Epidemiology and SARS-CoV-2 Infection Patterns among Youth Followed at a Large Los Angeles Health Network during 2020–2022: Clinical Presentation, Prevalent Strains, and Correlates of Disease Severity
Abstract
1. Introduction
2. Methods
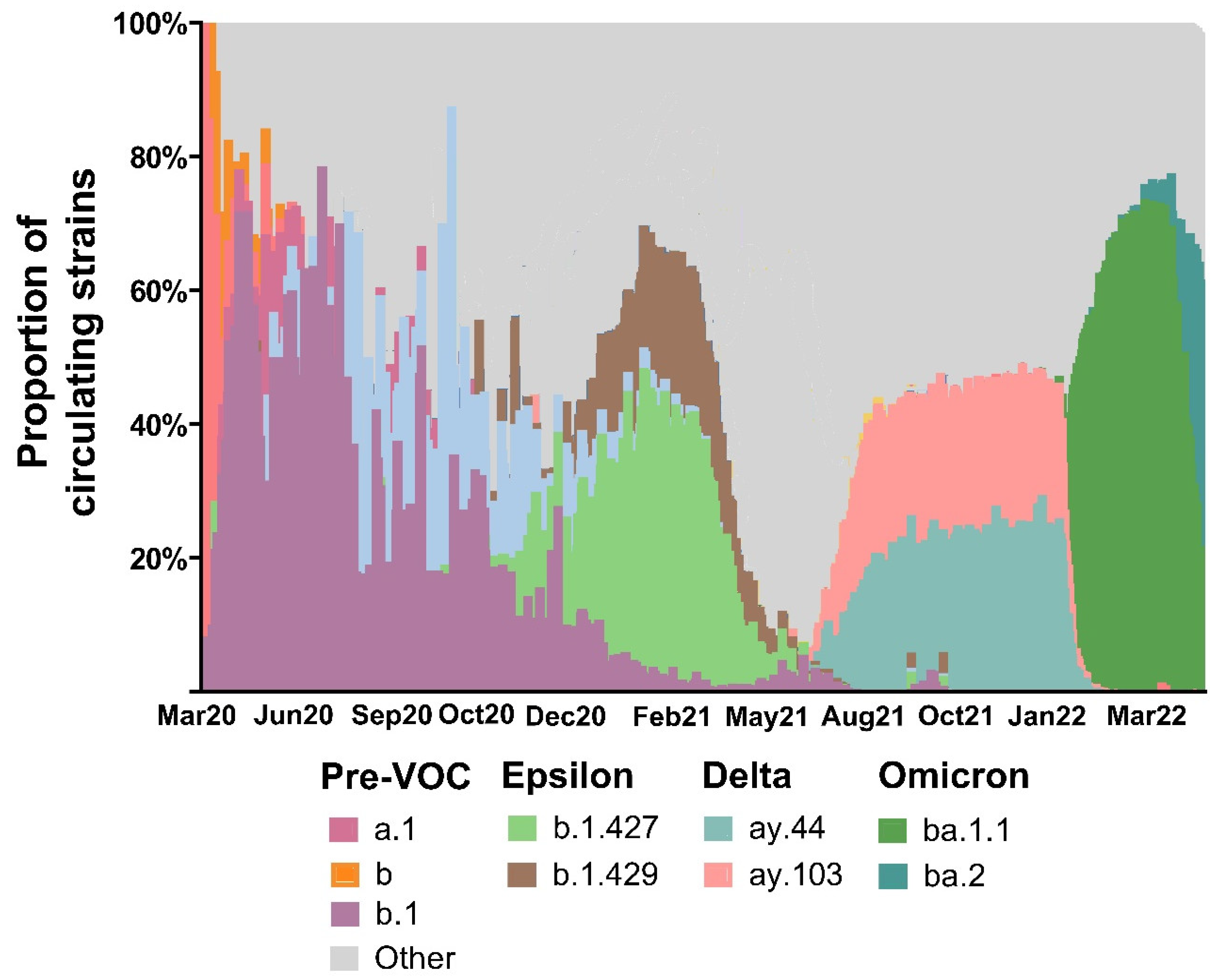
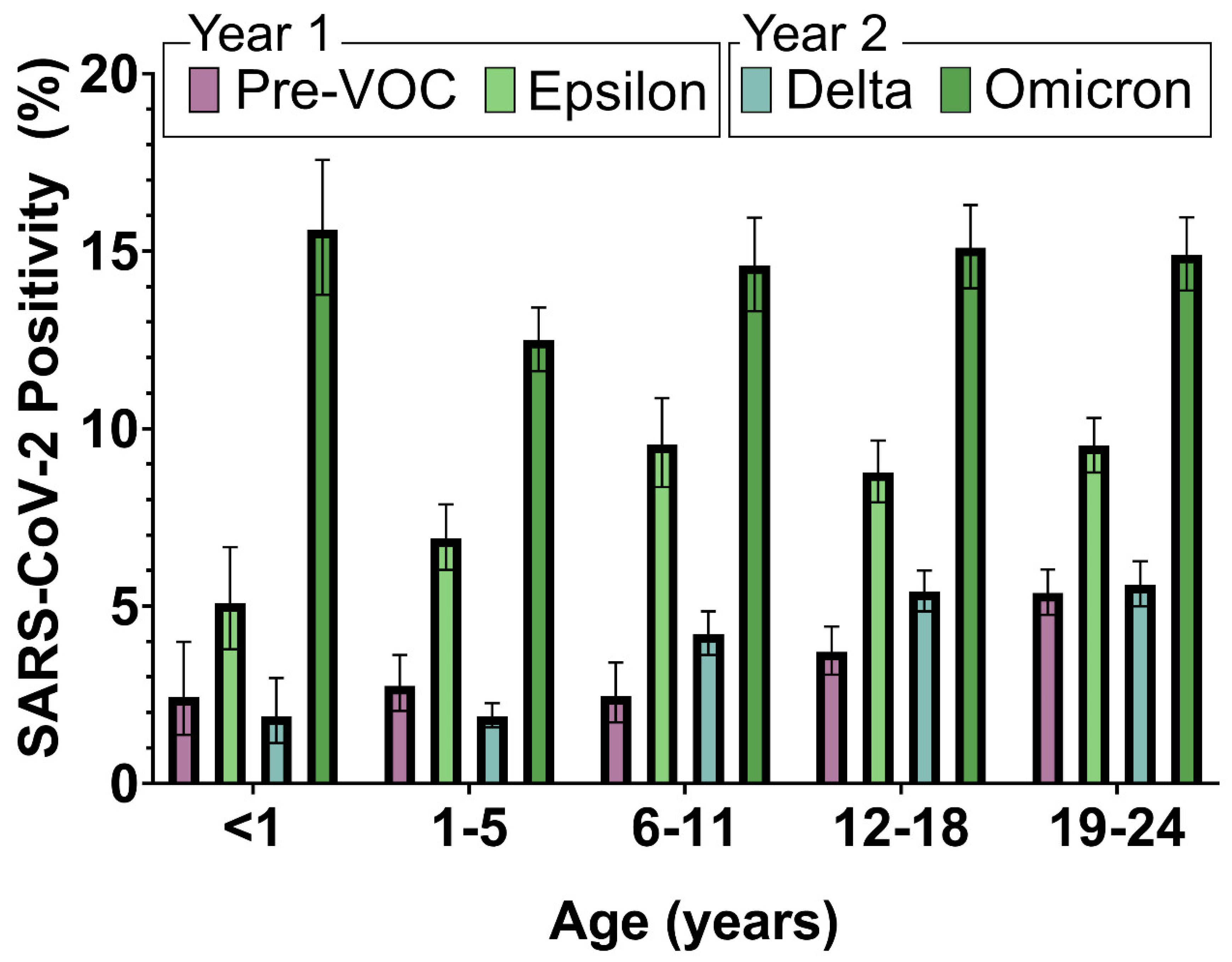
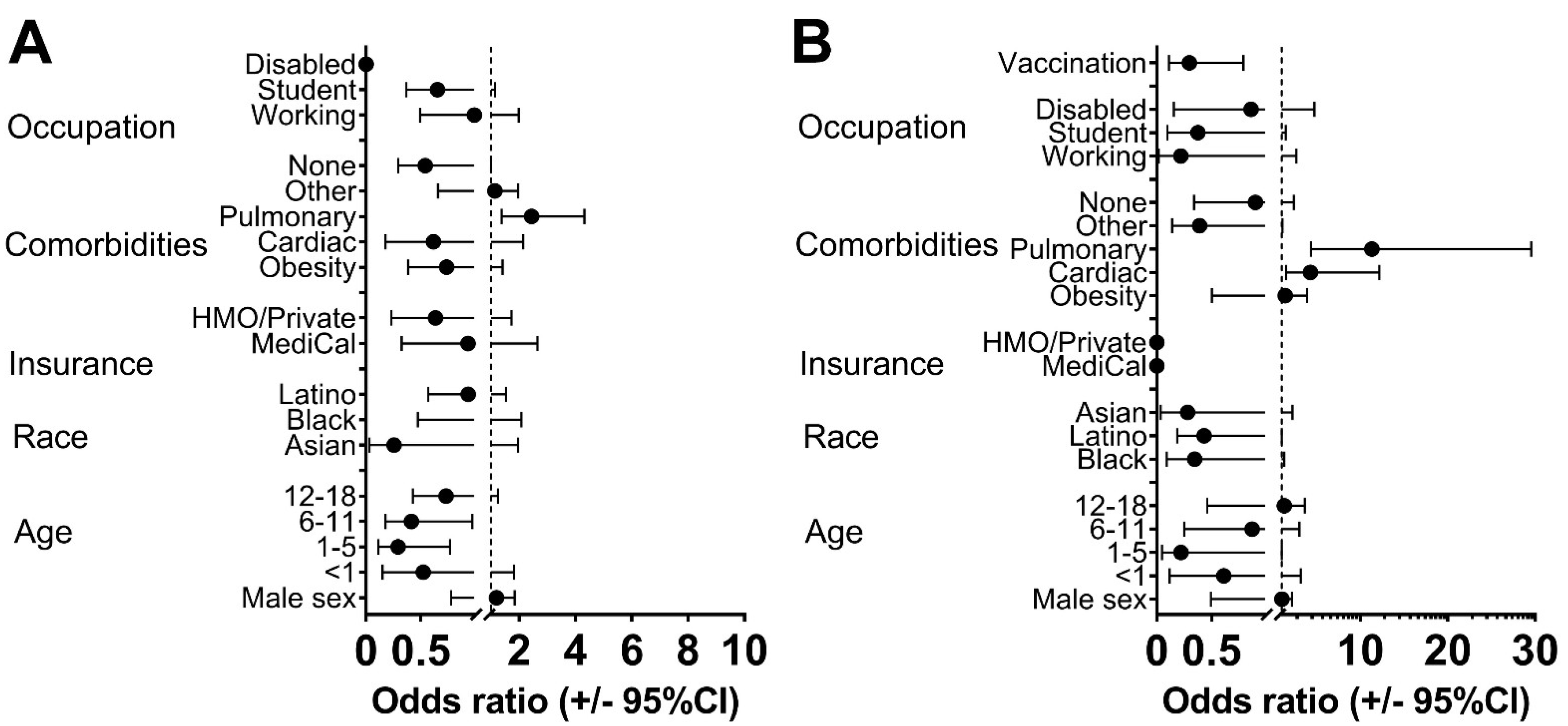
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- CDC COVID Data Tracker. Demographic Trends of COVID-19 Cases and Deaths in the US Reported to the CDC. Available online: www.cdc.gov/covid-data-tracker/index.html#demographics (accessed on 13 March 2023).
- Clarke, K.E.N.; Jones, J.M.; Deng, Y.; Nycz, E.; Lee, A.; Iachan, R.; Gundlapalli, A.V.; Hall, A.J.; MacNeil, A. Seroprevalence of Infection-Induced SARS-CoV-2 Antibodies—United States, September 2021–February 2022. Morb. Mortal. Wkly. Rep. 2022, 71, 606–608. [Google Scholar] [CrossRef] [PubMed]
- Couture, A.; Lyons, B.C.; Mehrotra, M.L.; Sosa, L.; Ezike, N.; Ahmed, F.S.; Brown, C.M.; Yendell, S.; Azzam, I.A.; Katić, B.J.; et al. Severe Acute Respiratory Syndrome Coronavirus 2 Seroprevalence and Reported Coronavirus Disease 2019 Cases in US Children, August 2020–May 2021. Open Forum Infect. Dis. 2022, 9, ofac044. [Google Scholar] [CrossRef] [PubMed]
- Hurst, J.H.; Heston, S.M.; Chambers, H.N.; Cunningham, H.M.; Price, M.J.; Suarez, L.; Crew, C.G.; Bose, S.; Aquino, J.N.; Carr, S.T.; et al. SARS-CoV-2 infections among children in the biospecimens from respiratory virus-exposed kids (BRAVE kids) study. medRxiv 2020. [Google Scholar] [CrossRef]
- Ochoa, V.; Díaz, F.E.; Ramirez, E.; Fentini, M.C.; Carobene, M.; Geffner, J.; Arruvito, L.; Remes Lenicov, F. Infants Younger than 6 Months Infected with SARS-CoV-2 Show the Highest Respiratory Viral Loads. J. Infect. Dis. 2022, 225, 392–395. [Google Scholar] [CrossRef] [PubMed]
- Lopez, A.S.; Hill, M.; Antezano, J.; Vilven, D.; Rutner, T.; Bogdanow, L.; Claflin, C.; Kracalik, I.T.; Fields, V.L.; Dunn, A.; et al. Transmission Dynamics of COVID-19 Outbreaks Associated with Child Care Facilities—Salt Lake City, Utah, April–July 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 1319–1323. [Google Scholar] [CrossRef]
- Qiu, H.; Wu, J.; Hong, L.; Luo, Y.; Song, Q.; Chen, D. Clinical and epidemiological features of 36 children with coronavirus disease 2019 (COVID-19) in Zhejiang, China: An observational cohort study. Lancet Infect. Dis. 2020, 20, 689–696. [Google Scholar] [CrossRef] [PubMed]
- Huff, H.V.; Singh, A. Asymptomatic Transmission During the Coronavirus Disease 2019 Pandemic and Implications for Public Health Strategies. Clin. Infect. Dis. 2020, 71, 2752–2756. [Google Scholar] [CrossRef] [PubMed]
- Karthik Gangavarapu, A.A.L.; Mullen, J.; Alkuzweny, M.; Hufbauer, E.; Tsueng, G.; Haag, E.; Zeller, M.; Christine, M.; Aceves, K.Z.; Cano, M.; et al. Outbreak Info Genomic Reports: Scalable and Dynamic Surveillance of SARS-CoV-2 Variants and Mutations. Available online: https://www.nature.com/articles/s41592-023-01769-3 (accessed on 23 February 2023).
- Marks, K.J.; Whitaker, M.; Anglin, O.; Milucky, J.; Patel, K.; Pham, H.; Chai, S.J.; Kirley, P.D.; Armistead, I.; McLafferty, S.; et al. Hospitalizations of Children and Adolescents with Laboratory-Confirmed COVID-19-COVID-NET, 14 States, July 2021–January 2022. Morb. Mortal. Wkly. Rep. 2022, 71, 271–278. [Google Scholar] [CrossRef]
- Shi, D.S.; Whitaker, M.; Marks, K.J.; Anglin, O.; Milucky, J.; Patel, K.; Pham, H.; Chai, S.J.; Kawasaki, B.; Meek, J.; et al. Hospitalizations of Children Aged 5–11 Years with Laboratory-Confirmed COVID-19—COVID-NET, 14 States, March 2020–February 2022. Morb. Mortal. Wkly. Rep. 2022, 71, 574–581. [Google Scholar] [CrossRef]
- Smith, C.; Odd, D.; Harwood, R.; Ward, J.; Linney, M.; Clark, M.; Hargreaves, D.; Ladhani, S.N.; Draper, E.; Davis, P.J.; et al. Deaths in children and young people in England after SARS-CoV-2 infection during the first pandemic year. Nat. Med. 2022, 28, 185–192. [Google Scholar] [CrossRef]
- Saleh, T.; Kerin, T.; Fuller, T.; Paiola, S.; Cambou, M.C.; Motwani, Y.; Newhouse, C.N.; Yang, S.; Kamau, E.; Garner, O.B.; et al. Clinical and epidemiological characteristics of SARS-CoV-2 Infection in Los Angeles County youth during the first year of the pandemic. Int. J. Infect. Dis. 2022, 122, 514–520. [Google Scholar] [CrossRef] [PubMed]
- Newhouse, C.N.; Saleh, T.; Fuller, T.; Kerin, T.; Cambou, M.C.; Swayze, E.J.; Le, C.; Seo, W.; Trejo, M.; Garner, O.B.; et al. Predictors of SARS-CoV-2 Infection in Youth at a Large, Urban Healthcare Center in California, March–September 2020. Front. Pediatr. 2021, 9, 1274. [Google Scholar] [CrossRef] [PubMed]
- NIH. Clinical Spectrum of SARS-CoV-2 Infection. COVID-19 Treatment Guidelines. Available online: https://www.covid19treatmentguidelines.nih.gov/ (accessed on 20 February 2023).
- Centers for Disease Control and Prevention. Centers for Disease Control and Prevention, Partner Updates: Case Definition for MISC. Available online: https://www.cdc.gov/mis-c/hcp/ (accessed on 20 February 2023).
- Melgar, M.; Lee, E.H.; Miller, A.D.; Lim, S.; Brown, C.M.; Yousaf, A.R.; Zambrano, L.D.; Belay, E.D.; Godfred-Cato, S.; Abrams, J.Y.; et al. Council of State and Territorial Epidemiologists/CDC Surveillance Case Definition for Multisystem Inflammatory Syndrome in Children Associated with SARS-CoV-2 Infection-United States. Recomm. Rep. 2022, 71, 1–14. [Google Scholar] [CrossRef] [PubMed]
- COVID19 Dashboard. Available online: http://dashboard.publichealth.lacounty.gov/covid19_surveillance_dashboard/ (accessed on 20 December 2022).
- United States Census Bureau: California. 2020. Available online: https://www.census.gov/library/stories/state-by-state/california-population-change-between-census-decade.html (accessed on 20 February 2023).
- Madewell, Z.J.; Yang, Y.; Longini, I.M., Jr.; Halloran, M.E.; Dean, N.E. Factors Associated with Household Transmission of SARS-CoV-2: An Updated Systematic Review and Meta-analysis. JAMA Netw. Open 2021, 4, e2122240. [Google Scholar] [CrossRef] [PubMed]
- Avanzato, V.A.; Matson, M.J.; Seifert, S.N.; Pryce, R.; Williamson, B.N.; Anzick, S.L.; Barbian, K.; Judson, S.D.; Fischer, E.R.; Martens, C.; et al. Case Study: Prolonged Infectious SARS-CoV-2 Shedding from an Asymptomatic Immunocompromised Individual with Cancer. Cell 2020, 183, 1901–1912.e1909. [Google Scholar] [CrossRef]
- Khatamzas, E.; Antwerpen, M.H.; Rehn, A.; Graf, A.; Hellmuth, J.C.; Hollaus, A.; Mohr, A.W.; Gaitzsch, E.; Weiglein, T.; Georgi, E.; et al. Accumulation of mutations in antibody and CD8 T cell epitopes in a B cell depleted lymphoma patient with chronic SARS-CoV-2 infection. Nat. Commun. 2022, 13, 5586. [Google Scholar] [CrossRef]
- Marks, K.J.; Whitaker, M.; Agathis, N.T.; Anglin, O.; Milucky, J.; Patel, K.; Pham, H.; Kirley, P.D.; Kawasaki, B.; Meek, J.; et al. Hospitalization of Infants and Children Aged 0–4 Years with Laboratory-Confirmed COVID-19—COVID-NET, 14 States, March 2020–February 2022. Morb. Mortal. Wkly. Rep. 2022, 71, 429–436. [Google Scholar] [CrossRef]
- Madewell, Z.J.; Yang, Y.; Longini, I.M., Jr.; Halloran, M.E.; Dean, N.E. Household Secondary Attack Rates of SARS-CoV-2 by Variant and Vaccination Status: An Updated Systematic Review and Meta-analysis. JAMA Netw. Open 2022, 5, e229317. [Google Scholar] [CrossRef] [PubMed]
- Flaxman, S.; Whittaker, C.; Semenova, E.; Rashid, T.; Parks, R.M.; Blenkinsop, A.; Unwin, H.J.T.; Mishra, S.; Bhatt, S.; Gurdasani, D.; et al. Assessment of COVID-19 as the Underlying Cause of Death Among Children and Young People Aged 0 to 19 Years in the US. JAMA Netw. Open 2023, 6, e2253590. [Google Scholar] [CrossRef]
- Choudhary, R.; Webber, B.J.; Womack, L.S.; Dupont, H.K.; Chiu, S.K.; Wanga, V.; Gerdes, M.E.; Hsu, S.; Shi, D.S.; Dulski, T.M.; et al. Factors Associated with Severe Illness in Patients Aged <21 Years Hospitalized for COVID-19. Hosp. Pediatr. 2022, 12, 760–783. [Google Scholar]
- Forrest, C.B.; Burrows, E.K.; Mejias, A.; Razzaghi, H.; Christakis, D.; Jhaveri, R.; Lee, G.M.; Pajor, N.M.; Rao, S.; Thacker, D.; et al. Severity of Acute COVID-19 in Children <18 Years Old March 2020 to December 2021. Pediatrics 2022, 149, e2021055765. [Google Scholar] [PubMed]
- Karron, R.A.; Hetrich, M.K.; Na, Y.B.; Knoll, M.D.; Schappell, E.; Meece, J.; Hanson, E.; Tong, S.; Lee, J.S.; Veguilla, V.; et al. Assessment of Clinical and Virological Characteristics of SARS-CoV-2 Infection Among Children Aged 0 to 4 Years and Their Household Members. JAMA Netw. Open 2022, 5, e2227348. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Choe, Y.J.; Lee, J.; Park, Y.J.; Park, O.; Han, M.S.; Kim, J.H.; Choi, E.H. Role of children in household transmission of COVID-19. Arch. Dis. Child. 2021, 106, 709–711. [Google Scholar] [CrossRef] [PubMed]
- Sumner, M.W.; Xie, J.; Zemek, R.; Winston, K.; Freire, G.; Burstein, B.; Kam, A.; Emsley, J.; Gravel, J.; Porter, R.; et al. Comparison of Symptoms Associated with SARS-CoV-2 Variants Among Children in Canada. JAMA Netw. Open 2023, 6, e232328. [Google Scholar] [CrossRef]
- Steponavičienė, A.; Burokienė, S.; Ivaškevičienė, I.; Stacevičienė, I.; Vaičiūnienė, D.; Jankauskienė, A. Influenza and Respiratory Syncytial Virus Infections in Pediatric Patients during the COVID-19 Pandemic: A Single-Center Experience. Children 2023, 10, 126. [Google Scholar] [CrossRef]
- Fedorczak, A.; Zielińska, N.; Nosek-Wasilewska, P.; Mikołajczyk, K.; Lisiak, J.; Zeman, K.; Tkaczyk, M. Comparison of COVID-19 and RSV Infection Courses in Infants and Children under 36 Months Hospitalized in Paediatric Department in Fall and Winter Season 2021/2022. J. Clin. Med. 2022, 11, 7088. [Google Scholar] [CrossRef]
- Pinky, L.; Dobrovolny, H.M. Epidemiological Consequences of Viral Interference: A Mathematical Modeling Study of Two Interacting Viruses. Front. Microbiol. 2022, 13, 830423. [Google Scholar] [CrossRef]
- Czerkies, M.; Kochańczyk, M.; Korwek, Z.; Prus, W.; Lipniacki, T. Respiratory Syncytial Virus Protects Bystander Cells against Influenza A Virus Infection by Triggering Secretion of Type I and Type III Interferons. J. Virol. 2022, 96, e01341-22. [Google Scholar] [CrossRef]
- Ptak, K.; Szymońska, I.; Olchawa-Czech, A.; Kukla, K.; Cisowska, M.; Kwinta, P. Comparison of the course of multisystem inflammatory syndrome in children during different pandemic waves. Eur. J. Pediatr. 2023, 182, 1647–1656. [Google Scholar] [CrossRef]
- Maiese, A.; Frati, P.; Del Duca, F.; Santoro, P.; Manetti, A.C.; La Russa, R.; Di Paolo, M.; Turillazzi, E.; Fineschi, V. Myocardial Pathology in COVID-19-Associated Cardiac Injury: A Systematic Review. Diagnostics 2021, 11, 1647. [Google Scholar] [CrossRef]
- Maiese, A.; Manetti, A.C.; Bosetti, C.; Del Duca, F.; La Russa, R.; Frati, P.; Di Paolo, M.; Turillazzi, E.; Fineschi, V. SARS-CoV-2 and the brain: A review of the current knowledge on neuropathology in COVID-19. Brain Pathol. 2021, 31, e13013. [Google Scholar] [CrossRef] [PubMed]
- Maiese, A.; Manetti, A.C.; La Russa, R.; Di Paolo, M.; Turillazzi, E.; Frati, P.; Fineschi, V. Autopsy findings in COVID-19-related deaths: A literature review. Forensic Sci. Med. Pathol. 2021, 17, 279–296. [Google Scholar] [CrossRef] [PubMed]
- Ye, Q.; Shao, W.X.; Meng, H.Y. Performance and application evaluation of SARS-CoV-2 antigen assay. J. Med. Virol. 2022, 94, 3548–3553. [Google Scholar] [CrossRef] [PubMed]
- Peeling, R.W.; Heymann, D.L.; Teo, Y.Y.; Garcia, P.J. Diagnostics for COVID-19: Moving from pandemic response to control. Lancet 2022, 399, 757–768. [Google Scholar] [CrossRef]

| 13 March 2020–31 March 2021 N = 1622 | 1 April 2021–31 March 2022 N = 3641 | p | |||
|---|---|---|---|---|---|
| Sex | N | % | N | % | 0.009 |
| Female | 795 | 49% | 1927 | 52.9% | |
| Male | 827 | 51% | 1714 | 47.1% | |
| Age group at testing | <0.001 | ||||
| <1 year | 59 | 3.6% | 248 | 6.8% | |
| 1–5 years | 257 | 15.8% | 886 | 24.3% | |
| 6–11 years | 209 | 12.9% | 672 | 18.5% | |
| 12–18 years | 468 | 28.8% | 959 | 26.3% | |
| 19–24 years | 630 | 38.8% | 876 | 24.1% | |
| Mean Age (SD) | 14.3 | 7.5 | 11.4 | 7.7 | <0.001 |
| Race/ethnicity | <0.001 | ||||
| Asian | 54 | 3.4% | 337 | 9.3% | |
| Black/African American | 172 | 10.8% | 409 | 11.3% | |
| Hispanic/Latino | 839 | 52.6% | 1477 | 40.7% | |
| White | 475 | 29.8% | 1374 | 37.8% | |
| Other | 55 | 3.4% | 35 | 1% | |
| Missing | 27 | 9 | |||
| Type of Insurance | <0.001 | ||||
| Uninsured | 55 | 3.4% | 215 | 5.9% | |
| Medical/Safety Net | 384 | 23.7% | 510 | 14% | |
| HMO/Private | 1184 | 73% | 2916 | 80.1% | |
| Comorbidities | |||||
| Obesity | 196 | 12.1% | 344 | 9.4% | 0.004 |
| Pulmonary | 173 | 10.7% | 415 | 11.4% | 0.432 |
| Cardiac | 56 | 3.5% | 70 | 1.9% | 0.01 |
| Other | 441 | 27.2% | 245 | 6.7% | <0.001 |
| None | 1088 | 67% | 2792 | 76.7% | <0.001 |
| Occupation (Patient) | |||||
| Working | 172 | 10.6% | 149 | 4.1% | <0.001 |
| Student | 1216 | 74.9% | 3216 | 88.3% | <0.001 |
| Disabled | 28 | 1.7% | 44 | 1.2% | 0.136 |
| Other | 103 | 6.3% | 240 | 6.6% | 0.739 |
| Disease Severity | <0.001 | ||||
| Asymptomatic | 394 | 24% | 706 | 19% | |
| Mild/moderate | 1127 | 70% | 2900 | 80% | |
| Severe or Critical | 98 | 6% | 35 | 1% | |
| Death | 3 | 0.18% | 4 | 0.11% | 0.45 |
| Severe/Critical | Vaccination Rate | ||||||
|---|---|---|---|---|---|---|---|
| Year 1 | Year 2 | p | Year 1 | Year 2 | p | ||
| Age (years) | <1, N (%) | 3/59 (5.1%) | 4/248 (1.6%) | 0.12 | 0/59 (0%) | 0/248 (0%) | 0.99 |
| 1–5, N (%) | 5/257 (1.9%) | 5/886 (0.6%) | <0.001 | 0/257 (0%) | 83/886 (9.4%) | <0.001 | |
| 6–11, N (%) | 7/209 (3.3%) | 7/672 (1.1%) | 0.03 | 0/209 (0%) | 452/672 (67.3%) | <0.001 | |
| 12–18, N (%) | 27/468 (5.8%) | 10/959 (1.1%) | <0.001 | 21/468 (4.5%) | 813/959 (84.8%) | <0.001 | |
| 19–24, N (%) | 56/630 (8.9%) | 9/876 (1%) | <0.001 | 15/630 (2.4%) | 827/876 (94.4%) | <0.001 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saleh, T.; Fuller, T.; Cambou, M.C.; Segura, E.R.; Kamau, E.; Yang, S.; Garner, O.B.; Nielsen-Saines, K. Epidemiology and SARS-CoV-2 Infection Patterns among Youth Followed at a Large Los Angeles Health Network during 2020–2022: Clinical Presentation, Prevalent Strains, and Correlates of Disease Severity. Vaccines 2023, 11, 1024. https://doi.org/10.3390/vaccines11061024
Saleh T, Fuller T, Cambou MC, Segura ER, Kamau E, Yang S, Garner OB, Nielsen-Saines K. Epidemiology and SARS-CoV-2 Infection Patterns among Youth Followed at a Large Los Angeles Health Network during 2020–2022: Clinical Presentation, Prevalent Strains, and Correlates of Disease Severity. Vaccines. 2023; 11(6):1024. https://doi.org/10.3390/vaccines11061024
Chicago/Turabian StyleSaleh, Tawny, Trevon Fuller, Mary C. Cambou, Eddy R. Segura, Edwin Kamau, Shangxin Yang, Omai B. Garner, and Karin Nielsen-Saines. 2023. "Epidemiology and SARS-CoV-2 Infection Patterns among Youth Followed at a Large Los Angeles Health Network during 2020–2022: Clinical Presentation, Prevalent Strains, and Correlates of Disease Severity" Vaccines 11, no. 6: 1024. https://doi.org/10.3390/vaccines11061024
APA StyleSaleh, T., Fuller, T., Cambou, M. C., Segura, E. R., Kamau, E., Yang, S., Garner, O. B., & Nielsen-Saines, K. (2023). Epidemiology and SARS-CoV-2 Infection Patterns among Youth Followed at a Large Los Angeles Health Network during 2020–2022: Clinical Presentation, Prevalent Strains, and Correlates of Disease Severity. Vaccines, 11(6), 1024. https://doi.org/10.3390/vaccines11061024





