Intention to Vaccinate against COVID-19 in Adolescents: A Systematic Review
Abstract
:1. Introduction
Aim
2. Methods
2.1. Data Sources
2.2. Search Strategy
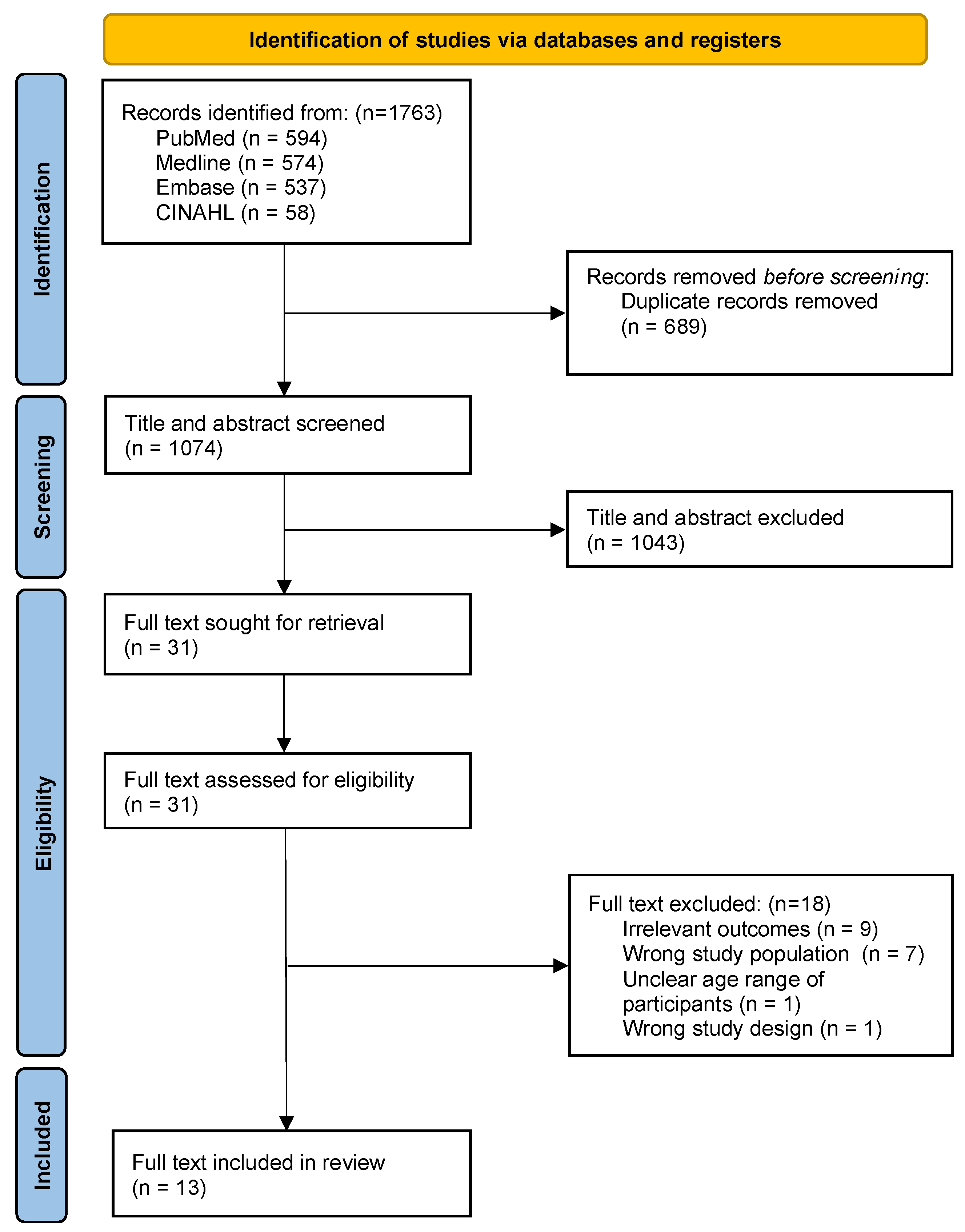
2.3. Data Collection and Study Selection
2.4. Inclusion Criteria
2.5. Exclusion Criteria
2.6. Data Extraction
2.7. Risk of Bias Appraisal
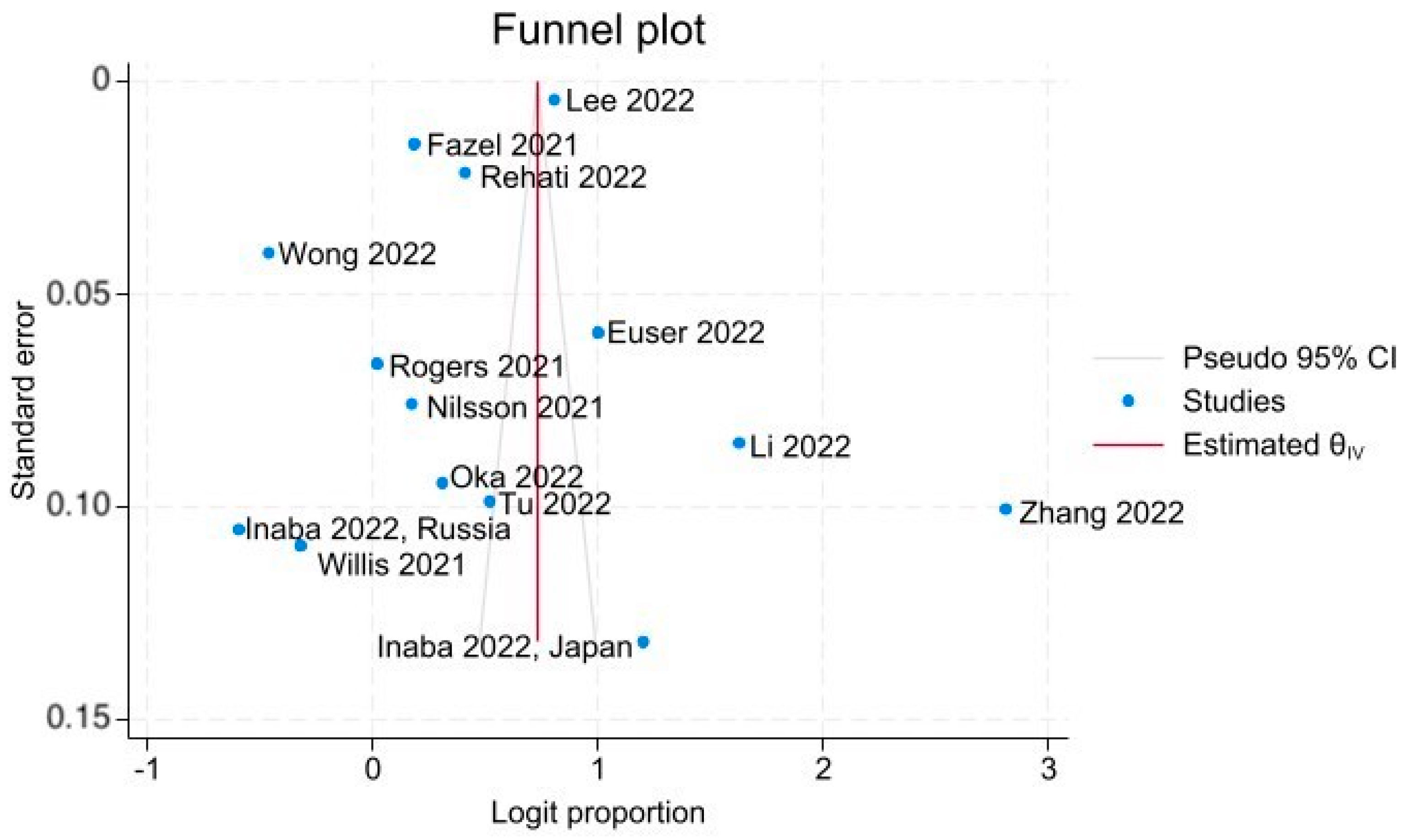
2.8. Publication Bias
2.9. Data Synthesis
2.10. Data Analysis
3. Results
3.1. Study Characteristics
3.2. Intention to Vaccinate against COVID-19 in Adolescents
3.3. Publication Bias
3.4. Factors Influencing Intention to Vaccinate against COVID-19 in Adolescents [48]
3.5. Socio-Demographic Determinants
3.6. Communication about COVID-19 Pandemic and Vaccine Related Factors
3.7. COVID-19 Vaccine-Related Factors
3.8. COVID-19 Infection-Related Factors
3.9. Other Factors
3.10. Risk of Bias in Studies
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Harvey, W.T.; Carabelli, A.M.; Jackson, B.; Gupta, R.K.; Thomson, E.C.; Harrison, E.M.; Ludden, C.; Reeve, R.; Rambaut, A.; COVID-19 Genomics UK (COG-UK) Consortium; et al. SARS-CoV-2 variants, spike mutations and immune escape. Nat. Rev. Microbiol. 2021, 19, 409–424. [Google Scholar] [CrossRef]
- WHO COVID-19 Dashboard [Internet]. Geneva: World Health Organization. 2020. Available online: https://covid19.who.int/ (accessed on 22 February 2023).
- COVID-19 Confirmed Cases and Deaths [Internet]. Available online: https://data.unicef.org/resources/covid-19-confirmed-cases-and-deaths-dashboard/ (accessed on 22 February 2023).
- Frenck, R.W., Jr.; Klein, N.P.; Kitchin, N.; Gurtman, A.; Absalon, J.; Lockhart, S.; Perez, J.L.; Walter, E.B.; Senders, S.; Bailey, R.; et al. Safety, immunogenicity, and efficacy of the BNT162b2 COVID-19 vaccine in adolescents. N. Engl. J. Med. 2021, 385, 239–250. [Google Scholar] [CrossRef]
- Lv, M.; Luo, X.; Shen, Q.; Lei, R.; Liu, X.; Liu, E.; Li, Q.; Chen, Y. Safety, Immunogenicity, and Efficacy of COVID-19 Vaccines in Children and Adolescents: A Systematic Review. Vaccines 2021, 9, 1102. [Google Scholar] [CrossRef]
- Du, Y.; Chen, L.; Shi, Y. Safety, Immunogenicity, and Efficacy of COVID-19 Vaccines in Adolescents, Children, and Infants: A Systematic Review and Meta-Analysis. Front. Public Health 2022, 10, 829176. [Google Scholar] [CrossRef] [PubMed]
- Muscillo, A.; Lombardi, G.; Sestini, E.; Garbin, F.; Tambone, V.; Campanozzi, L.L.; Pin, P. Adolescents’ Opinions on COVID-19 Vaccine Hesitancy: Hints toward Enhancing Pandemic Preparedness in the Future. Vaccines 2023, 11, 967. [Google Scholar] [CrossRef] [PubMed]
- Anthes, E. Younger Adults Are Less Likely to Get Vaccinated than Their Elders, New C.D.C. Studies Say. The New York Times. 2021. Available online: https://www.nytimes.com/2021/06/21/health/vaccination-young-adults.html (accessed on 21 June 2021).
- Scherer, A.M.; Gedlinske, A.M.; Parker, A.M.; Gidengil, C.A.; Askelson, N.M.; Petersen, C.A.; Woodworth, K.R.; Lindley, M.C. Acceptability of Adolescent COVID-19 Vaccination Among Adolescents and Parents of Adolescents—United States, 15–23 April 2021. MMWR Morb. Mortal. Wkly Rep. 2021, 70, 997–1003. [Google Scholar] [CrossRef]
- Schneiderman, M.; Rumain, B.; Kaganovskiy, L.; Geliebter, A. Incidence and Relative Risk of COVID-19 in Adolescents and Youth Compared with Older Adults in 19 US States, Fall 2020. JAMA Netw. Open 2022, 5, e2222126. [Google Scholar] [CrossRef] [PubMed]
- Rumain, B.; Schneiderman, M.; Geliebter, A. Prevalence of COVID-19 in adolescents and youth compared with older adults in states experiencing surges. PLoS ONE 2021, 16, e0242587. [Google Scholar] [CrossRef]
- Marks, K.J.; Whitaker, M.; Anglin, O.; Milucky, J.; Patel, K.; Pham, H.; Chai, S.J.; Kirley, P.D.; Armistead, I.; McLafferty, S.; et al. Hospitalizations of Children and Adolescents with Laboratory-Confirmed COVID-19—COVID-NET, 14 States, July 2021–January 2022. MMWR Morb. Mortal. Wkly Rep. 2022, 71, 271–278. [Google Scholar] [CrossRef]
- Thallapureddy, K.; Thallapureddy, K.; Zerda, E.; Suresh, N.; Kamat, D.; Rajasekaran, K.; Moreira, A. Long-Term Complications of COVID-19 Infection in Adolescents and Children. Curr. Pediatr. Rep. 2022, 10, 11–17. [Google Scholar] [CrossRef]
- Olson, S.M.; Newhams, M.M.; Halasa, N.B.; Price, A.M.; Boom, J.A.; Sahni, L.C.; Pannaraj, P.S.; Irby, K.; Walker, T.C.; Schwartz, S.P.; et al. Effectiveness of BNT162b2 Vaccine against Critical COVID-19 in Adolescents. N. Engl. J. Med. 2022, 386, 713–723. [Google Scholar] [CrossRef]
- Borel, M.; Xie, L.; Kapera, O.; Mihalcea, A.; Kahn, J.; Messiah, S.E. Long-term physical, mental and social health effects of COVID-19 in the pediatric population: A scoping review. World J. Pediatr. 2022, 18, 149–159. [Google Scholar] [CrossRef] [PubMed]
- Stephenson, T.; Pinto Pereira, S.M.; Shafran, R.; de Stavola, B.L.; Rojas, N.; McOwat, K.; Simmons, R.; Zavala, M.; O’Mahoney, L.; Chalder, T.; et al. Physical and mental health 3 months after SARS-CoV-2 infection (long COVID) among adolescents in England (CLoCk): A national matched cohort study. Lancet Child Adolesc. Health 2022, 6, 230–239. [Google Scholar] [CrossRef] [PubMed]
- Amodio, E.; Genovese, D.; Mazzeo, L.; Martino, L.; Restivo, V.; Vella, G.; Calamusa, G.; Vitale, F. Effectiveness of mRNA COVID-19 Vaccines in Adolescents Over 6 Months. Pediatrics 2022, 150, e2022057394. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Zhang, J.; Cai, J.; Deng, X.; Peng, C.; Chen, X.; Yang, J.; Wu, Q.; Chen, X.; Chen, Z. Herd immunity induced by COVID-19 vaccination programs and suppression of epidemics caused by the SARS-CoV-2 Delta variant in China. medRxiv 2021, preprint. [Google Scholar]
- Hess, S.; Lancsar, E.; Mariel, P.; Meyerhoff, J.; Song, F.; van den Broek-Altenburg, E.; Alaba, O.A.; Amaris, G.; Arellana, J.; Basso, L.J.; et al. The path towards herd immunity: Predicting COVID-19 vaccination uptake through results from a stated choice study across six continents. Soc. Sci. Med. 2022, 298, 114800. [Google Scholar] [CrossRef]
- Tan, L.F.; Huak, C.Y.; Siow, I.; Tan, A.J.; Venugopalan, P.M.; Premkumar, A.; Seetharaman, S.K.; Tan, B.Y.Q. The road to achieving herd immunity: Factors associated with Singapore residents’ uptake and hesitancy of the COVID-19 vaccination. Expert. Rev. Vaccines 2022, 21, 561–567. [Google Scholar] [CrossRef]
- CDC. CDC COVID Data Tracker [Internet]. Centers for Disease Control and Prevention. 2023. Available online: https://covid.cdc.gov/covid-data-tracker/#vaccine-confidence (accessed on 4 August 2023).
- Brandenberger, J.; Duchen, R.; Lu, H.; Wanigaratne, S.; Cohen, E.; To, T.; Piché-Renaud, P.-P.; Guttmann, A. COVID-19 Vaccine Uptake in Immigrant, Refugee, and Nonimmigrant Children and Adolescents in Ontario, Canada. JAMA Netw. Open 2023, 6, e2325636. [Google Scholar] [CrossRef]
- Hopcroft, L.E.; Curtis, H.J.; Brown, A.D.; Hulme, W.J.; Andrews, C.D.; Morton, C.E.; Inglesby, P.; Morley, J.; Mehrkar, A.; Bacon, S.C.; et al. First dose COVID-19 vaccine coverage amongst adolescents and children in England: An analysis of 3.21 million patients’ primary care records in situ using OpenSAFELY. Wellcome Open Res. 2023, 8, 70. [Google Scholar] [CrossRef]
- Rane, M.S.; Kochhar, S.; Poehlein, E.; You, W.; Robertson, M.M.; Zimba, R.; Westmoreland, A.D.; Romo, M.L.; Kulkarni, S.G.; Chang, M.; et al. Determinants and Trends of COVID-19 Vaccine Hesitancy and Vaccine Uptake in a National Cohort of US Adults: A Longitudinal Study. Am. J. Epidemiol. 2022, 191, 570–583. [Google Scholar] [CrossRef]
- Marzo, R.R.; Sami, W.; Alam, M.Z.; Acharya, S.; Jermsittiparsert, K.; Songwathana, K.; Pham, N.T.; Respati, T.; Faller, E.M.; Baldonado, A.M.; et al. Hesitancy in COVID-19 vaccine uptake and its associated factors among the general adult population: A cross-sectional study in six Southeast Asian countries. Trop. Med. Health 2022, 50, 4. [Google Scholar] [CrossRef]
- Tan, M.; Straughan, P.T.; Cheong, G. Information trust and COVID-19 vaccine hesitancy amongst middle-aged and older adults in Singapore: A latent class analysis Approach. Soc. Sci. Med. 2022, 296, 114767. [Google Scholar] [CrossRef]
- Wang, G.; Yao, Y.; Wang, Y.; Gong, J.; Meng, Q.; Wang, H.; Wang, W.; Chen, X.; Zhao, Y. Determinants of COVID-19 vaccination status and hesitancy among older adults in China. Nat. Med. 2023, 29, 623–631. [Google Scholar] [CrossRef] [PubMed]
- Afifi, T.O.; Salmon, S.; Taillieu, T.; Stewart-Tufescu, A.; Fortier, J.; Driedger, S.M. Older adolescents and young adults willingness to receive the COVID-19 vaccine: Implications for informing public health strategies. Vaccine 2021, 39, 3473–3479. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Ma, Q.; Liu, H.; Guo, Z. Public attitudes and influencing factors toward COVID-19 vaccination for adolescents/children: A scoping review. Public Health 2022, 205, 169–181. [Google Scholar] [CrossRef] [PubMed]
- Montalti, M.; Rallo, F.; Guaraldi, F.; Bartoli, L.; Po, G.; Stillo, M.; Perrone, P.; Squillace, L.; Dallolio, L.; Pandolfi, P.; et al. Would Parents Get Their Children Vaccinated against SARS-CoV-2? Rate and Predictors of Vaccine Hesitancy According to a Survey over 5000 Families from Bologna, Italy. Vaccines 2021, 9, 366. [Google Scholar] [CrossRef]
- Ruggiero, K.M.; Wong, J.; Sweeney, C.F.; Avola, A.; Auger, A.; Macaluso, M.; Reidy, P. Parents’ Intentions to Vaccinate Their Children against COVID-19. J. Pediatr. Health Care 2021, 35, 509–517. [Google Scholar] [CrossRef]
- Griva, K.; Tan, K.Y.K.; Chan, F.H.F.; Periakaruppan, R.; Ong, B.W.L.; Soh, A.S.E.; Chen, M.I. Evaluating Rates and Determinants of COVID-19 Vaccine Hesitancy for Adults and Children in the Singapore Population: Strengthening Our Community’s Resilience against Threats from Emerging Infections (SOCRATEs) Cohort. Vaccines 2021, 9, 1415. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.; He, Y.; Shi, Y. Parents’ and Guardians’ Willingness to Vaccinate Their Children against COVID-19: A Systematic Review and Meta-Analysis. Vaccines 2022, 10, 179. [Google Scholar] [CrossRef]
- Ruggeri, A.; Gummerum, M.; Hanoch, Y. Braving difficult choices alone: Children’s and adolescents’ medical decision making. PLoS ONE 2014, 9, e103287. [Google Scholar] [CrossRef]
- Euser, S.; Kroese, F.M.; Derks, M.; de Bruin, M. Understanding COVID-19 vaccination willingness among youth: A survey study in the Netherlands. Vaccine 2022, 40, 833–836. [Google Scholar] [CrossRef] [PubMed]
- Fazel, M.; Puntis, S.; White, S.R.; Townsend, A.; Mansfield, K.L.; Viner, R.; Herring, J.; Pollard, A.J.; Freeman, D. Willingness of children and adolescents to have a COVID-19 vaccination: Results of a large whole schools survey in England. EClinicalMedicine 2021, 40, 101144. [Google Scholar] [CrossRef]
- Inaba, H.; Rziankina, M.F.; Hoshino, F.; Takano, K.; Potapova, K.E.; Zhmerenetsky, K.V.; Ishigami, K. Self-Assessment of Health Status and Willingness to Be Vaccinated in Adolescents from the Niigata Prefecture and the Khabarovsk Region during COVID-19. Healthcare 2022, 10, 184. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Choe, Y.J.; Kim, S.; Cho, H.K.; Choi, E.H.; Lee, J.; Bae, H.; Choi, S.-R.; You, M. Attitude and Acceptance of COVID-19 Vaccine in Parents and Adolescents: A Nationwide Survey. J. Adolesc. Health 2022, 71, 164–171. [Google Scholar] [CrossRef]
- Li, T.; Qi, R.; Zhou, Y.-H.; Luo, Y.; Wang, S.-Y.; Chen, B.; Xu, B. Attitudes and Factors Associated with Intention to the Third Dose of COVID-19 Vaccine among Adolescents: A Cross-Sectional Survey in 3 Provinces of China. Disaster Med. Public Health Prep. 2022, 17, e201–e204. [Google Scholar] [CrossRef]
- Nilsson, S.; Mattson, J.; Berghammer, M.; Brorsson, A.L.; Forsner, M.; Jenholt Nolbris, M.; Kull, I.; Olinder, A.L.; Ragnarsson, S.; Rullander, A.-C.; et al. To be or not to be vaccinated against COVID-19—The adolescents’ perspective—A mixed-methods study in Sweden. Vaccine 2021, 9, 100117. [Google Scholar] [CrossRef]
- Oka, P.; Thia, B.W.Q.; Gunalan, S.Z.; Kwan, J.R.Y.; Ng, D.X.; Aau, W.K.; Wee, J.D.; Tan, N.C. Awareness, Barriers and Concerns of Adolescents toward the COVID-19 Vaccine: A Cross-Sectional Study in Singapore. Front. Public Health 2022, 10, 903152. [Google Scholar] [CrossRef]
- Rehati, P.; Amaerjiang, N.; Yang, L.; Xiao, H.; Li, M.; Zunong, J.; Wang, L.; Vermund, S.H.; Hu, Y. COVID-19 Vaccine Hesitancy among Adolescents: Cross-Sectional School Survey in Four Chinese Cities Prior to Vaccine Availability. Vaccines 2022, 10, 452. [Google Scholar] [CrossRef]
- Rogers, A.A.; Cook, R.E.; Button, J.A. Parent and Peer Norms are Unique Correlates of COVID-19 Vaccine Intentions in a Diverse Sample of U.S. Adolescents. J. Adolesc. Health 2021, 69, 910–916. [Google Scholar] [CrossRef]
- Tu, P.; Kotarba, M.; Bier, B.; Clark, R.; Lin, C. Internal and External Motivations and Risk Perception toward COVID-19 Vaccination in Adolescents in the U.S. Vaccines 2022, 10, 697. [Google Scholar] [CrossRef] [PubMed]
- Willis, D.E.; Presley, J.; Williams, M.; Zaller, N.; McElfish, P.A. COVID-19 vaccine hesitancy among youth. Hum. Vaccin. Immunother. 2021, 17, 5013–5015. [Google Scholar] [CrossRef]
- Wong, W.H.S.; Leung, D.; Chua, G.T.; Duque, J.S.R.; Peare, S.; So, H.K.; Chan, S.; Kwan, M.; Ip, P.; Lau, Y. Adolescents’ attitudes to the COVID-19 vaccination. Vaccine 2022, 40, 967–969. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; Li, Y.; Wang, H.; Luo, L.; Wang, P.; Wang, H.; Li, Q.; Meng, Z.; Yang, H.; Liu, Y.; et al. COVID-19 Vaccine Hesitancy among Older Adolescents and Young Adults: A National Cross-Sectional Study in China. Front. Public Health 2022, 10, 877668. [Google Scholar] [CrossRef]
- Joshi, A.; Kaur, M.; Kaur, R.; Grover, A.; Nash, D.; El-Mohandes, A. Predictors of COVID-19 Vaccine Acceptance, Intention, and Hesitancy: A Scoping Review. Front. Public Health 2021, 9, 698111. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.-W.; Wen, W.; Wang, N.; Zhou, M.-Y.; Wang, C.-Y.; Ni, J.; Jiang, J.-J.; Zhang, X.-W.; Feng, Z.-H.; Cheng, Y.-R. COVID-19 vaccination acceptance among healthcare workers and non-healthcare workers in China: A survey. Front. Public Health 2021, 9, 709056. [Google Scholar] [CrossRef] [PubMed]
- Hill, N.E.; Bromell, L.; Tyson, D.F.; Flint, R. Developmental commentary: Ecological perspectives on parental influences during adolescence. J. Clin. Child Adolesc. Psychol. 2007, 36, 367–377. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.H.-S.; Chun, J. Examining the Effects of Parental Influence on Adolescent Smoking Behaviors: A Multilevel Analysis of the Global School-Based Student Health Survey (2003–2011). Nicotine Tob. Res. 2015, 18, 934–942. [Google Scholar] [CrossRef]
- Soh, P.C.-H.; Chew, K.W.; Koay, K.Y.; Ang, P.H. Parents vs. peers’ influence on teenagers’ Internet addiction and risky online activities. Telemat. Inform. 2018, 35, 225–236. [Google Scholar] [CrossRef]
- Kaiser, S.; Kyrrestad, H.; Martinussen, M. Adolescents’ experiences of the information they received about the coronavirus (COVID-19) in Norway: A cross-sectional study. Child Adolesc. Psychiatry Ment. Health 2021, 15, 30. [Google Scholar] [CrossRef]
- Lazarus, J.V.; Wyka, K.; White, T.M.; Picchio, C.A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Ratzan, S.C.; Kamarulzaman, A.; El-Mohandes, A. A survey of COVID-19 vaccine acceptance across 23 countries in 2022. Nat. Med. 2023, 29, 366–375. [Google Scholar] [CrossRef]
- Piltch-Loeb, R.; Harriman, N.W.; Healey, J.; Bonetti, M.; Toffolutti, V.; Testa, M.A.; Su, M.; Savoia, E. COVID-19 Vaccine Concerns about Safety, Effectiveness, and Policies in the United States, Canada, Sweden, and Italy among Unvaccinated Individuals. Vaccines 2021, 9, 1138. [Google Scholar] [CrossRef]
- WHO. Interim Statement on COVID-19 Vaccination for Children and Adolescents: World Health Organisation WHO; 2021 [updated 24th November 2021]. Available online: https://www.who.int/news/item/24-11-2021-interim-statement-on-covid-19-vaccination-for-children-and-adolescents (accessed on 30 March 2023).
- Ahmed, S.; Rasul, M.E.; Cho, J. Social Media News Use Induces COVID-19 Vaccine Hesitancy through Skepticism Regarding Its Efficacy: A Longitudinal Study from the United States. Front. Psychol. 2022, 13, 900386. [Google Scholar] [CrossRef] [PubMed]
- Cascini, F.; Pantovic, A.; Al-Ajlouni, Y.A.; Failla, G.; Puleo, V.; Melnyk, A.; Lontano, A.; Ricciardi, W. Social media and attitudes towards a COVID-19 vaccination: A systematic review of the literature. EClinicalMedicine 2022, 48, 101454. [Google Scholar] [PubMed]
- Loomba, S.; de Figueiredo, A.; Piatek, S.J.; de Graaf, K.; Larson, H.J. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nat. Hum. Behav. 2021, 5, 337–348. [Google Scholar] [CrossRef] [PubMed]
- Ali, K.; Berman, G.; Zhou, H.; Deng, W.; Faughnan, V.; Coronado-Voges, M.; Ding, B.; Dooley, J.; Girard, B.; Hillebrand, W.; et al. Evaluation of mRNA-1273 SARS-CoV-2 vaccine in adolescents. N. Engl. J. Med. 2021, 385, 2241–2251. [Google Scholar] [CrossRef]
- Han, B.; Song, Y.; Li, C.; Yang, W.; Ma, Q.; Jiang, Z.; Li, M.; Lian, X.; Jiao, W.; Wang, L.; et al. Safety, tolerability, and immunogenicity of an inactivated SARS-CoV-2 vaccine (CoronaVac) in healthy children and adolescents: A double-blind, randomised, controlled, phase 1/2 clinical trial. Lancet Infect. Dis. 2021, 21, 1645–1653. [Google Scholar] [CrossRef]
- Tian, F.; Yang, R.; Chen, Z. Safety and efficacy of COVID-19 vaccines in children and adolescents: A systematic review of randomized controlled trials. J. Med. Virol. 2022, 94, 4644–4653. [Google Scholar] [CrossRef]
- Diekema, D.S. Adolescent Brain Development and Medical Decision-making. Pediatrics 2020, 146 (Suppl. S1), S18–S24. [Google Scholar] [CrossRef]
- Coetzee, B.J.; Kagee, A. Structural barriers to adhering to health behaviours in the context of the COVID-19 crisis: Considerations for low- and middle-income countries. Glob. Public Health 2020, 15, 1093–1102. [Google Scholar] [CrossRef]
- American Psychological Association. Literature Review Report: Youth Risk Perception and Decision-Making Related to Health Behaviors in the COVID-19 Era [Internet]. American Psychological Association. 2021. Available online: https://www.apa.org/topics/covid-19/youth-risk-perception.pdf (accessed on 11 November 2021).
- Cohn, L.D.; Macfarlane, S.; Yanez, C.; Imai, W.K. Risk-perception: Differences between adolescents and adults. Health Psychol. 1995, 14, 217. [Google Scholar] [CrossRef]

| No | Study | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Overall Appraisal |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Euser et al., 2021 [35] | Y | Y | Y | U | Y | N | Y | Y | N | Include |
| 2 | Fazel et al., 2021 [36] | Y | Y | Y | Y | N | Y | Y | Y | N | Include |
| 3 | Inaba et al., 2022 [37] | N | Y | Y | Y | N | Y | Y | N | N | Include |
| 4 | Lee et al., 2022 [38] | Y | Y | Y | Y | Y | N | Y | Y | N | Include |
| 5 | Li et al., 2022 [39] | Y | U | Y | Y | Y | N | Y | Y | Y | Include |
| 6 | Nilsson et al., 2021 [40] | Y | N | Y | N | Y | Y | Y | Y | N | Include |
| 7 | Oka et al., 2022 [41] | Y | N | Y | Y | N | N | Y | N | N | Include |
| 8 | Rehati et al., 2022 [42] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Include |
| 9 | Rogers et al., 2021 [43] | Y | Y | Y | Y | Y | N | Y | Y | Y | Include |
| 10 | Tu et al., 2022 [44] | Y | Y | Y | Y | Y | N | Y | Y | N | Include |
| 11 | Willis et al., 2021 [45] | Y | N | Y | Y | Y | Y | Y | Y | Y | Include |
| 12 | Wong et al., 2022 [46] | Y | Y | Y | Y | Y | N | Y | Y | N | Include |
| 13 | Zhang et al., 2022 [47] | Y | Y | Y | Y | Y | N | Y | Y | N | Include |
| Author | Period of Data Collection | Population | Age (Years) | Country | Instrument | Outcome | |
|---|---|---|---|---|---|---|---|
| Vaccine Acceptance | Vaccine Hesitancy | ||||||
| Euser 2022 [35] | June 2021 | 1465 | 16–17 | Netherlands | self-designed questionnaire | 73.1% | 26.9% |
| Fazel 2021 [36] | May to July 2021 | 33,556 ^ | 9–18 | England | Oxford COVID-19 vaccine hesitancy scale, Revised Children’s Anxiety and Depression Scales (RCADS), and Bird Checklist of Adolescent Paranoia (B-CAP) | 54.6% | 45.4% |
| Nilsson 2021 [40] | July to November 2020 | 702 | 15–19 | Sweden | Adapted questionnaire and numerical rating scale to assess anxiety | 54.3% | 45.7% |
| Inaba 2022 [37] | May 2021 | 394 (Russia) | 15 | Russia | self-designed questionnaire | 35.5% | 64.5% |
| Inaba 2022 [37] | July 2021 | 327 (Japan) | 15 | Japan | self-designed questionnaire | 76.9% | 23.1% |
| Lee 2022 [38] | June to July 2021 | 272,914 | 12–17 | Korea | self-designed questionnaire | 69.1% | 30.9% |
| Li 2022 [39] | August to October 2021 | 1847 | 12–17 | China | self-designed questionnaire | 94.3% | 5.7% |
| Rehati 2022 [42] | December 2020 | 9153 | 12–17.5 | China | self-designed questionnaire based on the health belief model | 60.1% | 39.9% |
| Zhang 2022 [47] | March to April 2021 | 2414 * | 16–21 | China | self-designed questionnaire with Psychosocial Index-Young (PSI-Y) and Social Support Rating Scale (SSRS) | 83.5% | 16.5% |
| Oka 2022 [41] | June to November 2021 | 460 | 16–17 | Singapore | face validated self-designed questionnaire | 57.6% | 42.4% |
| Wong 2022 [46] | June 2021 | 2609 | 12–18 | Hong Kong | self-designed questionnaire | 38.6% | 61.4% |
| Rogers 2021 [43] | June 2021 | 916 | 12–17 | United States | self-designed questionnaire | 50.4% | 49.6% |
| Tu 2022 [44] | October to November 2021 | 439 | 13–17 | United States | self-designed questionnaire based on protection motivation theory | 62.6% | 37.4% |
| Willis 2021 [45] | May 2021 | 345 | 12–15 | United States | self-designed questionnaire | 42% | 58% |
| Category | Factor | Number of Studies | References |
|---|---|---|---|
| Socio-demographic | Parental norms (parental acceptance of COVID-19 vaccination) | 4 | [39,43,44,46] |
| Parental wishes for adolescents to be vaccinated | 3 | [35,39,43] | |
| Higher education level | 3 | [35,38,39] | |
| Older age | 3 | [36,39,43] | |
| Subjective health perception | 2 | [38,47] | |
| Male gender | 1 | [40] | |
| Female gender | 1 | [36] | |
| Peer norms | 1 | [43] | |
| Being from rural area | 1 | [39] | |
| Higher parental education | 1 | [43] | |
| Higher household income | 1 | [43] | |
| Asian American or Latinx ethnicity | 1 | [43] | |
| Communication about COVID-19 pandemic and vaccination | Possessing information about vaccine safety | 1 | [44] |
| Want to do what is best according to the government | 1 | [35] | |
| COVID-19 vaccine and related issues | Confidence in vaccine effectiveness | 5 | [35,38,39,42,44] |
| Confidence in vaccine safety | 4 | [35,38,39,44] | |
| Perceived risk-benefit of vaccine | 1 | [38] | |
| COVID-19 infection and related issues | To protect others | 6 | [35,38,40,42,44,46] |
| To protect themselves | 4 | [38,42,44,46] | |
| Life affected by COVID-19 | 2 | [39,46] | |
| Perceived risk of COVID-19 | 2 | [38,42] | |
| Perceived severity of COVID-19 | 2 | [38,44] | |
| Previous quarantine due to COVID-19 | 1 | [39] | |
| Not living with someone with COVID-19 | 1 | [40] | |
| Knowing someone with COVID-19 | 1 | [46] | |
| Others | Return to Pre-COVID-19 lifestyle | 3 | [35,38,44] |
| Relieve public health measures | 3 | [38,40,44] | |
| Increased Anxiety (including COVID-19 related anxiety) | 3 | [38,40,44] | |
| Influenza vaccination in past year | 1 | [46] | |
| Recent childhood vaccination history | 1 | [38] |
| Category | Factor | Number of Studies | References |
|---|---|---|---|
| Socio-demographics | Female gender | 2 | [40,42] |
| Being from urban city | 1 | [42] | |
| Neither parent born in UK | 1 | [36] | |
| Staying in boarding school | 1 | [42] | |
| Lower socioeconomic status | 1 | [36] | |
| History of physical disease | 1 | [47] | |
| Lifestyle (smoking, less exercise) | 1 | [36] | |
| Communication about COVID-19 pandemic and vaccination | Unsure of vaccination application process | 1 | [41] |
| Lack of doctor recommendation | 1 | [42] | |
| Lack of access to vaccine-related information | 1 | [41] | |
| Vaccination conspiracy theories | 1 | [41] | |
| COVID-19 vaccine and related issues | Concerns over vaccine safety | 6 | [35,38,41,43,46,47] |
| Concerns over vaccine effectiveness | 5 | [35,41,43,46,47] | |
| Concerns over long term side effects of vaccine | 4 | [35,41,46,47] | |
| Low perceived necessity | 4 | [35,40,41,43] | |
| Needle phobia | 2 | [38,41] | |
| Fear it may cause them to be infected with COVID-19 | 1 | [43] | |
| High perceived knowledge of COVID-19 vaccine | 1 | [38] | |
| Cost concerns | 1 | [42] | |
| Belief that natural immunity is better than vaccination | 1 | [43] | |
| Unpleasant vaccination experience | 1 | [41] | |
| COVID-19 infection and related issues | Low perceived risk of infection | 3 | [42,44,47] |
| Low perceived risk of severe COVID-19 infection | 2 | [40,49] | |
| Public measures sufficient to prevent COVID-19 infection | 2 | [38,46] | |
| Fear it may affect COVID-19 swab test results | 1 | [41] | |
| Lack of information about COVID-19 | 1 | [42] | |
| Belief that COVID-19 did not influence their lives | 1 | [42] | |
| Others | Less social connection | 2 | [36,45] |
| Not refraining from their normal social activities or group training | 1 | [40] | |
| Do not want interruption to school and studies | 1 | [38] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tan, S.Y.; Oka, P.; Tan, N.C. Intention to Vaccinate against COVID-19 in Adolescents: A Systematic Review. Vaccines 2023, 11, 1393. https://doi.org/10.3390/vaccines11081393
Tan SY, Oka P, Tan NC. Intention to Vaccinate against COVID-19 in Adolescents: A Systematic Review. Vaccines. 2023; 11(8):1393. https://doi.org/10.3390/vaccines11081393
Chicago/Turabian StyleTan, Shyn Yi, Prawira Oka, and Ngiap Chuan Tan. 2023. "Intention to Vaccinate against COVID-19 in Adolescents: A Systematic Review" Vaccines 11, no. 8: 1393. https://doi.org/10.3390/vaccines11081393
APA StyleTan, S. Y., Oka, P., & Tan, N. C. (2023). Intention to Vaccinate against COVID-19 in Adolescents: A Systematic Review. Vaccines, 11(8), 1393. https://doi.org/10.3390/vaccines11081393






