Efficiency of Chitosan Nanocarriers in Vaccinology for Mucosal Immunization
Abstract
1. Introduction
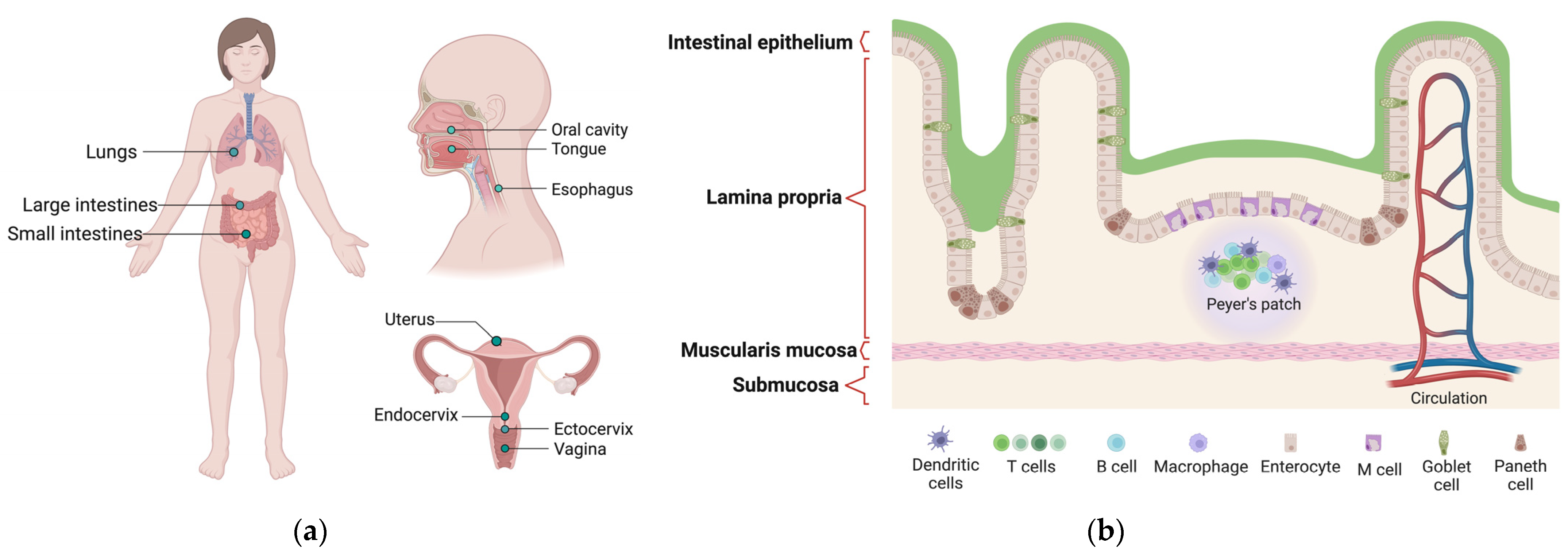
2. Mucosal Structure
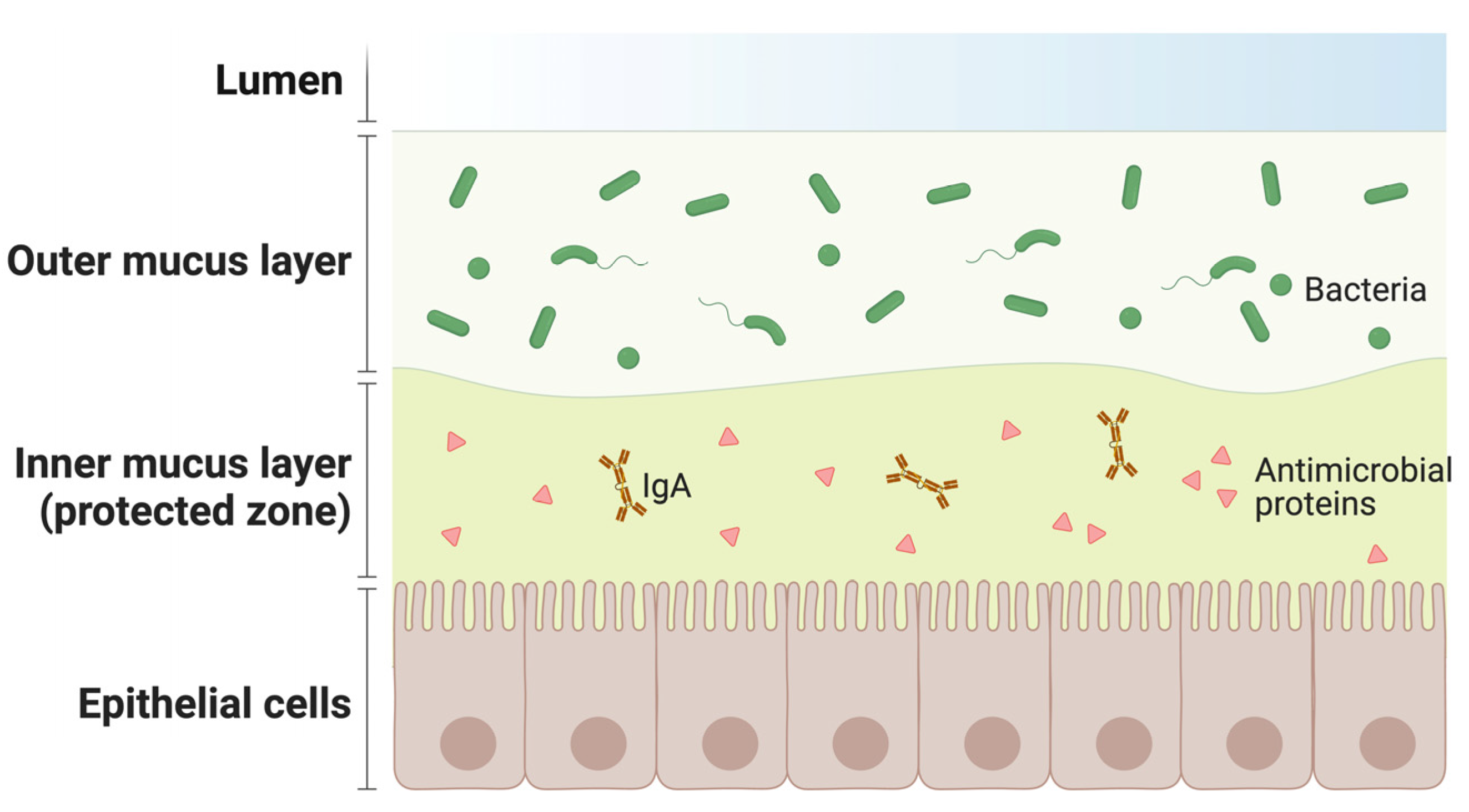
- The epithelial layer is the most superficial. Epithelial cells secrete a thick, gel-like mucus that protects the body from irritants and gives the mucous membrane its name. There may be one or more layers of cells and they may be stacked in columns or arranged like bricks. Epithelial cells also have a high turnover rate, frequently replacing each other to clear out invasive particles. Some cells in this layer have small complex structures called cilia, which help to remove extraneous substances.
- The lamina layer is a connective tissue to which the epithelium attaches, and it is considered the middle layer of the mucosa. The lamina is composed of structural protein molecules, nerves and veins. It thus plays a crucial role in blood supply to the epithelium, keeping cells in place and binding them to the underlying smooth muscle. Its nerves respond to muscle fluctuations to change the shape of the epithelium as needed. Several varieties of immune cells are present in this layer seeking out and destroying intrusive microbes.
- The deeper layer is named muscularis mucosae, as it is mainly composed of smooth muscles. The muscularis mucosae provides a perpetual motor function that keeps the mucosa moving. This dynamic feature helps the lining to stretch and contract along with the various organs of the digestive system during their activity. In addition, it helps the mucous membrane to perform cleaning functions by keeping the hair-like cilia moving on the surface layer cells.
3. Needle-Free Vaccines and Mucosal Vaccination
4. Mucosal Immunity and Immunization
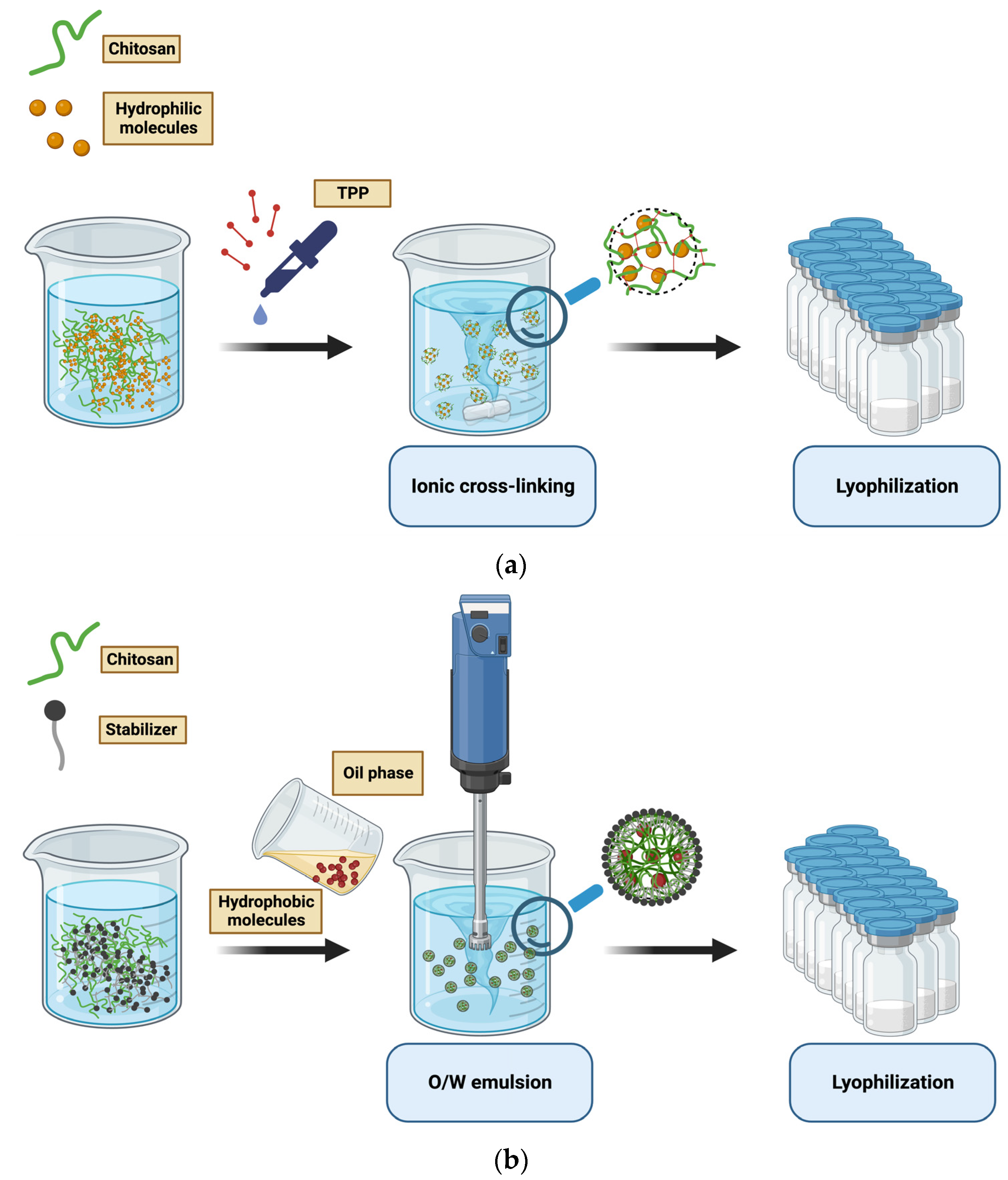
5. Chitosan in Mucosal Vaccine Design
6. Chitosan Outcome in SARS-CoV-2 Immunization
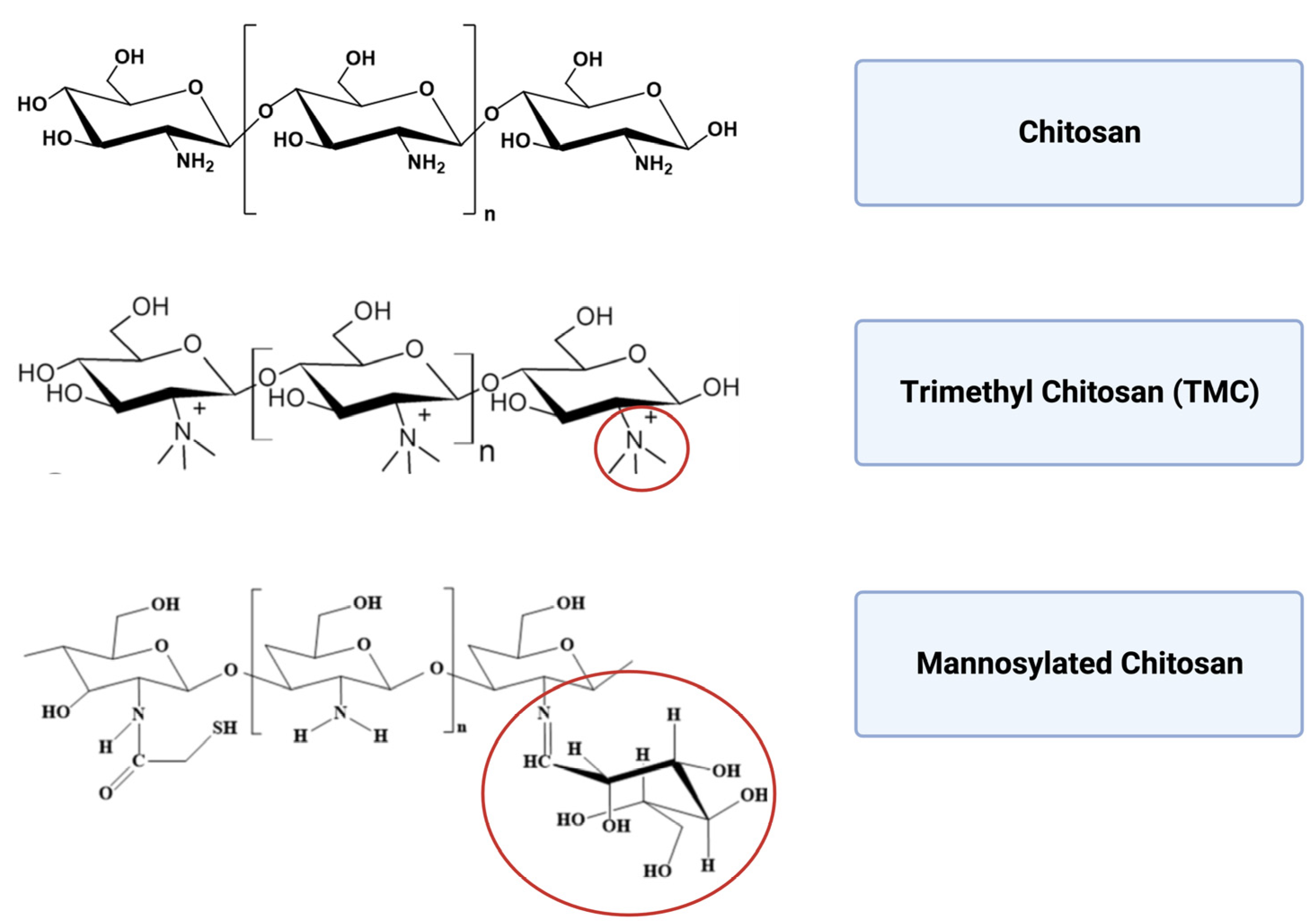
7. Modified Chitosan Nanocarriers and Pre-Clinical Trials
7.1. Trimethyl Chitosan
7.2. Mannosylated Chitosan
7.3. Chitosan Hydrogel
| Chitosan-Based Nanocarriers | Antigen | Application | Activity and Immune Response | Advantages and Disadvantages | Administration Route | Reference |
|---|---|---|---|---|---|---|
| Trimethyl chitosan | Ovalbumin | Prevention of respiratory infectious diseases | Eliciting sIgA levels in the mucosa | High water solubility and increased stability | Intranasal | [48,55,56,57] |
| Penetration of the mucosal epithelium and boosting the antigen presentation | Preserving the mucoadhesive properties and favouring the tight junctions crossing of epithelial cells | |||||
| Upregulation of B lymphocyte | ||||||
| Bacterial toxin | Prevention against Tetanus | IgA secretion in saliva and IgG were detected in blood serum | Decrease in nanoparticle size than non-modified chitosan | Intranasal | [58] | |
| Increasing the secretion of several proinflammatory cytokines and chemokines | Increased cellular uptake | |||||
| Increased loading efficiency and stronger positive surface | ||||||
| Domain III of dengue serotype-3 E protein | Prevention of tropical infectious diseases | Increase the secretion of several proinflammatory cytokines and chemokines | Intranasal | [52] | ||
| Up-regulation of maturation markers (CD80, CD83, CD86 and HLA-DR) for dendritic cells | ||||||
| Hepatitis B surface antigen | Immunization against Hepatitis B virus | Induced T cell proliferation and increased serum and nasal antibody titer | Intranasal | [59] | ||
| Omp31 | Protection against Brucellosis | Eliciting the Th1–Th17 immune response | Oral | [60] | ||
| O-2ʹ-HACC/pFDNA | Complete protection to Newcastle disease virus | Massive production of anti-NDV IgG and sIgA antibodies and increased lymphocyte proliferation | Intranasal | [61] | ||
| High levels of IL-2, IL-4, IFN-γ, CD4+ and CD8+ T lymphocytes | ||||||
| Mannosylated chitosan | MSC-DNA | Protection against Mycobacterium tuberculosis | Increase SIgA production in C57BL mice | Enhance chitosan nanoparticle uptake by APCs | Intranasal | [62,64] |
| Trigger a poly-functional CD4+/CD8+ T responses | ||||||
| Chitosan hydrogel | Influenza virus peptides | Protection against Influenza virus | Increase the proliferation of tissue resident memory CD8+ T cells within the nasal mucosa | Improve the antigen retention time | Intranasal | [65] |
| Confers high protective local immunity |
8. Chitosan-Based Vaccines in Clinical Trials
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AIDS | Acquired Immune Deficiency Syndrome |
| ASCs | Antibody secreting cells |
| APCs | Antigen presenting cells |
| AUC0→4 h | Area under the concentration time-curve |
| DC | Dendritic cells |
| EDIII-D3 | Domain III of dengue serotype-3 E protein |
| FDA | Food and Drug Administration |
| GRAS | Generally recognized as safe |
| HBV | Hepatitis B virus |
| HLA-DR | Human Leukocyte Antigen–DR isotype |
| HPV | Human Papilloma Virus infection |
| IgA | Immunoglobulin A |
| IBD | Inflammatory bowel disease |
| LNTI | Lymph node targeting index |
| MCS | Mannosylated chitosan |
| NPs | Nanoparticles |
| NDV | Newcastle disease virus |
| NALT | Nose-associated lymphoid tissue |
| O/W | Oil in water |
| OVA-NP | Ovalbumin-conjugated N-trimethylaminoethylmethacrylate chitosan NPs |
| SIgA | Secretory IgA |
| SBA | Serum bactericidal antibody |
| SARS | Severe acute respiratory syndrome |
| SARS-CoV-2 | Severe acute respiratory syndrome coronavirus 2 |
| (S@CS)NPs | Spike protein-loaded chitosan NPs |
| TMC(TT) NPs | Tetanus toxoid loaded TMC NPs |
| TRMT | Tissue-resident memory T |
| TMC | Trimethyl chitosan |
| VLP | Virus-like particle |
| WHO | World Health Organization |
References
- Nabel, G.J. Designing Tomorrow’s Vaccines. N. Engl. J. Med. 2013, 368, 551–560. [Google Scholar] [CrossRef]
- Lin, C.-H.; Lin, C.-J.; Kuo, Y.-W.; Wang, J.-Y.; Hsu, C.-L.; Chen, J.-M.; Cheng, W.-C.; Lee, L.-N. Tuberculosis mortality: Patient characteristics and causes. BMC Infect. Dis. 2014, 14, 5. [Google Scholar] [CrossRef]
- Black, R.E.; Cousens, S.; Johnson, H.L.; Lawn, J.E.; Rudan, I.; Bassani, D.G.; Jha, P.; Campbell, H.; Walker, C.F.; Cibulskis, R.; et al. Global, regional, and national causes of child mortality in 2008: A systematic analysis. Lancet 2010, 375, 1969–1987. [Google Scholar] [CrossRef]
- Miteva, D.; Peshevska-Sekulovska, M.; Snegarova, V.; Batselova, H.; Alexandrova, R.; Velikova, T. Mucosal COVID-19 vaccines: Risks, benefits and control of the pandemic. World J. Virol. 2022, 11, 221–236. [Google Scholar] [CrossRef]
- Lavelle, E.C.; Ward, R.W. Mucosal vaccines—Fortifying the frontiers. Nat. Rev. Immunol. 2022, 22, 236–250. [Google Scholar] [CrossRef]
- Pollard, A.J.; Bijker, E.M. A guide to vaccinology: From basic principles to new developments. Nat. Rev. Immunol. 2021, 21, 83–100. [Google Scholar] [CrossRef]
- Russell, M.W.; Moldoveanu, Z.; Ogra, P.L.; Mestecky, J. Mucosal Immunity in COVID-19: A Neglected but Critical Aspect of SARS-CoV-2 Infection. Front. Immunol. 2020, 11, 611337. [Google Scholar] [CrossRef] [PubMed]
- Reljic, R.; Sibley, L.; Huang, J.-M.; Pepponi, I.; Hoppe, A.; Hong, H.A.; Cutting, S.M. Mucosal Vaccination against Tuberculosis Using Inert Bioparticles. Infect. Immun. 2013, 81, 4071–4080. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.T.; Shen, X.; Walter, K.L.; LaBranche, C.C.; Wyatt, L.S.; Tomaras, G.D.; Montefiori, D.C.; Moss, B.; Barouch, D.H.; Clements, J.D.; et al. HIV-1 vaccination by needle-free oral injection induces strong mucosal immunity and protects against SHIV challenge. Nat. Commun. 2019, 10, 798. [Google Scholar] [CrossRef]
- Loenenbach, A.D.; Poethko-Müller, C.; Pawlita, M.; Thamm, M.; Harder, T.; Waterboer, T.; Schröter, J.; Deleré, Y.; Wichmann, O.; Wiese-Posselt, M. Mucosal and cutaneous Human Papillomavirus seroprevalence among adults in the prevaccine era in Germany—Results from a nationwide population-based survey. Int. J. Infect. Dis. 2019, 83, 3–11. [Google Scholar] [CrossRef]
- Matić, Z.; Šantak, M. Current view on novel vaccine technologies to combat human infectious diseases. Appl. Microbiol. Biotechnol. 2022, 106, 25–56. [Google Scholar] [CrossRef]
- Cho, C.-S.; Hwang, S.-K.; Gu, M.-J.; Kim, C.-G.; Kim, S.-K.; Ju, D.-B.; Yun, C.-H.; Kim, H.-J. Mucosal Vaccine Delivery Using Mucoadhesive Polymer Particulate Systems. Tissue Eng. Regen. Med. 2021, 18, 693–712. [Google Scholar] [CrossRef]
- Dmour, I.; Islam, N. Recent advances on chitosan as an adjuvant for vaccine delivery. Int. J. Biol. Macromol. 2022, 200, 498–519. [Google Scholar] [CrossRef]
- Barbieri, S.; Buttini, F.; Rossi, A.; Bettini, R.; Colombo, P.; Ponchel, G.; Sonvico, F.; Colombo, G. Ex vivo permeation of tamoxifen and its 4-OH metabolite through rat intestine from lecithin/chitosan nanoparticles. Int. J. Pharm. 2015, 491, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Feng, C.; Wang, Z.; Jiang, C.; Kong, M.; Zhou, X.; Li, Y.; Cheng, X.; Chen, X. Chitosan/o-carboxymethyl chitosan nanoparticles for efficient and safe oral anticancer drug delivery: In vitro and in vivo evaluation. Int. J. Pharm. 2013, 457, 158–167. [Google Scholar] [CrossRef]
- Liu, S.; Yang, S.; Ho, P.C. Intranasal administration of carbamazepine-loaded carboxymethyl chitosan nanoparticles for drug delivery to the brain. Asian J. Pharm. Sci. 2018, 13, 72–81. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Tan, Y.F.; Wong, Y.S.; Liew, M.W.J.; Venkatraman, S. Recent Advances in Chitosan-Based Carriers for Gene Delivery. Mar. Drugs 2019, 17, 381. [Google Scholar] [CrossRef] [PubMed]
- Boroumand, H.; Badie, F.; Mazaheri, S.; Seyedi, Z.S.; Nahand, J.S.; Nejati, M.; Baghi, H.B.; Abbasi-Kolli, M.; Badehnoosh, B.; Ghandali, M.; et al. Chitosan-Based Nanoparticles Against Viral Infections. Front. Cell. Infect. Microbiol. 2021, 11, 643953. [Google Scholar] [CrossRef]
- Pearson, J.P.; Brownlee, I.A. Structure and Function of Mucosal Surfaces. In Colonization of Mucosal Surfaces; Nataro, J.P., Cohen, P.S., Mobley, H.L.T., Weiser, J.N., Eds.; ASM Press: Washington, DC, USA, 2014; pp. 1–16. ISBN 978-1-68367-201-2. [Google Scholar]
- Kumar, R.; Srivastava, V.; Baindara, P.; Ahmad, A. Thermostable vaccines: An innovative concept in vaccine development. Expert Rev. Vaccines 2022, 21, 811–824. [Google Scholar] [CrossRef]
- Cook, I.F. Evidence based route of administration of vaccines. Hum. Vaccin. 2008, 4, 67–73. [Google Scholar] [CrossRef]
- Mohanan, D.; Slütter, B.; Henriksen-Lacey, M.; Jiskoot, W.; Bouwstra, J.A.; Perrie, Y.; Kündig, T.M.; Gander, B.; Johansen, P. Administration routes affect the quality of immune responses: A cross-sectional evaluation of particulate antigen-delivery systems. J. Control. Release 2010, 147, 342–349. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, P.; Tchitchek, N.; Joly, C.; Rodriguez Pozo, A.; Stimmer, L.; Langlois, S.; Hocini, H.; Gosse, L.; Pejoski, D.; Cosma, A.; et al. Vaccine Inoculation Route Modulates Early Immunity and Consequently Antigen-Specific Immune Response. Front. Immunol. 2021, 12, 645210. [Google Scholar] [CrossRef] [PubMed]
- Yu, C.; Walter, M. Needleless Injectors for the Administration of Vaccines: A Review of Clinical Effectiveness; CADTH Rapid Response Reports; Canadian Agency for Drugs and Technologies in Health: Ottawa, ON, Canada, 2020.
- Matchett, W.E.; Anguiano-Zarate, S.S.; Barry, M.A. Comparison of systemic and mucosal immunization with replicating Single cycle Adenoviruses. Glob. Vaccines Immunol. 2018, 3, 1–5. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Criscuolo, E.; Caputo, V.; Diotti, R.A.; Sautto, G.A.; Kirchenbaum, G.A.; Clementi, N. Alternative Methods of Vaccine Delivery: An Overview of Edible and Intradermal Vaccines. J. Immunol. Res. 2019, 2019, 8303648. [Google Scholar] [CrossRef] [PubMed]
- Holmgren, J.; Czerkinsky, C. Mucosal immunity and vaccines. Nat. Med. 2005, 11, S45–S53. [Google Scholar] [CrossRef]
- Mitragotri, S. Immunization without needles. Nat. Rev. Immunol. 2005, 5, 905–916. [Google Scholar] [CrossRef]
- Luczo, J.M.; Bousse, T.; Johnson, S.K.; Jones, C.A.; Pearce, N.; Neiswanger, C.A.; Wang, M.-X.; Miller, E.A.; Petrovsky, N.; Wentworth, D.E.; et al. Intranasal powder live attenuated influenza vaccine is thermostable, immunogenic, and protective against homologous challenge in ferrets. Npj Vaccines 2021, 6, 59. [Google Scholar] [CrossRef]
- Sterlin, D.; Mathian, A.; Miyara, M.; Mohr, A.; Anna, F.; Claër, L.; Quentric, P.; Fadlallah, J.; Devilliers, H.; Ghillani, P.; et al. IgA dominates the early neutralizing antibody response to SARS-CoV-2. Sci. Transl. Med. 2021, 13, eabd2223. [Google Scholar] [CrossRef]
- Wang, Z.; Lorenzi, J.C.C.; Muecksch, F.; Finkin, S.; Viant, C.; Gaebler, C.; Cipolla, M.; Hoffmann, H.-H.; Oliveira, T.Y.; Oren, D.A.; et al. Enhanced SARS-CoV-2 neutralization by dimeric IgA. Sci. Transl. Med. 2021, 13, eabf1555. [Google Scholar] [CrossRef]
- Dalle Carbonare, L.; Valenti, M.T.; Bisoffi, Z.; Piubelli, C.; Pizzato, M.; Accordini, S.; Mariotto, S.; Ferrari, S.; Minoia, A.; Bertacco, J.; et al. Serology study after BTN162b2 vaccination in participants previously infected with SARS-CoV-2 in two different waves versus naïve. Commun. Med. 2021, 1, 38. [Google Scholar] [CrossRef]
- Focosi, D.; Maggi, F.; Casadevall, A. Mucosal Vaccines, Sterilizing Immunity, and the Future of SARS-CoV-2 Virulence. Viruses 2022, 14, 187. [Google Scholar] [CrossRef] [PubMed]
- Darwich, A.; Pozzi, C.; Fornasa, G.; Lizier, M.; Azzolini, E.; Spadoni, I.; Carli, F.; Voza, A.; Desai, A.; Ferrero, C.; et al. BNT162b2 vaccine induces antibody release in saliva: A possible role for mucosal viral protection? EMBO Mol. Med. 2022, 14, e15326. [Google Scholar] [CrossRef]
- Lycke, N. Recent progress in mucosal vaccine development: Potential and limitations. Nat. Rev. Immunol. 2012, 12, 592–605. [Google Scholar] [CrossRef]
- Luria-Pérez, R.; Sánchez-Vargas, L.A.; Muñoz-López, P.; Mellado-Sánchez, G. Mucosal Vaccination: A Promising Alternative Against Flaviviruses. Front. Cell. Infect. Microbiol. 2022, 12, 887729. [Google Scholar] [CrossRef] [PubMed]
- Brandtzaeg, P. Secretory IgA: Designed for Anti-Microbial Defense. Front. Immunol. 2013, 4, 222. [Google Scholar] [CrossRef] [PubMed]
- Strugnell, R.A.; Wijburg, O.L.C. The role of secretory antibodies in infection immunity. Nat. Rev. Microbiol. 2010, 8, 656–667. [Google Scholar] [CrossRef]
- Rogier, E.; Frantz, A.; Bruno, M.; Kaetzel, C. Secretory IgA is Concentrated in the Outer Layer of Colonic Mucus along with Gut Bacteria. Pathogens 2014, 3, 390–403. [Google Scholar] [CrossRef]
- Rakhra, K.; Abraham, W.; Wang, C.; Moynihan, K.D.; Li, N.; Donahue, N.; Baldeon, A.D.; Irvine, D.J. Exploiting albumin as a mucosal vaccine chaperone for robust generation of lung-resident memory T cells. Sci. Immunol. 2021, 6, eabd8003. [Google Scholar] [CrossRef]
- Schenkel, J.M.; Masopust, D. Tissue-Resident Memory T Cells. Immunity 2014, 41, 886–897. [Google Scholar] [CrossRef]
- Bartolomé-Casado, R.; Landsverk, O.J.B.; Chauhan, S.K.; Sætre, F.; Hagen, K.T.; Yaqub, S.; Øyen, O.; Horneland, R.; Aandahl, E.M.; Aabakken, L.; et al. CD4+ T cells persist for years in the human small intestine and display a TH1 cytokine profile. Mucosal Immunol. 2021, 14, 402–410. [Google Scholar] [CrossRef]
- Yuan, R.; Yu, J.; Jiao, Z.; Li, J.; Wu, F.; Yan, R.; Huang, X.; Chen, C. The Roles of Tissue-Resident Memory T Cells in Lung Diseases. Front. Immunol. 2021, 12, 710375. [Google Scholar] [CrossRef]
- Beverley, P.C.L.; Sridhar, S.; Lalvani, A.; Tchilian, E.Z. Harnessing local and systemic immunity for vaccines against tuberculosis. Mucosal Immunol. 2014, 7, 20–26. [Google Scholar] [CrossRef]
- Shim, S.; Yoo, H.S. The Application of Mucoadhesive Chitosan Nanoparticles in Nasal Drug Delivery. Mar. Drugs 2020, 18, 605. [Google Scholar] [CrossRef]
- Gong, X.; Gao, Y.; Shu, J.; Zhang, C.; Zhao, K. Chitosan-Based Nanomaterial as Immune Adjuvant and Delivery Carrier for Vaccines. Vaccines 2022, 10, 1906. [Google Scholar] [CrossRef] [PubMed]
- Anthonsen, M.W.; Vårum, K.M.; Smidsrød, O. Solution properties of chitosans: Conformation and chain stiffness of chitosans with different degrees of N-acetylation. Carbohydr. Polym. 1993, 22, 193–201. [Google Scholar] [CrossRef]
- Lieder, R.; Gaware, V.S.; Thormodsson, F.; Einarsson, J.M.; Ng, C.-H.; Gislason, J.; Masson, M.; Petersen, P.H.; Sigurjonsson, O.E. Endotoxins affect bioactivity of chitosan derivatives in cultures of bone marrow-derived human mesenchymal stem cells. Acta Biomater. 2013, 9, 4771–4778. [Google Scholar] [CrossRef] [PubMed]
- Naskar, S.; Sharma, S.; Kuotsu, K. Chitosan-based nanoparticles: An overview of biomedical applications and its preparation. J. Drug Deliv. Sci. Technol. 2019, 49, 66–81. [Google Scholar] [CrossRef]
- Vasiliev, Y.M. Chitosan-based vaccine adjuvants: Incomplete characterization complicates preclinical and clinical evaluation. Expert Rev. Vaccines 2015, 14, 37–53. [Google Scholar] [CrossRef]
- Bakshi, P.S.; Selvakumar, D.; Kadirvelu, K.; Kumar, N.S. Chitosan as an environment friendly biomaterial—A review on recent modifications and applications. Int. J. Biol. Macromol. 2020, 150, 1072–1083. [Google Scholar] [CrossRef] [PubMed]
- Yanat, M.; Schroën, K. Preparation methods and applications of chitosan nanoparticles; with an outlook toward reinforcement of biodegradable packaging. React. Funct. Polym. 2021, 161, 104849. [Google Scholar] [CrossRef]
- Illum, L.; Jabbal-Gill, I.; Hinchcliffe, M.; Fisher, A.N.; Davis, S.S. Chitosan as a novel nasal delivery system for vaccines. Adv. Drug Deliv. Rev. 2001, 51, 81–96. [Google Scholar] [CrossRef]
- Zhao, J.; Li, J.; Jiang, Z.; Tong, R.; Duan, X.; Bai, L.; Shi, J. Chitosan, N,N,N-trimethyl chitosan (TMC) and 2-hydroxypropyltrimethyl ammonium chloride chitosan (HTCC): The potential immune adjuvants and nano carriers. Int. J. Biol. Macromol. 2020, 154, 339–348. [Google Scholar] [CrossRef]
- Norpi, A.S.M.; Nordin, M.L.; Ahmad, N.; Katas, H.; Fuaad, A.A.-H.A.; Sukri, A.; Marasini, N.; Azmi, F. New modular platform based on multi-adjuvanted amphiphilic chitosan nanoparticles for efficient lipopeptide vaccine delivery against group A streptococcus. Asian J. Pharm. Sci. 2022, 17, 435–446. [Google Scholar] [CrossRef]
- Mehrabi, M.; Mohamadpour Dounighi, N.; Montazeri, H.; Vakili-Ghartavol, R.; Rashti, A. Chitosan based nanoparticles in mucosal vaccine delivery. Arch. Razi Inst. 2018, 73, 165–176. [Google Scholar] [CrossRef] [PubMed]
- Dyer, A.M.; Hinchcliffe, M.; Watts, P.; Castile, J.; Jabbal-Gill, I.; Nankervis, R.; Smith, A.; Illum, L. Nasal delivery of insulin using novel chitosan based formulations: A comparative study in two animal models between simple chitosan formulations and chitosan nanoparticles. Pharm. Res. 2002, 19, 998–1008. [Google Scholar] [CrossRef]
- Kammona, O.; Kiparissides, C. Recent advances in nanocarrier-based mucosal delivery of biomolecules. J. Control. Release 2012, 161, 781–794. [Google Scholar] [CrossRef]
- Ways, T.M.M.; Filippov, S.K.; Maji, S.; Glassner, M.; Cegłowski, M.; Hoogenboom, R.; King, S.; Lau, W.M.; Khutoryanskiy, V.V. Mucus-penetrating nanoparticles based on chitosan grafted with various non-ionic polymers: Synthesis, structural characterisation and diffusion studies. J. Colloid Interface Sci. 2022, 626, 251–264. [Google Scholar] [CrossRef]
- Torres, F.G.; Troncoso, O.P.; Pisani, A.; Gatto, F.; Bardi, G. Natural Polysaccharide Nanomaterials: An Overview of Their Immunological Properties. Int. J. Mol. Sci. 2019, 20, 5092. [Google Scholar] [CrossRef]
- Nantachit, N.; Sunintaboon, P.; Ubol, S. Responses of primary human nasal epithelial cells to EDIII-DENV stimulation: The first step to intranasal dengue vaccination. Virol. J. 2016, 13, 142. [Google Scholar] [CrossRef] [PubMed]
- Zhuo, S.-H.; Wu, J.-J.; Zhao, L.; Li, W.-H.; Zhao, Y.-F.; Li, Y.-M. A chitosan-mediated inhalable nanovaccine against SARS-CoV-2. Nano Res. 2022, 15, 4191–4200. [Google Scholar] [CrossRef] [PubMed]
- Malik, A.; Gupta, M.; Gupta, V.; Gogoi, H.; Bhatnagar, R. Novel application of trimethyl chitosan as an adjuvant in vaccine delivery. Int. J. Nanomed. 2018, 13, 7959–7970. [Google Scholar] [CrossRef]
- Liu, Q.; Zheng, X.; Zhang, C.; Shao, X.; Zhang, X.; Zhang, Q.; Jiang, X. Antigen-conjugated N-trimethylaminoethylmethacrylate Chitosan Nanoparticles Induce Strong Immune Responses After Nasal Administration. Pharm. Res. 2015, 32, 22–36. [Google Scholar] [CrossRef]
- Slütter, B.; Bal, S.; Keijzer, C.; Mallants, R.; Hagenaars, N.; Que, I.; Kaijzel, E.; van Eden, W.; Augustijns, P.; Löwik, C.; et al. Nasal vaccination with N-trimethyl chitosan and PLGA based nanoparticles: Nanoparticle characteristics determine quality and strength of the antibody response in mice against the encapsulated antigen. Vaccine 2010, 28, 6282–6291. [Google Scholar] [CrossRef] [PubMed]
- Hagenaars, N.; Mania, M.; de Jong, P.; Que, I.; Nieuwland, R.; Slütter, B.; Glansbeek, H.; Heldens, J.; van den Bosch, H.; Löwik, C. Role of trimethylated chitosan (TMC) in nasal residence time, local distribution and toxicity of an intranasal influenza vaccine. J. Control. Release 2010, 144, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Chadhar, V.; Parashar, A.K.; Patel, M.; Nema, R.K. Development and Characterization of Tetanus Toxoid Loaded Trimethylchitosan Chloride Nanoparticles for Nasal Immunization. Curr. Res. Pharm. Sci. 2012, 2, 197–202. [Google Scholar]
- Tafaghodi, M.; Saluja, V.; Kersten, G.F.A.; Kraan, H.; Slütter, B.; Amorij, J.-P.; Jiskoot, W. Hepatitis B surface antigen nanoparticles coated with chitosan and trimethyl chitosan: Impact of formulation on physicochemical and immunological characteristics. Vaccine 2012, 30, 5341–5348. [Google Scholar] [CrossRef] [PubMed]
- Abkar, M.; Fasihi-Ramandi, M.; Kooshki, H.; Sahebghadam Lotfi, A. Oral immunization of mice with Omp31-loaded N-trimethyl chitosan nanoparticles induces high protection against Brucella melitensis infection. Int. J. Nanomed. 2017, 12, 8769–8778. [Google Scholar] [CrossRef] [PubMed]
- Zhao, K.; Sun, B.; Shi, C.; Sun, Y.; Jin, Z.; Hu, G. Intranasal immunization with O-2′-Hydroxypropyl trimethyl ammonium chloride chitosan nanoparticles loaded with Newcastle disease virus DNA vaccine enhances mucosal immune response in chickens. J. Nanobiotechnol. 2021, 19, 240. [Google Scholar] [CrossRef]
- Peng, Y.; Yao, W.; Wang, B.; Zong, L. Mannosylated Chitosan Nanoparticles Based Macrophage-Targeting Gene Delivery System Enhanced Cellular Uptake and Improved Transfection Efficiency. J. Nanosci. Nanotechnol. 2015, 15, 2619–2627. [Google Scholar] [CrossRef]
- Park, I.Y.; Kim, I.Y.; Yoo, M.K.; Choi, Y.J.; Cho, M.-H.; Cho, C.S. Mannosylated polyethylenimine coupled mesoporous silica nanoparticles for receptor-mediated gene delivery. Int. J. Pharm. 2008, 359, 280–287. [Google Scholar] [CrossRef]
- Wu, M.; Zhao, H.; Li, M.; Yue, Y.; Xiong, S.; Xu, W. Intranasal Vaccination with Mannosylated Chitosan Formulated DNA Vaccine Enables Robust IgA and Cellular Response Induction in the Lungs of Mice and Improves Protection against Pulmonary Mycobacterial Challenge. Front. Cell. Infect. Microbiol. 2017, 7, 445. [Google Scholar] [CrossRef] [PubMed]
- Bedford, J.G.; Caminschi, I.; Wakim, L.M. Intranasal Delivery of a Chitosan-Hydrogel Vaccine Generates Nasal Tissue Resident Memory CD8+ T Cells That Are Protective against Influenza Virus Infection. Vaccines 2020, 8, 572. [Google Scholar] [CrossRef] [PubMed]
- Johansson, E.-L.; Wassén, L.; Holmgren, J.; Jertborn, M.; Rudin, A. Nasal and Vaginal Vaccinations Have Differential Effects on Antibody Responses in Vaginal and Cervical Secretions in Humans. Infect. Immun. 2001, 69, 7481–7486. [Google Scholar] [CrossRef]
- Bergquist, C.; Johansson, E.L.; Lagergård, T.; Holmgren, J.; Rudin, A. Intranasal vaccination of humans with recombinant cholera toxin B subunit induces systemic and local antibody responses in the upper respiratory tract and the vagina. Infect. Immun. 1997, 65, 2676–2684. [Google Scholar] [CrossRef]
- Mills, K.H.G.; Cosgrove, C.; McNeela, E.A.; Sexton, A.; Giemza, R.; Jabbal-Gill, I.; Church, A.; Lin, W.; Illum, L.; Podda, A.; et al. Protective Levels of Diphtheria-Neutralizing Antibody Induced in Healthy Volunteers by Unilateral Priming-Boosting Intranasal Immunization Associated with Restricted Ipsilateral Mucosal Secretory Immunoglobulin A. Infect. Immun. 2003, 71, 726–732. [Google Scholar] [CrossRef]
- McNeela, E.A.; Jabbal-Gill, I.; Illum, L.; Pizza, M.; Rappuoli, R.; Podda, A.; Lewis, D.J.M.; Mills, K.H.G. Intranasal immunization with genetically detoxified diphtheria toxin induces T cell responses in humans: Enhancement of Th2 responses and toxin-neutralizing antibodies by formulation with chitosan. Vaccine 2004, 22, 909–914. [Google Scholar] [CrossRef] [PubMed]
- Huo, Z.; Sinha, R.; McNeela, E.A.; Borrow, R.; Giemza, R.; Cosgrove, C.; Heath, P.T.; Mills, K.H.G.; Rappuoli, R.; Griffin, G.E.; et al. Induction of Protective Serum Meningococcal Bactericidal and Diphtheria-Neutralizing Antibodies and Mucosal Immunoglobulin A in Volunteers by Nasal Insufflations of the Neisseria meningitidis Serogroup C Polysaccharide-CRM197 Conjugate Vaccine Mixed with Chitosan. Infect. Immun. 2005, 73, 8256–8265. [Google Scholar] [CrossRef]
- El-Kamary, S.S.; Pasetti, M.F.; Mendelman, P.M.; Frey, S.E.; Bernstein, D.I.; Treanor, J.J.; Ferreira, J.; Chen, W.H.; Sublett, R.; Richardson, C.; et al. Adjuvanted Intranasal Norwalk Virus-Like Particle Vaccine Elicits Antibodies and Antibody-Secreting Cells That Express Homing Receptors for Mucosal and Peripheral Lymphoid Tissues. J. Infect. Dis. 2010, 202, 1649–1658. [Google Scholar] [CrossRef]
- Ruiz, G.A.M.; Corrales, H.F.Z. Chitosan, Chitosan Derivatives and their Biomedical Applications. In Biological Activities and Application of Marine Polysaccharides; Shalaby, E.A., Ed.; InTech: London, UK, 2017; ISBN 978-953-51-2859-5. [Google Scholar]
- Rebouças, J.S.A.; Oliveira, F.P.S.; Araujo, A.C.D.S.; Gouveia, H.L.; Latorres, J.M.; Martins, V.G.; Prentice Hernández, C.; Tesser, M.B. Shellfish industrial waste reuse. Crit. Rev. Biotechnol. 2023, 43, 50–66. [Google Scholar] [CrossRef]
- Bellich, B.; D’Agostino, I.; Semeraro, S.; Gamini, A.; Cesàro, A. “The Good, the Bad and the Ugly” of Chitosans. Mar. Drugs 2016, 14, 99. [Google Scholar] [CrossRef]
- Paliwal, R.; Babu, R.J.; Palakurthi, S. Nanomedicine Scale-up Technologies: Feasibilities and Challenges. AAPS PharmSciTech 2014, 15, 1527–1534. [Google Scholar] [CrossRef] [PubMed]
- Van Der Lubben, I.M.; Verhoef, J.C.; Borchard, G.; Junginger, H.E. Chitosan for mucosal vaccination. Adv. Drug Deliv. Rev. 2001, 52, 139–144. [Google Scholar] [CrossRef] [PubMed]

| Administration | Advantages | Disadvantages |
|---|---|---|
| Injectable vaccines |
|
|
| Needle-free/mucosal |
|
|
| Chitosan-Based Nanocarriers | Antigen | Application | Activity and Immune Response | Advantages and Disadvantages | Administration Route | Reference |
|---|---|---|---|---|---|---|
| CRM197-Chitosan | CRM197 | Protection against Diphtheria | sIgA response | Efficient mucosal activation | Intranasal | [68,69] |
| Activation of nose-associated lymphoid tissue | Preserving the antigen structure without histological changes | |||||
| Presence of local antitoxin sIgA in the nasal mucus and in the circulating IgA antitoxin antibody secreting cells | Bio-adhesive property counteracts the mucociliary action, favoring the localization of the antigen inside the nose and allowing for prolonged absorption | |||||
| Strong increase in Th2-type responses, correlated with protective levels of toxin-neutralizing antibodies | ||||||
| (MCP)-CRM197 Chitosan | (MCP)-CRM197 conjugated | Protection against both C N. meningitidis and diphtheriae | Serum bactericidal antibody titer after two nasal immunizations | Improve the antigen retention time | Intranasal | [70] |
| Immunoglobulin G levels close to the ones obtained with parenteral administration | ||||||
| VLP-adjuvanted chitosan | Norwalk virus-like particle | Protection against Norwalk virus | Elicited mucosal dendritic cells to enhance the immune response locally and systemically | Triggering the mucosal priming phenomenon | Intranasal | [71] |
| Immunoglobulin G levels close to the ones obtained with parenteral administration | Inducing potent mucosal and systemic immune responses | |||||
| High levels of IgA and IgG ASCs in peripheral blood | Inducing mucosal immune responses at distant sites from the administration point, such as the gastrointestinal tract | |||||
| Presence of circulating ASCs of VLP-specific IgA and IgG with different homing potentials |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gaglio, S.C.; Perduca, M.; Zipeto, D.; Bardi, G. Efficiency of Chitosan Nanocarriers in Vaccinology for Mucosal Immunization. Vaccines 2023, 11, 1333. https://doi.org/10.3390/vaccines11081333
Gaglio SC, Perduca M, Zipeto D, Bardi G. Efficiency of Chitosan Nanocarriers in Vaccinology for Mucosal Immunization. Vaccines. 2023; 11(8):1333. https://doi.org/10.3390/vaccines11081333
Chicago/Turabian StyleGaglio, Salvatore Calogero, Massimiliano Perduca, Donato Zipeto, and Giuseppe Bardi. 2023. "Efficiency of Chitosan Nanocarriers in Vaccinology for Mucosal Immunization" Vaccines 11, no. 8: 1333. https://doi.org/10.3390/vaccines11081333
APA StyleGaglio, S. C., Perduca, M., Zipeto, D., & Bardi, G. (2023). Efficiency of Chitosan Nanocarriers in Vaccinology for Mucosal Immunization. Vaccines, 11(8), 1333. https://doi.org/10.3390/vaccines11081333









