Mpox Vaccination Hesitancy and Its Associated Factors among Men Who Have Sex with Men in China: A National Observational Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Measurement
2.3. Data Analysis
3. Results
3.1. Population Characteristics
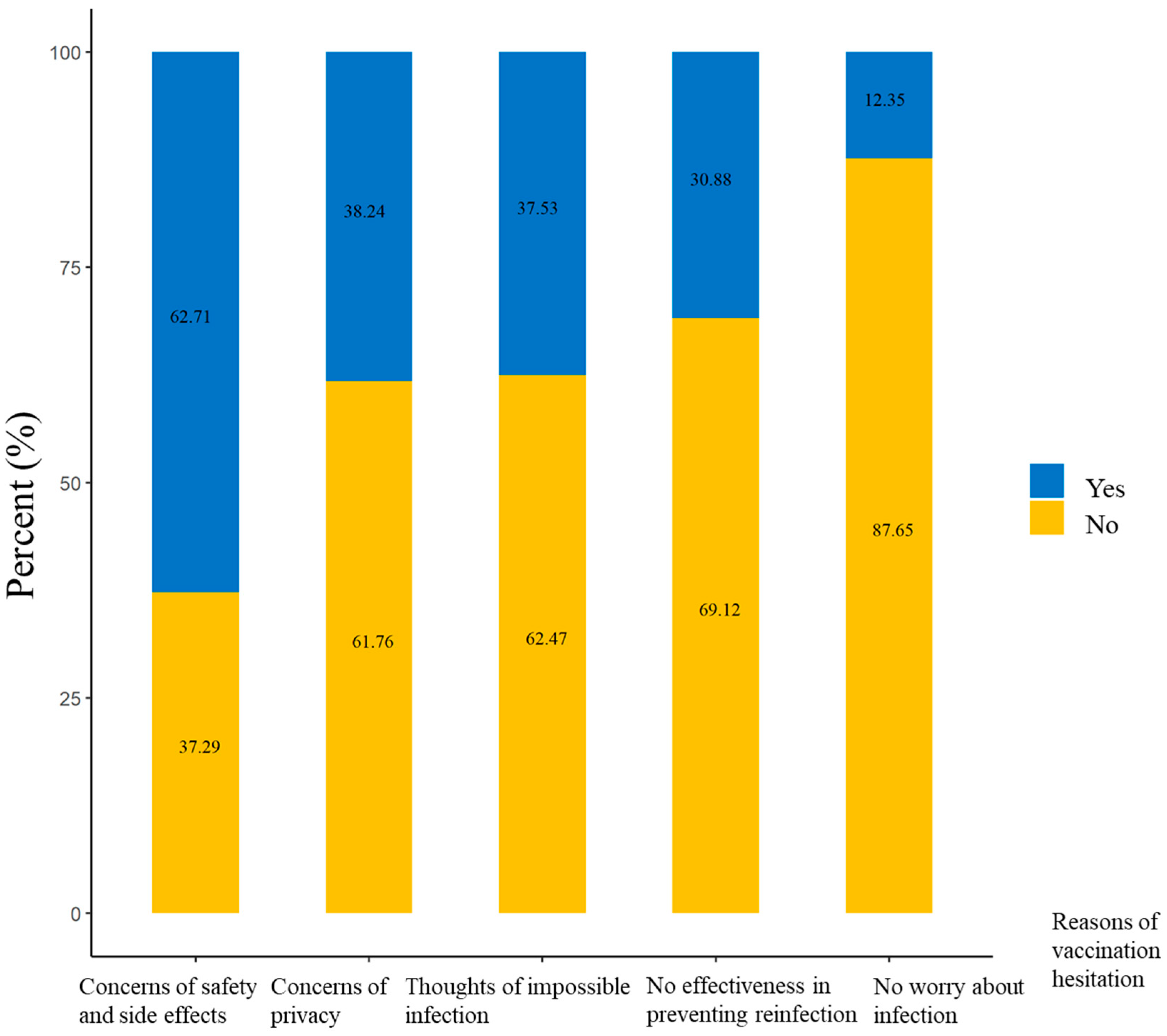
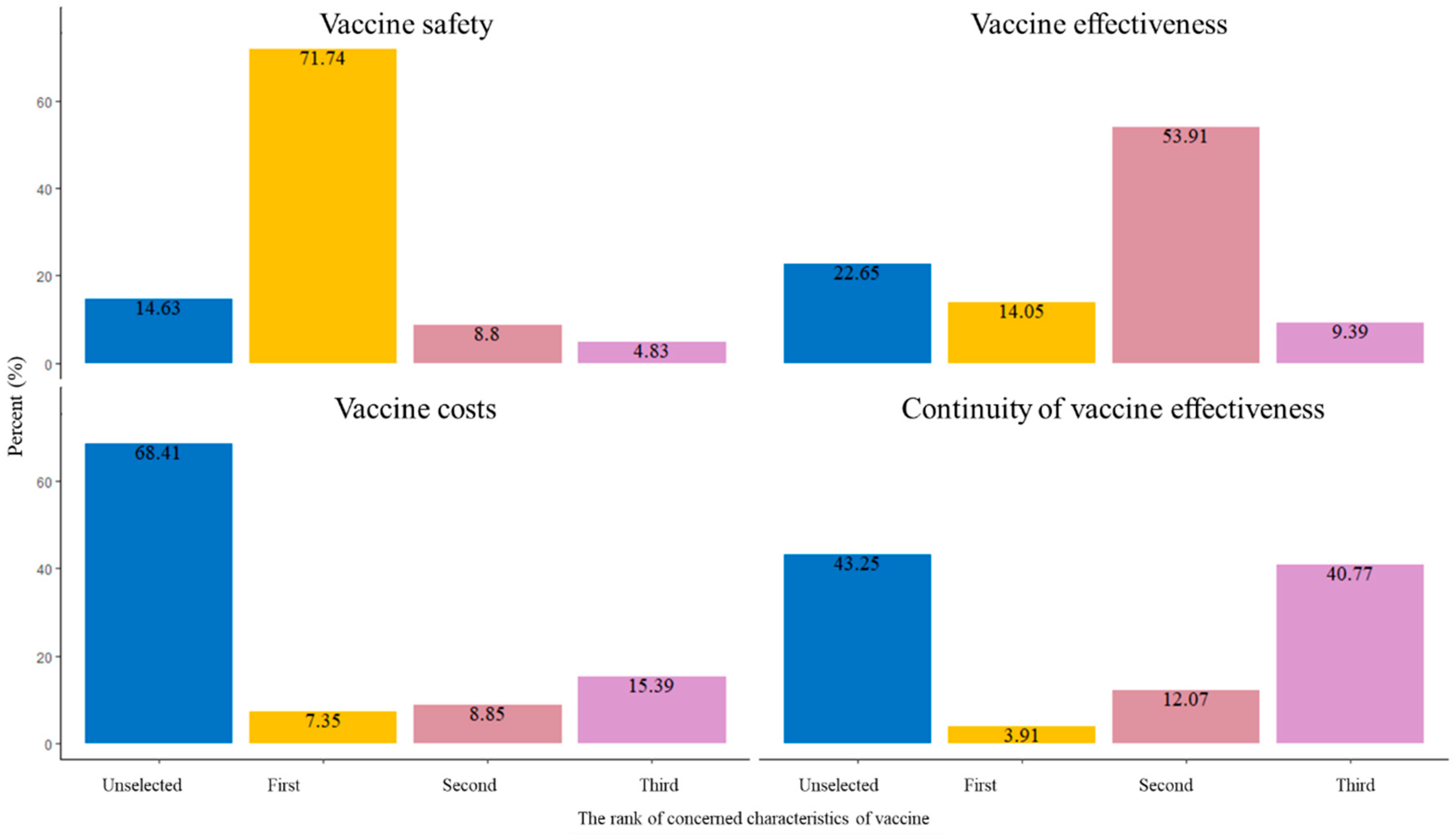
3.2. Reasons for Mpox Vaccination Hesitation and the Concerning Characteristics of Vaccines
3.3. Influencing Factors of Mpox Vaccination Hesitation
3.4. Influencing Factors of Mpox Vaccination Hesitation by HIV Status
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Financial Disclosures
References
- Walter, K.; Malani, P.N. What Is Monkeypox? JAMA 2022, 328, 222. [Google Scholar] [CrossRef] [PubMed]
- Mukinda, V.B.; Mwema, G.; Kilundu, M.; Heymann, D.; Khan, A.; Esposito, J. Re-emergence of human monkeypox in Zaire in 1996. Monkeypox Epidemiologic Working Group. Lancet 1997, 349, 1449–1450. [Google Scholar] [CrossRef]
- Rezza, G. Emergence of human monkeypox in west Africa. Lancet Infect. Dis. 2019, 19, 797–799. [Google Scholar] [CrossRef]
- Ng, O.T.; Lee, V.; Marimuthu, K.; Vasoo, S.; Chan, G.; Lin, R.T.P.; Leo, Y.S. A case of imported Monkeypox in Singapore. Lancet Infect. Dis. 2019, 19, 1166. [Google Scholar] [CrossRef]
- Costello, V.; Sowash, M.; Gaur, A.; Cardis, M.; Pasieka, H.; Wortmann, G.; Ramdeen, S. Imported Monkeypox from International Traveler, Maryland, USA 2021. Emerg. Infect. Dis. 2022, 28, 1002–1005. [Google Scholar] [CrossRef]
- Vaughan, A.; Aarons, E.; Astbury, J.; Balasegaram, S.; Beadsworth, M.; Beck, C.R.; Chand, M.; O’connor, C.; Dunning, J.; Ghebrehewet, S.; et al. Two cases of monkeypox imported to the United Kingdom, September 2018. Eurosurveillance 2018, 23, 1800509. [Google Scholar] [CrossRef]
- Second Meeting of the International Health Regulations (2005) (IHR) Emergency Committee Regarding the Multi-Country Outbreak of Monkeypox. Available online: https://www.who.int/news/item/23-07-2022-second-meeting-of-the-international-health-regulations-(2005)-(ihr)-emergency-committee-regarding-the-multi-country-outbreak-of-monkeypox (accessed on 13 August 2023).
- 2022 Monkeypox and Orthopoxvirus Outbreak Global Map. Available online: https://www.cdc.gov/poxvirus/monkeypox/response/2022/world-map.html (accessed on 13 August 2023).
- Laurenson-Schafer, H.; Sklenovská, N.; Hoxha, A.; Kerr, S.M.; Ndumbi, P.; Fitzner, J.; Almiron, M.; de Sousa, L.A.; Briand, S.; Cenciarelli, O.; et al. Description of the first global outbreak of mpox: An analysis of global surveillance data. Lancet Glob. Health 2023, 11, e1012–e1023. [Google Scholar] [CrossRef] [PubMed]
- Du, M.; Sun, H.; Zhang, S.; Yuan, J.; Yan, W.; Liu, Q.; Qin, C.; Liu, M.; Liu, J. Global Epidemiological Features of Human Monkeypox Cases and Their Associations With Social-Economic Level and International Travel Arrivals: A Systematic Review and Ecological Study. Int. J. Public Health 2023, 68, 1605426. [Google Scholar] [CrossRef]
- Poland, G.A.; Kennedy, R.B.; Tosh, P.K. Prevention of monkeypox with vaccines: A rapid review. Lancet Infect. Dis. 2022, 22, e349–e358. [Google Scholar] [CrossRef] [PubMed]
- 2022 Monkeypox Outbreak: Global Trends. Available online: https://worldhealthorg.shinyapps.io/mpx_global/ (accessed on 25 August 2023).
- Chinese Center for Disease Control and Prevention. Surveillance of Mpox Outbreak in July. Available online: https://www.chinacdc.cn/jkzt/crb/qt/szkb_13037/gwjszl_13092/202308/t20230809_268502.html (accessed on 13 August 2023).
- Notice on the Issuance of Monkeypox Diagnosis and Treatment Guidelines (2022 Edition). Available online: http://www.nhc.gov.cn/yzygj/s7653p/202206/d687b12fe8b84bbfaede2c7a5ca596ec.shtml20220711 (accessed on 13 August 2023).
- General Administration of Customs Announcement No. 65 of 2022 (Announcement on Preventing Monkeypox Epidemic from Entering China). Available online: http://www.customs.gov.cn/customs/302249/302266/302267/4482275/index.html (accessed on 13 August 2023).
- Chinese Center for Disease Control and Prevention. Mpox Prevention and Control Program. Available online: https://www.chinacdc.cn/ (accessed on 13 August 2023).
- Zhou, L.; Wang, Y.; Li, D.; Han, M.; Shi, G.; Li, Q. Consideration of Monkeypox Surveillance in China, 2022. China CDC Wkly. 2022, 4, 924–928. [Google Scholar]
- World Health Organization. Vaccines and Immunization for Monkeypox: Interim Guidance, 24 August 2022. Available online: https://www.who.int/news/item/24-08-2022-vaccines-and-immunization-for-monkeypox--interim-guidance--14-june-2022 (accessed on 13 August 2023).
- Xu, M.; Liu, C.; Du, Z.; Bai, Y.; Wang, Z.; Gao, C. Real-world effectiveness of mpox (monkeypox) vaccines: A systematic review. J. Travel Med. 2023, taad048. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Peng, X.; Li, Y.; Fu, L.; Tian, T.; Liang, B.; Sun, Y.; Chen, Y.; Wu, X.; Liu, Q.; et al. Perceptions, precautions, and vaccine acceptance related to monkeypox in the public in China: A cross-sectional survey. J. Infect. Public Health 2023, 16, 163–170. [Google Scholar] [CrossRef]
- Peng, X.; Wang, B.; Li, Y.; Chen, Y.; Wu, X.; Fu, L.; Sun, Y.; Liu, Q.; Lin, Y.-F.; Liang, B.; et al. Perceptions and worries about monkeypox, and attitudes towards monkeypox vaccination among medical workers in China: A cross-sectional survey. J. Infect Public Health 2023, 16, 346–353. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Li, Y.; Fu, L.; Zhou, X.; Wu, X.; Wang, B.; Peng, X.; Sun, Y.; Liu, Q.; Lin, Y.-F.; et al. Knowledge of Human Mpox (Monkeypox) and Attitude towards Mpox Vaccination among Male Sex Workers in China: A Cross-Sectional Study. Vaccines 2023, 11, 285. [Google Scholar] [CrossRef]
- Li, Y.; Peng, X.; Fu, L.; Wang, B.; Sun, Y.; Chen, Y.; Lin, Y.; Wu, X.; Liu, Q.; Gao, Y.; et al. Monkeypox awareness and low vaccination hesitancy among men who have sex with men in China. J. Med Virol. 2023, 95, e28567. [Google Scholar] [CrossRef]
- Zheng, M.; Qin, C.; Qian, X.; Yao, Y.; Liu, J.; Yuan, Z.; Ma, L.; Fan, J.; Tao, R.; Zhou, F.; et al. Knowledge and vaccination acceptance toward the human monkeypox among men who have sex with men in China. Front. Public Health 2022, 10, 997637. [Google Scholar] [CrossRef] [PubMed]
- Fu, L.; Sun, Y.; Li, Y.; Wang, B.; Yang, L.; Tian, T.; Wu, X.; Peng, X.; Liu, Q.; Chen, Y.; et al. Perception of and Vaccine Readiness towards Mpox among Men Who Have Sex with Men Living with HIV in China: A Cross-Sectional Study. Vaccines 2023, 11, 528. [Google Scholar] [CrossRef]
- Zheng, M.; Chen, W.; Qian, X.; Tao, R.; Ma, L.; Zhou, F.; Zhu, Z.; Yao, Y.; Yang, G. Awareness of mpox-related knowledge among men who have sex with men in China. BMC Public Health 2023, 23, 600. [Google Scholar] [CrossRef]
- Newsum, A.M.; Matser, A.; Schinkel, J.; van der Valk, M.; Brinkman, K.; van Eeden, A.; Lauw, F.N.; A Rijnders, B.J.; van de Laar, T.J.W.; van de Kerkhof, M.; et al. Incidence of HCV Reinfection Among HIV-Positive MSM and Its Association with Sexual Risk Behavior: A Longitudinal Analysis. Clin. Infect Dis. 2021, 73, 460–467. [Google Scholar] [CrossRef]
- Braun, D.L.; Marzel, A.; Steffens, D.; Schreiber, P.W.; Grube, C.; Scherrer, A.U.; Kouyos, R.D.; Günthard, H.F.; Anagnostopoulos, A.; Aubert, V.; et al. High Rates of Subsequent Asymptomatic Sexually Transmitted Infections and Risky Sexual Behavior in Patients Initially Presenting with Primary Human Immunodeficiency Virus-1 Infection. Clin. Infect. Dis. 2018, 66, 735–742. [Google Scholar] [CrossRef]
- Winters, M.; Malik, A.A.; Omer, S.B. Attitudes towards Monkeypox vaccination and predictors of vaccination intentions among the US general public. PLoS ONE 2022, 17, e0278622. [Google Scholar] [CrossRef] [PubMed]
- Sahin, T.K.; Erul, E.; Aksun, M.S.; Sonmezer, M.C.; Unal, S.; Akova, M. Knowledge and Attitudes of Turkish Physicians towards Human Monkeypox Disease and Related Vaccination: A Cross-Sectional Study. Vaccines 2023, 11, 19. [Google Scholar] [CrossRef] [PubMed]
- Yan, W.; Du, M.; Qin, C.; Liu, Q.; Wang, Y.; Liang, W.; Liu, M.; Liu, J. Association between public attention and monkeypox epidemic: A global lag-correlation analysis. J. Med. Virol. 2023, 95, e28382. [Google Scholar] [CrossRef] [PubMed]
- Du, M.; Qin, C.; Yan, W.; Liu, Q.; Wang, Y.; Zhu, L.; Liang, W.; Liu, M.; Liu, J. Trends in Online Search Activity and the Correlation with Daily New Cases of Monkeypox among 102 Countries or Territories. Int. J. Environ. Res. Public Health 2023, 20, 3395. [Google Scholar] [CrossRef]
| Characteristics | Overall (n, %) | Vaccination Acceptance (n, %) | Vaccination Hesitation (n, %) | p-Value |
|---|---|---|---|---|
| 7538 | 7117 (94.41) | 421 (5.59) | ||
| Age group (years) | <0.001 | |||
| 18–35 | 5463 (72.47) | 5190 (95.00) | 273 (5.00) | |
| 36–59 | 1941 (25.75) | 1813 (93.41) | 128 (6.59) | |
| ≥60 | 134 (1.78) | 114 (85.07) | 20 (14.93) | |
| Occupation | <0.001 | |||
| Employed | 6744 (89.47) | 6390 (94.75) | 354 (5.25) | |
| Unemployed | 794 (10.53) | 727 (91.56) | 67 (8.44) | |
| Education level | 0.006 | |||
| Junior high school and below | 664 (8.81) | 611 (92.02) | 53 (7.98) | |
| High school | 2990 (39.67) | 2831 (94.68) | 159 (5.32) | |
| Undergraduate | 3126 (41.47) | 2970 (95.01) | 156 (4.99) | |
| Postgraduate and above | 758 (10.06) | 705 (93.01) | 53 (6.99) | |
| Marital status | 0.001 | |||
| Married | 1008 (13.37) | 930 (92.26) | 78 (7.74) | |
| Unmarried | 5993 (79.50) | 5689 (94.93) | 304 (5.07) | |
| Widowed or divorced | 537 (7.12) | 498 (92.74) | 39 (7.26) | |
| Ethnicity | 0.05 | |||
| Han | 6773 (89.85) | 6407 (94.60) | 366 (5.40) | |
| Minorities | 765 (10.15) | 710 (92.81) | 55 (7.19) | |
| Residence | 0.425 | |||
| Eastern region | 3351 (44.45) | 3162 (94.36) | 189 (5.64) | |
| Western region | 2640 (35.02) | 2503 (94.81) | 137 (5.19) | |
| Central region | 1547 (20.52) | 1452 (93.86) | 95 (6.14) | |
| Sexual orientation | 0.006 | |||
| MSM | 5695 (75.55) | 5401 (94.84) | 294 (5.16) | |
| Bisexual or unsure | 1843 (24.45) | 1716 (93.11) | 127 (6.89) | |
| Risky sexual behavior | 0.017 | |||
| Low | 6003 (79.64) | 5688 (94.75) | 315 (5.25) | |
| Moderate | 1469 (19.49) | 1370 (93.26) | 99 (6.74) | |
| High | 66 (0.88) | 59 (89.39) | 7 (10.61) | |
| Mpox-related knowledge | <0.001 | |||
| Low | 537 (7.12) | 459 (85.47) | 78 (14.53) | |
| Moderate | 636 (8.44) | 583 (91.67) | 53 (8.33) | |
| High | 6365 (84.44) | 6075 (95.44) | 290 (4.56) | |
| Mpox virus infection | 0.009 | |||
| No | 7483 (99.27) | 7070 (94.48) | 413 (5.52) | |
| Yes | 55 (0.73) | 47 (85.45) | 8 (14.55) | |
| Sexual disease scores | 0.284 | |||
| 0 | 4798 (63.65) | 4517 (94.14) | 281 (5.86) | |
| 1~3 | 2688 (35.66) | 2552 (94.94) | 136 (5.06) | |
| 4~5 | 52 (0.69) | 48 (92.31) | 4 (7.69) |
| Characteristics | aOR (95% CI) | p-Value |
|---|---|---|
| Age group (years) | ||
| 18–35 | 1 (reference) | |
| 36–59 | 1.20 (0.93, 1.55) | 0.160 |
| ≥60 | 2.25 (1.31, 3.88) | 0.003 |
| Occupation | ||
| Employed | 1 (reference) | |
| Unemployed | 1.66 (1.25, 2.19) | <0.001 |
| Education level | ||
| Junior high school and below | 1 (reference) | |
| High school | 0.91 (0.65, 1.28) | 0.592 |
| Undergraduate | 1.03 (0.72, 1.46) | 0.887 |
| Postgraduate and above | 1.55 (1.01, 2.37) | 0.043 |
| Marital status | ||
| Married | 1 (reference) | |
| Unmarried | 0.81 (0.59, 1.10) | 0.173 |
| Widowed or divorced | 0.94 (0.62, 1.42) | 0.773 |
| Sexual orientation | ||
| MSM | 1 (reference) | |
| Bisexual or unsure | 1.21 (0.96, 1.53) | 0.106 |
| Risky sexual behavior | ||
| Low | 1 (reference) | |
| Moderate | 1.17 (0.92, 1.50) | 0.195 |
| High | 1.40 (0.60, 3.22) | 0.435 |
| Mpox-related knowledge | ||
| Low | 1 (reference) | |
| Moderate | 0.53 (0.36, 0.77) | <0.0001 |
| High | 0.30 (0.23, 0.40) | <0.0001 |
| Mpox virus infection | ||
| No | 1 (reference) | |
| Yes | 2.38 (1.08, 5.23) | 0.031 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zheng, M.; Du, M.; Yang, G.; Yao, Y.; Qian, X.; Zhi, Y.; Ma, L.; Tao, R.; Zhu, Z.; Zhou, F.; et al. Mpox Vaccination Hesitancy and Its Associated Factors among Men Who Have Sex with Men in China: A National Observational Study. Vaccines 2023, 11, 1432. https://doi.org/10.3390/vaccines11091432
Zheng M, Du M, Yang G, Yao Y, Qian X, Zhi Y, Ma L, Tao R, Zhu Z, Zhou F, et al. Mpox Vaccination Hesitancy and Its Associated Factors among Men Who Have Sex with Men in China: A National Observational Study. Vaccines. 2023; 11(9):1432. https://doi.org/10.3390/vaccines11091432
Chicago/Turabian StyleZheng, Min, Min Du, Guanghong Yang, Yongming Yao, Xiaohan Qian, Yuan Zhi, Lin Ma, Rui Tao, Zhilin Zhu, Feng Zhou, and et al. 2023. "Mpox Vaccination Hesitancy and Its Associated Factors among Men Who Have Sex with Men in China: A National Observational Study" Vaccines 11, no. 9: 1432. https://doi.org/10.3390/vaccines11091432
APA StyleZheng, M., Du, M., Yang, G., Yao, Y., Qian, X., Zhi, Y., Ma, L., Tao, R., Zhu, Z., Zhou, F., Dai, S., Yang, J., Liu, M., & Liu, J. (2023). Mpox Vaccination Hesitancy and Its Associated Factors among Men Who Have Sex with Men in China: A National Observational Study. Vaccines, 11(9), 1432. https://doi.org/10.3390/vaccines11091432







