Influenza Vaccination Coverage Rates and Determinants in Greek Children until the Age of Ten (2008–2019), the Rhea Mother–Child Cohort
Abstract
1. Introduction
Background
2. Methods
2.1. Study Design and Participants
2.2. Influenza Immunization Data
2.3. Statistics
3. Results
3.1. Descriptive Characteristics of the Study Population
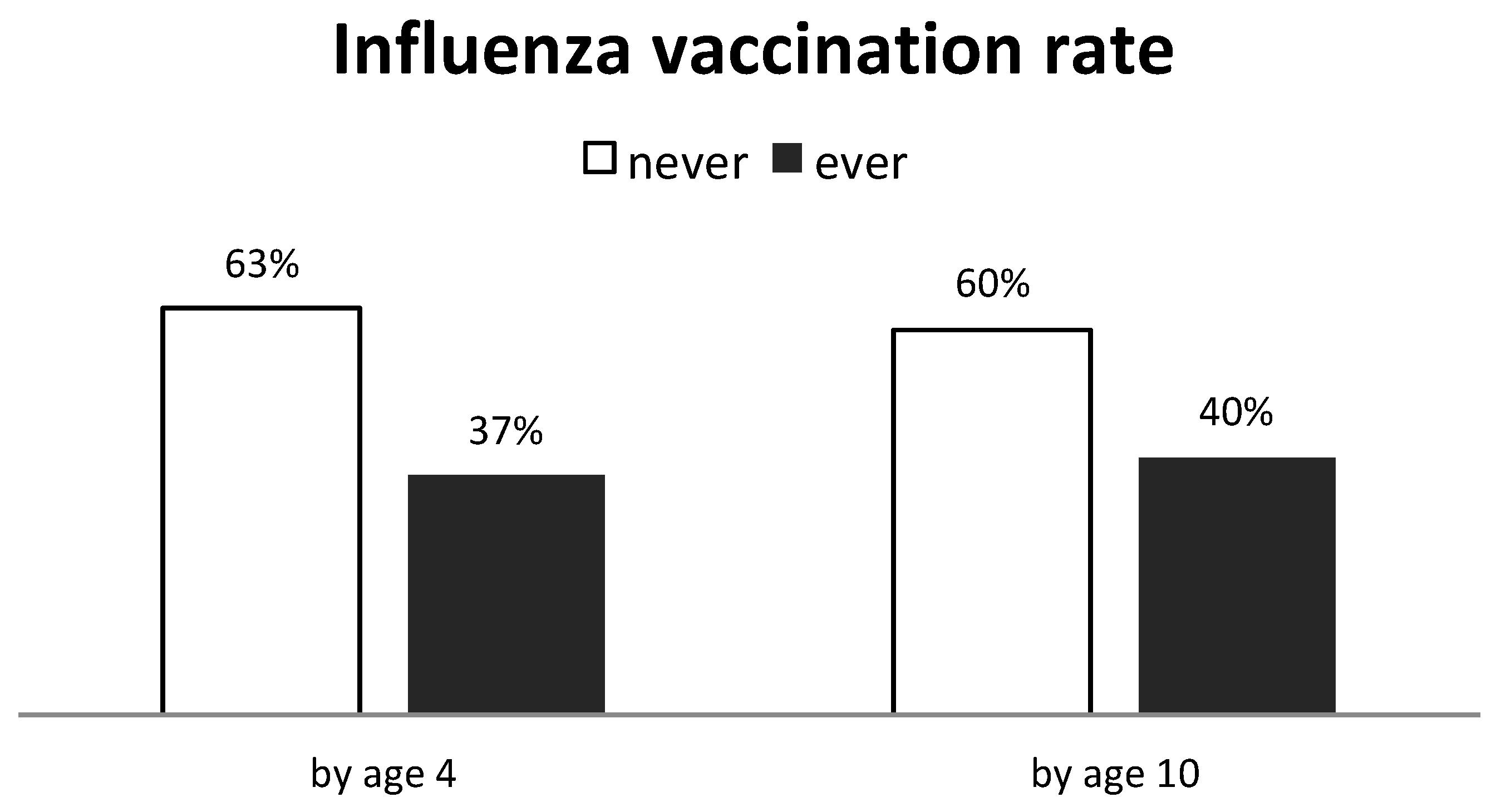
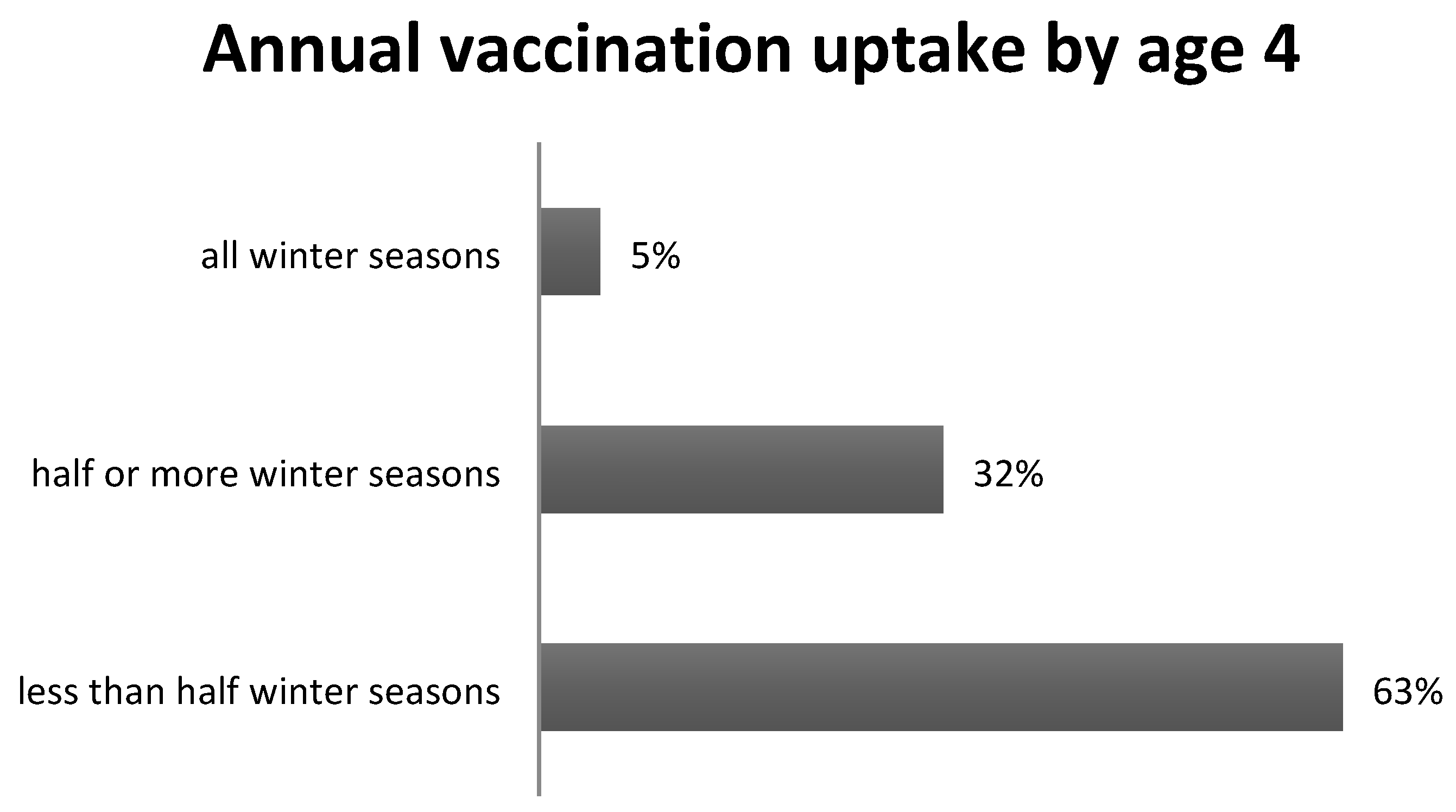
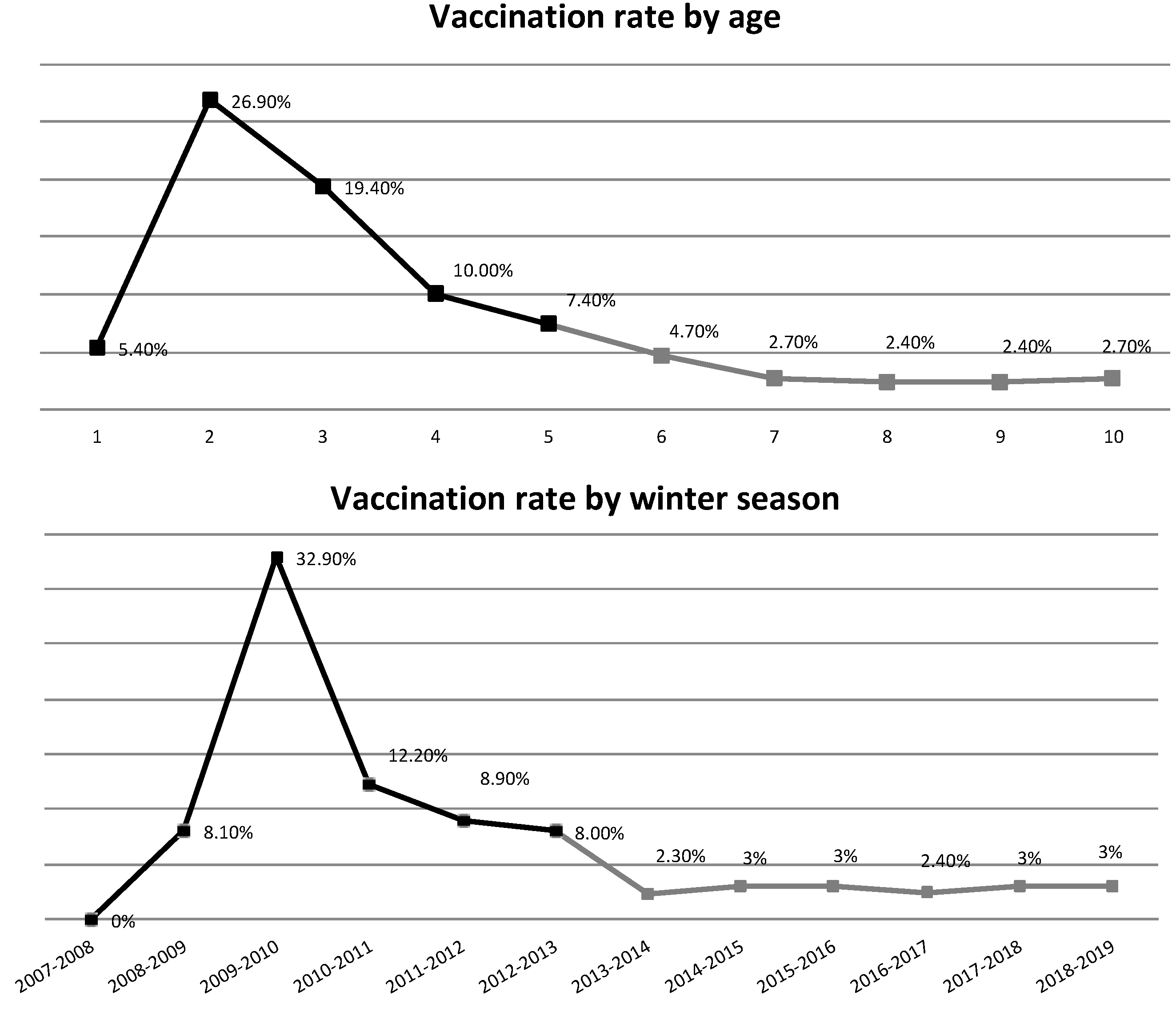
3.2. Influenza Vaccination Rate
3.3. Month of Vaccination and Number of Doses
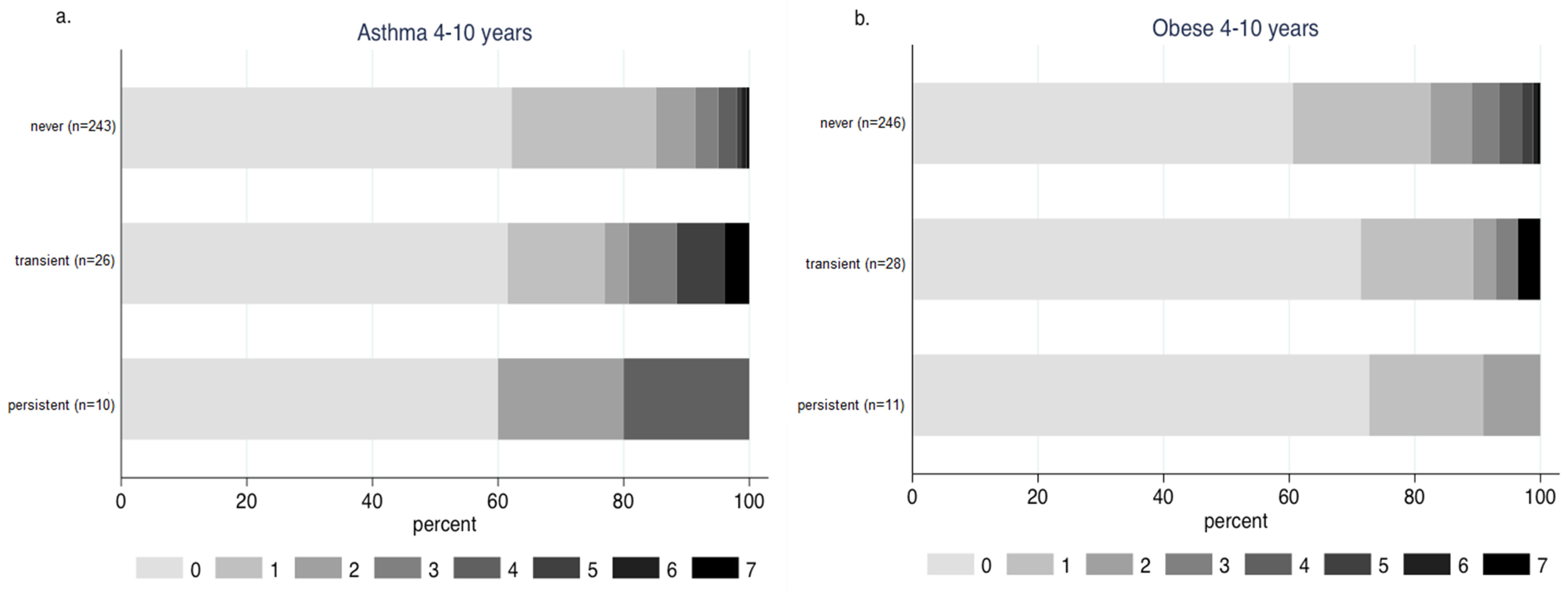
3.4. Influenza Vaccination Rates in Children with Asthma and Obesity
3.5. Determinants of Vaccination Uptake until Age Four
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| World Health Organization | (WHO) |
| Body mass index | (BMI) |
| Standard deviation | (SD) |
References
- Meade, P.; Kuan, G.; Strohmeier, S.; Maier, H.E.; Amanat, F.; Balmaseda, A.; Ito, K.; Kirkpatrick, E.; Javier, A.; Gresh, L.; et al. Influenza Virus Infection Induces a Narrow Antibody Response in Children but a Broad Recall Response in Adults. mBio 2020, 11, e03243-19. [Google Scholar] [CrossRef] [PubMed]
- Sakleshpur, S.; Steed, A.L. Influenza: Toward understanding the immune response in the young. Front. Pediatr. 2022, 10, 953150. [Google Scholar] [CrossRef]
- McElhaney, J.; Osterhaus, A. Third European Influenza Summit: Organized by the European Scientific Working group on Influenza (ESWI). Vaccine 2013, 31, 6161–6167. [Google Scholar] [CrossRef] [PubMed]
- Jefferson, T.; Rivetti, A.; Harnden, A.; Di Pietrantonj, C.; Demicheli, V. Vaccines for Preventing Influenza in Healthy Children. In Cochrane Database of Systematic Reviews; The Cochrane Collaboration, Ed.; John Wiley & Sons, Ltd.: Chichester, UK, 2008. [Google Scholar]
- Friedman, L.; Renaud, A.; Hines, D.; Winter, A.; Bolotin, S.; Johnstone, J.; Kwong, J.C.; McGeer, A.J.; Crowcroft, N.S.; Warshawsky, B.F. Exploring indirect protection associated with influenza immunization—A systematic review of the literature. Vaccine 2019, 37, 7213–7232. [Google Scholar] [PubMed]
- Principi, N.; Camilloni, B.; Esposito, S.; for the ESCMID Vaccine Study Group (EVASG). Influenza immunization policies: Which could be the main reasons for differences among countries? Hum. Vaccines Immunother. 2018, 14, 684–692. [Google Scholar] [CrossRef] [PubMed]
- Effraimidou, E.; Cassimos, D.C.; Medic, S.; Topalidou, M.; Theodoridou, M.; Maltezou, H.C. Vaccination programs for children aged up to 18 years in Europe, 2020. J. Child Health Care 2021, 136749352110552. [Google Scholar] [CrossRef]
- Álvarez García, F.J.; Cilleruelo Ortega, M.J.; Álvarez Aldeán, J.; Garcés-Sánchez, M.; Garrote Llanos, E.; Iofrío De Arce, A.; Melián, A.M.; Gómez, M.L.N.; Solas, V.P.; Calle, I.R.; et al. Immunization schedule of the Pediatric Spanish Association: 2022 recommendations. An. Pediatr. 2022, 96, 59.e1–59.e10. [Google Scholar] [CrossRef]
- Blank, P.R.; Van Essen, G.A.; Ortiz De Lejarazu, R.; Kyncl, J.; Nitsch-Osuch, A.; Kuchar, E.P.; Falup-Pecurariu, O.; Maltezou, H.C.; Zavadska, D.; Kristufkova, Z.; et al. Impact of European vaccination policies on seasonal influenza vaccination coverage rates: An update seven years later. Hum. Vaccines Immunother. 2018, 14, 2706–2714. [Google Scholar] [CrossRef]
- Giatraki, V.; Dimitriou, H.; Pappas, A.; Mamoulakis, D.; Makris, G.; Galanakis, E.; Perdikogianni, C. Vaccine coverage in children, adolescents and adults with type 1 diabetes and their close contacts in Crete. Hum. Vaccines Immunother. 2021, 17, 4291–4298. [Google Scholar] [CrossRef]
- Gkentzi, D.; Aggelopoulos, K.; Karatza, A.; Sinopidis, X.; Dimitriou, G.; Fouzas, S. Influenza vaccination among caregivers and household contacts of children with asthma. Vaccine 2021, 39, 2331–2334. [Google Scholar] [CrossRef]
- Panagiotopoulos, T. Ethnikí Meléti Katástasis Emvoliasmoú ton Paidión stin Elláda, 2012; ESDY: Athens, Greece, 2013. [Google Scholar]
- Vliora, C.; Papadakis, V.; Doganis, D.; Tourkantoni, N.; Paisiou, A.; Kottaridi, C.; Kourlamba, G.; Zaoutis, T.; Kosmidis, H.; Kattamis, A.; et al. A prospective study on the epidemiology and clinical significance of viral respiratory infections among pediatric oncology patients. Pediatr. Hematol. Oncol. 2019, 36, 173–186. [Google Scholar] [CrossRef]
- Smith, L.E.; Amlôt, R.; Weinman, J.; Yiend, J.; Rubin, G.J. Why do parents not re-vaccinate their child for influenza? A prospective cohort study. Vaccine 2020, 38, 4230–4235. [Google Scholar] [CrossRef]
- Chatzi, L.; Leventakou, V.; Vafeiadi, M.; Koutra, K.; Roumeliotaki, T.; Chalkiadaki, G.; Karachaliou, M.; Daraki, V.; Kyriklaki, A.; Kampouri, M.; et al. Cohort Profile: The Mother-Child Cohort in Crete, Greece (Rhea Study). Int. J. Epidemiol. 2017, 46, 1392–1393k. [Google Scholar] [CrossRef] [PubMed]
- Cole, T.J.; Lobstein, T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr. Obes. 2012, 7, 284–294. [Google Scholar] [CrossRef]
- UNICEF. A Situation Analysis of Children and Youth, Greece 2020; UNICEF: Athens, Greece, 2021. [Google Scholar]
- Danis, K.; Georgakopoulou, T.; Stavrou, T.; Laggas, D.; Panagiotopoulos, T. Socioeconomic factors play a more important role in childhood vaccination coverage than parental perceptions: A cross-sectional study in Greece. Vaccine 2010, 28, 1861–1869. [Google Scholar] [CrossRef]
- Pavlopoulou, I.D.; Michail, K.A.; Samoli, E.; Tsiftis, G.; Tsoumakas, K. Immunization coverage and predictive factors for complete and age-appropriate vaccination among preschoolers in Athens, Greece: A cross-sectional study. BMC Public Health 2013, 13, 908. [Google Scholar] [CrossRef]
- Oakley, S.; Bouchet, J.; Costello, P.; Parker, J. Influenza vaccine uptake among at-risk adults (aged 16–64 years) in the UK: A retrospective database analysis. BMC Public Health 2021, 21, 1734. [Google Scholar]
- Kazantzi, M.; Prapa, M.; Christakou, E.; Paraschou, D.; Kalabalikis, P.; Barbaressou, C.; Papaevangelou, V. Admissions due to vaccine preventable diseases in a large paediatric intensive care unit in Greece over a 10-year period. J. Paediatr. Child Health 2022, 58, 312–317. [Google Scholar] [CrossRef] [PubMed]
- Esposito, S.; Marchisio, P.; Cavagna, R.; Gironi, S.; Bosis, S.; Lambertini, L.; Droghetti, R.; Principi, N. Effectiveness of influenza vaccination of children with recurrent respiratory tract infections in reducing respiratory-related morbidity within the households. Vaccine 2003, 21, 3162–3168. [Google Scholar] [CrossRef] [PubMed]
- Poehling, K.A.; Fairbrother, G.; Zhu, Y.; Donauer, S.; Ambrose, S.; Edwards, K.M.; Staat, M.A.; Prill, M.M.; Finelli, L.; Allred, N.J.; et al. Practice and Child Characteristics Associated With Influenza Vaccine Uptake in Young Children. Pediatrics 2010, 126, 665–673. [Google Scholar] [CrossRef]
- Schmid, P.; Rauber, D.; Betsch, C.; Lidolt, G.; Denker, M.-L. Barriers of Influenza Vaccination Intention and Behavior—A Systematic Review of Influenza Vaccine Hesitancy, 2005–2016. PLoS ONE 2017, 12, e0170550. [Google Scholar]
| All Children | Children Ever Vaccinated against Influenza by Age Four | |||||||
|---|---|---|---|---|---|---|---|---|
| Univariate Models | Multivariate Stepwise Models 1 | |||||||
| n | % | n | % | OR | 95% CI | OR | 95% CI | |
| Determinants | ||||||||
| early daycare attendance | ||||||||
| yes | 182 | 22.0 | 80 | 26.1 | 1.44 * | [1.03, 2.02] | 1.45 | [0.95, 2.20] |
| no | 645 | 78.0 | 227 | 73.9 | 1.00 | 1.00 | ||
| younger siblings | ||||||||
| yes | 317 | 38.6 | 137 | 44.9 | 1.52 ** | [1.14, 2.03] | 1.65 ** | [1.14, 2.37] |
| no | 504 | 61.4 | 168 | 55.1 | 1.00 | 1.00 | ||
| passive smoking the first year | ||||||||
| yes | 423 | 56.3 | 142 | 51.3 | 0.72 * | [0.54, 0.97] | 0.69 * | [0.48, 0.98] |
| no | 328 | 43.7 | 135 | 48.7 | 1.00 | 1.00 | ||
| respiratory infections the first year | ||||||||
| 2–4 infections | 140 | 21.5 | 62 | 26.3 | 1.54 * | [1.05, 2.25] | 1.81 ** | [1.18, 2.77] |
| 0–1 infections | 511 | 78.5 | 174 | 73.7 | 1.00 | 1.00 | ||
| respiratory infections the fourth year | ||||||||
| 2–4 infections | 223 | 28.1 | 97 | 32.9 | 1.45 * | [1.05, 1.98] | 1.52 * | [1.03, 2.24] |
| 0–1 infections | 570 | 71.9 | 198 | 67.1 | 1.00 | 1.00 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karachaliou, M.; Damianaki, I.; Moudatsaki, M.; Margetaki, K.; Roumeliotaki, T.; Bempi, V.; Moudatsaki, M.; Chatzi, L.V.; Vafeiadi, M.; Kogevinas, M. Influenza Vaccination Coverage Rates and Determinants in Greek Children until the Age of Ten (2008–2019), the Rhea Mother–Child Cohort. Vaccines 2023, 11, 1241. https://doi.org/10.3390/vaccines11071241
Karachaliou M, Damianaki I, Moudatsaki M, Margetaki K, Roumeliotaki T, Bempi V, Moudatsaki M, Chatzi LV, Vafeiadi M, Kogevinas M. Influenza Vaccination Coverage Rates and Determinants in Greek Children until the Age of Ten (2008–2019), the Rhea Mother–Child Cohort. Vaccines. 2023; 11(7):1241. https://doi.org/10.3390/vaccines11071241
Chicago/Turabian StyleKarachaliou, Marianna, Irene Damianaki, Maria Moudatsaki, Katerina Margetaki, Theano Roumeliotaki, Vicky Bempi, Marina Moudatsaki, Lida Vaia Chatzi, Marina Vafeiadi, and Manolis Kogevinas. 2023. "Influenza Vaccination Coverage Rates and Determinants in Greek Children until the Age of Ten (2008–2019), the Rhea Mother–Child Cohort" Vaccines 11, no. 7: 1241. https://doi.org/10.3390/vaccines11071241
APA StyleKarachaliou, M., Damianaki, I., Moudatsaki, M., Margetaki, K., Roumeliotaki, T., Bempi, V., Moudatsaki, M., Chatzi, L. V., Vafeiadi, M., & Kogevinas, M. (2023). Influenza Vaccination Coverage Rates and Determinants in Greek Children until the Age of Ten (2008–2019), the Rhea Mother–Child Cohort. Vaccines, 11(7), 1241. https://doi.org/10.3390/vaccines11071241








