Mucosal Vaccination Strategies against Clostridioides difficile Infection
Abstract
1. Introduction
2. Animal Models Used for C. difficile Vaccination Studies
3. Immune Responses to Mucosal Vaccination
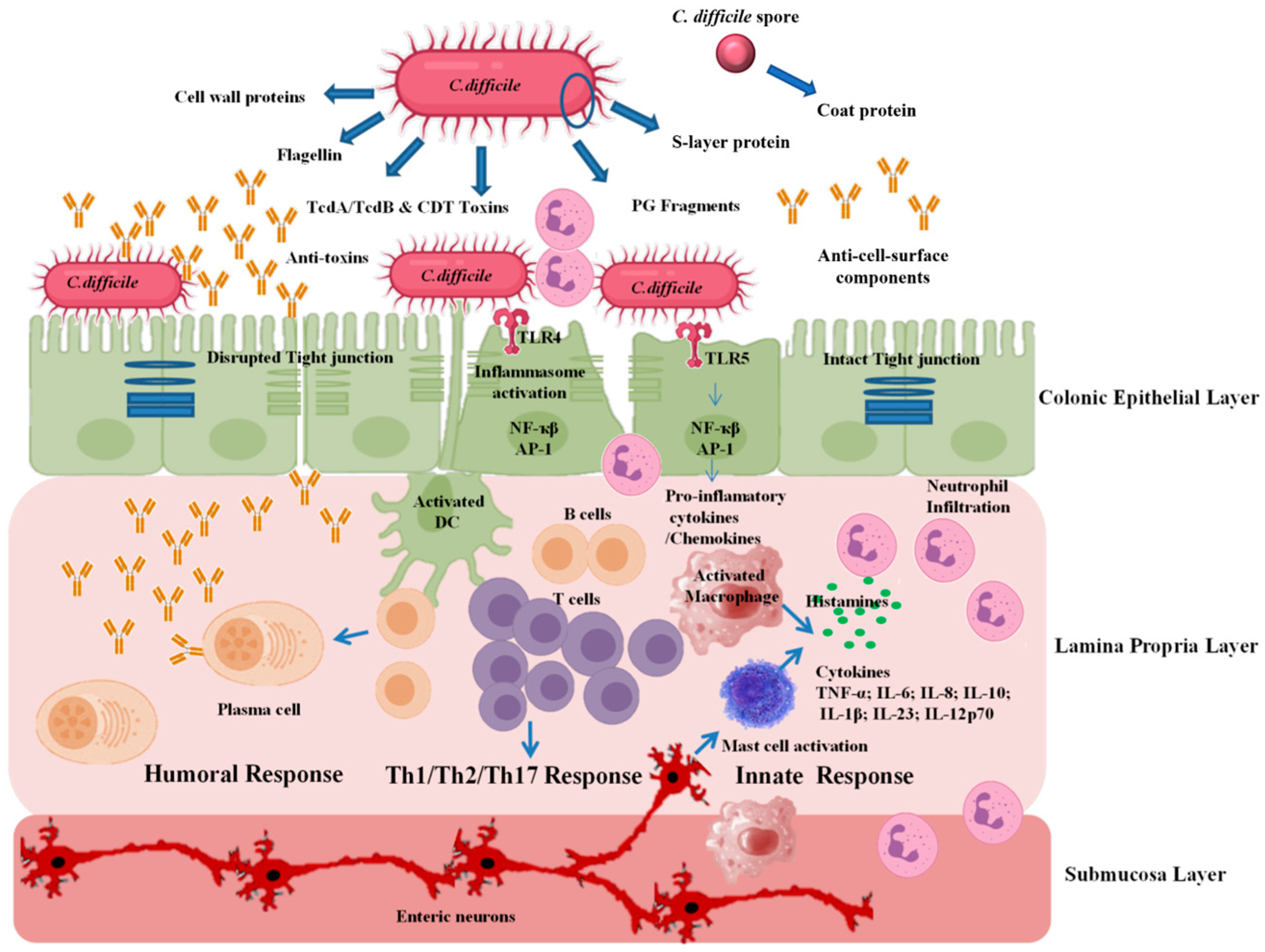
4. Mucosal Vaccination against C. difficile Toxins
4.1. Passive Mucosal Vaccination against C. difficile Toxins
4.1.1. Human Trials
4.1.2. Future Directions for Passive Mucosal Vaccination
4.2. Active Mucosal Vaccination against C. difficile Toxins
5. Surface-Antigen Mucosal Vaccine
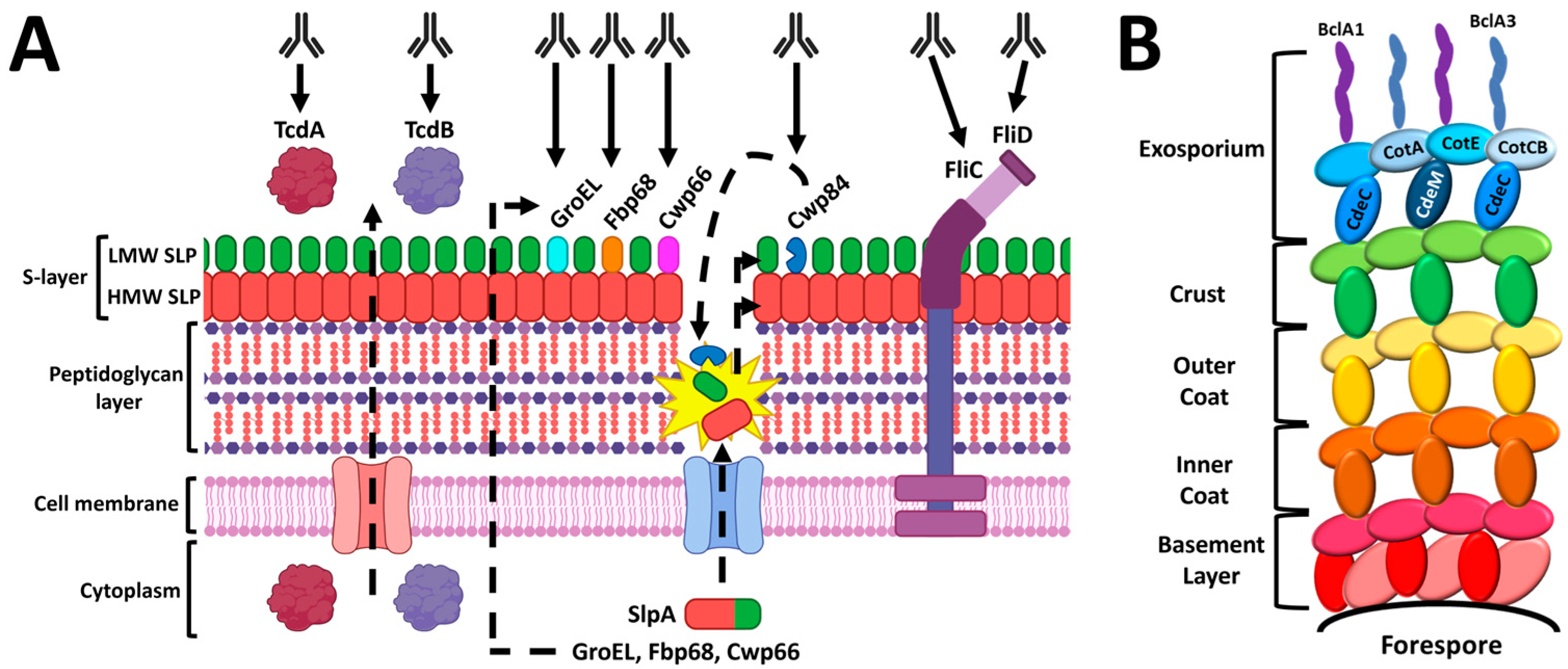
5.1. Surface-Layer Proteins
5.2. Flagellar Proteins
5.3. Spore Coat Proteins
6. Whole-C. difficile Mucosal Vaccine
7. Mucosal Vaccination of Vulnerable Patient Populations
8. Concluding Remarks
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lawson, P.A.; Citron, D.M.; Tyrrell, K.L.; Finegold, S.M. Reclassification of Clostridium difficile as Clostridioides difficile (Hall and O’Toole 1935) Prévot 1938. Anaerobe 2016, 40, 95–99. [Google Scholar] [CrossRef]
- Miller, B.A.; Chen, L.F.; Sexton, D.J.; Anderson, D.J. Comparison of the burdens of hospital-onset, healthcare facility-associated Clostridium difficile infection and of healthcare-associated infection due to methicillin-resistant Staphylococcus aureus in community hospitals. Infect. Control Hosp. Epidemiol. 2011, 32, 387–390. [Google Scholar] [CrossRef]
- Leffler, D.A.; Lamont, J.T. Clostridium difficile infection. N. Engl. J. Med. 2015, 372, 1539–1548. [Google Scholar] [CrossRef]
- Songer, J.G.; Uzal, F.A. Clostridial enteric infections in pigs. J. Vet. Diagn. Investig. 2005, 17, 528–536. [Google Scholar] [CrossRef]
- Songer, J.G.; Trinh, H.T.; Killgore, G.E.; Thompson, A.D.; McDonald, L.C.; Limbago, B.M. Clostridium difficile in retail meat products, USA, 2007. Emerg. Infect. Dis. 2009, 15, 819. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, C.; Hakimi, D.-E.; Vanleyssem, R.; Taminiau, B.; Van Broeck, J.; Delmée, M.; Korsak, N.; Daube, G. Clostridium difficile in beef cattle farms, farmers and their environment: Assessing the spread of the bacterium. Vet. Microbiol. 2017, 210, 183–187. [Google Scholar] [CrossRef] [PubMed]
- McLure, A.; Clements, A.C.; Kirk, M.; Glass, K. Modelling diverse sources of Clostridium difficile in the community: Importance of animals, infants and asymptomatic carriers. Epidemiol. Infect. 2019, 147, e152. [Google Scholar] [CrossRef] [PubMed]
- Khanna, S.; Gerding, D.N. Current and future trends in Clostridioides (Clostridium) difficile infection management. Anaerobe 2019, 58, 95–102. [Google Scholar] [CrossRef]
- Hedge, D.D.; Strain, J.D.; Heins, J.R.; Farver, D.K. New advances in the treatment of Clostridium difficile infection (CDI). Ther. Clin. Risk Manag. 2008, 4, 949. [Google Scholar] [PubMed]
- Freeman, J.; Vernon, J.; Morris, K.; Nicholson, S.; Todhunter, S.; Longshaw, C.; Wilcox, M.H. Pan-European longitudinal surveillance of antibiotic resistance among prevalent Clostridium difficile ribotypes. Clin. Microbiol. Infect. 2015, 21, 248.e9–248.e16. [Google Scholar] [CrossRef] [PubMed]
- Spigaglia, P. Recent advances in the understanding of antibiotic resistance in Clostridium difficile infection. Ther. Adv. Infect. Dis. 2016, 3, 23–42. [Google Scholar] [CrossRef] [PubMed]
- Peng, Z.; Jin, D.; Kim, H.B.; Stratton, C.W.; Wu, B.; Tang, Y.-W.; Sun, X. Update on antimicrobial resistance in Clostridium difficile: Resistance mechanisms and antimicrobial susceptibility testing. J. Clin. Microbiol. 2017, 55, 1998–2008. [Google Scholar] [CrossRef]
- Rao, K.; Safdar, N. Fecal microbiota transplantation for the treatment of Clostridium difficile infection. J. Hosp. Med. 2016, 11, 56–61. [Google Scholar] [CrossRef]
- Heuler, J.; Fortier, L.-C.; Sun, X. Clostridioides difficile phage biology and application. FEMS Microbiol. Rev. 2021, 45, fuab012. [Google Scholar] [CrossRef]
- Champredon, D.; Shoukat, A.; Moghadas, S.M. Effectiveness and cost-effectiveness of a Clostridium difficile vaccine candidate in a hospital setting. Vaccine 2020, 38, 2585–2591. [Google Scholar] [CrossRef] [PubMed]
- Kitchin, N.; Remich, S.A.; Peterson, J.; Peng, Y.; Gruber, W.C.; Jansen, K.U.; Pride, M.W.; Anderson, A.S.; Knirsch, C.; Webber, C. A phase 2 study evaluating the safety, tolerability, and immunogenicity of two 3-dose regimens of a Clostridium difficile vaccine in healthy US adults aged 65 to 85 years. Clin. Infect. Dis. 2020, 70, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Bézay, N.; Ayad, A.; Dubischar, K.; Firbas, C.; Hochreiter, R.; Kiermayr, S.; Kiss, I.; Pinl, F.; Jilma, B.; Westritschnig, K. Safety, immunogenicity and dose response of VLA84, a new vaccine candidate against Clostridium difficile, in healthy volunteers. Vaccine 2016, 34, 2585–2592. [Google Scholar] [CrossRef]
- National Institutes of Health. Study of a Candidate Clostridium difficile Toxoid Vaccine (Cdiffense) in Subjects at Risk for C. difficile. Infection 2014. [Google Scholar]
- Donald, R.G.; Flint, M.; Kalyan, N.; Johnson, E.; Witko, S.E.; Kotash, C.; Zhao, P.; Megati, S.; Yurgelonis, I.; Lee, P.K. A novel approach to generate a recombinant toxoid vaccine against Clostridium difficile. Microbiology 2013, 159, 1254. [Google Scholar] [CrossRef]
- Sheldon, E.; Kitchin, N.; Peng, Y.; Eiden, J.; Gruber, W.; Johnson, E.; Jansen, K.U.; Pride, M.W.; Pedneault, L. A phase 1, placebo-controlled, randomized study of the safety, tolerability, and immunogenicity of a Clostridium difficile vaccine administered with or without aluminum hydroxide in healthy adults. Vaccine 2016, 34, 2082–2091. [Google Scholar] [CrossRef]
- Tian, J.-H.; Fuhrmann, S.R.; Kluepfel-Stahl, S.; Carman, R.J.; Ellingsworth, L.; Flyer, D.C. A novel fusion protein containing the receptor binding domains of C. difficile toxin A and toxin B elicits protective immunity against lethal toxin and spore challenge in preclinical efficacy models. Vaccine 2012, 30, 4249–4258. [Google Scholar] [CrossRef] [PubMed]
- Sougioultzis, S.; Kyne, L.; Drudy, D.; Keates, S.; Maroo, S.; Pothoulakis, C.; Giannasca, P.J.; Lee, C.K.; Warny, M.; Monath, T.P. Clostridium difficile toxoid vaccine in recurrent C. difficile-associated diarrhea. Gastroenterology 2005, 128, 764–770. [Google Scholar] [CrossRef] [PubMed]
- Aboudola, S.; Kotloff, K.L.; Kyne, L.; Warny, M.; Kelly, E.C.; Sougioultzis, S.; Giannasca, P.J.; Monath, T.P.; Kelly, C.P. Clostridium difficile vaccine and serum immunoglobulin G antibody response to toxin A. Infect. Immun. 2003, 71, 1608–1610. [Google Scholar] [CrossRef]
- Kotloff, K.L.; Wasserman, S.S.; Losonsky, G.A.; Thomas, W., Jr.; Nichols, R.; Edelman, R.; Bridwell, M.; Monath, T.P. Safety and immunogenicity of increasing doses of a Clostridium difficile toxoid vaccine administered to healthy adults. Infect. Immun. 2001, 69, 988–995. [Google Scholar] [CrossRef]
- Greenberg, R.N.; Marbury, T.C.; Foglia, G.; Warny, M. Phase I dose finding studies of an adjuvanted Clostridium difficile toxoid vaccine. Vaccine 2012, 30, 2245–2249. [Google Scholar] [CrossRef]
- de Bruyn, G.; Gordon, D.L.; Steiner, T.; Tambyah, P.; Cosgrove, C.; Martens, M.; Bassily, E.; Chan, E.-S.; Patel, D.; Chen, J. Safety, immunogenicity, and efficacy of a Clostridioides difficile toxoid vaccine candidate: A phase 3 multicentre, observer-blind, randomised, controlled trial. Lancet Infect. Dis. 2021, 21, 252–262. [Google Scholar] [CrossRef]
- de Bruyn, G.; Saleh, J.; Workman, D.; Pollak, R.; Elinoff, V.; Fraser, N.J.; Lefebvre, G.; Martens, M.; Mills, R.E.; Nathan, R. Defining the optimal formulation and schedule of a candidate toxoid vaccine against Clostridium difficile infection: A randomized Phase 2 clinical trial. Vaccine 2016, 34, 2170–2178. [Google Scholar] [CrossRef]
- Kelly, C.P.; Pothoulakis, C.; LaMont, J.T. Clostridium difficile colitis. N. Engl. J. Med. 1994, 330, 257–262. [Google Scholar] [CrossRef]
- Best, E.L.; Freeman, J.; Wilcox, M.H. Models for the study of Clostridium difficile infection. Gut Microbes 2012, 3, 145–167. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Wang, S.; Bouillaut, L.; Li, C.; Duan, Z.; Zhang, K.; Ju, X.; Tzipori, S.; Sonenshein, A.L.; Sun, X. Oral immunization with nontoxigenic Clostridium difficile strains expressing chimeric fragments of TcdA and TcdB elicits protective immunity against C. difficile infection in both mice and hamsters. Infect. Immun. 2018, 86, e00489-18. [Google Scholar] [CrossRef]
- Lyerly, D.M.; Bostwick, E.; Binion, S.; Wilkins, T. Passive immunization of hamsters against disease caused by Clostridium difficile by use of bovine immunoglobulin G concentrate. Infect. Immun. 1991, 59, 2215–2218. [Google Scholar] [CrossRef]
- Péchiné, S.; Denève, C.; Le Monnier, A.; Hoys, S.; Janoir, C.; Collignon, A. Immunization of hamsters against Clostridium difficile infection using the Cwp84 protease as an antigen. FEMS Immunol. Med. Microbiol. 2011, 63, 73–81. [Google Scholar] [CrossRef]
- O’Brien, J.B.; McCabe, M.S.; Athié-Morales, V.; McDonald, G.S.; Ní Eidhin, D.B.; Kelleher, D.P. Passive immunisation of hamsters against Clostridium difficile infection using antibodies to surface layer proteins. FEMS Microbiol. Lett. 2005, 246, 199–205. [Google Scholar] [CrossRef] [PubMed]
- Siddiqui, F.; O’Connor, J.R.; Nagaro, K.; Cheknis, A.; Sambol, S.P.; Vedantam, G.; Gerding, D.N.; Johnson, S. Vaccination with parenteral toxoid B protects hamsters against lethal challenge with toxin A–negative, toxin B–positive Clostridium difficile but does not prevent colonization. J. Infect. Dis. 2012, 205, 128–133. [Google Scholar] [CrossRef]
- Ní Eidhin, D.B.; O’Brien, J.B.; McCabe, M.S.; Athié-Morales, V.; Kelleher, D.P. Active immunization of hamsters against Clostridium difficile infection using surface-layer protein. FEMS Immunol. Med. Microbiol. 2008, 52, 207–218. [Google Scholar] [CrossRef] [PubMed]
- Torres, J.F.; Lyerly, D.M.; Hill, J.E.; Monath, T.P. Evaluation of formalin-inactivated Clostridium difficile vaccines administered by parenteral and mucosal routes of immunization in hamsters. Infect. Immun. 1995, 63, 4619–4627. [Google Scholar] [CrossRef]
- Liu, Y.-W.; Chen, Y.-H.; Chen, J.-W.; Tsai, P.-J.; Huang, I.-H. Immunization with recombinant TcdB-encapsulated nanocomplex induces protection against Clostridium difficile challenge in a mouse model. Front. Microbiol. 2017, 8, 1411. [Google Scholar] [CrossRef] [PubMed]
- Guo, S.; Yan, W.; McDonough, S.P.; Lin, N.; Wu, K.J.; He, H.; Xiang, H.; Yang, M.; Moreira, M.A.S.; Chang, Y.-F. The recombinant Lactococcus lactis oral vaccine induces protection against C. difficile spore challenge in a mouse model. Vaccine 2015, 33, 1586–1595. [Google Scholar] [CrossRef]
- Péchiné, S.; Janoir, C.; Boureau, H.; Gleizes, A.; Tsapis, N.; Hoys, S.; Fattal, E.; Collignon, A. Diminished intestinal colonization by Clostridium difficile and immune response in mice after mucosal immunization with surface proteins of Clostridium difficile. Vaccine 2007, 25, 3946–3954. [Google Scholar] [CrossRef]
- Winter, K.; Xing, L.; Kassardjian, A.; Ward, B.J. Vaccination against Clostridium difficile by use of an attenuated Salmonella enterica serovar typhimurium vector (YS1646) protects mice from lethal challenge. Infect. Immun. 2019, 87, e00089-19. [Google Scholar] [CrossRef]
- Hutton, M.L.; Mackin, K.E.; Chakravorty, A.; Lyras, D. Small animal models for the study of Clostridium difficile disease pathogenesis. FEMS Microbiol. Lett. 2014, 352, 140–149. [Google Scholar] [CrossRef] [PubMed]
- Lawley, T.D.; Clare, S.; Walker, A.W.; Goulding, D.; Stabler, R.A.; Croucher, N.; Mastroeni, P.; Scott, P.; Raisen, C.; Mottram, L.; et al. Antibiotic Treatment of Clostridium difficile Carrier Mice Triggers a Supershedder State, Spore-Mediated Transmission, and Severe Disease in Immunocompromised Hosts. Infect. Immun. 2009, 77, 3661–3669. [Google Scholar] [CrossRef] [PubMed]
- Winston, J.A.; Thanissery, R.; Montgomery, S.A.; Theriot, C.M. Cefoperazone-treated mouse model of clinically-relevant Clostridium difficile strain R20291. JoVE (J. Vis. Exp.) 2016, 118, e54850. [Google Scholar]
- Owens, R.C., Jr.; Donskey, C.J.; Gaynes, R.P.; Loo, V.G.; Muto, C.A. Antimicrobial-associated risk factors for Clostridium difficile infection. Clin. Infect. Dis. 2008, 46, S19–S31. [Google Scholar] [CrossRef]
- Chen, X.; Katchar, K.; Goldsmith, J.D.; Nanthakumar, N.; Cheknis, A.; Gerding, D.N.; Kelly, C.P. A mouse model of Clostridium difficile–associated disease. Gastroenterology 2008, 135, 1984–1992. [Google Scholar] [CrossRef]
- Shin, J.H.; Pawlowski, S.W.; Warren, C.A. Teaching old mice new tricks: The utility of aged mouse models of C. difficile infection to study pathogenesis and rejuvenate immune response. Gut Microbes 2021, 13, 1966255. [Google Scholar] [CrossRef]
- Sun, X.; Wang, H.; Zhang, Y.; Chen, K.; Davis, B.; Feng, H. Mouse relapse model of Clostridium difficile infection. Infect. Immun. 2011, 79, 2856–2864. [Google Scholar] [CrossRef]
- Collins, J.; Auchtung, J.M.; Schaefer, L.; Eaton, K.A.; Britton, R.A. Humanized microbiota mice as a model of recurrent Clostridium difficile disease. Microbiome 2015, 3, 35. [Google Scholar] [CrossRef]
- Pasetti, M.F.; Simon, J.K.; Sztein, M.B.; Levine, M.M. Immunology of gut mucosal vaccines. Immunol. Rev. 2011, 239, 125–148. [Google Scholar] [CrossRef]
- Lavelle, E.C.; Ward, R.W. Mucosal vaccines—Fortifying the frontiers. Nat. Rev. Immunol. 2022, 22, 236–250. [Google Scholar] [CrossRef]
- Liu, J.; Zhang, X.; Cheng, Y.; Cao, X. Dendritic cell migration in inflammation and immunity. Cell. Mol. Immunol. 2021, 18, 2461–2471. [Google Scholar] [CrossRef] [PubMed]
- Mann, E.R.; Li, X. Intestinal antigen-presenting cells in mucosal immune homeostasis: Crosstalk between dendritic cells, macrophages and B-cells. World J. Gastroenterol. WJG 2014, 20, 9653. [Google Scholar] [CrossRef] [PubMed]
- Mowat, A.M.; Scott, C.L.; Bain, C.C. Barrier-tissue macrophages: Functional adaptation to environmental challenges. Nat. Med. 2017, 23, 1258–1270. [Google Scholar] [CrossRef] [PubMed]
- Cerovic, V.; Bain, C.C.; Mowat, A.M.; Milling, S.W. Intestinal macrophages and dendritic cells: What’s the difference? Trends Immunol. 2014, 35, 270–277. [Google Scholar] [CrossRef]
- Acheson, D.W.; Luccioli, S. Mucosal immune responses. Best Pract. Res. Clin. Gastroenterol. 2004, 18, 387–404. [Google Scholar] [CrossRef]
- Mörbe, U.M.; Jørgensen, P.B.; Fenton, T.M.; von Burg, N.; Riis, L.B.; Spencer, J.; Agace, W.W. Human gut-associated lymphoid tissues (GALT); diversity, structure, and function. Mucosal Immunol. 2021, 14, 793–802. [Google Scholar] [CrossRef] [PubMed]
- Kraehenbuhl, J.-P.; Neutra, M.R. Epithelial M cells: Differentiation and function. Annu. Rev. Cell Dev. Biol. 2000, 16, 301–332. [Google Scholar] [CrossRef]
- Li, M.; Wang, Y.; Sun, Y.; Cui, H.; Zhu, S.J.; Qiu, H.-J. Mucosal vaccines: Strategies and challenges. Immunol. Lett. 2020, 217, 116–125. [Google Scholar] [CrossRef] [PubMed]
- Knoop, K.A.; Newberry, R.D. Isolated lymphoid follicles are dynamic reservoirs for the induction of intestinal IgA. Front. Immunol. 2012, 3, 84. [Google Scholar] [CrossRef] [PubMed]
- Pioli, P.D. Plasma cells, the next generation: Beyond antibody secretion. Front. Immunol. 2019, 10, 2768. [Google Scholar] [CrossRef]
- Wei, H.; Wang, J.-Y. Role of polymeric immunoglobulin receptor in IgA and IgM transcytosis. Int. J. Mol. Sci. 2021, 22, 2284. [Google Scholar] [CrossRef]
- Neutra, M.R.; Kozlowski, P.A. Mucosal vaccines: The promise and the challenge. Nat. Rev. Immunol. 2006, 6, 148–158. [Google Scholar] [CrossRef]
- Komban, R.J.; Strömberg, A.; Biram, A.; Cervin, J.; Lebrero-Fernández, C.; Mabbott, N.; Yrlid, U.; Shulman, Z.; Bemark, M.; Lycke, N. Activated Peyer′ s patch B cells sample antigen directly from M cells in the subepithelial dome. Nat. Commun. 2019, 10, 2423. [Google Scholar] [CrossRef]
- Kordus, S.L.; Thomas, A.K.; Lacy, D.B. Clostridioides difficile toxins: Mechanisms of action and antitoxin therapeutics. Nat. Rev. Microbiol. 2022, 20, 285–298. [Google Scholar] [CrossRef]
- Smits, W.K.; Lyras, D.; Lacy, D.B.; Wilcox, M.H.; Kuijper, E.J. Clostridium difficile infection. Nat. Rev. Dis. Prim. 2016, 2, 16020. [Google Scholar] [CrossRef]
- Chandra, H.; Sharma, K.K.; Tuovinen, O.H.; Sun, X.; Shukla, P. Pathobionts: Mechanisms of survival, expansion, and interaction with host with a focus on Clostridioides difficile. Gut Microbes 2021, 13, 1979882. [Google Scholar] [CrossRef]
- Jafari, N.V.; Kuehne, S.A.; Bryant, C.E.; Elawad, M.; Wren, B.W.; Minton, N.P.; Allan, E.; Bajaj-Elliott, M. Clostridium difficile modulates host innate immunity via toxin-independent and dependent mechanism(s). PLoS ONE 2013, 8, e69846. [Google Scholar] [CrossRef]
- Yu, H.; Chen, K.; Sun, Y.; Carter, M.; Garey, K.W.; Savidge, T.C.; Devaraj, S.; Tessier, M.E.; von Rosenvinge, E.C.; Kelly, C.P.; et al. Cytokines Are Markers of the Clostridium difficile-Induced Inflammatory Response and Predict Disease Severity. Clin. Vaccine Immunol. 2017, 24, e00037-17. [Google Scholar] [CrossRef]
- Chen, Y.S.; Chen, I.B.; Pham, G.; Shao, T.Y.; Bangar, H.; Way, S.S.; Haslam, D.B. IL-17-producing γδ T cells protect against Clostridium difficile infection. J. Clin. Investig. 2020, 130, 2377–2390. [Google Scholar] [CrossRef]
- Clough, J.N.; Omer, O.S.; Tasker, S.; Lord, G.M.; Irving, P.M. Regulatory T-cell therapy in Crohn’s disease: Challenges and advances. Gut 2020, 69, 942–952. [Google Scholar] [CrossRef]
- Wilson, M.S.; Ramalingam, T.R.; Rivollier, A.; Shenderov, K.; Mentink-Kane, M.M.; Madala, S.K.; Cheever, A.W.; Artis, D.; Kelsall, B.L.; Wynn, T.A. Colitis and intestinal inflammation in IL10−/− mice results from IL-13Rα2-mediated attenuation of IL-13 activity. Gastroenterology 2011, 140, 254–264. [Google Scholar] [CrossRef]
- Chandrasekaran, R.; Lacy, D.B. The role of toxins in Clostridium difficile infection. FEMS Microbiol. Rev. 2017, 41, 723–750. [Google Scholar] [CrossRef] [PubMed]
- Voth, D.E.; Ballard, J.D. Clostridium difficile toxins: Mechanism of action and role in disease. Clin. Microbiol. Rev. 2005, 18, 247–263. [Google Scholar] [CrossRef]
- Carter, G.P.; Chakravorty, A.; Pham Nguyen, T.A.; Mileto, S.; Schreiber, F.; Li, L.; Howarth, P.; Clare, S.; Cunningham, B.; Sambol, S.P. Defining the roles of TcdA and TcdB in localized gastrointestinal disease, systemic organ damage, and the host response during Clostridium difficile infections. MBio 2015, 6, e00551-15. [Google Scholar] [CrossRef]
- Aktories, K.; Schwan, C.; Jank, T. Clostridium difficile toxin biology. Annu. Rev. Microbiol. 2017, 71, 281–307. [Google Scholar] [CrossRef] [PubMed]
- Casadevall, A.; Dadachova, E.; Pirofski, L.-a. Passive antibody therapy for infectious diseases. Nat. Rev. Microbiol. 2004, 2, 695–703. [Google Scholar] [CrossRef] [PubMed]
- Kelly, C.P.; Pothoulakis, C.; Vavva, F.; Castagliuolo, I.; Bostwick, E.F.; O’Keane, J.C.; Keates, S.; LaMont, J.T. Anti-Clostridium difficile bovine immunoglobulin concentrate inhibits cytotoxicity and enterotoxicity of C. difficile toxins. Antimicrob. Agents Chemother. 1996, 40, 373–379. [Google Scholar] [CrossRef]
- Kink, J.A.; Williams, J.A. Antibodies to recombinant Clostridium difficile toxins A and B are an effective treatment and prevent relapse of C. difficile-associated disease in a hamster model of infection. Infect. Immun. 1998, 66, 2018–2025. [Google Scholar] [CrossRef]
- van Dissel, J.T.; de Groot, N.; Hensgens, C.M.; Numan, S.; Kuijper, E.J.; Veldkamp, P.; van’t Wout, J. Bovine antibody-enriched whey to aid in the prevention of a relapse of Clostridium difficile-associated diarrhoea: Preclinical and preliminary clinical data. J. Med. Microbiol. 2005, 54, 197–205. [Google Scholar] [CrossRef]
- Mattila, E.; Anttila, V.-J.; Broas, M.; Marttila, H.; Poukka, P.; Kuusisto, K.; Pusa, L.; Sammalkorpi, K.; Dabek, J.; Koivurova, O.-P. A randomized, double-blind study comparing Clostridium difficile immune whey and metronidazole for recurrent Clostridium difficile-associated diarrhoea: Efficacy and safety data of a prematurely interrupted trial. Scand. J. Infect. Dis. 2008, 40, 702–708. [Google Scholar] [CrossRef]
- Dieterle, M.G.; Rao, K.; Young, V.B. Novel therapies and preventative strategies for primary and recurrent Clostridium difficile infections. Ann. N. Y. Acad. Sci. 2019, 1435, 110–138. [Google Scholar] [CrossRef]
- Abougergi, M.S.; Kwon, J.H. Intravenous immunoglobulin for the treatment of Clostridium difficile infection: A review. Dig. Dis. Sci. 2011, 56, 19–26. [Google Scholar] [CrossRef]
- Rhee, J.H. Current and new approaches for mucosal vaccine delivery. In Mucosal Vaccines; Elsevier: Amsterdam, The Netherlands, 2020; pp. 325–356. [Google Scholar]
- Madani, F.; Hsein, H.; Busignies, V.; Tchoreloff, P. An overview on dosage forms and formulation strategies for vaccines and antibodies oral delivery. Pharm. Dev. Technol. 2020, 25, 133–148. [Google Scholar] [CrossRef]
- Warny, M.; Fatimi, A.; Bostwick, E.; Laine, D.; Lebel, F.; LaMont, J.; Pothoulakis, C.; Kelly, C. Bovine immunoglobulin concentrate-Clostridium difficile retains C difficile toxin neutralising activity after passage through the human stomach and small intestine. Gut 1999, 44, 212–217. [Google Scholar] [CrossRef]
- Kelly, C.P.; Chetham, S.; Keates, S.; Bostwick, E.F.; Roush, A.M.; Castagliuolo, I.; LaMont, J.T.; Pothoulakis, C. Survival of anti-Clostridium difficile bovine immunoglobulin concentrate in the human gastrointestinal tract. Antimicrob. Agents Chemother. 1997, 41, 236–241. [Google Scholar] [CrossRef] [PubMed]
- Corthésy, B. Roundtrip ticket for secretory IgA: Role in mucosal homeostasis? J. Immunol. 2007, 178, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Fagarasan, S.; Honjo, T. Intestinal IgA synthesis: Regulation of front-line body defences. Nat. Rev. Immunol. 2003, 3, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Jones, R.G.; Martino, A. Targeted localized use of therapeutic antibodies: A review of non-systemic, topical and oral applications. Crit. Rev. Biotechnol. 2016, 36, 506–520. [Google Scholar] [CrossRef]
- Navalkele, B.D.; Chopra, T. Bezlotoxumab: An emerging monoclonal antibody therapy for prevention of recurrent Clostridium difficile infection. Biol. Targets Ther. 2018, 12, 11–21. [Google Scholar] [CrossRef]
- Wilcox, M.; Gerding, D.; Poxton, I.; Kelly, C.; Nathan, R.; Cornely, O.; Rahav, G.; Lee, C.; Eves, K.; Pedley, A. Bezlotoxumab alone and with actoxumab for prevention of recurrent Clostridium difficile infection in patients on standard of care antibiotics: Integrated results of 2 phase 3 studies (MODIFY I and MODIFY II). Open Forum Infect. Dis. 2015, 2, 67. [Google Scholar] [CrossRef]
- Wilcox, M.; Gerding, D.; Poxton, I.; Kelly, C.; Nathan, R.; Rahav, G.; Cornely, O.; Jenkin, G.; Jensen, W.; Eves, K. Phase 3 double-blind study of actoxumab (ACT) & bezlotoxumab (BEZ) for prevention of recurrent C. difficile infection (rCDI) in patients on standard of care (SoC) antibiotics (MODIFY I). In Proceedings of the Interscience Conference on Antimicrobial Agents and Chemotherapy, San Diego, CA, USA, 17–21 September 2015; pp. 17–21. [Google Scholar]
- Andersen, K.K.; Strokappe, N.M.; Hultberg, A.; Truusalu, K.; Smidt, I.; Mikelsaar, R.-H.; Mikelsaar, M.; Verrips, T.; Hammarström, L.; Marcotte, H. Neutralization of Clostridium difficile toxin B mediated by engineered lactobacilli that produce single-domain antibodies. Infect. Immun. 2016, 84, 395–406. [Google Scholar] [CrossRef] [PubMed]
- Riley, T.; Lyras, D.; Douce, G. Status of vaccine research and development for Clostridium difficile. Vaccine 2019, 37, 7300–7306. [Google Scholar] [CrossRef] [PubMed]
- Bruxelle, J.-F.; Péchiné, S.; Collignon, A. Immunization strategies against Clostridium difficile. In Updates on Clostridium difficile in Europe; Springer: Cham, Switzerland, 2018; pp. 197–225. [Google Scholar] [CrossRef]
- Ryan, E.T.; Butterton, J.R.; Smith, R.N.; Carroll, P.A.; Crean, T.I.; Calderwood, S.B. Protective immunity against Clostridium difficile toxin A induced by oral immunization with a live, attenuated Vibrio cholerae vector strain. Infect. Immun. 1997, 65, 2941–2949. [Google Scholar] [CrossRef]
- Ward, S.J.; Douce, G.; Figueiredo, D.; Dougan, G.; Wren, B.W. Immunogenicity of a Salmonella typhimurium aroA aroD vaccine expressing a nontoxic domain of Clostridium difficile toxin A. Infect. Immun. 1999, 67, 2145–2152. [Google Scholar] [CrossRef] [PubMed]
- Hong, H.A.; Hitri, K.; Hosseini, S.; Kotowicz, N.; Bryan, D.; Mawas, F.; Wilkinson, A.J.; van Broekhoven, A.; Kearsey, J.; Cutting, S.M. Mucosal antibodies to the C terminus of toxin A prevent colonization of Clostridium difficile. Infect. Immun. 2017, 85, e01060-16. [Google Scholar] [CrossRef]
- Permpoonpattana, P.; Hong, H.A.; Phetcharaburanin, J.; Huang, J.-M.; Cook, J.; Fairweather, N.F.; Cutting, S.M. Immunization with Bacillus spores expressing toxin A peptide repeats protects against infection with Clostridium difficile strains producing toxins A and B. Infect. Immun. 2011, 79, 2295–2302. [Google Scholar] [CrossRef]
- Leuzzi, R.; Adamo, R.; Scarselli, M. Vaccines against Clostridium difficile. Hum. Vaccines Immunother. 2014, 10, 1466–1477. [Google Scholar] [CrossRef]
- Monteiro, M.A.; Ma, Z.; Bertolo, L.; Jiao, Y.; Arroyo, L.; Hodgins, D.; Mallozzi, M.; Vedantam, G.; Sagermann, M.; Sundsmo, J. Carbohydrate-based Clostridium difficile vaccines. Expert Rev. Vaccines 2013, 12, 421–431. [Google Scholar] [CrossRef]
- Kyne, L.; Warny, M.; Qamar, A.; Kelly, C.P. Asymptomatic carriage of Clostridium difficile and serum levels of IgG antibody against toxin A. N. Engl. J. Med. 2000, 342, 390–397. [Google Scholar] [CrossRef]
- Shah, H.B.; Smith, K.; Scott, E.J.; Larabee, J.L.; James, J.A.; Ballard, J.D.; Lang, M.L. Human C. difficile toxin–specific memory B cell repertoires encode poorly neutralizing antibodies. JCI Insight 2020, 5, e138137. [Google Scholar] [CrossRef]
- Gerding, D.N.; Johnson, S.; Rupnik, M.; Aktories, K. Clostridium difficile binary toxin CDT: Mechanism, epidemiology, and potential clinical importance. Gut Microbes 2014, 5, 15–27. [Google Scholar] [CrossRef] [PubMed]
- Secore, S.; Wang, S.; Doughtry, J.; Xie, J.; Miezeiewski, M.; Rustandi, R.R.; Horton, M.; Xoconostle, R.; Wang, B.; Lancaster, C. Development of a novel vaccine containing binary toxin for the prevention of Clostridium difficile disease with enhanced efficacy against NAP1 strains. PLoS ONE 2017, 12, e0170640. [Google Scholar] [CrossRef] [PubMed]
- Péchiné, S.; Gleizes, A.; Janoir, C.; Gorges-Kergot, R.; Barc, M.-C.; Delmée, M.; Collignon, A. Immunological properties of surface proteins of Clostridium difficile. J. Med. Microbiol. 2005, 54, 193–196. [Google Scholar] [CrossRef]
- Senoh, M.; Iwaki, M.; Yamamoto, A.; Kato, H.; Fukuda, T.; Shibayama, K. Development of vaccine for Clostridium difficile infection using membrane fraction of nontoxigenic Clostridium difficile. Microb. Pathog. 2018, 123, 42–46. [Google Scholar] [CrossRef]
- Senoh, M.; Iwaki, M.; Yamamoto, A.; Kato, H.; Fukuda, T.; Shibayama, K. Inhibition of adhesion of Clostridium difficile to human intestinal cells after treatment with serum and intestinal fluid isolated from mice immunized with nontoxigenic C. difficile membrane fraction. Microb. Pathog. 2015, 81, 1–5. [Google Scholar] [CrossRef]
- Kirk, J.A.; Banerji, O.; Fagan, R.P. Characteristics of the Clostridium difficile cell envelope and its importance in therapeutics. Microb. Biotechnol. 2017, 10, 76–90. [Google Scholar] [CrossRef]
- Bradshaw, W.J.; Roberts, A.K.; Shone, C.C.; Acharya, K.R. The structure of the S-layer of Clostridium difficile. J. Cell Commun. Signal. 2018, 12, 319–331. [Google Scholar] [CrossRef] [PubMed]
- Paredes-Sabja, D.; Shen, A.; Sorg, J.A. Clostridium difficile spore biology: Sporulation, germination, and spore structural proteins. Trends Microbiol. 2014, 22, 406–416. [Google Scholar] [CrossRef]
- Dang, T.T.; Riva, L.d.L.; Fagan, R.P.; Storck, E.M.; Heal, W.P.; Janoir, C.; Fairweather, N.F.; Tate, E.W. Chemical probes of surface layer biogenesis in Clostridium difficile. ACS Chem. Biol. 2010, 5, 279–285. [Google Scholar] [CrossRef]
- Bruxelle, J.-F.; Mizrahi, A.; Hoys, S.; Collignon, A.; Janoir, C.; Péchiné, S. Immunogenic properties of the surface layer precursor of Clostridium difficile and vaccination assays in animal models. Anaerobe 2016, 37, 78–84. [Google Scholar] [CrossRef]
- Fagan, R.P.; Janoir, C.; Collignon, A.; Mastrantonio, P.; Poxton, I.R.; Fairweather, N.F. A proposed nomenclature for cell wall proteins of Clostridium difficile. J. Med. Microbiol. 2011, 60, 1225–1228. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Péchiné, S.; Janoir, C.; Collignon, A. Variability of Clostridium difficile surface proteins and specific serum antibody response in patients with Clostridium difficile-associated disease. J. Clin. Microbiol. 2005, 43, 5018–5025. [Google Scholar] [CrossRef] [PubMed]
- Sandolo, C.; Péchiné, S.; Le Monnier, A.; Hoys, S.; Janoir, C.; Coviello, T.; Alhaique, F.; Collignon, A.; Fattal, E.; Tsapis, N. Encapsulation of Cwp84 into pectin beads for oral vaccination against Clostridium difficile. Eur. J. Pharm. Biopharm. 2011, 79, 566–573. [Google Scholar] [CrossRef]
- Waligora, A.-J.; Hennequin, C.; Mullany, P.; Bourlioux, P.; Collignon, A.; Karjalainen, T. Characterization of a cell surface protein of Clostridium difficile with adhesive properties. Infect. Immun. 2001, 69, 2144–2153. [Google Scholar] [CrossRef] [PubMed]
- Wright, A.; Drudy, D.; Kyne, L.; Brown, K.; Fairweather, N.F. Immunoreactive cell wall proteins of Clostridium difficile identified by human sera. J. Med. Microbiol. 2008, 57, 750–756. [Google Scholar] [CrossRef]
- Bradshaw, W.J.; Bruxelle, J.-F.; Kovacs-Simon, A.; Harmer, N.J.; Janoir, C.; Péchiné, S.; Acharya, K.R.; Michell, S.L. Molecular features of lipoprotein CD0873: A potential vaccine against the human pathogen Clostridioides difficile. J. Biol. Chem. 2019, 294, 15850–15861. [Google Scholar] [CrossRef]
- Kovacs-Simon, A.; Leuzzi, R.; Kasendra, M.; Minton, N.; Titball, R.W.; Michell, S.L. Lipoprotein CD0873 is a novel adhesin of Clostridium difficile. J. Infect. Dis. 2014, 210, 274–284. [Google Scholar] [CrossRef]
- Karyal, C.; Hughes, J.; Kelly, M.L.; Luckett, J.C.; Kaye, P.V.; Cockayne, A.; Minton, N.P.; Griffin, R. Colonisation factor CD0873, an attractive oral vaccine candidate against Clostridioides difficile. Microorganisms 2021, 9, 306. [Google Scholar] [CrossRef]
- Karyal, C.; Palazi, P.; Hughes, J.; Griffiths, R.C.; Persaud, R.R.; Tighe, P.J.; Mitchell, N.J.; Griffin, R. Mimicking Native Display of CD0873 on Liposomes Augments Its Potency as an Oral Vaccine against Clostridioides difficile. Vaccines 2021, 9, 1453. [Google Scholar] [CrossRef]
- Hennequin, C.; Porcheray, F.; Waligora-Dupriet, A.-J.; Collignon, A.; Barc, M.-C.; Bourlioux, P.; Karjalainen, T. GroEL (Hsp60) of Clostridium difficile is involved in cell adherence. Microbiology 2001, 147, 87–96. [Google Scholar] [CrossRef]
- Péchiné, S.; Hennequin, C.; Boursier, C.; Hoys, S.; Collignon, A. Immunization using GroEL decreases Clostridium difficile intestinal colonization. PLoS ONE 2013, 8, e81112. [Google Scholar] [CrossRef]
- Tasteyre, A.; Barc, M.-C.; Collignon, A.; Boureau, H.; Karjalainen, T. Role of FliC and FliD flagellar proteins of Clostridium difficile in adherence and gut colonization. Infect. Immun. 2001, 69, 7937–7940. [Google Scholar] [CrossRef] [PubMed]
- Ghose, C.; Eugenis, I.; Sun, X.; Edwards, A.N.; McBride, S.M.; Pride, D.T.; Kelly, C.P.; Ho, D.D. Immunogenicity and protective efficacy of recombinant Clostridium difficile flagellar protein FliC. Emerg. Microbes Infect. 2016, 5, 1–10. [Google Scholar] [CrossRef]
- Negri, A.; Potocki, W.; Iwanicki, A.; Obuchowski, M.; Hinc, K. Expression and display of Clostridium difficile protein FliD on the surface of Bacillus subtilis spores. J. Med. Microbiol. 2013, 62, 1379–1385. [Google Scholar] [CrossRef] [PubMed]
- Permpoonpattana, P.; Phetcharaburanin, J.; Mikelsone, A.; Dembek, M.; Tan, S.; Brisson, M.-C.; La Ragione, R.; Brisson, A.R.; Fairweather, N.; Hong, H.A. Functional characterization of Clostridium difficile spore coat proteins. J. Bacteriol. 2013, 195, 1492–1503. [Google Scholar] [CrossRef] [PubMed]
- Pizarro-Guajardo, M.; Ravanal, M.C.; Paez, M.D.; Callegari, E.; Paredes-Sabja, D. Identification of Clostridium difficile immunoreactive spore proteins of the epidemic strain R20291. PROTEOMICS–Clin. Appl. 2018, 12, 1700182. [Google Scholar] [CrossRef]
- Pizarro-Guajardo, M.; Olguín-Araneda, V.; Barra-Carrasco, J.; Brito-Silva, C.; Sarker, M.R.; Paredes-Sabja, D. Characterization of the collagen-like exosporium protein, BclA1, of Clostridium difficile spores. Anaerobe 2014, 25, 18–30. [Google Scholar] [CrossRef]
- Ghose, C.; Eugenis, I.; Edwards, A.N.; Sun, X.; McBride, S.M.; Ho, D.D. Immunogenicity and protective efficacy of Clostridium difficile spore proteins. Anaerobe 2016, 37, 85–95. [Google Scholar] [CrossRef]
- Calderon-Romero, P.; Castro-Cordova, P.; Reyes-Ramirez, R.; Milano-Cespedes, M.; Guerrero-Araya, E.; Pizarro-Guajardo, M.; Olguin-Araneda, V.; Gil, F.; Paredes-Sabja, D. Clostridium difficile exosporium cysteine-rich proteins are essential for the morphogenesis of the exosporium layer, spore resistance, and affect C. difficile pathogenesis. PLoS Pathog. 2018, 14, e1007199. [Google Scholar] [CrossRef]
- Díaz-González, F.; Milano, M.; Olguin-Araneda, V.; Pizarro-Cerda, J.; Castro-Córdova, P.; Tzeng, S.-C.; Maier, C.S.; Sarker, M.R.; Paredes-Sabja, D. Protein composition of the outermost exosporium-like layer of Clostridium difficile 630 spores. J. Proteom. 2015, 123, 1–13. [Google Scholar] [CrossRef]
- Maia, A.R.; Reyes-Ramírez, R.; Pizarro-Guajardo, M.; Saggese, A.; Castro-Córdova, P.; Isticato, R.; Ricca, E.; Paredes-Sabja, D.; Baccigalupi, L. Induction of a Specific Humoral Immune Response by Nasal Delivery of Bcla2ctd of Clostridioides difficile. Int. J. Mol. Sci. 2020, 21, 1277. [Google Scholar] [CrossRef]
- Maia, A.R.; Reyes-Ramírez, R.; Pizarro-Guajardo, M.; Saggese, A.; Ricca, E.; Baccigalupi, L.; Paredes-Sabja, D. Nasal immunization with the C-terminal domain of BclA3 induced specific IgG production and attenuated disease symptoms in mice infected with Clostridioides difficile spores. Int. J. Mol. Sci. 2020, 21, 6696. [Google Scholar] [CrossRef]
- Aubry, A.; Zou, W.; Vinogradov, E.; Williams, D.; Chen, W.; Harris, G.; Zhou, H.; Schur, M.J.; Gilbert, M.; Douce, G.R.J.V. In Vitro Production and Immunogenicity of a Clostridium difficile Spore-Specific BclA3 Glycopeptide Conjugate Vaccine. Vaccines 2020, 8, 73. [Google Scholar] [CrossRef]
- Burns, D.A.; Heap, J.T.; Minton, N.P. SleC is essential for germination of Clostridium difficile spores in nutrient-rich medium supplemented with the bile salt taurocholate. J. Bacteriol. 2010, 192, 657–664. [Google Scholar] [CrossRef] [PubMed]
- Gutelius, D.; Hokeness, K.; Logan, S.M.; Reid, C.W. Functional analysis of SleC from Clostridium difficile: An essential lytic transglycosylase involved in spore germination. Microbiology 2014, 160, 209. [Google Scholar] [CrossRef]
- Arruda, P.H.; Madson, D.M.; Ramirez, A.; Rowe, E.W.; Songer, J.G. Bacterial probiotics as an aid in the control of Clostridium difficile disease in neonatal pigs. Can. Vet. J. 2016, 57, 183. [Google Scholar]
- Gerding, D.N.; Sambol, S.P.; Johnson, S. Non-toxigenic Clostridioides (formerly Clostridium) difficile for prevention of C. difficile infection: From bench to bedside back to bench and back to bedside. Front. Microbiol. 2018, 9, 1700. [Google Scholar] [CrossRef]
- Gerding, D.N.; Meyer, T.; Lee, C.; Cohen, S.H.; Murthy, U.K.; Poirier, A.; Van Schooneveld, T.C.; Pardi, D.S.; Ramos, A.; Barron, M.A. Administration of spores of nontoxigenic Clostridium difficile strain M3 for prevention of recurrent C difficile infection: A randomized clinical trial. JAMA 2015, 313, 1719–1727. [Google Scholar] [CrossRef]
- Wang, S.; Zhu, D.; Sun, X. Development of an Effective Nontoxigenic Clostridioides difficile–Based Oral Vaccine against C. difficile Infection. Microbiol. Spectr. 2022, 10, e00263-22. [Google Scholar] [CrossRef] [PubMed]
- Hughes, J.; Aston, C.; Kelly, M.L.; Griffin, R. Towards Development of a Non-Toxigenic Clostridioides difficile Oral Spore Vaccine against Toxigenic C. difficile. Pharmaceutics 2022, 14, 1086. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Heuler, J.; Wickramage, I.; Sun, X. Genomic and Phenotypic Characterization of the Nontoxigenic Clostridioides difficile Strain CCUG37785 and Demonstration of Its Therapeutic Potential for the Prevention of C. difficile Infection. Microbiol. Spectr. 2022, 10, e01788-21. [Google Scholar] [CrossRef] [PubMed]
- Brouwer, M.S.; Roberts, A.P.; Hussain, H.; Williams, R.J.; Allan, E.; Mullany, P. Horizontal gene transfer converts non-toxigenic Clostridium difficile strains into toxin producers. Nat. Commun. 2013, 4, 2601. [Google Scholar] [CrossRef] [PubMed]
- Mills, J.P.; Rao, K.; Young, V.B. Probiotics for prevention of Clostridium difficile infection. Curr. Opin. Gastroenterol. 2018, 34, 3. [Google Scholar] [CrossRef] [PubMed]
- Revolinski, S.L.; Munoz-Price, L.S. Clostridium difficile in immunocompromised hosts: A review of epidemiology, risk factors, treatment, and prevention. Clin. Infect. Dis. 2019, 68, 2144–2153. [Google Scholar] [CrossRef]
- Lamb, C.A.; Kennedy, N.A.; Raine, T.; Hendy, P.A.; Smith, P.J.; Limdi, J.K.; Hayee, B.H.; Lomer, M.C.; Parkes, G.C.; Selinger, C. British Society of Gastroenterology consensus guidelines on the management of inflammatory bowel disease in adults. Gut 2019, 68, s1–s106. [Google Scholar] [CrossRef]
- Macaluso, F.S.; Liguori, G.; Galli, M. Vaccinations in patients with inflammatory bowel disease. Dig. Liver Dis. 2021, 53, 1539–1545. [Google Scholar] [CrossRef]
- Manser, C.N.; Maillard, M.H.; Rogler, G.; Schreiner, P.; Rieder, F.; Bühler, S. Vaccination in patients with inflammatory bowel diseases. Digestion 2020, 101, 58–68. [Google Scholar] [CrossRef]
- See, K.C. Vaccination for the prevention of infection among immunocompromised patients: A concise review of recent systematic reviews. Vaccines 2022, 10, 800. [Google Scholar] [CrossRef]
- Ljungman, P. Vaccination of immunocompromised patients. Clin. Microbiol. Infect. 2012, 18, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Sobh, A.; Bonilla, F.A. Vaccination in primary immunodeficiency disorders. J. Allergy Clin. Immunol. Pract. 2016, 4, 1066–1075. [Google Scholar] [CrossRef]
- Löbermann, M.; Boršo, D.; Hilgendorf, I.; Fritzsche, C.; Zettl, U.K.; Reisinger, E.C. Immunization in the adult immunocompromised host. Autoimmun. Rev. 2012, 11, 212–218. [Google Scholar] [CrossRef] [PubMed]
- Daniels, L.M.; Kufel, W.D. Clinical review of Clostridium difficile infection: An update on treatment and prevention. Expert Opin. Pharmacother. 2018, 19, 1759–1769. [Google Scholar] [CrossRef] [PubMed]
- Shogbesan, O.; Poudel, D.R.; Victor, S.; Jehangir, A.; Fadahunsi, O.; Shogbesan, G.; Donato, A. A systematic review of the efficacy and safety of fecal microbiota transplant for Clostridium difficile infection in immunocompromised patients. Can. J. Gastroenterol. Hepatol. 2018, 2018, 1394379. [Google Scholar] [CrossRef] [PubMed]

| Target Antigen | Advantages | Disadvantages |
|---|---|---|
| TcdA and TcdB | ||
| C. difficile membrane preparation |
| |
| SlpA |
|
|
| Cwp84 | ||
| Cwp66 |
| |
| CD0873 |
| |
| GroEL |
|
|
| Fbp68 |
| |
| FliC and FliD |
| |
| CdeC and CdeM |
| |
| BclA2 |
| |
| Bcla3 |
| |
| Bcla1 | ||
| SleC |
| |
| CotA |
| |
| Non-toxigenic C. difficile (NTCD) |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heuler, J.; Chandra, H.; Sun, X. Mucosal Vaccination Strategies against Clostridioides difficile Infection. Vaccines 2023, 11, 887. https://doi.org/10.3390/vaccines11050887
Heuler J, Chandra H, Sun X. Mucosal Vaccination Strategies against Clostridioides difficile Infection. Vaccines. 2023; 11(5):887. https://doi.org/10.3390/vaccines11050887
Chicago/Turabian StyleHeuler, Joshua, Harish Chandra, and Xingmin Sun. 2023. "Mucosal Vaccination Strategies against Clostridioides difficile Infection" Vaccines 11, no. 5: 887. https://doi.org/10.3390/vaccines11050887
APA StyleHeuler, J., Chandra, H., & Sun, X. (2023). Mucosal Vaccination Strategies against Clostridioides difficile Infection. Vaccines, 11(5), 887. https://doi.org/10.3390/vaccines11050887





