Surviving COVID-19: Biopsychosocial Impacts, Death Anxiety, and Coping Strategies
Abstract
:1. Introduction
2. Literature Review
2.1. Contextual Models to Examine COVID-19 and Its Implications
2.2. Anxiety and Coping Strategies in the Context of COVID-19
3. Materials and Methods
3.1. The Key Concepts, Research Method, and Sampling Strategy
3.2. Measures
3.2.1. Demographic Information Sheet
3.2.2. The Biopsychosocial Symptoms Questionnaire
3.2.3. The Death Anxiety Scale
3.2.4. The Brief COPE Scale
3.3. Statistical Analysis
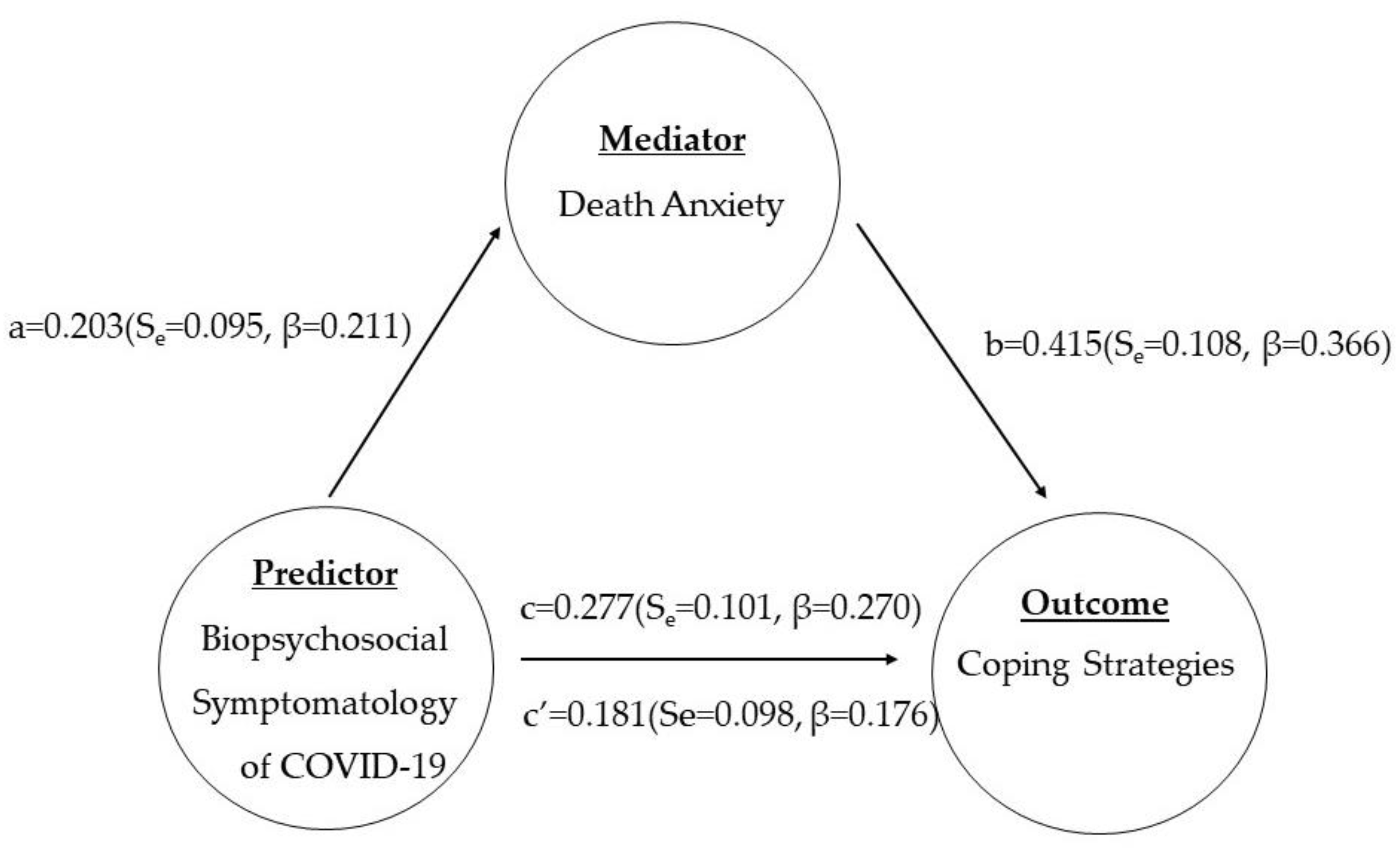
4. Results
4.1. Descriptive Analysis of Study Variables
4.2. Correlation between Variables
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Anderson, M.; Mckee, M.; Mossialos, E. Developing a sustainable exit strategy for COVID-19: Health, economic and public policy implications. J. R. Soc. Med. 2020, 113, 176–178. [Google Scholar] [CrossRef] [PubMed]
- Parry, L.J.; Asenbaum, H.; Ercan, S.A. Democracy in flux: A systemic view on the impact of COVID-19. Transform. Gov. People Process Policy 2021, 15, 197–205. [Google Scholar] [CrossRef]
- Renda, A. COVID-19 and privacy: A European dilemma. Digit. Policy Regul. Gov. 2022, 24, 109–117. [Google Scholar] [CrossRef]
- Kundu, S.; Latif, M.; Hořejší, P. Using DES to Improve the Efficiency of a COVID-19 Vaccination Centre. In RIIFORUM 2022: Research and Innovation Forum 2022; Visvizi, A., Troisi, O., Grimaldi, M., Eds.; Springer Proceedings in Complexity; Springer: Cham, Switzerland, 2023. [Google Scholar] [CrossRef]
- Wang, J.; Peng, Y.; Xu, H.; Cui, Z.; Williams, R.O. The COVID-19 Vaccine Race: Challenges and Opportunities in Vaccine Formulation. AAPS Pharmscitech 2020, 21, 225. [Google Scholar] [CrossRef]
- Ferreras-Garcia, R.; Sales-Zaguirre, J.; Serradell-López, E. Generic Competences in Higher Education after COVID-19 Pandemic. In RIIFORUM 2022: Research and Innovation Forum 2022; Visvizi, A., Troisi, O., Grimaldi, M., Eds.; Springer Proceedings in Complexity; Springer: Cham, Switzerland, 2023. [Google Scholar] [CrossRef]
- Daniela, L.; Visvizi, A. (Eds.) Remote Learning in Times of Pandemic: Issues, Implications and Best Practice; Routledge: London, UK; New York, NY, USA, 2021. [Google Scholar]
- Engel, G.L. The need for a new medical model: A challenge for biomedicine. Science 1977, 196, 129–136. [Google Scholar] [CrossRef]
- Wainwright, T.W.; Low, M. Why the biopsychosocial model needs to be the underpinning philosophy in rehabilitation pathways for patients recovering from COVID-19. Integr. Healthc. J. 2020, 2, e000043. [Google Scholar] [CrossRef]
- Galbadage, T.; Peterson, B.M.; Wang, D.C.; Wang, J.S.; Gunasekera, R.S.; Richard, S. Biopsychosocial and Spiritual Implications of Patients With COVID-19 Dying in Isolation. Front. Psychol. 2020, 11, 588623. [Google Scholar] [CrossRef]
- Kop, W.J. Biopsychosocial Processes of Health and Disease During the COVID-19 Pandemic. Psychosom. Med. 2021, 83, 304–308. [Google Scholar] [CrossRef]
- Guaracha-Basáñez, G.A.; Contreras-Yáñez, I.; Hernández-Molina, G.; Estrada-González, V.A.; Pacheco-Santiago, L.D.; Valverde-Hernández, S.S.; Galindo-Donaire, J.R.; Peláez-Ballestas, I.; Pascual-Ramos, V. Quality of life of patients with rheumatic diseases during the COVID-19 pandemic: The biopsychosocial path. PLoS ONE 2022, 17, e0262756. [Google Scholar] [CrossRef]
- Brailovskaia, J.; Margraf, J. The relationship between burden caused by coronavirus (COVID-19), addictive social media use, sense of control and anxiety. Comput. Hum. Behav. 2021, 119, 106720. [Google Scholar] [CrossRef]
- Brailovskaia, J.; Truskauskaite-Kuneviciene, J.; Margraf, J.; Kazlauskas, E. Coronavirus (COVID-19) outbreak: Addictive social media use, depression, anxiety and stress in quarantine—An exploratory study in Germany and Lithuania. J. Affect. Disord. Rep. 2021, 5, 100182. [Google Scholar] [CrossRef]
- Güldal, Ş.; Kılıçoğlu, N.; Kasapoğlu, F. Psychological Flexibility, Coronavirus Anxiety, Humor and Social Media Addiction During COVID-19 Pandemic in Turkey. Int. J. Adv. Couns. 2022, 44, 220–242. [Google Scholar] [CrossRef]
- Qi, R.; Chen, W.; Liu, S.; Thompson, P.M.; Zhang, L.J.; Xia, F.; Cheng, F.; Hong, A.; Surento, W.; Luo, S.; et al. Psychological morbidities and fatigue in patients with confirmed COVID-19 during disease outbreak: Prevalence and associated biopsychosocial risk factors. medRxiv 2020. [Google Scholar] [CrossRef]
- Lahav, Y. Psychological distress related to COVID-19—The contribution of continuous traumatic stress. J. Affect. Disord. 2020, 277, 129–137. [Google Scholar] [CrossRef]
- Tuason, M.T.; Güss, C.D.; Boyd, L. Thriving during COVID-19: Predictors of psychological well-being and ways of coping. PLoS ONE 2021, 16, e0248591. [Google Scholar] [CrossRef]
- McLaren, N. A Critical Review of the Biopsychosocial Model. Aust. N. Z. J. Psychiatry 1998, 32, 86–92. [Google Scholar] [CrossRef]
- Suls, J.; Rothman, A. Evolution of the Biopsychosocial Model: Prospects and Challenges for Health Psychology. Health Psychol. 2004, 23, 119–125. [Google Scholar] [CrossRef]
- Ghaemi, S. The rise and fall of the biopsychosocial model. Br. J. Psychiatry 2009, 195, 3–4. [Google Scholar] [CrossRef] [Green Version]
- Adler, R.H. Engel’s biopsychosocial model is still relevant today. J. Psychosom. Res. 2009, 67, 607–611. [Google Scholar] [CrossRef]
- Kelly, M.M.; Li, K. Poverty, Toxic Stress, and Education in Children Born Preterm. Nurs. Res. 2019, 68, 275–284. [Google Scholar] [CrossRef]
- Kliegman, R.M. Developmental and Behavioral Theories. In Nelson Textbook of Pediatrics; Kliegman, R.M., Geme, J., Eds.; Elsevier: London, UK; New York, NY, USA, 2019. [Google Scholar]
- Huang, C.-C.; Chen, Y.; Cheung, S. Early childhood exposure to intimate partner violence and teen depression symptoms in the U.S. Health Soc. Care Community 2021, 29, e47–e55. [Google Scholar] [CrossRef] [PubMed]
- Garner, A.S. Thinking Developmentally: The Next Evolution in Models of Health. J. Dev. Behav. Pediatr. 2016, 37, 579–584. [Google Scholar] [CrossRef] [PubMed]
- Herman-Smith, R. Intimate Partner Violence Exposure in Early Childhood: An Ecobiodevelopmental Perspect. Health Soc. Work. 2013, 38, 231–239. [Google Scholar] [CrossRef] [PubMed]
- Voith, L.A.; Hamler, T.; Francis, M.W.; Lee, H.; Korsch-Williams, A. Using a Trauma-Informed, Socially Just Research Framework with Marginalized Populations: Practices and Barriers to Implementation. Soc. Work. Res. 2020, 44, 169–181. [Google Scholar] [CrossRef]
- Banerjee, D.; Kosagisharaf, J.R.; Sathyanarayana Rao, T.S. ‘The dual pandemic’ of suicide and COVID-19: A biopsychosocial narrative of risks and prevention. Psychiatry Res. 2021, 295, 113577. [Google Scholar] [CrossRef]
- Ali, J.S. COVID-19 pandemic is a worldwide typical Biopsychosocial crisis. J. Ideas Health 2020, 3, 152–154. [Google Scholar] [CrossRef]
- Bourgonje, A.R.; Abdulle, A.E.; Timens, W.; Hillebrands, J.L.; Navis, G.J.; Gordijn, S.J.; Bolling, M.C.; Dijkstra, G.; Voors, A.A.; Osterhaus, A.D.; et al. Angiotensin-converting enzyme 2 (ACE2), SARS-CoV-2 and the pathophysiology of coronavirus disease 2019 (COVID-19). J. Pathol. 2020, 251, 228–248. [Google Scholar] [CrossRef]
- Wong, S.Y.S.; Zhang, D.; Sit, R.W.S.; Yip, B.H.K.; Chung, R.Y.; Wong, C.K.M.; Chan, D.C.C.; Sun, W.; Kwok, K.O.; Mercer, S.W. Impact of COVID-19 on loneliness, mental health, and health service utilization: A prospective cohort study of older adults with multimorbidity in primary care. Br. J. Gen. Pract. 2020, 70, 817–824. [Google Scholar] [CrossRef]
- Méndez, R.; Balanzá-Martínez, V.; Luperdi, S.C.; Estrada, I.; Latorre, A.; González-Jiménez, P.; Feced, L.; Bouzas, L.; Yépez, K.; Ferrando, A.; et al. Short-term neuropsychiatric outcomes and quality of life in COVID-19 survivors. J. Int. Med. 2021, 290, 621–631. [Google Scholar] [CrossRef]
- Monaghan, L.F. Coronavirus (COVID-19), pandemic psychology and the fractured society: A sociological case for critique, foresight and action. Sociol. Health Illn. 2020, 42, 1982–1995. [Google Scholar] [CrossRef]
- Waters, L.; Algoe, S.B.; Dutton, J.; Emmons, R.; Fredrickson, B.L.; Heaphy, E.; Moskowitz, J.T.; Neff Niemiec, K.R.; Pury, C.; Steger, M. Positive psychology in a pandemic: Buffering, bolstering, and building mental health. J. Posit. Psychol. 2022, 17, 303–323. [Google Scholar] [CrossRef]
- Spoorthy, M.S.; Pratapa, S.K.; Mahant, S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic—A review. Asian J. Psychiatry 2020, 51, 102119. [Google Scholar] [CrossRef]
- Li, J.B.; Yang, A.; Dou, K.; Cheung, R.Y.M. Self-control moderates the association between the perceived severity of the coronavirus disease 2019 (COVID-19) and mental health problems among the Chinese public. Int. J. Environ. Res. Public Health 2020, 17, 4820. [Google Scholar] [CrossRef]
- Becker, E. The Denial of Death; Free Press: New York, NY, USA, 1973. [Google Scholar]
- Menzies, R.E.; Menzies, R.G.; Iverach, L. Curing the Dread of Death: Theory, Research and Practice; Australian Academic Press: Samford Valley, QLD, Australia, 2018; ISBN 9781925644111. [Google Scholar]
- Greenberg, J.; Solomon, S.; Pyszczynski, T. Terror Management Theory of Self-Esteem and Cultural Worldviews: Empirical Assessments and Conceptual Refinements. Adv. Exp. Soc. Psychol. 1997, 29, 61–139. [Google Scholar] [CrossRef]
- Shakil, M.; Ashraf, F.; Muazzam, A.; Amjad, M.; Javed, S. Work status, death anxiety, and psychological distress during COVID-19 pandemic: Implications of the terror management theory. Death Stud. 2021, 46, 1100–1105. [Google Scholar] [CrossRef]
- Witkowski, J. Coping and attitudes toward dying and death in German adults. OMEGA J. Death Dying 2016, 72, 316–339. [Google Scholar] [CrossRef]
- Abedini, S.M.; Montazeri, S.; Khalatbari, J. Comparison between Styles of Coping with Stress in Patients with Multiple Sclerosis and Healthy people in the East of Mazandaran. J. Maz. Univ. Med. Sci. 2012, 22, 71–77. [Google Scholar]
- Lazarus, R.; Folkman, S. Coping and Adaptation; Gilford Press: New York, NY, USA, 1985. [Google Scholar]
- Partouche-Sebban, J.; Vessal, S.R.; Sorio, R.; Castellano, S.; Khelladi, I.; Orhan, M.A. How death anxiety influences coping strategies during the COVID-19 pandemic: Investigating the role of spirituality, national identity, lockdown, and trust. J. Mark. Manag. 2021, 37, 1815–1839. [Google Scholar] [CrossRef]
- Menzies, R.E.; Menzies, R.G. Death anxiety in the time of COVID-19: Theoretical explanations and clinical implications. Cogn. Behav. Ther. 2020, 13, e19. [Google Scholar] [CrossRef]
- Griffith, D.M.; Sharma, G.; Holliday, C.S.; Enyia, O.K.; Valliere, M.; Semlow, A.R.; Stewart, E.; Blumenthal, R.S. Men and COVID-19: A biopsychosocial approach to understanding sex differences in mortality and recommendations for practice and policy interventions. Prev. Chronic Dis. 2020, 17, E63. [Google Scholar] [CrossRef]
- Leonardi, M.; Lee, H.; Van der, V.S.; Maribo, T.; Cuenot, M.; Simon, L.; Paltamaa, J.; Maart, S.; Tucker, C.; Besstrashnova, Y.; et al. Avoiding the banality of evil in times of COVID-19: Thinking differently with a biopsychosocial perspective for future health and social policies development. SN Compr. Med. 2020, 2, 1758–1760. [Google Scholar] [CrossRef] [PubMed]
- Fernández-de-las-Peñas, C.; Palacios-Ceña, D.; Gómez-Mayordomo, V.; Florencio, L.L.; Cuadrado, M.L.; Plaza-Manzano, G.; Navarro-Santana, M. Prevalence of post-COVID-19 symptoms in hospitalized and non-hospitalized COVID-19 survivors: A systematic review and meta-analysis. Eur. J. Intern. Med. 2021, 92, 55–70. [Google Scholar] [CrossRef] [PubMed]
- Mazza, M.G.; De Lorenzo, R.; Conte, C.; Poletti, S.; Vai, B.; Bollettini, I.; Melloni, E.M.T.; Furlan, R.; Ciceri, F.; Rovere-Querini, P.; et al. Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors. Brain Behav. Immun. 2020, 89, 594–600. [Google Scholar] [CrossRef] [PubMed]
- Naseem, F. Biopsychosocial Symptoms Questionnaire. Unpublished. Master’s Thesis, Lahore College for Women University, Lahore, Pakistan, 2020. [Google Scholar]
- Liaqat, A. Development of Death Anxiety Scale; [Unpublished Article]; Lahore College for Women University: Lahore, Pakistan, 2019. [Google Scholar]
- Carver, C.S. You want to measure coping, but your protocol’s too long: Consider the brief COPE. Int. J. Behav. Med. 1997, 4, 92–100. [Google Scholar] [CrossRef]
- Vindegaard, N.; Benros, M.E. COVID-19 pandemic and mental health consequences: A systematic review of the current evidence. Brain Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef]
- Zhang, Q.; Zheng, R.; Fu, Y.; Mu, Q.; Li, J. Mental health consequences during alerting situations and recovering to a new normal of coronavirus epidemic in 2019: A cross-sectional study based on the affected population. BMC Public Health 2021, 21, 1499. [Google Scholar] [CrossRef]
- Özgüç, S.; Kaplan, S.E.; Tanriverdi, D. Death anxiety associated with coronavirus (COVID-19) disease: A systematic review and meta- analysis. Omega 2021. Online ahead of print. [Google Scholar] [CrossRef]
- Nia, H.S.; Soleimani, M.A.; Ebadi, A.; Taghipour, B.; Zera’Tgar, L.; Shahidifar, S. The relationship between spiritual intelligence, spiritual well-being, and death anxiety among Iranian veterans. J. Mil. Med. 2017, 19, 336–343. [Google Scholar]
- Freh, F.M.; Chung, M.C. Post-traumatic stress disorder and death anxiety among Iraqi civilians exposed to a suicide car bombing: The role of religious coping and attachment. J. Ment. Health 2021, 30, 743–750. [Google Scholar] [CrossRef]
- Ghanem, I.; Castelo, B.; Jimenez-Fonseca, P.; Carmona-Bayonas, A.; Higuera, O.; Beato, C.; García, T.; Hernández, R.; Calderon, C. Coping strategies and depressive symptoms in cancer patients. Clin. Transl. Oncol. 2019, 22, 330–336. [Google Scholar] [CrossRef]
- Loughan, A.R.; Husain, M.; Ravyts, S.G.; Willis, K.D.; Braun, S.E.; Brechbiel, J.K.; Aslanzadeh, F.J.; Rodin, G.; Svikis, D.S.; Thacker, L. Death anxiety in patients with primary brain tumor: Measurement, prevalence, and determinants. Palliat. Support. Care 2021, 19, 672–680. [Google Scholar] [CrossRef]
- Joaquim, R.M.; Pinto AL, C.B.; Guatimosim, R.F.; de Paula, J.J.; Costa, D.S.; Diaz, A.P.; da Silva, A.G.; Pinheiro, M.I.; Serpa, A.L.; Miranda, D.M.; et al. Bereavement and psychological distress during COVID-19 pandemics: The impact of death experience on mental health. Curr. Res. Behav. Sci. 2021, 2, 100019. [Google Scholar] [CrossRef]
- Fereidooni, R.; Mootz, J.; Sabaei, R.; Khoshnood, K.; Heydari, S.T.; Moradian, M.J.; Taherifard, E.; Nasirian, M.; Vardanjani, H.M. The COVID-19 pandemic, socioeconomic effects, and intimate partner violence against women: A population-based cohort study in Iran. SSRN Electron. J. 2021. [Google Scholar] [CrossRef]
- Sheida, S.S.; Ahmad, A.; Alireza, A.; Reza, M.M.; Bagher, G.B. Relationship of Attachment Styles to God and Depression with Death Anxiety as a Mediator among Women with Breast Cancer. Relig. Health 2019, 7, 1–11. [Google Scholar]
- Salopek-Žiha, D.; Hlavati, M.; Gvozdanović, Z.; Gašić, M.; Placento, H.; Jakić, H.; Klapan, D.; Šimić, H. Differences in distress and coping with the COVID-19 stressor in nurses and physicians. Psychiatr. Danub. 2020, 32, 287–293. [Google Scholar] [CrossRef]
- Tanhan, A.; Yavuz, K.F.; Young, J.S.; Nalbant, A.; Arslan, G.; Yıldırım, M.; Çiçek, İ. A Proposed Framework Based on Literature Review of Online Contextual Mental Health Services to Enhance Wellbeing and Address Psychopathology During COVID-19. Electron. J. Gen. Med. 2020, 17, em254. [Google Scholar] [CrossRef]
- Mukaetova-Ladinska, E.B.; Kronenberg, G. Psychological and neuropsychiatric implications of COVID-19. Eur. Arch. Psychiatry Clin. Neurosci. 2021, 271, 235–248. [Google Scholar] [CrossRef]
| Variables | F | % |
|---|---|---|
| Gender | ||
| Male | 53 | 52.5 |
| Female | 47 | 46.5 |
| Marital Status | ||
| Married | 48 | 47.5 |
| Unmarried | 50 | 49.5 |
| Widow | 2 | 2.0 |
| Number of symptoms experienced by COVID-19 survivors | ||
| One symptom | 9 | 8.9 |
| Two symptoms | 8 | 7.9 |
| Three symptoms | 11 | 10.9 |
| Four symptoms | 25 | 24.8 |
| Five symptoms | 46 | 45.5 |
| Six symptoms | 1 | 1.0 |
| Variables | Coping Strategies | Death Anxiety | Biopsychosocial Symptoms of COVID-19 |
|---|---|---|---|
| Coping strategies | 1 | −0.063 * | −0.096 |
| Death anxiety | 1 | 0.025 ** | |
| Biopsychosocial symptoms of COVID-19 | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Muazzam, A.; Naseem, F.; Shakil, M.; Visvizi, A.; Klemens, J. Surviving COVID-19: Biopsychosocial Impacts, Death Anxiety, and Coping Strategies. Vaccines 2023, 11, 705. https://doi.org/10.3390/vaccines11030705
Muazzam A, Naseem F, Shakil M, Visvizi A, Klemens J. Surviving COVID-19: Biopsychosocial Impacts, Death Anxiety, and Coping Strategies. Vaccines. 2023; 11(3):705. https://doi.org/10.3390/vaccines11030705
Chicago/Turabian StyleMuazzam, Amina, Faiqa Naseem, Muneeba Shakil, Anna Visvizi, and Jolanta Klemens. 2023. "Surviving COVID-19: Biopsychosocial Impacts, Death Anxiety, and Coping Strategies" Vaccines 11, no. 3: 705. https://doi.org/10.3390/vaccines11030705
APA StyleMuazzam, A., Naseem, F., Shakil, M., Visvizi, A., & Klemens, J. (2023). Surviving COVID-19: Biopsychosocial Impacts, Death Anxiety, and Coping Strategies. Vaccines, 11(3), 705. https://doi.org/10.3390/vaccines11030705










