Assessing the Influence of COVID-19 Vaccination Coverage on Excess Mortality across 178 Countries: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Sources
2.2. Statistical Analysis
2.3. Ethical Considerations
3. Results
3.1. All-Cause Excess Mortality Rate
3.2. COVID-19 Vaccination Coverage
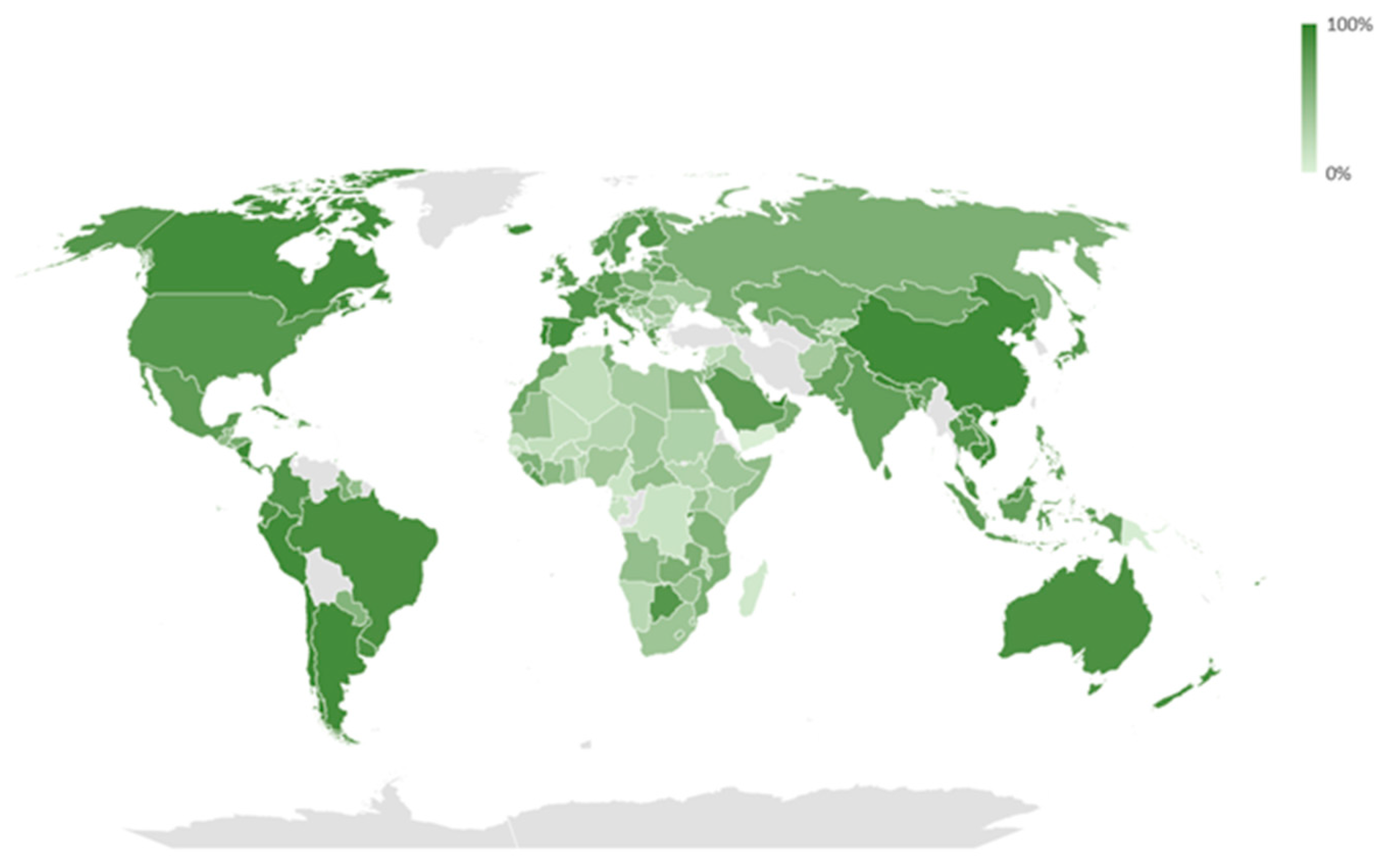
3.3. All-Cause Excess Mortality Rate and COVID-19 Vaccination Coverage
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Liu, K.; Lou, Y. Optimizing COVID-19 vaccination programs during vaccine shortages. Infect. Dis. Model. 2022, 7, 286–298. [Google Scholar] [CrossRef]
- Stefanelli, P.; Rezza, G. COVID-19 Vaccination Strategies and Their Adaptation to the Emergence of SARS-CoV-2 Variants. Vaccines 2022, 10, 905. [Google Scholar] [CrossRef] [PubMed]
- Aruffo, E.; Yuan, P.; Tan, Y.; Gatov, E.; Gournis, E.; Collier, S.; Ogden, N.; Bélair, J.; Zhu, H. Community structured model for vaccine strategies to control COVID19 spread: A mathematical study. PLoS ONE 2022, 17, e0258648. [Google Scholar] [CrossRef] [PubMed]
- Barnard, S.; Chiavenna, C.; Fox, S.; Charlett, A.; Waller, Z.; Andrews, N.; Goldblatt, P.; Burton, P.; De Angelis, D. Methods for modelling excess mortality across England during the COVID-19 pandemic. Stat. Methods Med. Res. 2022, 31, 1790–1802. [Google Scholar] [CrossRef]
- Tang, B.; Zhang, X.; Li, Q.; Bragazzi, N.L.; Golemi-Kotra, D.; Wu, J. The minimal COVID-19 vaccination coverage and efficacy to compensate for a potential increase of transmission contacts, and increased transmission probability of the emerging strains. BMC Public Health 2022, 22, 1258. [Google Scholar] [CrossRef]
- Kunyenje, C.A.; Chirwa, G.C.; Mboma, S.M.; Ng’ambi, W.; Mnjowe, E.; Nkhoma, D.; Ngwira, L.G.; Chawani, M.S.; Chilima, B.; Mitambo, C.; et al. COVID-19 vaccine inequity in African low-income countries. Front. Public Health 2023, 11, 1087662. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Methods for Estimating the Excess Mortality Associated with the COVID-19 Pandemic. Available online: https://cdn.who.int/media/docs/default-source/world-health-data-platform/COVID-19-excessmortality/who_methods_for_estimating_the_excess_mortality_associated_with_the_COVID-19_pandemic.pdf?sfvrsn=5a05fa76_2&download=true (accessed on 28 June 2023).
- United Nations. Department of Economic and Social Affairs. Methodology Report: World Population Prospects. 2022. Available online: https://population.un.org/wpp/Publications/Files/WPP2022_Methodology.pdf (accessed on 28 June 2023).
- Hoxha, I.; Agahi, R.; Bimbashi, A.; Aliu, M.; Raka, L.; Bajraktari, I.; Beqiri, P.; Adams, L.V. Higher COVID-19 Vaccination Rates Are Associated with Lower COVID-19 Mortality: A Global Analysis. Vaccines 2022, 11, 74. [Google Scholar] [CrossRef]
- Bilinski, A.; Thompson, K.; Emanuel, E. COVID-19 and Excess All-Cause Mortality in the US and 20 Comparison Countries, June 2021–March 2022. JAMA 2023, 329, 92–94. [Google Scholar] [CrossRef]
- Juul, F.E.; Jodal, H.C.; Barua, I.; Refsum, E.; Olsvik, O.; Helsingen, L.M.; Loberg, M.; Bretthauer, M.; Kalager, M.; Emilsson, L. Mortality in Norway and Sweden during the COVID-19 pandemic. Scand. J. Public Health 2022, 50, 38–45. [Google Scholar] [CrossRef]
- Ramirez-Soto, M.C.; Ortega-Caceres, G. Analysis of Excess All-Cause Mortality and COVID-19 Mortality in Peru: Observational Study. Trop. Med. Infect. Dis. 2022, 7, 44. [Google Scholar] [CrossRef]
- Murillo-Zamora, E.; Trujillo, X.; Huerta, M.; Rios-Silva, M.; Guzman-Esquivel, J.; Benites-Godinez, V.; Ochoa-Castro, M.R.; Guzman-Solorzano, J.A.; Mendoza-Cano, O. COVID-19 vaccines provide better protection against related pneumonia than previous symptomatic infection. Int. J. Infect. Dis. 2022, 120, 142–145. [Google Scholar] [CrossRef] [PubMed]
- Baker, T.B.; Bolt, D.M.; Smith, S.S.; Piasecki, T.M.; Conner, K.L.; Bernstein, S.L.; Hayes-Birchler, T.; Theobald, W.E.; Fiore, M.C. The Relationship of COVID-19 Vaccination with Mortality Among 86,732 Hospitalized Patients: Subpopulations, Patient Factors, and Changes over Time. J. Gen. Intern. Med. 2023, 38, 1248–1255. [Google Scholar] [CrossRef]
- Smith, J.B.; Gonzales, E.G.; Li, B.H.; Langer-Gould, A. Analysis of Rituximab Use, Time Between Rituximab and SARS-CoV-2 Vaccination, and COVID-19 Hospitalization or Death in Patients With Multiple Sclerosis. JAMA Netw. Open 2022, 5, e2248664. [Google Scholar] [CrossRef]
- Hernandez-Suarez, C.; Murillo-Zamora, E. Waning immunity to SARS-CoV-2 following vaccination or infection. Front. Med. 2022, 9, 972083. [Google Scholar] [CrossRef] [PubMed]
- Rasambainarivo, F.; Ramiadantsoa, T.; Raherinandrasana, A.; Randrianarisoa, S.; Rice, B.L.; Evans, M.V.; Roche, B.; Randriatsarafara, F.M.; Wesolowski, A.; Metcalf, J.C. Prioritizing COVID-19 vaccination efforts and dose allocation within Madagascar. BMC Public Health 2022, 22, 724. [Google Scholar] [CrossRef] [PubMed]
- Watson, O.J.; Barnsley, G.; Toor, J.; Hogan, A.B.; Winskill, P.; Ghani, A.C. Global impact of the first year of COVID-19 vaccination: A mathematical modelling study. Lancet Infect. Dis. 2022, 22, 1293–1302. [Google Scholar] [CrossRef] [PubMed]
- van Iersel, S.; McDonald, S.A.; de Gier, B.; Knol, M.J.; de Melker, H.E.; Henri van Werkhoven, C.H.; Hahne, S.J.M. Number of COVID-19 hospitalisations averted by vaccination: Estimates for the Netherlands, January 6, 2021 through August 30, 2022. Vaccine 2023, 41, 3847–3854. [Google Scholar] [CrossRef]
- Aburto, J.M.; Villavicencio, F.; Basellini, U.; Kjaergaard, S.; Vaupel, J.W. Dynamics of life expectancy and life span equality. Proc. Natl. Acad. Sci. USA 2020, 117, 5250–5259. [Google Scholar] [CrossRef] [Green Version]
- Vaupel, J.W.; Villavicencio, F.; Bergeron-Boucher, M.P. Demographic perspectives on the rise of longevity. Proc. Natl. Acad. Sci. USA 2021, 118, e2019536118. [Google Scholar] [CrossRef]
- Javed, Z.; Valero-Elizondo, J.; Cainzos-Achirica, M.; Sharma, G.; Mossialos, E.; Parekh, T.; Hagan, K.; Hyder, A.A.; Kash, B.; Nasir, K. Race, Social Determinants of Health, and Risk of All-Cause and Cardiovascular Mortality in the United States. J. Racial Ethn. Health Disparities 2023, 1–2. [Google Scholar] [CrossRef]
- Mas-Ubillus, G.; Ortiz, P.J.; Huaringa-Marcelo, J.; Sarzo-Miranda, P.; Munoz-Aguirre, P.; Diaz-Ramos, A.; Arribasplata-Purizaca, K.; Mendoza, D.; Rojas-Poma, J.; Marcelo-Ruiz, C.; et al. High mortality among hospitalized adult patients with COVID-19 pneumonia in Peru: A single centre retrospective cohort study. PLoS ONE 2022, 17, e0265089. [Google Scholar] [CrossRef] [PubMed]
- Musa, S.S.; Tariq, A.; Yuan, L.; Haozhen, W.; He, D. Infection fatality rate and infection attack rate of COVID-19 in South American countries. Infect. Dis. Poverty 2022, 11, 40. [Google Scholar] [CrossRef] [PubMed]
- Cajachagua-Torres, K.N.; Quezada-Pinedo, H.G.; Huayanay-Espinoza, C.A.; Obeso-Manrique, J.A.; Pena-Rodriguez, V.A.; Vidal, E.; Huicho, L. COVID-19 and drivers of excess death rate in Peru: A longitudinal ecological study. Heliyon 2022, 8, e11948. [Google Scholar] [CrossRef] [PubMed]


| Variable | ||
|---|---|---|
| Bivariate Analysis | Multiple Analysis | |
| COVID-19 vaccination coverage | −44.6 (−101.1 to 12.0), 0.122 | −106.8 (−175.4 to −38.2), 0.002 |
| Life expectancy at birth | 1.4 (−0.5 to 3.3), 0.147 | 3.5 (1.2 to 5.8), 0.003 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mendoza-Cano, O.; Trujillo, X.; Huerta, M.; Ríos-Silva, M.; Guzmán-Esquivel, J.; Lugo-Radillo, A.; Benites-Godínez, V.; Bricio-Barrios, J.A.; Cárdenas-Rojas, M.I.; Ríos-Bracamontes, E.F.; et al. Assessing the Influence of COVID-19 Vaccination Coverage on Excess Mortality across 178 Countries: A Cross-Sectional Study. Vaccines 2023, 11, 1294. https://doi.org/10.3390/vaccines11081294
Mendoza-Cano O, Trujillo X, Huerta M, Ríos-Silva M, Guzmán-Esquivel J, Lugo-Radillo A, Benites-Godínez V, Bricio-Barrios JA, Cárdenas-Rojas MI, Ríos-Bracamontes EF, et al. Assessing the Influence of COVID-19 Vaccination Coverage on Excess Mortality across 178 Countries: A Cross-Sectional Study. Vaccines. 2023; 11(8):1294. https://doi.org/10.3390/vaccines11081294
Chicago/Turabian StyleMendoza-Cano, Oliver, Xóchitl Trujillo, Miguel Huerta, Mónica Ríos-Silva, José Guzmán-Esquivel, Agustin Lugo-Radillo, Verónica Benites-Godínez, Jaime Alberto Bricio-Barrios, Martha Irazema Cárdenas-Rojas, Eder Fernando Ríos-Bracamontes, and et al. 2023. "Assessing the Influence of COVID-19 Vaccination Coverage on Excess Mortality across 178 Countries: A Cross-Sectional Study" Vaccines 11, no. 8: 1294. https://doi.org/10.3390/vaccines11081294
APA StyleMendoza-Cano, O., Trujillo, X., Huerta, M., Ríos-Silva, M., Guzmán-Esquivel, J., Lugo-Radillo, A., Benites-Godínez, V., Bricio-Barrios, J. A., Cárdenas-Rojas, M. I., Ríos-Bracamontes, E. F., Guzman-Solorzano, H. P., Baltazar-Rodríguez, G. M., Ruiz-Montes de Oca, V., Ortega-Macías, V. M., Ortega-Ramírez, A. D., & Murillo-Zamora, E. (2023). Assessing the Influence of COVID-19 Vaccination Coverage on Excess Mortality across 178 Countries: A Cross-Sectional Study. Vaccines, 11(8), 1294. https://doi.org/10.3390/vaccines11081294








