COVID-19 Vaccine Coverage in India: A District-Level Analysis
Abstract
1. Introduction
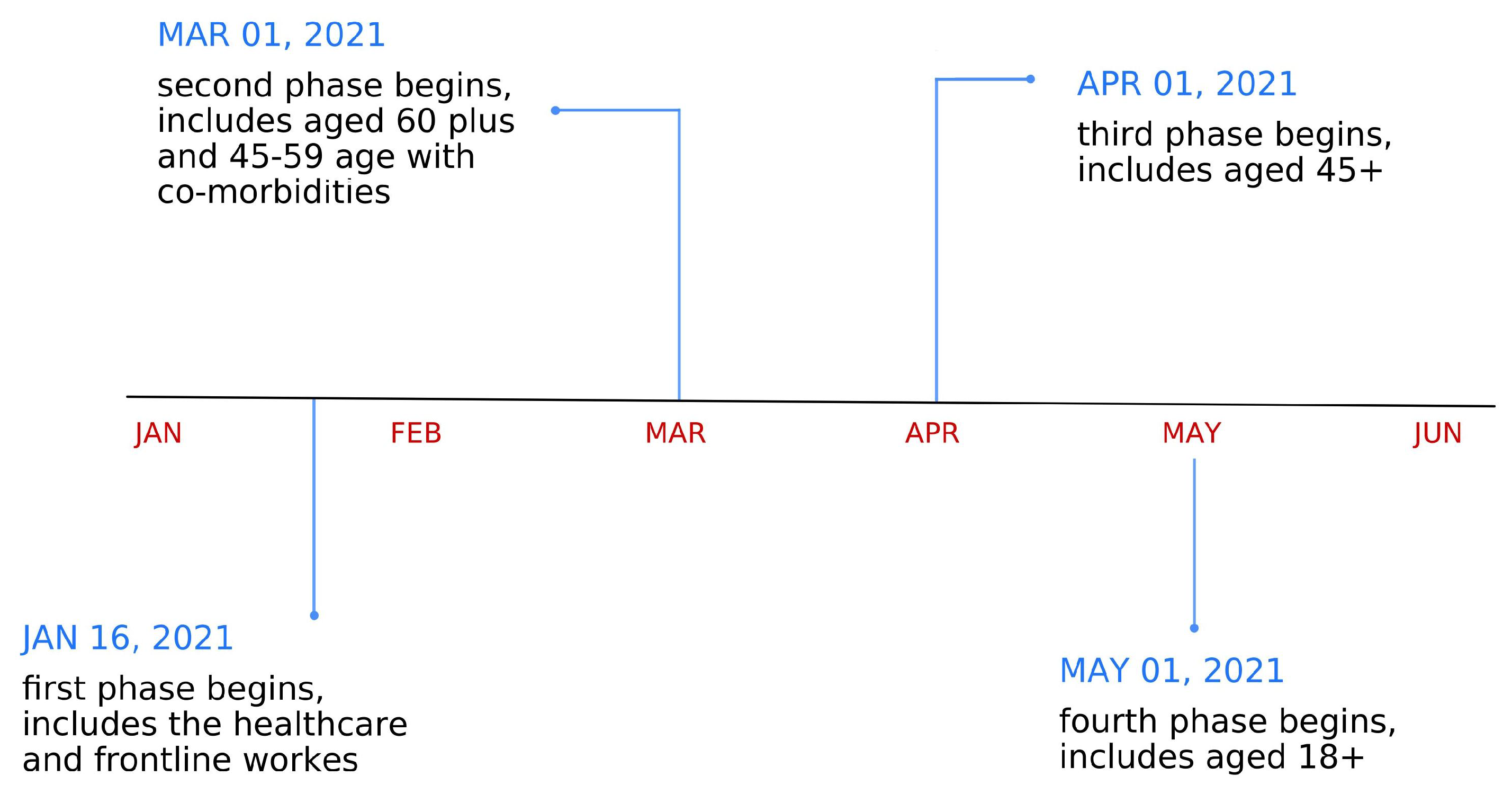
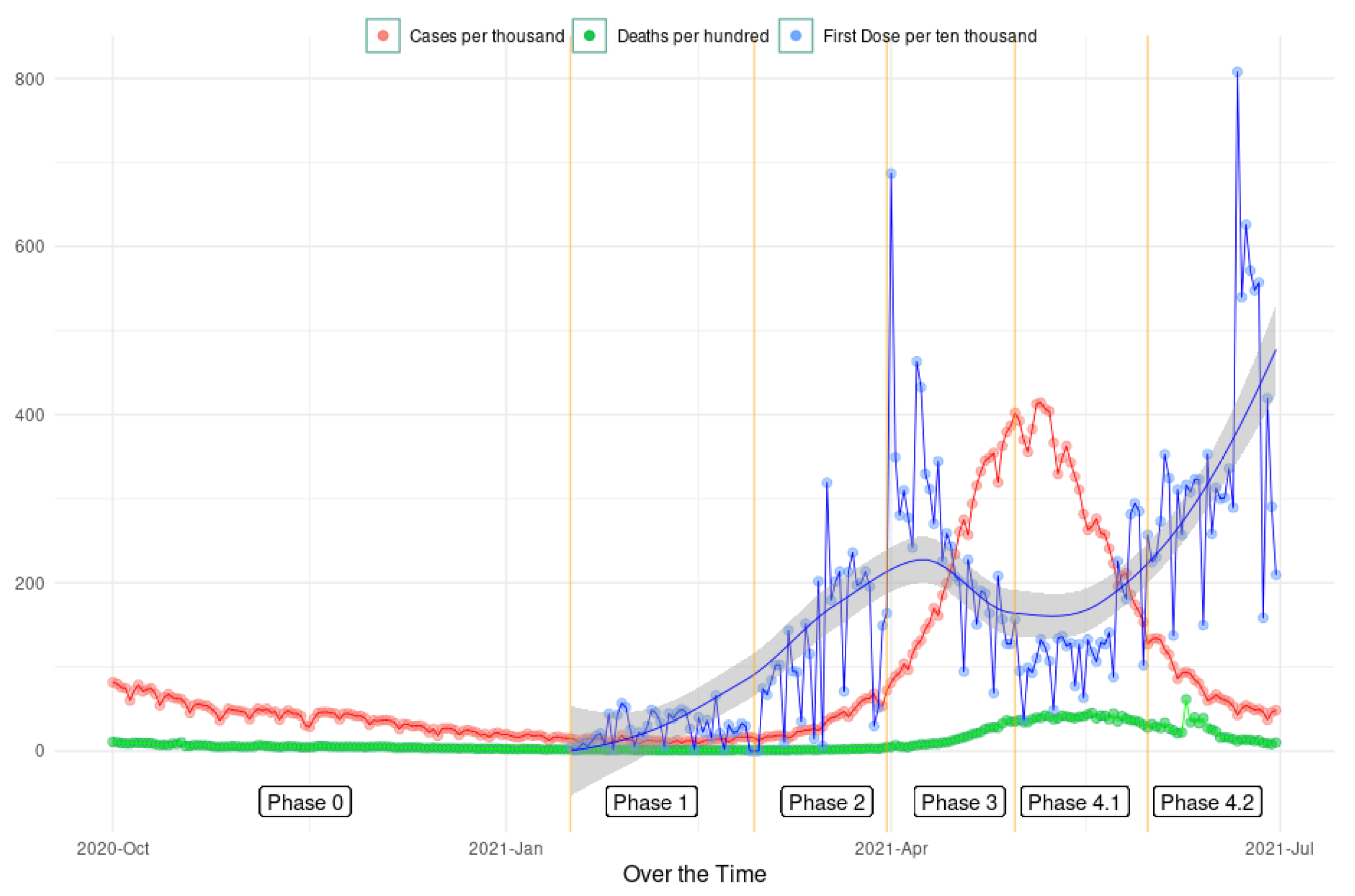
2. Background
3. Materials and Methods
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Susskind, D.; Vines, D. The economics of the COVID-19 pandemic: An assessment. Oxf. Rev. Econ. Policy 2020, 36, S1–S13. [Google Scholar] [CrossRef]
- Sturgis, P.; Brunton-Smith, I.; Jackson, J. Trust in science, social consensus and vaccine confidence. Nat. Hum. Behav. 2021, 5, 1528–1534. [Google Scholar] [CrossRef] [PubMed]
- Benziman, Y. “winning” the “battle” and “beating” the COVID-19 “enemy”: Leaders’ use of war frames to define the pandemic. Peace Confl. J. Peace Psychol. 2020, 26, 247. [Google Scholar] [CrossRef]
- Tornero, J.M.P.; Lladó, C.M.; Cervi, L. Pandemic and war: Crisis narrative and leadership. analysis of the presidential speeches at the beginning of the COVID-19 pandemic. Rev. Lat. Comun. Soc. 2021, 79, 1–21. [Google Scholar]
- Krishnatray, P.; Shrivastava, S. Coronavirus pandemic: How national leaders framed their speeches to fellow citizens. Asia Pac. Media Educ. 2021, 31, 195–211. [Google Scholar] [CrossRef]
- Randolph, H.E.; Barreiro, L. Herd immunity: Understanding COVID-19. Immunity 2020, 52, 737–741. [Google Scholar] [CrossRef]
- Fontanet, A.; Cauchemez, S. COVID-19 herd immunity: Where are we? Nat. Rev. Immunol. 2020, 20, 583–584. [Google Scholar] [CrossRef]
- Sharma, O.; Sultan, A.A.; Ding, H.; Triggle, C.R. A review of the progress and challenges of developing a vaccine for COVID-19. Front. Immunol. 2020, 11, 585354. [Google Scholar] [CrossRef]
- Wouters, O.; Shadlen, K.; Salcher-Konrad, M.; Pollard, A.; Larson, H.; Teerawattananon, Y.; Jit, M. Health policy challenges in ensuring global access to COVID-19 vaccines: Production, affordability, allocation, and deployment. Health Policy 2021, 397, 1023–1034. [Google Scholar]
- Black, S.; Rappuoli, R. A crisis of public confidence in vaccines. Sci. Transl. Med. 2010, 2, 61mr1. [Google Scholar] [CrossRef]
- Larson, H.J.; Cooper, L.Z.; Eskola, J.; Katz, S.L.; Ratzan, S. Addressing the vaccine confidence gap. Lancet 2011, 378, 526–535. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, E.; Smith, J.; Appleton, M. Risk perception, risk management and safety assessment: What can governments do to increase public confidence in their vaccine system? Biologicals 2012, 40, 384–388. [Google Scholar] [CrossRef] [PubMed]
- Larson, H.J.; Jarrett, C.; Schulz, W.S.; Chaudhuri, M.; Yuqing, Z.; Dube, E.; Schuster, M.; MacDonald, N.E.; Wilson, R. Measuring vaccine hesitancy: The development of a survey tool. Vaccine 2015, 33, 4165–4175. [Google Scholar] [CrossRef] [PubMed]
- Solís Arce, J.S.; Warren, S.S.; Meriggi, N.F.; Scacco, A.; McMurry, N.; Voors, M.; Syunyaev, G.; Malik, A.A.; Aboutajdine, S.; Adeojo, O.; et al. COVID-19 vaccine acceptance and hesitancy in low-and middle-income countries. Nat. Med. 2021, 27, 1385–1394. [Google Scholar] [CrossRef] [PubMed]
- Reza, H.M.; Agarwal, V.; Sultana, F.; Bari, R.; Mobarak, A.M. Why are vaccination rates lower in low and middle income countries, and what can we do about it? BMJ 2022, 378, e069506. [Google Scholar] [CrossRef] [PubMed]
- Wolf, C.; Matthews, A.L.; Alas, H. Wealthy Countries Are Outpacing Poor Nations in COVID-19 Vaccination Rates. 2022. Available online: https://www.usnews.com/news/best-countries/articles/covid-19-vaccination-rates-by-country (accessed on 13 December 2022).
- Kavanagh, M.M.; Gostin, L.O.; Sunder, M. Sharing technology and vaccine doses to address global vaccine inequity and end the COVID-19 pandemic. JAMA 2021, 326, 219–220. [Google Scholar] [CrossRef]
- Gonsalves, G.; Omer, S. Scale up production of COVID-19 vaccines in lmics. Science 2022, 375, 1107. [Google Scholar]
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2020, 27, 225–228. [Google Scholar] [CrossRef]
- Kharel, A.; Warren, S. Is vaccine hesitancy a problem? Science 2022, 375, 1107–1108. [Google Scholar]
- Lazarus, J.; Wyka, K.; White, T.; Picchio, C.; Rabin, K.; Ratzan, S.; Leigh, J.P.; Hu, J.; El-Mohandes, A. Revisiting COVID-19 vaccine hesitancy around the world using data from 23 countries in 2021. Nat. Commun. 2022, 13, 2022. [Google Scholar] [CrossRef]
- Lazarus, J.V.; Wyka, K.; White, T.M.; Picchio, C.A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Ratzan, S.C.; Kamarulzaman, A.; El-Mohandes, A. A survey of COVID-19 vaccine acceptance across 23 countries in 2022. Nat. Med. 2023, 29, 366–375. [Google Scholar] [CrossRef] [PubMed]
- Katz, I.T.; Weintraub, R.; Bekker, L.-G.; Brandt, A.M. From vaccine nationalism to vaccine equity—Finding a path forward. N. Engl. J. Med. 2021, 384, 1281–1283. [Google Scholar] [CrossRef]
- Gupta, S.S.; Nair, G.B.; Arora, N.K.; Ganguly, N.K. Vaccine development and deployment: Opportunities and challenges in india. Vaccine 2013, 31, B43–B53. [Google Scholar] [CrossRef] [PubMed]
- Choi, E.M. COVID-19 vaccines for low- and middle-income countries. Trans. R. Soc. Trop. Med. AndHygiene 2021, 115, 447–456. [Google Scholar] [CrossRef]
- Padma, T.V. India’s covid-vaccine woes—By the numbers. Nature 2021, 592, 500–501. [Google Scholar] [CrossRef]
- Sanghi, N. How the Modi Government Overestimated India’s Capacity to Make Covid Vaccines. 2021. Available online: https://thewire.in/health/how-the-modi-government-overestimated-indias-capacity-to-make-covid-vaccines (accessed on 1 December 2022).
- Kumar, S. India in the Global Vaccine Market Prior to and during COVID-19; ISID: New Delhi, India, 2022. [Google Scholar]
- Hindu, T. India Supplies Nearly 60% of Vaccines Used Worldwide: Nirmala Sitharaman. 2022. Available online: https://www.businesstoday.in/latest/economy/story/india-supplies-nearly-60-of-vaccines-used-worldwide-finance-minister-344907-2022-08-17 (accessed on 1 December 2022).
- Bagcchi, S. The world’s largest COVID-19 vaccination campaign. Lancet Infect. Dis. 2021, 21, 323. [Google Scholar] [CrossRef]
- Choudhary, O.P.; Choudhary, P.; Singh, I. India’s COVID-19 vaccination drive: Key challenges and resolutions. Lancet Infect. Dis. 2021, 21, 1483–1484. [Google Scholar] [CrossRef]
- Prasad, L. India vs. Rest of World: What the COVID Vaccine Numbers Say. 2021. Available online: http://indianexpress.com/article/india/india-vs-rest-of-world-what-the-covid-vaccine-numbers-say-7583334/ (accessed on 1 December 2022).
- Jha, A.K. India’s Covid Vaccination Was One of Most Impressive in World: Dr ashish k jha. 2022. Available online: http://www.hindustantimes.com/india-news/indias-covid-vaccination-was-one-of-most-impressive-in-world-dr-ashish-k-jha-101667911490579.html (accessed on 1 December 2022).
- India’s Vaccination Drive Outpaces Most Countries as It Breaches 100 Crore Inoculation Mark. The Economic Times, 21 October 2021.
- Tamrakar, V.; Srivastava, A.; Saikia, N.; Parmar, M.C.; Shukla, S.K.; Shabnam, S.; Boro, B.; Saha, A.; Debbarma, B. District level correlates of COVID-19 pandemic in india during march-october 2020. PLoS ONE 2021, 16, e0257533. [Google Scholar] [CrossRef]
- Ghosh, D.D.; Sarkar, A.; Chouhan, D.P. COVID-19 second wave: District level study of concentration and fatality in india. Environ. Chall. 2021, 5, 100221. [Google Scholar] [CrossRef]
- Kodama, C.; Kuniyoshi, G.; Abubakar, A. Lessons learned during COVID-19: Building critical care/icu capacity for resource limited countries with complex emergencies in the world health organization eastern mediterranean region. J. Glob. Health 2021, 11, 03088. [Google Scholar] [CrossRef]
- Dhalaria, P.; Arora, H.; Singh, A.K.; Mathur, M.; Kumar S, A. COVID-19 vaccine hesitancy and vaccination coverage in india: An exploratory analysis. Vaccines 2022, 10, 739. [Google Scholar] [CrossRef] [PubMed]
- Vasudevan, V.; Gnanasekaran, A.; Bansal, B.; Lahariya, C.; Parameswaran, G.G.; Zou, J. Assessment of COVID-19 data reporting in 100+ websites and apps in india. PLoS Glob. Public Health 2022, 2, e0000329. [Google Scholar] [CrossRef] [PubMed]
- Mittal, R.M.; Kurian, O.C. Bringing the COVID-19 Vaccine to Every Hamlet: The Story of Raigarh. 2022. Available online: https://policycommons.net/artifacts/2480831/bringing-the-covid-19-vaccine-to-every-hamlet/3503015/ (accessed on 1 December 2022).
- Perappadan, B.S. India’s COVID-19 Vaccine Pace Is Inspirational to Lower Income Countries, Says Vaccine Alliance Official. The Hindu, 4 October 2021. [Google Scholar]
- Brimnes, N. Fallacy, sacrilege, betrayal and conspiracy: The cultural construction of opposition to immunisation in india. In The Politics of Vaccination; Manchester University Press: Manchester, UK, 2017; pp. 51–76. [Google Scholar]
- Vashishtha, V.M. Status of immunization and need for intensification of routine immunization in india. Indian Pediatr. 2012, 49, 357–361. [Google Scholar] [CrossRef]
- Cousins, S. India is declared free of maternal and neonatal tetanus. BMJ 2015, 350, h3092. [Google Scholar] [CrossRef] [PubMed]
- Purohit, N.; Chugh, Y.; Bahuguna, P.; Prinja, S. COVID-19 management: The vaccination drive in india. Health Policy Technol. 2022, 11, 100636. [Google Scholar] [CrossRef]
- Asher, S.; Lunt, T.; Matsuura, R.; Novosad, P. Development research at high geographic resolution: An analysis of night lights, firms, and poverty in india using the shrug open data platform. Policy Res. Work. Pap. 2021, 35, 845–871. [Google Scholar]
- Wang, W.; Kim, R.; Subramanian, S.V. Population Estimates for Districts and Parliamentary Constituencies in India, 2020. Harv. Dataverse V1 2021.
- Rural Health Statistics, 2020–21; Government of India, Ministry of Health and Family Welfare Statistics Division: New Delhi, India, 2022.
- NITI Aayog. Aspirational Districts: Unlocking Potentials; NITI Aayog, Government of India: New Delhi, India, 2018.
- Samarasekera, U. India grapples with second wave of COVID-19. Lancet Microbe 2021, 2, e238. [Google Scholar] [CrossRef] [PubMed]
- The Lancet. India’s COVID-19 emergency. Lancet 2021, 397, 1683. [Google Scholar] [CrossRef]
- Aiyar, Y.; Chandru, V.; Chatterjee, M.; Desai, S.; Fernandez, A.; Gupta, A.; Kang, G.; Khanna, T.; Mazumdar-Shaw, K.; Mor, N.; et al. India’s resurgence of COVID-19: Urgent actions needed. Lancet 2021, 397, 2232–2234. [Google Scholar] [CrossRef]
- Kumar, S. Second wave of COVID-19: Emergency situation in india. J. Travel Med. 2021, 28, taab082. [Google Scholar] [CrossRef]
- Chakraborty, C.; Sharma, A.R.; Bhattacharya, M.; Agoramoorthy, G.; Lee, S.-S. The current second wave and COVID-19 vaccination status in india. Brain Behav. Immun. 2021, 96, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Thiagarajan, K. Why is india having a COVID-19 surge? BMJ 2021, 373, n1124. [Google Scholar] [CrossRef] [PubMed]
- Sarkar, A.; Chakrabarti, A.K.; Dutta, S. COVID-19 infection in india: A comparative analysis of the second wave with the first wave. Pathogens 2021, 10, 1222. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, R.M.; Targonski, P.V.; Poland, G.A. A taxonomy of reasoning flaws in the anti-vaccine movement. Vaccine 2007, 25, 3146–3152. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, S. Actor’s Death Fuels Vaccine Hesitancy in Tamil Nadu Amid Covid Surge, Misinformation Adds Fire. The Print, 10 May 2021. [Google Scholar]
- Mustafa, R. Villagers Jump into River in up’s Barabanki to Escape Covid Vaccination. 2021. Available online: https://www.indiatoday.in/coronavirus-outbreak/story/villagers-jump-river-up-barabanki-to-escape-covid-vaccination-1806217-2021-05-24 (accessed on 1 December 2022).
- Singh, M.; Mishra, A.; Singh, R.P.; Singh, R.K. ’Those Who Take the Jab Die’: Rumours mar Covid Vaccination Drive in Rural India. 2021. Available online: https://www.indiatoday.in/coronavirus-outbreak/story/those-who-take-the-jab-die-rumours-mar-covid-vaccination-drive-rural-india-rajasthan-bihar-uttar-pradesh-madhya-1809812-2021-06-02 (accessed on 1 December 2022).
- Nibedita, S.; Sultan, N. COVID-19: Vaccination Rumours Afflict mp Villages, Frontline Workers Face the Brunt. 2021. Available online: https://www.downtoearth.org.in/blog/health/covid-19-vaccination-rumours-afflict-mp-villages-frontline-workers-face-the-brunt-77113 (accessed on 1 December 2022).
- Ali, S.; Hanif, W.; Patel, K.; Khunti, K. Ramadan and COVID-19 vaccine hesitancy—A call for action. Lancet 2021, 397, 1443–1444. [Google Scholar] [CrossRef] [PubMed]
- Mozid, N.-E.; Amin, M.A.; Jhumur, S.S.; Monju, I.H.; Ahmed, S.B.; Sharmin, S.; Sarker, W.; Hawlader, M.D.H. COVID-19 risk of infection and vaccination during ramadan fasting: Knowledge and attitudes of bangladeshi general population. Heliyon 2021, 7, e08174. [Google Scholar] [CrossRef] [PubMed]
- Sahar, N. Muslim Clergy Must Spread the Message Loud—Covid Vaccine Won’t Invalidate Ramzan Fast. 2021. Available online: https://theprint.in/opinion/muslim-clergy-must-spread-the-message-loud-covid-vaccine-wont-invalidate-ramzan-fast/642412/ (accessed on 1 December 2022).
- Diamond-Smith, N.G.; Sharma, P.; Duggal, M.; Gill, N.; Gupta, J.; Kumar, V.; Kaur, J.; Singh, P.; Vosburg, K.B.; El Ayadi, A.M. The supply is there. so why can’t pregnant and breastfeeding women in rural india get the COVID-19 vaccine? PLoS Glob. Public Health 2022, 2, e0001321. [Google Scholar] [CrossRef]
- Kumari, A.; Mahey, R.; Kachhawa, G.; Kumari, R.; Bhatla, N. Knowledge, attitude, perceptions, and concerns of pregnant and lactating women regarding COVID-19 vaccination: A cross-sectional survey of 313 participants from a tertiary care centre of north india. Diabetes Metab. Syndr. Clin. Res. Rev. 2022, 16, 102449. [Google Scholar] [CrossRef] [PubMed]
- Shashidhara, S.; Barnhardt, S.; Mukherjee, S. COVID-19 Vaccination Status and Hesitancy: Survey Evidence from Rural India; Working Paper; Centre for Social and Behaviour Change, Ashoka University: Haryana, India, 2022; p. 11. [Google Scholar]
- Shrivastwa, N.; Gillespie, B.W.; Kolenic, G.E.; Lepkowski, J.M.; Boulton, M.L. Predictors of vaccination in india for children aged 12–36 months. Vaccine 2015, 33 (Suppl. 4), D99–D105. [Google Scholar] [CrossRef]
- Shrivastwa, N.; Wagner, A.; Boulton, M. Analysis of state-specific differences in childhood vaccination coverage in rural india. Vaccines 2019, 7, 24. [Google Scholar] [CrossRef] [PubMed]
- Perroud, J.M.; Soldano, S.; Avanceña, A.L.; Wagner, A. Adult vaccination uptake strategies in low- and middle-income countries: A systematic review. Vaccine 2022, 40, 5313–5321. [Google Scholar] [CrossRef] [PubMed]
| Phase 1 | Obs | Mean | Median | Max | Min | St. Dev |
|---|---|---|---|---|---|---|
| FDV % | 729 | 0.95 | 0.77 | 5.75 | 0.13 | 0.65 |
| IR % | 629 | 0.04 | 0.01 | 1.48 | 0.00 | 0.18 |
| PIR % | 629 | 0.64 | 0.44 | 6.05 | 0.00 | 0.68 |
| PDR % | 629 | 0.01 | 0.00 | 0.11 | 0.00 | 0.01 |
| (PDR/PIR) % | 625 | 1.18 | 1.05 | 4.99 | 0.00 | 0.84 |
| Phase 2 | Obs | Mean | Median | Max | Min | St. Dev |
| FDV % | 729 | 2.97 | 2.48 | 17.12 | 0.21 | 2.05 |
| IR % | 629 | 0.05 | 0.01 | 1.48 | 0.00 | 0.13 |
| PIR % | 629 | 0.674 | 0.450 | 7.007 | 0.000 | 0.75 |
| PDR % | 629 | 0.01 | 0.00 | 0.11 | 0.00 | 0.01 |
| (PDR/PIR) % | 626 | 1.17 | 1.04 | 4.99 | 0.00 | 0.82 |
| Phase 3 | Obs | Mean | Median | Max | Min | St. Dev |
| FDV % | 729 | 6.02 | 5.04 | 23.40 | 0.40 | 3.88 |
| IR % | 629 | 1.11 | 0.72 | 9.66 | 0.00 | 1.22 |
| PIR % | 629 | 0.73 | 0.48 | 7.36 | 0.00 | 0.82 |
| PDR % | 629 | 0.01 | 0.00 | 0.12 | 0.00 | 0.01 |
| (PDR/PIR) % | 626 | 1.11 | 1.03 | 4.27 | 0.00 | 0.73 |
| Phase 4—Month 1 | Obs | Mean | Median | Max | Min | St. Dev |
| FDV % | 729 | 3.35 | 2.62 | 21.01 | 0.20 | 2.62 |
| IR % | 629 | 0.64 | 0.42 | 8.18 | 0.00 | 0.69 |
| PIR % | 629 | 1.84 | 1.18 | 17.02 | 0.00 | 2.01 |
| PDR % | 629 | 0.01 | 0.01 | 0.13 | 0.00 | 0.015 |
| (PDR/PIR) % | 626 | 0.59 | 0.56 | 2.41 | 0.00 | 0.36 |
| Phase 4—Month 2 | Obs | Mean | Median | Max | Min | St. Dev |
| FDV % | 729 | 8.42 | 6.82 | 41.56 | 0.94 | 5.90 |
| IR % | 629 | 2.48 | 1.70 | 20.30 | 0.00 | 2.56 |
| PIR % | 629 | 0.18 | 0.06 | 2.61 | 0.00 | 0.29 |
| PDR % | 629 | 0.02 | 0.01 | 0.16 | 0.00 | 0.02 |
| (PDR/PIR) % | 626 | 0.79 | 0.72 | 3.77 | 0.00 | 0.49 |
| Var | Des | Obs | Mean | Median | Max | Min | St. Dev |
|---|---|---|---|---|---|---|---|
| Rural | % Rural households | 729 | 74.1 | 80.4 | 100.0 | 0.0 | 21.4 |
| Literacy | % Population literate | 729 | 62.1 | 61.8 | 88.7 | 28.8 | 10.5 |
| Muslim | % Population Muslim | 729 | 12.3 | 7.2 | 98.5 | 0.3 | 17.0 |
| SC | % Population SC | 729 | 14.6 | 15.5 | 50.2 | 0.0 | 9.3 |
| ST | % Population ST | 729 | 19.3 | 4.8 | 99.4 | 0.0 | 28.4 |
| Pop_den | Population density | 729 | 1145 | 421 | 82,845 | 1.5 | 4780 |
| Sex ratio | Sex ratio of total population | 729 | 1022 | 1016 | 1332 | 755 | 72.7 |
| (females per 1000 males) | |||||||
| Pop_15 | % Population below age 15 years | 729 | 26.4 | 25.3 | 50.6 | 16.0 | 5.3 |
| Insurance | % Households with any usual | 729 | 40.2 | 35.7 | 97.8 | 1.2 | 23.05 |
| member covered under a health | |||||||
| insurance/financing scheme | |||||||
| Water_impr | % Population living in | 729 | 93.6 | 96.9 | 100.0 | 41.2 | 9.1 |
| households with an improved | |||||||
| drinking-water source | |||||||
| Pre-primary | % Children aged 5 years who | 729 | 12.7 | 9.8 | 52.9 | 0.0 | 10.3 |
| attended pre-primary school | |||||||
| during the school years 2019–2020 | |||||||
| Tetanus_mother | % Mothers whose last birth | 729 | 91.1 | 92.6 | 100.0 | 55.1 | 6.2 |
| was protected against | |||||||
| neonatal tetanus | |||||||
| Vax_full_child | % Children age 12–23 months | 729 | 76.3 | 77.5 | 100.0 | 0.0 | 15.7 |
| fully vaccinated based on | |||||||
| information from either | |||||||
| vaccination card or | |||||||
| mother’s recall | |||||||
| Vax_polio_child | % Children aged 12–23 months | 729 | 80.0 | 81.9 | 100.0 | 0.0 | 14.8 |
| vaccinated with 3 polio doses | |||||||
| Sterilization | % Female sterilization | 729 | 34.9 | 34.0 | 76.5 | 1.1 | 18.9 |
| School_women | % Women with 10 or more | 729 | 40.4 | 39.3 | 88.2 | 13.6 | 14.1 |
| years of schooling | |||||||
| Early_marriage | % Women age 20–24 years | 729 | 20.6 | 18.6 | 80.9 | 0.0 | 12.7 |
| married before 18 yrs | |||||||
| Early_pregnant | % Women age 15–19 years | 729 | 6.5 | 4.9 | 91.9 | 0.0 | 6.5 |
| who were already mothers | |||||||
| or pregnant at the time of | |||||||
| the survey | |||||||
| HT_female | % Females with elevated blood | 729 | 21.5 | 21.1 | 42.1 | 8.5 | 5.2 |
| pressure (BP) or taking | |||||||
| medicine to control BP | |||||||
| Breastfed_child | % Children under age of 6 months | 729 | 41.3 | 55.0 | 94.0 | 0.0 | 33.5 |
| exclusively breastfed (%) | |||||||
| Wasted_child | Children under 5 years who were | 729 | 18.5 | 18.0 | 48.0 | 4.5 | 6.5 |
| wasted (weight for height) | |||||||
| SHC_burden | Population served by an | 727 | 2768 | 2557 | 21045 | 179 | 1574 |
| average sub-heath centre | |||||||
| SHC_density | Average number of sub-health | 727 | 0.3 | 0.2 | 21.8 | 0.0 | 1.1 |
| centres per sq. km | |||||||
| Adist | Dummy for aspirational district | 729 | 0.16 | 0.00 | 1.00 | 0.00 | 0.37 |
| Dependent Variable: FDV% | |||||
|---|---|---|---|---|---|
| (P1) | (P2) | (P3) | (P4_1) | (P4_2) | |
| PIR% | 0.67 *** | 1.16 *** | 2.04 *** | 0.19 *** | 1.54 *** |
| (0.05) | (0.10) | (0.15) | (0.06) | (0.15) | |
| PDR% | −12.69 *** | −80.44 *** | |||
| (3.28) | (15.65) | ||||
| (PDR/PIR)% | 0.09 ** | −0.87 *** | 1.25 *** | ||
| (0.04) | (0.24) | (0.47) | |||
| IR | 0.81 *** | ||||
| (0.20) | |||||
| SHC_burden | −0.0002 *** | −0.0003 *** | −0.0002 *** | −0.001 *** | |
| (0.0000) | (0.0001) | (0.0001) | (0.0001) | ||
| SHC_density | −4.69 *** | ||||
| (1.03) | |||||
| Rural | −0.03 *** | −0.03 ** | |||
| (0.01) | (0.01) | ||||
| Literacy | 0.08 *** | 0.03 *** | 0.09 *** | ||
| (0.01) | (0.01) | (0.02) | |||
| Pop_den | 0.0002 *** | 0.001 *** | |||
| (0.0001) | (0.0002) | ||||
| Sex ratio | 0.002 ** | 0.003 ** | |||
| (0.001) | (0.001) | ||||
| SC | −0.06 ** | ||||
| (0.02) | |||||
| ST | 0.01 *** | ||||
| (0.001) | |||||
| Muslim | −0.01 ** | 0.04 *** | |||
| (0.005) | (0.01) | ||||
| Constant | −0.03 | −0.32 | −5.83 *** | 4.36 *** | 2.54 |
| (0.13) | (1.03) | (1.70) | (0.99) | (2.16) | |
| State FE | Yes | Yes | Yes | Yes | Yes |
| Observations | 625 | 629 | 629 | 626 | 626 |
| AIC | 604.79 | 2030.32 | 2561.77 | 2279.99 | 3195.05 |
| BIC | 751.23 | 2190.3 | 2726.2 | 2439.81 | 3372.62 |
| R | 0.64 | 0.70 | 0.78 | 0.66 | 0.72 |
| Adjusted R | 0.62 | 0.68 | 0.77 | 0.65 | 0.71 |
| Dependent Variable: FDV | |||||
|---|---|---|---|---|---|
| (P1) | (P2) | (P3) | (P4_1) | (P4_2) | |
| PIR% | 0.61 *** | 1.09 *** | 2.03 *** | 0.34 *** | 1.53 *** |
| (0.05) | (0.10) | (0.15) | (0.09) | (0.14) | |
| PDR% | −11.16 *** | −26.52 ** | −72.47 *** | ||
| (3.20) | (10.58) | (15.42) | |||
| (PDR/PIR)% | 0.08 ** | 0.02 | 0.09 | −0.38 | 1.33 *** |
| (0.04) | (0.09) | (0.16) | (0.29) | (0.47) | |
| IR% | 0.77 *** | ||||
| (0.19) | |||||
| SHC_burden | −0.0002 *** | −0.0003 *** | −0.0002 *** | −0.001 *** | |
| (0.0000) | (0.0001) | (0.0001) | (0.0001) | ||
| SHC_density | −3.81 *** | ||||
| (1.02) | |||||
| Rural | −0.04 *** | ||||
| (0.01) | |||||
| Literacy | 0.12 *** | ||||
| (0.02) | |||||
| Pop_den | 0.001 *** | ||||
| (0.0002) | |||||
| Sex ratio | −0.01 *** | ||||
| (0.002) | |||||
| SC | −0.07 *** | ||||
| (0.02) | |||||
| ST | 0.01 *** | −0.01 *** | |||
| (0.001) | (0.005) | ||||
| Muslim | −0.01 *** | 0.04 *** | |||
| (0.005) | (0.01) | ||||
| Pop_15 | −0.02 *** | ||||
| (0.01) | |||||
| Insurance | 0.01 *** | 0.02 ** | 0.05 *** | ||
| (0.002) | (0.01) | (0.02) | |||
| HT_female | 0.07 *** | 0.10 *** | |||
| (0.01) | (0.02) | ||||
| Pre-primary | −0.02 *** | ||||
| (0.01) | |||||
| School_women | 0.05 *** | ||||
| (0.01) | |||||
| Early_marriage | 0.09 *** | ||||
| (0.02) | |||||
| Early_pregnant | −0.13 *** | ||||
| (0.05) | |||||
| Breastfed_child | −0.01 *** | ||||
| (0.002) | |||||
| Tetanus_mother | 0.05 * | ||||
| (0.03) | |||||
| Vax_full_child | 0.05 ** | 0.08 ** | |||
| (0.02) | (0.04) | ||||
| Vax_polio_child | −0.06 ** | −0.10 ** | |||
| (0.02) | (0.04) | ||||
| Wasted_child | −0.05 *** | ||||
| (0.01) | |||||
| Sterilization | −0.01 *** | ||||
| (0.002) | |||||
| Water_impr | 0.02 ** | ||||
| (0.01) | |||||
| Adist | 0.15 *** | 0.31 ** | |||
| (0.05) | (0.14) | ||||
| Constant | 0.21 | −1.72 * | −1.10 | 5.40 *** | −2.50 |
| (0.29) | (0.98) | (0.87) | (0.94) | (3.96) | |
| State FE | Yes | Yes | Yes | Yes | Yes |
| Observations | 625 | 626 | 626 | 626 | 626 |
| AIC | 571.81 | 1996.14 | 2527.83 | 2255.96 | 3174.98 |
| BIC | 736.01 | 2164.84 | 2696.52 | 2429.1 | 3379.19 |
| R | 0.66 | 0.71 | 0.79 | 0.68 | 0.74 |
| Adjusted R | 0.64 | 0.69 | 0.78 | 0.66 | 0.72 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Agarwal, S.K.; Naha, M. COVID-19 Vaccine Coverage in India: A District-Level Analysis. Vaccines 2023, 11, 948. https://doi.org/10.3390/vaccines11050948
Agarwal SK, Naha M. COVID-19 Vaccine Coverage in India: A District-Level Analysis. Vaccines. 2023; 11(5):948. https://doi.org/10.3390/vaccines11050948
Chicago/Turabian StyleAgarwal, Sandip K., and Maharnab Naha. 2023. "COVID-19 Vaccine Coverage in India: A District-Level Analysis" Vaccines 11, no. 5: 948. https://doi.org/10.3390/vaccines11050948
APA StyleAgarwal, S. K., & Naha, M. (2023). COVID-19 Vaccine Coverage in India: A District-Level Analysis. Vaccines, 11(5), 948. https://doi.org/10.3390/vaccines11050948






