Abstract
Human papilloma virus (HPV) vaccination rates remain below national goals in the United States despite the availability of evidence-based strategies to increase rates. The Adolescent Vaccination Program (AVP) is a multi-component intervention demonstrated to increase HPV vaccination rates in pediatric clinics through the implementation of six evidence-based strategies. The purpose of this study, conducted in Houston, Texas, from 2019–2021, was to adapt the AVP into an online decision support implementation tool for standalone use and to evaluate its feasibility for use in community clinics. Phase 1 (Adaptation) comprised clinic interviews (n = 23), literature review, Adolescent Vaccination Program Implementation Tool (AVP-IT) design documentation, and AVP-IT development. Phase 2 (Evaluation) comprised usability testing with healthcare providers (HCPs) (n = 5) and feasibility testing in community-based clinics (n = 2). AVP-IT decision support provides an Action Plan with tailored guidance on implementing six evidence-based strategies (immunization champions, assessment and feedback, continuing education, provider prompts, parent reminders, and parent education). HCPs rated the AVP-IT as acceptable, credible, easy, helpful, impactful, and appealing (≥80% agreement). They rated AVP-IT supported implementation as easier and more effective compared to usual practice (p ≤ 0.05). The clinic-based AVP-IT uses facilitated strategy implementation by 3-month follow-up. The AVP-IT promises accessible, utilitarian, and scalable decision support on strategies to increase HPV vaccination rates in pediatric clinic settings. Further feasibility and efficacy testing is indicated.
1. Introduction
In the U.S., infections of human papillomavirus (HPV) approximate 79 million people, with an expected 14 million newly infected persons each year [1]. Persistent infection with high-risk HPV types (mainly 16 and 18) are associated with cervical and anal cancers (>90%), oropharyngeal cancers (70%), vaginal and vulvar cancers (70%), and penile cancers (>60%) and with associated increases in health costs [2,3,4,5,6,7,8]. The HPV vaccine is efficacious in decreasing HPV infections, precancerous lesions, and genital warts [9,10,11,12]. The Advisory Committee on Immunization Practices (ACIP) recommends the HPV vaccination series be initiated in both males and females by 11 to 12 years of age [13,14]. There is evidence for the safety [15,16] and effectiveness [10] of HPV vaccination, yet rates are below the Healthy People 2030 goal of 80% for series completion in adolescents 13 to 15 years of age [17]. Rates are also below those of acellular pertussis and meningococcal conjugate vaccines [18]. A robust evidence base exists for strategies that increase HPV vaccination, including healthcare provider (HCP) assessment and feedback [19], prompts to providers [20], patient reminder systems [21], and both provider- and patient-directed education when implemented in combination with other healthcare-system-based strategies [22]. Healthcare-system-based implementation strategies are effective because they can operate simultaneously at the organizational, provider, and patient levels. Despite this, there is inconsistency in the strategies that are adopted and the degree of implementation across clinics, even within clinical networks [22,23,24].
The Adolescent Vaccination Program (AVP) is a multi-component program to increase HPV vaccination rates in pediatric clinics. The AVP targets HCPs and parents of pediatric patients 11–17 years of age [23]. The AVP contains a suite of evidence-based strategies that include: (1) immunization champions, (2) provider assessment and feedback, (3) provider continuing education, (4) provider prompts, (5) parent (patient) reminders, and (6) parent (patient) education. The AVP has been successful in significantly increasing initiation and completion of the HPV vaccine series in large urban networks in Houston and San Antonio, Texas [24,25,26].
The existence of such evidence-based strategies does not mean that clinics will necessarily adopt or implement them. Therefore, implementation researchers have compiled a set of effective implementation strategies identified to support implementation of evidence-based clinical practices [27]. Delivery of implementation strategies using theoretically and empirically based decision support tools could assist HCPs and clinic managers to determine their clinic’s readiness to adopt evidence-based strategies and could provide utilitarian guides for their implementation.
Online decision support tools can effectively aid decision making in varied settings, including healthcare [28]. They can enhance HCP practice in drug dosing, preventive care, and active medical care [29,30]. Given their effectiveness, experts in dissemination research have encouraged the use of decision support tools to translate evidence-based science into practice [31].
The efficacy of the AVP and the potential of online decision support in enhancing quality improvement in clinical settings suggest the potential benefits of adapting the AVP to be an online decision support tool. This implementation support tool could enable clinics to independently implement the bundle of six evidence-based strategies under their own auspices and provide scalability to the AVP to accommodate broad geographic reach.
Individual and organizational factors can facilitate decisions to adopt and implement technology-based interventions [32]. These factors include individual user perceptions of the intervention’s acceptability, credibility, ease of use, simplicity, scope, benefit, impact, understandability, duration, scalability, relative advantage, and appeal [33]. They also include an organization’s capacity to support implementation that include management support, resources, and accommodation in existing schedules and flow [34]. Usability and feasibility testing of intervention prototypes is an important formative step to ensure confidence that the digital intervention functions the way it is designed to while not disrupting or comprising the organizational flow [35].
The purpose of this study was to (1) adapt the AVP to provide online decision support to implement six evidence-based AVP strategies in pediatric clinics throughout Texas, (2) assess its usability and acceptability with end-users, and (3) assess the feasibility for its use in community clinic settings. This study contributes to the literature on adapting existing evidence-based protocols into online decision support applications.
2. Materials and Methods
The Adolescent Vaccination Program Implementation Tool (AVP-IT) is a decision-support website designed to support the implementation of AVP strategies into pediatric clinics. The development of the AVP-IT comprised 2 phases to: (1) adapt the existing in-person AVP evidence-based program into a completely Internet-based decision support program for implementation (AVP-IT) and (2) formatively evaluate the AVP-IT for usability and feasibility (Table 1). This study was conducted in Houston, Texas, USA, between March, 2019 and November, 2021.

Table 1.
Phases and Steps in AVP Adaptation and Formative Evaluation.
2.1. Phase 1: Adaptation
Goals for adaptation were to ensure that original content, objectives, and functionality of the AVP was retained in the new online program and that it was acceptable to end users, feasible for delivery in the community clinic setting, and potentially impactful in motivating change in clinic practice. Stepped translation frameworks described by Card et al. (2011) and Bartholomew et al. (2006), respectively, guided the incorporation of theoretically and empirically based evidence in the adaptation process [36,37].
2.1.1. Step 1: Semi-Structured Interviews
Active participatory research with an expert advisory group informed the translation of existing AVP protocols throughout the AVP-IT development. The expert advisory group comprised 10 decision-makers and stakeholders representing pediatric clinic management, pediatric clinical healthcare providers (HCPs), researchers in public health immunization, and representatives from community organizations with a mission focus on immunization. The expert advisory group was established to formatively evaluate content, strategies, and methods to include in the AVP-IT and how to best package the tool to support implementation and ensure generalizability to a breadth of clinic environments.
Expert advisory group members assisted in identifying HCPs and clinic managers from a sample of 23 clinics that varied by size (small of <3 HCPs vs. large of ≥3 HCPs), location (rural vs. urban), affiliation (single vs. network affiliated), medical record type (EMR vs. paper-based), and primary patient payment (Medicaid vs. commercial insurance). Clinic heterogeneity was important for generalizability, ensuring the tool has utility in varied clinic environments. An ethnographic protocol was employed to describe facilitators and barriers within Texas clinics to (1) implement evidence-based strategies to increase HPV vaccination rates and (2) adopt and implement an online tool to guide this implementation [38,39,40,41].
HCPs and clinic managers were invited to provide their perspectives in 30 min semi-structured phone interviews on the features of a decision support system that would promote acceptability, utility, and ease of use. Semi-structured interviews were selected (as opposed to structured interviews) because they provided more scope for respondents to elaborate on their perspective while still maintaining enough structure for interviews to be compared [39]. Measurement instruments comprised an interview guide that focused on the barriers and facilitators to implementing online decision support and a brief survey to confirm each clinic’s structure and demographic characteristics. The interview guide was designed to understand the daily functions of the clinics, how changes are implemented, and how a decision tool could make it easier for clinics to adopt evidence-based strategies. Interviews were analyzed thematically for common themes, including facilitators and barriers, around implementation of a decision support tool.
2.1.2. Step 2: Literature Review
A brief scoping review was conducted to append the research team’s existing literature base. The review was designed to identify: (1) behavioral and environmental factors that impact HPV vaccination; (2) behavioral and environmental barriers to the adoption and implementation of evidence-based strategies designed to increase HPV vaccination (including organizational factors); (3) interventions that have successfully mitigated these barriers; and (4) successful theory-based and empirically based frameworks (e.g., IM-ADAPT, RE-AIM, CFIR, and Fishbein’s Integrative Model of Behavior Change) to enhance adoption and implementation. The research team identified relevant studies and synthesized the literature into evidence tables for review by the expert advisory group. Results are described in Section 3.1.2 below and informed the concept, content, architecture, and functional design specifications of the AVP-IT.
2.1.3. Step 3: Develop the AVP-IT Design Document
The AVP-IT design document was developed to describe program specifications including core content, scope, function, flow, and methods and strategies. Content analysis of the original AVP design document (describing its aims, target population, objectives, behavioral matrices, content, and tools) provided the foundation for AVP-IT design. The Intervention Mapping (IM) framework had guided the original AVP development [23]. Core content, scope, and best practice characteristics were represented in behavioral change matrices, a product of the IM process. These cross-referenced targeted behavioral outcomes, performance objectives, behavioral mediators, and learning objectives [36]. Targeted behavioral outcomes for the original AVP program are described elsewhere [23]. These included: (1) collaboration with AVP champions in each clinic regarding implementation of strategies and immunization rates; (2) HCP review of assessment and feedback reports on their HPV vaccination rates; (3) coordination with clinical staff to provide consistent messaging to patient/parents regarding HPV vaccination; (4) checking for vaccine eligibility at every clinic encounter; (5) delivering strong presumptive recommendations to eligible patients at time of visit; (6) bundling HPV vaccine recommendations with other vaccines; (7) determining patient/parent concerns if they are vaccine hesitant; (8) communicating tailored messages to address specific patient/parent concerns; and (9) reminding patients to schedule follow-up HPV vaccine dose(s) before leaving the clinic.
The original AVP program was designed to target behavioral antecedents of knowledge, self-efficacy, outcome expectations, and normative beliefs. Upon review, the research team determined that the targeted behaviors (performance objectives) and antecedents were relevant and valid for current HPV vaccination behaviors. Design document development was iterative. An expert advisory group reviewed the design for appropriateness, clarity, layout, and language. Theoretical methods (i.e., self-assessment, role modeling, and guided practice) and practical strategies (i.e., stepped Action Plan, role model video, photo-based interactive activities) were included in the AVP-IT design to increase clinic staff knowledge, skills, and self-efficacy. The design document was the ‘blue print’ for the AVP-IT production. Design features for the AVP-IT were informed by the results from Steps 1 and 2 (refer to Section 3.1.3 below for further detail).
2.1.4. Step 4: Produce the AVP-IT
An agile and iterative programming schedule was employed to produce the AVP-IT. The AVP-IT was programmed in HTML5, accessible from any internet-enabled device, and included a data input ‘Wizard’ to create a dynamically built Action Plan. Asset development included role-model testimonial videos, an automated assessment and feedback spreadsheet developed in Excel that enabled conversion of clinic- and provider-based vaccination data (inputted into 10 data cells) into dynamically generated quarterly reports, links to continued medical education (CME) content and previous publications, and embedded tools corresponding to each of the six evidence-based strategies (described more fully in Section 3.1.3 below). A back-end database was produced to track visits and maintain a deidentified record of data responses to data inputted for the Action Plan. The AVP-IT was alpha tested in-house to ensure it conformed to intended design and functional specifications.
2.2. Phase 2: Formative Evaluation
Usability and feasibility testing followed previously published protocols from the research team [42].
2.2.1. Step 5: Usability Testing
Study Design and Participants: Expert advisory group members (n = 5) were sent the AVP-IT website URL, reviewer instructions, and a usability survey in July 2021. They were instructed to access all elements of the AVP-IT—including the Action Plan Wizard, their clinic’s tailored Action Plan, and accompanying resources—and then to complete the usability survey with demographic questionnaire (including items on age, gender, race/ethnicity and job title) and a debriefing session with the research principal investigator. The adapted usability survey assessed functions of the AVP-IT and potential improvements of content, function, and interface design [42]. Participants were asked to pay particular attention to evaluating the content located in the ‘How To’ section of each Action Plan strategy. This was to ensure that user guidance on implementation steps was explained appropriately and was understandable. Usability parameters included acceptability (likability), credibility, ease of use, information scope, duration, helpfulness, perceived impact, and motivational appeal adapted from pre-existing usability assessment instruments [42]. The sample size was suitable for usability testing which is typically descriptive, not requiring statistical significance as a criteria for determining usability problems [43].
Measurement and Analysis: Acceptability was assessed by how much participants liked the AVP-IT and various components, including the ‘About’ page, Action Plan, and Action Plan Wizard (response ratings: dislike a lot, dislike a little, like a little, like a lot, did not use). Credibility was assessed from the perceived correctness of the content (response ratings: accurate, inaccurate, no opinion) and whether the content could be trusted (response ratings: can be trusted, can’t be trusted, no opinion). Ease of use was assessed from the perceived difficulty in using the AVP-IT and completing the clinic Action Plan (response ratings: very easy, kind of easy, kind of hard, very hard, did not use). Complexity was assessed from perceptions of whether the AVP-IT was unnecessarily complex or cumbersome, if components were well integrated, and if participant’s felt the AVP-IT required technical support or extensive training to be able to use it (response ratings: strongly agree, agree, neither agree nor disagree, disagree, strongly disagree). Information scope was assessed by perceptions on the amount of information provided (response ratings: just right, too much, too little). Duration was assessed from the perception of how long it would take to use the AVP-IT and complete the Action Plan Wizard (response ratings: too quick, just right, too long). Helpfulness was assessed from perceptions of helpfulness of the ‘About’ page (response ratings: helpful, not helpful, don’t know) and the AVP-IT program components (response ratings: extremely helpful, very helpful, somewhat helpful, not at all helpful). Perceived impact was assessed from perceptions of whether the AVP-IT would help clinics adopt, implement, and maintain HPV implementation strategies (response ratings: strongly agree, agree, neither agree nor disagree, disagree, strongly disagree, don’t know). Motivational appeal was assessed from the likelihood of AVP-IT use by other clinics and if they should use it (response ratings: yes, no, maybe) and the participants’ interest in using the AVP-IT (response ratings: strongly agree, agree, neither agree nor disagree, disagree, strongly disagree). Open-ended questions were included to assess what participants liked best and liked least about the AVP-IT and its three main components: ‘About AVP-IT’, ‘My Action Plan’, ‘My Toolkit.’ Participants were also asked what else they would have liked to see in these components and how the AVP-IT could be made more appealing.
Relative advantage of the AVP-IT was assessed from HCP expectations of impact on implementing evidence-based strategies when using the AVP-IT compared to usual practice (i.e., implementing strategies to increase HPV vaccination without the AVP-IT) using 5-point (range: 1–5) semantic differential scale assessing: ease of use (easier/harder), time (less time/more time), and effectiveness (more effective/less effective) [42]. Each participant was given 10 days to review the AVP-IT website and complete the usability survey. Usability data was assessed using descriptive statistics of central tendency. The semantic differential scale was assessed using a paired 2-tailed t-test comparison of responses against neutral ratings using STATA IC Version 17 analytic software [44]. The hypotheses tested was that those exposed to the AVP-IT would perceive its use as providing significant advantage (easier, less time intensive, and more efficacious) compared to their usual practice. Semi-structured 30 min debrief interviews with each participant provided information on recommended enhancements to improve the user experience and to facilitate the adoption and implementation of the AVP-IT in clinics.
2.2.2. Step 6: Feasibility Testing Case Study
A pilot test of the AVP-IT was conducted to determine the feasibility of delivery in typical community clinic settings and its impact. Study Design and Participants: A single-group, pre-test/post-test design was conducted in two community clinics, comprising one and four physicians, respectively, that were part of a broader clinic network of seven community clinics in the Greater Houston area. The clinics provided medical, specialty, behavioral health, diagnostic, and immunization services to a patient population comprising mainly Hispanic (43%, 67%), African American (32%, 14%), and South Asian (19%, 11%) patients who were mainly uninsured or self-pay (74%, 94%).
Measurement and Analysis: At each site, clinic directors selected an AVP Champion.
AVP Champions could be chief medical officers, practice managers, HCPs, clinic administrators, or clinic staff. They were responsible for coordinating rollout of strategies in accordance with the Action Plan. Champions provided demographic data, including age, gender, education level, race/ethnicity, and job title. They then received an e-mail with the AVP-IT link and further instructions for the feasibility trial. They then visited the online AVP-IT and completed the Action Plan Wizard and printed their clinic’s tailored Action Plan. They were asked to follow the steps in the plan to implement each of the AVP strategies in their clinic and, at 3-month follow-up, to again complete the Action Plan Wizard. The AVP-IT Action Plan was used to assess pre- and 3-month post-test implementation with six items that asked about implementation status (pending, partial, full) based on AVP-IT criteria. Strategies were defined as ‘fully implemented’ if they were implemented in accordance with the AVP-IT Action Plan criteria, or else they were defined as ‘partially implemented’. Strategies defined as ‘pending’ were yet to be initiated. Implementation of AVP strategies was compared descriptively between baseline and at 3-month follow-up. Monitoring call field notes provided qualitative feedback on the AVP-IT implementation process. Over the three-month study period, bimonthly monitoring calls were conducted to obtain status updates and troubleshoot challenges associated with the AVP-IT or implementation of AVP strategies in clinics. The champions were asked to complete 15 min exit interviews with research staff to provide a summary of their experiences and recommendations for AVP-IT enhancements. Champions received a $25 gift card for completing pre- and post-test assessment respectively.
3. Results
3.1. Phase 1: Adaptation
3.1.1. Step 1. Semi-Structured Interviews
Respondents were clinic staff from five urban clinics comprising two large (≥3 HCPs) and one small clinic (<3 HCPs) with a mainly Medicaid patient population and one large and one small clinic with a mainly commercially insured patient population [41]. Interviews provided information on the varying priorities and preferred strategies for varied clinic types. A clinic’s core mission orientation was a critical factor in adopting and implementing strategies. Clinics with a majority percentage of Medicaid or uninsured patients (e.g., safety net clinics, community-based Federally Qualified Health Centers) and oriented to providing care to a maximum number of underserved patients preferred in-person training for evidence-based strategies to increase HPV rates. They emphasized that strategies of greatest utility were provider prompts, patient reminders, and patient education tools. Clinics with a majority percentage of commercially insured patients (e.g., health maintenance organizations) preferred online training for evidence-based strategies to increase HPV rates. They emphasized that strategies of greatest utility were immunization champions, provider education, and assessment and feedback reports. Structural considerations of clinic size, location, insurance, and EHR were not considered to be critical barriers in the clinic staff’s decision to implement evidence-based strategies to increase HPV vaccination rates or to adopt and implement an online tool to guide this implementation.
3.1.2. Step 2: Literature Review
Tables of facilitators and barriers were constructed to categorize implementation of decision support, multi-component interventions, and evidence-based strategies within the AVP (Table 2 and Table 3). Facilitators to adoption and implementation included the right people receiving the right information at appropriate times, training and leadership support, printed copies of documents and reports, incentivization, adding prompts to visit preparation, and previous messaging experience. Barriers to adopting and implementing strategies within the AVP include lack of funding, staff turnover and lack of staff buy-in, limited access to resources, lack of time and difficulty in changing workflow, and competing priorities.

Table 2.
Facilitators and Barriers to Implementation of Evidence-based Strategies: Provider Education, Provider Prompts, and Patient Reminders.

Table 3.
Facilitators and Barriers to Implementation of Evidence-based Strategies: Decision Support and Multi-component Programs.
3.1.3. Steps 3 and 4: AVP-IT Design and Production
The AVP-IT is designed to assist clinic staff in the adoption, implementation, and maintenance of evidence-based HPV vaccination strategies within their clinic. AVP-IT provides guidance in (1) determining the level of readiness of the clinic for implementation of each AVP strategy, (2) implementing each strategy regardless of the size and type of pediatric clinic or clinic network, and (3) increasing systems knowledge and capacity to address low HPV vaccination rates.
For stand-alone functionality, the AVP-IT required a robust, simple, intuitive architecture and navigation and sufficient scaffolding to inform naïve users of its purpose and use. This need prompted core features of (1) a tailored implementation Action Plan dynamically generated in response to data (input into an AVP-IT Action Plan ‘Wizard’) on clinic parameters that provides guidance on rolling out each evidence-based strategy; (2) an automatic assessment and feedback report generator, responsive to each provider’s immunization data that provides graphic confirmation of the provider performance in relation to other providers; and (3) video-based testimonials from credible stakeholders who emphasize the ease and importance of each evidence-based strategy. The AVP-IT website is housed on a secure UTHealth server and is accessible online to any clinic (https://avp.sph.uth.edu/, accessed on 20 May 2023). It comprises four webpages: (1) About AVP-IT, (2) My Action Plan, (3) My Toolkit, and (4) Contact Us, designed for user-friendly and tailored guidance to assist clinics in implementing AVP strategies regardless of clinic size and type (Figure 1).
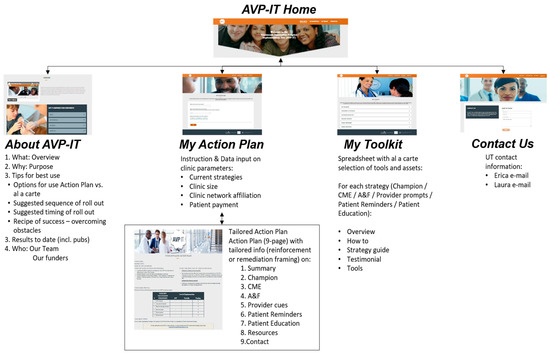
Figure 1.
AVP-IT contents.
AVP-IT use by AVP Champions. The AVP Champion (previously described) can use the AVP-IT by following the four steps that correspond to the page structure of the AVP-IT site:
- (1)
- About AVP-IT provides an overview and background on the AVP in video and text with links to research publications.
- (2)
- My Action Plan provides an Action Plan Wizard. The AVP Champion can enter descriptive data about their clinic (e.g., clinic size, location, EHR platform, affiliation) and status of the six AVP strategies by responding to six multiple choice questions (Table 4). They then receive a printable Action Plan that is dynamically compiled within the AVP-IT based on the answers provided in the Action Plan Wizard. The Action Plan provides tailored feedback responsive to the implementation status (pending, partial, or full) for each strategy, stepped guidance on how to implement each strategy (Table 5), and an array of resources developed from previous AVP studies that are designed to facilitate implementation of each strategy. No sensitive information is collected.
 Table 4. My Action Plan Wizard Data Input.
Table 4. My Action Plan Wizard Data Input. Table 5. Summary of AVP Champion Tasks by Strategy.
Table 5. Summary of AVP Champion Tasks by Strategy. - (3)
- My Toolkit provides the AVP Champion with an ‘à la carte’ selection of printable resources, video testimonials on the importance of each strategy, and tips on successful implementation.
- (4)
- Contact Us provides the AVP Champion with a form to contact the AVP research team with questions or to report issues with the AVP-IT website. A back-end database collects metrics including Action Plan data and Google analytic data (e.g., time spent on the AVP-IT and pages and resources accessed).
Action Plan Printout: The Action Plan comprises sections that describe each of the six intervention strategies. These are listed in order of the recommended implementation sequence: establish an AVP Champion, link provider to CME, institute quarterly assessment and feedback reports, develop a patient reminder system, develop a provider EMR prompt to cue to the presence of vaccine eligible youth, and promote a patient education app (HPVcancerFree) [23,25]. Each of the six strategy sections provides information describing the strategy and its importance: ‘How To’ steps to follow to implement the strategy, ‘Tools’ that link to resources needed in the implementation process, ‘Tips for Success’ that list bulleted practical recommendations for success informed by previous studies, and ‘Quotes from the Field’ that provides tips from HPCs who have implemented the strategies. Downloadable, printable, and/or viewable ‘tools’ include instructional videos, assessment and feedback report templates, algorithms for programming EHR-based provider and patient reminders, promotional flyers (i.e., for the AVP continued medical (CME) and nursing (CNE) education activity and HPVcancerFree app), tracking forms, and scripts to facilitate communication. The AVP Champions were responsible for approximately 16 itemized tasks (Table 5).
3.2. Phase 2: Formative Evaluation
3.2.1. Step 5: AVP-IT Usability Results
Five members of the expert advisory group completed the usability rating scales. The sample comprised physicians (n = 3), a clinic administrator (n = 1), and a community non-profit manger (n = 1), who were mostly male, 50–59 years of age, and non-Hispanic white (Table 6). Most participants reported reviewing all the AVP-IT pages: About AVP-IT’ (5 of 5), Action Plan Wizard (3 of 5), tailored Action Plan printout (3 of 5), and ‘My Toolkit’ (5 of 5). The AVP-IT was rated positively for most usability parameters assessing acceptability (Table 7) and utility (Table 8). Three participants completed a 30 min follow-up debriefing session.

Table 6.
Demographic Characteristics of AVP-IT Usability Sample (N = 5).

Table 7.
Acceptability: Usability Ratings for AVP-IT (N = 5) 1.

Table 8.
Utility: Usability Ratings for AVP-IT (N = 5) 1.
Acceptability: All participants rated the AVP-IT and Action Plan as acceptable. Credibility: The information in the AVP-IT was rated as accurate and trustworthy by all respondents. Ease of use: All participants rated the AVP-IT was easy to use, stating that it is “easy to use and easy to navigate” (Participant 3) and that “It can be a good tool for clinics who have a state of readiness so they can develop a strategy … it was easy to utilize.” (Participant 4). Complexity: All participants that the AVP-IT functions were well integrated. At least four of five participants agreed that the AVP-IT was not overly complex, that the AVP-IT did not require technical support to be able to use it, and that extensive learning was not necessary for its use. Participants stated that they liked the “organization” (Participant 1), “the sequence and flow of the overview [and] the simplicity” (Participant 4), and that it was “clean and clear” (Participant 3). They noted that “the Action Plan was very detailed” (Participant 1) and liked the “option to review information in multiple ways (pop-ups, downloads)” on the tools page (Participant 4). Information scope: All participants rated the AVP-IT and the tailored Action Plan as providing an appropriate amount of information stating that it “has good information … it sums up and gives clear details regarding the work to improve HPV vaccination rates.” (Participant 3) Duration: Participants stated that AVP-IT was “short and snappy, I didn’t have to click previous page etc.-it was drop down” (Participant 5) and all rated the Action Plan as being of appropriate duration.
Helpfulness: All participants rated the ‘About AVP-IT’ page as helpful. Three out of four participants stated that the Action Plan Overview, How To, Tools, and Tips for Success was helpful, and at least four or five stated that the ‘My Toolkit’ page sections of About, How To, Tools, and Tips for Success were helpful. Fewer participants (two of five) perceived the ‘Testimonial’ section as extremely helpful or very helpful.
Recommendations for improvement within the AVP-IT website included more role modelling stories on “challenges practices have had and how they overcame them” that are “tailored to the practice” (Participant 1) and to “show actual improvement in practices sites that had already used the website [using] examples of real-life scenarios” (Participant 2), and to show “Actual physician-family scenarios showing effective communication/actions taken by the provider to deal with specific parental concerns” (Participant 2). Recommendations for improvement of the tailored Action Plan included a comment on the challenge “that sometimes the person entering the answer may be unsure of the correct response. Since the survey only includes two responses options for some of the questions, it might be a little challenging” (Participant 4) and to “add information about anticipated response time” in the ‘Contact Us’ page (Participant 4).
Perceived impact: All participants rated the information received in the tailored Action Plan as impactful in enabling clinics to adopt, implement, and maintain evidence-based strategies to increase HPV immunization. Participants stated that they “found it helpful,” (Participant 1), that “all practice sites can benefit from the information on the website,” (Participant 2), that “this can be an impactful tool … I think it is a great platform to get centers started in the right direction … [to] meet the needs of centers to enhance their vaccination strategy,” (Participant 4) and that “other clinics will see value in the tool … it gives a clear outline/road map to improve quality.” (Participant 3). One participant suggested the need for a partner to advertise at a statewide level (Participant 5).
Motivational appeal: All participants agreed that other clinics should use the AVP-IT website and will use the Action Plan. Most participants agreed that they would like to use the AVP-IT (4 of 5) but fewer agreed that other clinics would use the AVP-IT website (2 of 5). Participants indicated they found it appealing. Recommendations to improve AVP-IT user appeal included adding suggestions to add a section on “how to respond to specific parental concerns/comments” (Participant 3) in the tools page and to update the testimonials section to be more dynamic “since the photos were stagnant and did not change.” (Participant 4)
Relative advantage: Participant ratings comparing the AVP-IT to usual practice (i.e., implementing strategies to increase HPV vaccination without the AVP-IT) were significantly skewed toward increased perceived ease and effectiveness (Table 9).

Table 9.
Provider Ratings of AVP-IT (Comparison to Usual Practice) (n = 5).
3.2.2. Step 6: Feasibility Case Study Results
Participating AVP Champions were medical assistants in the two participating clinics. They were female, Hispanic, between the ages of 20 and 29, reported their highest level of education as high school or GED (n = 1) and college degree (n = 1). At baseline, initiation of AVP strategies was classified as ‘pending.’ The exception was ‘parent education.’ This was classified as ‘partial’ because one clinic was providing parent education but had not yet provided the HPVcancerFree app. During the feasibility study, one of the champions resigned from the clinic to pursue other employment opportunities. This limited follow-up data to a single clinic site. At three-month follow-up, the strategies of AVP Champion, provider prompts, and parent education had been fully implemented and parent reminders had been partially implemented in accordance with AVP criteria (Table 10). Strategies of assessment and feedback and provider CME were ‘pending’.

Table 10.
AVP-IT Feasibility Case Study: Change in Implementation of AVP Evidence-based Strategies from Baseline to 3-month Follow-up (n = 1).
3.3. Exit Interview Results
An exit interview was completed with one AVP Champion. She reported reviewing the AVP-IT Action Plan with her clinic manger and beginning to implement patient reminders by calling parents, since they did not have an automatic reminder system in place. She informed physicians to check if patients were due for the HPV vaccination through the state immunization tracking system (ImmTrac) and began referring parents to the HPVcancerFree app. She also reported that both the AVP continuing medical (CME) and nursing education (CNE) activity and AVP parent education app was being promoted through flyers hung up in the clinic as well as emails sent to clinic staff. Despite some challenges in gaining momentum on the AVP strategy rollout, she did not report any difficulty using the AVP-IT or her clinic’s tailored Action Plan, and she did not have any suggestions for improving the tool for future use.
3.4. Monitoring Calls
Although both champions completed the AVP-IT Action Wizard and obtained their tailored Action Plans without any trouble, they both encountered challenges with beginning the roll out of AVP strategies in their clinics. Little progress was reported during the first two months. The research team liaised with the deputy general manager of the clinic network who then provided closer oversight on the initiative. The order of rollout of AVP strategies was adjusted to commence with strategies that were less complex to implement (e.g., promoting and linking providers to the AVP-IT CME and promoting the HPVcancerFree parent education app).
4. Discussion
There is evidence for the efficacy of presumptive bundled messaging, assessment and feedback, provider prompts, patient reminders, and consumer education as strategies to increase HPV vaccination rates [19,20,21]. Historically, there has been uneven adoption and implementation of these strategies. Repeated in-person training and technical assistance have been conventionally employed to overcome individual and organizational barriers to implementing these strategies [47]. This study demonstrated that the evidence-based Adolescent Vaccination Program (AVP), a multi-component program originally delivered in-person in clinic settings to increase HPV vaccination, can be adapted to an online self-guided format. This online tool can provide guidance to implement these strategies, offering an innovative self-directed ‘do-it-yourself’ alternative to usual implementation practice.
The AVP-IT is designed to mitigate barriers to dissemination. Online delivery is intuitively appealing because it can offer intervention fidelity, tailor guidance to the clinic’s readiness to implement strategies, and reduce costs of training or materials. The utility of Internet-based decision support has been demonstrated in public health practice [28,29,30].
The premise for the adaptation of the AVP to the online AVP-IT (rather than development of the intervention from scratch) resided in the evidence for efficacy of the original AVP, the accessibility of the AVP creators to advise on adaptation, and the existence of original assets that could be modified for standalone use [37,38]. Irrespective, challenges in creating the AVP-IT included ensuring representation and fidelity to the original behavioral objectives, functionality of the original fully supported strategies, acceptability to end-users, feasibility for clinic-based delivery, and positive impact on implementation efforts.
4.1. Usability
HCPs rated the AVP-IT as acceptable, credible, easy to use, simple, of sufficient scope, helpful, impactful, and appealing. Results of usability testing suggested that the AVP-IT could be acceptable as a standalone do-it-yourself intervention without the need for external support from a research or technical support team. This is consistent with the accruing evidence for the efficacy of digital decision support applications in impacting community health decision making [28,29,30]. Expert stakeholders were supportive of the design specifications to provide a simple, easy, rigorous (long digital lifespan), salient (tailored), and motivational intervention. The AVP-IT was also rated as adding significant thoroughness and fidelity to the implementation process. It was not, however, rated as a significant time saver. Feedback on the relative advantage of the AVP-IT was commensurate with those of similar clinic- and community-based implementation decision support [42,55]. The more temperate ratings for timeliness tend to occur in lockstep when the thoroughness and fidelity of a given practice are improved [40,42]. Usability is a necessary, but not sufficient, indicator of successful implementation in the clinic setting. Feasibility testing is an important next step in moving digital decision support interventions toward adoption.
4.2. Feasibility
The feasibility testing case study also provides initial evidence for the feasibility of the AVP Implementation Tool (AVP-IT) in guiding clinic staff to implement the AVP unassisted. The AVP-IT is designed to provide high-fidelity stand-alone support that requires little-to-no intervention from developers outside the clinic. The AVP-IT remained accessible to clinic staff and the program functioned as designed in the field trial. No problems or disruptions to regular clinic functions were reported by participants in accessing and using the online AVP-IT website and creating and downloading the tailored Action Plan. During the feasibility test, the utility of the Action Plan was demonstrated with movement of three strategies (AVP Champion, provider prompts, and parent education) from ‘pending’ (not implemented) to ‘fully implemented’ by 3-month follow-up. Despite these changes, the feasibility testing highlighted a number of important facilitators and barriers to the successful deployment of the AVP-IT in clinics [32,45,46,47,49,50,52,53,54,56,57].
4.3. Facilitators and Barriers of Strategy Roll Out
The AVP-IT feasibility testing case study confirmed that individual- and clinic-level capacity was essential in successful Action Plan implementation of the AVP Champion, provider assessment and feedback, provider education, and patient education.
AVP Champion: Vaccination champions can encourage HPV vaccination as a clinic priority. In this feasibility study the role of the AVP Champion was to follow the AVP Action Plan guidelines for the roll out of AVP strategies. This role was prescriptive to provide clear and manageable tasks that could be transferred between staff members. Engagement in more elaborate promotional work, while potentially beneficial, was not expected. In this study, the clinic leadership recommended medical assistants (MAs) to be AVP Champions because these staff were based within a given clinic, familiar with clinic operations, and, unlike clinicians in this setting, had the operational bandwidth. The participation of MAs in this role was a departure from previous AVP studies and represented a ‘test case’ for this staff category. Even with the AVP-IT strategies to build champion capacity (tailored stepped Action Plan and a well-delineated website with informational videos), the MAs had difficulty accomplishing the tasks. This was due to interrelated issues of uncertainty about work priorities and competing demands to meet clinic metrics, expectations from leadership regarding this, and inertia to follow through on the Action Plan tasks.
Leadership support was established at the front end of the study but insufficiently exploited during it. Providing a tailored Action Plan can be an innovative contribution to the field but is still subject to organizational barriers. This includes the concerns of clinic leadership regarding resource allocation to implement the recommended strategies that are dedicated to a single vaccination issue. Despite monthly updates by the research coordinator with the AVP Champions, there was initial inertia in enacting the Action Plan. While antithetical to the goal of a stand-alone implementation tool, clinic leadership was engaged by the AVP team to more actively direct the AVP-IT Champions. This catalyzed MA activity to implement the AVP strategies and underscores the importance of leadership involvement.
The study confirmed the advantages of having leadership or clinicians taking on the champions role, or, if a clinic lacked this capacity, to provide the appropriate support to the assigned champion. This study also reinforced the importance of champions having a solid understanding of the initiative as well as enthusiasm and the authority to drive the implementation process in the clinic setting. More testimonials featuring coping role models describing successful implementation (suggested in usability testing) provide important added training and motivation to champions, influencing normative perceptions as well as skills and self-efficacy.
In previous studies, informational webinars had been used to train champions before each strategy rollout. Webinars were not employed within the concentrated timeframe of this feasibility study and may have played an important facilitation role. These are recommended for future work. The findings of this study highlighted the utility of checklists to accompany the Action Plan. These can provide a greater degree of ‘hand holding’ if lower-level staff are in the champion role. These also have facility in providing a concrete guide for leadership to assess progress and set common expectations. The feasibility of checklists is being assessed in a current field trial.
AVP-IT field testing confirmed the importance of organizational factors of strong prescriptive leadership to support the implementation and help to prioritize competing demands on staff in busy clinics. This included regular status update meetings with clinic/network leadership, stepped written guides for staff at a more granular level than that of the Action Plan (e.g., checklists in accompaniment of monitoring calls), and enhanced tools to assist with rapid onboarding, orientation, and training to accommodate a continual staff turnover (e.g., training videos and testimonials of implementation success). Given this, it is premature to declare that AVP-IT has achieved ‘standalone’ status.
Provider Assessment and Feedback: The EHR system is critical to the HPV initiative because it provides tracking as well as prompting functions [54]. The quality of assessment and feedback reporting and evaluation success of the AVP-IT depends on the quality of data available within the system. The AVP has been successful in large pediatric clinic networks with robust data management systems. This study provided insight into the challenges of implementing the AVP in smaller safety-net clinic networks. The strategy to provide assessment and feedback reports to HCPs was not implemented (remained ‘pending’) in the current study due to incongruity between data elements required for the report and the data available within the clinic EHR. Modifications to the existing EHR was beyond the scope of this feasibility study, as was programming EHR-based provider prompts. To mitigate technological resource barriers, the specificity of assessment and feedback can be downgraded (e.g., reporting number of clinic encounters referencing HPV vaccination vs. identifying initiation and completion rates within the clinic population) until such time that clinics adopt greater breadth and specificity of data entry for HPV vaccinations.
Provider Continuing Education: It is necessary that adequate knowledge and skills training be provided to HCPs and MAs who are frontline workers assigned to educate and motivate patients about the HPV vaccine [50]. Often, this training comes from in-person orientations and training (e.g., ACS, pharmaceutical representatives) [54]. Barriers to provider and staff trainings in busy clinics are that they involve provider absence that can adversely impact clinic productivity, provision of patient care, and revenue [54]. AVP-IT linkage to online CME was designed to provide scheduling flexibility to overcome this barrier while providing high fidelity skills training with ethics credit. Within the 3-month feasibility study, the AVP Champion had fully implemented the promotion about the CME. Immediate HCP registration in the CME was not observed. A longer-term implementation trial would allow sufficient time to determine if HCPs had incorporated the CME in their regular training schedules.
4.4. Parent Education
Patient-related barriers to HPV vaccination can include misinformation, language challenges, and low levels of literacy. Concerns of HCPs regarding antivaccine sentiments of stakeholders (parents) and perceived controversy over the stigma associated with the vaccine and the pervasion of internet-based antivaccine messaging have been reported as ‘outer setting’ barriers to implementation of HPC vaccination [58]. The AVP-IT provides adjunct materials such as posters and the AVP HPVcancerFree app (HPVCF) that highlight HPV vaccination, cuing parents to action and to help initiate conversation. The HPVCF app is designed to persuade parents by addressing perceived barriers. The impact of this has been previously described [25]. The AVP Champion fully implemented the promotion of the HPVCF. However, uptake of the app by parents was not observed. This study identified language barriers to existing materials that indicated the need for materials to accommodate non–English-speaking (Hispanic) patients. Addition of Spanish language materials and translation of the HPVCF is underway.
4.5. Limitations
Usability results should be interpreted in light of study limitations. Usability was conducted with five healthcare providers of varied job description. These respondents were sufficiently experienced and the sample size was appropriate for usability testing protocols that are designed to determine problems with the user experience, programming logic, and/or program bugs prior to field testing [43]. While statistical significance is less of an issue in prototype testing, conclusions regarding generalizability to other users, clinic types, and geographic region are naturally limited.
Feasibility case study results also need to be interpreted in light of study limitations. Assessment of AVP-IT affect was restricted to immediate pre-post change in implementation within a limited 3-month time frame in two test sites (with loss of one clinic site). This is preliminary formative work. The results indicate the need for a more robust AVP-IT evaluation. Longer-term follow-up with a larger sample of clinics is necessary to evaluate the implementation and impact of the AVP-IT on HPV vaccination rates and provide an understanding of generalizability across clinics.
A single-clinic experience is informative in the adaptation process but is in no way definitive of end results. Pilot feasibility studies are often limited in scope but sufficient to enable confidence that further field testing can be undertaken and to highlight anomalies such as program bugs, usability problems, or negative or harmful effects that indicate expanded testing may be premature. AVP-IT is being evaluated in a community-based trial in two safety-net clinic networks. More rigorous future RCTs are required to demonstrate the relative efficacy of this innovative digital approach compared with usual practice and could also inform on the cost-effectiveness implications of this implementation strategy.
The feasibility trial highlighted an implicit paradox in implementation research, that a tool designed to facilitate implementation of an evidence-based program is, itself, subject to implementation barriers. The AVP-IT may facilitate the implementation of the AVP, but what facilitates the implementation of the AVP-IT? If the AVP-IT ‘works,’ how do you get clinics to use it? Does the implementation tool require an implementation intervention for its use? Do pre-implementation activities that build clinic capacity (e.g., EHR upgrades for assessment and feedback data assessment or patient reminders) constitute an implementation intervention for the implementation tool?
4.6. Future/Policy
Progress in disseminating interventions to increase HPV vaccination has been pursued through academic institutions, government agencies, and private enterprises that have targeted clinic practices, provider knowledge and attitudes, and parent perceptions. Ongoing initiatives through vested national entities, including the National Cancer Institute (NCI), Centers of Disease Control and Prevention (CDC), and American Cancer Society (ACS); state organizations, such as the Cancer Prevention Research Initiative of Texas (CPRIT) and the HPV Coalition of Texas; and local organizations, such as the MD Anderson’s HPV Vaccination Initiative, have been contributing to mitigating the individual (attitudinal) and organizational (infrastructure) level barriers to HPV vaccination. These initiatives explore how to successfully facilitate the dissemination and implementation of evidence-based strategies to increase HPV vaccination. These initiatives may increase awareness and lower confusion regarding HPV vaccination guidelines, increase skills and self-efficacy for high-fidelity adaptation of strategies for the local clinic setting, and lower negative attitudes towards the HPV vaccination among HCPs. To date, the concerted efforts have demonstrated some success. HPV vaccination rates continue to rise with continued triangulation of efforts including increasing the vaccination eligible age, lowering dose requirements, inclusion of promotion of the vaccine among males, and shifts to presumptive bundled messaging. New innovations such as single-dose HPV vaccination are on the horizon. Contributory to this HPV-related ‘innovation agenda’ is the AVP-IT, which is among the first decision support tools that enable pediatric and community clinics to autonomously implement evidence-based strategies to increase HPV vaccination rates.
5. Conclusions
The AVP-IT and the provision of a stepped, tailored, clinic-based Action Plan that has acceptability as a guide to implement strategies to increase HPV vaccination may be feasible. Features of the adaptation, development, and testing of the AVP-IT reported here included a rigorous, stepped adaptation protocol with adaptation steps informed by iterative formative prototype testing (usability, feasibility, and perceived impact), providing empirical evidence to inform each subsequent development step. The AVP-IT decision support provides an Action Plan with tailored guidance to implement six evidence-based strategies (immunization champions, assessment and feedback, continuing education, provider prompts, parent reminders, and parent education). Healthcare providers rated the AVP-IT as acceptable, credible, easy, helpful, impactful, and appealing (≥80% agreement). They rated AVP-IT as making implementation easier and more effective compared to usual practice (p ≤ 0.05). Clinic-based AVP-IT use increased strategy implementation by 3-month follow-up. Study results need to be interpreted in the context of study limitations that include limited sample size, limited clinic-based testing, and no comparison sites. Irrespective, this study supports the translation of evidence-based programs for the clinic setting. The critical implementation facilitators and barriers described in the study can inform future work. The AVP-IT may provide an innovative contribution to accessible, utilitarian, and scalable decision support on implementing strategies to increase HPV vaccination rates in pediatric clinic settings.
Author Contributions
Authors contributing to the study and manuscript development were as follows: Conceptualization, R.S., L.S.S., S.W.V., E.L.F., L.C.T., C.M.H. and L.A.S.; methodology, R.S., L.S.S., E.L.F. and J.S.; software, R.S., L.C.T. and T.T.; validation, E.L.F. and L.C.T.; formal analysis, R.S., T.T., E.L.F. and J.S.; investigation, R.S., L.S.S. and S.W.V.; resources, S.W.V.; data curation, E.L.F., T.T., J.S. and L.C.T.; writing—original draft preparation, R.S. and E.L.F.; writing—review and editing, R.S., E.L.F., L.S.S., C.M.H., S.W.V., L.A.S., S.P. and L.A.S.; visualization, R.S. and E.L.F.; supervision, R.S. and E.L.F.; project administration, E.L.F. and L.C.T.; funding acquisition, R.S., L.S.S. and S.W.V. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by The Cancer Prevention and Research Institute of Texas (CPRIT), grant number PP190041.
Institutional Review Board Statement
This study was approved by the University of Texas Health Science Center at Houston Institutional Review Board (HSC-SPH-19-0197).
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to security restrictions.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Satterwhite, C.L.; Torrone, E.; Meites, E.; Dunne, E.F.; Mahajan, R.; Ocfemia, M.C.; Su, J.; Xu, F.; Weinstock, H. Sexually transmitted infections among US women and men: Prevalence and incidence estimates, 2008. Sex. Transm. Dis. 2013, 40, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Saraiya, M.; Unger, E.R.; Thompson, T.D.; Lynch, C.F.; Hernandez, B.Y.; Lyu, C.W.; Steinau, M.; Watson, M.; Wilkinson, E.J.; Hopenhayn, C.; et al. US assessment of HPV types in cancers: Implications for current and 9-valent HPV vaccines. J. Natl. Cancer Inst. 2015, 107, djv086. [Google Scholar] [CrossRef] [PubMed]
- Viens, L.J.; Henley, S.J.; Watson, M.; Markowitz, L.E.; Thomas, C.C.; Thompson, T.D.; Razzaghi, H.; Saraiya, M. Human Papillomavirus-Associated Cancers—United States, 2008–2012. MMWR Morb. Mortal. Wkly. Rep. 2016, 65, 661–666. [Google Scholar] [CrossRef] [PubMed]
- Chaturvedi, A.K.; Engels, E.A.; Pfeiffer, R.M.; Hernandez, B.Y.; Xiao, W.; Kim, E.; Jiang, B.; Goodman, M.T.; Sibug-Saber, M.; Cozen, W.; et al. Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J. Clin. Oncol. 2011, 29, 4294–4301. [Google Scholar] [CrossRef]
- Johnson, L.G.; Madeleine, M.M.; Newcomer, L.M.; Schwartz, S.M.; Daling, J.R. Anal cancer incidence and survival: The surveillance, epidemiology, and end results experience, 1973–2000. Cancer 2004, 101, 281–288. [Google Scholar] [CrossRef]
- Mehanna, H.; Beech, T.; Nicholson, T.; El-Hariry, I.; McConkey, C.; Paleri, V.; Roberts, S. Prevalence of human papillomavirus in oropharyngeal and nonoropharyngeal head and neck cancer—Systematic review and meta-analysis of trends by time and region. Head Neck 2013, 35, 747–755. [Google Scholar] [CrossRef]
- Calo, W.A.; Brewer, N.T. Trends in Genital Warts in the Era of Human Papillomavirus Vaccination. Sex. Transm. Dis. 2015, 42, 669–670. [Google Scholar] [CrossRef]
- Lairson, D.R.; Fu, S.; Chan, W.; Xu, L.; Shelal, Z.; Ramondetta, L. Mean direct medical care costs associated with cervical cancer for commercially insured patients in Texas. Gynecol. Oncol. 2017, 145, 108–113. [Google Scholar] [CrossRef]
- Oliver, S.E.; Unger, E.R.; Lewis, R.; McDaniel, D.; Gargano, J.W.; Steinau, M.; Markowitz, L.E. Prevalence of Human Papillomavirus Among Females After Vaccine Introduction-National Health and Nutrition Examination Survey, United States, 2003–2014. J. Infect. Dis. 2017, 216, 594–603. [Google Scholar] [CrossRef]
- Garland, S.M.; Kjaer, S.K.; Munoz, N.; Block, S.L.; Brown, D.R.; DiNubile, M.J.; Lindsay, B.R.; Kuter, B.J.; Perez, G.; Dominiak-Felden, G.; et al. Impact and Effectiveness of the Quadrivalent Human Papillomavirus Vaccine: A Systematic Review of 10 Years of Real-world Experience. Clin. Infect. Dis. 2016, 63, 519–527. [Google Scholar] [CrossRef]
- Ali, H.; Guy, R.J.; Wand, H.; Read, T.R.; Regan, D.G.; Grulich, A.E.; Fairley, C.K.; Donovan, B. Decline in in-patient treatments of genital warts among young Australians following the national HPV vaccination program. BMC Infect. Dis. 2013, 13, 140. [Google Scholar] [CrossRef]
- Baandrup, L.; Blomberg, M.; Dehlendorff, C.; Sand, C.; Andersen, K.K.; Kjaer, S.K. Significant decrease in the incidence of genital warts in young Danish women after implementation of a national human papillomavirus vaccination program. Sex. Transm. Dis. 2013, 40, 130–135. [Google Scholar] [CrossRef]
- Petrosky, E.; Bocchini, J.A., Jr.; Hariri, S.; Chesson, H.; Curtis, C.R.; Saraiya, M.; Unger, E.R.; Markowitz, L.E. Use of 9-valent human papillomavirus (HPV) vaccine: Updated HPV vaccination recommendations of the advisory committee on immunization practices. MMWR Morb. Mortal. Wkly. Rep. 2015, 64, 300–304. [Google Scholar]
- Meites, E.; Kempe, A.; Markowitz, L.E. Use of a 2-Dose Schedule for Human Papillomavirus Vaccination—Updated Recommendations of the Advisory Committee on Immunization Practices. MMWR Morb. Mortal. Wkly. Rep. 2016, 65, 1405–1408. [Google Scholar] [CrossRef]
- Moreira, E.D., Jr.; Block, S.L.; Ferris, D.; Giuliano, A.R.; Iversen, O.E.; Joura, E.A.; Kosalaraksa, P.; Schilling, A.; Van Damme, P.; Bornstein, J.; et al. Safety Profile of the 9-Valent HPV Vaccine: A Combined Analysis of 7 Phase III Clinical Trials. Pediatrics 2016, 138, e20154387. [Google Scholar] [CrossRef]
- Stillo, M.; Carrillo Santisteve, P.; Lopalco, P.L. Safety of human papillomavirus vaccines: A review. Expert. Opin. Drug Saf. 2015, 14, 697–712. [Google Scholar] [CrossRef]
- Office of Disease Prevention and Health Promotion. Vaccination. Available online: https://health.gov/healthypeople/objectives-and-data/browse-objectives/vaccination (accessed on 10 January 2022).
- Reagan-Steiner, S.; Yankey, D.; Jeyarajah, J.; Elam-Evans, L.D.; Curtis, C.R.; MacNeil, J.; Markowitz, L.E.; Singleton, J.A. National, Regional, State, and Selected Local Area Vaccination Coverage Among Adolescents Aged 13–17 Years—United States, 2015. MMWR Morb. Mortal. Wkly. Rep. 2016, 65, 850–858. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Vaccination Programs: Provider Assessment and Feedback. Available online: https://www.thecommunityguide.org/findings/vaccination-programs-provider-assessment-and-feedback (accessed on 10 January 2022).
- Centers for Disease Control and Prevention. Vaccination Programs: Provider Reminders. Available online: https://www.thecommunityguide.org/findings/vaccination-programs-provider-reminders (accessed on 10 January 2022).
- Centers for Disease Control and Prevention. Vaccination Programs: Client Reminder and Recall Systems. Available online: https://www.thecommunityguide.org/findings/vaccination-programs-client-reminder-and-recall-systems (accessed on 10 January 2022).
- Centers for Disease Control and Prevention. Vaccination Programs: Health Care System-Based Interventions Implemented in Combination. Available online: https://www.thecommunityguide.org/findings/vaccination-programs-health-care-system-based-interventions-implemented-combination (accessed on 10 January 2022).
- Crawford, C.A.; Shegog, R.; Savas, L.S.; Frost, E.L.; Healy, C.M.; Coan, S.P.; Gabay, E.K.; Spinner, S.W.; Vernon, S.W. Using Intervention Mapping to Develop an Efficacious Multicomponent Systems-Based Intervention to Increase Human Papillomavirus (HPV) Vaccination in a Large Urban Pediatric Clinic Network. J. Appl. Res. Child. 2019, 10, 9. [Google Scholar] [CrossRef]
- Vernon, S.W.; Savas, L.S.; Shegog, R.; Healy, C.M.; Frost, E.L.; Coan, S.P.; Gabay, E.K.; Preston, S.M.; Crawford, C.A.; Spinner, S.W.; et al. Increasing HPV Vaccination in a Network of Pediatric Clinics using a Multi-component Approach. J. Appl. Res. Child. 2019, 10, 11. [Google Scholar] [CrossRef]
- Shegog, R.; Savas, L.S.; Healy, C.M.; Frost, E.L.; Coan, S.P.; Gabay, E.K.; Preston, S.M.; Spinner, S.W.; Wilbur, M.; Becker, E.; et al. AVPCancerFree: Impact of a digital behavior change intervention on parental HPV vaccine-related perceptions and behaviors. Hum. Vaccin. Immunother. 2022, 18, 2087430. [Google Scholar] [CrossRef]
- Savas, L.S.; Farias, A.J.; Healy, C.M.; Shegog, R.; Fernandez, M.F.; Frost, E.L.; Coan, S.P.; Crawford, C.; Spinner, S.; Vernon, S.W. Wording Matters When Pediatricians Recommend HPV Vaccination. J. Appl. Res. Child. 2021, 12, 5:1–5:16. [Google Scholar] [CrossRef]
- Powell, B.J.; Waltz, T.J.; Chinman, M.J.; Damschroder, L.J.; Smith, J.L.; Matthieu, M.M.; Proctor, E.K.; Kirchner, J.E. A refined compilation of implementation strategies: Results from the Expert Recommendations for Implementing Change (ERIC) project. Implement. Sci. 2015, 10, 21. [Google Scholar] [CrossRef] [PubMed]
- Holstiege, J.; Mathes, T.; Pieper, D. Effects of computer-aided clinical decision support systems in improving antibiotic prescribing by primary care providers: A systematic review. J. Am. Med. Inform. Assoc. 2015, 22, 236–242. [Google Scholar] [CrossRef]
- Bright, T.J.; Wong, A.; Dhurjati, R.; Bristow, E.; Bastian, L.; Coeytaux, R.R.; Samsa, G.; Hasselblad, V.; Williams, J.W.; Musty, M.D.; et al. Effect of clinical decision-support systems: A systematic review. Ann. Intern. Med. 2012, 157, 29–43. [Google Scholar] [CrossRef] [PubMed]
- Kruse, C.S.; Ehrbar, N. Effects of Computerized Decision Support Systems on Practitioner Performance and Patient Outcomes: Systematic Review. JMIR Med. Inform. 2020, 8, e17283. [Google Scholar] [CrossRef]
- Green, L.W. From research to “best practices” in other settings and populations. Am. J. Health Behav. 2001, 25, 165–178. [Google Scholar] [CrossRef]
- Greenes, R.A.; Bates, D.W.; Kawamoto, K.; Middleton, B.; Osheroff, J.; Shahar, Y. Clinical decision support models and frameworks: Seeking to address research issues underlying implementation successes and failures. J. Biomed. Inform. 2018, 78, 134–143. [Google Scholar] [CrossRef]
- Yi, M.Y.; Hwang, Y. Predicting the use of web-based information systems: Self-efficacy, enjoyment, learning goal orientation, and the technology acceptance model. Int. J. Hum. Comput. 2003, 59, 431–449. [Google Scholar] [CrossRef]
- Dixon, B.E.; Kasting, M.L.; Wilson, S.; Kulkarni, A.; Zimet, G.D.; Downs, S.M. Health care providers’ perceptions of use and influence of clinical decision support reminders: Qualitative study following a randomized trial to improve HPV vaccination rates. BMC Med. Inform. Decis. Mak. 2017, 17, 119. [Google Scholar] [CrossRef]
- Pearson, N.; Naylor, P.J.; Ashe, M.C.; Fernandez, M.; Yoong, S.L.; Wolfenden, L. Guidance for conducting feasibility and pilot studies for implementation trials. Pilot. Feasibility Stud. 2020, 6, 167. [Google Scholar] [CrossRef]
- Bartholomew, L.K.; Parcel, G.S.; Kok, G.; Gottlieb, N.; Fernandez, M.E. Planning Health Promotion Programs: An Intervention Mapping Approach, 3rd ed.; Jossey-Bass: San Francisco, CA, USA, 2011. [Google Scholar]
- Card, J.J.; Solomon, J.; Cunningham, S.D. How to adapt effective programs for use in new contexts. Health Promot. Pract. 2011, 12, 25–35. [Google Scholar] [CrossRef]
- Wingood, G.M.; DiClemente, R.J. The ADAPT-ITT Model. A novel strategy of adapting evidence-based HIV interventions. J. Acquir. Immune Defic. Syndr. 2008, 47, S40–S46. [Google Scholar] [CrossRef]
- Spradley, J.P. The Ethnographic Interview; Holt, Rhinehart and Winston: New York, NY, USA, 1979. [Google Scholar]
- Shegog, R.; Bartholomew, L.K.; Czyzewski, D.I.; Sockrider, M.M.; Craver, J.; Pilney, S.; Mullen, P.D.; Koeppl, P.; Gold, R.S.; Fernandez, M.; et al. Development of an expert system knowledge base: A novel approach to promote guideline congruent asthma care. J. Asthma 2004, 41, 385–402. [Google Scholar] [CrossRef]
- Steffy, J.; Shegog, R.; Savas, L.; Frost, E.; Castillo-Alaniz, L.; Teague, T. An Anthropological Approach to the Adolescent Vaccination Program: Using Semi-structured Interviews to Inform a Public Health Intervention. In Proceedings of the 2019 Innovation in Cancer Prevention Research Experience for Undergraduates Closing Ceremony, Houston, TX, USA, 8 August 2019. [Google Scholar]
- Shegog, R.; Begley, C.E. Clinic-Based Mobile Health Decision Support to Enhance Adult Epilepsy Self-Management: An Intervention Mapping Approach. Front. Public. Health 2017, 5, 256. [Google Scholar] [CrossRef]
- Nielsen, J. Usability Engineering; Morgan Kaufmann: San Francisco, CA, USA, 1993. [Google Scholar]
- StataCorp. Stata Statistical Software: Release 16; StataCorp LLC: College Station, TX, USA, 2019. [Google Scholar]
- Calo, W.A.; Gilkey, M.B.; Leeman, J.; Heisler-MacKinnon, J.; Averette, C.; Sanchez, S.; Kornides, M.L.; Brewer, N.T. Coaching primary care clinics for HPV vaccination quality improvement: Comparing in-person and webinar implementation. Transl. Behav. Med. 2019, 9, 23–31. [Google Scholar] [CrossRef]
- Rand, C.M.; Tyrrell, H.; Wallace-Brodeur, R.; Goldstein, N.P.N.; Darden, P.M.; Humiston, S.G.; Albertin, C.S.; Stratbucker, W.; Schaffer, S.J.; Davis, W.; et al. A Learning Collaborative Model to Improve Human Papillomavirus Vaccination Rates in Primary Care. Acad. Pediatr. 2018, 18, S46–S52. [Google Scholar] [CrossRef]
- Groom, H.C.; Irving, S.A.; Caldwell, J.; Larsen, R.; Beaudrault, S.; Luther, L.M.; Naleway, A.L. Implementing a Multipartner HPV Vaccination Assessment and Feedback Intervention in an Integrated Health System. J. Public. Health Manag. Pract. 2017, 23, 589–592. [Google Scholar] [CrossRef]
- Henrikson, N.B.; Zhu, W.; Baba, L.; Nguyen, M.; Berthoud, H.; Gundersen, G.; Hofstetter, A.M. Outreach and Reminders to Improve Human Papillomavirus Vaccination in an Integrated Primary Care System. Clin. Pediatr. 2018, 57, 1523–1531. [Google Scholar] [CrossRef]
- Mann, D.; Hess, R.; McGinn, T.; Mishuris, R.; Chokshi, S.; McCullagh, L.; Smith, P.D.; Palmisano, J.; Richardson, S.; Feldstein, D.A. Adaptive design of a clinical decision support tool: What the impact on utilization rates means for future CDS research. Digit. Health 2019, 5, 2055207619827716. [Google Scholar] [CrossRef]
- Walling, E.B.; Dodd, S.; Bobenhouse, N.; Reis, E.C.; Sterkel, R.; Garbutt, J. Implementation of Strategies to Improve Human Papillomavirus Vaccine Coverage: A Provider Survey. Am. J. Prev. Med. 2019, 56, 74–83. [Google Scholar] [CrossRef]
- Eisen, J.C.; Marko-Holguin, M.; Fogel, J.; Cardenas, A.; Bahn, M.; Bradford, N.; Fagan, B.; Wiedmann, P.; Van Voorhees, B.W. Pilot Study of Implementation of an Internet-Based Depression Prevention Intervention (CATCH-IT) for Adolescents in 12 US Primary Care Practices: Clinical and Management/Organizational Behavioral Perspectives. Prim. Care Companion CNS Disord. 2013, 15, PCC.10m01065. [Google Scholar] [CrossRef] [PubMed]
- Kempe, A.; O’Leary, S.T.; Shoup, J.A.; Stokley, S.; Lockhart, S.; Furniss, A.; Dickinson, L.M.; Barnard, J.; Daley, M.F. Parental Choice of Recall Method for HPV Vaccination: A Pragmatic Trial. Pediatrics 2016, 137, e20152857. [Google Scholar] [CrossRef] [PubMed]
- Police, R.L.; Foster, T.; Wong, K.S. Adoption and use of health information technology in physician practice organisations: Systematic review. Inform. Prim. Care 2010, 18, 245–258. [Google Scholar] [CrossRef] [PubMed]
- Escoffery, C.; Riehman, K.; Watson, L.; Priess, A.S.; Borne, M.F.; Halpin, S.N.; Rhiness, C.; Wiggins, E.; Kegler, M.C. Facilitators and Barriers to the Implementation of the HPV VACs (Vaccinate Adolescents Against Cancers) Program: A Consolidated Framework for Implementation Research Analysis. Prev. Chronic Dis. 2019, 16, E85. [Google Scholar] [CrossRef]
- Hernandez, B.F.; Peskin, M.F.; Shegog, R.; Gabay, E.K.; Cuccaro, P.M.; Addy, R.C.; Ratliff, E.; Emery, S.T.; Markham, C.M. iCHAMPSS: Usability and Psychosocial Impact for Increasing Implementation of Sexual Health Education. Health Promot. Pract. 2017, 18, 366–380. [Google Scholar] [CrossRef]
- Farias, A.J.; Savas, L.S.; Fernandez, M.E.; Coan, S.P.; Shegog, R.; Healy, C.M.; Lipizzi, E.; Vernon, S.W. Association of physicians perceived barriers with human papillomavirus vaccination initiation. Prev. Med. 2017, 105, 219–225. [Google Scholar] [CrossRef]
- Damschroder, L.J.; Aron, D.C.; Keith, R.E.; Kirsh, S.R.; Alexander, J.A.; Lowery, J.C. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implement. Sci. 2009, 4, 50. [Google Scholar] [CrossRef]
- McKenzie, A.H.; Shegog, R.; Savas, L.S.; Healy, C.M.; Shay, L.A.; Preston, S.; Coan, S.; Teague, T.; Frost, E.; Spinner, S.W.; et al. Parents’ stigmatizing beliefs about the HPV vaccine and their association with information seeking behavior and vaccination communication behaviors. Hum. Vaccin. Immunother. 2023, 19, 2214054. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).