Not All Conservatives Are Vaccine Hesitant: Examining the Influence of Misinformation Exposure, Political Ideology, and Flu Vaccine Acceptance on COVID-19 Vaccine Hesitancy
Abstract
1. Introduction
2. Materials and Methods
2.1. Data
2.2. Measures
2.3. Covariates
2.4. Analysis
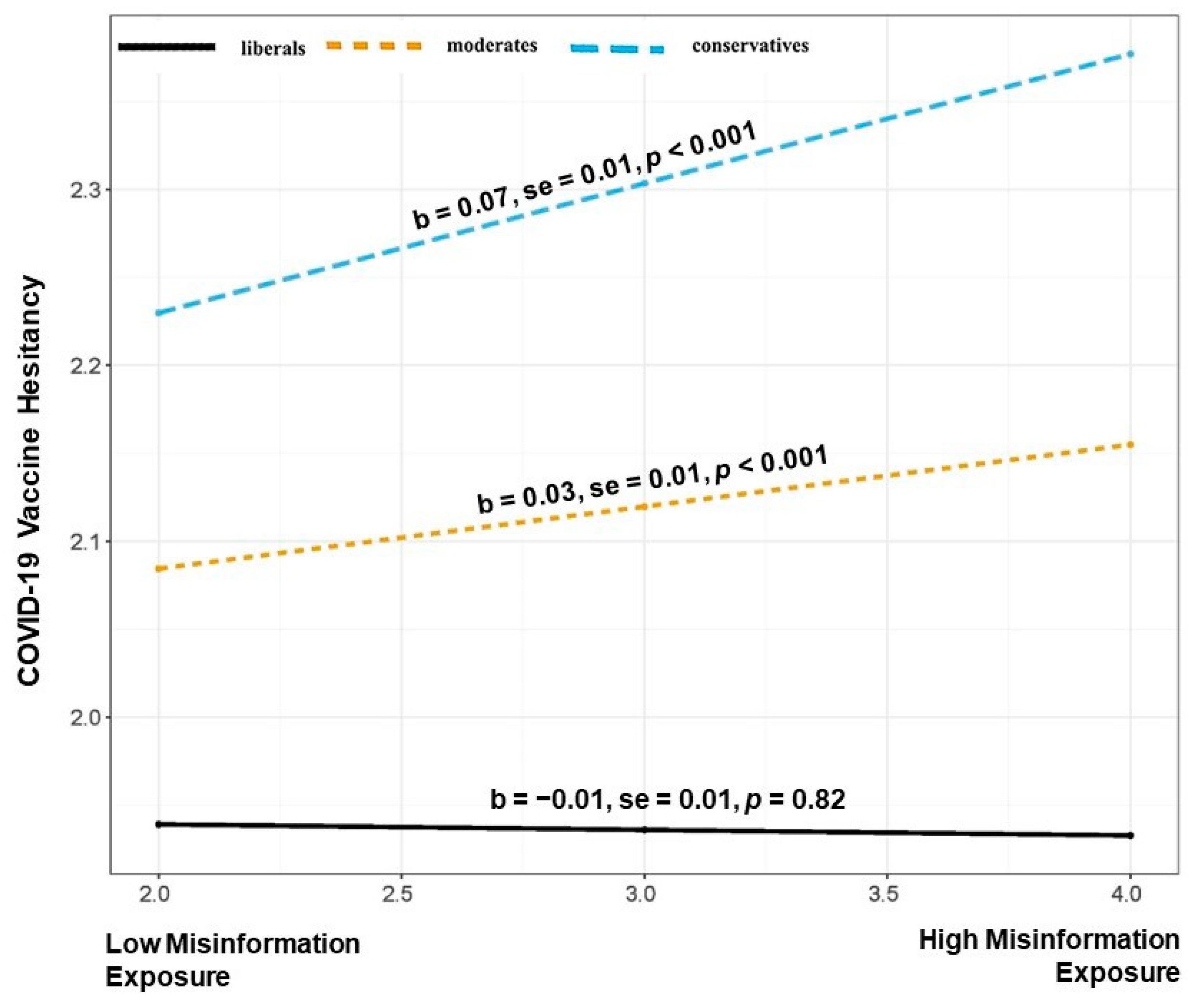
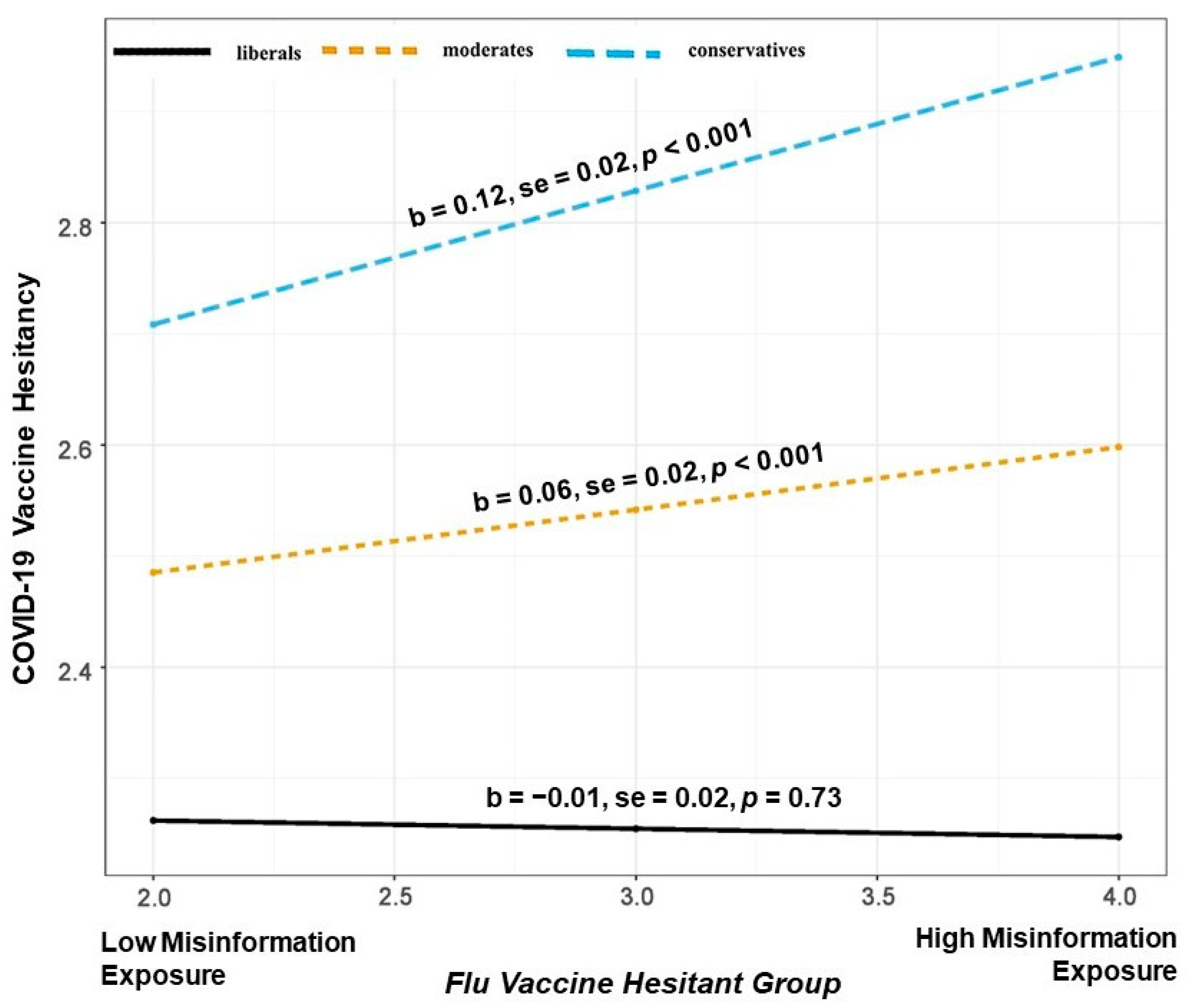
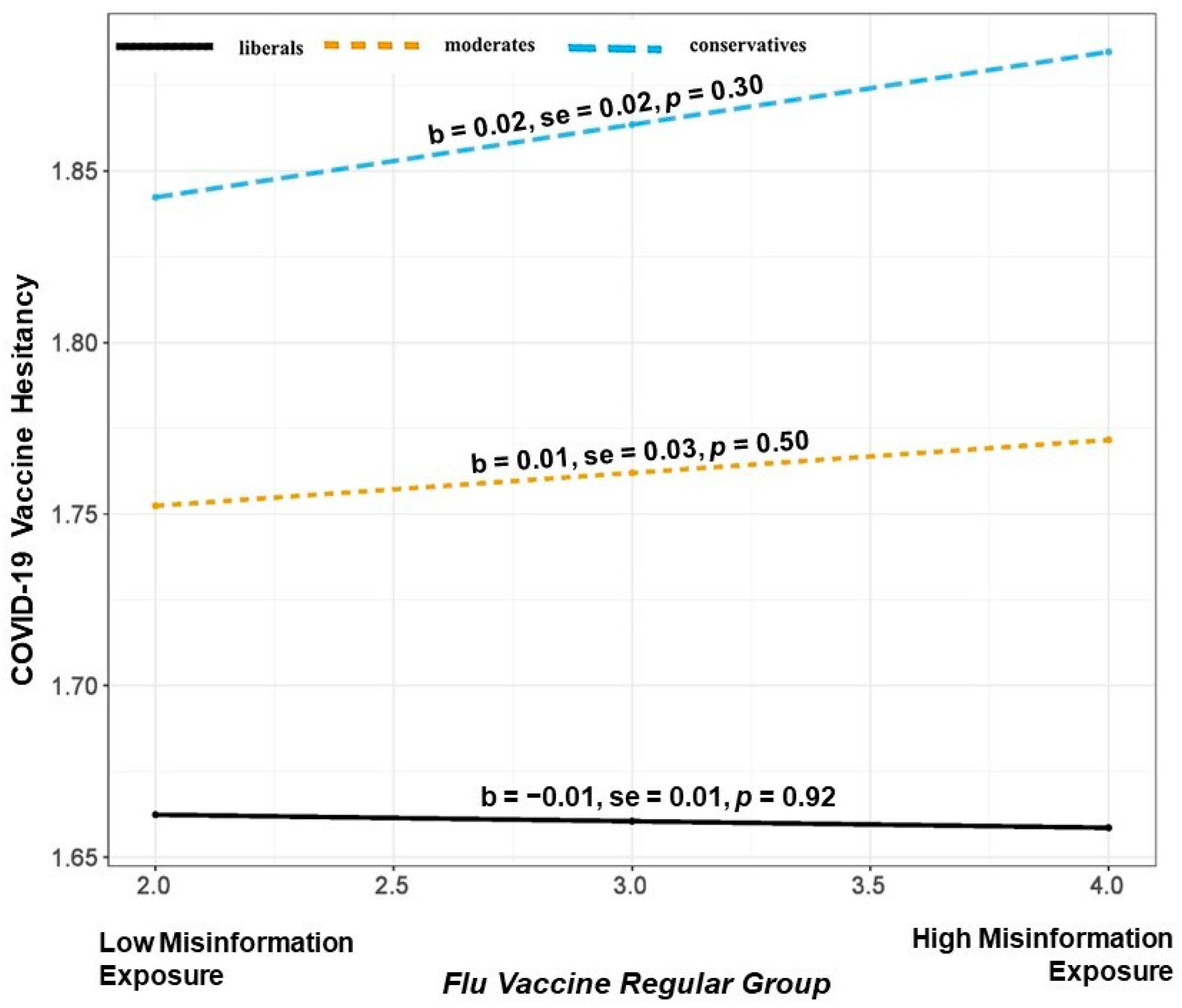
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Coronavirus Disease (COVID-19) Advice for the Public. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public#:~:text=If%20COVID%2D19%20is%20spreading,a%20bent%20elbow%20or%20tissue (accessed on 14 January 2023).
- CDC COVID Data Tracker. Centers for Disease Control and Prevention. Available online: https://covid.cdc.gov/covid-data-tracker/#datatracker-home (accessed on 15 January 2023).
- MacDonald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Courtney, D.S.; Bliuc, A.M. Antecedents of Vaccine Hesitancy in WEIRD and East Asian Contexts. Front. Psych. 2021, 12, 747721. [Google Scholar] [CrossRef]
- Wang, Y.; Zhang, X. Influence of Parental Psychological Flexibility on Pediatric COVID-19 Vaccine Hesitancy: Mediating Role of Self-Efficacy and Coping Style. Front. Psych. 2021, 12, 783401. [Google Scholar] [CrossRef]
- Troiano, G.; Nardi, A. Vaccine hesitancy in the era of COVID-19. Public Health 2021, 194, 245–251. [Google Scholar] [CrossRef]
- Wood, S.; Schulman, K. Beyond politics—Promoting Covid-19 vaccination in the United States. N. Eng. J. Med. 2021, 384, e23. [Google Scholar] [CrossRef]
- Ahmed, S.; Rasul, M.E.; Cho, J. Social media news use induces COVID-19 vaccine hesitancy through skepticism regarding its efficacy: A longitudinal study from the United States. Front. Psych. 2022, 13, 900386. [Google Scholar] [CrossRef] [PubMed]
- Loomba, S.; de Figueiredo, A.; Piatek, S.J.; de Graaf, K.; Larson, H.J. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nat. Hum. Behav. 2021, 5, 337–348. [Google Scholar] [CrossRef]
- Chen, Q.; Min, C.; Zhang, W.; Wang, G.; Ma, X.; Evans, R. Unpacking the black box: How to promote citizen engagement through government social media during the COVID-19 crisis. Computers Hum. Behav. 2020, 110, 106380. [Google Scholar] [CrossRef]
- Karami, A.; Zhu, M.; Goldschmidt, B.; Boyajieff, H.R.; Najafabadi, M.M. COVID-19 vaccine and social media in the US: Exploring emotions and discussions on Twitter. Vaccines 2021, 9, 1059. [Google Scholar] [CrossRef]
- Tsao, S.F.; Chen, H.; Tisseverasinghe, T.; Yang, Y.; Li, L.; Butt, Z.A. What social media told us in the time of COVID-19: A scoping review. Lancet Digit. Health 2021, 3, e175–e194. [Google Scholar] [CrossRef]
- Stevens, H.; Rasul, M.E.; Oh, Y.J. Emotions and Incivility in Vaccine Mandate Discourse: Natural Language Processing Insights. JMIR Infodemiology 2022, 2, e37635. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, W.; Vidal-Alaball, J.; Downing, J.; Seguí, F.L. COVID-19 and the 5G conspiracy theory: Social network analysis of Twitter data. J. Med. Internet Res. 2020, 22, e19458. [Google Scholar] [CrossRef]
- Cinelli, M.; Quattrociocchi, W.; Galeazzi, A.; Valensise, C.M.; Brugnoli, E.; Schmidt, A.L.; Zola, P.; Zollo, F.; Scala, A. The COVID-19 social media infodemic. Sci. Rep. 2020, 10, 1–10. [Google Scholar] [CrossRef]
- Ferrara, E.; Cresci, S.; Luceri, L. Misinformation, manipulation, and abuse on social media in the era of COVID-19. J. Comput. Soc. Sci. 2020, 3, 271–277. [Google Scholar] [CrossRef]
- Ahmed, S.; Rasul, M.E. Social Media News Use and COVID-19 Misinformation Engagement: Survey Study. J. Med. Internet Res. 2022, 24, e38944. [Google Scholar] [CrossRef]
- Hart, P.S.; Chinn, S.; Soroka, S. Politicization and polarization in COVID-19 news coverage. Sci. Commun. 2020, 42, 679–697. [Google Scholar] [CrossRef]
- Motta, M.; Stecula, D.; Farhart, C. How right-leaning media coverage of COVID-19 facilitated the spread of misinformation in the early stages of the pandemic in the US. Can. J. Political Sci. 2020, 53, 335–342. [Google Scholar] [CrossRef]
- Dechêne, A.; Stahl, C.; Hansen, J.; Wänke, M. The truth about the truth: A meta-analytic review of the truth effect. Personal. Soc. Psych. Rev. 2010, 14, 238–257. [Google Scholar] [CrossRef] [PubMed]
- Pennycook, G.; Cannon, T.D.; Rand, D.G. Prior exposure increases perceived accuracy of fake news. J. Exp. Psych. Gen. 2018, 147, 1865. [Google Scholar] [CrossRef]
- Kricorian, K.; Civen, R.; Equils, O. COVID-19 vaccine hesitancy: Misinformation and perceptions of vaccine safety. Hum. Vaccines Immunother. 2022, 18, 1950504. [Google Scholar] [CrossRef] [PubMed]
- Neely, S.R.; Eldredge, C.; Ersing, R.; Remington, C. Vaccine hesitancy and exposure to misinformation: A survey analysis. J. Gen. Intern. Med. 2022, 37, 179–187. [Google Scholar] [CrossRef] [PubMed]
- Milligan, S. The Political Divide over the Coronavirus. US News & World Report. Available online: https://www.usnews.com/news/politics/articles/2020-03-18/the-politicaldivide-over-the-coronavirus (accessed on 18 January 2023).
- Roberts, D. Partisanship Is the Strongest Predictor of Coronavirus Response. Vox. Available online: https://www.vox.com/science-and-health/2020/3/31/21199271/coronavirus-in-us-trump-republicans-democrats-survey-epistemic-crisis (accessed on 18 January 2023).
- Van Green, T.; Tyson, A. 5 Facts about Partisan Reactions to COVID-19 in the U.S. Pew Research Center. Available online: https://www.pewresearch.org/facttank/2020/04/02/5-facts-about-partisan-reactions-to-covid-19-in-the-u-s/ (accessed on 19 January 2023).
- Allcott, H.; Boxell, L.; Conway, J.; Gentzkow, M.; Thaler, M.; Yang, D. Polarization and public health: Partisan differences in social distancing during the coronavirus pandemic. J. Public Econ. 2020, 191, 104254. [Google Scholar] [CrossRef]
- Roozenbeek, J.; Schneider, C.R.; Dryhurst, S.; Kerr, J.; Freeman, A.L.; Recchia, G.; van der Bles, A.M.; van der Linden, S. Susceptibility to misinformation about COVID-19 around the world. R. Soc. Open. Sci. 2020, 7, 201199. [Google Scholar] [CrossRef] [PubMed]
- Stevens, H.; Palomares, N.A. Constituents’ Inferences of Local Governments’ Goals and the Relationship Between Political Party and Belief in COVID-19 Misinformation: Cross-sectional Survey of Twitter Followers of State Public Health Departments. JMIR Infodemiology 2022, 2, e29246. [Google Scholar] [CrossRef]
- Slothuus, R.; de Vreese, C.H. Political parties, motivated reasoning, and issue framing effects. J. Politics 2010, 72, 630–645. [Google Scholar] [CrossRef]
- Taber, C.S.; Cann, D.; Kucsova, S. The motivated processing of political arguments. Pol. Behav. 2009, 31, 137–155. [Google Scholar] [CrossRef]
- Fridman, A.; Gershon, R.; Gneezy, A. COVID-19 and vaccine hesitancy: A longitudinal study. PLoS ONE 2021, 16, e0250123. [Google Scholar] [CrossRef]
- Khubchandani, J.; Sharma, S.; Price, J.H.; Wiblishauser, M.J.; Sharma, M.; Webb, F.J. COVID-19 vaccination hesitancy in the United States: A rapid national assessment. J. Community Health 2021, 46, 270–277. [Google Scholar] [CrossRef]
- Kreps, S.E.; Goldfarb, J.L.; Brownstein, J.S.; Kriner, D.L. The relationship between US adults’ misconceptions about COVID-19 vaccines and vaccination preferences. Vaccines 2021, 9, 901. [Google Scholar] [CrossRef]
- Chen, E.; Chang, H.; Rao, A.; Lerman, K.; Cowan, G.; Ferrara, E. COVID-19 misinformation and the 2020 U.S. presidential election. Harv. Kennedy Sch. (HKS) Misinfo. Rev. 2021. [Google Scholar] [CrossRef]
- Grech, V.; Borg, M. Influenza vaccination in the COVID-19 era. Early Hum. Dev. 2020, 148, 105116. [Google Scholar] [CrossRef]
- Gostin, L.O.; Salmon, D.A. The dual epidemics of COVID-19 and influenza: Vaccine acceptance, coverage, and mandates. Jama 2020, 324, 335–336. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC). Routine and Influenza Immunization Services during the COVID-19 Pandemic: Interim Guidance; Centers for Disease Control and Prevention: Atlanta, GA, USA. Available online: https://www.cdc.gov/vaccines/pandemic-guidance/index.html (accessed on 19 January 2023).
- Costantino, C.; Ledda, C.; Squeri, R.; Restivo, V.; Casuccio, A.; Rapisarda, V.; Graziano, G.; Alba, D.; Cimino, L.; Conforto, A.; et al. Attitudes and perception of healthcare workers concerning influenza vaccination during the 2019/2020 season: A survey of Sicilian university hospitals. Vaccines 2020, 8, 686. [Google Scholar] [CrossRef]
- Pastorino, R.; Villani, L.; Mariani, M.; Ricciardi, W.; Graffigna, G.; Boccia, S. Impact of COVID-19 pandemic on flu and COVID-19 vaccination intentions among university students. Vaccines 2021, 9, 70. [Google Scholar] [CrossRef]
- Caserotti, M.; Girardi, P.; Rubaltelli, E.; Tasso, A.; Lotto, L.; Gavaruzzi, T. Associations of COVID-19 risk perception with vaccine hesitancy over time for Italian residents. Soc. Sci. Med. 2021, 272, 113688. [Google Scholar] [CrossRef]
- Nyhan, B.; Reifler, J. Does correcting myths about the flu vaccine work? An experimental evaluation of the effects of corrective information. Vaccine 2015, 33, 459–464. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.; Madrid-Morales, D.; Tully, M. Social media, misinformation, and age inequality in online political engagement. J. Info. Tech. Politics 2022, 1–17. [Google Scholar] [CrossRef]
- Hameleers, M.; Brosius, A.; de Vreese, C.H. Whom to trust? Media exposure patterns of citizens with perceptions of misinformation and disinformation related to the news media. Europ. J. Commun. 2022, 37, 237–268. [Google Scholar] [CrossRef]
- Wasserman, H.; Madrid-Morales, D. An exploratory study of “fake news” and media trust in Kenya, Nigeria and South Africa. Afr. J. Stud. 2019, 40, 107–123. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Publi-Cations: New York, NY, USA, 2018; ISBN 9781462549030. [Google Scholar]
- Enders, A.M.; Uscinski, J.; Klofstad, C.; Stoler, J. On the relationship between conspiracy theory beliefs, misinformation, and vaccine hesitancy. PLoS ONE 2022, 17, e0276082. [Google Scholar] [CrossRef]
- Chou, W.Y.S.; Budenz, A. Considering emotion in COVID-19 vaccine communication: Addressing vaccine hesitancy and fostering vaccine confidence. Health Commun. 2020, 35, 1718–1722. [Google Scholar] [CrossRef]
- Bolsen, T.; Druckman, J.N.; Cook, F.L. The influence of partisan motivated reasoning on public opinion. Pol. Behav. 2014, 36, 235–262. [Google Scholar] [CrossRef]
- Druckman, J.N.; Bolsen, T. Framing, motivated reasoning, and opinions about emergent technologies. J. Commun. 2011, 61, 659–688. [Google Scholar] [CrossRef]
- Mourão, R.R.; Thorson, E.; Chen, W.; Tham, S.M. Media repertoires and news trust during the early Trump administration. Journal. Stud. 2018, 19, 1945–1956. [Google Scholar] [CrossRef]
- Tsfati, Y.; Cappella, J.N. Do people watch what they do not trust? Exploring the association between news media scepticism and exposure. Commun. Res. 2003, 30, 504–529. [Google Scholar] [CrossRef]
- Fletcher, R.; Park, S. The impact of trust in the news media on online news consumption and participation. Digit. Journal. 2017, 5, 1281–1299. [Google Scholar] [CrossRef]
- Egelhofer, J.L.; Lecheler, S. Fake news as a two-dimensional phenomenon: A framework and research agenda. Ann. Internat. Commun. Assoc. 2019, 43, 97–116. [Google Scholar] [CrossRef]
- Cadeddu, C.; Castagna, C.; Sapienza, M.; Lanza, T.E.; Messina, R.; Chiavarini, M.; Ricciardi, W.; de Waure, C. Understanding the determinants of vaccine hesitancy and vaccine confidence among adolescents: A systematic review. Hum. Vaccines Immunother. 2021, 17, 4470–4486. [Google Scholar] [CrossRef]
- Pennycook, G.; McPhetres, J.; Bago, B.; Rand, D.G. Beliefs about COVID-19 in Canada, the United Kingdom, and the United States: A novel test of political polarization and motivated reasoning. Personal. Soc. Psych. Bull. 2022, 48, 750–765. [Google Scholar] [CrossRef]
- Allen, M.S.; Iliescu, D.; Greiff, S. Single item measures in psychological science. Eur. J. Psychol. Assess. 2022, 38, 1–5. [Google Scholar] [CrossRef]
- Bergkvist, L.; Rossiter, J.R. The predictive validity of multiple-item versus single-item measures of the same constructs. J. Mark. Res. 2007, 44, 175–184. [Google Scholar] [CrossRef]
- Vraga, E.K.; Bode, L.; Tully, M. Creating news literacy messages to enhance expert corrections of misinformation on Twitter. Commun. Res. 2022, 49, 245–267. [Google Scholar] [CrossRef]

| Variable | COVID-19 Vaccine Hesitancy | |
|---|---|---|
| Β | Std. Error | |
| Protestant | −0.082 *** | 0.024 |
| Unaffiliated | −0.044 *** | 0.023 |
| Others | −0.056 *** | 0.033 |
| 30–49 Years Old | −0.004 | 0.026 |
| 50–64 Years Old | −0.075 *** | 0.028 |
| 65+ Years Old | −0.142 *** | 0.031 |
| Education | −0.006 | 0.006 |
| Income | −0.032 *** | 0.003 |
| Female | 0.157 *** | 0.018 |
| Others | 0.013 | 0.090 |
| Marital Status | 0.033 *** | 0.020 |
| Black | 0.087 *** | 0.029 |
| Asian | −0.056 *** | 0.039 |
| Mixed Race | 0.011 | 0.045 |
| Other Race | −0.026 ** | 0.042 |
| Political Ideology | 0.165 *** | 0.009 |
| Flu Vaccine Acceptance | −0.347 *** | 0.004 |
| Perceived Misinformation Exposure | 0.019 * | 0.010 |
| Total R2 | 0.252 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rasul, M.E.; Ahmed, S. Not All Conservatives Are Vaccine Hesitant: Examining the Influence of Misinformation Exposure, Political Ideology, and Flu Vaccine Acceptance on COVID-19 Vaccine Hesitancy. Vaccines 2023, 11, 586. https://doi.org/10.3390/vaccines11030586
Rasul ME, Ahmed S. Not All Conservatives Are Vaccine Hesitant: Examining the Influence of Misinformation Exposure, Political Ideology, and Flu Vaccine Acceptance on COVID-19 Vaccine Hesitancy. Vaccines. 2023; 11(3):586. https://doi.org/10.3390/vaccines11030586
Chicago/Turabian StyleRasul, Muhammad Ehab, and Saifuddin Ahmed. 2023. "Not All Conservatives Are Vaccine Hesitant: Examining the Influence of Misinformation Exposure, Political Ideology, and Flu Vaccine Acceptance on COVID-19 Vaccine Hesitancy" Vaccines 11, no. 3: 586. https://doi.org/10.3390/vaccines11030586
APA StyleRasul, M. E., & Ahmed, S. (2023). Not All Conservatives Are Vaccine Hesitant: Examining the Influence of Misinformation Exposure, Political Ideology, and Flu Vaccine Acceptance on COVID-19 Vaccine Hesitancy. Vaccines, 11(3), 586. https://doi.org/10.3390/vaccines11030586








