1. Introduction
Since 2019, the COVID-19 virus has rapidly spread from China to the rest of the world, becoming one of the most widespread pandemics in modern human history. In a short period, the global number of confirmed cases and fatalities grew, making it a leading cause of death. To substantially reduce the risk of severe illness and death, countries relied on vaccine development and the production of oral medications. Vaccination can help alleviate the burden of the disease, reduce pressure on healthcare systems, and prevent outbreaks. Moreover, when a large proportion of a population is immunized, disease transmission is significantly decreased and herd immunity can be achieved [
1,
2].
Vaccination acts as a protective measure that builds individual’s defenses and disrupts transmission chains. It bolsters the body’s immune system and is the most effective and cost-efficient method to control infectious diseases. Vaccines can successfully prevent severe symptoms after infection, thus reducing hospitalization and death rates [
2,
3,
4]. Numerous past empirical studies have used the Health Belief Model to explore changes in health behaviors during the SARS and H1N1 outbreaks. These studies show that when people are convinced of a pandemic’s severity, they perceive an increased risk of illness, trust the effectiveness of preventive measures, and consider the costs of adopting such behaviors as low, making them more likely to engage in preventive actions [
5].
A review of the literature on vaccine acceptance reveals that the “Health Belief Model” has been widely discussed as a theoretical basis for preventive health behaviors since the 1970s. Many researchers have used this theory to study vaccine acceptance in relation to H1N1, measles, human papillomavirus, and rabies vaccines [
6,
7,
8]. Wong [
9] applied the Health Belief Model to investigate the acceptance of COVID-19 vaccines among the Hong Kong population, while Ao [
10] employed the model to examine the acceptance of COVID-19 vaccines among adults in Lilongwe, Malawi’s capital.
Earlier studies have confirmed that online WOM and recommendations in healthcare impact patients’ medical decisions and the adoption of new medications [
11,
12]. The research findings mentioned above indicate that prior studies using the Health Belief Model for COVID-19 vaccine-related research have primarily focused on specific populations in certain areas. However, a significant gap exists in the literature regarding the relationship between the Health Belief Model, vaccine acceptance, and positive and negative WOM evaluations.
Although medical word-of-mouth is a common phenomenon, previous studies in both the medical field and vaccine acceptance have rarely addressed the influence of WOM evaluations. Additionally, research has explored patient satisfaction and the effects of service quality, WOM, and trust on satisfaction with medical services [
13]. In summary, given the variations in positive and negative WOM evaluations, public perceptions of vaccination may be affected. This study aims to address the knowledge gap in the literature by using positive and negative types of WOM as moderating variables to investigate how positive and negative WOM evaluations may influence people’s health beliefs and vaccine acceptance amid the ongoing COVID-19 pandemic. The goal is to further analyze the differences in the relationships among the various factors.
2. Literature Review
2.1. Health Belief Model, HBM
The Health Belief Model is frequently employed to examine care and medication-taking behaviors among elderly individuals with chronic illnesses, as well as to conduct cross-sectional research on behavioral influences and predictions. It is also utilized in health prevention programs and vaccination research studies. The results indicate that the Health Belief Model can effectively predict and analyze health behaviors.
Perceived susceptibility refers to an individual’s subjective evaluation of the likelihood of getting a disease or confidence in a diagnosis. A stronger perception of susceptibility is linked to a greater health belief and an increased likelihood of engaging in health prevention behaviors. This perception varies among individuals due to differing opinions, resulting in significant differences in vulnerability to a disease. A study by Delshad [
14] found that all aspects of the Health Belief Model were associated with epidemic prevention behaviors and predicted these behaviors significantly.
Perceived seriousness refers to an individual’s assessment of the severity of a disease, including the potential harm to their health and social well-being. People’s perceptions of the severity of a disease can differ considerably, and those who underestimate the risk may engage in unhealthy behaviors. This evaluation includes beliefs about the disease and its impact on work and social roles relevant to the individual. Perceived seriousness, along with perceived susceptibility, are cognitive variables that can be influenced by education and knowledge.
Perceived benefits of taking action refer to an individual’s initial assessment of whether a particular action can reduce their susceptibility and severity to a disease while preserving personal health benefits. This belief is influenced by social norms and pressures, which can lead to different actions being embraced. However, the perceived benefits of action may sometimes be influenced by group norms and pressures, as noted by Adams [
15].
Perceived barriers to taking action refers to an individual’s assessment of the challenges or obstacles they may face when undertaking a specific action, such as inconvenient transportation, high costs, physical or mental discomfort, unsafe side effects, and negative media coverage. Conflicting information and frequent updates on the COVID-19 situation were perceived as barriers by 65.9% of respondents, according to a study by Jose [
16]. Shahnazi [
17] highlighted that perceived barriers and self-efficacy were the most significant factors influencing COVID-19 prevention behaviors, with a strong correlation between the two.
Cues to action refer to the motivation or triggers that prompt individuals to take action, which can be internal, such as physical discomfort or symptoms, or external, such as advice from friends and family, social media, healthcare professionals, and health education campaigns. The intensity of the stimulus needed to initiate action depends on the situation. Several studies have investigated factors influencing the intent or behavior of getting vaccinated, including information from healthcare providers and health education, media advocacy, frequent exposure to related information, friends and family suffering from the disease, and individuals with middle to upper socioeconomic status, who are more likely to receive more cues and pay more attention to relevant information.
Self-efficacy refers to an individual’s belief in their ability to perform a specific health behavior in different situations and is part of the Health Belief Model. The stronger a person’s self-efficacy for a particular task, the more confident they are in their ability to complete the task. This confidence leads to a greater willingness to continue participating and putting in more effort to achieve the desired outcome. Many studies have found a significant correlation between self-efficacy and epidemic prevention behaviors, meaning that the higher an individual’s confidence in adopting prevention measures, the more likely they are to engage in such behaviors. Researchers such as Barakat [
18], Fathian-Dastgerdi [
19], Shahnazi [
17], and Koesnoe [
20] have demonstrated that higher self-efficacy and perceived benefits of action lead to a greater willingness to engage in epidemic prevention measures.
According to the motivations and literature mentioned earlier, this study derives the following research hypotheses:
H1. There will be a significant impact of health beliefs (Perceived susceptibility, Perceived seriousness, Perceived benefits to taking action, Perceived barriers to taking action, Cue to action, and Self-efficacy) on the willingness to receive the COVID-19 vaccine.
2.2. Positive and Negative Word-of-Mouth
The concept of “word-of-mouth” dates back to the 1950s, when it was first discovered and began to be studied academically. Word-of-mouth is an important form of communication that involves the flow of information through interpersonal sources or orally transmitted information. Initially, word-of-mouth refers to the exchange of information through spoken communication between people who are discussing a brand, product, or service without any intention of promoting it commercially. It refers to everyday interactions between people, generating a non-commercial form of communication through natural exchange, and discussing various pieces of information about brands, products, and services. It is also a way for people to understand specific brands, products, and personal ideas through sharing [
21,
22]. Under high-pressure care situations, consumers will seek information to reduce risk when using medical services. Chang [
23] also mentioned that consumers search for product- or service-related information online or offline before making a decision to reduce potential risks [
24]. Erkan and Evans [
25] found that the adoption of word-of-mouth positively correlates with purchase intention, meaning that as consumers’ willingness to adopt word-of-mouth increases, purchase intention also rises.
Word-of-mouth can be positive or negative and has a significant impact on consumer behavior, affecting purchase decisions and product sales. Positive word-of-mouth is associated with recommendation and persuasion, while negative word-of-mouth is linked to customer complaints and can harm a company’s reputation. Negative word-of-mouth can be damaging as it spreads quickly and may result in decreased consumption and brand attitudes. Therefore, companies should monitor and manage word-of-mouth to ensure positive perceptions of their products or services [
26,
27].
Based on the aforementioned literature, scholars do not have a consistent conclusion regarding whether positive or negative word-of-mouth has a greater impact, which makes this study even more valuable. According to the motivations and literature mentioned earlier, this study derives the following research hypotheses:
H2. Positive word-of-mouth evaluations will have a significant moderating effect on the relationship between health beliefs (Perceived susceptibility, Perceived seriousness, Perceived benefits of taking action, Perceived barriers of taking action, Cue to action, and Self-efficacy) and the willingness to receive the COVID-19 vaccine.
H3. Negative word-of-mouth evaluations will have a significant moderating effect on the relationship between health beliefs (Perceived susceptibility, Perceived seriousness, Perceived benefits of taking action, Perceived barriers of taking action, Cue to action, and Self-efficacy) and the willingness to receive the COVID-19 vaccine.
3. Methods
The purpose of this study is to investigate the impact of various variables of the Health Belief Model on the willingness to receive COVID-19 vaccinations, and to examine the effects of positive and negative word-of-mouth as intervening variables. Empirical research is conducted with selected participants who reside in Taiwan and have received COVID-19 vaccinations. The paper concludes with a description of the questionnaire distribution, sample characteristics, and methods of questionnaire content analysis. The conceptual framework is shown in
Figure 1:
The nine research variables in this study are measured using the Likert 7-point scale. The questionnaire items are referenced from relevant literature and appropriate scales were selected for each, with the principle of not losing the original intention of the questions, and then making minor adjustments and modifications. SUS references the Walker [
28] and Khalafalla [
29] studies with four items. SER references the Walker [
28] and Jones [
30] studies with five items. BEN references the Walker [
28] and Berni [
31] studies with four items. BAR references the Walker [
28] and Berni [
31] studies with four items. CUE references the Walker [
28] and Khalafalla [
29] studies with five items. SEFF references the Yoo [
32] and Koesnoe [
20] studies with four items. PWOM and NWOM reference the Maisam [
33], Popp [
34], and An [
35] studies with eight items. WRV references the Nga [
36] and Ning [
37] studies with a total of five items.
In this study, judgmental sampling was used to gather samples. Google online surveys were employed, and six private educational institutions assisted in distributing paper surveys to students and their parents for completion. Further discussions were held regarding survey distribution and collection methods. The survey distribution period lasted from 15 March 2023 to 25 March 2023. Out of the 500 surveys distributed, 433 valid responses were collected after excluding missing responses, blanks, incomplete answers, and invalid multiple selections, resulting in an effective response rate of 86.6%. After collecting the surveys, the study first carried out encoding and data archiving of the questionnaires to facilitate subsequent statistical analysis. SPSS 23.0 statistical software was chosen for data analysis and processing.
5. Conclusions
Previous research on the influence of various independent variables on willingness in health behavior patterns has seldom considered the impact of word-of-mouth reviews. This study reveals that both positive and negative word-of-mouth can have an interference effect, even though some statistical results do not fully support the research hypotheses. Nonetheless, our findings offer an opportunity to investigate topics not covered in past research, aiming to fill the gap in the literature on word-of-mouth. Prior studies have indicated that the influence of positive and negative word-of-mouth information varies, leading to different conclusions. This research discovers that both positive and negative word-of-mouth information have significant interference effects in the dimension of behavioral barriers, with negative word-of-mouth having a more pronounced impact than positive word-of-mouth. This finding aligns with the majority of past research on word-of-mouth effects, which has shown that negative word-of-mouth has a greater influence than positive word-of-mouth in shaping consumer product attitudes or evaluating.
In the ANOVA statistical analysis of this study, it was found that the variables of marital status, residency status, and average monthly income had no significant effect. This study identified significant gender differences in perceived severity, perceived benefits of action, cues to action, and self-efficacy, with males scoring higher averages than females in all four aspects. Age differences revealed significant disparities in self-efficacy, as those aged 20 or younger had considerably higher self-efficacy than those aged 31 to 40. Education level displayed significant differences in cues to action and self-efficacy, with individuals educated up to junior high school having notably higher cues to action than those educated at the high school (vocational) level and higher than those educated at the university (professional) level. Additionally, the study explored the moderating effects of positive and negative word-of-mouth. As shown in
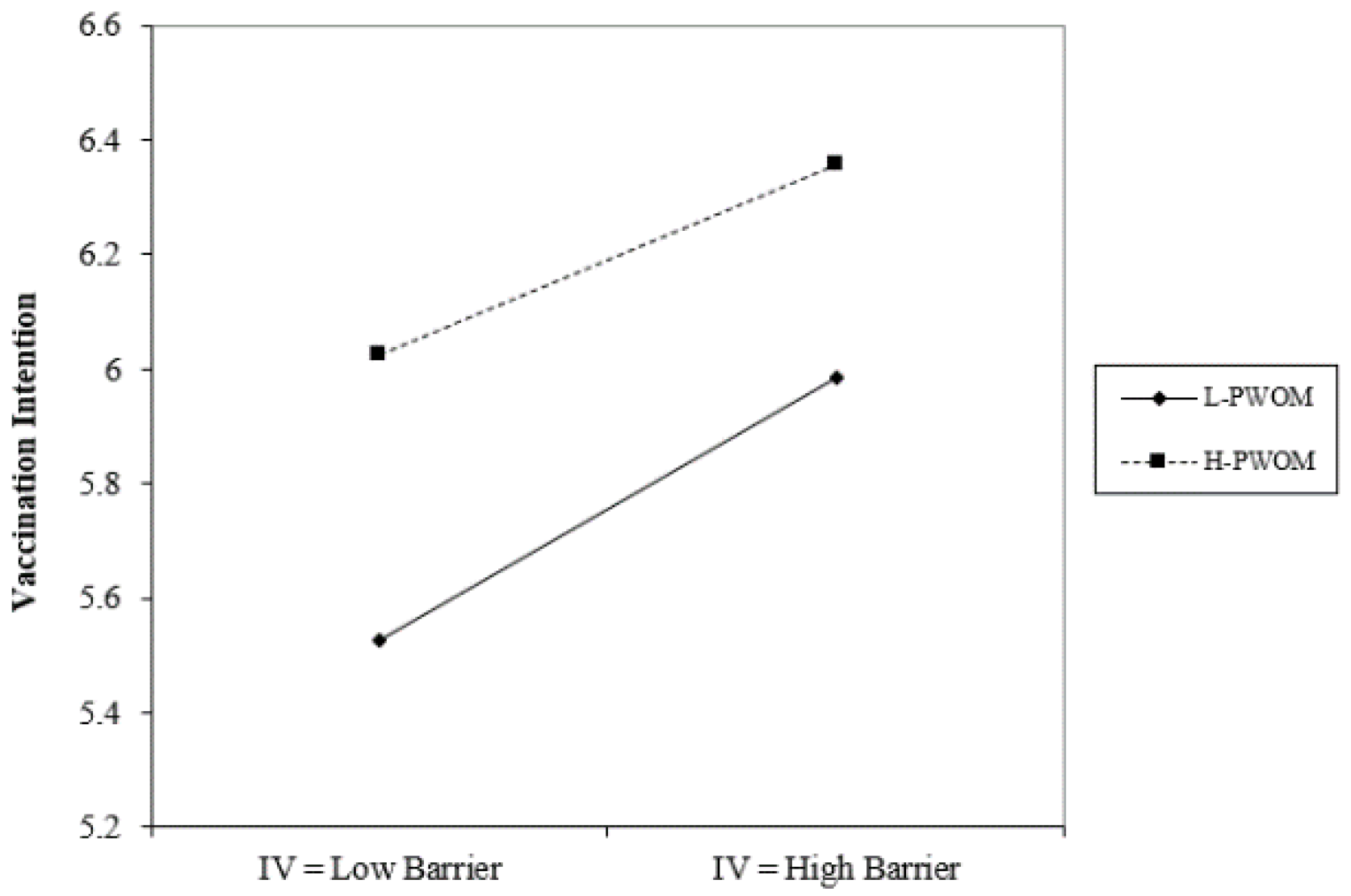
Figure 2, under conditions of high positive word-of-mouth, action benefits have a negative impact on the willingness to receive the COVID-19 vaccine; in contrast, when positive word-of-mouth is lower, action benefits have a positive impact on the willingness to receive the COVID-19 vaccine. On the other hand, as can be seen from
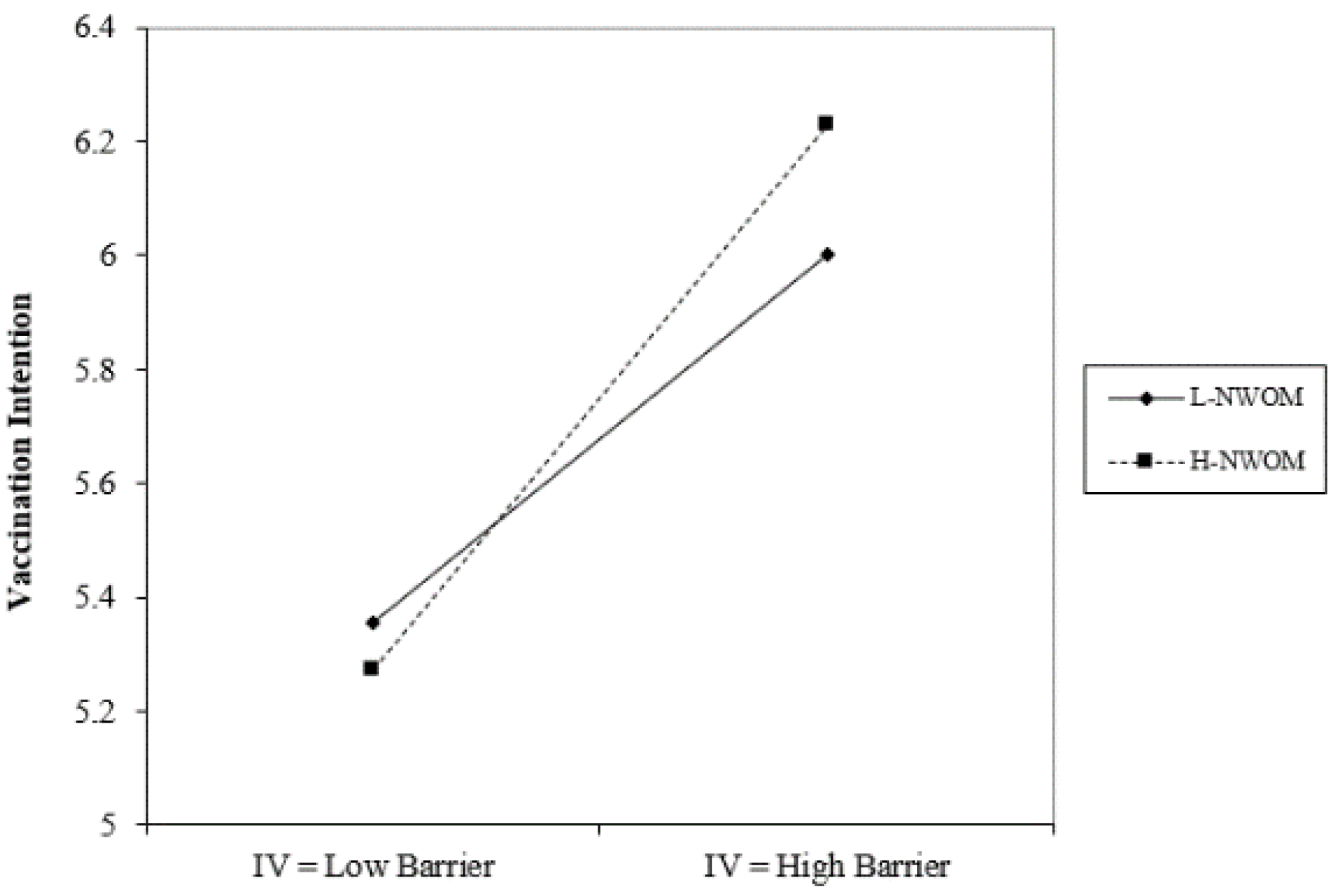
Figure 3 and
Figure 4, regardless of whether positive or negative word-of-mouth is high or low, mobility barriers have a positive impact on the willingness to inject COVID-19 vaccines; in addition, situations with high negative word-of-mouth have a more severe impact.
Compared to the results of previous studies, Tadesse [
38] found that factors most closely associated with employees’ preventive behaviors were monthly income, perceived behavioral barriers, cues to action, and self-efficacy. They also discovered that individuals with lower levels of cues to action and self-efficacy were less likely to adopt preventive behaviors. However, some studies have produced different results. For example, Shahnazi [
17] found that perceived severity was not significantly related to preventive behavior, while perceived benefits, self-efficacy, behavioral barriers, and cues to action had significant effects. In contrast, Barakat [
18] reported that cues to action were not significantly related to preventive behavior. Additionally, Fathian-Dastgerdi [
19] found significant negative correlations between adolescents’ perceived susceptibility, behavioral barriers, and preventive behaviors. Shahnazi [
17] discovered that while participants had higher perceived susceptibility, severity, benefits, and self-efficacy, their overall preventive behavior was ideal; however, perceived susceptibility and severity were not significantly related to preventive behavior. Furthermore, Alagili [
39] found that only perceived susceptibility and severity were not significantly related to preventive behavior.
This study’s practical contributions include investigating the interference effects of positive and negative word-of-mouth reviews, and allowing future epidemic prevention efforts to better understand vaccine recipients’ psychological state after receiving such information. To improve overall epidemic prevention effectiveness, future messages can be promoted through various social media platforms, using vivid descriptions, increasing interactions with consumers, and presenting information through images and videos. Word-of-mouth effects can save costs associated with large-scale vaccine promotion campaigns and help increase vaccination rates more quickly.
However, this study has limitations, such as being cross-sectional, using an online structured questionnaire, and having a limited sample size. Future research should expand the geographical scope, increase the sample size, and consider other variables, such as personal characteristics and organizational culture. Long-term follow-up studies can analyze the public’s changes in vaccine-related knowledge, attitudes, and behavior as the epidemic evolves. Lastly, future research can focus on the influence of social media word-of-mouth on vaccination intentions.