interview study to explore the views of undocumented migrants, asylum seekers, and refugees. J. Migr. Health 2021, 4, 100050. [Google Scholar] [CrossRef] [PubMed]
- Kerrigan, D.; Mantsios, A.; Karver, T.S.; Davis, W.; Taggart, T.; Calabrese, S.K.; Mathews, A.; Robinson, S.; Ruffin, R.; Feaster-Bethea, G.; et al. Context and considerations for the development of community-informed health communication messaging to support equitable uptake of COVID-19 vaccines among communities of color in Washington, DC. J. Racial Ethn. Health Disparities 2023, 10, 395–409. [Google Scholar] [CrossRef]
- Eberhardt, J.; Ling, J.; Horsley, L.; Cunnet, J.; Fryer-Smith, E.; Lant, J.; Edwards, S.; Ross, E. Exploring COVID-19 vaccine confidence with people from Black and Asian backgrounds in England. J. Racial Ethn. Health Disparities 2022, 10, 1899–1909. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Data for Action: Achieving High Uptake of COVID-19 Vaccines. 2021. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-vaccination-demand-planning-2021.1 (accessed on 2 June 2023).
- Mays, N.; Pope, C. Rigour and qualitative research. BMJ 1995, 311, 109–112. [Google Scholar] [CrossRef]
- Berg, B.; Howard, L. Qualitative Research Methods for the Social Sciences, 8th ed.; Pearson Education: Upper Saddle River, NJ, USA, 2012. [Google Scholar]
- Agency for Toxic Substances and Disease Registry. Models and frameworks for the practice of community engagement. In Principles of Community Engagement; Agency for Toxic Substances and Disease Registry: Atlanta, GA, USA, 2015. Available online: https://www.atsdr.cdc.gov/communityengagement/pce_models.html#figure1 (accessed on 1 June 2023).
- Lin, S. COVID-19 pandemic and im/migrants’ elevated health concerns in Canada: Vaccine hesitancy, anticipated stigma, and risk perception of accessing care. J. Immigr. Minor. Health 2022, 24, 896–908. [Google Scholar] [CrossRef]
| Key Informant Breakdown by Position and Gender (n = 13) | |||||||
| Position in Vaccination Systems | Gender (n) | ||||||
| Medical Professionals (n) | Public Health Representatives (n) | Immigrant Serving Agency Staff (n) | Community Advocates (n) | International Medical Graduates and Other Staff (n) | Men | Women | |
| 2 | 2 | 5 | 2 | 2 | 7 | 6 | |
| Refugee and Sponsor Breakdown by Language and Gender (n = 48) | |||||||
| Participant Type (n) | Language of Interview (n) | Gender (n) | |||||
| Dari | Pashto | Arabic | Amharic | English | Men | Women | |
| GAR (n = 39) | 20 | 19 | 26 | 13 | |||
| PSR (n = 6) | 6 | 4 | 2 | ||||
| Sponsor (n = 3) | 1 | 1 | 1 | 1 | 2 | ||
| Vaccine Accessibility/Barriers | Structural Factors | Other Determinants |
|---|---|---|
| Appointment times | Vaccine eligibility | Legal status |
| Booking pathways (skill requirements, complexity, wait times) | Mandates or incentives | Time in Canada |
| Geography and transportation | Access to tailored models | Knowledge of English |
| Availability of reliable information | Public health information | Literacy levels |
| Access to first language information | Pre-migration experiences with health systems | |
| Lack of cultural or faith accommodations | Level of Education | |
| Lack of first language services | ||
| Employer resistance to vaccinations | ||
| English bureaucracy |
| Factors | Responses |
|---|---|
| Individual, interpersonal, and community factors | |
| Concerns about side effects: | “Yes, for the first dose, I was very worried as the rumors were there, and in Kabul they were saying the vaccines are outdated and it may have lots of side effects in the future. I was worried that the side effects could affect me. But in the second dose I was not worried as it was well explained to me what the effects of the vaccine are”. (GAR participant 05) |
| Personal ‘disbelief’ in vaccine necessity or effectiveness and/or preference to avoid medical intervention: | “Personally, I do not believe in COVID vaccine myself and since I have not used lots of medicine since my childhood so I think my body should be able to fight for me”. (GAR participant 20) |
| Concerns about risks to subpopulations: | “Sometimes If there is a pregnant woman or any kids or children [that] are suffering from congenital disease or abnormalities, their parents, they have some concern”. (Key Informant participant 07) |
| Misinformation: | “I have a sister [who] has not visited in a long time just so she doesn’t have to take the vaccine (laughs)…She is the type of person that anything she watched on the news or social media she straight away believes. She was saying no, God forbid, this is bad for you, and all these sorts of stories”. (PSR participant 06) |
| Pre-migration experiences: | “The first two dose were done in Afghanistan… When the COVID vaccine came in, the first 6 months it was only the governmental people who were receptive. No other ordinary person was talking about the vaccine, and no one wanted to get the vaccine. But later everyone wanted to get the vaccine and I had to visit many clinics to be able to get my shot. So eventually after visiting several clinics, I went to a clinic for the vaccination in the morning and I only received at 3 pm, I had to wait for a long time as there were many people who came for vaccination. In Afghanistan the vaccine availability was very low. My third dose was done in Greece”. (GAR participant 02) |
| Fatigue, indifference, and booster-specific hesitancy: | “… As for my wife, she didn’t want to take the third shot, I tried to convince her to take the third shot, but she refused, she said two shots are enough”. (PSR participant 01) |
| Fear of adverse consequences: | “Sometimes If there is a pregnant woman or any kids or children [that] are suffering from congenital disease or abnormalities, their parents, they have some concern”. (Key Informant participant 07) |
| Information overload: | “It was overwhelming, we had some people sit at our desks and agonize over, you know, Moderna or Pfizer. For and you know, and I’m saying it’s Coke or Pepsi. Just you know, just take one right, and but they just like “well I read about this one and it looks like this one is 93% effective. But now we have a new variant, and what if it’s not as effective on the new variant” and you could see people kind of spinning with all this information right and fair enough. Because it was [difficult]. But yeah, we definitely found it was an overwhelming lot of information for a lot of people especially I would say people that have either a medical or a science background were almost overthinking it, too much, too much research”. (Key Informant participant 02) |
| Desire to protect others: | “I did not want to be contagious and transfer COVID to other people, so I went for my vaccination. It was only me who decided to go for vaccination”. (GAR participant 06) |
| Influence of family members: | “If you want me to tell you honestly. I don’t like vaccines. For me, I did not want to get it done. However my husband, you can say he decided for all of us. He said we have to take the vaccine, so we all took the vaccine”. (PSR participant 06) |
| Access to evidence-based information: | “Before my doses of COVID vaccination in Afghanistan and in Canada, they told me about the effects of vaccines. There were nurses both in Afghanistan and in here and I had enough time to ask them any questions. Their behaviour, it was very similar to those in here (Canada) and I think they did well. They made me aware of the effects of vaccine and helped me to be ready mentally for the vaccination. Everyone at the clinic was helpful but I think it was more nurses who were involved”. (GAR participant 20) |
| Secondary information sources and personal networks: | “Social Media, Facebook, TikTok, many stars, like the president, football players all went on and encouraged everyone to go for vaccination. In Greece, there were many nurses and there were some psychiatrists who gave us energy and encouragement to go for vaccination”. (GAR participant 07) |
| Societal factors | |
| Vaccine incentives and mandates: | “I had to get the vaccine as it was a necessity for my work and my travel, so I had to go for vaccination. If it was to myself, I probably may not go for vaccination. My family [also played] a role, and they were very important [as I wanted my] family not to be in any danger of not being vaccinated. It is for the formal things rather than my own choice, traveling to some places want you to have your vaccination”. (GAR participant 20) |
| Shifting public health information: | “[…] so many people took Sinopharm, so many people took Johnson and Johnson [prior to being with our clinic]. And the system just said no, this is not something legit or not something approved by our healthcare system. You have to take a full new series, either Moderna or you have to take Pfizer. In just like 2–3 weeks after that, they put on their website like this is all OK”. (Key Informant participant 01) |
| Accepted vaccines by public health agencies: | “My only suggestion is that during my stay as a refugee, I experienced the hard days. Many of my friends have had five doses of vaccine. Pakistan does not accept the vaccine that was given in Afghanistan. In Canada they do not accept the one that was given in Albania. I suggest that these countries become united, and they accept each other’s vaccine”. (GAR participant 05) |
| Hesitancy Factors | Vaccine Motivating Factors | ||
|---|---|---|---|
| Refusal to be vaccinated | Delay vaccination | Accept vaccine but maintain sentiments of hesitancy | Vaccine confidence |
| Do not believe in vaccine necessity or effectiveness (may be all or specific vaccines) | Preference to wait for more research, more definitive/convincing research, and/or critical mass of vaccination | Mandates/unreasonable consequences | Fear of personal, family or broader social health consequences of not being vaccinated |
| Do not believe in medical intervention globally (medicine, vaccines) and/or belief in body’s inherent capacities | Waiting to see what happens in social networks/anecdotal evidence | Pressure from family members | Access to evidence-based information |
| Vaccine ingredients (not compatible with faith, allergies) | Undecided | Family members at high risk | Personal capacity and ability to navigate competing sources of information |
| Lack of confidence in vaccine effectiveness/potential side effects | Fear of negative side effects, influenced by knowledge sources and personal observation | Pressure from family members | |
| Refusal of booster doses only (possible vaccine fatigue) | Inconvenience/competing priorities | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aghajafari, F.; Wall, L.; Weightman, A.; Ness, A.; Lake, D.; Anupindi, K.; Moorthi, G.; Kuk, B.; Santana, M.; Coakley, A. COVID-19 Vaccinations, Trust, and Vaccination Decisions within the Refugee Community of Calgary, Canada. Vaccines 2024, 12, 177. https://doi.org/10.3390/vaccines12020177
Aghajafari F, Wall L, Weightman A, Ness A, Lake D, Anupindi K, Moorthi G, Kuk B, Santana M, Coakley A. COVID-19 Vaccinations, Trust, and Vaccination Decisions within the Refugee Community of Calgary, Canada. Vaccines. 2024; 12(2):177. https://doi.org/10.3390/vaccines12020177
Chicago/Turabian StyleAghajafari, Fariba, Laurent Wall, Amanda Weightman, Alyssa Ness, Deidre Lake, Krishna Anupindi, Gayatri Moorthi, Bryan Kuk, Maria Santana, and Annalee Coakley. 2024. "COVID-19 Vaccinations, Trust, and Vaccination Decisions within the Refugee Community of Calgary, Canada" Vaccines 12, no. 2: 177. https://doi.org/10.3390/vaccines12020177
APA StyleAghajafari, F., Wall, L., Weightman, A., Ness, A., Lake, D., Anupindi, K., Moorthi, G., Kuk, B., Santana, M., & Coakley, A. (2024). COVID-19 Vaccinations, Trust, and Vaccination Decisions within the Refugee Community of Calgary, Canada. Vaccines, 12(2), 177. https://doi.org/10.3390/vaccines12020177







